Abstract
Background
Heart failure is a common and growing health problem. Depression is prevalent among these patients and is associated with an increased risk of mortality, in some, but not all, studies. Depression may increase the risk of recurrent cardiac events and death, either through direct pathophysiological mechanisms such as thrombogenesis or ventricular arrhythmias, or through behavioural mechanisms. Depressed patients are less likely to adhere to their medication regimen and modify their lifestyle appropriately, thereby increasing the likelihood of recurrent cardiac events and death. The effects of psychological interventions for depression in terms of reducing depression and improving prognosis in patients with heart failure are unknown.
Objectives
To assess the effects of psychological interventions for depression in people with heart failure on depression and quality of life, morbidity, and mortality in these patients.
Search methods
We searched the Cochrane Central Register of Controlled Trials and The Database of Abstracts of Reviews of Effects on The Cochrane Library (Issue 3, 2003), MEDLINE (1951 to August 2003), PsycINFO (1887 to August 2003), CINAHL (1980 to August 2003) and EMBASE (1980 to August 2003). Searches of reference lists of retrieved papers were also made and expert advice was sought. Abstracts from national and international cardiology, psychology, and psychiatry conferences in 2003 and dissertation abstracts were also searched. All relevant foreign language papers were translated.
Selection criteria
RCTs of psychological interventions for depression in adults (18 years or older) with heart failure. The primary outcome was a significant reduction in depression. The secondary outcomes were the acceptability of treatment, quality of life, cardiac morbidity (hospital re‐admission for heart failure and non‐fatal cardiovascular events), reduction of cardiovascular behavioural risk factors, health economics, and death.
Data collection and analysis
Two reviewers independently screened titles and abstracts of potential studies. Two reviewers independently assessed the full papers for inclusion criteria. Further information was sought from the authors where papers contained insufficient information to make a decision about eligibility.
Main results
No RCTs of psychological interventions for depression in patients with heart failure were identified.
Authors' conclusions
Depression is common among patients with heart failure. Randomised controlled trials of psychological interventions for depression in heart failure patients are needed to investigate the impact of such interventions on depression, quality of life, behavioural CVD risk factors, cardiac morbidity, health economics and mortality, given the paucity of such trials in this area and the increasing prevalence of heart failure.
Plain language summary
Psychological interventions for depression in heart failure
It is not known whether psychological interventions for people with heart failure reduce symptoms of depression and improve outcome. Occasionally adults with heart failure suffer from depression. Psychological interventions, such as cognitive‐behavioural therapy and other types of counseling or supportive therapy, have been tried in order to reduce depression. Unfortunately, this review found no randomised trials of psychological interventions aimed at reducing depression in heart failure patients. Less carefully conducted studies, however, suggest that small reductions in the symptoms of depression and improvements in exercise capacity might result from psychological interventions.
Background
Heart failure is the end stage of all diseases of the heart and is a major cause of morbidity and mortality. The mortality associated with heart failure remains very high despite recent pharmacologic interventions that improve survival. The five‐year mortality rate following the first admission for heart failure exceeds that of all cancers with the exception of lung cancer (Davis 2000). The prevalence of heart failure in the population above the age of 45 years old in England is estimated to be about 3.1% (Davis 2000). The overall prevalence of heart failure is 3 to 20 per 1000 population, although among those aged 65 years and older this exceeds 100 people per 1000. The annual incidence of heart failure is 1 to 5 per 1000, although the relative incidence doubles for each decade of life after the age of 45 years. One reason for this increase may be medical advances in the management of acute myocardial infarction which have led to improved survival in patients, but with impaired cardiac function. This, in conjunction with the ageing population means that the overall incidence of heart failure is likely to increase in the future (Davis 2000). It is also estimated that heart failure accounts for about 5% of admissions to hospital medical wards, with over 100 000 admissions in the United Kingdom annually, constituting an increasing burden on resources, both personally for patients, and financially for health care services (Adams 1998).
The psychological sequelae of heart disease, particularly depression, have received increasing scrutiny in recent years. Indeed, some studies have reported that the presence of depression in patients with cardiovascular disease is associated with increased morbidity (Frasure‐Smith 1995) and both cardiovascular and all‐cause mortality (e.g. Barefoot 1996; Frasure‐Smith 1993), but not all (e.g. Lane 2001; Lane 2002; Mayou 2000). This may be due to indirect influences on health, such as poor self‐care behaviours in relation to diet, smoking (Anda 1990; Glassman 1990), decreased exercise participation (Stewart 1989), non‐adherence to medication (Carney 1995), and attendance at rehabilitation programmes (Blumenthal 1982), or more directly, by suppression of the immune response, thus leaving the patient open to opportunistic infection (Kiecolt‐Glaser 1992), or by increasing the likelihood of thrombogenic (Jern 1989), or arrhythmic events (Ahern 1990).
