Abstract
The aim of this study was to investigate beneficiary panel characteristics associated with rheumatologists’ prescribing of biologic DMARDs (bDMARDs) for older adults.
In this retrospective observational study, we used Medicare Public Use Files (PUFs) to identify rheumatologists who met criteria for high-prescribing, defined as bDMARD prescription constituting ≥20% of their DMARD claims for beneficiaries ≥65 years of age. We first used descriptive analysis then multivariable regression model to test the association of high prescribing of bDMARDs with rheumatologists’ panel size and beneficiary characteristics. In particular, we quantified the proportion of panel beneficiaries ≥75 years of age to assess how caring for an older panel correlate with prescribing of bDMARDs.
We identified 3197 unique rheumatologists, of whom 405 (13%) met criteria for high prescribing of bDMARDs for Medicare beneficiaries ≥65 years of age. The high-prescribers provided care to 12% of study older adults, and yet accounted for 21% of bDMARD prescriptions for them. High prescribing of bDMARDs was associated with smaller panel size, and their beneficiaries were more likely to be non-black, ≥75 years of age, non-dual eligible, have diagnosis of CHF, however, less likely to have CKD.
Rheumatologists differ in their prescribing of bDMARDs for older adults, and those caring for more beneficiaries ≥75 years of age are more likely to be high-prescribers. Older adults are more prone to the side-effects of bDMARDs and further investigation is warranted to understand drivers of differential prescribing behaviors to optimize use of these high-risk and high-cost medications.
Keywords: age, arthritis, biologic therapy, epidemiology
1. Introduction
The advent of biologic disease modifying antirheumatic drugs (bDMARDs) has fundamentally shifted the paradigm in treatment of rheumatic diseases with improved clinical, functional, and radiographic outcomes.[1,2] Introduction of self-administered bDMARDs covered by the Medicare Part D prescription drug benefit greatly expanded access to bDMARDs to older adults. Although efficacious, bDMARD use is associated with dose-dependent side effects, such as increased risk of serious infections and malignancy especially in older adults.[3] In addition, bDMARDs are costly, accounting for more than half of all direct medical costs related to rheumatic diseases, and they are a main driver of Medicare prescription drug spending growth.[4] Therefore, understanding how bDMARD prescribing varies among rheumatologists can identify opportunities to optimize their use that aligns quality of care, outcomes, and cost considerations in older adults with rheumatic diseases.
Some studies have shown variation in receipt of bDMARDs is associated with individual patient sociodemographic factors and preferences, along with reimbursement policies and physician preferences.[5–8] To our knowledge, there has not been any study evaluating patient panel characteristics related to rheumatologists prescribing of bDMARDs. In this study, we identify rheumatologists whose proportion of all DMARDs prescriptions that are biologics (bDMARD) for older adults under Medicare Part D is high and the factors associated with their high bDMARD prescribing.
2. Methods
We used 2 sets of Medicare Public Use Files (PUFs) for this study: Physician supplier and beneficiary summary (PSBS) file to identify rheumatologists and their panel characteristics, and Part D Prescriber file to analyze each providers’ proportion of bDMARDs prescriptions.[9] PUFs are developed by the Center for Medicare & Medicaid Services (CMS) and contain nonidentifiable claim-specific information made available to researchers within the public domain.[9] Users of PUFs do not need to obtain approval or seek a determination that the use of the public data files meet criteria for being exempt from Institutional Review Board review.
The PSBS file identifies providers by their National Provider identifier (NPI) and we used the Healthcare Provide Taxonomy Code (HPTC) to select for rheumatologists. We obtained information on aggregate characteristics of all fee-for-service (FFS) beneficiaries seen by each rheumatologist, including beneficiary sex, age, race, dual eligibility for Medicaid and Medicare, and chronic conditions status based on CMS Chronic Conditions Data Warehouse (CCW).[9] The CCW includes variables for 27 common chronic conditions and is predefined to categorize together beneficiaries with claims for either rheumatoid arthritis or osteoarthritis.
The Part D Prescriber PUF also identifies providers by their NPI and has information on total number of prescriptions that were dispensed for specific drugs. We restricted prescriptions for adults aged 65 and older. We identified 13 DMARDs, 8 of them bDMARDs that are most commonly used and have the most overlap in recommendations by the American College of Rheumatology for treatment of rheumatic diseases[1,2]: adalimumab, etanercept, abatacept, certolizumab, golimumab, anakinra, tocilizumab and tofacitinib. The 5 non-bDMARDs were: methotrexate, azathioprine, leflunomide, hydroxychloroquine, and sulfasalazine. For each rheumatologist, we measured the proportion of bDMARD prescriptions among the total number of DMARD prescriptions for adults ≥65 years of age.
