Abstract
Background
For many years, topical use of fluorides has gained greater popularity than systemic use of fluorides. A possible adverse effect associated with the use of topical fluoride is the development of dental fluorosis due to the ingestion of excessive fluoride by young children with developing teeth.
Objectives
To describe the relationship between the use of topical fluorides in young children and the risk of developing dental fluorosis.
Search methods
Electronic search of the Cochrane Oral Health Group Trials Register, CENTRAL, MEDLINE, EMBASE, BIOSIS, Dissertation Abstracts and LILACS/BBO. Reference lists from relevant articles were searched. Date of the most recent searches: 9th March 09.
Selection criteria
Randomised controlled trials (RCTs), quasi‐RCTs, cohort studies, case‐control studies and cross‐sectional surveys, in which fluoride toothpastes, mouthrinses, gels, foams, paint‐on solutions, and varnishes were compared to an alternative fluoride treatment, placebo or no intervention group. Children under the age of 6 years at the time topical fluorides were used.
Data collection and analysis
Data from all included studies were extracted by two review authors. Risk ratios for controlled, prospective studies and odds ratios for case‐control studies or cross‐sectional surveys were extracted or calculated. Where both adjusted and unadjusted risk ratios or odds ratios were presented, the adjusted value was included in the meta‐analysis.
Main results
25 studies were included: 2 RCTs, 1 cohort study, 6 case‐control studies and 16 cross‐sectional surveys. Only one RCT was judged to be at low risk of bias. The other RCT and all observational studies were judged to be at moderate to high risk of bias. Studies were included in four intervention/exposure comparisons. A statistically significant reduction in fluorosis was found if brushing of a child's teeth with fluoride toothpaste commenced after the age of 12 months odds ratio 0.70 (random‐effects: 95% confidence interval 0.57 to 0.88) (data from observational studies). Inconsistent statistically significant associations were found between starting using fluoride toothpaste/toothbrushing before or after the age of 24 months and fluorosis (data from observational studies). From the RCTs, use of higher level of fluoride was associated with an increased risk of fluorosis. No significant association between the frequency of toothbrushing or the amount of fluoride toothpaste used and fluorosis was found.
Authors' conclusions
There should be a balanced consideration between the benefits of topical fluorides in caries prevention and the risk of the development of fluorosis. Most of the available evidence focuses on mild fluorosis. There is weak unreliable evidence that starting the use of fluoride toothpaste in children under 12 months of age may be associated with an increased risk of fluorosis. The evidence for its use between the age of 12 and 24 months is equivocal. If the risk of fluorosis is of concern, the fluoride level of toothpaste for young children (under 6 years of age) is recommended to be lower than 1000 parts per million (ppm).
More evidence with low risk of bias is needed. Future trials assessing the effectiveness of different types of topical fluorides (including toothpastes, gels, varnishes and mouthrinses) or different concentrations or both should ensure that they include an adequate follow‐up period in order to collect data on potential fluorosis. As it is unethical to propose RCTs to assess fluorosis itself, it is acknowledged that further observational studies will be undertaken in this area. However, attention needs to be given to the choice of study design, bearing in mind that prospective, controlled studies will be less susceptible to bias than retrospective and/or uncontrolled studies.
Plain language summary
Is the use of fluoride toothpaste during early childhood associated with discolouration/mottling of teeth?
There is strong evidence that the use of toothpaste containing fluoride can prevent tooth decay (caries) in both children and adults. However, a possible adverse effect associated with the use of fluoride toothpaste is the mottling of permanent teeth due to the swallowing of excessive fluoride by young children with developing teeth. This dental fluorosis can range from, typically, mild white patches on the teeth to severe mottling of the teeth with brown staining. The aim of this review was to evaluate whether the use of fluoride toothpaste by children is associated with an increased risk of developing dental fluorosis in children. The review included 25 studies of different designs; some providing stronger evidence than others. There is some evidence that brushing a child's teeth with a toothpaste containing fluoride, before the age of 12 months, may be associated with an increased risk of developing fluorosis. There is stronger evidence that higher levels of fluoride (1000 parts per million (ppm) or more) in toothpaste are associated with an increased risk of fluorosis when given to children under 5 to 6 years of age. However, for some children (those considered to be at high risk of tooth decay by their dentist), the benefit to health of preventing decay may outweigh the risk of fluorosis. In such circumstances, careful brushing by parents/adults with toothpastes containing higher levels of fluoride would be beneficial.
Background
Use of fluorides has been the most important caries prevention method since the introduction of water fluoridation in the 1940s (Kargul 2003).
For many years, the topical use of fluorides has gained greater popularity than systemic use of fluorides. The term 'topical fluoride application' is used here to describe methods that provide fluoride to exposed tooth surfaces at a high concentration for a local protective effect. Fluoride containing toothpastes (dentifrices), mouthrinses, gels and varnishes are the most commonly used topical fluoride agents. These can be used individually or in combination and have been shown to significantly reduce caries in children (Marinho 2002; Marinho 2002b; Marinho 2003; Marinho 2003b; Marinho 2003c; Marinho 2004; Marinho 2004b; Walsh 2010). Unlike the systemic use of fluoride such as fluoride tablets, the topically applied fluorides are not intended for ingestion. Despite this, as the fluorides are put into the mouth, they will eventually be ingested if not removed from the mouth after application. Much of the ingested fluorides will be absorbed by the body and produce systemic effects (Ekstrand 1996).
A possible adverse effect associated with the use of topical fluoride is the development of dental fluorosis due to the ingestion of excessive fluoride by young children with developing teeth. Dental fluorosis is a hypomineralization of tooth enamel caused by the ingestion of an amount of fluoride that is above the optimal level during enamel formation. Clinically, the appearance of teeth with fluorosis depends on the severity of the condition. In its mildest form, there are faint white lines or streaks visible only to trained examiners under controlled examination conditions. In more involved cases, fluorosis manifests as mottling of the teeth in which noticeable white lines or streaks often have coalesced into larger opaque areas. In the most severe form, brown staining or pitting of the tooth enamel may be present and actual breakdown of the enamel may occur (Pendrys 2000; Rozier 1994).
The exact mechanism through which dental fluorosis develops is not fully understood. There is some evidence in support of the hypothesis that excessive levels of fluoride can interfere with dental enamel formation and cause fluorosis (Chen 2006; Kubota 2005).
The use of topical fluorides in young children is usually associated with inadvertent ingestion and systemic absorption of fluoride. The amount of fluoride ingested depends upon several factors, including the fluoride concentration of the product, quantity used, suction use, etc and may range from approximately 0.1 mg, in the case of dentifrices and mouthrinses, to more than 20 mg, in the case of professionally applied fluoride gels without proper suction (Barnhart 1974; Ekstrand 1987; Lecompte 1987). Although the very mild forms of dental fluorosis do not pose a public health problem, more severe forms will be of aesthetic concern, especially when the upper front teeth are substantially involved. Depending on the magnitude of the alteration in tooth appearance, the severity of fluorosis and the vulnerability of an individual to psychological harm, there can be different degrees of interference with a person's quality of life. There is a need to get the appropriate balance between the beneficial and harmful effects of topical fluoride therapies (Do 2007).
There have been some earlier traditional narrative reviews on the use of topical fluorides and the risk of developing dental fluorosis (Levy 1994; Pendrys 1990; Stookey 1994). However, a systematic quantitative evaluation of the available evidence has never been undertaken.
Objectives
The primary objective of this systematic review was to describe the relationship between the use of topical fluorides in young children and the risk of developing dental fluorosis.
This review attempted to evaluate the available evidence of different topical fluoride treatment modalities (including gels, toothpastes, varnishes and mouthrinses) used at different concentrations, and at varying duration of use/exposure in increasing the risk of developing dental fluorosis in children with different exposure to systemic fluoride (such as water or salt fluoridation).
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs), quasi‐RCTs, cohort studies, case‐control studies and cross‐sectional surveys in which fluoride toothpastes, mouthrinses, gels, foams, paint‐on solutions and varnishes were compared to an alternative fluoride treatment, placebo or no intervention group.
Types of participants
Children under the age of 6 years at the time topical fluorides were used.
Types of interventions
Topical fluoride therapy (TFT) in the form of toothpastes, mouthrinses, gels, foams, paint‐on solutions and varnishes, using any fluoride agent (which may be formulated with any compatible abrasive system, in the case of fluoride toothpastes), at any concentration (ppm F), amount or duration of application, and with any technique or method of application, provided the frequency of application was at least once a year. The comparison group was an alternative fluoride treatment group or placebo (for any method of fluoride application) or no intervention (except for brushing or flossing methods of application) resulting in the following comparison: Any single TFT described above compared with an alternative TFT or placebo or no TFT.
Types of outcome measures
The primary outcome measure was the percentage prevalence of fluorosis in the permanent dentition. The timing of the outcome measurement should have been taken when most of permanent teeth of interest were erupted in the study subjects.
If available, the prevalence of fluorosis for each tooth type was recorded.
In measuring the percentage prevalence of fluorosis, all children with fluorosis according to the index used were classified as 'fluorosed' as opposed to normal. As measured by the common epidemiologic indices for dental fluorosis (Rozier 1994), children with a TSIF (Tooth Surface Index of Fluorosis), TFI (Thylstrup and Fejerskov Index) score greater than zero or Dean’s classification of 'questionable' or higher were classified as fluorosed.
If the other indices were used, the percentage prevalence of fluorosis as reported by the original investigators using other methods (e.g. photographic method or other index) was to be considered and adopted.
Search methods for identification of studies
With a comprehensive search, we attempted to identify all relevant studies irrespective of language. Papers not in English were considered and translated.
Electronic searches
Relevant studies were identified by searching several electronic databases from date of inception:
The Cochrane Oral Health Group Trials Register (whole database to 9 March 2009)
The Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2009, Issue 1)
MEDLINE (1950 to 9 March 2009)
EMBASE (1980 to 9 March 2009)
BIOSIS (1969 to 9 March 2009)
Dissertation Abstracts (1900 to 9 March 2009)
LILACS/BBO (1982 to 9 March 2009).
A sensitive search strategy using controlled vocabulary and free text terms was developed for each database (seeAppendices).
Searching other resources
Reference lists
All eligible studies retrieved from the searches, meta‐analyses and review articles were checked for relevant references. Reference lists of relevant chapters from preventive dentistry textbooks on topically applied fluoride interventions were also reviewed.
Handsearching
Prospective handsearching of five journals (Community Dentistry and Oral Epidemiology, Caries Research, Journal of Dental Research, British Dental Journal, Journal of Public Health Dentistry) as identified as having the highest yield of eligible clinical studies (at least two) was carried out from January 2007.
Personal contact
Searching for unpublished studies (or 'grey' literature such as technical reports and dissertations, or studies published in languages other than English which may not have been indexed to major databases) by contacting experts in the field of preventive dentistry and oral epidemiology was carried out.
Data collection and analysis
Management of records produced by the searches
Because multiple databases were searched, the downloaded sets of records from each database, starting with MEDLINE, were imported to the bibliographic software package EndNote Library and merged into one core database to remove duplicate records and to facilitate retrieval of relevant articles.
Relevance assessment
All records identified by the searches were printed and checked first on the basis of title, then by abstract (when this was available in English or in languages known by the review authors) and/or keywords by one review author. Records that were obviously irrelevant were discarded and the full text of all remaining records obtained. Records were considered irrelevant according to study design/duration, participants, or interventions/comparisons (if the article was a case report; or the study was not on children younger than 6 years old; or the study did not address one of the topical fluoride therapies (TFTs); or the study did not compare a TFT to an alternative TFT or placebo or no treatment).
Selection of studies for inclusion
An inclusion criteria form was prepared and pilot tested, one review author assessed all studies for inclusion in the review, and a second review author independently duplicated the process. A third review author was consulted to achieve consensus.
Data extraction and management
Data from all included studies were extracted by two review authors independently using a pilot tested data extraction form. Again, any disagreements were discussed and a third review author consulted to achieve consensus where necessary. If data were presented only in graphs and figures, we intended to extract it where possible, however, this did not occur in any of the included studies. Data were extracted from tables and text for all included studies. Attempts were made to contact authors in order to obtain missing information or for clarification whenever necessary. Papers not in English had the data extracted with help from appropriate translation.