Depression in heart failure patients is also associated with a poorer prognosis (Faris 2002; Jiang 2001; Jiang 2002; Vaccarino 2001) and the mechanisms responsible may well be similar to those mentioned above. In the rat model of depression and heart failure, the response to rewarding brain electrical stimulation (a measure of anhedonia) is reduced in rats with heart failure. However, following acute treatment with etanercept, a tumor necrosis factor antagonist, circulating levels of tumor necrosis factor alpha decreased and response for electrical brain stimulation is restored (Grippo 2002). This supports the hypothesis that depression in heart failure may be directly mediated by cytokines. Of further interest is that depressed patients in the Systolic Hypertension in the Elderly Program (SHEP) were twice as likely as non‐depressed patients to develop heart failure which was not mediated by myocardial infarction (Abramson 2001). Moreover, patients with treated depression but no other risk factors for coronary heart disease have impaired arterial endothelial function but whether as a consequence of depression or drug treatment is unknown (Broadley 2002). Indeed, it is increasingly recognised that endothelial dysfunction plays a key role in atherogenesis. On the one hand, depression may precede the development of heart failure but on the other, the association may not be causal.
The study of psychological variables in patients with heart failure has been notably lacking. To date, eight studies have examined the prevalence of depression in patients with heart failure: six have assessed depressive symptomatology (Havranek 1999; Jiang 2001; Koenig 1998; Murberg 1999; Vaccarino 2001; Zuccala 1995) and four have assessed major depression (Faris 2002; Freedland 1991; Jiang 2001; Koenig 1998). The prevalence of depressive symptomatology ranged from 24% to 85% (Havranek 1999; Jiang 2001; Koenig 1998; Murberg 1999; Vaccarino 2001; Zuccala 1995); with major depression prevalent in 14% to 26% (Faris 2002, Freedland 1991, Jiang 2001, Koenig 1998). The variation in prevalence rates is almost certainly a function of varying sample sizes, selection criteria, and different methods of assessing depression. Of these eight studies, six have examined the influence of depression on mortality. One found a non‐significant increase in the mortality rate associated with major depression (Freedland 1991), one found that depression was not an independent risk factor for mortality (Koenig 1998), whilst the most recent studies (Faris 2002; Jiang 2001; Murberg 1999; Vaccarino 2001) reported that depression was a significant risk factor for death, even after controlling for disease severity. A recent RCT of six months of cognitive‐behavioural therapy (CBT) in depressed patients following myocardial infarction revealed a small but significant reduction in depression following the intervention compared to patients receiving usual care (Berkman 2003). However, CBT had no effect on reinfarction or mortality (Berkman 2003). A recent Cochrane review (Rees 2004) of psychological interventions for coronary heart disease patients revealed that stress management interventions did not significantly reduce total or cardiac mortality or revascularisation. However, psychological and stress management interventions did reveal small reductions in depression (Rees 2004). However, it is not yet known whether treating depression in heart failure patients would alter symptoms of depression or prognosis.
In addition, depression impacts on a patient's quality of life and that of his/her family. The association between depression and poor perceived quality‐of‐life in medically‐ill patients may be partly attributable to the impact of depression on impaired physical functioning (Mendes de Leon 1998). Evidence from the Medical Outcomes Study indicates that depressed patients without chronic medical conditions can have worse general health perceptions, physical, social, and role limitations, and report more bodily pain than non‐depressed patients with chronic medical conditions, such as heart disease (Wells 1989). In addition, chronic medical conditions also reduce physical activity and well‐being (Stewart 1989). Therefore, the co‐existence of depression and chronic medical conditions may be additive in their effect on both physical and social functioning (Penninx 1998; Wells 1989). Given the large number of people living with heart failure, the high prevalence of depressive symptomatology in this patient group and the associated poorer prognosis (Faris 2002; Jiang 2001; Murberg 1999; Vaccarino 2001), it is important to identify psychological interventions that have attempted to alleviate symptoms of depression.
Objectives
To determine the effects (both benefits and harms) of psychological interventions for treating depression in adults with heart failure on reducing depression.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) of any length of follow‐up and any language were included.
Types of participants
Adults (aged 18 years or older) with heart failure, defined as New York Heart Association (NYHA 1964) grade I to IV at rest or during exercise, with or without objective evidence of left ventricular dysfunction (i.e., echocardiography or radionuclide ventriculography) at rest (Cleland 1995), with depression were considered eligible for inclusion in this review. Depression was defined as either major depression (APACNS 1994) and/or depressive symptomatology (above or below a predefined cut‐off on the questionnaire employed in each study).