We linked the 2 dataset by the NPI to derive our final analytic file that contains information on beneficiary panel characteristics and DMARD prescriptions for older adults for each rheumatologist. We compared Medicare beneficiary panel size, demographics, and chronic conditions status, among rheumatologists with varying proportions of bDMARD prescriptions using descriptive statistics. In particular, we compared high bDMARD prescribers, defined as rheumatologists with bDMARDs constituting ≥20% of their DMARD claims, to those with <20% claims for older adults using t test for continuous measures and χ2 or Fisher exact for categorical measures. Variables with P value <.1 in univariate analyses or with clinical significance were then included in a multivariable logistic regression model to assess factors associated with high bDMARDs prescribing for older adults. For the multivariable model, panels were dichotomized using the 75th percentile value for each demographic characteristic and 20% for each chronic conditions status. If there are <11 beneficiaries or claims for a particular variable the values are suppressed in PUFs, and in such instances we imputed the mean value to account for missing variables. Data were analyzed using Stata/IC 14.2 (Stata Corp).
3. Results
We identified 3197 unique rheumatologists, with an average panel size of 403 (interquartile range [IQR] 359) FFS beneficiaries (Table 1). On average, most beneficiaries on each rheumatologists’ panel were women (median 75.1%, IQR 7.5%) and had diagnosis of arthritis (median 76.9%, IQR 14.6%) broadly defined by on billing diagnoses.[9] The panel average median percentage of white was 75.1% (IQR 7.5%), 38.5% (IQR 44.6%) were 75 years of age or older, and 16.6% (IQR 16.7%) were dual eligible for Medicare and Medicaid.
Table 1.
Comparison of FFS Medicare beneficiary panel characteristics among all rheumatologists and those who are high-prescribers of Part D bDMARD prescriptions for adults ≥65 years of age.
| Variables | All rheumatologists | High-prescribers (≥20% bDMARDs) |
| No. of rheumatologists, n (%) | 3197 (100) | 405 (12.7) |
| Percent bDMARDs∗, median% (25th, 75th percentile) | 7.2 (2.9, 12.8) | 30.1 (23.9, 44.4) |
| Panel size, median (25th, 75th percentile) | 340 (188, 547) | 287 (162, 484) |
| Panel characteristics, median percentage of beneficiaries (25th, 75th percentile) | ||
| Race | ||
| White | 68.1 (42.9, 91.1) | 78.0 (55.6, 88.3) |
| Black | 6.8 (2.7, 14.9) | 6.8 (3.0, 14.4) |
| Hispanic | 3.3 (1.5, 8.3) | 5.4 (2.2, 13.8) |
| Non-Hispanic other | 5.4 (3.2, 10.0) | 6.6 (4.0, 13.4) |
| Female | 75.1 (71.1, 78.6) | 74.0 (68.2, 78.2) |
| Age ≥75 y | 38.5 (31.2, 75.8) | 40.2 (31.3, 48.3) |
| Dual eligible | 16.6 (9.9, 26.6) | 17.6 (7.8, 31.0) |
| Comorbid conditions | ||
| Cancer | 10.1 (8.0, 13.8) | 11.3 (8.8, 15.5) |
| Congestive heart failure | 17.1 (14.1, 21.4) | 18.2 (4.4, 23.8) |
| Chronic kidney disease | 18.4 (15.1, 22.6) | 17.9 (14.5,22.8) |
| Diabetes | 27.2 (23.2, 32.5) | 28.4 (23.3, 36.0) |
| Hypertension | 66.3 (60.3, 71.7) | 66.3 60.0,72.8) |
| Rheumatoid arthritis/osteoarthritis | 76.9 (69.1, 83.7) | 75.4 (68.4, 83.1) |
Among all rheumatologists, the proportion of bDMARD prescriptions was positively skewed with mean of 10.4% (SD 12.7%) and median of 7.2% (IQR 9.9%) (Fig. 1). When divided in quartiles by proportion of bDMARDs prescribed, the average median proportion of bDMARD prescription was 2.9% (IQR 5.0%) for rheumatologists in the two lowest quartiles, compared to 19.9% (IQR 14.7%) for those in the top-quartile (Supplemental Table 1).
Figure 1.