Descriptive data that were extracted from each study in addition to those described for participants, interventions, outcome measures and methodological quality include: exposure to other fluorides, mode and setting of use, year study started, country/place of study, duration of study, age at which topical fluoride was used, dose of fluoride, duration of use, level of caries reduction.
In addition, outcomes may have been assessed at more than one period of follow‐up. We intended to make decisions on which outcome assessment timing to use however once again this did not occur in the included studies.
Assessment of risk of bias
An assessment of the risk of bias in included studies was undertaken following the recommendations as described in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions 5.0.1 (Higgins 2008).
A specific tool for assessing risk of bias in each included study was adopted. This comprised a description and a judgement for each entry in a risk of bias table, where each entry addressed a specific feature of the study:
Adequate sequence generation
Allocation concealment
Blinding
Incomplete outcome data addressed
Free of selective reporting
Free of other bias.
The judgement for each entry involved answering a question, with answers 'Yes' indicating low risk of bias, 'No' indicating high risk of bias, and 'Unclear' indicating either lack of information or uncertainty over the potential for bias. An assessment of the overall risk of bias was summarized involving the consideration of the relative importance of different domains.
It is reminded that the above tool was not developed with non‐randomised studies (NRS) in mind, and the six domains are not necessarily appropriate for NRS. However, the general structure of the tool and the assessments were useful to follow when creating risk of bias assessments for NRS. For non‐randomised interventional studies, the methods that The Cochrane Collaboration recommends for randomised trials were applied. For cohort and case‐control studies, the Newcastle‐Ottawa Scale was used (Wells 2008).
We developed our own criteria for the assessment of risk of bias of the cross‐sectional surveys with retrospective assessment of exposure:
Sampling procedure
Diagnosis of fluorosis
Ascertainment of exposure
Non‐response rate (considered response rate >65% as adequate).
Assessment of quality of outcome measures was based on the training, calibration and experience of examiners.
Due to the diversity of study designs, a team of at least three experienced review authors discussed the methods of the individual included studies in detail until consensus was reached regarding the risk of bias.
Where uncertainty could not be resolved, efforts were made to contact authors directly for clarification.
Data analyses
Main outcome
The chosen measure of treatment effect was risk ratio for controlled studies or prospective studies, while for the case‐control studies or cross‐sectional surveys, odds ratio was chosen as the measure of treatment effect. Where both adjusted and unadjusted risk ratios or odds ratios were presented for case‐control and cross‐over studies the adjusted value was included in the meta‐analysis.
Since the data from non‐randomised studies are more prone to bias and are often heterogeneous (Loke 2007), separate meta‐analyses were carried out and results presented according to different study designs.
The Cochrane Review Manager software (RevMan) was used for estimation of overall treatment effects/meta‐analysis of results whenever possible. Random‐effects (RE) models were used to calculate a weighted average of the treatment effects across the studies under review, after adjusting for the effects of the confounding factors such as exposure to systemic fluoride. If there were fewer than four studies, fixed‐effect (FE) analysis was used, as the estimate of between‐study variance is poor for analyses with low numbers of studies.
Investigation of heterogeneity
Heterogeneity in the results of the studies was assessed by inspection of a graphical display of results and by formal tests of homogeneity using I2; the significance of any heterogeneity was reported. Potential sources of heterogeneity were to be investigated where appropriate, and 'post hoc' analyses reported as such, with findings treated with caution.
Results
Description of studies
Results of the search
There were 3573 de‐duplicated papers identified from the electronic databases (from the date of inception until March 2009) using the search strategy. All records were screened on the basis of title, keywords and abstracts, 3497 papers that were obviously irrelevant were discarded. Then 76 papers were considered potentially eligible and full text reports were retrieved for further assessment. From these, 14 review articles/guidelines were identified and references were examined for additional relevant studies (Alvarez 2009; Clark 1993; Cunha 2006; Gillcrist 1996; Holloway 1997; Ismail 2008; Manji 1986; Mascarenhas 2000; Ripa 1991; Steiner 2004; Stookey 1994; Tobin 1988; Warren 1999; Whelton 2004). Thirteen studies were identified, however, all these had been included in the original search, thus no additional studies were included.
Excluded studies
From the remaining 55 studies (62 papers ), 29 studies (29 papers) were excluded (seeCharacteristics of excluded studies for the description of reasons of exclusion for each study). Five studies were conference proceedings/abstracts which did not provide sufficient information. Eleven studies had no or unclear investigation of topical fluoride exposure before the age of 6 years. Five studies investigated the combined exposures of systemic and/or topical fluoride. Four studies used the DDE index or evaluation of enamel defects as the outcome measure. One study had no clinical assessment of fluorosis. Two studies reported were unobtainable. One study's database no longer existed, thus data from 5 years old could not be extracted.
One study (Larsen 1987) is still pending for eligibility for this review awaiting translation.
Included studies
A total of 25 studies (32 papers) were included in this review with one non‐English report (seeCharacteristics of included studies for details of each study). All the reports were published between 1988 and 2006. There were two randomised controlled trials (RCTs) (Holt 1994; Tavener 2006), one cohort study (Franzman 2006), six case‐control studies (Osuji 1988; Pendrys 1989; Pendrys 1994; Pendrys 1996; Pendrys 1998; Skotowski 1995), and 16 cross‐sectional surveys (Beltran‐Valladares 2005; Bottenberg 2004; Brothwell 1999; Conway 2005; Do 2007; Mascarenhas 1998; Maupome 2003; Morgan 1998; Pereira 2000; Riordan 1993; Riordan 2002; Rock 1997; Sagheri 2007; Szpunar 1988; Tabari 2000; Wang 1997). Of these, 12 had data available to be extracted for analyses; 13 studies had only limited data available that were not in a useable form or missing data. Results of these 13 studies are summarized in Additional Table 1.
1. Summary of included studies with limited or missing data and not included in 'Data and analyses'.
| Study | Summary of data | Note |
| Brothwell 1999 | Age parent brushed with fluoridated paste (<1 year = 0, 1‐3 years = 1, >3 years = 2), OR = 0.93 (95% CI 0.40 to 2.19). | Categorization of the age started using fluoride toothpaste not compatible with Comparison 2, so data were not used in the meta‐analysis. |
| Franzman 2006 | Permanent incisor fluorosis was significantly associated with fluoride ingestion from dentifrice at age 24 months (OR = 1.30, 95% CI 1.02 to 1.65, P = 0.04), while results did not reach significance (P = 0.07) for AUD (area‐under‐the‐curve) 16‐ to 36‐month fluoride ingestion from dentifrice. | Fluorosis Risk Index was used. |
| Maupome 2003 | Early age when starting brushing teeth with toothpaste and more intensive regimens of fluoride supplement use were also associated with higher TFI mean scores. | Severity of fluorosis using TFI score was analysed using Poisson regression. |
| Morgan 1998 | The fluoride history variables, in aggregate, were not significantly associated with clinical assessments of fluorosis. | No estimates of ORs or count data were reported. |
| Pendrys 1989 | Mantel‐Haenszel OR estimates, adjusted for fluoride supplement, showed no statistically significant association between the use of fluoride dentifrice throughout the third through sixth years of life and fluorosis on any enamel surface (OR = 2.9, 99% CI 0.5 to 15.8). | Fluorosis Risk Index was used. |
| Pendrys 1994 | Frequent brushing with fluoride toothpaste throughout the first 8 years conveyed an increase in the risk of fluorosis on FRI classification I (OR = 2.80, 95% CI 1.15 to 6.81) and classification II (OR = 2.63, 95% CI 1.03 to 6.73) enamel surfaces as compared with non‐frequent brushing. The reported usual use of more than a pea size amount of toothpaste during brushing was not found to be statistically significant (classification I: OR = 3.07, 95% CI 0.76 to 12.36; classification II: OR = 1.75, 95% CI 0.35 to 8.89). | Fluorosis Risk Index was used. |
| Pendrys 1996 | A history of beginning to brush during the first 2 years while usually brushing more than once per day with fluoride toothpaste conveyed statistically significant adjusted ORs of 2.56 (95% CI 1.34 to 4.88) and 4.23 (95% CI 1.72 to 10.41) for mild‐to‐moderate fluorosis on FRI classification I and II enamel surfaces, respectively, as compared with subjects who did not begin to brush until after the second year and who usually brushed only once per day. | Fluorosis Risk Index was used. |
| Pendrys 1998 | A history of usually brushing with more than a pea size amount of toothpaste with a frequency of more than once per day conveyed statistically significant adjusted ORs of 6.35 (95% CI 1.21 to 33.40) and 8.37 (95% CI 1.68 to 41.72) for mild‐to‐moderate fluorosis on FRI classification I and II enamel surfaces, respectively, as compared with subjects who usually used a pea size amount of toothpaste and brushed only once per day. | Fluorosis Risk Index was used. |
| Pereira 2002 | Children who started using fluoride toothpaste before the age of 3 were 4.43 times more likely to have dental fluorosis than those who started using it after the age of 3. | TF>1 was used as criterion for defining fluorosis instead of TF>0 used in the review. |
| Riordan 1993 | ‐‐‐ | No data reported regarding the association between prevalence of fluorosis and the age of commencement of toothpaste use. |
| Riordan 2002 | No relationship was found between the presence of fluorosis and the age of commencement of toothpaste use. | No estimates of ORs or count data were reported. |
| Rock 1997 | A higher proportion of parents of children in the fluorosis group reported using high fluoride (1500 ppm) toothpaste (Chi2 12.052, P < 0.001). | No reported data regarding the association of prevalence of fluorosis and the age of commencement of toothbrushing or toothpaste use. |
| Szpunar 1988 | Variables that were not statistically significant related to the prevalence of fluorosis included the age at which a child began to brush, the age at which a parent began to brush the child's teeth, and the age at start of fluoride rinsing. | No estimates of ORs or count data were reported. |
CI = confidence interval; FRI = Fluorosis Risk Index; OR = odds ratio; TFI = Thylstrup and Fejerskov Index.
Of the 25 included studies, nine (36%) were conducted in Europe (UK, Belgium, Norway, Sweden); eight (32%) in the USA; three (12%) in Canada; two (8%) in Australia; one in Brazil (4%); one in Mexico (4%) and one in India (4%). Twelve studies (48%) were conducted in non‐fluoridated areas (Bottenberg 2004; Brothwell 1999; Conway 2005; Franzman 2006; Holt 1994; Mascarenhas 1998; Pendrys 1989; Pendrys 1996; Pereira 2000; Skotowski 1995; Tavener 2006; Wang 1997); eight (32%) in fluoridated areas (Beltran‐Valladares 2005; Maupome 2003; Morgan 1998; Osuji 1988; Pendrys 1994; Pendrys 1998; Riordan 1993; Rock 1997) and five in both non‐fluoridated and fluoridated areas (20%) (Do 2007; Riordan 2002; Sagheri 2007; Szpunar 1988; Tabari 2000).
The age range of the children at the time of the assessment of fluorosis was 6 to 17 years.
Characteristics of interventions/exposure
From the two RCTs, toothpastes at different fluoride levels were compared. In one trial (440 ppm versus 1450 ppm fluoride toothpaste), children entered the trial when they were approximately 12 months old until they were 5 to 6 years old (Holt 1994). They were then followed up for the assessment of fluorosis in school when they were 8 to 10 years old. Children in the other trial (550 ppm versus 1000 ppm fluoride toothpaste) entered the trial at the age of 2 years until they were 5 years old (Tavener 2006). They were followed up for the fluorosis assessment when they were 9 years old.
For the cohort study, a birth cohort from eight hospitals was followed up, with fluorosis examined at 7 to 11 years of age. Data on toothbrushing patterns and used of fluoride toothpaste were collected through questionnaires sent to mothers at 6 weeks, 3 months and then at 3 to 6 monthly intervals(Franzman 2006).
For the case‐control studies and cross‐sectional surveys, topical fluoride (TF) exposures of the children before the age of 6 years were mostly investigated using parental retrospective self‐administrated questionnaires. Variables concerning these exposures included: age started toothbrushing, age started using fluoride toothpaste, frequency of toothbrushing, amount of fluoride toothpaste used, and fluoride level of toothpaste used.
