Supplemental Digital Content is available in the text.
Keywords: early mobilization, intensive care, mechanical ventilation, patient monitoring, rehabilitation, respiratory therapy
Abstract
Objectives:
This scoping review is aimed to summarize current knowledge on respiratory support adjustments and monitoring of metabolic and respiratory variables in mechanically ventilated adult patients performing early mobilization.
Data Sources:
Eight electronic databases were searched from inception to February 2021, using a predefined search strategy.
Study Selection:
Two blinded reviewers performed document selection by title, abstract, and full text according to the following criteria: mechanically ventilated adult patients performing any mobilization intervention, respiratory support adjustments, and/or monitoring of metabolic/respiratory real-time variables.
Data Extraction:
Four physiotherapists extracted relevant information using a prespecified template.
Data Synthesis:
From 1,208 references screened, 35 documents were selected for analysis, where 20 (57%) were published between 2016 and 2020. Respiratory support settings (ventilatory modes or respiratory variables) were reported in 21 documents (60%). Reported modes were assisted (n = 11) and assist-control (n = 9). Adjustment of variables and modes were identified in only seven documents (20%). The most frequent respiratory variable was the Fio2, and only four studies modified the level of ventilatory support. Mechanical ventilator brand/model used was not specified in 26 documents (74%). Monitoring of respiratory, metabolic, and both variables were reported in 22 documents (63%), four documents (11%) and 10 documents (29%), respectively. These variables were reported to assess the physiologic response (n = 21) or safety (n = 13). Monitored variables were mostly respiratory rate (n = 26), pulse oximetry (n = 22), and oxygen consumption (n = 9). Remarkably, no study assessed the work of breathing or effort during mobilization.
Conclusions:
Little information on respiratory support adjustments during mobilization of mechanically ventilated patients was identified. Monitoring of metabolic and respiratory variables is also scant. More studies on the effects of adjustments of the level/mode of ventilatory support on exercise performance and respiratory muscle activity monitoring for safe and efficient implementation of early mobilization in mechanically ventilated patients are needed.
Early mobilization (EM) has been proposed as a promising intervention to counteract ICU-acquired weakness and to recover functional status (1). Even though EM has been extensively advocated, its benefits have remained elusive (2, 3). Clinical trials have described inconsistent effects on functional outcomes of mechanically ventilated patients who received EM (4–8). These results have been traditionally explained by a lack of knowledge on the optimal dosage of ICU mobilization (9–12) and by the use of inadequate functional outcome measures (3). Alternatively, during exercise, a mismatch between respiratory support and exercise-induced ventilatory demand may excessively increase work of breathing, limiting mobilization performance and eventually leading to fatigue (13).
Several respiratory support strategies (e.g., assisted or proportional modes) have been studied to improve patient-ventilator synchrony during stationary conditions (14, 15), but little is known about respiratory support during EM in the ICU. Ideally, mechanical ventilation adjustments during EM should increase physical therapy efficiency while avoiding excessive work of breathing and fatigue (16).
Expert recommendations for safe EM include monitoring of cardiovascular, respiratory, and neurologic variables (17). However, in contrast to the extensive knowledge of exercise physiology outside of the ICU (18), assessment of the physiologic response to EM in critically ill patients remains underexplored. Mechanically ventilated patients are usually those most closely monitored; this includes metabolic and respiratory variables currently available in modern mechanical ventilators and ICU monitors (e.g., indirect calorimetry and volumetric capnography) (19–21). The availability of real-time monitored variables could allow better decision-making on dosage of EM and could guide respiratory support adjustments according to exercise intensity in this setting.
Systematic reviews of EM in mechanically ventilated patients have only focused on safety, feasibility, effectiveness, and definitions of the interventions (12, 22–25), obviating the issue of ventilatory adjustments to cope with the additional ventilatory demand of exercise. Furthermore, although the Pain, Agitation/sedation, Delirium, Immobility/mobilization, and Sleep disruption 2018 guidelines recommend that mechanical ventilation should not be considered a barrier to mobility (26), there are no guidelines on ventilatory assistance adjustments during EM. Based on the recommendations for reviews, a scoping review emerged as the most appropriate first step to systematically address the issue of adjustment and monitoring of mechanical ventilation during EM (27).
The aim of this review is to summarize current knowledge on respiratory support adjustments and monitoring of metabolic and respiratory variables in mechanically ventilated adult patients performing EM.
MATERIALS AND METHODS
The research questions of this scoping review were as follows: “What respiratory support adjustments have been studied in mechanically ventilated adult patients performing EM in the ICU?” and “What metabolic and respiratory variables have been studied to monitor the physiologic response to EM in mechanically ventilated adult patients in the ICU?”
This scoping review was conducted using the Joanna Briggs Institute framework (28, 29) as initially conceived by Arksey and O’Malley (30). To preserve the quality of this review, the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews Checklist was used (31). This review was approved and registered by the Research and Clinical Trials Unit of Clínica Alemana de Santiago (register number: 2019–752). The methods details of this review were recently published elsewhere as a study protocol (32).
Operational Definitions
The operationalized relevant terms for this scoping review were defined for the selection, data extraction, and analysis (Table S1, Supplemental Digital Content 1, http://links.lww.com/CCX/A596), including terms such as “early mobilization intervention,” “respiratory support,” “ventilatory mode” and “respiratory variable”.
Search Strategy
A biomedical librarian (A.J.S.) and two critical care physiotherapists (F.G.-S., A.C.-M.) performed the search strategy combined keywords and medical subject headings for the concepts of “early mobilization”, “ICU” and “mechanical ventilation”. The original search included documents from inception (start of online availability) to November 2019, and the search strategy was adapted to the following eight relevant biomedical databases (Table S2, Supplemental Digital Content 2, http://links.lww.com/CCX/A596): PubMed (National Center for Biotechnology Information [NCBI]), Cumulative Index to Nursing and Allied Health Literature plus with full text (EBSCO), Rehabilitation and Sport Medicine (EBSCO), Scielo Citation Index (Clarivate), Epistemónikos, ClinicalTrials.gov, Cochrane Library (free access by the Chilean Ministry of Health), and Physiotherapy Evidence Database. In addition, a hand search was performed to identify the relevant titles from the reference lists of the documents identified in the eight-biomedical databases. A search update was performed in PubMed (NCBI) in February 2021 including references between November 2019 and February 2021 using the same original search strategy. The references identified in all sources were collected in EndNote (Clarivate Analytics, Boston, MA).
