Abstract
Background
Back pain is a common disorder that has a tendency to recur. It is unclear if exercises, either as part of treatment or as a post‐treatment programme, can reduce back pain recurrences.
Objectives
To investigate the effectiveness of exercises for preventing new episodes of low‐back pain or low‐back pain‐associated disability.
Search methods
We searched CENTRAL (The Cochrane Library 2009, issue 3), MEDLINE, EMBASE and CINAHL up to July 2009.
Selection criteria
Inclusion criteria were: participants who had experienced back pain before, an intervention that consisted of exercises without additional specific treatment and outcomes that measured recurrence of back pain or time to recurrence.
Data collection and analysis
Two review authors independently judged if references met the inclusion criteria. The same review authors independently extracted data and judged the risk of bias of the studies. Studies were divided into post‐treatment intervention programmes and treatment studies. Study results were pooled with meta‐analyses if participants, interventions, controls and outcomes were judged to be sufficiently homogenous.
Main results
We included 13 articles reporting on nine studies with nine interventions. Four studies with 407 participants evaluated post‐treatment programmes and five studies with 1113 participants evaluated exercise as a treatment modality. Four studies had a low risk of bias, one study a high risk and the remainder an unclear risk of bias.
We found moderate quality evidence that post‐treatment exercises were more effective than no intervention for reducing the rate of recurrences at one year (Rate Ratio 0.50; 95% Confidence Interval 0.34 to 0.73). There was moderate quality evidence that the number of recurrences was significantly reduced in two studies (Mean Difference ‐0.35; 95% CI ‐0.60 to ‐0.10) at one‐half to two years follow‐up. There was very low quality evidence that the days on sick leave were reduced by post‐treatment exercises (Mean Difference ‐4.37; 95% CI ‐7.74 to ‐0.99) at one‐half to two years follow‐up.
We found conflicting evidence for the effectiveness of exercise treatment in reducing the number of recurrences or the recurrence rate.
Authors' conclusions
There is moderate quality evidence that post‐treatment exercise programmes can prevent recurrences of back pain but conflicting evidence was found for treatment exercise. Studies into the validity of measurement of recurrences and the effectiveness of post‐treatment exercise are needed.
Plain language summary
Exercises for the prevention of recurrences of episodes of low‐back pain
Back pain is a common disorder that has a tendency to recur. We conducted this review to see if exercises, either as part of treatment or as a post‐treatment programme could reduce back pain recurrences. We searched for studies that included persons with back pain experience, interventions consisting of only exercises and that measured recurrences of back pain.
There were nine studies with 1520 participants. There was moderate quality evidence that post‐treatment exercises can reduce both the rate and the number of recurrences of back pain. However, the results of exercise treatment studies were conflicting.
Adverse (side) effects of exercising were not mentioned in any of the studies. Limitations of this review include the difference in exercises across studies, thus making it difficult to specify the content of such a programme to prevent back pain recurrences.
Summary of findings
Summary of findings for the main comparison. Post‐treatment exercise compared to no intervention for preventing recurrences of low‐back pain.
| Post‐treatment exercise compared to no intervention for preventing recurrences of low‐back pain | ||||||
| Patient or population: patients with recurrences of low‐back pain Settings: Intervention: post‐treatment exercise Comparison: no intervention | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| no intervention | post‐treatment exercise | |||||
| Number of subjects with recurrent LBP Follow‐up: 0.5 to 2 years | Low risk population | RR 0.5 (0.34 to 0.73) | 130 (2 studies) | ⊕⊕⊕⊝ moderate1 | ||
| 10 per 100 | 5 per 100 (3 to 7) | |||||
| High risk population | ||||||
| 70 per 100 | 35 per 100 (24 to 51) | |||||
| Number of subjects with recurrent LBP Follow‐up: 2 to 5 years | Low risk population | RR 0.75 (0.53 to 1.07) | 66 (1 study) | ⊕⊕⊕⊝ moderate2 | ||
| 10 per 100 | 8 per 100 (5 to 11) | |||||
| High risk population | ||||||
| 70 per 100 | 52 per 100 (37 to 75) | |||||
| Time to LBP recurrence self‐report Follow‐up: 0.5 to 2 years | Medium risk population | HR 0.43 (0.21 to 0.87) | 69 (1 study) | ⊕⊕⊕⊝ moderate3 | ||
| 57 per 100 | 30 per 100 (16 to 52) | |||||
| Time to LBP recurrence self‐report Follow‐up: 2 to 5 years | Medium risk population | HR 0.5 (0.28 to 0.9) | 66 (1 study) | ⊕⊕⊕⊝ moderate3 | ||
| 77 per 100 | 52 per 100 (34 to 73) | |||||
| Number of recurrences of LBP recurrences. Scale from: 0 to 10. Follow‐up: 0.5 to 2 years | The mean number of recurrences of lbp in the control groups was 1.44 | The mean Number of recurrences of LBP in the intervention groups was 0.35 lower (0.6 to 0.1 lower) | 154 (2 studies) | ⊕⊕⊕⊝ moderate5 | ||
| Number of recurrences of LBP Scale from: 0 to 10. Follow‐up: 2 to 5 years | The mean number of recurrences of lbp in the control groups was 1.6 | The mean Number of recurrences of LBP in the intervention groups was 1.97 lower (3.84 to 0.1 lower) | 66 (1 study) | ⊕⊕⊕⊝ moderate3 | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; HR: Hazard ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 The studies of Donchin and Soukup had both an unclear risk of bias 2 Soukup 1999 95% CI included both negligible and appreciable benefit 3 Only one small study included 4 The average recurrence in studies with 0.5 to 2 years follow‐up was 1.5 per person 5 Kellett 1991 had a high risk of bias and Soukup 1999 unclear risk of bias
Background
Low‐back pain (LBP) is a major health disorder with a high prevalence rate and heavy burden of cost internationally. The point prevalence of LBP varies between reports and countries from 26.4% in the USA (Deyo 2006) to 19% in Denmark (Harreby 1996), 27% in Hong Kong (Tse 2003), 28.7% in Canada (Cassidy 1998), 16% in England (McKinnon 1997), 14.7% in Australia (Strauss 1993), 13.4% in Norway and 18.2% in Sweden (Ihlebaek 2006). The costs of LBP are enormous and are attributed to both tangible costs (i.e. medical care and indemnity payments) and intangible costs (i.e. production loss, employee retraining, litigation) (Woolf 2003). In the UK, it was estimated that the direct costs of LBP were £1.6 billion and the total costs (direct and indirect) ranged from £6.6 billion to £12.3 billion (Maniadakis 2000). In the US, a comparative cost of illness study showed that the annual per capita health and disability costs for LBP were comparable with heart disease and diabetes in a major US corporation (Druss 2000). Also, LBP is one of the main causes for work absenteeism (Andersson 1999). Expenditures are expected to grow with the trend of an aging population worldwide.
One of the features of back pain is its tendency to recur. In a prospective study in North Carolina, 208 patients, randomly recruited after the first episode of LBP, were followed for 22 months. Thirty‐five per cent to 44% of all patients experienced a recurrence at six‐month follow‐up and 50% to 59% at 22‐month follow‐up (Carey 1999). In other studies, the LBP recurrence rate was found to be even higher, with over 60% of all patients experiencing a recurrence at one‐year follow‐up (Bergquist 1977; Von Korff 1993) These high figures suggest that it is important to find an effective method to prevent recurrences.
For an individual, a new episode of back pain is at the very least an unpleasant experience and is sometimes very debilitating. One complaint of patients about their treatment of back pain is that they do not receive concrete information and instructions from their care providers (Verbeek 2004). Prescribing specific exercises or activities to prevent a recurrence of back pain could help to meet these expectations.
The effectiveness of interventions for treating back pain has been extensively studied. It has been found that staying active is more effective than resting in bed for treating acute back pain (Hagen 2004). In another systematic review, exercise therapy was found to be slightly more effective than no treatment and other conservative treatments in reducing pain and improving function in patients with chronic LBP (Hayden 2005). However, no information about LBP recurrences was used in this review and patients were classified by the duration of their LBP.
It is conceivable that continuing to do exercises could help to prevent recurrences of back pain (Soukup 1999). Some studies have shown that using a specific type of exercise during treatment helped in avoiding recurrences (Cairns 2006; Hides 2001). In a randomised controlled trial using a specific stabilizing exercise for patients after their first episode of LBP, the patients in the exercise group were 2.1 times less likely to suffer from LBP recurrences than those in the control group at three‐year follow‐up (Hides 2001).
This is a relevant question for clinicians, because it means that the focus of treatment should also be directed towards a more preventive perspective. There are reviews that summarized the literature on the prevention of pain severity and duration, and the reduction of sick days and disability from LBP (Lahad 1994; Linton 2001). The preventive interventions investigated in the two reviews included educational strategies, lumbar supports, exercises, ergonomics, and risk factor modification. Based on randomised trials, only exercise was shown to have a consistent, limited effect on the prevention of new episodes of low‐back pain. In these reviews, it was unclear if the back pain episodes were first or recurrent episodes. However, so far no one has reviewed the evidence provided only from randomised controlled trials for preventing recurrences after an episode of back pain.
Objectives
The primary objective of this study is to investigate the effectiveness of exercises for preventing new episodes of low‐back pain or low‐back pain‐associated disability.
Methods
Criteria for considering studies for this review
Types of studies
Only randomised controlled trials (RCTs) are included. We did not use language restrictions for studies but we did not find any relevant studies in languages other than English.
Types of participants
Inclusion criteria
We included studies with both male and female adults, aged 18 or older, who currently had, or had ever had at least one prior episode of non‐specific LBP. Non‐specific LBP is defined as low‐back pain below the costal margin and above the inferior gluteal folds with or without leg pain, that has no specific underlying pathology.
Exclusion criteria
Studies on back pain due to infections, metastatic diseases, neoplasm, osteoarthritis, rheumatoid arthritis, or fractures were excluded as well as studies on back pain related to pregnancy.
Types of interventions
Inclusion criteria
Studies with an exercise intervention aimed at the prevention of recurrences of LBP were included. Exercise were defined as physical activity that is planned or structured and may be done to improve or maintain one or more components of physical fitness (ACSM 2006). The types of exercises were not limited.
We divided exercises into strengthening exercises, endurance training and aerobic exercises. We defined strengthening exercises as exercises to strengthen back and trunk muscles by repeated movements with loads. Endurance training was defined as exercises to increase the endurance of back and trunk muscles by repeated movements with loads. Aerobics were defined as any form of activities to improve cardiopulmonary fitness.
