Abstract
Background:
Neck pain is common musculoskeletal disorders in adult population. Acupuncture treatment has been widely used for treating neck pain. Nevertheless, previous systematic reviews (SRs) on acupuncture for neck pain remain controversial, and there is no SR for the comparative efficacy and safety of various types of acupuncture. Therefore, this study aims to evaluate and rank the effectiveness and safety of different types of acupuncture for neck pain by SR and network meta-analysis.
Methods:
Nine databases will be searched, including Ovid-MEDLINE, EMBASE, Cochrane library, China National Knowledge Infrastructure (CNKI), KoreaMed, Korean medical database (KMBASE), Korean Studies Information Service System (KISS), ScienceON, and Oriental Medicine Advanced Searching Integrated System (OASIS) from their inception to July 2021. The primary outcome is the change of pain intensity. A frequentist network meta-analysis will be performed to compare all relative outcomes of different acupuncture methods, using R software. The quality of included randomized controlled trials will be assessed by Cochrane Collaboration “risk of bias” tools and the evidence will be evaluated by the Grading of Recommendations Assessment, Development and Evaluation instrument.
Results:
The final findings of this network meta-analysis will be published in a recognized journal.
Conclusions:
Our study will evaluate and compare the effectiveness of various types of acupuncture for neck pain and provide clinicians with best option for what types of acupuncture treatments are effective.
Trial registration number:
INPLASY202120041
Keywords: acupuncture, neck pain, network meta-analysis, protocol, systematic review
1. Introduction
Neck pain is one of the common musculoskeletal disorders in adult population. According to 2018 health statistics—National Health Interview Survey, the incidence of neck pain accounts for 15.7% for adults.[1] Some studies suggested that a high prevalence of neck pain is associated with women, performing occupational activities while sitting and leaning, low levels of education and income, and suffering from ≥2 diseases.[2,3]
A high proportion of the neck pain becomes recurrent or chronic. Most people with neck pain do not experience complete symptom relief, and recur within 1 to 5 years in 50% to 85% of patients with neck pain. One study reported that 30% of patients show chronic progress and the problems persist for at least 12 months in 37% of patients with neck pain.[4] It affects the physical, social, and psychological well-being of individuals, and increases the costs in health care expenditure. According to Global Burden of Disease 2010 study of 291 conditions, neck pain ranked 21st in terms of overall burden and 4th in terms of overall disability.[5]
Although conventional treatments such as medication, injection, or surgery have a therapeutic effect on neck pain,[6–9] some of these treatments have poor evidence, and even had some serious adverse effects including renal dysfunction, hemorrhagic gastritis/ulcer, myocardial infarction, spinal cord and nerve injury, epidural hematoma.[10–12] For these reasons, many patients divert their attention to other treatments, such as complementary and alternative medicine (CAM).
As one of CAM therapies, acupuncture treatment has analgesic effects on musculoskeletal pain through neurophysiological and neurochemical mechanisms. Acupuncture can mediate short term analgesia by activating endogenous antinociceptive systems and descending inhibitory systems.[13] Acupuncture-induced analgesia also can be associated with biopsychosocial pain management system in prefrontal cortex. The dual, opposing roles of medial prefrontal cortex mediate pain chronification or inhibition of pain perception so these opposite interactions should be considered for pain control.[14]
Acupuncture is frequently accepted and recommended for neck pain in Korea.[15] Recently, while many randomized controlled trials (RCTs) have conducted various types of acupuncture treatment for cervical pain,[16–18] the systematic reviews (SRs) have shown the effectiveness of acupuncture to be controversy. Several SRs have reported that acupuncture improves pain and disability associated with neck pain superior to sham acupuncture or no treatment but similar to active control group such as medications, massage, and physical therapy.[19,20] Furthermore, Smith et al[21] suggested it is no more effective than placebo, and some SRs[19,22,23] reported inconsistent comparative effects between acupuncture and other interventions. These reviews included various types of acupuncture treatments, and due to the its diversity, the relative effects of each individual option have not yet been studied and compared.
Therefore, we will conduct SR and network meta-analysis to evaluate the effectiveness on neck pain and to estimate comparative effectiveness of different types of acupuncture.