Eligibility Criteria
Inclusion and exclusion criteria for documents were defined based on the recommended Population, Concept, and Context method (27, 28). For the Population criterion, documents including adult patients on mechanical ventilation for at least 48 hours (including any ventilation through an endotracheal tube, tracheostomy tube, and/or noninvasive ventilation) were selected. For the Concept criterion (intervention), documents including any EM intervention performed by physiotherapy, nurse, and/or other allied-health professional were selected. For the Concept criterion (outcomes), documents reporting about respiratory support settings for the EM (including ventilatory mode or respiratory variable) or documents reporting any metabolic and/or respiratory variables used to monitor before, during, or after EM interventions were selected. For the Context criterion (studies), all types of English or Spanish scientific documents about critical care, including original studies, conference abstracts available in the same biomedical databases, reviews, clinical practice guidelines, expert recommendations, and protocols studies were selected. The exclusion criteria were documents including pediatric or neonatal population, animal models or in vitro studies, interventions initiated outside the ICU, only thoracic or respiratory physiotherapy interventions (e.g., inspiratory muscle training and airway clearance techniques), studies including only non–real-time metabolic or respiratory variables, full text not available, duplicates not eliminated automatically, and protocols of a study already included.
Document Selection
Screening and selection of documents were performed with the Covidence systematic review software (Veritas Health Innovation, Melbourne, VIC, Australia) (available at www.covidence.org). All references were imported from EndNote to Covidence, and once the duplicates were removed the document screening started. Two blinded reviewers to each other judgment (F.G.-S., A.C.-M.) screened independently by title and abstract all documents about EM on mechanically ventilated patients and accepted the documents according to the selection criteria previously described. The conflicts between reviewers were resolved with a third one (R.P-A) by consensus. If it was not possible to determine suitability for inclusion following title and abstract review, the reference was accepted and full text reviewed (33). An attempt was made to retrieve the full text of all accepted abstracts. If the accepted title or abstract existed only as such or as protocol study, the authors searched for its final publication. If full text was not found, the reference was excluded. Full text review was conducted to determine final eligibility by the same two authors blinded to each other judgment (F.G.-S., A.C.-M.).
Data Extraction and Analysis
Following the data extraction template previously designed by the researchers (32), four critical care physiotherapists (F.G.-S., A.C.-M., J.M., R.P.-A) extracted the variables and data from each selected document, including information from supplementary materials and appendices. The four reviewers met to determine by consensus if the information extracted was consistent. The following data were extracted from each selected document: bibliometric data (e.g., authors, year of publication, journal scope, document type), characteristics of the intervention (e.g., type of EM, type of respiratory support), and outcomes (e.g., respiratory support adjustments, metabolic, and respiratory variables). From each original study, the brand and model of mechanical ventilators and monitoring devices used were extracted, if available. The study design and the results of the measured metabolic and respiratory variables were also extracted from the original research documents. The discrepancies or uncertainties in the synthesis and analysis of information were discussed with a senior critical care physician (J.G.). The results were summarized descriptively as counts and percentages.
RESULTS
Data Synthesis and Documents Characteristics
This scoping review was performed within a 7-month period from November 2019 (bibliographic search) to May 2020 (data extraction and analysis), plus the search update conducted in February 2021. After removing duplicates, title and abstract screening was performed for 1,208 references. From 109 full text documents assessed for eligibility, 35 were selected for analysis (Fig. 1). Thirty-two original studies, two study protocols and one narrative review were selected, all of them in English. For study protocols, we extracted only the planning of metabolic and respiratory variables measuring, the brand/model of ventilators to be used, as well as the assistive rehabilitation equipment. References from the included narrative review that met the selection criteria had already been included as original articles, and there was no overlap. An overview of documents characteristics is summarized in Table 1.
Figure 1.
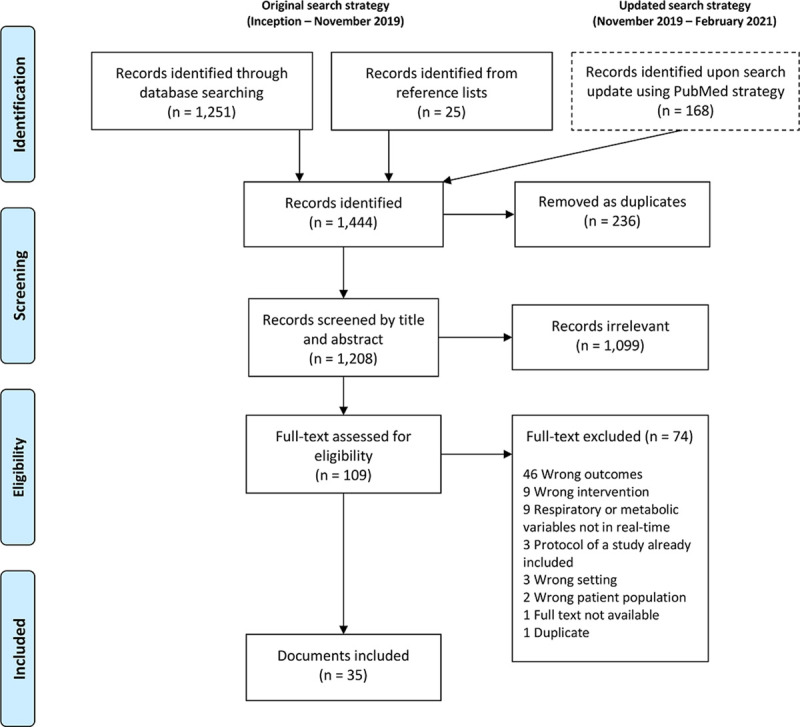
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram of documents selection process.
TABLE 1.