Interventions were further divided into post‐treatment interventions and treatment interventions. Post‐treatment interventions were defined as interventions that were provided to patients after their regular treatment for an episode of back pain had been finished with the explicit aim to prevent new occurrences of back pain. Treatment interventions were defined as treatment for a current episode of back pain with the aim to also prevent new episodes of back pain.
Exclusion criteria
Studies using an exercise intervention that was combined with other interventions such as psychotherapy, specific medication, back school, electro‐physical therapies, or lumbar traction were excluded.
Types of outcome measures
The primary outcome was recurrences of LBP, measured either as frequency or duration of new episodes of LBP within a specified time‐period or the time to a LBP recurrence (time between the previous episode or start of the study and the LBP episode). An episode of LBP was defined as a period of pain in the lower back lasting for more than 24 hours, preceded and followed by a period of at least one month without low‐back pain (De Vet 2002). A recurrence of LBP was defined as an episode of pain, sickness absence or disability resulting from the pain as defined by Wasiak 2009.
The follow‐up times for outcome measures were categorized as short‐term, with a follow‐up of less than half a year; medium‐term, from one‐half to two years; and long‐term, from two to five years after the intervention. We realise that this is an arbitrary categorisation but it seems to fit the increasing frequency of recurrences of back pain, which is the main focus of this review.
Search methods for identification of studies
Electronic searches
We used the search strategy that was developed by the Cochrane Back Review Group (Furlan 2009; van Tulder 2003). We searched CENTRAL (The Cochrane Library 2009, issue 3), MEDLINE, EMBASE and CINAHL up to July 24, 2009. The full search strategies for MEDLINE and EMBASE are outlined in Appendix 1 and Appendix 2; the others are available on request.
Other sources
The reference lists of relevant reviews and papers were screened for additional studies and we also used citation tracking of all relevant trials. We contacted the following authors for additional information: Cherkin, Lonn, Soukup and Donchin.
Data collection and analysis
Study selection
Using the inclusion and exclusion criteria, a pair of review authors (BC, JV, WT) on a rotatory basis independently screened the identified titles and abstracts to choose potentially relevant studies. We obtained the full text of articles for those that appeared to meet the inclusion criteria in order to make the final selection. Disagreements were solved by discussion. A third review author was consulted if disagreements persisted.
Data Extraction
A pair of review authors (BC, JV, WT) on rotatory basis independently extracted the data. We extracted data on participant characteristics, intervention parameters, results of outcomes of interest, duration of outcome measurements, country and sponsorship of the studies. We also checked for any adverse events due to exercises reported in the studies.
To make sure all reviewer authors interpreted the criteria in the same way, we pre‐tested all the forms to be used to assess study eligibility and risk of bias and to extract data by using a set of similar studies on a related topic that was not included in this review. We did not blind the articles since the review authors are familiar with the literature and would recognise the trials.
Risk of bias assessment
The risk of bias was independently assessed by a pair of review authors (BC JV WT) on a rotatory basis, who used a consensus method when disagreements occurred. A third review author was consulted if disagreement persisted.
We used the criteria recommended by the Cochrane Back Review Group (Furlan 2009; van Tulder 2003) to assess the risk of bias of the selected RCTs. The criteria and their operational definitions are outlined in Appendix 3. Each of the criteria was scored "yes", "no" or "unclear", depending on the information supplied in the report. Studies were classified as having a low risk of bias if they fulfilled six or more of the eleven criteria and had no serious flaws. Studies that fulfilled fewer than six criteria were determined to have a high risk of bias. Studies were determined to have an unclear risk of bias if one or more key domains were assessed as unclear (Higgins 2008).
Clinical relevance
We intended to assess the clinical relevance of the included studies according to the following questions as recommended by the Cochrane Back Review Group (Furlan 2009; van Tulder 2003).
Are the patients described in detail so that you can decide whether they are comparable to those that you see in your practice?
Are the interventions and treatment settings described well enough so that you can provide the same for your patients?
Were all clinically relevant outcomes measured and reported?
Is the size of the effect clinically important?
Are the likely treatment benefits worth the potential harms?
When doing so, we realised that it is difficult to assess clinical relevance for preventive interventions as they have a benefit at both individual and group level. Even though the improvements for an individual could be marginal, they still could be worthwhile at the group level.
Data Analysis
Separate analyses were made for post‐treatment exercises that were provided after regular treatment had ended and treatment exercises that were provided as regular treatment for the current episode of back pain and at the same time intended to prevent future episodes of back pain.
Data synthesis
We first decided if studies were sufficiently clinically homogeneous to be able to synthesize the results into one summary measure. Clinically homogeneous studies were defined as those with similar populations, interventions, and outcomes measured at the same follow‐up point. We pooled studies with sufficiently reported numerical data, judged to be clinically homogeneous, with RevMan 4.2 software (RevMan 2003) and later converted to RevMan 5. We tested for statistical heterogeneity and assessed if studies were statistically heterogeneous as judged by the I² measure. If I² was greater than 50% we used a random‐effects model for pooling.
Measures of treatment effect
The results of each trial were plotted as means and standard deviations (SD) for continuous outcomes, risk ratios (RR) for dichotomous outcomes and Hazard Ratios (HR) for time‐to‐event data.
Regardless of whether there were sufficient data available to use quantitative analyses to summarize the data, we assessed the overall quality of the evidence for each outcome using the GRADE approach as described in the Cochrane Handbook (Higgins 2008) and the Cochrane Back Review Group method guidelines (Furlan 2009).
Sensitivity analysis
The results were analysed again by only including studies that had a low risk of bias to find out if the risk of bias altered the synthesized results.
Dealing with missing data
We contacted the following authors of the studies to provide information on missing data: Soukup, Cherkin, Donchin and Lonn. Soukup provided extra information on the nature of the measurement of recurrences. Cherkin was not able to provide additional information on the number of recurrences. Donchin provided extra information on the number of subjects with recurrent LBP. Lonn confirmed in which articles their three‐armed study with different follow‐up times was reported.
We computed Standard Deviations from P values for the duration of episodes in Faas 1998, and for the number of recurrences in Soukup 1999. We calculated Hazard Ratios from the Gehan‐test in Soukup 1999.
Assessment of publication bias
We did not assess publication bias with a funnel plots or Egger's test because we had fewer than five studies in all comparisons (Egger 1997).
Subgroup analysis
We had intended to stratify the included studies by types of exercises such as strengthening, endurance training, and aerobics, to find out the effects of different types of exercises on recurrence of LBP. However, all interventions included all types of exercises except for Hides 2001 who looked specifically at improving the multifidus muscle. The two studies that used the McKenzie exercises were combined separately.
Results
Description of studies
We identified a total of 2053 potentially relevant articles with 102 articles from CENTRAL, 178 from MEDLINE, 1596 from EMBASE and 177 articles from CINAHL. After screening the titles and abstracts of the potential articles, we selected 33 articles to evaluate their full texts and finally included 13 articles in this review. The flow of relevant articles selection is displayed in Figure 1.
1.
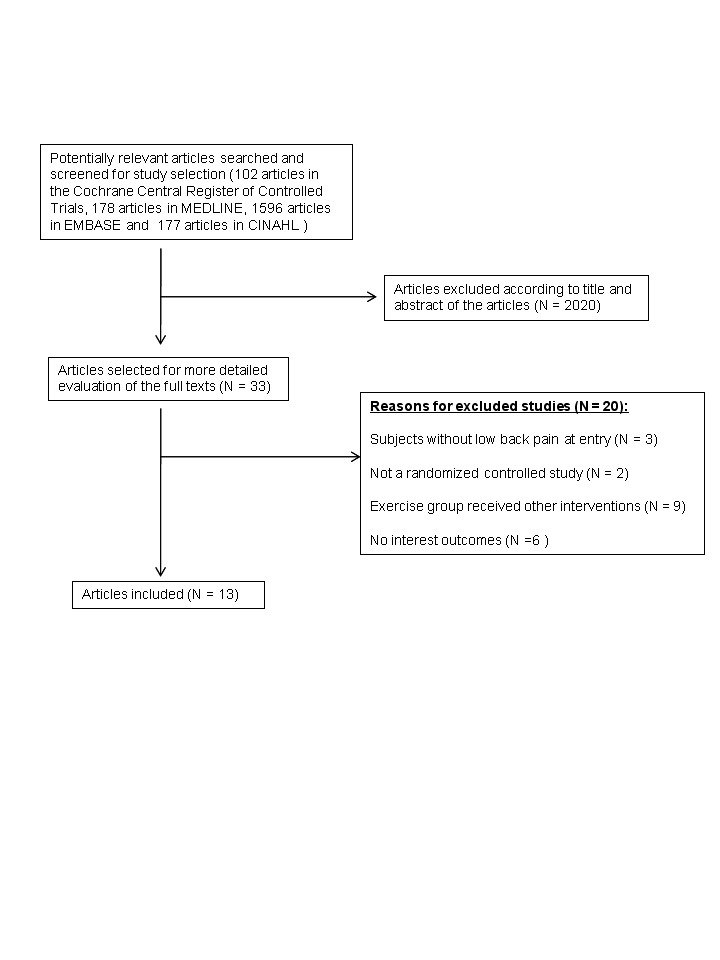
Flowchart for inclusion/exclusion of studies
The Characteristics of included studies table shows the summary of methods, participants, interventions, outcomes and study quality of the included studies (Cherkin 1998; Donchin 1990; Faas 1998; Hagen 2003; Hides 2001; Kellett 1991; Ljunggren 1997; Soukup 1999; Stankovic 1990). Four articles reported on the outcomes of the study at two follow‐up times (Soukup 1999); this was also the case with another two articles (Stankovic 1990). Thus we had 13 articles reporting on nine studies and nine different interventions.
Four interventions were post‐treatment exercises, intended to specifically prevent recurrences of back pain (Donchin 1990; Kellett 1991; Ljunggren 1997; Soukup 1999). The other five interventions were exercises that formed part of the treatment for back pain that were also intended to prevent recurrences of back pain.
The post‐treatment interventions consisted of a mixture of back stretching, leg stretching, muscle contractions and muscle relaxation exercises. In one study, the Mensendieck method of exercises was followed (Soukup 1999). All interventions contained additional advice or information on back pain, such as might be found in a back school. The control treatment in these studies was no intervention (Donchin 1990; Kellett 1991; Soukup 1999) and general exercises (Ljunggren 1997).
The treatment interventions consisted of: general exercises led by a physiotherapist in one study (Faas 1998), promoting physical activity and exercises in one study (Hagen 2003), specific multifidus muscle exercises in one study (Hides 2001) and McKenzie exercises in two studies (Cherkin 1998; Stankovic 1990). The control interventions were sham ultra‐sound therapy (Faas 1998), usual care (Faas 1998; Hagen 2003; Hides 2001), an educational booklet (Cherkin 1998) and a mini‐back school (Stankovic 1990).