2. Methods
This protocol will be reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols (PRISMA-P) Statement.[24] The research protocol has been registered on INPLASY (Registration number: INPLASY202120041). No ethical statement is required as this study does not require patient recruitment and personal data collection.
2.1. Eligibility criteria
2.1.1. Type of participants
Adult patients (>18 years) who had cervical pain or cervical intervertebral disc herniation with or without radicular symptoms will be included. We will exclude patients who have specific reasons for neck pain, including whiplash injuries, athletic injuries. There will be no restriction on sex, ethnicity, duration of illness, or disease severity.
2.1.2. Type of interventions and comparators
We will include a single use of acupuncture to compare the effects of various types of acupuncture treatments. Interventions in the treatment group will include manual acupuncture, electroacupuncture, warm acupuncture, fire acupuncture, and acupuncture point thread-embedding. Control interventions will include sham acupuncture, usual care, western medication, no treatment, and one of the aforementioned acupuncture treatments.
2.1.3. Type of outcomes
The primary outcome measure is the change of pain intensity, as measured by Visual Analogue Scale, Neck Pain Questionnaire, or other validated assessment tools. Secondary outcome measures are to be considered depending on review findings, such as functional status (effective rate, curative rate, and range of motion), disability (Neck Disability Index), and adverse events.
2.1.4. Type of studies
This study will include all relevant RCTs using various types of acupuncture therapies for neck pain and the first period in randomized cross-over trials. Non-RCT studies including care studies, quasi-RCT, experimental studies, cohort studies, and RCTs published in the form of letters-to-the-editor, and conference abstracts will be excluded.
2.2. Information sources and search strategy
The following electronic databases will be searched from their inception to July 2021: Ovid-MEDLINE, EMBASE, Cochrane library, China National Knowledge Infrastructure (CNKI), KoreaMed, Korean medical database (KMBASE), Korean Studies Information Service System (KISS), ScienceON, and Oriental Medicine Advanced Searching Integrated System (OASIS).
Researchers will search using medical search headings (MeSH) terms and key words with the limitation of Chinese, English, and Korean language. The following search terms will be used in each database's own language: researchers will perform search using terms with combination of neck pain related terms (such as neck pain, cervical pain, cervicodynia, cervicalgia, cervical intervertebral disc displacement/degeneration, cervical spondylosis) and treatments (the names of various acupuncture types, such as acupuncture, electroacupuncture, warm acupuncture, fire acupuncture, thread-embedding). If needed, a manual search, such as the textbooks on acupuncture and the references of the retrieved SRs, will be also done (Table 1).
Table 1.
Search strategy in MEDILINE (Ovid SP).
| No. | Search terms |
| 1 | Neck pain/or thoracic outlet syndrome/or cervical rib syndrome/or Torticollis/ |
| 2 | (“cervical pain” or “neckache” or “cervicodynia” or “cervicalgia” or “brachialgia” or “brachial neuritis” or “brachial neuralgia” or “neck pain” or neck injur∗ or brachial plexus neuropath∗ or “brachial plexus neuritis”).mp. |
| 3 | exp Brachial Plexus Neuropathies/ or exp brachial plexus neuropathies/ or exp brachial plexus neuritis/ |
| 4 | (cervico brachial neuralgia or cervicobrachial neuralgia).ti,ab. |
| 5 | (monoradicul∗ or monoradicl∗).tw. |
| 6 | Or 1 to 5 |