Overview of Included Documents Reporting the respiratory Support Adjustments and Monitoring of Mechanically Ventilated Patients on Early Mobilization
| Characteristics | N = 35, n (%) |
|---|---|
| Year of publication | |
| 2016–2020 | 20 (57) |
| 2011–2015 | 9 (26) |
| 2006–2010 | 4 (11) |
| Before 2006 | 2 (6) |
| Study design | |
| Observational study | 21 (60) |
| Clinical trial | 8 (23) |
| Cross-over study | 3 (9) |
| Study protocol | 2 (6) |
| Narrative review | 1 (3) |
| Journal scope | |
| Critical Care and Intensive Care Medicine | 12 (34) |
| Physical Therapy and Rehabilitation | 7 (20) |
| Medicine miscellaneous | 7 (20) |
| Pulmonary and Respiratory Medicine | 5 (14) |
| Anesthesiology | 2 (6) |
| Surgery | 1 (3) |
| ClinicalTrials.gov | 1 (3) |
| Respiratory support variables reported | |
| Reported ventilatory mode | 6 (17) |
| Reported respiratory variable | 6 (17) |
| Both ventilatory mode and respiratory variable | 9 (26) |
| Adjusted ventilatory variable | 7 (20) |
| Not reported | 14 (40) |
| Monitored variables reported | |
| Respiratory variables | 22 (63) |
| Metabolic variables | 4 (11) |
| Both respiratory and metabolic variables | 10 (29) |
| Not reported | 1 (3) |
| Reason to measure variables | |
| To assess physiologic response | 21 (60) |
| To assess safety response | 13 (37) |
| Not specified | 1 (3) |
EM Interventions
Based on the operational definitions used in this review, 10 types of EM interventions on mechanically ventilated patients were identified (Table S3, Supplemental Digital Content 3, http://links.lww.com/CCX/A596). The interventions were mostly leg/arm cycling (n = 18 [51%]) and progressive mobility (n = 14 [40%]).
Ventilatory Modes and Respiratory Variables Used During EM
From the 35 analyzed documents, 14 (40%) did not report any details on respiratory support used before, during, and/or after EM. All documents included patients with invasive mechanical ventilation (by endotracheal or tracheostomy tube), and none studied EM under noninvasive ventilation in the ICU. Respiratory support settings (ventilatory modes or respiratory variables) were reported in 21 documents (60%) (Table 2). Setting of both modes and variables were identified in only nine documents (26%). The ventilatory modes reported were assisted (n = 11) and assisted-controlled modes (n = 9). In addition, eight different respiratory variables were identified, mainly including Fio2 and pressure support level. Only seven studies reported adjustments or titration of respiratory support during EM (Table 3); five documents reported the Fio2 adjustment (13, 34, 47–49), and in only four documents, the level of pressure support was adjusted (13, 16, 34, 40). From the documents reporting the use of assisted modes (e.g., pressure support ventilation and proportional modes), cycling-off and inspiratory triggering were reported in one study (13). Only nine of 21 documents reporting ventilatory modes or respiratory variables specified the brand and model of the mechanical ventilator used.
TABLE 2.
Ventilatory Modes and Respiratory Variables on Early Mobilization of Mechanically Ventilated Adult Patientsa
| Respiratory Support | N = 21, n (%) |
|---|---|
| Ventilatory mode used during mobilization | |
| Assisted mode | 11 (52) |
| Pressure support (13, 16, 34–39) | 8 (38) |
| Pressure support, proportional assist ventilation, and neurally adjusted ventilatory assist (13) | 1 (5) |
| Not reported (40–42) | 3 (14) |
| Assist-control mode | 9 (43) |
| Volume (34, 39, 43) | 3 (14) |
| Pressure (44) | 1 (5) |
| Volume and pressure (36, 45, 46) | 3 (14) |
| Pressure, pressure-regulated volume control ventilation, and synchronized intermittent mandatory ventilation (37) | 1 (5) |
| Not reported (47) | 1 (5) |
| Respiratory variable reported during mobilization | |
| Fio2 (13, 34, 35, 47–51) | 8 (38) |
| Pressure support level (13, 16, 34, 35, 40) | 5 (24) |
| Positive end-expiratory pressure (35, 46) | 2 (11) |
| Inspiratory triggering (13) | 1 (5) |
| Cycling-off (13) | 1 (5) |
| Tidal volume (volume-controlled ventilation) (43) | 1 (5) |
| ECMO blood flow (49) | 1 (5) |
| ECMO sweep flow (49) | 1 (5) |
| Variables were not changed for early mobilization (44, 45, 52) | 3 (14) |
ECMO = extracorporeal membrane oxygenation.
aEach of the 21 documents reported one or more ventilatory modes and/or respiratory variable.
TABLE 3.
Summary of Studies in Which Mechanical Ventilator Were Adjusted During Early Mobilization
| References | Study Design | Sample | Type of Mobilization Intervention | Ventilatory Mode /Mechanical Ventilation Brand and Model | Respiratory Support Adjustments During Mobilization | Metabolic/Respiratory Real-Time Variables Measured |
|---|---|---|---|---|---|---|
| Black et al (40) | Observational study | 26 mechanically ventilated via tracheostomy from a medical-surgical ICU. | SOEOB, balance activities, standing, transferring and walking. Patients were encouraged to achieve their maximum functional level following the Functional Status Score for the ICU activities. | None specified | PS level adjustment.There were no Fio2 adjustments. | RR, VE, Vo2, Co2 production, and respiratory exchange ratio. |
| Akoumianaki et al (13) | Cross-over study | 10 mechanically ventilated from a medical-surgical ICU. Most patients had a tracheostomy. | Leg cycling (MOTOmed Letto 2; RECK-Technik, Betzenweiler, Germany): The intensity was selected according to a prior incremental workload test to determine the maximum resistance level capacity. Cycling started from passive mobilization and the resistance was gradually increased based on patient’s tolerance to cycle between 30 and 60 rpm. | Servo I, Maquet, Solna, Sweden PSV and NAVA Puritan Bennett 840, Covidien, Mansfield, MA: PSV and PAV+ |
PS level was set to attain Vt 6–8 mL/kg. The NAVA/PAV support was titrated to attain the same mean airway pressure that PSV.Flow triggering was set as the most sensitive possible evading autotriggering on PSV/PAV, and 0.5µV on NAVA.Cycling-off criterion was 25% (40% for chronic obstructive pulmonary disease) on PSV, 3 L/min on PAV and 70% on NAVA.PEEP remained at the same level and RR ≤ 30 beats/min.Fio2 was titrated to attain Spo2 > 95%. | Vo2, Vt, VE, Spo2, RR, and asynchrony index. |