In seven studies, recurrences were measured as the number of persons with a recurrence or the rate of recurrence (Cherkin 1998; Donchin 1990; Faas 1998; Hagen 2003; Hides 2001; Soukup 1999; Stankovic 1990). The time to recurrence was measured in one study only (Soukup 1999). The number of recurrences was measured in three studies (Hides 2001; Kellett 1991; Soukup 1999). Episodes of sickness absence and the duration of sick leave were also measured in some of the studies. Three studies had long‐term follow‐up (Hagen 2003; Hides 2001; Stankovic 1990) and all the other studies measured outcomes at medium‐term follow‐up.
Participants in the treatment studies were acute back pain patients in four studies and sub‐acute patients in one study (Hagen 2003); chronic patients were not included in any studies.
Three studies were carried out in Norway, one in Australia, two in Sweden, one in the US, one in the Netherlandsand and one in Israel. Seven studies were carried out in the 1990s and two in the first decennium of the 21st century.
Risk of bias in included studies
Details of the results of the risk of bias assessment of the included studies are shown in Figure 2.
2.
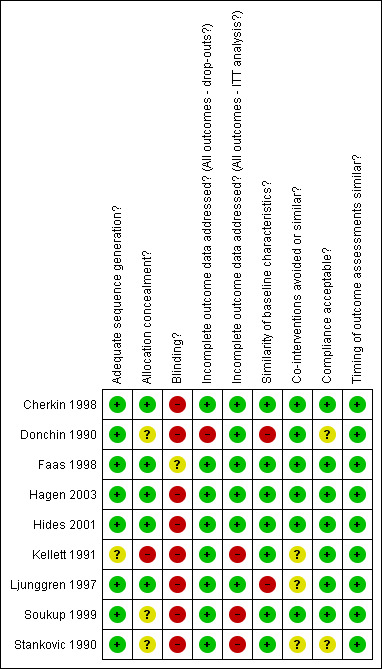
Review authors' judgements for each risk of bias item for each study.
We used the following categorisation for limitations in study design to downgrade the level of evidence. Four studies were assessed as having a low risk of bias (Cherkin 1998; Faas 1998; Hagen 2003; Hides 2001). These studies only failed to meet the blinding requirement which is very difficult to meet in exercise studies where neither the provider, patient nor outcome assessor can be blinded. One study was rated as having a high risk of bias (Kellett 1991), because it had an unclear randomisation procedure in addition to several other risks of bias. The rest of the studies were rated as having an unclear risk of bias, because most studies failed to meet criteria such as concealed allocation, co‐intervention avoidance, and intention‐to‐treat analysis. The level of evidence was downgraded because of serious limitations in study design only when the evidence was based in whole or in part, on results of Kellett 1991.
Effects of interventions
See: Table 1
The recurrence rate as the percentage of persons with a recurrence in the control and intervention groups at one‐half to two years follow‐up was, on average, 58% (range 32% to 80%); at two to five years follow‐up, the rate was, on average, 72% ( range 58% to 88%).The average number of recurrences across studies, in both the control and the intervention group, was 1.5 per person at one‐half to two year follow‐up (range 0.3 to 4.2 per person); at two to five year follow‐up, the average number of recurrences was 2.0 per person (range 1.0 to 3.0 per person). This confirms the general notion that back pain recurs ‐‐– often more than once.
Post‐treatment exercise versus no intervention
There were three studies that evaluated post‐treatment exercise versus no intervention (Donchin 1990; Kellett 1991; Soukup 1999). The number of subjects with recurrences was significantly lower with a RR of 0.50 (95% CI 0.34 to 0.73) at medium‐term follow‐up in two studies (Donchin 1990; Soukup 1999), but not at long‐term follow‐up, with a RR of 0.75 (95% CI 0.53 to 1.07) (Soukup 1999). One study measured the time to recurrence, which yielded a HR of 0.43 (95% CI 0.21 to 0.87) at medium‐term follow‐up (Soukup 1999), and a slightly higher HR 0.50 (95% CI 0.28 to 0.90) at long‐term follow‐up (Soukup 1999). The number of recurrences was measured in two studies (Kellett 1991; Soukup 1999) with a mean difference (MD) of ‐0.35 (95% CI ‐0.60 to ‐0.10) at medium‐term follow‐up, and in one study (Soukup 1999) at long‐term follow‐up with a MD of ‐1.97 (95% CI ‐3.84 to ‐0.10).
Post‐treatment exercise did not influence the number of persons on sick leave as a result of recurrences at medium or long‐term follow‐ups, but did decrease the number of days on sick leave due to recurrences in two studies (Kellett 1991; Soukup 1999) at medium‐term follow‐up with MD of ‐ 4.37 (95% CI ‐7.74 to ‐ 0.99).
In summary, we found moderate quality evidence (serious limitations in design) from two RCTs (Donchin 1990; Soukup 1999, N = 130) that post‐treatment exercises were more effective compared with no intervention in reducing the number of subjects with recurrences at medium‐term follow‐up (RR 0.50; 95% CI 0.34 to 0.73), and moderate quality evidence (serious limitations in design) from two RCTs (Kellett 1991; Soukup 1999, N = 154) that they were more effective at reducing the number of recurrences of back pain at medium‐term follow‐up. For sick leave at medium‐term follow‐up, there is very low quality evidence (serious limitations in design and very serious inconsistency) from two RCTs (Kellett 1991; Soukup 1999, N = 154) that the number of days on sick leave decreased more with post‐treatment exercises than with no intervention.
Post‐treatment exercise plus TerapiMaster machine versus general exercises
One study (Ljunggren 1997) evaluated the effect of an additional exercise machine on the number of days on sick leave. This did not significantly reduce the number of days on sick leave.
Exercise treatment versus care as usual
Exercise as a treatment for acute back pain did not influence the number of persons with recurrences in one big study (Faas 1998) and lowered the number of persons with recurrences in another small study (Hides 2001). The exercises in the latter study were specifically focused on improving the strength of the multifidus muscle. In the same study, the number of recurrences did not decrease nor did the number of subjects on sick leave because of recurrences. In another big study in which persons were encouraged to exercise individually (Hagen 2003), there was no difference in the rate of recurrences between control and intervention groups.
Thus, there was very low quality evidence (limitations in design and serious inconsistency) that the recurrence rate at medium‐term follow‐up (RR 0.63; 95% CI 0.23 to 1.76) from two RCTs (Faas 1998; Hides 2001, N = 358) and at long‐term follow‐up (RR 0.74; 95% CI 0.35 to 1.55) from two RCTs (Hagen 2003; Hides 2001, N = 493) was similar between the exercise and the care as usual group.
Exercise treatment versus sham treatment
Exercise treatment was compared to ultra‐sound sham treatment in one study (Faas 1998; N = 473) but it resulted in neither fewer persons with recurrences nor a shorter duration of recurrent back pain.
McKenzie exercises versus back pain education
McKenzie exercises were compared to back pain education in two studies (Cherkin 1998; Stankovic 1990), which yielded different results on the number of subjects with recurrences. The small study Stankovic 1990 (N = 96) found a significant decrease, both at medium and long‐term follow‐ups, but the big study Cherkin 1998 (N = 323) did not find a decrease. However, the pooled results found no significant difference in the number of subjects who had recurrences (RR 0.75; 95% CI 0.42 to 1.35; N = 294) in the medium‐term follow‐up.
There was no significant difference in the number of days on sick leave between those who had McKenzie exercises and those who received back pain education at medium (MD ‐13.10; 95% CI ‐30.79 to 4.59; N = 95) and long‐term (MD ‐19.80; 95% CI ‐86.53 to 46.93; N = 89) follow‐ups in one study (Stankovic 1990).
In summary, there was very low quality evidence (limitations in design, serious inconsistency and imprecision) from two RCTs (Cherkin 1998; Stankovic 1990, N = 294) that McKenzie exercises are similar to back pain education at reducing recurrences of back pain at medium‐term follow‐up and very low quality evidence (very serious imprecision) from one RCT (Stankovic 1990) that the number of sick leave days is similar after back pain education in the medium and long‐term follow‐ups.
Sensitivity analyses
Meta‐analyses were conducted with only the studies at low risk of bias. One post‐treatment study was at an especially high risk of bias (Kellett 1991). Leaving this study out did not decrease the evidence for post‐treatment exercise considerably.
Adverse events due to exercises
There were no reports of adverse events mentioned in any of the selected studies.
Discussion
We found that the recurrence rate and the number of recurrences of back pain could be reduced and the time to recurrence could be prolonged by providing post‐treatment exercises. The number of days on sick leave in the post‐treatment follow‐up period was reduced by post‐treatment exercises but not the rate of sick leave in the post‐treatment period. We found conflicting results for the effectiveness of exercise treatment in reducing the number of recurrences or the recurrence rate.
The overall quality of the evidence was moderate with four studies assessed as having a low risk of bias, most studies an unclear risk of bias and only one study a high risk of bias. However, the post‐treatment exercise studies in particular had a higher risk of bias, which makes it difficult to draw strong conclusions.
The strength of our review is that we are the first to systematically look into recurrences as an outcome of back pain interventions. Outcome measurement in back pain is difficult as there are many ways to measure back pain. Even though the recurrence rate and the number of recurrences seem a straight forward outcome, studies show that this is not the case (Stanton 2009). Wasiak has studied the differences in recurrence rates based on differences in definitions and found a great difference if he used care‐based or lost‐work‐time‐based definitions (Wasiak 2003; Wasiak 2009). This is reflected in the outcomes found in this review, where different definitions of recurrences yielded different results. However, we found that the number of recurrences increased with longer follow‐up over most studies. This finding increases the probability of a valid measurement of recurrences.
We divided the studies into post‐treatment exercises and treatment exercise studies. This approach can potentially answer the question about whether we should have more exercise‐directed treatment during an episode of back pain, or whether we should encourage and possibly supervise exercises after treatment that are geared towards preventing recurrences. This review suggests that the latter is more effective in preventing recurrences of LBP. Even though we made a clear distinction between post‐treatment and treatment studies, this was not always clear from the studies themselves. Some studies clearly stated that they were post‐treatment and the patients should be at work (Soukup 1999), while others just recruited participants who had experienced at least three episodes of back pain in the past (Donchin 1990). However, the intention of all these studies was to prevent recurrences and the outcomes were measured as recurrences of back pain.