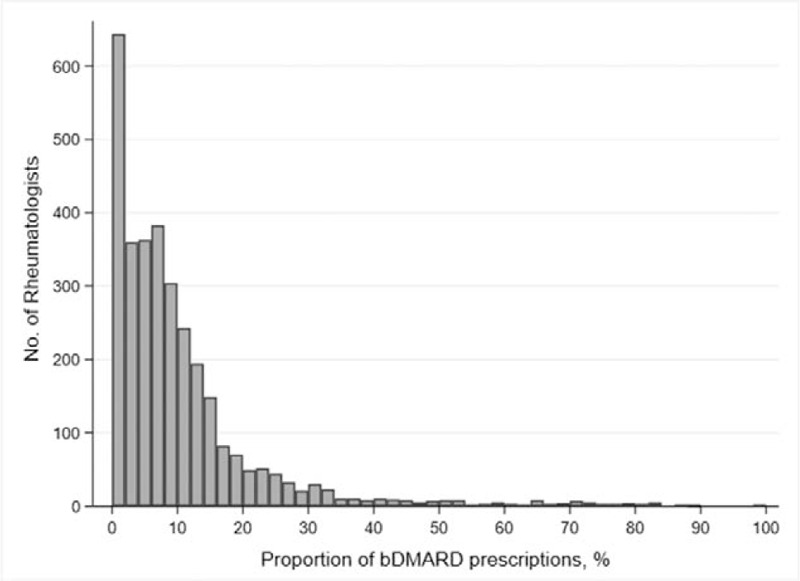
Distribution of rheumatologists by the proportion of bDMARD prescription for adults ≥65 years of age. Among all rheumatologists, the mean proportion of bDMARD prescription was 10.4% (SD 12.7) and the median was 7.2% (IQR 9.95). There were 405 (12.7%) rheumatologists for whom bDMARDs constituted ≥20% of their DMARD claims for older adults. bDMARDs = biologic disease-modifying anti-rheumatic drugs.
We identified 405 (12.7%) rheumatologists who met criteria for high bDMARDs prescribing for adults ≥65 years of age. The high prescribing rheumatologists provided care to 11.6% of beneficiaries ≥65 years of age in this study and accounted for 21.5% of all bDMARD claims for older adults under Medicare Part D. In multivariable logistic analysis, high bDMARD prescribing for older adults was associated with having a smaller panel size, and their beneficiaries were more likely to be non-black, ≥75 years of age, non-dual eligible, and have diagnosis of congestive heart failure, however, less likely to have chronic kidney disease (Table 2).
Table 2.
Medicare beneficiary panel characteristics associated with being a rheumatologist whose bDMARDs prescription constitute ≥20% DMARD claims for adults ≥65 years of age.
| OR (95% CI) | ||
| Variables | Unadjusted | Adjusted |
| Beneficiary panel size | ||
| <300 Beneficiaries | Reference | Reference |
| 300–600 Beneficiaries | 0.75 (0.59–0.95) | 0.74 (0.57–0.96)∗ |
| >600 Beneficiaries | 0.60 (0.44–0.80) | 0.87 (0.41–0.79)∗ |
| ≥80% Female | 0.83 (0.63–1.11) | 0.87 (0.65–1.16) |
| ≥15% Black | 0.91 (0.71–1.17) | 0.74 (0.56–0.97)∗ |
| ≥50% 75 y of age or older | 1.49 (1.14–1.94) | 1.50 1.14–1.99)∗ |
| <25% Dual eligible | 0.70 (0.56–0.88) | 0.70 (0.54–0.00∗ |
| Comorbid conditions | ||
| ≥20% Cancer | 1.29 (0.96–1.73) | 0.94 (0.67–1.31) |
| ≥20% Congestive heart failure | 1.51 (1.22–1.87) | 1.48 (1.15–1.91)∗ |
| ≥20% Chronic kidney disease | 1.00 (0.81–1.24) | 0.74 (0.57–0.95)∗ |
4. Discussion
In this study, rheumatologists differed in their prescribing of bDMARDs for older adults, with a small group of providers accounting for a greater proportion of bDMARD prescriptions. The high-prescribing rheumatologists had patient panels with more Medicare beneficiaries over ≥75 years of age and fewer blacks.