Data from all the included studies, with data available for analysis, were categorised into the following comparisons according to the TF exposures:
Comparison 1: Age started using fluoride toothpaste/toothbrushing: case‐control study (Osuji 1988; Skotowski 1995)
Comparison 2: Age started using fluoride toothpaste/toothbrushing: cross‐sectional survey (Beltran‐Valladares 2005; Bottenberg 2004; Brothwell 1999; Conway 2005; Do 2007; Mascarenhas 1998; Sagheri 2007; Tabari 2000; Wang 1997)
Comparison 3: Frequency of toothbrushing: cross‐sectional survey (Beltran‐Valladares 2005; Conway 2005; Do 2007; Tabari 2000)
Comparison 4: Amount of fluoride toothpaste used: cross‐sectional survey (Conway 2005; Do 2007; Tabari 2000)
Comparison 5: Fluoride level of toothpaste used: RCT (Holt 1994; Tavener 2006)
Comparison 6: Fluoride level of toothpaste used: cross‐sectional survey (Conway 2005; Do 2007; Tabari 2000).
Characteristics of outcome measures
In measuring the percentage prevalence of fluorosis, 14 studies used the Thylstrup and Fejerskov Index (TFI) score (Bottenberg 2004;Conway 2005; Do 2007; Holt 1994; Mascarenhas 1998; Maupome 2003; Osuji 1988; Pereira 2000; Riordan 1993; Riordan 2002; Rock 1997; Tabari 2000; Tavener 2006; Wang 1997), five studies used the Fluorosis Risk Index (FRI) (Franzman 2006; Pendrys 1989; Pendrys 1994; Pendrys 1996; Pendrys 1998), three studies used the Tooth Surface Index of Fluorosis (TSIF) score (Brothwell 1999; Skotowski 1995; Szpunar 1988) and three studies used Dean's Index (Beltran‐Valladares 2005; Morgan 1998; Sagheri 2007). The percentage prevalence of fluorosis ranged from 10% to 72% (see Additional Table 2 for the reported prevalence of each study).
2. Percentage prevalence of fluorosis.
| Study | Index used | Prevalence | Remark |
| RCT | |||
| Holt 1994 | TFI. | 18% | |
| Tavener 2006 | TFI. | 22% | |
| Cohort study | |||
| Franzman 2006 | Fluorosis Risk Index. | 27% | Fluorosis on 2 or more permanent incisors. |
| Case‐control study | |||
| Osuji 1988 | TFI. | 13% | |
| Skotowski 1995 | TSIF. | 72% | |
| Pendrys 1989 | Fluorosis Risk Index. | ‐‐‐ | Not reported. |
| Pendrys 1994 | Fluorosis Risk Index. | ‐‐‐ | Not reported. |
| Pendrys 1996 | Fluorosis Risk Index. | ‐‐‐ | Not reported. |
| Pendrys 1998 | Fluorosis Risk Index. | ‐‐‐ | Not reported. |
| Cross‐sectional survey | |||
| Beltran‐Valadares 2005 | Dean's Index. | 56% | |
| Bottenberg 2004 | TFI. | 10% | |
| Brothwell 1999 | TSIF. | 23% | |
| Conway 2005 | TFI. | 49% | |
| Do 2007 | TFI. | 27% | |
| Maupome 2003 | TFI. | 33% | |
| Mascarenhas 1998 | TFI. | 13% | |
| Morgan 1998 | Dean's Index. | 69% | |
| Pereira 2000 | TFI. | 10% | |
| Riordan 1993 | TFI. | 48% | |
| Riordan 2002 | TFI. | 18% | |
| Rock 1997 | TFI. | 35% | |
| Sagheri 2007 | Dean's Index. | 26% | Dublin (fluoridated area). |
| Sagheri 2007 | Dean's Index. | 18% | Freiburg (non‐fluoridated area). |
| Szpunar 1988 | TSIF. | 36% | |
| Tabari 2000 | TFI. | 54% | Newcastle (fluoridated area). |
| Tabari 2000 | TFI. | 23% | Northumberland (non‐fluoridated area). |
| Wang 1997 | TFI. | 36% | |
TFI = Thylstrup and Fejerskov Index; TSIF = Tooth Surface Index of Fluorosis.
Risk of bias in included studies
Risk of bias is reported separately for randomised controlled trials (RCTs), cohort study, case‐control studies and cross‐sectional surveys and presented in Additional Tables 3 to 6. Greater weighting is given to intervention studies over observational studies (and prospective, controlled observational studies over retrospective studies) in the interpretation of the findings.
For the two RCTs, one trial had adequate sequence generation (Tavener 2006) and the other was not clear (Holt 1994). Both trials had provided information on allocation concealment, had addressed the issue of incomplete outcome data and were free of selective reporting. One trial had been able to blind the outcome assessor but not the participants (Tavener 2006) while the other had been able to blind the participants and was not clear regarding the blinding of the outcome assessor (Holt 1994). One RCT was considered at low risk of bias (Tavener 2006). The results of the assessment of risk of bias for the RCTs is presented in Table 3.
3. Assessment of risk of bias: RCT.
| Holt 1994 | ||
| Adequate sequence generation? | Unclear | Quoted "randomly allocated..." but no detailed description. |
| Allocation concealment? | Yes | Quoted "toothpaste was supplied ... and the group code". |
| Incomplete outcome data addressed? | Yes | Comment: 490 out of 568 children in group 1 and 469 out of 531 chlidren in group 2 were analysed for fluorosis. Films with insufficient quality or no erupted maxillary permanent incisors were excluded. Missing data accounted for. |
| Free of selective reporting? | Yes | |
| Blinding of participants? | Yes | Quoted "double blinded clinical trial". |
| Blinding of outcome assessors? | Unclear | Quoted "double blinded clinical trial". |
| Tavener 2006 | ||
| Adequate sequence generation? | Yes | Comment: Undertaken by statistician using computer generated scheme. |
| Allocation concealment? | Yes | Comment: Allocation done at birth. |
| Incomplete outcome data addressed? | Yes | Comment: 726 children living in 3 less deprived districts attended schools with 4 or more children and 592 children living in 4 deprived districts attended schools with 6 or more children were followed up for examination of fluorosis. Missing data accounted for. |
| Free of selective reporting? | Yes | |
| Blinding of participants? | No | Comment: No masking of toothpaste tube. |
| Blinding of outcome assessors? | Yes | Comment: All assessors masked to toothpaste type. |
Given the inherent biases associated with observational studies, none were judged to be at low risk of bias. The assessment of each included study, grouped by design, is presented in Table 4; Table 5 and Table 6. Only one study met all the assessment criteria for its study design (case‐control) (Osuji 1988).
4. Assessment of risk of bias: cohort study.
| Franzman 2006 | ||
| Adequate sampling procedure? | Unclear | Unclear how representative the 8 hospitals were. Unclear if there is bias in who returned questionnaires at 16, 24 and 36 months n = 343. |
| Ascertainment of exposure? | Yes | Comment: Current parental questionnaires at regular intervals. |
| Adequate diagnosis of fluorosis? | Yes | Fluorosis Risk Index criteria. |
| Incomplete outcome data addressed? | Unclear | Insufficient information. |
| Free of selective reporting? | Yes | Probably. |
| Blinding of outcome assessors? | Yes | |
5. Assessment of risk of bias: case‐control study.
| Osuji 1998 | ||
| Is the case definition adequate? | Yes | Comment: TFI > 0 and intra‐examiner reliability assessed. |
| Representativeness of the cases? | Yes | Comment: Invited all schools >100 children. |
| Selection of controls? | Yes | Comment: Examined all children from the same classes with age and sex matched. |
| Definition of controls? | Yes | Comment: TF score = 0. |
| Comparability of cases and controls? | Yes | Comment: Children in the same classes and age and sex matched. |
| Ascertainment of exposure? | Yes | Comment: Interviewer not blinded, however time gap between screening and interview. No blinding for the parents, not possible to blind the parents. |
| Same method of ascertainment of cases and controls? | Yes | |
| Adequate response rate? | Yes | Comment: 82% for cases and 84% for controls. |
| Pendrys 1989 | ||
| Is the case definition adequate? | Yes | Comment: Fluorosis positive score on 2 or more enamel surface zones assigned to 1 of the 2 classifications (according to age of formation) in the Fluorosis Risk Index. |
| Representativeness of the cases? | Unclear | Comment: 1242 fluorosis examinations undertaken of 11 to 14 year olds. Unclear if all schools in area included. 850 cases and controls of the 1242 'selected'. |
| Selection of controls? | Yes | Comment: Children from same population, sex and age matched to within 6 months. |
| Definition of controls? | Yes | Comment: No fluorosis positive or questionable scores on any of the surface zones assigned to each classification in the Fluorosis Risk Index. |
| Comparability of cases and controls? | Yes | Comment: Children age and sex matched. |
| Ascertainment of exposure? | Unclear | Comment: Parental retrospective questionnaires. Reliability assessment undertaken using repeat questionnaire in 14% of sample (randomly drawn). |
| Same method of ascertainment of cases and controls? | Yes | |
| Adequate response rate? | Yes | Comment: 680/850 (80%) questionnaires returned. Response rate similar for cases and controls. |
| Pendrys 1994 | ||
| Is the case definition adequate? | Yes | Comment: Fluorosis positive score on 2 or more enamel surface zones assigned to 1 of the 2 classifications (according to age of formation) in the Fluorosis Risk Index. |
| Representativeness of the cases? | Yes | Comment: All eligible children enrolled in participating school districts. |
| Selection of controls? | Yes | Comment: Children from same population. |
| Definition of controls? | Yes | Comment: No fluorosis positive or questionable scores on any of the surface zones assigned to each classification in the Fluorosis Risk Index. |
| Comparability of cases and controls? | Unclear | Comment: Insufficient information. |
| Ascertainment of exposure? | Unclear | Comment: Parental retrospective questionnaires. Reliability assessment undertaken using repeat questionnaire in randomly drawn sample. |
| Same method of ascertainment of cases and controls? | Yes | |
| Adequate response rate? | Unclear | Comment: 568/637 (89%) questionnaires returned. However, only 401 (63%) used in analysis due to mixed/non‐fluoridated residency or excluded informant. |
| Pendrys 1996 | ||
| Is the case definition adequate? | Yes | Comment: Fluorosis positive score on 2 or more enamel surface zones assigned to 1 of the 2 classifications (according to age of formation) in the Fluorosis Risk Index. |
| Representativeness of the cases? | Yes | Comment: All eligible children enrolled in participating school districts. |
| Selection of controls? | Yes | Comment: Children from same population. |
| Definition of controls? | Yes | Comment: No fluorosis positive or questionable scores on any of the surface zones assigned to each classification in the Fluorosis Risk Index. |
| Comparability of cases and controls? | Unclear | Comment: Insufficient information. |
| Ascertainment of exposure? | Unclear | Comment: Parental retrospective questionnaires. Reliability assessment undertaken using repeat questionnaire in randomly drawn sample. |
| Same method of ascertainment of cases and controls? | Yes | |
| Adequate response rate? | Unclear | Comment: 754/767 (98%) questionnaires returned. However, only 460 (60%) used in analysis due to mixed/non‐fluoridated residency, excluded informant, or born before 1980. |
| Pendrys 1998 | ||
| Is the case definition adequate? | Yes | Comment: Fluorosis positive score on 2 or more enamel surface zones assigned to 1 of the 2 classifications (according to age of formation) in the Fluorosis Risk Index. |
| Representativeness of the cases? | Yes | Comment: All eligible children enrolled in participating school districts. |
| Selection of controls? | Yes | Comment: Children from same population. |
| Definition of controls? | Yes | Comment: No fluorosis positive or questionable scores on any of the surface zones assigned to each classification in the Fluorosis Risk Index. |
| Comparability of cases and controls? | Unclear | Insufficient information. |
| Ascertainment of exposure? | Unclear | Comment: Parental retrospective questionnaires. Reliability assessment undertaken using repeat questionnaire in randomly drawn sample. |
| Same method of ascertainment of cases and controls? | Yes | |
| Adequate response rate? | Unclear | Comment: 326/357 (91%) questionnaires returned. However, only 233 (65%) used in analysis due to mixed/non‐fluoridated residency, excluded informant, or born before 1980. |
| Skotowski 1995 | ||
| Is the case definition adequate? | Unclear | Comment: TSIF, but no intra‐ or inter‐examiner reliability assessed. |
| Representativeness of the cases? | No | Comment: Convenience sample. |
| Selection of controls? | Yes | Comment: Same group of children, age and sex matched. |
| Definition of controls? | Yes | Comment: Same index used. |
| Comparability of cases and controls? | Yes | Comment: Children age and sex matched. |
| Ascertainment of exposure? | Yes | Comment: No blinding for the parents, not possible to blind the parents. Unclear if the analysis of questionnaire was blinded to fluorosis exposure. |
| Same method of ascertainment of cases and controls? | Yes | |
| Adequate response rate? | Yes | Comment: 100% for cases and controls. |
TFI = Thylstrup and Fejerskov Index; TSIF = Tooth Surface Index of Fluorosis.