The judgement of clinical relevance was difficult. Most of the included studies described the patients and treatments in detail but we were not able to identify potential harms in the included studies. In prevention studies in general, it is difficult to assess a clinically important size of the effect since even small effects can be worthwhile at the group level. It is mainly a matter of cost‐effectiveness that is used to judge if preventive interventions are worthwhile. The effects in the post‐treatment studies were considerable, with a relative risk reduction of 25% for the recurrence rate and 22% reduction in the number of recurrences. These effects are certainly clinically worthwhile (Table 2).
1. Clinical relevance.
| Study | Patient Description | Treatment description | All outcomes reported | Outcome size clinically important | Benefits worth the harms |
| Cherkin 1998 | yes | yes | yes | no | yes |
| Doncin 1990 | no | no | no | unclear | unclear |
| Faas 1998 | yes | yes | yes | yes | yes |
| Hagen 2003 | yes | no | yes | yes | yes |
| Hides 2001 | yes | yes | yes | yes | yes |
| Kellett 1991 | yes | yes | yes | unclear | yes |
| Ljungren 1997 | yes | yes | no | yes | yes |
| Soukup 1999 | yes | yes | yes | yes | yes |
| Stankovic 1995 | no | yes | no | unclear | yes |
The exercises that were prescribed in the various studies incorporated more or less similar ingredients, except for the multifidus muscles exercises studied by Hides 2001 and the McKenzie exercises, as shown in Table 3. Therefore it is difficult to make inferences about the content of the interventions. There was a wide variation in the rate and number of recurrences between studies that we could not explain and that might be due to differences in measurement, biomechanical exposure or low exercise levels.
2. Details of exercise intervention.
| Study | Exercise protocol | Back stretching | Leg stretching | Leg mobilization | Back mobilization | Abdomen strength | Back strength | Relaxation exercise | Back care advice |
| Cherkin 1998 | 9 times, supervision by physiotherapist | ++ | ? | ? | ++ | ? | ++ | ? | ‐ |
| Donchin 1990 | 45 minutes each session, 24 sessions, twice a week for 3 months, supervision by physical education instructor | ‐ | ‐ | ‐ | ++ | ++ | + | ‐ | + |
| Faas 1998 | 20 minutes each session, 10 sessions, twice a week for 5 weeks, supervision by physiotherapist | + | + | ‐ | + | + | + | ‐ | ++ |
| Hagen 2003 | Protocol not mentioned, supervision by a physiotherapist | ? | ? | ++ | ? | ? | ? | ‐ | +++ |
| Hides 2001 | 8 sessions, twice a week | ‐ | ‐ | ‐ | ? | +++ | +++ | ‐ | ++ |
| Kellett 1991 | 35‐45 minutes each session, supervision by physiotherapist and physical fitness instructor | + | + | + | + | + | + | + | + |
| Ljunggren 1997 | 15‐30 minutes each session, 144 sessions, triple a week for a year, supervision by physiotherapist | + | ‐ | ++ | ++ | ++ | ++ | ++ | ‐ |
| Soukup 1999 | 1 hour each session, 20 sessions, twice a week for first 7 weeks; once a week for last 6 weeks, supervision by physiotherapist | + | ++ | ‐ | ++ | ++ | ++ | + Breathing relaxation | ++ |
| Stankovic 1990 | 20 minutes each session, 2 sessions, separated by 2 weeks | + | ‐ | ‐ | ++ | ++ | ++ | ‐ | + |
Key: ‐ does not contain; + contains some of it; ++ consists mostly of it; +++ consists entirely of it
The picture that emerges from this review is that post‐treatment exercises likely reduce the rate and the number of recurrences and the days on sick leave, and increase the time to recurrence. If the rate of recurrences is reduced, then it is unclear why this is not reflected in the rate of sick leave, but the duration of sick leave is reduced. This would mean that even though the same number of persons start sick leave, they return to work sooner as a result of doing exercises.
For exercise therapy, the evidence is conflicting. It is unclear why post‐treatment exercise would be more beneficial than exercise treatment. It could be possible that post‐treatment exercises focus more on changing behaviour and treatment exercises are considered treatment and stopped after the treatment programme is finished.
We could not formally assess publication bias due to a lack of comparable studies. However, the studies with the most positive results are small and the results are not replicated in larger studies. It is therefore probable that publication bias plays some role in this review.
Authors' conclusions
Implications for practice.
It might be beneficial to have additional exercise programmes after formal treatment for back pain has been completed. The content of such a programme is difficult to specify because the contents varied and did not relate to the outcomes. Therefore, any general exercise such as stretching, strengthening, endurance training and posture education could be adequate.
Treatment does not seem to influence the number of recurrences in acute and sub‐acute back pain patients and is therefore best focused on the treatment outcome for the current episode.
Implications for research.
Prevention of recurrences of back pain is a little studied but clinically relevant back pain outcome. Studies that better validate the measurement of recurrences of back pain are needed. Intervention studies should at least address the rate, the number of and the time to recurrences of LBP. Given the low number of studies found, more studies are needed to evaluate post‐treatment supervised and non‐supervised exercise programmes.
What's new
| Date | Event | Description |
|---|---|---|
| 19 January 2011 | Amended | Contact details updated. |
History
Protocol first published: Issue 2, 2007 Review first published: Issue 1, 2010
| Date | Event | Description |
|---|---|---|
| 17 February 2010 | Amended | Contact details updated. |
| 22 August 2008 | Amended | Converted to new review format. |
Acknowledgements
We would like to express our sincere gratitude toward Vicki Pennick, Managing Editor of the Cochrane Back Review Group and Dr. Tang Jin‐Ling, Professor of the Department of Community and Family Medicine, The Chinese University of Hong Kong, who provided us with expert advice during the development of this systematic review. Also, we thank Rachel Couban, Trials Search Co‐ordinator of the Cochrane Back Review Group, for her professional assistance with the development of the search strategies. We would like to acknowledge the help of the Cochrane Occupational Health Field in the realisation of this review.
Appendices
Appendix 1. MEDLINE search strategy
1. exp "Clinical Trial [Publication Type]"/ 2. randomized.ab,ti. 3. placebo.ab,ti. 4. dt.fs. 5. randomly.ab,ti. 6. trial.ab,ti. 7. groups.ab,ti. 8. or/1‐7 9. Animals/ 10. Humans/ 11. 9 not (9 and 10) 12. 8 not 11 13. dorsalgia.ti,ab. 14. exp Back Pain/ 15. backache.ti,ab. 16. (lumbar adj pain).ti,ab. 17. coccyx.ti,ab. 18. coccydynia.ti,ab. 19. sciatica.ti,ab. 20. sciatica/ 21. spondylosis.ti,ab. 22. lumbago.ti,ab. 23. or/13‐22 24. exp Exercise/ 25. exercis$.mp. 26. physical exercis$.mp. 27. exp Exercise Therapy/ 28. exp Exercise Movement Techniques/ 29. exp Physical Therapy Modalities/ 30. McKenzie.mp. 31. Alexander.mp. 32. William.mp. 33. feldenkrais.mp. 34. exp Yoga/ 35. exp Recreation/ 36. or/24‐35 37. exp Alexander Disease/ 38. exp Williams Syndrome/ 39. 37 or 38 40. 36 not 39 41. exp Recurrence/ 42. recur$.mp. 43. relaps$.mp. 44. reappearance$.mp. 45. reoccurence$.mp. 46. return.mp. 47. or/41‐46 48. 12 and 23 and 40 and 47
Appendix 2. EMBASE search strategy
1. Clinical Article/ 2. exp Clinical Study/ 3. Clinical Trial/ 4. Controlled Study/ 5. Randomized Controlled Trial/ 6. Major Clinical Study/ 7. Double Blind Procedure/ 8. Multicenter Study/ 9. Single Blind Procedure/ 10. Phase 3 Clinical Trial/ 11. Phase 4 Clinical Trial/ 12. crossover procedure/ 13. placebo/ 14. or/1‐13 15. allocat$.mp. 16. assign$.mp. 17. blind$.mp. 18. (clinic$ adj25 (study or trial)).mp. 19. compar$.mp. 20. control$.mp. 21. cross?over.mp. 22. factorial$.mp. 23. follow?up.mp. 24. placebo$.mp. 25. prospectiv$.mp. 26. random$.mp. 27. ((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).mp. 28. trial.mp. 29. (versus or vs).mp. 30. or/15‐29 31. 14 and 30 32. human/ 33. Nonhuman/ 34. exp ANIMAL/ 35. Animal Experiment/ 36. 33 or 34 or 35 37. 32 not 36 38. 31 not 36 39. 37 and 38 40. 38 or 39 41. dorsalgia.mp. 42. back pain.mp. 43. exp BACKACHE/ 44. (lumbar adj pain).mp. 45. coccyx.mp. 46. coccydynia.mp. 47. sciatica.mp. 48. exp ISCHIALGIA/ 49. spondylosis.mp. 50. lumbago.mp. 51. or/41‐50 52. exp Exercise/ 53. exercis$.mp. 54. exp Kinesiotherapy/ 55. physical exercise.mp. 56. exercise therapy.mp. 57. McKenzie.mp. 58. exp ALEXANDER TECHNIQUE/ 59. Alexander.mp. 60. William.mp. 61. exp FELDENKRAIS METHOD/ 62. Feldenkrais.mp. 63. exp YOGA/ 64. yoga.mp. 65. or/52‐64 66. Alexander disease.mp. or exp Alexander Disease/ 67. Williams Beuren Syndrome.mp. or exp Williams Beuren Syndrome/ 68. or/66‐67 69. 65 not 68 70. recur$.mp. 71. relaps$.mp. 72. reappearance$.mp. 73. reoccurence$.mp. 74. return.mp. 75. exp RELAPSE/ 76. or/69‐75 77. 40 and 51 and 69 and 76
Appendix 3. Criteria and definitions for risk of bias assessment (van Tulder 2003)
Was the method of randomisation adequate? A random (unpredictable) assignment sequence. Examples of adequate methods are computer‐generated random numbers table and use of sealed opaque envelopes. Methods of allocation using date of birth, date of admission, hospital numbers, or alternation should not be regarded as appropriate.
Was the treatment allocation concealed? Assignment generated by an independent person not responsible for determining the eligibility of the patients. This person has no information about the persons included in the trial and has no influence on the assignment sequence or on the decision about eligibility of the patient.
Was knowledge of the allocated interventions adequately prevented during the study?
Was the patient blinded to the intervention? The review author determines if enough information about the blinding is given in order to score a "yes."
Was the care provider blinded to the intervention? The review author determines if enough information about the blinding is given in order to score a "yes."
Was the outcome assessor blinded to the intervention? The review author determines if enough information about the blinding is given in order to score a "yes."