| 7 | neck/ or neck muscles/ or atlanto-axial joint/ or atlanto-occipital joint/ or Cervical Atlas/ or spinal nerve roots/ or axis/ or odontoid process/ or Thoracic Vertebrae/ |
| 8 | exp cervical plexus/ or exp cervical vertebrae/ or exp brachial plexus/ |
| 9 | (odontoid∗ or cervical or occip∗ or atlant∗).tw. |
| 10 | (“cervical vertebrae” or “cervical plexus” or “cervical spine” or “neck” or “trapezius” or (neck adj3 muscles) or (brachial adj3 plexus) or (thoracic adj3 vertebrae) or (thoracic adj3 spine) or (thoracic adj3 outlet)).mp. |
| 11 | Or 7 to 10 |
| 12 | exp pain/ or exp injuries/ |
| 13 | (“pain” or “ache” or “sore” or “stiff” or “discomfort” or injur∗ or neuropath∗).mp. |
| 14 | 12 or 13 |
| 15 | 11 and 14 |
| 16 | Radiculopathy/ or myofascial pain syndromes/ or Polyradiculopathy/ or Fibromyalgia/ or spondylitis/ or discitis/ or spondylosis/ or spondylolysis/ or spondylolisthesis/ |
| 17 | exp temporomandibular joint disorders/ or exp temporomandibular joint dysfunction syndrome/ or exp “Sprains and Strains”/ or exp Spinal Osteophytosis/ or exp Neuritis/ or exp Arthritis/ |
| 18 | (“radiculopathy” or “radiculitis” or “temporomandibular” or myofascial pain syndrome∗ or thoracic outlet syndrome∗ or “spinal osteophytosis” or “neuritis” or “spondylosis” or “spondylitis” or “spondylolisthesis”).mp. |
| 19 | Or 16 to 18 |
| 20 | 11 and 19 |
| 21 | exp neck/ or exp cervical vertebrae/ |
| 22 | Thoracic Vertebrae/ |
| 23 | (“neck” or “cervical spine” or (thoracic adj3 vertebrae) or (thoracic adj3 spine)).mp. |
| 24 | Or 21 or 23 |
| 25 | Intervertebral Disk/ |
| 26 | ((disc or discs) or (disk or disks)).mp. |
| 27 | 25 or 26 |
| 28 | 24 and 27 |
| 29 | (herniat∗ or prolapsed∗ or displace∗ or degenerate∗ or “slipped” or (bulge or bulged or bulging)).mp. |
| 30 | 28 and 29 |
| 31 | intervertebral disk degeneration/ or intervertebral disk displacement/ |
| 32 | (“intervertebral disc displacement” or “intervertebral disc degeneration” or “intervertebral disc degeneration”).mp. |
| 33 | 31 or 32 |
| 34 | 24 and 33 |
| 35 | 6 or 15 or 20 or 30 or 34 |
| 36 | (“acupuncture” or “acu-puncture” or “needling” or “acupressure” or “electric acupuncture” or “electroacupuncture” or “warm needle” or “warming acupuncture” or “warmed electroacupuncture” or “warm acupuncture” or “fire needle” or “fire acupuncture” or “catgut implantation” or catgut emb∗ or thread emb∗).tw. |
| 37 | exp Acupuncture Points/ or exp Acupuncture Therapy/ or exp Acupuncture/ or exp Electroacupuncture/ or exp Catgut/ |
| 38 | 36 or 37 |
| 39 | 35 and 38 |
| 40 | (randomized controlled trial or controlled clinical trial).pt. |
| 41 | (randomized or placebo or randomly or trial or groups).ab. |
| 42 | drug therapy.fs. |
| 43 | Or 40 to 42 |
| 44 | exp animals/ not humans.sh. |
| 45 | 43 not 44 |
| 46 | 39 and 45 |
2.3. Literature selection and data extraction
All searched studies will be imported into Endnote X20. Two independent researchers will screen the output based on the titles, abstracts, and full-text (if needed) to exclude the duplicates and irrelevant articles. After then, the 2 researchers will review the studies by reading the full-texts. Data extraction will be performed independently by 2 authors and included the following data: study characteristics (author and publication year), sample size, age range, sex, intervention, comparator, treatment frequency, duration, outcomes, results, and adverse events from each of the included RCTs. If necessary, we will try to contact the original author for missing data or clarification for unclear information. If there are any discrepancies, 2 reviewers will solve the problem through discussion. If the disagreement persists, a third reviewer will make final decision (Fig. 1).
Figure 1.