Prescribing for older adults pose unique challenges and variation in bDMARD use may exist as they are more prone to the additive, sometimes multiplicative, negative effects associated with high risk medications for reasons of polypharmacy and multimorbidity that are the norm rather than the exception in older adults.[10] Increased life expectancy in the past few decades, along with advancement in understanding and treatment have led to a growing population of older adults living with rheumatic diseases such as rheumatoid arthritis.[11] Although current guidelines recommend tailoring DMARD therapy to achieve disease remission in rheumatic diseases, physician factors influence prescription patterns, at times independent of disease activity.[8] Moreover, older adults are less likely to receive aggressive treatment despite some data suggesting the relative risk of adverse effects associated with bDMARD use such as serious infection may be similar across the older age spectrum which raise concern for poor quality of care.[12–14] And yet, rheumatologists with higher proportion of bDMARD prescriptions in this study were more likely to care for an older panel with more beneficiaries ≥75 years of age. Physician experience and perception of medications are important factors that influence prescribing behavior and, specialty trained geriatricians are known to differ in prescribing behavior and assessment of geriatric syndromes compared to generalists.[15] Rheumatologists with more experience caring for an older panel may have more familiarity and comfort in prescribing and managing risks associated with use of bDMARDs for older adults. Whether outcomes differ when older adults with rheumatic diseases are cared for by rheumatologists with higher proportion of older adults on their panel may be an area of future investigation.
In addition to an older panel, high prescribers had fewer black beneficiaries on their panels. Racial disparity in the care of rheumatic diseases has been observed and is thought to be propagated by provider, patient, and systemic factors. Patients under the care of a rheumatologist are more likely to be prescribed DMARDs,[16] and although Medicare provides insurance coverage, older blacks may have limited access to or underutilize specialty care for socioeconomic reasons. The 2015 Rheumatology Workforce Study showed that regional maldistribution of rheumatologists in the Unites States exist,[17] which may further propagate racial disparity in access to rheumatologic care. In addition to provider and systemic factors, some data suggest racial differences in treatment may in part be due to patient preferences as fewer blacks prefer aggressive treatment compared to their white counterparts with similar disease activity.[6]
This study has several limitations common to claims-based observational analyses. We rely on the completeness and accuracy of administrative bills recorded by physicians, and some measure such as disease activity, function, or disability are not available. In addition, we are limited to variable definitions provided by CMS in the PUFs and cannot distinguish whether beneficiaries billed for arthritis have either inflammatory arthritis or osteoarthritis. The PUFs used in this study summarize patient characteristics at the level of a physician panel and do not provide data for more specific individual disease measures but do allow generation of preliminary estimates on variation in physician practice using 100% of physicians and beneficiaries in FFS Medicare. Future work using the research identifiable data will allow more refined analyses at the patient level.
In conclusion, rheumatologists differ in their propensity to prescribe bDMARDs for older adults, and although older adults are less likely to receive aggressive treatment, high-prescribers are more likely to care for FFS Medicare beneficiaries ≥75 years of age which suggest experience caring for an older panel may influence prescribing behavior. In addition, high-prescribers are less likely to care for blacks which may allude to disparity in access to rheumatologic care independent of insurance coverage. Further research is needed to understand drivers of differential prescription patterns of bDMARDs to optimize use of these high-risk and high-cost medications in older adults.
Author contributions
Conceptualization: Jiha Lee, Chiang-Hua Chang, Julie P.W. Bynum.
Data curation: Jiha Lee, Chiang-Hua Chang.
Formal analysis: Jiha Lee, Chiang-Hua Chang.
Funding acquisition: Jiha Lee, Raymond Yung.
Investigation: Jiha Lee.
Methodology: Jiha Lee, Chiang-Hua Chang, Raymond Yung, Julie P.W. Bynum.
Project administration: Jiha Lee.
Resources: Jiha Lee.
Software: Jiha Lee.
Supervision: Chiang-Hua Chang, Julie P.W. Bynum.
Visualization: Jiha Lee, Chiang-Hua Chang, Julie P.W. Bynum.
Writing – original draft: Jiha Lee.
Writing – review & editing: Jiha Lee, Chiang-Hua Chang, Raymond Yung, Julie P.W. Bynum.
Supplementary Material
Footnotes
Abbreviations: bDMARDs = biologic disease-modifying anti-rheumatic drugs, CCW = Chronic Conditions Data Warehouse, CMS = Center for Medicare & Medicaid Services, FFS = Fee-for-service, HPTC = Healthcare Provide Taxonomy Code, IQR = interquartile range, NPI = National Provider identifier, PSBS = physician supplier and beneficiary summary, PUF = Public Use Files.
How to cite this article: Lee J, Chang CH, Yung R, Bynum JP. Medicare beneficiary panel characteristics associated with high Part D biologic disease-modifying anti-rheumatic drug prescribing for older adults among rheumatologists. Medicine. 2021;100:16(e25644).