6. Assessment of risk of bias: cross‐sectional survey.
| Beltran‐Valladares 2005 | ||
| Adequate sampling procedure? | Unclear | Comment: Children from 3 public schools. Unclear of representativeness of the schools in the area. |
| Adequate diagnosis of fluorosis? | Yes | Comment: Modified Dean's Index. |
| Ascertainment of exposure? | Unclear | Comment: Self‐administered parental retrospective questionnaires. |
| Adequate response rate? | Yes | Comment: 100%. |
| Bottenberg 2004 | ||
| Adequate sampling procedure? | Yes | Comment: Random samples from representative cohorts were selected. |
| Adequate diagnosis of fluorosis? | Yes | Comment: TFI with inter‐examiner reliability. |
| Ascertainment of exposure? | Unclear | Comment: Parental retrospective questionnaires distributed through schools. |
| Adequate response rate? | Unclear | Comment: Unknown number of subjects used in the analysis. |
| Brothwell 1999 | ||
| Adequate sampling procedure? | Yes | Comment: All children from mandatory health programme. |
| Adequate diagnosis of fluorosis? | Yes | Comment: TSIF with intra‐examiner reliability. |
| Ascertainment of exposure? | Unclear | Comment: Parental retrospective questionnaires distributed through schools. |
| Adequate response rate? | No | Comment: 55%. |
| Conway 2005 | ||
| Adequate sampling procedure? | Yes | Comment: Random selection of schools from all schools in the region. |
| Adequate diagnosis of fluorosis? | Yes | Comment: Modified TFI with intra‐examiner reliability. |
| Ascertainment of exposure? | Unclear | Comment: Self‐administered postal questionnaires. |
| Adequate response rate? | No | Comment: 53%. |
| Do 2007 | ||
| Adequate sampling procedure? | Yes | Comment: Random sample of South Australian children selected for Child Oral Health Study were invited to take part. |
| Adequate diagnosis of fluorosis? | Yes | Comment: TFI with intra‐examiner reliability. |
| Ascertainment of exposure? | Unclear | Comment: Self‐administered parental retrospective questionnaires. |
| Adequate response rate? | No | Comment: 52%. |
| Mascarenhas 1998 | ||
| Adequate sampling procedure? | No | Comment: Affluent schools selected. |
| Adequate diagnosis of fluorosis? | Yes | Comment: TFI with intra‐examiner reliability. |
| Ascertainment of exposure? | Unclear | Comment: Self‐administered parental retrospective questionnaires. |
| Adequate response rate? | Yes | Comment: 95%. |
| Maupome 2003 | ||
| Adequate sampling procedure? | Yes | Comment: Children participated in the British Columbia Fluoridation Cessation Study. |
| Adequate diagnosis of fluorosis? | Yes | Comment: TFI with intra‐ and inter‐examiner reliability. |
| Ascertainment of exposure? | Unclear | Comment: Self‐administered parental retrospective questionnaires. |
| Adequate response rate? | Unclear | Comment: Not reported. |
| Morgan 1998 | ||
| Adequate sampling procedure? | No | Comment: Single dental practice. |
| Adequate diagnosis of fluorosis? | Yes | Comment: Modified Dean's Index with intra‐examiner reliability. |
| Ascertainment of exposure? | Unclear | Comment: Self‐administered parental retrospective questionnaires. |
| Adequate response rate? | Yes | Comment: 81%. |
| Pereira 2000 | ||
| Adequate sampling procedure? | Yes | Comment: Children randomly selected from schools. |
| Adequate diagnosis of fluorosis? | Yes | Comment: TFI with intra‐examiner reliability. |
| Ascertainment of exposure? | Unclear | Comment: Self‐administered parental retrospective questionnaires. |
| Adequate response rate? | Unclear | Comment: Not reported. |
| Riordan 1993 | ||
| Adequate sampling procedure? | Unclear | Comment: Insufficient information. |
| Adequate diagnosis of fluorosis? | Yes | Comment: TFI with intra‐examiner reliability. |
| Ascertainment of exposure? | Unclear | Comment: Self‐administered parental retrospective questionnaires. |
| Adequate response rate? | Yes | Comment: 84%. |
| Riordan 2002 | ||
| Adequate sampling procedure? | Unclear | Comment: Insufficient information. |
| Adequate diagnosis of fluorosis? | Yes | Comment: TFI with intra‐examiner reliability. |
| Ascertainment of exposure? | Unclear | Comment: Self‐administered parental retrospective questionnaires. |
| Adequate response rate? | Yes | Comment: 87%. |
| Rock 1997 | ||
| Adequate sampling procedure? | No | Comment: Schools selected "based on local knowledge", no detailed description. |
| Adequate diagnosis of fluorosis? | Unclear | Comment: TFI, unknown intra‐examiner reliability. |
| Ascertainment of exposure? | Unclear | Comment: Self‐administered parental retrospective questionnaires. |
| Adequate response rate? | Yes | Comment: 99.7%. |
| Sagheri 2007 | ||
| Adequate sampling procedure? | Yes | Comment: Representative random sample of 12 years old children. |
| Adequate diagnosis of fluorosis? | Yes | Comment: Dean's Index and intra‐examiner reliability. |
| Ascertainment of exposure? | Unclear | Comment: Self‐administered parental retrospective questionnaires. |
| Adequate response rate? | Yes | Comment: 81% (fluoridated) and 85% (non‐fluoridated). |
| Szpunar 1998 | ||
| Adequate sampling procedure? | Unclear | Comment: Insufficient information. |
| Adequate diagnosis of fluorosis? | Yes | Comment: TSIF and intra‐examiner reliability. |
| Ascertainment of exposure? | Unclear | Comment: Self‐administered parental retrospective questionnaires. |
| Adequate response rate? | Unclear | Comment: Not reported. |
| Tabari 2000 | ||
| Adequate sampling procedure? | Unclear | Comment: Insufficient information. |
| Adequate diagnosis of fluorosis? | Yes | Comment: TFI and intra‐examiner reliability. |
| Ascertainment of exposure? | Unclear | Comment: Self‐administered parental retrospective questionnaires. |
| Adequate response rate? | Yes | Comment: 78% (fluoridated) and 79% (non‐fluoridated). |
| Wang 1997 | ||
| Adequate sampling procedure? | Yes | Comment: Inclusive of all school districts excluding those with potential water fluoridation. |
| Adequate diagnosis of fluorosis? | Yes | Comment: TFI and intra‐examiner reliability. |
| Ascertainment of exposure? | Unclear | Comment: Self‐administered parental retrospective questionnaires. |
| Adequate response rate? | Yes | Comment: 70%. |
TFI = Thylstrup and Fejerskov Index; TSIF = Tooth Surface Index of Fluorosis.
Effects of interventions
Data extracted from the study reports are given in Additional Table 7 which includes both adjusted and unadjusted values if both were presented. The data presented in the forest plots and meta‐analyses are adjusted risk ratios (RRs) and odds ratios (ORs), when both were presented in the same paper.
7. Data extracted from the study reports.
| Study | Unadjusted OR/RR (95% CI) | Adjusted OR/RR (95% CI) | |
| Comparison 1: Age started using fluoride toothpaste/toothbrushing: case‐control study | |||
| Osuji 1988 | >24 months versus <=24 months | 0.09 (0.04‐0.21) | 0.09 (0.04‐0.24) |
| Skotowski 1995 | >=24 months versus <24 months | 0.70 (0.3‐1.6) | |
| Comparison 2: Age started using fluoride toothpaste/toothbrushing: cross‐sectional survey | |||
| Brothwell 1999 | >=12 months versus <12 months | 0.60 (0.48‐0.76) | |
| Conway 2005 | >12 months versus <=12 months | 0.93 (0.61‐1.39) | 0.95 (0.61‐1.49) |
| Tabari 2000 | >=12 months versus >12 months (Northumberland) | 0.82 (0.51‐1.31) | |
| Tabari 2000 | >=12 months versus <12 months (Newcastle) | 0.76 (0.52‐1.12) | |
| Wang 1997 | >14 months versus <=14 months | 0.41 (0.18‐0.93) | |
| Beltran‐Valladares 2005 | >24 months versus <24 months | 0.73 (0.43‐1.24) | 1.09 (0.58‐2.05) |
| Bottenberg 2004 | >24 months versus <24 months | 1.20 (0.89‐1.64) | |
| Do 2007 | >24 months versus <=24 months | 0.69 (0.49‐0.98) | |
| Mascarenhas 1998 | >=24 months versus <24 months | 0.73 (0.71‐1.18) | |
| Sagheri 2007 | >24 months versus <=24 months (Freilburg) | 0.64 (0.30‐1.39) | |
| Sagheri 2007 | >24 months versus <=24 months (Dublin) | 1.29 (0.78‐2.11) | |
| Comparison 3: Frequency of toothbrushing: cross‐sectional survey | |||
| Conway 2005 | <=2x per day versus >2x per day | 0.88 (0.53‐1.45) | 0.96 (0.55‐1.67) |
| Do 2007 | <2x per day versus >=2x per day | 0.81 (0.56‐1.18) | |
| Tabari 2000 | <2x per day versus >=2x per day (Northumberland) | 0.86 (0.55‐1.35) | |
| Tabari 2000 | <2x per day versus >=2x per day (Newcastle) | 0.91 (0.63‐1.33) | |
| Beltran‐Valladares 2005 | <7 times per week versus >=1x per day | 0.77 (0.42‐1.40) | |
| Comparison 4: Amount of fluoride toothpaste used: cross‐sectional survey | |||
| Conway 2005 | <=pea size versus >pea size | 1.25 (0.81‐1.92) | 1.30 (0.84‐2.02) |
| Do 2007 | Small versus medium or large | 0.63 (0.43‐0.91) | 0.56 (0.34‐0.93) |
| Tabari 2000 | <=pea size versus >pea size (Newcastle) | 1.04 (0.7‐1.53) | |
| Tabari 2000 | <=pea size versus >pea size (Northumberland) | 0.89 (0.56‐1.42) | |
| Tabari 2000 | <=0.25 g versus >0.25 g (Newcastle) | 0.91 (0.55‐1.49) | |
| Tabari 2000 | <=0.25 g versus >0.25 g (Northumberland) | 1.87 (1.05‐3.34) | |
| Comparison 5: Fluoride level of toothpaste used: RCT | |||
| Holt 1994 | 550 ppm versus 1000 ppm | 0.75 (0.57‐0.99) | |
| Tavener 2006 | 440 ppm versus 1450 ppm | 0.59 (0.44‐0.79) | |
| Comparison 6: Fluoride level of toothpaste used: cross‐sectional survey | |||
| Conway 2005 | 250/500 ppm versus >=1000 ppm | 0.99 (0.49‐1.99) | 0.84 (0.40‐1.75) |
| Do 2007 | 400‐550 ppm versus 1000 ppm | 0.89 (0.61‐1.31) | |
| Tabari 2000 | Children versus family fluoride toothpaste (Northumberland) | 0.94 (0.53‐1.67) | |
| Tabari 2000 | Children versus family fluoride toothpaste (Newcastle) | 0.54 (0.32‐0.9) | |
CI = confidence interval; OR = odds ratio; RR = risk ratio.
Comparison 1: Age started using fluoride toothpaste/toothbrushing: case‐control study
(Figure 1). Data from two case‐control studies were included in this meta‐analysis, with both providing data on whether the child brushed/had their teeth brushed with fluoride toothpaste before or after 24 months (Osuji 1988; Skotowski 1995). One study showed a statistically significant reduction in fluorosis in starting brushing after 24 months (Osuji 1988) and the meta‐analysis also found a significant reduction in fluorosis (OR 0.29, fixed‐effect (FE) 95% confidence interval (CI) 0.15 to 0.53). There was an indication of significant heterogeneity between the two studies (P = 0.002, I2 = 90%). It is not possible to investigate heterogeneity with only two studies, however, one study was conducted in a fluoridated (Osuji 1988) and the other in a non‐fluoridated (Skotowski 1995) area. One study (Osuji 1988) was assessed as at low risk of bias, with Skotowski 1995 assessed as moderate as the cases were not felt to be representative.