Types of interventions
All non‐pharmacological psychological interventions delivered by healthcare workers with specific training in these techniques were considered. These interventions included cognitive‐behavioural therapy (based on the definition employed by Jones 2001), psychotherapy (encompassing psychodynamic and interpersonal therapy and any psychological intervention described as non‐cognitive behavioural therapy), other psychosocial interventions (such as non‐directive counselling and supportive therapy and other 'talking therapies'), and interventions where participants were involved in educational, relaxation or exercise programmes. Trials, which used a combination of psychological intervention and exercise and/or education as the intervention unless they were compared with the psychological intervention alone, were excluded. Trials were only considered where the comparison group was usual care or no intervention.
Types of outcome measures
The primary outcome was a significant reduction in depression following the intervention. The secondary outcomes were the acceptability of treatment, assessed indirectly by the number of people who failed to complete the intervention; quality of life; hospital re‐admission for heart failure; non‐fatal cardiovascular events (stroke, myocardial infarction, angina pectoris, pulmonary embolism, peripheral arterial embolism, gastrointestinal embolism); behavioural cardiovascular disease (CVD) risk factor reduction (e.g., smoking, exercise, alcohol consumption, and compliance with medication); health economics (i.e., the financial gain to the health service by intervening) and death (cardiovascular and all‐cause mortality).
Search methods for identification of studies
We searched the Cochrane Central Register of Controlled Trials (CENTRAL) on The Cochrane Library (Issue 3, 2003), MEDLINE (1951 to August 2003), PsycINFO (1887 to August 2003), the Database of Abstracts of Reviews of Effectiveness (DARE) (The Cochrane Library issue 3, 2003), CINAHL (1980 to August 2003) and EMBASE (1980 to August 2003). Abstract books from national and international cardiology (European Society of Cardiology 2003 and American College of Cardiology 2003), psychology (Society for Behavioural Medicine and the Health Psychology conference), and psychiatry conferences (Royal College of Psychiatrists Annual Meeting 2003) were hand‐searched. Dissertation abstracts (UMI ProQuest Digital Dissertations, 1861 to August 2003) were also searched. All relevant foreign language papers were translated. Reference lists of all relevant papers were searched to identify other potentially relevant articles. We wrote to the lead author of all relevant reports and to investigators interested in heart failure to see if they knew of any additional published or unpublished studies that might be relevant to the review.
The following strategy was used to search CENTRAL and DARE databases on The Cochrane Library and adapted for use with the other databases (see Table 1 and Table 2), with the addition of a methodological filter to identify RCTs on MEDLINE (Dickersin 1994).
1. MEDLINE Search Strategy.
| Search strategy for MEDLINE (1951 to August 2003), CINAHL (1980 to August 2003), and EMBASE (1974 to August 2003) MeSH, EMTREE, AND CINAHL thesaurus terms for MEDLINE, EMBASE, and CINAHL databases, respectively, are in capitals and textwords are in lower case. Filters to identify clinical trials, controlled clinical trials, randomised controlled trials, and studies involving humans were also employed. 1HEART FAILURE CONGESTIVE 2(heart ADJ failure) 3(cardiac ADJ failure) 4VENTRICULAR DYSFUNCTION LEFT 5(ventricular ADJ dysfunction ADJ left) 61 OR 2 OR 3 OR 4 OR 5 7PSYCHOTHERAPY 8psychotherap$ 9(psycho$ WITH therap$) 10COUNSELING 11counsel$ 12COGNITIVE THERAPY 13(cognitive$ WITH therap$) 14(behavio$ WITH therap$) 15(psychodynamic WITH therap$) 16talk$ 17ipt 18psychol$ 19(non WITH pharmacolog$4) 207 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16 OR 17 OR 18 OR 19 21DEPRESSION 22DEPRESSIVE DISORDER 23DYSTHYMIC DISORDER 24depress$3 AND (symptom$ OR mood) 25(depress$3 WITH patient$2) 2621 OR 22 OR 23 OR 24 OR 25 2720 OR 26 2827 AND 6 |
2. Search Strategy for UMI ProQuest Digital Dissertations.
| Search strategy for UMI ProQuest Digital Dissertations We browsed all abstracts, titles, and keywords using the following search strategy. 1congestive heart failure 2heart failure 3cardiac failure 4ventricular dysfunction left 5#1 OR #2 OR #3 OR #4 6psychotherapy 7psychotherap? 8counseling 9counsel? 10cognitive therapy 11(cognitive? WITH therap?) 12(behavio? WITH therap?) 13(psychodynamic WITH therap?) 14talk? 15ipt 16psychol? 17(non WITH pharmacolog?) 18#6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 19depression 20depressive disorder 21dysthymic disorder 22depress? AND (symptom? OR mood) 23(depress? WITH patient?) 24#19 OR #20 OR #21 OR #22 OR #23 2518 OR 24 2625 AND 5 |
Cochrane Central Register of Controlled Trials (CENTRAL) and DARE
1 HEART FAILURE CONGESTIVE 2 (heart next failure) 3 (cardiac next failure) 4 VENTRICULAR DYSFUNCTION LEFT 5 (ventricular next dysfunction next left) 6 (#1 or #2 or #3 or #4 or #5) 7 PSYCHOTHERAPY 8 COUNSELING 9 Counsel* 10 (cognitive near therap*) 11 (behavi* near therap*) 12 psychotherap* 13 psych‐therap* 14 (#7 or #8 or #9 or #10 or #11 or #12 or #13) 15 depression 16 psycho* therap* 17 ipt 18 (non next pharmacolog*) 19 talk* 20 psychol* 21 (#15 or #16 or #17 or #18 or #19 or #20) 22 (#21 or #14) 23 DEPRESSION 24 DEPRESSIVE DISORDER 25 (depressed near patient*) 26 (depressive near symptom*) 27 psychosocial* 28 (#23 or #24 or #25 or #26 or #27) 29 (#14 or #21 or #28) 30 (#29 and #6)
MeSH terms are in capitals and textwords are in lower case.