Were incomplete outcome data adequately addressed?
Was the drop‐out rate described and acceptable? The number of participants who were included in the study but did not complete the observation period or were not included in the analysis must be described and reasons given. If the percentage of withdrawals and drop‐outs does not exceed 20% for immediate and short‐term follow‐ups, 30% for intermediate and long‐term follow‐ups and does not lead to substantial bias a "yes" is scored.
Did the analysis include an intention‐to‐treat analysis? All randomised patients are reported/analyzed in the group to which they were allocated by randomisation for the most important moments of effect measurement (minus missing values), irrespective of noncompliance and co‐interventions.
Other sources of potential bias:
Were the groups similar at baseline regarding the most important prognostic indicators? In order to receive a "yes," groups have to be similar at baseline regarding demographic factors, duration and severity of complaints, percentage of patients with neurological symptoms, and value of main outcome measure(s).
Were co‐interventions avoided or similar? Co‐interventions should either be avoided in the trial design or be similar between the index and control groups.
Was the compliance acceptable in all groups? The review author determines if the compliance to the interventions is acceptable, based on the reported intensity, duration, number and frequency of sessions for both the index intervention and control intervention(s).
Was the timing of the outcome assessment in all groups similar? Timing of outcome assessment should be identical for all intervention groups and for all important outcome assessments.
Appendix 4. Clinical relevance assessment
Are the patients described in detail so that you can decide whether they are comparable to those that you see in your practice?
Are the interventions and treatment settings described well enough so that you can provide the same for your patients?
Were all clinically relevant outcomes measured and reported?
Is the size of the effect clinically important?
Are the likely treatment benefits worth the potential harms?
Data and analyses
Comparison 1. Post‐treatment Exercise vs No Intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of subjects with recurrent LBP | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 follow‐up 1/2 to 2 years | 2 | 130 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.34, 0.73] |
| 1.2 follow‐up 2‐5 years | 1 | 66 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.53, 1.07] |
| 2 Time to LBP recurrence | 1 | Hazard Ratio (Random, 95% CI) | Subtotals only | |
| 2.1 follow‐up 1/2 to 2 years | 1 | Hazard Ratio (Random, 95% CI) | 0.43 [0.21, 0.87] | |
| 2.2 follow‐up 2 to 5 years | 1 | Hazard Ratio (Random, 95% CI) | 0.50 [0.28, 0.90] | |
| 3 Number of recurrences of LBP | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 follow‐up 1/2 to 2 years | 2 | 154 | Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.60, ‐0.10] |
| 3.2 follow‐up 2 to 5 years | 1 | 66 | Mean Difference (IV, Random, 95% CI) | ‐1.97 [‐3.84, ‐0.10] |
| 4 Number of subjects with sick leave due to recurrent LBP | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 follow‐up 1/2 to 2 years | 2 | 154 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.50, 1.41] |
| 4.2 follow‐up 2‐5 years | 1 | 66 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.48, 1.38] |
| 5 Days of sick leave due to recurrent LBP | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 follow‐up 1/2 to 2 years | 2 | 154 | Mean Difference (IV, Fixed, 95% CI) | ‐4.37 [‐7.74, ‐0.99] |
| 5.2 follow‐up 2‐5 years | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | ‐11.5 [‐54.24, 31.24] |
1.1. Analysis.
Comparison 1 Post‐treatment Exercise vs No Intervention, Outcome 1 Number of subjects with recurrent LBP.
1.2. Analysis.
Comparison 1 Post‐treatment Exercise vs No Intervention, Outcome 2 Time to LBP recurrence.
1.3. Analysis.
Comparison 1 Post‐treatment Exercise vs No Intervention, Outcome 3 Number of recurrences of LBP.
1.4. Analysis.
Comparison 1 Post‐treatment Exercise vs No Intervention, Outcome 4 Number of subjects with sick leave due to recurrent LBP.
1.5. Analysis.
Comparison 1 Post‐treatment Exercise vs No Intervention, Outcome 5 Days of sick leave due to recurrent LBP.
Comparison 2. Post treatment Exercise plus Terapimaster machine vs General exercise.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of sick leave days due to recurrent LBP | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only |
2.1. Analysis.
Comparison 2 Post treatment Exercise plus Terapimaster machine vs General exercise, Outcome 1 Number of sick leave days due to recurrent LBP.
Comparison 3. Exercise Treatment vs Usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of subjects with recurrent LBP | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 follow‐up 1/2 to 2 years | 2 | 348 | Risk Ratio (M‐H, Random, 95% CI) | 0.63 [0.23, 1.76] |
| 1.2 follow‐up 2‐5 years | 2 | 493 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.35, 1.55] |
| 2 Duration of recurrent LBP | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3 Number of recurrences of LBP | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 follow‐up 1/2 to 2 years | 1 | 39 | Mean Difference (IV, Random, 95% CI) | ‐1.40 [‐3.16, 0.36] |
| 3.2 follow‐up 2 to 5 years | 1 | 36 | Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐3.88, 3.08] |
| 4 Number of subjects with sick leave due to recurrent LBP | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 follow‐up 1/2 to 2 years | 1 | 39 | Risk Ratio (M‐H, Random, 95% CI) | 0.36 [0.11, 1.15] |
| 4.2 follow‐up 2‐5 years | 1 | 36 | Risk Ratio (M‐H, Random, 95% CI) | 0.8 [0.24, 2.71] |
3.1. Analysis.
Comparison 3 Exercise Treatment vs Usual care, Outcome 1 Number of subjects with recurrent LBP.
3.2. Analysis.
Comparison 3 Exercise Treatment vs Usual care, Outcome 2 Duration of recurrent LBP.
3.3. Analysis.
Comparison 3 Exercise Treatment vs Usual care, Outcome 3 Number of recurrences of LBP.
3.4. Analysis.
Comparison 3 Exercise Treatment vs Usual care, Outcome 4 Number of subjects with sick leave due to recurrent LBP.
Comparison 4. Exercise Treatement vs Sham Ultrasound.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of subjects with recurrent LBP (follow‐up 1/2 to 2 years) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2 Duration of recurrent LBP | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only |
4.1. Analysis.
Comparison 4 Exercise Treatement vs Sham Ultrasound, Outcome 1 Number of subjects with recurrent LBP (follow‐up 1/2 to 2 years).
4.2. Analysis.
Comparison 4 Exercise Treatement vs Sham Ultrasound, Outcome 2 Duration of recurrent LBP.
Comparison 5. Specific McKenzie Exercise Treatment vs Minimal booklet/back school.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of subjects with recurrent LBP | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 follow‐up 1/2 to 2 years | 2 | 294 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.42, 1.35] |
| 1.2 follow‐up 2‐5 years | 1 | 89 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.57, 0.92] |
| 2 Number of sick leaves caused by recurrent LBP | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 follow‐up 1/2 to 2 years | 1 | 95 | Mean Difference (IV, Random, 95% CI) | ‐13.10 [‐30.79, 4.59] |
| 2.2 follow‐up 2‐5 years | 1 | 93 | Mean Difference (IV, Random, 95% CI) | ‐19.80 [‐86.53, 46.93] |
5.1. Analysis.
Comparison 5 Specific McKenzie Exercise Treatment vs Minimal booklet/back school, Outcome 1 Number of subjects with recurrent LBP.
5.2. Analysis.
Comparison 5 Specific McKenzie Exercise Treatment vs Minimal booklet/back school, Outcome 2 Number of sick leaves caused by recurrent LBP.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Cherkin 1998.
| Methods | Randomised, controlled, concealed allocation, and intention‐to‐treat basis. No blinding. | |
| Participants | Adults with LBP for 7 days. Total participants eligible for the study was 323. After excluding 2 participants, the further intervention and analysis were performed on the following distribution: Booklet group, N = 66; Chiropractic group, N = 122; Physical therapy group, N = 133; Inclusion criteria: all who did not meet exclusion criteria. Exclusion criteria: mild or no pain 7 days after the visit to the physician, history of back surgery, sciatica, or severe concurrent illnesses. 169 men and 154 women, mean age 41 years in exercise group, 40 years in both Chiropractic manipulation group and control group. |
|
| Interventions | Exercise group: Subjects received McKenzie exercise class by physiotherapists within four days after randomisation for first visit and up to eight more visits. Patients received a self‐learning book and a lumbar cushion. Chiropractic manipulation group: Subjects received chiropractic manipulation by chiropractors within four days after randomisation for first visit and up to eight more visits. Chiropractors could suggest exercises and activity restriction as their usual practices. Minimal‐intervention control group: Subjects received an educational booklet only. |
|
| Outcomes | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | After baseline assessment, subjects were randomly assigned without stratification. |
| Allocation concealment? | Low risk | Adequate, the use of sealed and opaque envelopes. |
| Blinding? All outcomes | High risk | No blinding reported. |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | Low risk | Between 89 and 96 percent of the subjects responded to the follow‐up questionnaires. |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | ITT was used to address the loss of follow‐up outcomes. |
| Similarity of baseline characteristics? | Low risk | Most baseline characteristics were similar except that subjects in the physical therapy group had more bothersome symptoms and subjects in the educational‐booklet group reported fewer days with restricted activity. |
| Co‐interventions avoided or similar? | Low risk | The reported use of exercise was almost identical in all groups at baseline and 1 month. |
| Compliance acceptable? | Low risk | Around 96 percent of the subjects complied with their assigned visits to the care provider at least once. |
| Timing of outcome assessments similar? | Low risk | Outcomes were assessed 1, 4, 12, 52 and 104 weeks after the beginning of study in all groups. |
Donchin 1990.
| Methods | Randomised, controlled, and intention‐to‐treat basis. No reports of concealed allocation and blinding. | |
| Participants | Hospital employees reporting at least 3 annual episodes of LBP. Total of 142 hospital employees were assigned to: Calisthetics for the back (CAL) group, N = 46; Back school group, N = 46; Control group, N = 50; 48 men and 94 women, mean age 45 years in Calisthenics group, 48 years in Back school group, and 45 years in Control group. All who agreed took part in the study. |
|
| Interventions | Post‐ treatment Calisthenics exercise group: Subjects underwent 45 minutes exercise, bi‐weekly for 3 months. Flexion and pelvic tilt exercise, based on the Williams method, aimed at strengthening the abdominal muscles, expanding spinal forward flexion, and rectifying the general posture. Back school group: Subjects received four 90 minutes sessions during a 2‐week period plus a fifth session after 2 months. The physiotherapist taught proper body mechanics and exercises for back and abdominal muscles. Home exercise was encouraged for the subjects. Control group: No intervention. |
|
| Outcomes | Number of subjects with recurrent low‐back pain. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | The subjects were allocated to the three groups by a systematic random sampling method. |
| Allocation concealment? | Unclear risk | Unclear. |
| Blinding? All outcomes | High risk | No blinding reported. |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | High risk | Not stated. |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | ITT analysis was used. |
| Similarity of baseline characteristics? | High risk | Calisthenics group had more subjects with a more recent episode and more painful days before intervention. |
| Co‐interventions avoided or similar? | Low risk | |
| Compliance acceptable? | Unclear risk | Not stated. |
| Timing of outcome assessments similar? | Low risk | Outcomes were assessed after 3 months of intervention and after an additional 6 months of follow‐up. |
Faas 1998.