1.
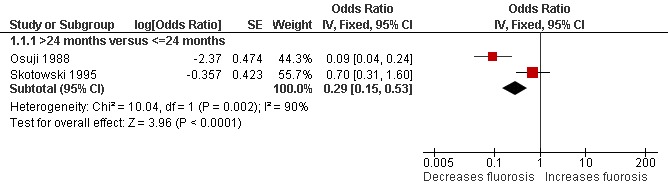
Forest plot of comparison: 1 Age started using fluoride toothpaste/toothbrushing: case‐control study, outcome: 1.1 Fluorosis.
Comparison 2: Age started using fluoride toothpaste/toothbrushing: cross‐sectional survey
(Figure 2). Nine cross‐sectional surveys were included in this meta‐analysis. Seven additional cross‐sectional surveys collected data on age at commencement of toothbrushing, however, no useful data were available for inclusion in the meta‐analysis (Table 1).
2.
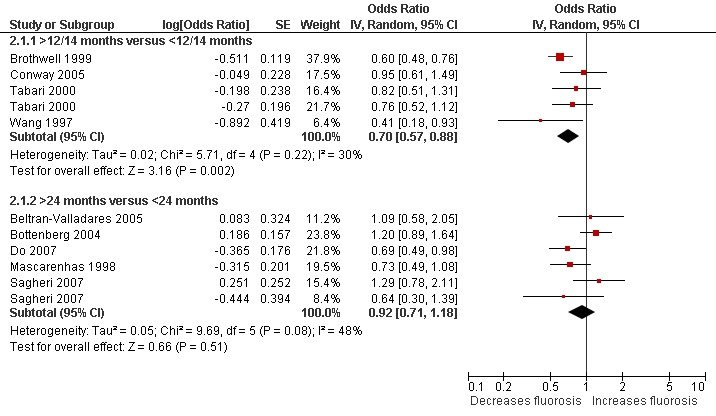
Forest plot of comparison: 2 Age started using fluoride toothpaste/toothbrushing: cross‐sectional survey, outcome: 2.1 Fluorosis.
Three studies provided data on brushing with fluoride toothpaste before or after 12 months (Brothwell 1999; Conway 2005; Tabari 2000) (with one study providing data in two areas); one study provided data on brushing with fluoride toothpaste before or after 14 months (Wang 1997); and five studies provided data on brushing before or after 24 months (Beltran‐Valladares 2005; Bottenberg 2004; Do 2007; Mascarenhas 1998; Sagheri 2007), with one study providing data in two areas (Sagheri 2007).
Brushing before 12/14 months
The data for the four studies brushing before 12 and 14 months were combined in the meta‐analysis and showed a significant reduction in risk of fluorosis if children brushed their teeth/had their teeth brushed after 12 to 14 months (OR 0.70, random‐effects (RE) 95% CI 0.57 to 0.88), with no evidence of heterogeneity (P = 0.22, I2 = 30%). None of the four studies were considered to be at low risk of bias and all were conducted in non‐fluoridated areas, other than one with both fluoridated and non‐fluoridated areas included in the study by Tabari 2000.
Brushing before 24 months
The meta‐analysis result for brushing before versus after 24 months was not significant (OR 0.92, RE 95% CI 0.71 to 1.18). None of the five studies were considered to be at low risk of bias, with one being conducted in a fluoridated area (Beltran‐Valladares 2005), two in non‐fluoridated areas (Bottenberg 2004; Mascarenhas 1998) and two in both fluoridated and non‐fluoridated areas (Do 2007; Sagheri 2007).
Comparison 3: Frequency of toothbrushing: cross‐sectional survey
(Figure 3). Four cross‐sectional studies provided data for the forest plots (Beltran‐Valladares 2005; Conway 2005; Do 2007; Tabari 2000). Four additional cross‐sectional surveys collected data on frequency of toothbrushing, however, no useful data were available for inclusion in the meta‐analysis (Table 1).
3.
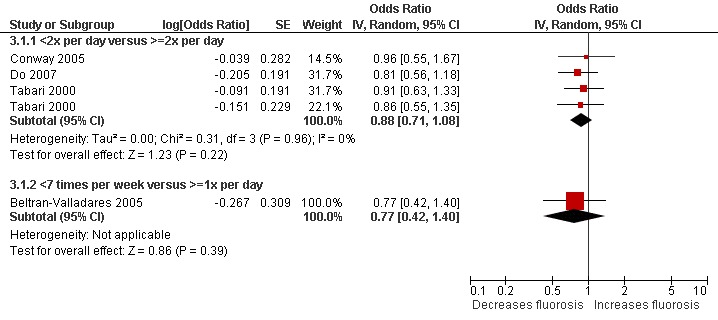
Forest plot of comparison: 3 Frequency of toothbrushing: cross‐sectional survey, outcome: 3.1 Fluorosis.
The frequency of toothbrushing was presented as less than or equal to 7 times per week versus 1 or more times per day in one study (Beltran‐Valladares 2005), and this study found no significant association between toothbrushing frequency and fluorosis. The other three cross‐sectional surveys (Conway 2005; Do 2007; Tabari 2000) presented data as brushing less than twice per day versus twice a day or more. The meta‐analysis also did not find a significant difference (OR 0.88, RE 95% CI 0.71 to 1.08). None of the studies were assessed as at low risk of bias. One study was conducted in a non‐fluoridated community (Conway 2005) and the other two in both fluoridated and non‐fluoridated communities (Do 2007; Tabari 2000).
Comparison 4: Amount of fluoride toothpaste used: cross‐sectional survey
(Figure 4). Three cross‐sectional studies presented data on the association between the amount of fluoride toothpaste and fluorosis for the forest plots (Conway 2005; Do 2007; Tabari 2000). Three additional cross‐sectional surveys collected data on amount of fluoride toothpaste, however, no useful data were available for inclusion in the meta‐analysis (Table 1).
4.
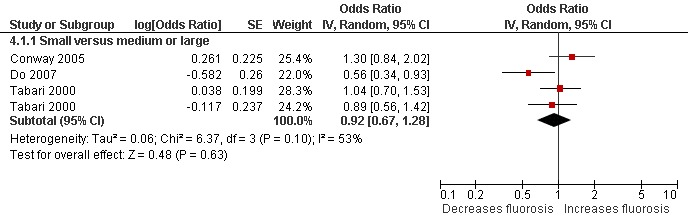
Forest plot of comparison: 4 Amount of fluoride toothpaste used: cross‐sectional survey, outcome: 4.1 Fluorosis.
Available data were presented as a small versus medium to large amount of fluoride toothpaste on the toothbrush (Do 2007) and pea size versus greater than pea size (Conway 2005; Tabari 2000). One study also presented <0.25 grams versus >0.25 grams (Tabari 2000; data shown in Table 7). The small amount and pea size estimates were combined in the meta‐analysis which found no significant effect (OR 0.92, RE 95% CI 0.67 to 1.28). None of the studies were assessed as at low risk of bias. One study was conducted in a non‐fluoridated community (Conway 2005), and the other two in both fluoridated and non‐fluoridated communities (Do 2007; Tabari 2000).
Comparison 5: Fluoride level of toothpaste used: RCT
(Figure 5). Two randomised controlled trials compared the effect of giving children different levels of fluoride toothpaste. One study compared 550 with 1000 ppm fluoride (Holt 1994) and the other compared 440 with 1450 ppm fluoride (Tavener 2006). Both studies found statistically significant differences (RR 0.75, 95% CI 0.57 to 0.99) and (RR 0.59, 95% CI 0.44 to 0.79), indicating a higher level of fluoride toothpaste was associated with an increased risk of fluorosis. One study was assessed as at low risk of bias (Tavener 2006) and both studies were in non‐fluoridated areas.
5.
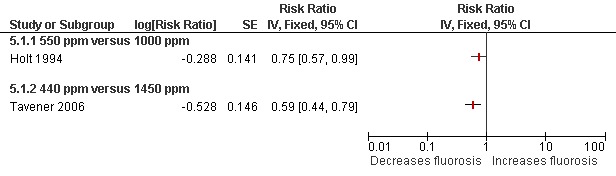
Forest plot of comparison: 5 Fluoride level of toothpaste used: RCT, outcome: 5.1 Fluorosis.
Comparison 6: Fluoride level of toothpaste used: cross‐sectional survey
(Figure 6). Three studies (one in two different areas) presented data for the meta‐analysis (Conway 2005; Do 2007; Tabari 2000). An additional cross‐sectional survey collected data on fluoride level, however, no useful data were available for inclusion in the meta‐analysis (Table 1).
6.
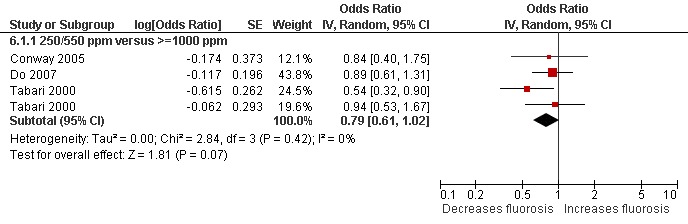
Forest plot of comparison: 6 Fluoride level of toothpaste used: cross‐sectional survey, outcome: 6.1 Fluorosis.
Among these three studies, two gave information about the levels of fluoride in the toothpastes being used by the children (250‐500 versus >1000 ppm fluoride; Conway 2005) and (400‐550 versus 1000 ppm fluoride; Do 2007). The other study classified this as 'children's' versus 'family' fluoride toothpaste (Tabari 2000). The meta‐analysis found no statistically significant difference. Neither of the studies were assessed as at low risk of bias. One study was conducted in a non‐fluoridated community (Conway 2005), the others in both fluoridated and non‐fluoridated communities (Do 2007; Tabari 2000).
Discussion
The objective of this review was to evaluate the available evidence in increasing the risk of developing dental fluorosis in children of different topical fluoride treatment modalities (including gels, toothpastes, varnishes and mouthrinses) used at different concentrations, and with varying duration of use/exposure. The Developmental Defects of Enamel (DDE) Index was not included as an outcome measure within the current review. The DDE Index is not fluorosis specific and, as such, it may not be appropriate to extract information on the prevalence and severity of fluorosis in studies on children using the DDE Index alone. Three papers which had used the DDE Index were excluded from this review. In two of these papers (Ellwood 1994; Evans 1991), the authors specifically referred to their observations as enamel opacities or diffuse enamel defects. In the other one (van der Hoek 2003), the authors mentioned that the prevalence of diffuse opacities was only an approximation to the prevalence of fluorosis. Studies using the Fluorosis Risk Index (FRI) were included, however, the way the results were presented made it difficult to extract the relevant data and pool them with those from other studies which used other indices of fluorosis measurement based on examination of all teeth and all surfaces. Thus results from these studies are reported in Additional Table 1.
The review used a binary approach to the presence/absence of fluorosis. The inclusion of a level of fluorosis that is of aesthetic concern is subject to debate as there is no consensus on this. This was included in the original protocol but removed following peer review. It is acknowledged that the available evidence in the review focuses on mild fluorosis.
Among the 25 included studies, many evaluated the age toothbrushing/use of fluoride toothpaste started, frequency of toothbrushing, amount of fluoride toothpaste used and fluoride level of toothpaste used before the age of 6 years. In two studies (Bottenberg 2004; Skotowski 1995), data on the above mentioned topical fluoride exposures were not included in the meta‐analysis because they referred to the exposure at the time of the investigation of fluorosis (i.e. older than 6 years). Also for Mascarenhas 1998, no clear categorization of the frequency of toothbrushing and amount of fluoride toothpaste used was reported, thus these data were also not included in the meta‐analysis. In the original protocol, it was intended to include different topical fluoride therapies in the form of toothpastes, mouthrinses, gels, foams, paint‐on solutions, and varnishes. However, after conducting the review, evidence generally focused on fluoride toothpaste. A few studies evaluated the use of mouthrinses (Brothwell 1999; Osuji 1988; Szpunar 1988) or professional application of fluoride (Brothwell 1999; Morgan 1998; Osuji 1988), however, these evaluations did not clearly specify the ages at which the children were exposed to the topical fluorides and were not included in the meta‐analysis. Thus, the meta‐analyses performed in this review mainly focused on the associations between age started using fluoride toothpaste/toothbrushing, frequency of toothbrushing, amount of fluoride toothpaste used, and of fluoride level of toothpaste used and fluorosis. If information on the use of other topical fluoride therapies in causing fluorosis is available in future publications, it will be included in the update of the review.