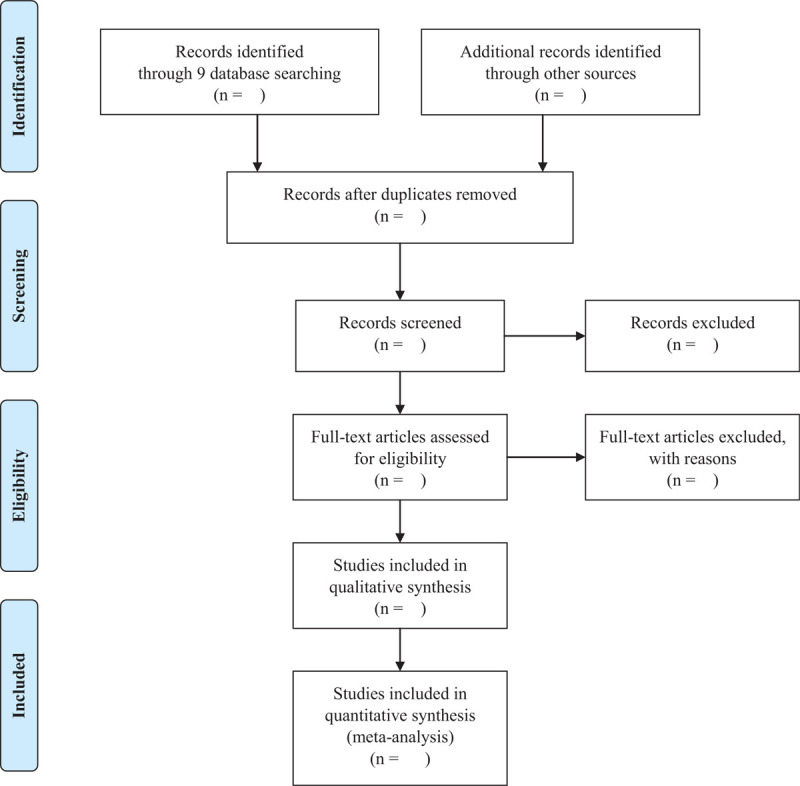
PRISMA flow diagram. PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
2.4. Quality assessment
The “Risk of Bias (RoB) Tool” of Cochrane Collaboration will be used to assess the risk of bias. In 7 domains (sequence generation, allocation concealment, blinding of participants, blinding of outcome assessors, incomplete outcome data, selective outcome reporting, and other bias), the assessment result will be divided into “low risk,” “high risk,” and “unclear” by independent 2 reviewers. If there is a disagreement between 2 researchers, the final evaluation will be conducted by a third researcher.[25]
2.5. Statistical analysis
We will adopt the random-effects model for pairwise meta-analyses of direct evidence, while a random-effects network meta-analysis within a frequentist framework will be performed. A different measure used for evaluating the same outcomes will be analyzed by calculating the dichotomous data as Mantel-Haenszel odds ratios (ORs) and the continuous outcomes as standardized mean difference (SMD). We will present 95% confidence intervals for all outcomes.
We will use R software (http://www.r-project.org/, version 4.0.3) for network meta-analysis to compare direct and indirect evidence. The numerical variables will be presented as the ORs and SMD with 95% credible intervals. The rank of treatments for each outcome will be conducted as surface under the cumulative ranking curve (SUCRA), where SUCRA values indicate the efficacy possibility of the intervention.[26] If the available data are not suitable for synthesis, we will conduct a narrative review and summarize the evidences.
2.6. Heterogeneity test
Before the combination of effect size, we will examine the potential effects of heterogeneity on the effect estimates. The heterogeneity assessment will be estimated by I2. When I2 > 50%, there is heterogeneity between studies and the source of heterogeneity need to be further searched. When I2 < 50%, it is considered to be less heterogeneity or no obvious heterogeneity.
2.7. Consistency assessment
We will evaluate the presence of local inconsistency and global inconsistency between direct and indirect evidence. If there is no significant difference (P > .05) between direct and indirect comparisons, a consistency model is adopted, and stability of the results is verified by the inconsistency model.
2.8. Subgroup analysis
If possible, the subgroup analysis will be conducted based on age, sex, and duration of disease and sensitivity analysis will be performed additionally.
2.9. Small sample effect/publication bias
If >10 studies are included in the network meta-analysis, a funnel plot is planned to evaluate the presence of small sample effects or publication bias.