Data collection and analysis
Selection of studies for inclusion/exclusion Two of the reviewers (AYC, DAL), independently selected suitable studies for inclusion/exclusion in this review as detailed below. A list of all titles and abstracts of studies, identified by searching electronic databases, was printed out excluding the author's names, institutions, and journal title, to minimise bias. If the title and abstract contained sufficient information to determine that the article did not meet the inclusion criteria, it was rejected. A record of all rejected papers and the reasons for rejection were documented.
The full papers of all remaining titles and abstracts deemed relevant were then retrieved and reviewed by two reviewers (AYC, DAL). In addition, all other potentially relevant articles identified by the various search strategies (reference checking, personal communications etc) were also reviewed. All relevant foreign language papers were translated into English. Where the two reviewers disagreed about the inclusion of a study, the third reviewer (GYHL) was asked to review the article. Disagreements were resolved by consensus of opinion. The reasons for exclusion are documented in the Table entitled "Characteristics of excluded studies".
The reviewers were unable to find any studies that fitted the inclusion criteria for this systematic review. However, the section below describes how data from studies, found in future updates of this review, would be extracted, assessed for quality, and analysed.
Data extraction For each trial, the following data would be extracted using paper data collection forms: participants (sample size, age, sex, ethnicity, marital status, NYHA grade of heart failure); type of depression (clinical diagnosis of major or minor depression, or depressive symptomatology assessed by questionnaire); type of assessment tool used to assess depression (questionnaire and/or structured interview); cut‐off used to indicate depression on each scale; the prevalence of depression and the mean (standard deviation) depression score; type and duration of the interventions (cognitive‐behavioural therapy, psychotherapy, 'talking/counselling' therapy, supportive therapy versus usual care or no intervention); primary and secondary outcomes; length of follow‐up; statistical methods employed; the effect size and its precision.
Critical appraisal of studies Two reviewers, blinded to the author's names, institutions and journal title, would independently assess the methodological quality of each trial in accordance with guidelines in the Cochrane Reviewers' Handbook (Clarke 2002). Each study would be assessed in terms of the randomisation process, allocation concealment (adequate, unclear, inadequate, or not used), degree of blinding, particularly of the outcome assessors, and patient attrition rate. The possibility of publication bias would be addressed by entering data from all selected trials into a funnel plot (size of study versus effect size).
Data Analysis Statistical analysis would be undertaken as follows: for continuous variables (e.g., changes on the depression scale), the weighted mean difference would be used and for dichotomous variables (e.g., either depressed or not depressed) the odds ratio with its associated 95% confidence intervals would be employed. As a summary measure of effectiveness, where possible, the number needed to treat (NNT) statistic would also be calculated. The results would also be analysed using both a fixed effect and random effects model.
In addition, the following subgroup analyses would be performed: men versus women and NYHA class II versus class III and IV. Further, sensitivity analyses would be employed to examine factors that may lead to differences between the results of individual trials: clinician diagnosis of depression versus validated questionnaire, and poor quality versus good quality trials.
Results
Description of studies
We found no studies that met our inclusion criteria.
Risk of bias in included studies
Not relevant as no completed studies were identified.
Effects of interventions
No RCTs of psychological interventions, aimed at reducing depression, in heart failure patients were identified. Over 700 potentially relevant publications were identified and screened for retrieval, although the majority were excluded on the basis of title and/or abstract, generally due to lack of suitability of study design or intervention. Only seven studies were retrieved for a more detailed evaluation but none met the inclusion criteria for this review. The QUOROM diagram (Figure 1) describes the reasons why these seven studies were excluded.
1.