| Kho et al (48) | Observational study | 33 mechanically ventilated from a medical-surgical ICU (96% via endotracheal tube and 4% via tracheostomy). | Leg cycling (RT-300 supine cycle; Restorative Therapies, Baltimore, MD): 30 min of leg cycling with an additional 1 min cool down, starting with passive cycling using 5 rpm. Patients were encouraged as much active cycling as possible using low resistance. | None specified | Fio2 was adjusted to attain Spo2 > 88%.The mean Fio2 used pre during and after cycling ranged from 37.3% to 38.8%. | Spo2 and asynchrony |
| Chen et al (16) | Observational study | 15 patients who were undergoing prolonged mechanical ventilation (between 24 and 114 mechanical ventilation days). | Upper extremity ergometer test (Active Passive Train, Tzora Co, Kibbutz Tzora, Israel) in upright bed position. Constant-load, symptom-limited exercise test with fixed resistance (approximately 10W) until intolerable shortness of breath, discomfort, or exhaustion. | PSV (brand/model not specified) | Ventilator mode was shifted from A/C to PSV.Three PS levels were titrated: baseline PS level, PS level +2 cm H2O, and PS level +4 cm H2O.PEEP and Fio2 were not changed throughout the study. | Spo2 and RR |
| Ko et al (49) | Observational study | 8 ECMO patients (one venoarterial ECMO and seven venovenous ECMO). | PROM, neuromuscular electrical stimulation, sitting in reclined bed or on SOEOB, strengthening using elastic band in sitting position, standing out of bed or marching in place with or without device, and assisted walking. | None specified | As needed during exercise, perfusionist and respiratory therapist performed ECMO and ventilatory management, respectively, including adjustments of Fio2, ECMO blood flow, and sweep gas flow. | Spo2, RR, and ECMO blood flow |
| Mah et al (34) | Clinical trial (quazi-experimental trial) | 28 mechanically ventilated from a surgical ICU. | Stepwise fashion based on physical assessment and clinical condition using a progressive five-level activity protocol ranged from PROM for unconscious patient to walking without assistance. | Volume-controlled ventilation and PSV (brand/model not specified) | Increased PS level or place on A/C starting 30 min before and continue 30 min after activity.Increased Fio2 by 20% before activityDefer weaning during mobility | None reported |
| Bailey et al (47) | Observational study | 103 patients with mechanical ventilation for > 4 d from a respiratory ICU. | Progressive mobility and walking including SOEOB without back support, sit in a chair after transfer from the hospital bed, and ambulate with or without assistance. | A/C (brand/model not specified) | A pre-/postactivity rest period with A/C for 30 min as needed.Fio2 was increased by 20% before initiation.Defer weaning during mobility. | Spo2 |
A/C = assist-control mode, ECMO = extracorporeal membrane oxygenation, NAVA = neurally adjusted ventilatory assist, PAV = proportional assist ventilation, PEEP = positive end-expiratory pressure, PROM = in-bed passive exercise, PS = pressure support, PSV = pressure support ventilation, RR = respiratory rate, SOEOB = sitting on the edge of the bed, Spo2 = pulse oximetry saturation, VE = minute ventilation, Vo2 = O2 consumption, Vt = tidal volume.
Respiratory and Metabolic Real-Time Variables Monitored on EM
Thirty-four documents reported real-time respiratory or metabolic monitoring before, during, and/or after EM interventions. The acquisition of the variables was through indirect calorimetry (n = 10 [29%]), bedside ICU monitor (n = 9 [26%]), pneumotachograph, or respiratory mechanics monitor (n = 3 [9%]), and 14 (42%) did not specify monitoring equipment brand or model used. Among 18 monitored variables, 11 were respiratory and seven metabolic (Table 4). Metabolic and respiratory monitoring was performed to assess the physiologic response in 21 documents (62%) and safety of EM in 13 (38%). Remarkably, no study assessed the work of breathing or respiratory effort using an esophageal balloon during EM.
TABLE 4.
Respiratory and Metabolic Real-Time Variables Monitored on Early Mobilization of Mechanically Ventilated Adult Patientsa
| Variables | To Assess Safety | To Assess Physiologic Response | Overall |
|---|---|---|---|
| N = 13, n (%) | N = 21, n (%) | N = 34, n (%) | |
| Respiratory rate | 9 (69) | 17 (81) | 26 (77) |
| Pulse oximetry saturation | 10 (77) | 12 (57) | 22 (65) |
| O2 consumption | 9 (43) | 9 (27) | |
| Co2 production | 8 (38) | 8 (24) | |
| Tidal volume | 8 (38) | 8 (24) | |
| Energy expenditure | 5 (24) | 5 (15) | |
| Minute ventilation | 4 (19) | 4 (12) | |
| Respiratory exchange ratiob | 3 (14) | 3 (9) | |
| Asynchrony index | 2 (16) | 1 (5) | 3 (9) |
| Rapid shallow breathing index | 1 (8) | 1 (5) | 2 (6) |
| Inspiratory time | 1 (5) | 1 (3) | |
| Expiratory time | 1 (5) | 1 (3) | |
| Peak inspiratory pressure | 1 (5) | 1 (3) | |
| End-tidal Co2 | 1 (5) | 1 (3) | |
| Extracorporeal membrane oxygenation blood flow | 1 (8) | 1 (3) | |
| Oxyhemoglobin (NIRS) | 1 (5) | 1 (3) | |
| Deoxyhemoglobin (NIRS) | 1 (5) | 1 (3) | |
| Tissue O2 saturation (NIRS) | 1 (5) | 1 (3) |
NIRS = near infrared spectroscopy.
aEach of the 34 documents reported one or more variables.
bAlso reported as respiratory quotient.
A summary of the metabolic and respiratory variables monitored in each document is presented in Table S4 (Supplemental Digital Content 4, http://links.lww.com/CCX/A596).
DISCUSSION
This is the first review on respiratory support adjustments and monitoring in mechanically ventilated patients performing EM. Regarding the first research question, 60% of documents informed about ventilatory modes and respiratory variables, and 25% reported the brand and model of the mechanical ventilators used. In addition, adjustments or titration of respiratory support during EM were identified in only seven documents. Regarding the second research question, 97% of documents assessed metabolic and/or respiratory variables; however, 40% of them did not specify the device used to acquire these variables in real time.