Regarding the age use of fluoride toothpaste/toothbrushing started, a significant reduction in the risk of fluorosis was found if children did not brush their teeth/have their teeth brushed with fluoride toothpaste until after the age of 12 months. However, inconsistent associations were found regarding children beginning to brush their teeth/have their teeth brushed with fluoride toothpaste after the age of 24 months and fluorosis. Data from the case‐control studies showed significant reductions when not starting until after 24 months but data from cross‐sectional surveys did not. It is noted that the results of the two case‐control studies were very different, one had a very small and significant odds ratio (OR) indicating significant reduction in the risk of fluorosis if toothbrushing started after 24 months (Osuji 1988) and the other study (Skotowski 1995) had an insignificant OR laying within the range of ORs from the cross‐sectional surveys. When pooling the data from these two studies, an overall significant result was obtained. One should be cautious in interpreting such results and more evidence with low risk of bias is needed to clarify the inconsistency in the association.
No significant association was found between frequency of toothbrushing and fluorosis. Also no significant association was found between the amount of fluoride toothpaste used and fluorosis. It should be noted that the measurements used in determining the amount of fluoride toothpaste used in the included studies were actually vague and subjective: small versus medium to large amount of fluoride toothpaste on the toothbrush, or pea size versus greater than pea size. The frequency of toothbrushing and the amount of fluoride toothpaste used were actually proxy measurements for the amount of fluoride toothpaste being ingested, as part of the ingested fluoride will be absorbed by the body and produce the systemic effects which lead to development of fluorosis in the developing permanent teeth during early childhood (Ekstrand 1996). However, to measure the amount of fluoride toothpaste being ingested has been a very difficult task. Among the included studies, a few studies (Do 2007; Mascarenhas 1998; Riordan 1993; Wang 1997) had collected information on whether the children liked, swallowed or ate fluoride toothpaste as another proxy measure for the amount of ingestion. All these additional measures are considered to be subjective, and thus data from these investigations were not included in the present review.
Regarding the fluoride level of the toothpaste used, results from the two randomised controlled trials (RCTs) found that using toothpaste with a higher level of fluoride was significantly associated with an increase in fluorosis. The study in which children were recruited at 12 months and the fluoride toothpaste intervention was given until the age of 5 to 6 years (Tavener 2006) demonstrated a higher risk of developing fluorosis compared to the other study in which children were recruited at age 2 years and the fluoride toothpaste intervention programme was given for a 3‐year period (Holt 1994). However, it is noted that the levels of fluoride used in the former study was 440 versus 1450 ppm while the latter study used 550 versus 1000 ppm. Whether the increase in the risk of fluorosis in the former study was due to the higher fluoride level of the toothpaste was confounded by the longer duration of exposure and the younger age at which use of fluoride toothpaste was started. In addition, results from the meta‐analysis in pooling the data from the cross‐sectional surveys did not support the association between the fluoride concentration of toothpaste used and fluorosis. However, it is noted that the pooled OR (0.79) was only marginally insignificant (random‐effects (RE): 95% confidence interval (CI) 0.61 to 1.02; P = 0.07). More evidence with low risk of bias is needed to clarify the inconsistency in the association.
It was originally intended to analyse the associations with respect to the different exposure of systemic fluoride using subgroup analysis, however, with very few studies being available for such comparison, subgroup analysis was not performed. Only information on the number of studies conducted in fluoridated, non‐fluoridated or both fluoridated and non‐fluoridated areas was reported in each comparison.
The available evidence shows an increased association of fluorosis and age started using fluoride toothpaste/toothbrushing before 12 months, and an inconsistent association between fluorosis and age started using fluoride toothpaste/toothbrushing before 24 months. From the RCTs, higher concentration of fluoride toothpaste was associated with an increase in fluorosis, even though such finding is not supported by the data from cross‐sectional surveys. No significant association between the frequency of toothbrushing or the amount of fluoride toothpaste used and fluorosis was found.
Authors' conclusions
Implications for practice.
There should be a balanced consideration between the benefits of topical fluorides in caries prevention and the risk of the development of fluorosis. Most of the available evidence focuses on mild fluorosis. There is weak unreliable evidence that starting the use of fluoride toothpaste in children under 12 months of age may be associated with an increased risk of fluorosis. The evidence for its use between the age of 12 and 24 months is equivocal. If the risk of fluorosis is of concern, the fluoride level of toothpaste for young children is recommended to be lower than 1000 ppm.
Implications for research.
More evidence with low risk of bias is needed. Future trials assessing the effectiveness of different types of topical fluorides (including toothpastes, gels, varnishes and mouthrinses) and/or different concentrations should ensure that they include an adequate follow‐up period in order to collect data on potential fluorosis. As it is unethical to propose randomised controlled trials to assess fluorosis itself, it is acknowledged that further observational studies will be undertaken in this area. However, attention needs to be given to the choice of study design, bearing in mind that prospective, controlled studies will be less susceptible to bias than retrospective and/or uncontrolled studies.
What's new
| Date | Event | Description |
|---|---|---|
| 12 May 2010 | Amended | Minor edit. |
Acknowledgements
Thanks go to Sylvia Bickley and Anne Littlewood (Trials Search Co‐ordinator, Cochrane Oral Health Group) for carrying out the searches for the review; Philip Riley (Assistant Managing Editor, Cochrane Oral Health Group) for his help with the administration of the review which included locating all the articles for the review. Thanks also to Luisa Fernandez Mauleffinch (Managing Editor, Cochrane Oral Health Group) for her help with the administration of the review. Our thanks also to those who assisted with translation of the foreign language manuscripts. We would also like to thank the referees for all their constructive comments.
Appendices
Appendix 1. Cochrane Oral Health Group Trials Register search strategy
((fluor* or “PPMF” or “PPM F” or “APF” or “NAF” or “sodium* F” or “amin* F” or “SNF2” or “stannous$ F” or “acidulat* F” or “phosphat* F” or fluorophosphat* or “SMFP” or “MFP” or monofluor*) AND (fluorosis or flurosis or fluorose* or fluorotic or "enamel opacit*" or "enamel hypomineral*" or "enamel hypoplasi*" or "enamel defect*" or "enamel porosit*" or "enamel* whit*" or mottle* or mottling))
Appendix 2. CENTRAL search strategy
#1 Explode FLUORIDES #2 (fluor* or “PPMF” or “PPM F” or “APF” or “NAF” or “sodium* F” or “amin* F” or “SNF2” or “stannous$ F” or “acidulat* F” or “phosphat* F” or fluorophosphat* or “SMFP” or “MFP” or monofluor*) [in title,abstract,or keywords] #3 #1 or #2 #4 FLUOROSIS,DENTAL #5 fluorosis or flurosis or fluorose* or fluorotic #6 ((enamel* NEAR/6 opacit*) or (enamel* NEAR/6 hypomineral*) or (enamel NEAR/6 hypoplasi*) or (enamel* NEAR/6 defect*) or (enamel* NEAR/6 porosit*) or (enamel* NEAR/6 white*)) #7 mottle* or mottling #8 #4 or #5 or #6 or #7 #9 #3 AND #8
Appendix 3. MEDLINE (via OVID) search strategy
1. exp Fluorides/ 2. Fluorides, Topical/ 3. (fluor* or "PPMF" or "PPM F" or "APF" or "NAF" or "sodium* F" or "amin* F" or "SNF2" or "stannous* F" or "acidulat* F" or "phosphat* F" or fluorophosphat* or "SMFP" or "MFP" or monofluor*).ab,ti. 4. 1 or 2 or 3 5. Fluorosis, Dental/ 6. (fluorosis or flurosis or fluorose* or fluorotic).mp. [mp=title, original title, abstract, name of substance word, subject heading word] 7. (enamel* adj6 (opacit* or hypomineral* or hypoplasi* or defect* or porosit* or white*)).ab,ti. 8. (mottle or mottling).mp. [mp=title, original title, abstract, name of substance word, subject heading word] 9. 5 or 6 or 7 or 8 10. 4 and 9
Appendix 4. EMBASE (via OVID) search strategy
1. Fluoride/ 2. "Topical fluoride*".mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] 3. (fluor* or "PPMF" or "PPM F" or "APF" or "NAF" or "sodium* F" or "amin* F" or "SNF2" or "stannous* F" or "acidulat* F" or "phosphat* F" or fluorophosphat* or "SMFP" or "MFP" or monofluor*).ab,ti. 4. 1 or 2 or 3 5. Fluorosis, Dental/ 6. (fluorosis or flurosis or fluorose* or fluorotic).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] 7. (enamel* adj6 (opacit* or hypomineral* or hypoplasi* or defect* or porosit* or white*)).ab,ti. 8. (mottle or mottling).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] 9. 5 or 6 or 7 or 8 10. 4 and 9
Appendix 5. BIOSIS (via Web of Knowledge) search strategy
1. TS=(fluorosis or flurosis or flurose* or fluorotic) 2. TS=("enamel* opacit*" or "enamel* hypomineral*" or "enamel* hypoplasi*" or "enamel* defect*" or "enamel* porosit*" or "enamel* whit*") 3. TS=(mottle or mottling) 4. #3 OR #2 OR #1 5. TI=(fluor* or "sodium* F" or "amin* F" or "stannous* F" or "acidulat* F" or "phosphat* F" or fluorophosphat* or monofluor*) 6. TI=(PPMF or "PPM F" or APF or NAF or SNF2 or SMFP or MFP) 7. #6 OR #5 8. #7 AND #4
Appendix 6. LILACS search strategy
(fluorosis or flurosis or flurose$ or fluorotic or “enamel$ opacity$” or “enamel$ hypomineral$” or “enamel$ hypoplasi$” or “enamel$ defect$” or “enamel$ porosit$” or “enamel$ white$”)
Appendix 7. Dissertation Abstracts (via ProQuest) search strategy
1. (fluor* or “sodium* F” or “amin* F” or “stannous* F” or “acidulat* F” or “phosphate F” or fluorophosphat or monofluor) in Citation and Abstract
OR
2. (PPMF or “PPM F” or APF or NAF or SNF2 or SMFP or MFP )
AND
3. (fluorosis or flurosis or flurose* or fluorotic or “enamel* opacit*” or “enamel* hypomineral*” or “enamel* hypoplasi*” or “enamel* defect*” or “enamel* porosit*” or “enamel* white*”)
Data and analyses
Comparison 1. Age started using fluoride toothpaste/toothbrushing: case‐control study.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Fluorosis | 2 | Odds Ratio (Fixed, 95% CI) | Subtotals only | |
| 1.1 >24 months versus <=24 months | 2 | Odds Ratio (Fixed, 95% CI) | 0.29 [0.15, 0.53] |
1.1. Analysis.
Comparison 1 Age started using fluoride toothpaste/toothbrushing: case‐control study, Outcome 1 Fluorosis.
Comparison 2. Age started using fluoride toothpaste/toothbrushing: cross‐sectional survey.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Fluorosis | 9 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 1.1 >12/14 months versus <12/14 months | 4 | Odds Ratio (Random, 95% CI) | 0.70 [0.57, 0.88] | |
| 1.2 >24 months versus <24 months | 5 | Odds Ratio (Random, 95% CI) | 0.92 [0.71, 1.18] |
2.1. Analysis.
Comparison 2 Age started using fluoride toothpaste/toothbrushing: cross‐sectional survey, Outcome 1 Fluorosis.
Comparison 3. Frequency of toothbrushing: cross‐sectional survey.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Fluorosis | 4 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 1.1 <2x per day versus >=2x per day | 3 | Odds Ratio (Random, 95% CI) | 0.88 [0.71, 1.08] | |
| 1.2 <7 times per week versus >=1x per day | 1 | Odds Ratio (Random, 95% CI) | 0.77 [0.42, 1.40] |
3.1. Analysis.
Comparison 3 Frequency of toothbrushing: cross‐sectional survey, Outcome 1 Fluorosis.