2.10. Sensitivity analysis
If necessary, a sensitivity analysis will be conducted by the exclusion method that eliminates effects of trials with small sample size and removes studies rated as high risk of bias. When each of these studies is excluded, the remaining studies will be reanalyzed to verify the stability of the results. If the qualitative change in the combined effect is not observed, it can be indicated that the results are stable.
2.11. Evaluating the quality of the evidence
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) method will also be used to grade the quality of evidence for each outcome.[27] The GRADE rates evidence quality into “high,” “medium,” “low,” and “very low” on the basis of risk of bias, inconsistency, imprecision, indirection, and publication bias.
3. Discussion
Neck pain is a common musculoskeletal disorder that causes morbidity and disability in daily life and at work. Conventional treatments and surgical methods are helpful but have some limitations. Acupuncture has been widely used for musculoskeletal pain, but inconsistent results have been reported across SRs. In addition, there is no SR for the relative effect of acupuncture in various types, thus lacking clear guideline for clinicians. Therefore, we will use network meta-analysis to compare and rank the effectiveness of different types of acupuncture therapies and assess the quality of evidence with the GRADE approach. We hope that our results will provide clinicians with the best options and help lower uncertainty about the effectiveness of acupuncture treatment for treating neck pain.
Author contributions
Conceptualization: Hyo-Rim Jo, Eun-Ji Noh, Se-Hee Oh.
Data curation: Su-Ji Choi.
Formal analysis: Eun-Ji Noh, Seung-Ug Hong.
Funding acquisition: Eun-Jung Kim.
Methodology: Hyo-Rim Jo, Eun-Ji Noh, Se-Hee Oh.
Project administration: Dong-Il Kim, Seung-Ug Hong.
Supervision: Eun-Jung Kim.
Writing – original draft: Hyo-Rim Jo, Se-Hee Oh.
Writing – review & editing: Seong-Kyeong Choi, Won-Suk Sung, Eun-Jung Kim
Footnotes
Abbreviations: CAM = complementary and alternative medicine, GRADE = Grading of Recommendations Assessment, Development and Evaluation, OR = odds ratio, RCT = randomized controlled trial, SMD = standardized mean difference, SR = systematic review.
How to cite this article: Jo HR, Noh EJ, Oh SH, Choi SK, Sung WS, Choi SJ, Kim DI, Hong SU, Kim EJ. The effectiveness of different acupuncture therapies for neck pain: A protocol for systematic review and/or network meta-analysis. Medicine. 2021;100:16(e25379).
This study was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HF20C0210). There was no involvement with funder in the review, editing, or the submission of the manuscript for publication.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Migraines and Pain in Neck, Lower Back, Face, or Jaw Among Adults Aged 18 and Over. National Center for Health Statistics; 2018. Available at: https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2018_SHS_Table_A-5.pdf. Accessed February 24, 2021. [Google Scholar]
- [2].Genebra CVDS, Maciel NM, Bento TPF, et al. Prevalence and factors associated with neck pain: a population-based study. Braz J Phys Ther 2017;21:274–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Strine TW, Hootman JM. US national prevalence and correlates of low back and neck pain among adults. Arthritis Rheum 2007;57:656–65. [DOI] [PubMed] [Google Scholar]
- [4].Childs JD, Cleland JA, Elliott JM, et al. Neck pain: clinical practice guidelines linked to the International Classification of Functioning, Disability, and Health from the Orthopaedic Section of the American Physical Therapy Association. J Orthop Sports Phys Ther 2008;38:01–34. [DOI] [PubMed] [Google Scholar]
- [5].Hoy D, March L, Woolf A, et al. The global burden of neck pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis 2014;73:1309–15. [DOI] [PubMed] [Google Scholar]
- [6].Roelofs PD, Deyo RA, Koes BW, et al. Nonsteroidal anti-inflammatory drugs for low back pain: an updated Cochrane review. Spine (Phila Pa 1976) 2008;33:1766–74. [DOI] [PubMed] [Google Scholar]