| Methods | Randomised, placebo‐controlled, concealed allocation, and intention‐to‐treat basis. | |
| Participants | Patients who consulted their general practitioner for a new LBP episode. Total of 473 participants were assigned to: Exercise group, N = 156; Usual care group, N = 155; Placebo group, N = 162; 270 men and 203 women, mean age 36 years in exercise group, 36 years in usual care group and 38 years in sham Ultrasound group. Inclusion criteria: pain between T‐12 and the gluteal folds with or without radiation into the upper leg, pain for 3 weeks or less and age between 16 and 65 years. Exclusion criteria: Radiation pain below the knee, nerve compression, previous back episode within 2 moths before entry, and back surgery. |
|
| Interventions | Exercise group: Subjects were instructed individually by a physiotherapist for 20 minutes twice a week for 5 weeks. The exercises consisted of semi‐fowler resting position, a resting position with knees on the chest, a limbering exercise by alternating side movements with knees bent, a stretching exercise of the iliopsoas , pelvic flexion in supine position, in hand‐knee and in up‐right position, and isometric abdominal exercises. Advices on daily activities were suggested. Usual care group: Subjects received information on back pain and was given analgesics on demand without further therapy. Sham Ultrasound group: Subjects received Ultrasonography for 20 minutes by a physiotherapist, twice a week for 5 weeks with the lowest possible dose next to zero (0.1 watt/cm2, intermittent, no heat effect). |
|
| Outcomes | Number of subjects with recurrent LBP, and duration of recurrent LBP. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Random assignment was performed in blocks of six for each general practitioner. |
| Allocation concealment? | Low risk | Adequate, The doctor's assistant handed to the patient a sealed envelope containing the kind of therapy. |
| Blinding? All outcomes | Unclear risk | No blinding reported. |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | Low risk | 23 subjects in usual care group, 17 in placebo group and 20 in exercise group dropped out. |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | ITT analysis was used. |
| Similarity of baseline characteristics? | Low risk | All baseline characteristics were not significantly different. |
| Co‐interventions avoided or similar? | Low risk | Close to zero dose of Ultrasonography was given in placebo group. |
| Compliance acceptable? | Low risk | 75% of intervention group and 89% of placebo group complied with the treatment. |
| Timing of outcome assessments similar? | Low risk | Outcomes were assessed 2 and 4 weeks, 1 year after the beginning of study in all groups. |
Hagen 2003.
| Methods | Randomised, controlled, concealed allocation, and intention‐to‐treat basis. | |
| Participants | Patients sick‐listed for at least 8 weeks for LBP, mean age 41 years. Total 437 participants were randomised into: Intervention group, N = 237; Control group, N = 220; Inclusion criteria: age 18 to 60 years, a sick leave of 8 to 12 weeks. Exclusion criteria: pregnancy, recent low‐back trauma, and concurrent disorders. |
|
| Interventions | Exercise group: Subjects were advised and instructed individually by physiotherapists in how to train and stretch at home, coping with daily activities at home and work, and how to resume normal activities. Control group: Subjects were treated within the primary health care. |
|
| Outcomes | Number of subjects with recurrent LBP, and days of sick leaves due to LBP. | |
| Notes | 510 people were randomised. The study analysis is based on the following distribution: Intervention, N = 237; Control, N = 220; It appears that 53 participants dropped out after being randomised, which is 10.4% of the population, but before the beginning of the intervention. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | Low risk | Adequate. |
| Blinding? All outcomes | High risk | Patients and providers not blinded; unclear if outcome assessors were blinded: 'data from the National Insurance Office'. |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity of baseline characteristics? | Low risk | |
| Co‐interventions avoided or similar? | Low risk | There were no significant differences between the intervention and the control group in the use of analgesics, contacting the physician and relaxation as coping strategies to reduce LBP. |
| Compliance acceptable? | Low risk | |
| Timing of outcome assessments similar? | Low risk | |
Hides 2001.
| Methods | Randomised, controlled, concealed allocation, and single‐blinded (outcome assessor). | |
| Participants | Patients with acute, first‐episode LBP. For this study, total of 39 participants were accepted. 16 men and 23 women, mean age 31 years. Intervention group, N = 20; Control group, N = 19; Inclusion criteria: participants of both genders, age 18 to 45 years, first episode of LBP for less than 3 weeks, presented to the accident and emergency department. Exculsion criteria: provided elsewhere. |
|
| Interventions | Exercise group: Subjects performed specific localized exercises aimed at restoring the stabilizing protective function of the multifidus, twice a week for 4 weeks. Usual care group: Subjects received medical management, including advice on bed rest, absence from work, prescription of medication, and advice to resume normal activity as tolerated. |
|
| Outcomes | Number of subjects with recurrent LBP, number of recurrences of LBP, and number of subjects with sick leave due to LBP. | |
| Notes | This is a follow‐up study. The original study is not included in the review. It is possible that the N participants in the original study was greater than N=39 identified for the follow‐up. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | Low risk | Adequate. |
| Blinding? All outcomes | High risk | Patient's and Providers not blinded; Outcome assessor blinded: 'research assistant who was blinded to group allocation'. |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | Outcomes for patients lost to follow‐up imputed. |
| Similarity of baseline characteristics? | Low risk | |
| Co‐interventions avoided or similar? | Low risk | |
| Compliance acceptable? | Low risk | |
| Timing of outcome assessments similar? | Low risk | |
Kellett 1991.
| Methods | No reports of randomisation process, concealed allocation, and blinding. | |
| Participants | Employees of Scandinavia's major producer of kitchen units. Inclusion criteria: self‐reported current or previous back pain. Exclusion criteria: any period of sick leave longer than 50 days. 59 men and 26 women, mean age 41 years in exercise group and 42 years in control group. Total 125 participants were recruited. After initial dropouts, 58 were randomly selected to form an exercise group, and 53 for a control group. |
|
| Interventions | Post‐treatment exercise group: Subjects participated in the exercise programme once a week during working hours for one and half years. Intensity of exercise was progressively increased according to the comfort of subjects. Each session started with a warm‐up and gentle stretching exercises and continued with strengthening, cardiovascular fitness exercises, and coordination exercises. Control group: No report. |
|
| Outcomes | Number of recurrences of LBP, number of subjects with sick leave due to LBP, and days of sick leaves due to LBP. | |
| Notes | After random selection, the further analysis is based on the following distribution of participants: Intervention group, N = 37; Control group, N = 48. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | No other information provided than '58 individuals were randomly selected to form the exercise group'. |
| Allocation concealment? | High risk | No other information provided than '58 individuals were randomly selected to form the exercise group'. |
| Blinding? All outcomes | High risk | Outcome assessor: 'sick leave data from the National Insurance Board'. Patients and providers not blinded. |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | High risk | 14 control participants dropped out after randomisation and before intervention. |
| Similarity of baseline characteristics? | Low risk | |
| Co‐interventions avoided or similar? | Unclear risk | No information provided about medical treatment even though all participants reported current or previous back pain. |
| Compliance acceptable? | Low risk | |
| Timing of outcome assessments similar? | Low risk | |
Ljunggren 1997.
| Methods | Randomised, concealed allocation, and intention‐to‐treat basis. No control and blinding. | |
| Participants | The study was conducted at four physiotherapy centres in southern Norway. Participants were selected after ordinary physio treatment for LBP. Inclusion criteria: both genders, age 18 to 65 years, and history of back problems. Exclusion criteria: participants for whom any of exercises were contraindicated. Total of 153 participants were included and 126 completed. The analysis is based on 126 participants. Terapimaster group, N = 62; Conventional Training group, N = 64; 70 men and 56 women, mean age 40 years in Conventional exercise group and 39 years in TerapiMaster exercise group. |
|
| Interventions | Post‐ treatment TerapiMaster programme group: Subjects underwent an exercise programme for one year, which consisted of 9 back, abdominal and whole body strengthening exercises by TerapiMaster device in 3 sets of 10 repetitions for 15 to 30 minutes each session, 3 sessions a week at home. Progression in the programme, decided in cooperation with the physiotherapist, was done by adding extra weights. Conventional exercise programme: Subjects underwent a conventional exercise programme for one year, without TerapiMaster device at home. The exercise programme was consisted of 9 back, abdominal and whole body strengthening exercises in 3 sets of 10 repetitions for 15 to 30 minutes each session, 3 sessions a week. |
|
| Outcomes | Days of sick leaves due to LBP. | |
| Notes | There was no mentioning of the initial numbers of participants randomised into Intervention group and a control group. Dropout rate is 17.6%. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | Low risk | Adequate. |
| Blinding? All outcomes | High risk | Patients and providers not blinded; outcome assessment was by self‐report. |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity of baseline characteristics? | High risk | Fewer men in the intervention group. |
| Co‐interventions avoided or similar? | Unclear risk | No information provided on regular medical treatment. |
| Compliance acceptable? | Low risk | |
| Timing of outcome assessments similar? | Low risk | |
Soukup 1999.