The increasing number of publications identified between 2016 and 2020 suggests a growing interest in EM of mechanically ventilated patients. However, active mobilization in patients with an endotracheal tube or tracheostomy has been infrequently reported in 1-day prevalence studies worldwide (53–57). This can be explained by deep sedation during mechanical ventilation (57) and because not all intubated patients need EM. Intense mobilization strategies to minimize muscle weakness and rest-effects should start as early as possible, focusing on patients who will likely require prolonged invasive mechanical ventilation (58–60). Most of the EM interventions identified in this review were in-bed and low intensity activities. These interventions were performed mostly using assistive rehabilitation equipment, which allow EM when out-of-bed mobility is unfeasible and as a progressive mobility aid (61). For example, Medrinal et al (35) reported that functional electrical stimulation cycling increases oxygen uptake of the vastus lateralis muscle and cardiac output in sedated mechanically ventilated patients. From a monitoring perspective, Akoumianaki et al (13) reported that awake mechanically ventilated patients increase oxygen consumption (Vo2) and Co2 production (Vco2) when performing active cycling. In mechanically ventilated patients, mobilization could therefore lead to insufficient respiratory support or asynchrony due to unmet ventilatory demand, either in sedated (44) or awake (13) patients, particularly if weak (16).
The prevalence of asynchronies remains high in critically ill patients during stationary conditions (62, 63); ideally asynchronies should be managed adjusting respiratory support rather than increasing sedation (64, 65). This review identified 15 documents describing respiratory support variables for EM, including Fio2 (13, 34, 35, 47–51), pressure support level (13, 16, 34, 35, 40), positive end-expiratory pressure (13, 35), inspiratory triggering, and cycling-off (13). However, most of the documents using assisted modes did not report the nature of these adjustments, and none reported inspiratory time or inspiratory rise time during EM (66). If these adjustments are vital to minimize asynchronies and excessive work of breathing during assisted ventilation at rest (64), their relevance should be even more under conditions of variable ventilatory demand (44).
During exercise, increased whole body Vo2 and Vco2 must be coupled to increased minute ventilation and work of breathing; however, during sustained exercise, work of breathing and the proportion of whole body oxygen consumed by the respiratory muscles exponentially rises (67). Interestingly, exercise physiology has shown a competitive blood flow distribution between respiratory and locomotor muscles (18, 68, 69). In healthy volunteers, Harms et al (68) demonstrated that respiratory muscle unloading using proportional assist ventilation during cycling increased leg blood flow and regional Vo2, whereas the opposite effect was induced by resistive respiratory muscle loading. Twenty years later, Dominelli et al (69) assessed work of breathing and blood flow to respiratory and locomotor muscles during submaximal exercise under spontaneous, assisted, and loaded ventilation. Work of breathing was positively correlated to respiratory muscle blood flow and negatively correlated to locomotor blood flow. In fact, respiratory muscle unloading using proportional assist ventilation in healthy subjects markedly reduced the rate of rise of respiratory and limb discomfort perception, extending time to exhaustion by 14% (70). Furthermore, in congestive heart failure outpatients performing constant-load exercise, inspiratory pressure support not only decreased work of breathing and the rate of rise in respiratory effort but increased exercise endurance by 40% (71). In other words, decreasing the work of breathing by adequate respiratory support can improve peripheral muscle performance in healthy individuals and likely in ICU patients. Within this scoping review, only four studies reported ventilatory support adjustments during active exercise (13, 16, 34, 40). For example, Chen et al (16) were able to extend arm cycling duration and tolerance increasing pressure support level in patients with documented respiratory weakness, and Akoumianaki et al (13) were able to improve exercise efficiency switching from pressure support ventilation to proportional modes during leg cycling in chronically critically ill patients. Then, by efficiently alleviating respiratory muscle work, longer duration and/or intensity of exercise should be feasible.
From a technical perspective, it is remarkable that 25% of the published documents reported the brand and model of the mechanical ventilators used. This information is specially important when using assisted modes; Thille et al (72) reported that the performance of inspiratory trigger, pressurization capacity, and expiratory resistance differs considerably across new-generation ventilators. If ventilators may still have difficulties in providing adequate support during stationary conditions (72, 73), technical sources of mismatch between patient demand and respiratory support could be magnified during EM. This phenomenon could be more relevant in weak patients due to prolonged ventilation and when the level of sedation is reduced.
Respiratory support adjustments are generally used to minimize ventilation-induced lung injury (74), improve oxygenation (75), decrease asynchronies (64), avoid disproportionate work of breathing (76), and promote weaning (77). Real-time ICU monitoring should provide information to guide respiratory support adjustments during both stationary and nonstationary conditions (78). Monitoring of metabolic and respiratory variables identified in this review was used to assess physiologic response (n = 21) and as safety measurements to start or stop EM (n = 13). However, no document reported ventilatory adjustment based on the interpretation of these variables. Additionally, no document reported monitoring of variables related to work of breathing or respiratory effort during EM (e.g., using esophageal balloon or electrical activity of the diaphragm). Measuring these mechanical variables could not only allow to adjust respiratory support and/or exercise intensity but also to avoid the potential of exercise-inflicted lung injury during EM as an extension of the concept of patient self-inflicted lung injury at rest (79).
Safety assessment of EM using ICU monitoring has been studied extensively (17, 80). This review highlights the incorporation of metabolic variables to assess the physiologic response to exercise in patients on invasive mechanical ventilation. The use of indirect calorimetry in the ICU setting allows to measure Vo2, Vco2, energy expenditure, and respiratory exchange ratio (20). According to the available evidence, passive mobilization does not generate significant changes in the metabolism of sedated and ventilated patients compared with active mobilization (35, 41, 42, 81, 82). Due to changes in sedation practices of recent years, patients may wake up earlier anticipating active mobilization in those who still require mechanical ventilation (26). This challenges mobilization teams to adjust the exercise dose and/or respiratory support, incorporating the interpretation of respiratory and metabolic real-time monitoring during EM.
This scoping review has limitations that deserve to be explained. Although an exhaustive search and selection process was conducted, given the novelty of the topic, some studies may have been inadvertently lost. To compensate, a hand search was performed to include documents that were not identified in the eight selected databases. Based on the selection criteria, some documents that monitored EM through metabolic and respiratory variables were not included because these variables were not measured in real time. This criterion was chosen to identify variables that are readily available for decision-making during EM. This scoping review did not include studies on exercise of mechanically ventilated patients in non-ICU settings. Unexpectedly, no EM studies were identified in ICU patients under noninvasive ventilation. Therefore, findings of this review only pertain to patients with invasive ventilation in the ICU setting.