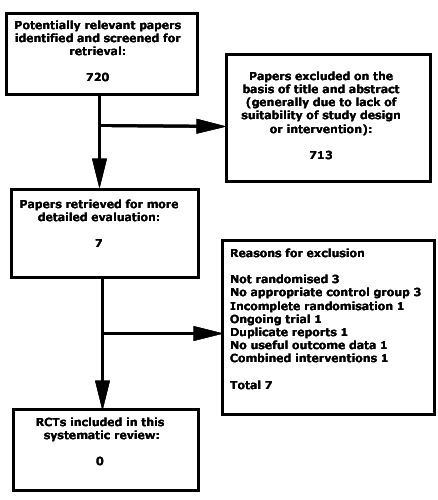
QUOROM statement flow diagram
Discussion
This review found no completed RCTs of psychological interventions for depression in patients with heart failure. Our search strategy included a comprehensive search of electronic databases, meticulous hand‐searching of relevant journal articles and abstracts and personal communication with experts in heart failure. Therefore, we believe that it is highly unlikely that we have simply 'missed' important studies.
Although there are no completed randomised controlled trials, observational data suggest that psychological interventions, either alone (Luskin 2002; McCraty 2002), or in combination with exercise and education (Kostis 1994), reduces depression in adults with heart failure. One study also revealed that non‐pharmacologic therapy (CBT, exercise and education) significantly improved exercise tolerance compared to pharmacological therapy with either digoxin or placebo (Kostis 1994) and reduced weight compared to those receiving digoxin (Kostis 1994). However, given the various methodological problems, particularly the extremely small sample sizes, with their associated lack of power, we advise caution in the interpretation of these results. Moreover, since the non‐pharmacologic intervention involved exercise therapy and dietary control in addition to CBT, it is not possible to identify which of these components lead to the improvement or whether it is the combination of therapies that is important.
Previous studies have shown that exercise improves mood (Byrne 1993; Milani 1996; Norris 1992) and reduces weight. In addition, a reduction in depression improves compliance with medication (Carney 1995) and reduces behavioural risk factors for CVD (Anda 1990; Blumenthal 1982; Glassman 1990). Given that these three elements often comprise standard cardiac rehabilitation programmes and appear to have beneficial effects on patient's mood, exercise capacity and weight (an important CVD risk factor), this setting would be a good place to conduct a RCT to investigate the benefits of psychological intervention alone, comprehensive cardiac rehabilitation (including psychological intervention) and usual care to identify which component is most important. Reduction in depression may also lead to a corresponding increase in quality of life.
This systematic review has highlighted the paucity of RCTs of psychological interventions aimed at ameliorating depression in adult patients with heart failure. This is disappointing given that several prospective studies have demonstrated a high prevalence of depression in this patient group (Faris 2002; Freedland 1991; Havranek 1999; Jiang 2001; Koenig 1998; Murberg 1999; Vaccarino 2001; Zuccala 1995) and an increased risk of mortality associated with depression, in some (Faris 2002; Jiang 2001; Murberg 1999; Vaccarino 2001), but not all studies (Freedland 1991; Koenig 1998). Observational studies of heart failure patients, despite the extremely small sample sizes studied, indicate that interventions (both stress management and CBT in combination with exercise and education) significantly reduce depression compared to controls (Kostis 1994; Luskin 2002; McCraty 2002). In addition, a recent Cochrane review (Rees 2004) revealed that psychological and stress management interventions also demonstrate small reductions in depression, however, stress management interventions did not appear to have any impact on reducing total or cardiac mortality, or the need for revascularisation (Rees 2004). Further, a recently published RCT of CBT for depression following myocardial infarction revealed a significant reduction in symptoms of depression after the intervention compared to usual care but no impact on mortality (Berkman 2003). The available evidence, based on observational studies (Kostis 1994; Luskin 2002; McCraty 2002) and two RCTs (Berkman 2003; Rees 2004) suggests that psychological and/or stress management interventions reduce symptoms of depression in patients with coronary heart disease (Berkman 2003; Kostis 1994; Luskin 2002; McCraty 2002; Rees 2004) but do not impact significantly on mortality (Berkman 2003; Rees 2004). Therefore, it is possible that depressed patients with heart failure would also benefit from CBT or some another type of psychological intervention aimed at reducing their symptoms of depression.
Authors' conclusions
Implications for practice.
None identified from this systematic review.
Implications for research.
This review highlights the need for a RCT of psychological interventions aimed at ameliorating depression in patients with heart failure. A recent RCT in depressed patients following myocardial infarction revealed a small but significant improvement in depression following a six‐month CBT intervention. Anecdotal evidence from prospective studies has identified depression as a significant problem for many heart failure patients with an associated greater risk of mortality, in some, but not all, studies. Although no RCTs were identified, observational studies suggest that psychological interventions in patients with heart failure do reduce symptoms of depression and improve exercise capacity. However, methodological weaknesses cast doubt on these findings and emphasise the importance of a RCT in this context.