| Methods | Randomised, controlled, and intention‐to‐treat basis. No reports of concealed allocation and blinding. | |
| Participants | Most subjects were recruited from outpatient medical, chiropractic and physiotherapy practices in south‐east Norway. Supervised Mensendieck arm: total 77 participants were randomised into a Mensendieck exercise group (N = 39). 12 month follow‐up: During the 12 month of follow‐up treatment, 5 participants dropped out. Analysis is performed on N = 34. 3‐year follow‐up: the analysis included Mensendieck group, N = 31. Control group for both intervention and all follow‐ups was (N = 38). During the 12 month of follow‐up treatment, 3 participants dropped out. Dropouts are discussed, but excluded from the analysis. Analysis is performed on N = 35. Inclusion criteria: men and women 18 to 50 years old who had experienced one or more episodes of pain localised to the lumber region, with or without pain radiation to the lower extremities. It was required that patients had finished their treatment for LBP episode prior to enrolment. Exclusion criteria: back surgery, pregnancy, specific diseases, and spinal fracture. |
|
| Interventions | Post‐treatment Mensendieck exercise group: Subjects received exercises and biomechanical/ ergonomic education in 20 sessions of 60 minutes each for 13 weeks, twice a week for first 7 weeks and once a week for the last 6 weeks. Each session was consisted of warm‐up and stretching exercises for 15 minutes, a combination of ergonomic education and pelvic, hip, back, and abdominal exercises for 35 minutes, and stretching and relaxation exercises for 10 minutes. Control group: Subjects did not receive any attention but were free to choose other treatments for LBP or engage in other physical activities. Apart from the follow‐up assessments, the group did not receive any further attention or information. |
|
| Outcomes | Number of subjects with recurrent LBP, number of recurrences of LBP, time to LBP recurrences, number of subjects with sick leave due to LBP, and days of sick leaves due to LBP. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Subjects were randomised in blocks of six to maintain a consistent class size. |
| Allocation concealment? | Unclear risk | Unclear. |
| Blinding? All outcomes | High risk | No blinding reported. |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | Low risk | No significant difference was found between the two groups with regard to drop‐out rate and time until drop out (5 in intervention and 3 in control). |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | High risk | No ITT analysis. |
| Similarity of baseline characteristics? | Low risk | No statistically significant difference between the intervention and control group was found in baseline characteristics. |
| Co‐interventions avoided or similar? | Low risk | No exercise was given in control group. |
| Compliance acceptable? | Low risk | Average compliance: 85%; Range: 65‐100%. |
| Timing of outcome assessments similar? | Low risk | Outcomes were measured at baseline and 1 year. |
Stankovic 1990.
| Methods | Randomised, controlled, concealed allocation, and intention‐to‐treat basis. No report of blinding. | |
| Participants | Patients with acute LBP. Total of 100 participants were randomised into: Initially, McKenzie group (group 1) consisted of (N = 50) and a "Mini Back School" (group2) of (N = 50). Statistical analysis is performed on McKenzie group, N = 49, and a"Mini Back School", N = 46. Inclusion criteria: being employed. Exclusion criteria: participants with chronic LBP, pregnancy, and back surgery. 77 men and 23 women, mean age 34 years. 5‐year follow‐up included 89 of the initial subjects: 67 men and 22 women, mean age 40 years. McKenzie group (group 1), N = 47; a "Mini Back School" (group2), N = 42. |
|
| Interventions | McKenzie exercise group: The patients received 20 minutes session with emphasis on maintaining the lordosis at all times with or without lumbar support. Subjects were instructed to do back extension exercise in prone position by repeated full elbows extended while keeping the pelvis, hips and legs relaxed on a table, then in standing position. After 2 weeks training, subjects continued with flexion in lying, in sitting and in standing. Postural and ergonomic instructions were given. Subjects were instructed to continue the training programme by themselves. Mini‐back school group: Subjects only received back school education without exercises, consisting one 45 minutes lesson to discuss back anatomy and function, strain‐relieving positions and the importance of staying active. 5‐year follow‐up included: McKenzie exercise group (N = 47): the same exercise as described the above; Mini‐back school group (N = 42): the same education as described the above. |
|
| Outcomes | Number of subjects with recurrent LBP, and days of sick leaves due to LBP. | |
| Notes | Dropouts are not discussed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 100 subjects were randomised into two groups by drawing a sealed envelope with random numbers, which had been produced by a random‐number generator. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | High risk | No blinding reported. |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | Low risk | It was observed from the result table for 1 year follow‐up that there were 4 dropouts. For 5‐year follow‐up the dropout rate increased to 11 participants. |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | High risk | No ITT analysis. |
| Similarity of baseline characteristics? | Low risk | It was reported that no difference in several demographical variables (age, occupation and derangements). |
| Co‐interventions avoided or similar? | Unclear risk | Not mentioned. |
| Compliance acceptable? | Unclear risk | Not mentioned. |
| Timing of outcome assessments similar? | Low risk | Outcomes were measured at baseline and 5 years. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Alexandre 2001 | The exercise group received other intervention (back school). |
| Amako 2003 | All of the included subjects had no low‐back pain at entry of the study. |
| Buchbinder 2002 | The article is a synopsis. |
| Cairns 2006 | The exercise group received other interventions such as manual therapy, electrotherapy, and lumbar traction. |
| Gundewall 1993 | The subjects did not experience back pain before. Impossible to extract recurrences from the data. |
| Helewa 1999 | All of the included subjects had no low‐back pain at entry of the study. |
| Hides 1996 | The exercise group received other non‐exercise interventions such as medications (analgesics). No interest outcomes were found in the study. |
| Hlobil 2005 | Behavioural approach was co‐intervention. |
| Kofotolis 2005 | The article is a review. |
| Koumantakis 2005 | No relevant outcome was found in the study. |
| Koumantakis 2005a | No relevant outcome was found in the study. |
| Kuukkanen 2000 | No relevant outcome was found in the study. |
| Leclaire 1996 | In both arms physiotherapy was a co‐intervention. |
| Maul 2005 | No relevant outcome was found in the study. |
| Medina 1995 | The exercise group received other non‐exercise interventions. |
| Sjogren 2006 | No relevant outcomes were found in the study. |
| Staal 2004 | Behavioural approach was co‐intervention. |
| Suni 2006 | No relevant outcome was found in the study. |
Differences between protocol and review
In the protocol we stated that we would divide studies into high and low quality. In the time this review was written, the GRADE approach for grading the level of evidence seemed more appropriate to use. Therefore we left our original idea and used the GRADE approach instead.
Contributions of authors
Brian Choi ‐ registered title, formed review team, wrote protocol, developed search strategy with CBRG editorial office assistance, ran searches, selected references, developed and tested data extraction forms, wrote the text of the review.
Jos Verbeek ‐ formed review team, wrote protocol, helped with development of search strategy, ran searches, selected references, developed and tested data extraction forms, wrote the text of the review.
Wilson Tam ‐ ran searches, selected references, developed and tested data extraction forms.
Yu Jiang ‐ ran searches, developed and tested data extraction forms.
Declarations of interest
There is no potential conflict of interest among the review authors.
Edited (no change to conclusions)
References
References to studies included in this review
Cherkin 1998 {published data only}
- Cherkin, DC, R A Deyo, M Battie, J Street, W Barlow. A comparison of physical therapy, chiropractic manipulation, and provision of an educational booklet for the treatment of patients with low back pain. New England Journal of Medicine 1998;339(15):1021‐9. [DOI] [PubMed] [Google Scholar]
Donchin 1990 {published data only}
- Donchin, M, O Woolf, L Kaplan, Y Floman. Secondary prevention of low‐back pain. A clinical trial. Spine 1990;15(12):1317‐20. [DOI] [PubMed] [Google Scholar]
Faas 1998 {published data only}
- Faas, A, A W Chavannes, J T van Eijk, J W Gubbels. A randomized, placebo‐controlled trial of exercise therapy in patients with acute low back pain. Spine 1993;18(11):1388‐95. [PubMed] [Google Scholar]
Hagen 2003 {published data only}
- Hagen EM, Grasdal A, Eriksen HR. Does early intervention with a light mobilization program reduce long‐term sick leave for low back pain: A 3‐year follow‐up study. Spine 2003;28(20):2309‐15. [DOI] [PubMed] [Google Scholar]
Hides 2001 {published data only}
- Hides JA, Jull GA, Richardson CA. Long‐term effects of specific stabilizing exercises for first‐episode low back pain. Spine 2001;26(11):E243‐8. [DOI] [PubMed] [Google Scholar]
Kellett 1991 {published data only}
- Kellett KM, Kellett DA, Nordholm LA. Effects of an exercise program on sick leave due to back pain. Physical Therapy 1991;71(4):283‐93. [DOI] [PubMed] [Google Scholar]
Ljunggren 1997 {published data only}
- Ljunggren AE, Weber H, Kogstad O, Thom E, Kirkesola G, Nordin M. Effect of exercise on sick leave due to low back pain: A randomized, comparative, long‐term study. Spine 1997;22(14):1610‐7. [DOI] [PubMed] [Google Scholar]
Soukup 1999 {published data only}
- Glomsrød B, Lønn JH, Soukup MG, Bo K, Larsen S. "Active back school", prophylactic management for low back pain: three‐year follow‐up of a randomized, controlled trial. Journal of Rehabilitation Medicine 2001;33(1):26‐30. [DOI] [PubMed] [Google Scholar]
- Lønn JH, Glømsrod B, Soukup MG, Bo K, Larsen S. Active back school: prophylactic management for low back pain: A randomized, controlled, 1‐year follow‐up study. Spine 1999;24(9):865‐71. [DOI] [PubMed] [Google Scholar]
- Soukup MG, Glømsrod B, Lønn JH, Bo K, Larsen S. The effect of a Mensendieck exercise program as secondary prophylaxis for recurrent low back pain. A randomized, controlled trial with 12‐month follow‐up. Spine 1999;24(15):1585‐91; discussion 1592. [DOI] [PubMed] [Google Scholar]