Comparison 4. Amount of fluoride toothpaste used: cross‐sectional survey.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Fluorosis | 3 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 1.1 Small versus medium or large | 3 | Odds Ratio (Random, 95% CI) | 0.92 [0.67, 1.28] |
4.1. Analysis.
Comparison 4 Amount of fluoride toothpaste used: cross‐sectional survey, Outcome 1 Fluorosis.
Comparison 5. Fluoride level of toothpaste used: RCT.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Fluorosis | 2 | Risk Ratio (Fixed, 95% CI) | Totals not selected | |
| 1.1 550 ppm versus 1000 ppm | 1 | Risk Ratio (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 440 ppm versus 1450 ppm | 1 | Risk Ratio (Fixed, 95% CI) | 0.0 [0.0, 0.0] |
5.1. Analysis.
Comparison 5 Fluoride level of toothpaste used: RCT, Outcome 1 Fluorosis.
Comparison 6. Fluoride level of toothpaste used: cross‐sectional survey.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Fluorosis | 3 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 1.1 250/550 ppm versus >=1000 ppm | 3 | Odds Ratio (Random, 95% CI) | 0.79 [0.61, 1.02] |
6.1. Analysis.
Comparison 6 Fluoride level of toothpaste used: cross‐sectional survey, Outcome 1 Fluorosis.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Beltran‐Valladares 2005.
| Methods | Cross‐sectional survey conducted in fluoridated area in Mexico. | |
| Participants | 320 school children aged 6‐9 years from 3 public schools. The children had participated in a preventive dental programme consisting of regular application of 2% topical fluoride gel and toothbrushing instructions during pre‐school years (duration/frequency not stated). | |
| Interventions | Exposure: toothbrushing frequency and other fluoride use (professionally applied fluoride, mouthrinse use, self‐administered fluoride gel) during the first 6 years. | |
| Outcomes | Modified Dean's Index. | |
| Notes | No inter/intra‐rater reliability reported. | |
Bottenberg 2004.
| Methods | Cross‐sectional survey conducted in non‐fluoridated areas in Belgium. | |
| Participants | 5071 7 years old children (at the start of the study) selected, 4128 examined for fluorosis at 11 years old and 3939 valid questionnaires returned out of 5071 distributed. | |
| Interventions | Exposure: frequency of toothbrushing, age of commencement of toothbrushing (<2 years), quantity of fluoride toothpaste, use of fluoride fluoride toothpaste. | |
| Outcomes | TFI. | |
| Notes | Inter‐examiner reliability (14 examiners with Kappa >0.60). Only unadjusted ORs were reported because of the high proportion of missing values over the different covariates, no multivariate analysis was performed. |
|
Brothwell 1999.
| Methods | Cross‐sectional survey conducted in non‐fluoridated areas in Canada. | |
| Participants | 1739 7‐8 years old children screened in 55 out of 95 local schools, 1367 had been given a TSIF score and questionnaires to parents were distributed through schools, 752 returned questionnaires (55% response rate) and available information for analysis. | |
| Interventions | Exposure: toothbrushing, professional topical fluoride treatment, fluoride mouthwash. | |
| Outcomes | TSIF. | |
| Notes | Inter‐examiner reliability during calibration exercise (weighted Kappa = 0.89); intra‐examiner reliability (weighted Kappa = 0.75). | |
Conway 2005.
| Methods | Cross‐sectional survey conducted in non‐fluoridated areas in Sweden. | |
| Participants | 1039 7‐9 years old children questionnaires distributed, 757 returned questionnaire with positive consent for the diagnosis of fluorosis, 620 screened for fluorosis and 548 with available information for analysis. | |
| Interventions | Exposure: toothbrushing practices, fluoride toothpaste usage behaviour during infancy. | |
| Outcomes | Modified TFI. | |
| Notes | Intra‐examiner reliability (Kappa = 0.92). | |
Do 2007.
| Methods | Cross‐sectional survey conducted in fluoridated and non‐fluoridated areas in South Australia. | |
| Participants | 1401 children took part in Child Oral Health Study survey, self‐administered parental questionnaires were distributed. 684 attended the examination and 677 8‐13 years old children with valid data for analysis. | |
| Interventions | Exposure: age of fluoridated toothpaste began, pattern of toothbrushing, type of fluoride toothpaste, amount of fluoride toothpaste, after brushing routine at the time when toothbrushing with fluoride toothpaste started. | |
| Outcomes | TFI. | |
| Notes | Intra‐examiner reliability (Kappa = 0.74‐0.79). | |
Franzman 2006.
| Methods | Cohort study conducted in a non‐fluoridated area in US. | |
| Participants | Birth cohort from 8 hospitals. Fluorosis examined at 7‐11 years. Questionnaires sent to mothers at 6 weeks, 3 months then at 3‐, 4‐ or 6‐month intervals. Analysis based on children with questionnaires returned at ages 16, 24 and 36 months n = 343. | |
| Interventions | Exposure: toothbrushing patterns and use of fluoride dentifrice. | |
| Outcomes | FRI. | |
| Notes | 2 trained examiners. Inter‐examiner reliability (Kappa = 0.53). | |
Holt 1994.
| Methods | RCT conducted in non‐fluoridated areas in UK. | |
| Participants | 1099 out of the potential 2177 children aged 9 years old (who participated in the trial at 2 years old for a period of 3 years) gave positive consent to the follow‐up study. | |
| Interventions | Group 1: Fluoride toothpaste (550 ppm) (n = 568).
Group 2: Fluoride toothpaste (1000 ppm) (n = 531). A sample of children who did not participate in the trial formed a third group and not included in this review. |
|
| Outcomes | TFI. DDE Index. Both assessed from photographic digital images. | |
| Notes | Intra‐ and inter‐examiner reliability for TFI (Kappa = 0.68 and 0.78 respectively). Data for the third group not used within this review. |
|
Mascarenhas 1998.
| Methods | Cross‐sectional survey conducted in non‐fluoridated cities in India. | |
| Participants | 1250 of 1276 7th grade children (12‐13 years) from 11 affluent schools were examined, questionnaires returned for 1189 children. | |
| Interventions | Exposure: history of fluoride toothpaste use, brushing habits before the age of 6 years and at the present time. | |
| Outcomes | TFI. | |
| Notes | Intra‐examiner reliability (Kappa = 0.75). | |
Maupome 2003.
| Methods | Cross‐sectional survey conducted in communities with recently de‐fluoridated and still fluoridated water supply in Canada. | |
| Participants | 8277 children (grades 2 and 3) and adolescents (grades 8 and 9) were examined. | |
| Interventions | Exposure: frequency of toothbrushing, fluoride toothpaste used in first 4 years, age started toothbrushing. | |
| Outcomes | TFI. | |
| Notes | Intra‐ and inter‐examiner reliability (Kappa = 0.72 and 0.63 respectively). Inconsistency in the reporting of the number of participants in the text and the tables. |
|
Morgan 1998.
| Methods | Cross‐sectional survey conducted in a fluoridated area in US. | |
| Participants | 246 children examined in a single paediatric dental practice (met the study criteria) and 197 7‐11 years old children included with parental questionnaires returned. | |
| Interventions | Exposure: professional fluoride treatments; initiation and frequency of toothbrushing; adult assistance with toothbrushing; use of fluoride toothpaste; amount of fluoride toothpaste used. | |
| Outcomes | Modified Dean's Index. | |
| Notes | Intra‐examiner reliability (Kappa = 0.58‐0.89). | |
Osuji 1988.
| Methods | Case‐control study conducted in a fluoridated community in Canada. | |
| Participants | 633 children aged 8, 9 and 10 years old screened for fluorosis and 177 interviewed and 139 with full data available for analysis. | |
| Interventions | Case: fluorosis index score >0 (n = 65).
Control: the next non‐case of the same age and sex in the classroom (n = 74). Exposure: professional application of fluoride; early use of fluoride mouthrinses; early use of fluoride toothpaste during the child's first 5 years. |
|
| Outcomes | TFI. Photographic assessment. | |
| Notes | Intra‐examiner reliability (Kappa = 0.93). Small discrepancies in the ORs estimates used in the review (generated by RevMan) compared to the original study. |
|
Pendrys 1989.
| Methods | Case‐control study in non‐fluoridated areas in Massachusetts and Connecticut, US. | |
| Participants | 1242 fluorosis examinations, undertaken in schools, of 11 to 14 year olds (born between 1972 and 1975). 850 cases and controls selected. 680 (80%) questionnaires on exposure returned. | |
| Interventions | Exposure: fluoride supplements (drops or tablets) during each of the first 6 years of life; fluoride toothpaste use during each of the first 6 years of life. | |
| Outcomes | FRI. | |
| Notes | Intra‐ and inter‐examiner reliability of fluorosis examinations checked (Kappa ranging from 0.76 to 1.0). | |
Pendrys 1994.
| Methods | Case‐control study conducted in fluoridated communities in Connecticut, US. | |
| Participants | All 12‐16 years old in participating school districts, and born prior to 1980. 916 examined for enamel fluorosis. 644 diagnosed as either case or control, of which 637 sent questionnaires. 568 questionnaires on exposure returned. 401 used in analysis. | |
| Interventions | Exposure: frequency of brushing, typical amount of toothpaste, and use of fluoride supplements during first 8 years of life; age of commencing toothbrushing. | |
| Outcomes | FRI. | |
| Notes | Intra‐ and inter‐examiner reliability of fluorosis examinations checked between cases and controls (100% agreement). | |
Pendrys 1996.
| Methods | Case‐control study in non‐fluoridated areas in Massachusetts and Connecticut, US. | |
| Participants | All 10‐13 year olds enrolled in participating school districts. 1091 examined for enamel fluorosis. 767 diagnosed as either case or control, of which 754 sent questionnaire. 677 questionnaires on exposure returned. 460 used in analysis. | |
| Interventions | Exposure: frequency of brushing, typical amount of toothpaste, and use of fluoride supplements during first 8 years of life; age of commencing toothbrushing. | |
| Outcomes | FRI. | |
| Notes | Intra‐ and inter‐examiner reliability of fluorosis examinations checked (Kappa ranging from 0.93 and 0.73 respectively). | |
Pendrys 1998.
| Methods | Case‐control study in optimally fluoridated communities in Connecticut, US. | |
| Participants | All 10 to 14 year olds enrolled in participating school districts. 867 examined for enamel fluorosis. 360 diagnosed as either case or control, of which 357 sent questionnaire. 326 (91%) questionnaires on exposure returned. | |
| Interventions | Exposure: frequency of brushing, typical amount of toothpaste, and use of fluoride supplements during first 8 years of life; age of commencing toothbrushing. | |
| Outcomes | FRI. | |
| Notes | Intra‐ and inter‐examiner reliability of fluorosis examinations checked (Kappa = 1.0 and 0.70 respectively). | |
Pereira 2000.
| Methods | Cross‐sectional survey conducted in a non‐fluoridated city in Brazil. | |
| Participants | Children 11‐12 years old randomly selected from school lists and 314 gave parental consent and were examined and parental questionnaires. | |
| Interventions | Exposure: age started using fluoride toothpaste. | |
| Outcomes | TFI. | |
| Notes | Intra‐examiner reliability (Kappa >0.85). | |
Riordan 1993.
| Methods | Cross‐sectional survey conducted in a fluoridated area in Western Australia. | |
| Participants | 418 invited to participate and 350 children 7 years old examined and with parental questionnaires. | |
| Interventions | Exposure: age started using fluoride toothpaste. | |
| Outcomes | TFI. | |
| Notes | Intra‐examiner reliability (weighted Kappa = 0.78). | |
Riordan 2002.
| Methods | Cross‐sectional survey conducted in fluoridated and non‐fluoridated areas in Western Australia. | |
| Participants | Randomly selected 14 schools in fluoridated area and 1 school in non‐fluoridated area. 672 were invited and 582 10 years old children remained and with parental questionnaires. | |
| Interventions | Exposure: age started using fluoride toothpaste. | |
| Outcomes | TFI. | |
| Notes | Intra‐examiner reliability (weighted Kappa = 0.75). | |
Rock 1997.
| Methods | Cross‐sectional survey conducted in a fluoridated area in UK. | |
| Participants | 326 invited and 325 8‐9 years old children from 5 junior schools were examined with parental questionnaires. | |
| Interventions | Exposure: frequency of toothbrushing, age started toothbrushing, type of fluoride toothpaste, amount of fluoride toothpaste used at the time when toothbrushing with fluoride toothpaste started. | |
| Outcomes | TFI. | |
| Notes | Intra‐examiner reliability (Kappa value not reported). | |
Sagheri 2007.
| Methods | Cross‐sectional survey conducted in Germany (non‐fluoridated) and Ireland (fluoridated). | |
| Participants | 377 out of 464 invited (81%, Ireland) and 322 out of 378 invited (85%, Germany) 12 years old children (1 randomly selected class from all schools) examined and with parental questionnaires. | |
| Interventions | Exposure: use of fluoride toothpaste, early experiences of toothbrushing. | |
| Outcomes | Dean's Index. | |
| Notes | Intra‐examiner reliability (Kappa = 0.84). | |
Skotowski 1995.
| Methods | Case‐control study conducted in non‐fluoridated areas in US. | |
| Participants | 157 children 8‐17 years old examined at a university paediatric clinic. | |
| Interventions | Case: children with TSIF >0 (n = 54).