Future research on EM should specify the devices used (e.g., mechanical ventilators, monitoring equipment) and the adjustments used before (baseline), during, and after mobilization. Based on the findings of this review, no recommendations can be yet defined for respiratory adjustments in mechanically ventilated patients who perform EM, but it is likely that more attention should be given to the level/mode of ventilatory support rather than just focusing on the amount of oxygen delivered. If there is still controversy on ventilatory settings during the initial stage of protective ventilation and weaning, the choice of adequate respiratory support during EM to avoid respiratory muscle overload and improve exercise performance may be even a greater challenge. Further research is required to identify variables to balance exercise dosing (intensity, frequency, type, and duration) and respiratory support adjustment during EM. In this review, specific respiratory adjustments and settings for EM were identified. However, we found no study reporting respiratory adjustments during mobilization based on available real-time metabolic or respiratory monitoring. This review only reports information available in the literature but not necessarily in clinical practice. A point prevalence study could be a next step to identify if ventilator variables are adjusted during EM or to describe detailed ventilator information during EM sessions.
CONCLUSIONS
Little information on respiratory support adjustments during EM of mechanically ventilated patients was identified. Furthermore, the vast majority of documents identified did not specify the mechanical ventilator used. The most frequent adjustment was to increase the Fio2 rather than the level or mode of ventilatory support. Monitoring of metabolic and respiratory variables is also scant, and nearly half of them did not specify the monitoring devices used; remarkably, no study assessed the work of breathing or respiratory effort during mobilization. More studies on the effects of adjustments of ventilatory support on exercise performance and respiratory muscle activity monitoring for safe and efficient implementation of EM in mechanically ventilated patients are needed.
Supplementary Material
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccejournal).
The authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Zhang L, Hu W, Cai Z, et al. Early mobilization of critically ill patients in the intensive care unit: A systematic review and meta-analysis. PLoS One. 2019; 14:e0223185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Waldauf P, Jiroutková K, Krajčová A, et al. Effects of rehabilitation interventions on clinical outcomes in critically ill patients: Systematic review and meta-analysis of randomized controlled trials. Crit Care Med. 2020; 48:1055–1065 [DOI] [PubMed] [Google Scholar]
- 3.Castro-Avila AC, Serón P, Fan E, et al. Effect of early rehabilitation during intensive care unit stay on functional status: Systematic review and meta-analysis. PLoS One. 2015; 10:e0130722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morris PE, Berry MJ, Files DC, et al. Standardized rehabilitation and hospital length of stay among patients with acute respiratory failure: A randomized clinical trial. JAMA. 2016; 315:2694–2702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moss M, Nordon-Craft A, Malone D, et al. A randomized trial of an intensive physical therapy program for patients with acute respiratory failure. Am J Respir Crit Care Med. 2016; 193:1101–1110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wright SE, Thomas K, Watson G, et al. Intensive versus standard physical rehabilitation therapy in the critically ill (EPICC): A multicentre, parallel-group, randomised controlled trial. Thorax. 2018; 73:213–221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schaller SJ, Anstey M, Blobner M, et al. ; International Early SOMS-guided Mobilization Research Initiative. Early, goal-directed mobilisation in the surgical intensive care unit: A randomised controlled trial. Lancet. 2016; 388:1377–1388 [DOI] [PubMed] [Google Scholar]
- 8.Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: A randomised controlled trial. Lancet. 2009; 373:1874–1882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stiller K. Physiotherapy in intensive care: An updated systematic review. Chest. 2013; 144:825–847 [DOI] [PubMed] [Google Scholar]
- 10.Hodgson CL, Capell E, Tipping CJ. Early mobilization of patients in intensive care: Organization, communication and safety factors that influence translation into clinical practice. Crit Care. 2018; 22:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Winkelman C, Sattar A, Momotaz H, et al. Dose of early therapeutic mobility: Does frequency or intensity matter? Biol Res Nurs. 2018; 20:522–530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clarissa C, Salisbury L, Rodgers S, et al. Early mobilisation in mechanically ventilated patients: A systematic integrative review of definitions and activities. J Intensive Care. 2019; 7:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Akoumianaki E, Dousse N, Lyazidi A, et al. Can proportional ventilation modes facilitate exercise in critically ill patients? A physiological cross-over study: Pressure support versus proportional ventilation during lower limb exercise in ventilated critically ill patients. Ann Intensive Care. 2017; 7:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moerer O. Effort-adapted modes of assisted breathing. Curr Opin Crit Care. 2012; 18:61–69 [DOI] [PubMed] [Google Scholar]
- 15.Wrigge H, Reske AW. Patient-ventilator asynchrony: Adapt the ventilator, not the patient! Crit Care Med. 2013; 41:2240–2241 [DOI] [PubMed] [Google Scholar]
- 16.Chen YH, Lin HL, Hsiao HF, et al. Effects of an additional pressure support level on exercise duration in patients on prolonged mechanical ventilation. J Formos Med Assoc. 2015; 114:1204–1210 [DOI] [PubMed] [Google Scholar]
- 17.Hodgson CL, Stiller K, Needham DM, et al. Expert consensus and recommendations on safety criteria for active mobilization of mechanically ventilated critically ill adults. Crit Care. 2014; 18:658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sheel AW, Boushel R, Dempsey JA. Competition for blood flow distribution between respiratory and locomotor muscles: Implications for muscle fatigue. J Appl Physiol (1985). 2018; 125:820–831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cheifetz IM, Myers TR. Respiratory therapies in the critical care setting. Should every mechanically ventilated patient be monitored with capnography from intubation to extubation? Respiratory care. 2007; 52:423–438 [PubMed] [Google Scholar]