- Soukup MG, Lønn J, Glømsrod B, Bo K, Larsen S. Exercises and education as secondary prevention for recurrent low back pain. Physiotherapy research international : the journal for researchers and clinicians in physical therapy 2001;6:27‐39. [DOI] [PubMed] [Google Scholar]
Stankovic 1990 {published data only}
- Stankovic R, Johnell O. Conservative treatment of acute low back pain. A 5‐year follow‐up study of two methods of treatment. Spine 1995;20(4):469‐72. [DOI] [PubMed] [Google Scholar]
- Stankovic R, Johnell O. Conservative treatment of acute low‐back pain. A prospective randomized trial: McKenzie method of treatment versus patient education in "mini back school". Spine 1990;15(2):120‐3. [PubMed] [Google Scholar]
References to studies excluded from this review
Alexandre 2001 {published data only}
- Alexandre NMC, Moraes MAA, Correa Filho HR, Jorge SA. Evaluation of a program to reduce back pain in nursing personnel. Revista de Saude Publica 2001;35(4):356‐61. [DOI] [PubMed] [Google Scholar]
Amako 2003 {published data only}
- Amako M, Oda T, Masuoka K, Yokoi H, Campisi P. Effect of static stretching on prevention of injuries for military recruits. Military Medicine 2003;168(6):442‐6. [PubMed] [Google Scholar]
Buchbinder 2002 {published data only}
Cairns 2006 {published data only}
- Cairns MC, Foster NE, Wright C. Randomized controlled trial of specific spinal stabilization exercises and conventional physiotherapy for recurrent low back pain. Spine 2006;31(19):E670‐81. [DOI] [PubMed] [Google Scholar]
Gundewall 1993 {published data only}
- Gundewall B, Liljeqvist M, Hansson T. Primary prevention of back symptoms and absence from work: A prospective randomized study among hospital employees. Spine 1993;18(5):587‐94. [DOI] [PubMed] [Google Scholar]
Helewa 1999 {published data only}
- Helewa A, Goldsmith CH, Lee P, Smythe HA, Forwell L. Does strengthening the abdominal muscles prevent low back pain ‐ A randomized controlled trial. Journal of Rheumatology 1999;26(8):1808‐15. [PubMed] [Google Scholar]
Hides 1996 {published data only}
- Hides JA, Richardson CA, Jull GA. Multifidus muscle recovery is not automatic after resolution of acute, first‐episode low back pain. Spine 1996;21:2763‐9. [DOI] [PubMed] [Google Scholar]
Hlobil 2005 {published data only}
- Hlobil, H, J B Staal, J Twisk, A Koke, G Ariens, T Smid, W van Mechelen. The effects of a graded activity intervention for low back pain in occupational health on sick leave, functional status and pain: 12‐month results of a randomized controlled trial. Journal of Occupational Rehabilitation 2005;15(4):569‐80. [DOI] [PubMed] [Google Scholar]
Kofotolis 2005 {published data only}
- Kofotolis N, Sambanis M. The influence of exercise on musculoskeletal disorders of the lumbar spine. Journal of Sports Medicine & Physical Fitness 2005;45(1):84‐92. [PubMed] [Google Scholar]
Koumantakis 2005 {published data only}
- Koumantakis GA, Watson PJ, Oldham JA. Supplementation of general endurance exercise with stabilisation training versus general exercise only. Physiological and functional outcomes of a randomized controlled trial of patients with recurrent low back pain. Clinical Biomechanics, 2005;20(5):474‐82. [DOI] [PubMed] [Google Scholar]
Koumantakis 2005a {published data only}
- Koumantakis GA, Watson PJ, Oldham JA. Trunk muscle stabilization training plus general exercise versus general exercise only: randomized controlled trial of patients with recurrent low back pain. Physical Therapy 2005;85(3):209‐25. [PubMed] [Google Scholar]
Kuukkanen 2000 {published data only}
- Kuukkanen TM, Malkia EA. An experimental controlled study on postural sway and therapeutic exercise in subjects with low back pain. Clinical Rehabilitation 2000;14(2):192‐202. [DOI] [PubMed] [Google Scholar]
Leclaire 1996 {published data only}
- Leclaire R, Esdaile JM, Suissa S, Rossignol M, Proulx R, Dupuis M. Back school in a first episode of compensated acute low back pain: a clinical trial to assess efficacy and prevent relapse. Archives of physical medicine and rehabilitation 1996;77:673‐9. [DOI] [PubMed] [Google Scholar]
Maul 2005 {published data only}
- Maul I, Laubli T, Oliveri M, Krueger H. Long‐term effects of supervised physical training in secondary prevention of low back pain. European Spine Journal 2005;14(6):599‐611. [DOI] [PMC free article] [PubMed] [Google Scholar]
Medina 1995 {published data only}
- Medina MF, Brotons RJ, Manrique SJ. Comparative study on the influence of health education on perceived recurrences after physiotherapy [Spanish]. Atencion Primaria 1995;16(8):464‐8. [PubMed] [Google Scholar]
Sjogren 2006 {published data only}
- Sjogren T, Nissinen KJ, Jarvenpaa SK, Ojanen MT, Vanharanta H, Malkia EA. Effects of a workplace physical exercise intervention on the intensity of low back symptoms in office workers: A cluster randomized controlled cross‐over design. Journal of Back & Musculoskeletal Rehabilitation 2006;19(1):13‐24. [Google Scholar]
Staal 2004 {published data only}
- Staal JB, Hlobil H, Twisk JW, Smid T, Koke AJ, Mechelen W. Graded activity for low back pain in occupational health care. Annals of Internal Medicine 2004;140(2):77‐84. [DOI] [PubMed] [Google Scholar]
Suni 2006 {published data only}
- Suni J, Rinne M, Natri A, Statistisian MP, Parkkari J, Alaranta H. Control of the lumbar neutral zone decreases low back pain and improves self‐evaluated work ability: a 12‐month randomized controlled study. Spine 2006;31(18):E611‐20. [DOI] [PubMed] [Google Scholar]
Additional references
ACSM 2006
- ACSM. Benefits and Risks associated with Physical Activity. In: Whaley MH editor(s). ACSM's guidelines for exercise testing and prescription. 7th Edition. London: Lippincott Williams & Wilkins, 2006. [Google Scholar]
Andersson 1999
- Andersson GB. Epidemiological features of chronic low‐back pain. Lancet 1999;354:581‐5. [DOI] [PubMed] [Google Scholar]
Bergquist 1977
- Bergquist‐Ullman M, Larsson U. Acute low back pain in industry. A controlled prospective study with special reference to therapy and confounding factors. Acta Orthopaedica Scandinavica 1977;170:1‐117. [DOI] [PubMed] [Google Scholar]
Carey 1999
- Carey TS, Garrett JM, Jackman A, Hadler N. Recurrence and care seeking after acute back pain: results of a long‐term follow‐up study. North Carolina back pain project. Medical Care 1999;37(2):157‐64. [DOI] [PubMed] [Google Scholar]
Cassidy 1998
- Cassidy JD, Carroll LJ, Côté P. The Saskatchewan health and back pain survey. The prevalence of low back pain and related disability in Saskatchewan adults. Spine 1998;23(17):1860‐7. [DOI] [PubMed] [Google Scholar]
De Vet 2002
- Vet HCW, Heymans MW, Dunn KM, Pope DP, Beek AJ, Macfarlane GJ, et al. Episodes of Low Back Pain: A proposal for Uniform definitions to be used in research. Spine 2002;27:2409‐16. [DOI] [PubMed] [Google Scholar]
Deyo 2006
- Deyo RA, Mirza SK, Martin BI. Back pain prevalence and visit rates: estimates from U.S. national surveys, 2002. Spine 2006;31(23):2724‐7. [DOI] [PubMed] [Google Scholar]
Druss 2000
- Druss BG, Rosenheck RA, Sledge WH. Health and disability costs of depressive illness in a major U.S. corporation. American Journal of Psychiatry 2000;157(8):1274‐8. [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315(7109):629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Furlan 2009
Hagen 2004
- Hagen KB, Hilde G, Jamtvedt G, Winnem M. Bed rest for acute low‐back pain and sciatica. Cochrane Database of Systematic Reviews 2004, Issue 4. [DOI: 10.1002/14651858.CD001254.pub2] [DOI] [PubMed] [Google Scholar]
Harreby 1996
- Harreby M, Kjer J, Hesselsoe G, Neergaard K. Epidemiological aspects and risk factors for low back pain in 38‐year‐old men and women: a 25‐year prospective cohort study of 640 school children. European Spine Journal 1996;5(5):312‐8. [DOI] [PubMed] [Google Scholar]
Hayden 2005
- Hayden JA, Tulder MW, Malmivaara A, Koes BW. Exercise therapy for treatment of non‐specific low back pain. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD000335.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions. Chichester: John Wiley & Sons, 2008. [Google Scholar]
Ihlebaek 2006
- Ihlebaek C, Hansson TH, Laerum E, Brage S, Eriksen HR, Holm SH, et al. Prevalence of low back pain and sickness absence: a "borderline" study in Norway and Sweden. Scandinavian Journal of Public health 2006;34(5):555‐8. [DOI] [PubMed] [Google Scholar]
Lahad 1994
- Lahad A, Malter AD, Berg AO, Deyo RA. The effectiveness of four interventions for the prevention of low back pain. JAMA. 1994;272(16):1286‐91. [PubMed] [Google Scholar]
Linton 2001
- Linton SJ, Tulder MW. Preventive interventions for back and neck pain problems: what is the evidence?. Spine 2001;26(7):778‐87. [DOI] [PubMed] [Google Scholar]
Maniadakis 2000
- Maniadakis N, Gray A. The economic burden of back pain in the UK. Pain 2000;84(1):95‐103. [DOI] [PubMed] [Google Scholar]
McKinnon 1997
- McKinnon ME, Vickers MR, Ruddock VM, Townsend J, Meade TW. Community studies of the health service implications of low back pain. Spine 1997;22(18):2161‐6. [DOI] [PubMed] [Google Scholar]
RevMan 2003 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 4.2 for Windows. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2003.
Stanton 2009
- Stanton TR, Latimer J, Maher CG, Hancock M. Definitions of Recurrence of an Episode of Low Back Pain: A Systematic Review. Spine 2009;34(9):E316‐22. [DOI] [PubMed] [Google Scholar]
Strauss 1993
- Strauss S, Guthrie F, Nicolisi F. Prevalence of pain complaints in a general population: an Australian study. Australian Association Musculoskeletal Medicine Bulletin 1993;9:54–61. [Google Scholar]
Tse 2003
- Tse LY, Lam TH, Yip HK. Physical Health. Report on Population Health Survey. Department of Health, Hong Kong. 2003/2004:31.
van Tulder 2003
- Tulder M, Furlan A, Bombardier C, Bouter L. Updated method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group. Spine 2003;28(12):1290‐9. [DOI] [PubMed] [Google Scholar]
Verbeek 2004
- Verbeek J, Sengers MJ, Riemens L, Haafkens J. Patient expectations of treatment for back pain: a systematic review of qualitative and quantitative studies. Spine 2004;29(20):2309‐18. [DOI] [PubMed] [Google Scholar]
Von Korff 1993
- Korff M, Deyo RA, Cherkin D, Barlow W. Back pain in primary care. Outcomes at 1 year. Spine 1993;18(7):855‐62. [DOI] [PubMed] [Google Scholar]
Wasiak 2003
- Wasiak R, Pransky G, Verma S, Webster B. Recurrence of low back pain: definition‐sensitivity analysis using administrative data. Spine 2003;28(19):2283‐91. [DOI] [PubMed] [Google Scholar]
Wasiak 2009
- Wasiak R, Young AE, Dunn KM, Côté P, Gross DP, Heymans MW, et al. Back Pain Recurrence: An Evaluation of Existing Indicators and Direction for Future Research. Spine 2009;34(9):970‐7. [DOI] [PubMed] [Google Scholar]
Woolf 2003
- Woolf AD, Hazes JM, Akesson K, Khaltaev N, Cimmino M, Dieppe P, et al. The Burden of Musculoskeletal Conditions at the Start of the New Millennium. Report of a WHO Scientific Group, in WHO Technical Report Series; 919. 2003:102‐3.