- [7].Boswell MV, Hansen HC, Trescot AM, et al. Epidural steroids in the management of chronic spinal pain and radiculopathy. Pain Physician 2003;6:319–34. [PubMed] [Google Scholar]
- [8].Mesregah MK, Feng W, Huang WH, et al. Clinical effectiveness of interlaminar epidural injections of local anesthetic with or without steroids for managing chronic neck pain: a systematic review and meta-analysis. Pain Physician 2020;23:335–48. [PubMed] [Google Scholar]
- [9].Peng B, DePalma MJ. Cervical disc degeneration and neck pain. J Pain Res 2018;11:2853–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Fine M. Quantifying the impact of NSAID-associated adverse events. Am J Manag Care 2013;19:s267–72. [PubMed] [Google Scholar]
- [11].Manchikanti L, Nampiaparampil DE, Candido KD, et al. Do cervical epidural injections provide long-term relief in neck and upper extremity pain? A systematic review. Pain Physician 2015;18:39–60. [PubMed] [Google Scholar]
- [12].Rampersaud YR, Moro ER, Neary MA, et al. Intraoperative adverse events and related postoperative complications in spine surgery: implications for enhancing patient safety founded on evidence-based protocols. Spine (Phila Pa 1976) 2006;31:1503–10. [DOI] [PubMed] [Google Scholar]
- [13].Irnich D, Beyer A. Neurobiologische Grnundlagen der Akupunkturanalgesie [Neurobiological mechanisms of acupuncture analgesia]. Schmerz 2002;16:93–102. [DOI] [PubMed] [Google Scholar]
- [14].Ong WY, Stohler CS, Herr DR. Role of the prefrontal cortex in pain processing. Mol Neurobiol 2019;56:1137–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Korean medicine clinical practice guidelines for neck pain. Guideline center for Korean Medicine; 2016. Available at: http://nikom.or.kr/nckm/module/practiceGuide/view.do?guide_idx=25&menu_idx=14. Accessed February 24, 2021. [Google Scholar]
- [16].Zhou JF, Li XW, Zhao JC, et al. Treatment of 30 patients with cervical spondylotic radiculopathy by acupuncture plus warming-needle moxibustion:a randomized controlled trial. World J Acupunct Moxibustion 2014;24:24–8. [Google Scholar]
- [17].Liu XQ, Jin XF. Clinical effect of Jingjin therapy combined with fire needle in the treatment of cervical spondylosis of cervical type. China Mod Med 2016;23:158–63. [Google Scholar]
- [18].Sun WH, Wang YM, Lu WZ. PGLA embedding for the treatment of cervical spondylosis of nerve root type. J Clin Acupunct Moxibustion 2013;29:43–5. [Google Scholar]
- [19].Yuan QL, Guo TM, Liu L, et al. Traditional Chinese medicine for neck pain and low back pain: a systematic review and meta-analysis. PLoS One 2015;10:e0117146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Seo SY, Lee KB, Shin JS, et al. Effectiveness of acupuncture and electroacupuncture for chronic neck pain: a systematic review and meta-analysis. Am J Chin Med 2017;45:1573–95. [DOI] [PubMed] [Google Scholar]
- [21].Smith LA, Oldman AD, McQuay HJ, et al. Teasing apart quality and validity in systematic reviews: an example from acupuncture trials in chronic neck and back pain. Pain 2000;86:119–32. [DOI] [PubMed] [Google Scholar]
- [22].Fu LM, Li JT, Wu WS. Randomized controlled trials of acupuncture for neck pain: systematic review and meta-analysis. J Altern Complement Med 2009;15:133–45. [DOI] [PubMed] [Google Scholar]
- [23].Trinh K, Graham N, Irnich D, et al. Acupuncture for neck disorders. Cochrane Database Syst Rev 2016;5:CD004870. [DOI] [PubMed] [Google Scholar]
- [24].Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Kim SY, Park JE, Seo HJ, et al. NECA's Guidance for Undertaking Systematic Reviews and Meta-analyses for Intervention. 2011;Seoul, Korea: National Evidence-based Healthcare Collaborating Agency, 64–85. [Google Scholar]
- [26].Salanti G, Ades AE, Ioannidis JPA. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol 2011;64:163–71. [DOI] [PubMed] [Google Scholar]
- [27].Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 2011;64:383–94. [DOI] [PubMed] [Google Scholar]