- 20.De Waele E, Honore PM, Spapen HD. New generation indirect calorimeters for measuring energy expenditure in the critically ill: A rampant or reticent revolution? Crit Care. 2016; 20:138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sundström M, Tjäder I, Rooyackers O, et al. Indirect calorimetry in mechanically ventilated patients. A systematic comparison of three instruments. Clin Nutr. 2013; 32:118–121 [DOI] [PubMed] [Google Scholar]
- 22.Tipping CJ, Harrold M, Holland A, et al. The effects of active mobilisation and rehabilitation in ICU on mortality and function: A systematic review. Intensive Care Med. 2017; 43:171–183 [DOI] [PubMed] [Google Scholar]
- 23.Reid JC, Unger J, McCaskell D, et al. Physical rehabilitation interventions in the intensive care unit: A scoping review of 117 studies. J Intensive Care. 2018; 6:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li Z, Peng X, Zhu B, et al. Active mobilization for mechanically ventilated patients: A systematic review. Arch Phys Med Rehabil. 2013; 94:551–561 [DOI] [PubMed] [Google Scholar]
- 25.Ding N, Zhang Z, Zhang C, et al. What is the optimum time for initiation of early mobilization in mechanically ventilated patients? A network meta-analysis. PLoS One. 2019; 14:e0223151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Devlin JW, Skrobik Y, Gélinas C, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2018; 46:e825–e873 [DOI] [PubMed] [Google Scholar]
- 27.Munn Z, Peters MDJ, Stern C, et al. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018; 18:143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peters MD, Godfrey CM, Khalil H, et al. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015; 13:141–146 [DOI] [PubMed] [Google Scholar]
- 29.The Joanna Briggs Institute. The Joanna Briggs Institute. Reviewers’ Manual 2015: Methodology for JBI Scoping Reviews. 2015, Adelaide, South Australia: The Joanna Briggs Institute; 1–24 [Google Scholar]
- 30.Arksey H, O’Malley L. Scoping studies: Towards a methodological framework. Int J Soc Res Methodol Theory Pract. 2005; 8:19–32 [Google Scholar]
- 31.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. 2018; 169:467–473 [DOI] [PubMed] [Google Scholar]
- 32.González-Seguel F, Camus-Molina A, Jasmén Sepúlveda A, et al. Settings and monitoring of mechanical ventilation during physical therapy in adult critically ill patients: Protocol for a scoping review. BMJ Open. 2019; 9:e030692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration; 2011. Available at: http://www.cochrane-handbookorg. Accessed May 26, 2015
- 34.Mah JW, Staff I, Fichandler D, et al. Resource-efficient mobilization programs in the intensive care unit: Who stands to win? Am J Surg. 2013; 206:488–493 [DOI] [PubMed] [Google Scholar]
- 35.Medrinal C, Combret Y, Prieur G, et al. Comparison of exercise intensity during four early rehabilitation techniques in sedated and ventilated patients in ICU: A randomised cross-over trial. Crit Care. 2018; 22:110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hickmann CE, Castanares-Zapatero D, Bialais E, et al. Teamwork enables high level of early mobilization in critically ill patients. Annals of Intensive Care. 2016; 6:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Genc A, Koca U, Gunerli A. What are the hemodynamic and respiratory effects of passive limb exercise for mechanically ventilated patients receiving low-dose vasopressor/inotropic support? Crit Care Nurs Q. 2014; 37:152–158 [DOI] [PubMed] [Google Scholar]
- 38.Hickmann CE, Roeseler J, Castanares-Zapatero D, et al. Energy expenditure in the critically ill performing early physical therapy. Int Care Med. 2014; 40:548–555 [DOI] [PubMed] [Google Scholar]
- 39.Gerovasili V, Tripodaki E, Karatzanos E, et al. Short-term systemic effect of electrical muscle stimulation in critically ill patients. Chest. 2009; 136:1249–1256 [DOI] [PubMed] [Google Scholar]
- 40.Black C, Grocott M, Singer M. The oxygen cost of rehabilitation interventions in mechanically ventilated patients: An observational study. Physiotherapy. 2020; 107:169–175 [DOI] [PubMed] [Google Scholar]
- 41.Collings N, Cusack R. A repeated measures, randomised cross-over trial, comparing the acute exercise response between passive and active sitting in critically ill patients. BMC Anesthesiol. 2015; 15:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nydahl P, Schuchhardt D, Jüttner F, et al. Caloric consumption during early mobilisation of mechanically ventilated patients in intensive care units. Clin Nutr. 2020; 39:2442–2447 [DOI] [PubMed] [Google Scholar]
- 43.Santos LMH, Novaes APL de, Dantas FM de NA, et al. Acute effect of passive cycloergometry on the cardiovascular system and respiratory mechanics of critically ill patients: A randomized controlled trial. Fisioterapia em Movimento. 2019; 32:1–10 [Google Scholar]
- 44.Silva JR, Reboredo MM, Bergamini BC, et al. Impact of early passive exercise with cycle ergometer on ventilator interaction. Respir Care. 2020; 65:1547–1554 [DOI] [PubMed] [Google Scholar]
- 45.Camargo Pires-Neto R, Fogaça Kawaguchi YM, Sayuri Hirota A, et al. Very early passive cycling exercise in mechanically ventilated critically ill patients: Physiologic and safety aspects - a case series. Plos One. 2013; 8:e74182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chang MY, Chang LY, Huang YC, et al. Chair-sitting exercise intervention does not improve respiratory muscle function in mechanically ventilated ICU patients. Respir Care. 2011; 56:1533–1538 [DOI] [PubMed] [Google Scholar]
- 47.Bailey P, Thomsen GE, Spuhler VJ, et al. Early activity is feasible and safe in respiratory failure patients. Crit Care Med. 2007; 35:139–145 [DOI] [PubMed] [Google Scholar]
- 48.Kho ME, Molloy AJ, Clarke FJ, et al. ; Canadian Critical Care Trials Group. TryCYCLE: A prospective study of the safety and feasibility of early in-bed cycling in mechanically ventilated patients. PLoS One. 2016; 11:e0167561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ko Y, Cho YH, Park YH, et al. Feasibility and safety of early physical therapy and active mobilization for patients on extracorporeal membrane oxygenation. ASAIO J. 2015; 61:564–568 [DOI] [PubMed] [Google Scholar]
- 50.Chang AT, Boots RJ, Hodges PW, et al. Standing with the assistance of a tilt table improves minute ventilation in chronic critically ill patients. Arch Phys Med Rehabil. 2004; 85:1972–1976 [DOI] [PubMed] [Google Scholar]
- 51.Zafiropoulos B, Alison JA, McCarren B. Physiological responses to the early mobilisation of the intubated, ventilated abdominal surgery patient. Aust J Physiother. 2004; 50:95–100 [DOI] [PubMed] [Google Scholar]