What's new
| Date | Event | Description |
|---|---|---|
| 9 February 2021 | Review declared as stable | This Cochrane Review has been superseded by a review of a broader scope (CD013508). |
History
Protocol first published: Issue 4, 2001 Review first published: Issue 1, 2005
| Date | Event | Description |
|---|---|---|
| 9 April 2008 | Amended | Converted to new review format. |
| 1 November 2004 | New citation required and conclusions have changed | Review first published |
Acknowledgements
We would like to thank Margaret Burke (Cochrane Heart Group) for her help with developing and running the search strategy and Theresa Moore (Cochrane Heart Group) for her advice on the preparation of the review. We would also like to thank Jet Veldhuijzen van Zanten for translating.
AYC is funded by a Sandwell and West Birmingham Hospitals NHS Trust grant.
Characteristics of studies
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Hawthorne 1994 | Not a randomised controlled trial; no useful outcome data |
| Jaarsma 2003 | Ongoing trial; intervention not targeted at depression and depression is not assessed as an outcome |
| Konstam 1999 | Not a randomised controlled trial; no appropriate control group |
| Kostis 1994 | No appropriate control group; psychological intervention combined with exercise and education |
| Luskin 2002 | Incomplete randomisation |
| McCraty 2002 | Abstract version of the full paper by Luskin 2002; incomplete randomisation |
| Nelson 2001 | Not a randomised controlled trial; no appropriate control group |
Contributions of authors
All co‐reviewers were involved in the design of the protocol and provided critical comments about the manuscript. Deirdre Lane and Aun Yeong Chong selected studies for inclusion, abstracted data from the source papers, and wrote the first draft of the review. Gregory Lip obtained funding for the review and was the principal advisor.
Sources of support
Internal sources
Haemostatis, Thrombosis and Vascular Biology Unit, University Department of Medicine, City Hospital, Sandwell and West Birmingham Hospitals NHS Trust, UK
External sources
Supported in part by educational non‐promotional grants from Roche UK and Astra Zeneca, UK
Declarations of interest
None known
Stable (no update expected for reasons given in 'What's new')
References
References to studies excluded from this review
Hawthorne 1994 {published data only}
- Hawthorne MH, Hixon ME. Functional status, mood disturbance and quality of life in patients with heart failure. Progress in Cardiovascular Nursing 1994;9:22-32. [PubMed] [Google Scholar]
Jaarsma 2003 {published data only}
- Jaarsma T, Veldhuisen DJ. Effectiveness of heart failure clinics in the Netherlands: Research program set-up [Onderzoek opgezet naar het effect van hartfalenpoliklinieken in Nederland]. Nederlands Tijdschrift voor Geneeskunde 2003;147:513-4. [PubMed] [Google Scholar]
Konstam 1999 {published data only}
- Konstam V, Hurley L, Hijjazi K, Perry K, Konstam MA. Positive affect: A neglected group treatment outcome in assessing efficacy of psychosocial group interventions in individuals with heart failure. Group 1999;23:37-46. [Google Scholar]
Kostis 1994 {published data only}
- Kostis JB, Rosen RC, Cosgrove NM, Shindler DM, Wilson AC. Nonpharmacologic therapy improves functional and emotional status in congestive heart failure. Chest 1994;106:996-1001. [DOI] [PubMed] [Google Scholar]
Luskin 2002 {published data only}
- Luskin F, Reitz M, Newell K, Quinn TG, Haskell W. A controlled pilot study of stress management training of elderly patients with congestive heart failure. Preventive Cardiology 2002;5:168-172. [DOI] [PubMed] [Google Scholar]
McCraty 2002 {published data only}
- McCraty R. Effects of an emotional restructuring program on psychological functioning and functional capacity in patients with congestive heart failure. International Journal of Psychophysiology 2002;5:168-72. [Google Scholar]
Nelson 2001 {published data only}
- Nelson EA, Jordan DM, II. Preliminary results of a pilot program on depression in patients with congestive heart failure. Psychological Reports 2001;88:42-4. [DOI] [PubMed] [Google Scholar]
Additional references
Abramson 2001
- Abramson J, Berger A, Krumholz HM, Vaccarino V. Depression and risk of heart failure among older persons with isolated systolic hypertension. Archives of Internal Medicine 2001;161:1725-30. [DOI] [PubMed] [Google Scholar]
Adams 1998
- Adams KF, Zannad F. Clinical definition and etiology of advanced heart failure. American Heart Journal 1998;135:S204-S215. [DOI] [PubMed] [Google Scholar]
Ahern 1990