Source of Support: Research reported in this publication was supported by the National Institute on Aging, part of the National Institutes of Health, under Award Number P30AG024824-06 (Yung) and 1R03AG067975-01 (Lee).
The authors report no conflicts of interest.
The datasets generated during and/or analyzed during the current study are publicly available.
Supplemental digital content is available for this article.
Percentage bDMARDs = proportion of bDMARD claims among the total number of DMARD clams for adults.
≥65 years of age; Panel size = in number of FFS Medicare beneficiaries.
bDMARDs = biologic disease-modifying anti-rheumatic drugs, FFS = fee-for-service.
bDMARDs = biologic disease-modifying anti-rheumatic drugs, CI = confidence interval; DMARDS = biologic disease modifying anti-rheumatic drugs, OR = odds ratio.
Statistically significant with P < .05.
References
- [1].Singh JA, Saag KG, Bridges SL, Jr, et al. 2015 american college of rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Care Res 2016;68:01–25. [DOI] [PubMed] [Google Scholar]
- [2].Ward MM, Deodhar A, Gensler LS, et al. 2019 update of the american college of rheumatology/spondylitis association of america/spondyloarthritis research and treatment network recommendations for the treatment of ankylosing spondylitis and nonradiographic axial spondyloarthritis. Arthritis Rheum 2019;71:1599–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Cho SK, Sung YK, Kim D, et al. Drug retention and safety of tnf inhibitors in elderly patients with rheumatoid arthritis. BMC Musculoskelet Disord 2016;17:333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Harrold LR, Peterson D, Beard AJ, et al. Time trends in medication use and expenditures in older patients with rheumatoid arthritis. Am J Med 2012;125:937.e9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Schmajuk G, Trivedi AN, Solomon DH, et al. Receipt of disease-modifying antirheumatic drugs among patients with rheumatoid arthritis in medicare managed care plans. JAMA 2011;305:480–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Constantinescu F, Goucher S, Weinstein A, et al. Racial disparities in treatment preferences for rheumatoid arthritis. Med Care 2009;47:350–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].DeWitt EM, Glick HA, Albert DA, et al. Medicare coverage of tumor necrosis factor ( inhibitors as an influence on physicians’ prescribing behavior. Arch Int Med 2006;166:57–63. [DOI] [PubMed] [Google Scholar]
- [8].Curtis JR, Chen L, Harrold LR, et al. Physician preference motivates the use of anti–tumor necrosis factor therapy independent of clinical disease activity. Arthritis Care Res 2010;62:101–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Center for medicare and medicaid services(cms) research, statistics, data & systems. [Internet accessed October 28, 2020]; Available from: https://www.cms.gov/Research-Statistics-Data-and-Systems/Research-Statistics-Data-and-Systems. [Google Scholar]
- [10].Makris UE, Misra D, Yung R. Gaps in aging research as it applies to rheumatologic clinical care. Clin Geriatr Med 2017;33:119–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Chen C-I, Wang L, Wei W, et al. Burden of rheumatoid arthritis among us medicare population: co-morbidities, health-care resource utilization and costs. Rheumatol Adv Pract 2018;2:rky005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Schmajuk G, Schneeweiss S, Katz JN, et al. Treatment of older adult patients diagnosed with rheumatoid arthritis: Improved but not optimal. Arthritis Rheum 2007;57:928–34. [DOI] [PubMed] [Google Scholar]
- [13].Ikari Y, Yajima N, Miwa Y. The association between age and adverse events due to biologic disease-modifying antirheumatic drugs in patients with rheumatoid arthritis: A retrospective cohort study. Medicine (Baltimore) 2020;99:e23861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Galloway JB, Hyrich KL, Mercer LK, et al. Anti-tnf therapy is associated with an increased risk of serious infections in patients with rheumatoid arthritis especially in the first 6 months of treatment: Updated results from the british society for rheumatology biologics register with special emphasis on risks in the elderly. Rheumatology (Oxford) 2011;50:124–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Phelan EA, Genshaft S, Williams B, et al. A comparison of how generalists and fellowship-trained geriatricians provide “geriatric” care. J Am Geriatr Soc 2008;56:1807–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Solomon DH, Ayanian JZ, Yelin E, et al. Use of disease-modifying medications for rheumatoid arthritis by race and ethnicity in the national ambulatory medical care survey. Arthritis Care Res 2012;64:184–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].2015 rheumatology workforce study. [Internet accessed October 28, 2020]; Available from: https://www.rheumatology.org/Learning-Center/Statistics/Workforce-Study. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