- 52.Pohlman MC, Schweickert WD, Pohlman AS, et al. Feasibility of physical and occupational therapy beginning from initiation of mechanical ventilation. Crit Care Med. 2010; 38:2089–2094 [DOI] [PubMed] [Google Scholar]
- 53.Sibilla A, Nydahl P, Greco N, et al. Mobilization of mechanically ventilated patients in Switzerland. J Intensive Care Med. 2020; 35:55–62 [DOI] [PubMed] [Google Scholar]
- 54.Tadyanemhandu C, van Aswegen H, Ntsiea V. Organizational structures and early mobilization practices in South African public sector intensive care units-A cross-sectional study. J Eval Clin Pract. 2021; 27:42–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Timenetsky KT, Neto AS, Assunção MSC, et al. ; e-MOTION group. Mobilization practices in the ICU: A nationwide 1-day point- prevalence study in Brazil. PLoS One. 2020; 15:e0230971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nydahl P, Ruhl AP, Bartoszek G, et al. Early mobilization of mechanically ventilated patients: A 1-day point-prevalence study in Germany. Crit Care Med. 2014; 42:1178–1186 [DOI] [PubMed] [Google Scholar]
- 57.Jolley SE, Moss M, Needham DM, et al. ; Acute Respiratory Distress Syndrome Network Investigators. Point prevalence study of mobilization practices for acute respiratory failure patients in the United States. Crit Care Med. 2017; 45:205–215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rak KJ, Ashcraft LE, Kuza CC, et al. Effective care practices in patients receiving prolonged mechanical ventilation. An ethnographic study. Am J Respir Crit Care Med. 2020; 201:823–831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Schreiber AF, Ceriana P, Ambrosino N, et al. Physiotherapy and weaning from prolonged mechanical ventilation. Respir Care. 2019; 64:17–25 [DOI] [PubMed] [Google Scholar]
- 60.Dunn H, Quinn L, Corbridge SJ, et al. Mobilization of prolonged mechanical ventilation patients: An integrative review. Heart Lung. 2017; 46:221–233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mayer KP, Carper RA, Henson SC, et al. Three-fourths of ICU physical therapists report use of assistive equipment and technology in practice. J Acute Care Physical Therapy. 2020. Jun. [online ahead of print] [Google Scholar]
- 62.Blanch L, Villagra A, Sales B, et al. Asynchronies during mechanical ventilation are associated with mortality. Intensive Care Med. 2015; 41:633–641 [DOI] [PubMed] [Google Scholar]
- 63.Murias G, Lucangelo U, Blanch L. Patient-ventilator asynchrony. Curr Opin Crit Care. 2016; 22:53–59 [DOI] [PubMed] [Google Scholar]
- 64.Subirà C, de Haro C, Magrans R, et al. Minimizing asynchronies in mechanical ventilation: Current and future trends. Respir Care. 2018; 63:464–478 [DOI] [PubMed] [Google Scholar]
- 65.de Haro C, Magrans R, López-Aguilar J, et al. ; Asynchronies in the Intensive Care Unit (ASYNICU) Group. Effects of sedatives and opioids on trigger and cycling asynchronies throughout mechanical ventilation: An observational study in a large dataset from critically ill patients. Crit Care. 2019; 23:245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Murata S, Yokoyama K, Sakamoto Y, et al. Effects of inspiratory rise time on triggering work load during pressure-support ventilation: A lung model study. Respir Care. 2010; 55:878–884 [PubMed] [Google Scholar]
- 67.Aaron EA, Johnson BD, Seow CK, et al. Oxygen cost of exercise hyperpnea: Measurement. J Appl Physiol (1985). 1992; 72:1810–1817 [DOI] [PubMed] [Google Scholar]
- 68.Harms CA, Babcock MA, McClaran SR, et al. Respiratory muscle work compromises leg blood flow during maximal exercise. J Appl Physiol (1985). 1997; 82:1573–1583 [DOI] [PubMed] [Google Scholar]
- 69.Dominelli PB, Archiza B, Ramsook AH, et al. Effects of respiratory muscle work on respiratory and locomotor blood flow during exercise. Exp Physiol. 2017; 102:1535–1547 [DOI] [PubMed] [Google Scholar]
- 70.Harms CA, Wetter TJ, St Croix CM, et al. Effects of respiratory muscle work on exercise performance. J Appl Physiol (1985). 2000; 89:131–138 [DOI] [PubMed] [Google Scholar]
- 71.O’Donnell DE, D’Arsigny C, Raj S, et al. Ventilatory assistance improves exercise endurance in stable congestive heart failure. Am J Respir Crit Care Med. 1999; 160:1804–1811 [DOI] [PubMed] [Google Scholar]
- 72.Thille AW, Lyazidi A, Richard JC, et al. A bench study of intensive-care-unit ventilators: New versus old and turbine-based versus compressed gas-based ventilators. Intensive Care Med. 2009; 35:1368–1376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Younes M, Kun J, Webster K, et al. Response of ventilator-dependent patients to delayed opening of exhalation valve. Am J Respir Crit Care Med. 2002; 166:21–30 [DOI] [PubMed] [Google Scholar]
- 74.Pelosi P, Rocco PRM, Gama de Abreu M. Close down the lungs and keep them resting to minimize ventilator-induced lung injury. Crit Care. 2018; 22:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kacmarek RM, Villar J, Sulemanji D, et al. ; Open Lung Approach Network. Open lung approach for the acute respiratory distress syndrome: A pilot, randomized controlled trial. Crit Care Med. 2016; 44:32–42 [DOI] [PubMed] [Google Scholar]
- 76.Carteaux G, Mancebo J, Mercat A, et al. Bedside adjustment of proportional assist ventilation to target a predefined range of respiratory effort. Crit Care Med. 2013; 41:2125–2132 [DOI] [PubMed] [Google Scholar]
- 77.Kollef MH, Shapiro SD, Silver P, et al. A randomized, controlled trial of protocol-directed versus physician-directed weaning from mechanical ventilation. Crit Care Med. 1997; 25:567–574 [DOI] [PubMed] [Google Scholar]
- 78.Bekos V, Marini JJ. Monitoring the mechanically ventilated patient. Crit Care Clin. 2007; 23:575–611 [DOI] [PubMed] [Google Scholar]
- 79.Brochard L, Slutsky A, Pesenti A. Mechanical ventilation to minimize progression of lung injury in acute respiratory failure. Am J Respir Crit Care Med. 2017; 195:438–442 [DOI] [PubMed] [Google Scholar]
- 80.Conceição TMAD, Gonzáles AI, Figueiredo FCXS, et al. Safety criteria to start early mobilization in intensive care units. Systematic review. Rev Bras Ter Intensiva. 2017; 29:509–519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sommers J, Klooster E, Zoethout SB, et al. Feasibility of exercise testing in patients who are critically ill: A prospective, observational multicenter study. Arch Phys Med Rehabil. 2019; 100:239–246 [DOI] [PubMed] [Google Scholar]
- 82.Wollersheim T, Haas K, Wolf S, et al. Whole-body vibration to prevent intensive care unit-acquired weakness: Safety, feasibility, and metabolic response. Crit Care. 2017; 21:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