- Ahern DK, Gorkin L, Anderson JL, Tierney C, Hallstrom A, Ewart C, et al for the CAPS Investigators. Biobehavioural variables and mortality or cardiac arrest in the Cardiac Arrhythmias Pilot Study (CAPS). American Journal of Cardiology 1990;66:59-62. [DOI] [PubMed] [Google Scholar]
Anda 1990
- Anda RF, Williamson DF, Escobedo LG, Mast EE, Giovino GA, Remington PL. Depression and the dynamics of smoking: a national perspective. Journal of the American Medical Association 1990;264:1541-5. [PubMed] [Google Scholar]
APACNS 1994
- American Psychiatric Committee on Nomenclature and Statistics. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). 4th edition. Washington DC: American Psychiatric Association, 1994. [Google Scholar]
Barefoot 1996
- Barefoot JC, Helms MJ, Mark DB, Blumenthal JA, Califf RM, Haney TL et al. Symptoms of depression, acute myocardial infarction, and total mortality in a community sample. Circulation 1996;93:1976-80. [DOI] [PubMed] [Google Scholar]
Berkman 2003
- Berkman LF, Blumenthal J, Burg M, Carney RM, Catellier D, Cowan MJ et al. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. Journal of the American Medical Association 2003;289:3106-16. [DOI] [PubMed] [Google Scholar]
Blumenthal 1982
- Blumenthal JA, Williams RS, Wallace AG, Williams RB, Needles TL. Physiological and psychological variables predict compliance to prescribed exercise therapy in patients recovering from myocardial infarction. Psychosomatic Medicine 1982;44:519-27. [DOI] [PubMed] [Google Scholar]
Broadley 2002
- Broadley AJM, Korszun A, Jones CJH, Frenneaux MP. Arterial endothelial function is impaired in treated depression. Heart 2002;88:521-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Byrne 1993
- Byrne A, Byrne DG. The effect of exercise on depression, anxiety and other mood states. Journal of Psychosomatic Research 1993;37:565-74. [DOI] [PubMed] [Google Scholar]
Carney 1995
- Carney RM, Freedland KE, Eisen SA, Rich MW, Jaffe AS. Major depression and medication adherence in elderly patients with coronary artery disease. Health Psychology 1995;14:88-90. [DOI] [PubMed] [Google Scholar]
Clarke 2002
- Clarke M, Oxman A (ed). Cochrane Reviewers Handbook 4.1.5 [updated April 2002]. Vol. 2. Oxford: Update Software, 2002. [Google Scholar]
Cleland 1995
- Cleland JGF, Erdmann E, Ferrari R. Guidelines for the diagnosis of heart failure. The Task Force on Heart Failure of the European Society of Cardiology. European Heart Journal 1995;16:741-51. [PubMed] [Google Scholar]
Davis 2000
- Davis RC, Hobbs FDR, Lip GYH. ABC of heart failure: history and epidemiology. British Medical Journal 2000;320:39-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dickersin 1994
- Dickersin K, Scherer R, Lefebvre C. Identifying relevant studies for systematic reviews. British Medical Journal 1994;309:1286-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Faris 2002
- Faris R, Purcell H, Henein M, Coats A. Clinical depression is common and significantly associated with reduced survival in patients with non-ischaemic heart failure. European Journal of Heart Failure 2002;4:541-51. [DOI] [PubMed] [Google Scholar]
Frasure‐Smith 1993
- Frasure-Smith N, Lesperance F, Talajic M. Depression following myocardial infarction. Journal of the American Medication Association 1993;270:1819-25. [PubMed] [Google Scholar]
Frasure‐Smith 1995
- Frasure-Smith N, Lesperance F, Talajic M. The impact of negative emotions on prognosis following myocardial infarction: is it more than just depression? Health Psychology 1995;14:388-98. [DOI] [PubMed] [Google Scholar]
Freedland 1991
- Freedland KE, Carney RM, Rich MW, Caracciolo A, Krotenberg JA, Smith LJ et al. Depression in elderly patients with congestive heart failure. Journal of Geriatric Psychology 1991;24:59-71. [Google Scholar]
Glassman 1990
- Glassman AH, Helzer JE, Covey LS, Cottler LB, Stetner F, Tipp JE et al. Smoking, smoking cessation, and major depression. Journal of the American Medication Association 1990;264:1546-9. [PubMed] [Google Scholar]
Grippo 2002
- Grippo AJ, Francis J, Weiss RM, Felder RB, Johnson AK. Cytokine mediation of experimental heart failure-induced anhedonia. American Journal of Physiology - Regulatory, Integrative and Comparative Physiology 2002;284:R666-R673. [DOI] [PubMed] [Google Scholar]
Havranek 1999
- Havranek EP, Ware MG, Lowes BD. Prevalence of depression in congestive heart failure. American Journal of Cardiology 1999;84:348-50. [DOI] [PubMed] [Google Scholar]
Jern 1989
- Jern C, Erikksson E, Tengbom L, Risberg B, Wadenvik H, Jern S. Changes of plasma coagulation and fibrinolysis in response to mental stress. Thrombosis and Haemostasis 1989;62:767-71. [PubMed] [Google Scholar]
Jiang 2001
- Jiang W, Alexander J, Christopher E, Kuchibhatla M, Gaulden LH, Cuffe MS et al. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Archives of Internal Medicine 2001;161:1849-56. [DOI] [PubMed] [Google Scholar]
Jiang 2002
- Jiang W, Hasselbad V, Krishnan RR, O'Connor CM. Patients with CHF and depression have greater risk of mortality and morbidity than patients without depression. Journal of the American College of Cardiology 2002;39:919-21. [DOI] [PubMed] [Google Scholar]
Jones 2001
- Jones C, Cormac I, Mota J, Campbell C. Cognitive behaviour therapy for schizophrenia (Cochrane Review). The Cochrane Library 2001, Issue 2. [DOI] [PubMed] [Google Scholar]
Kiecolt‐Glaser 1992
- Kiecolt-Glaser JK, Glaser R. Psychoneuroimmunology: can psychological interventions modulate immunity? Journal of Consulting and Clinical Psychology 1992;60:569-75. [DOI] [PubMed] [Google Scholar]
Koenig 1998
- Koenig HG. Depression in hospitalized older patients with congestive heart failure. General Hospital Psychiatry 1998;20:29-43. [DOI] [PubMed] [Google Scholar]
Lane 2001
- Lane D, Carroll D, Ring C, Beevers DG, Lip GYH. Mortality and quality of life twelve months after myocardial infarction: effects of depression and anxiety. Psychosomatic Medicine 2001;63:221-30. [DOI] [PubMed] [Google Scholar]
Lane 2002
- Lane D, Carroll D, Ring C, Beevers DG, Lip GYH. In-hospital symptoms of depression do not predict mortality 3 years after myocardial infarction. International Journal of Epidemiology 2002;31:1179-82. [DOI] [PubMed] [Google Scholar]
Mayou 2000
- Mayou RA, Gill D, Thompson DR, Day A, Hicks N, Volmink J et al. Depression and anxiety as predictors of outcomes after myocardial infarction. Psychosomatic Medicine 2000;62:212-9. [DOI] [PubMed] [Google Scholar]
Mendes de Leon 1998
- Mendes de Leon CF, Krumholz HM, Seeman TS, Vaccarino V, Williams CS, Kasl SV et al. Depression and risk of coronary heart disease in elderly men and women. Archives of Internal Medicine 1998;158:2341-8. [DOI] [PubMed] [Google Scholar]
Milani 1996
- Milani RV, Lavie CJ, Cassidy MM. Effects of cardiac rehabilitation and exercise training programs on depression in patients after major coronary events. American Heart Journal 1996;132:726-32. [DOI] [PubMed] [Google Scholar]
Murberg 1999
- Murberg TA, Bru E, Svebak S, Tvetaras R, Aarsland T. Depressed mood and subjective symptoms as predictors of mortality in patients with congestive heart failure: A two-years follow-up study. International Journal of Psychiatry in Medicine 1999;29:311-26. [DOI] [PubMed] [Google Scholar]
Norris 1992
- Norris R, Carroll D, Cochrane R. The effects of physical activity and exercise training on psychological stress and well-being in an adolescent population. Journal of Psychosomatic Research 1992;36:55-65. [DOI] [PubMed] [Google Scholar]
NYHA 1964
- New York Heart Association. Diseases of the heart and blood vessels. Nomenclature and criteria for diagnosis. 6th edition. Boston: Little Brown, 1964. [Google Scholar]
Penninx 1998
- Penninx BWJH, Guralnik JM, Ferrucci L, Simonsick EM, Deeg DJH, Wallace RB. Depressive symptoms and physical decline in community-dwelling older persons. Journal of the American Medical Association 1998;279:1720-6. [DOI] [PubMed] [Google Scholar]
Rees 2004
- Rees K, Bennett P, West R, Davey Smith G, Ebrahim S. Psychological interventions for coronary heart disease (Cochrane Review). The Cochrane Library 2004, Issue 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stewart 1989
- Stewart AL, Greenfield S, Hays RD, Wells K, Rogers WH, Berry SD et al. Functional status and well-being of patients with chronic conditions: results from the Medical Outcomes Study. Journal of the American Medical Association 1989;262:907-13. [PubMed] [Google Scholar]
Vaccarino 2001
- Vaccarino V, Kasl SV, Abramson J, Krumholz HM. Depressive symptoms and risk of functional decline and death in patients with heart failure. Journal of the American College of Cardiology 2001;38:199-205. [DOI] [PubMed] [Google Scholar]
Wells 1989
- Wells KB, Stewart A, Hays RD, Burnam A, Rogers W, Daniels M et al. The functioning and well-being of depressed patients: results from the Medical Outcomes Study. Journal of the American Medical Association 1989;262:914-9. [PubMed] [Google Scholar]
Zuccala 1995
- Zuccala G, Cocchi A, Carbonin P. The impact of depression on self-perceived health status. Journal of the American Geriatric Society 1995;43:198-9. [DOI] [PubMed] [Google Scholar]