Control: children with TSIF = 0, age and sex matched (n = 54). Exposure: early use of fluoride toothpaste. |
|
| Outcomes | TSIF index. | |
| Notes | No intra‐ or inter‐examiner reliability assessment. | |
Szpunar 1988.
| Methods | Cross‐sectional survey conducted in fluoridated and non‐fluoridated areas in US. | |
| Participants | 1103 6‐12 years old examined and 556 lifetime residents with parental questionnaires were used for analysis. | |
| Interventions | Exposure: age started toothbrushing, age started using fluoride mouthrinse. | |
| Outcomes | TSIF. | |
| Notes | Intra‐examiner reliability (Kappa = 0.85). | |
Tabari 2000.
| Methods | Cross‐sectional survey conducted in fluoridated and non‐fluoridated areas in UK. | |
| Participants | 14 schools in fluoridated area and 15 in non‐fluoridated area were chosen to provide children from a spectrum of socioeconomic background. 718 (fluoridated) and 709 (non‐fluoridated) 8‐9 years old children were eligible, 591 and 585 questionnaires were returned (82% and 83%), 524 and 510 eligible, 409 and 403 provided completed data for analysis. | |
| Interventions | Exposure: age started toothbrushing, frequency of toothbrushing, type of fluoride toothpaste used and the quantity of fluoride toothpaste used when the child's teeth were first brushed. | |
| Outcomes | TFI. | |
| Notes | Intra‐examiner reliability (Kappa = 0.73). | |
Tavener 2006.
| Methods | RCT conducted in non‐fluoridated areas in UK. | |
| Participants | 1009 out of the potential 1318 children aged 8‐10 years old (who participated in a randomised controlled trial at 12 months old until 5‐6 years) were examined. | |
| Interventions | Group 1: Fluoride toothpaste (440 ppm) from 12 months of age to 5‐6 years of age (n = 496).
Group 2: Fluoride toothpaste (1450 ppm) from 12 months of age to 5‐6 years of age (n = 513). A sample of children who were not given toothpaste formed a third group and not included in this review. |
|
| Outcomes | TFI assessed from photographic digital images. | |
| Notes | Intra‐examiner reliability (weighted Kappa = 0.73). Data for the third group not used within this review. Small discrepancies in the ORs estimates used in the review (generated by RevMan) compared to the original study. |
|
Wang 1997.
| Methods | Cross‐sectional survey conducted in a non‐fluoridated area in Norway. | |
| Participants | All except 2 school districts were included, 551 children born in 1988, questionnaires mailed to parents, 383 examined and used in the analysis. | |
| Interventions | Exposure: age started using fluoride toothpaste. | |
| Outcomes | TFI. | |
| Notes | Intra‐examiner reliability (Kappa = 0.71). | |
DDE Index = Developmental Defects of Enamel Index; FRI = Fluorosis Risk Index; ORs = odds ratios; RCT = randomised controlled trial; TFI = Thylstrup and Fejerskov Index; TSIF = Tooth Surface Index of Fluorosis.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Alonge 2000 | No investigation of the exposure of topical fluoride. |
| Bohaty 1989 | Cross‐sectional survey, unclear regarding exposure of topical fluoride under the age of 6 years. |
| Burgstahler 2008 | Conference proceedings. |
| Clark 1994 | Cross‐sectional survey with retrospective, self‐reporting of fluoride supplement use. All children exposed to fluoride toothpaste. |
| Connett 2008 | Conference proceedings. |
| D'Hoore 1992 | Cross‐sectional survey, unclear regarding exposure of topical fluoride under the age of 6 years. |
| Disney 1992 | Conference abstract, insufficient information reported. |
| Ellwood 1992 | Conference abstract, insufficient information reported. Potentially linked with Ellwood 1994. |
| Ellwood 1994 | Toothbrushing habit at 12 years old and assessing enamel opacities by DDE Index. |
| Evans 1991 | DDE Index was used to assess diffuse defects. |
| Gomez‐Santos 2008 | Cross‐sectional surveys at 3 time points evaluating water fluoridation. |
| Gopalakrishnan 1999 | Cross‐sectional survey with no data on the exposure of topical fluoride before the age of 6 years. |
| Heller 1996 | Study report unobtainable. |
| Hong 2006a | Fluorosis in relation to total fluoride intake was investigated, no data on the effects of topical fluoride could be separated for analysis. |
| Hong 2006b | Fluorosis in relation to total fluoride intake was investigated, no data on the effects of topical fluoride could be separated for analysis. |
| Houwink 1979 | Controlled clinical trial investigating enamel defects not specifically for fluorosis. |
| Kumar 2000 | The analysis of the effect of early brushing has been investigated in different combinations with the effects of water fluoridation and fluoride supplement, no data on the effect of early brushing could be separated for analysis. |
| Larsen 1985a | Retrospective cohort investigating the effects of fluoride gel treatment started at 6‐7 years of age. |
| Larsen 1985b | Retrospective cohort. Fluoride tablets plus toothbrushing at school with fluoride toothpaste compared with nothing. No comparison of TFT versus other TFT, placebo or nothing. |
| Levy 1991 | Fluorosis was not clinically assessed. |
| Machado 2008 | Study report unobtainable. |
| Martignon 2000 | Conference abstract, insufficient information reported. |
| Martins 2008 | Cohort study. 2 convenience samples based on socioeconomic status rather than fluoride exposure. Data not useable. |
| Momeni 2007 | No differentiation between different fluoride preventive programmes. |
| Nowjack‐Raymer 1995 | Database no longer exists ‐ data from 5 years old cannot be extracted. |
| Toassi 2005 | Uncertain of timing of exposure to topical fluoride. |
| van der Hoek 2003 | DDE Index was used to assess diffuse opacities as an approximation to fluorosis. |
| Wetzel 1989 | Case series or single cohort study, unclear investigation of topical fluoride exposure before the age of 6 years. |
| Wotlgens 1989 | Children in one group all took fluoride tablets, no investigation of the exposure of topical fluoride. |
DDE Index = Developmental Defects of Enamel Index; TFT = topical fluoride therapy.
Contributions of authors
Designing the review: May Wong (MW), Edward Lo (EL), Helen Worthington (HW) Co‐ordinating the review: Valeria Marinho (VM), Anne‐Marie Glenny (AMG), Boyd Tsang (BT) Undertaking searches and screening search results and retrieved papers against inclusion criteria: MW, EL, BT Appraising quality and extracting data from papers: HW, AMG, MW, VM Writing to authors for additional information: EL, MW Data management for the review and entering data into RevMan: MW Analysis and interpretation of data: HW, MW, VM Writing the review: MW, EL, HW, VM, AMG, BT Providing general advice on the review: EL, HW, VM.
Sources of support
Internal sources
-
School of Dentistry, The University of Manchester, UK.
The University of Manchester pays the salaries of Helen Worthington and Anne‐Marie Glenny. The Cochrane Oral Health Group is supported by the Department of Health, the Manchester Academic Health Sciences Centre (MAHSC) and the NIHR Manchester Biomedical Research Centre.
The University of Hong Kong, CRCG grant, Hong Kong.
External sources
-
Department of Health Cochrane Review Incentive Scheme 2008, UK.
Provided GBP 5000 to support this review.
-
National Institute for Health Research (NIHR), UK.
Funds the editorial base of the Cochrane Oral Health Group.
Declarations of interest
Helen Worthington has an office located in the University of Manchester's Dental Health Unit which is jointly supported by the University of Manchester and Colgate Palmolive. Helen Worthington does not receive any funding from Colgate Palmolive and does not view this as a conflict of interest. There are no other known potential conflicts of interest.
Edited (no change to conclusions)
References
References to studies included in this review
Beltran‐Valladares 2005 {published data only}
- Beltran‐Valladares PR, Cocom‐Tun H, Casanova‐Rosado JF, Vallejos‐Sanchez AA, Medina‐Solis CE, Maupome G. Prevalence of dental fluorosis and additional sources of exposure to fluoride as risk factors to dental fluorosis in schoolchildren of Campeche, Mexico. Revista de Investigacion Clinica 2005;57(4):532‐9. [PubMed] [Google Scholar]
Bottenberg 2004 {published data only}
- Bottenberg P, Declerck D, Ghidey W, Bogaerts K, Vanobbergen J, Martens L. Prevalence and determinants of enamel fluorosis in Flemish schoolchildren. Caries Research 2004;38(1):20‐8. [DOI] [PubMed] [Google Scholar]
Brothwell 1999 {published data only}
- Brothwell DJ, Limeback H. Fluorosis risk in grade 2 students residing in a rural area with widely varying natural fluoride. Community Dentistry & Oral Epidemiology 1999;27(2):130‐6. [DOI] [PubMed] [Google Scholar]
Conway 2005 {published data only}
- Conway DI, MacPherson LMD, Stephen KW, Gilmour WH, Petersson LG. Prevalence of dental fluorosis in children from non‐water‐fluoridated Halmstad, Sweden: fluoride toothpaste use in infancy. Acta Odontologica Scandinavica 2005;63(1):56‐63. [DOI] [PubMed] [Google Scholar]
Do 2007 {published data only}
- Do LG, Spencer AJ. Decline in the prevalence of dental fluorosis among South Australian children. Community Dentistry & Oral Epidemiology 2007;35(4):282‐91. [DOI] [PubMed] [Google Scholar]
- Do LG, Spencer AJ. Risk‐benefit balance in the use of fluoride among young children. Journal of Dental Research 2007;86(8):723‐8. [DOI] [PubMed] [Google Scholar]
- Spencer AJ, Do LG. Changing risk factors for fluorosis among South Australian children. Community Dentistry & Oral Epidemiology 2008;36(3):210‐8. [DOI] [PubMed] [Google Scholar]
Franzman 2006 {published data only}
- Franzman MR, Levy SM, Warren JJ, Broffitt B. Fluoride dentifrice ingestion and fluorosis of the permanent incisors. Journal of the American Dental Association 2006;137(5):645‐52. [DOI] [PubMed] [Google Scholar]
Holt 1994 {published data only}
- Holt RD, Morris CE, Winter GB, Downer MC. Enamel opacities and dental caries in children who used a low fluoride toothpaste between 2 and 5 years of age. International Dental Journal 1994;44(4):331‐41. [PubMed] [Google Scholar]
Mascarenhas 1998 {published data only}
- Mascarenhas AK. Fluoride Toothpaste: a Risk Factor in Dental Fluorosis. Michigan, USA: University of Michigan, 1995. [Google Scholar]
- Mascarenhas AK, Burt BA. Fluorosis risk from early exposure to fluoride toothpaste. Community Dentistry & Oral Epidemiology 1998;26(4):241‐8. [DOI] [PubMed] [Google Scholar]
Maupome 2003 {published data only}
- Clark DC, Berkowitz J. The influence of various fluoride exposures on the prevalence of esthetic problems resulting from dental fluorosis. Journal of Public Health Dentistry 1997;57(3):144‐9. [DOI] [PubMed] [Google Scholar]
- Maupome G, Shulman JD, Clark DC, Levy SM. Socio‐demographic features and fluoride technologies contributing to higher fluorosis scores in permanent teeth of Canadian children. Caries Research 2003;37(5):327‐34. [DOI] [PubMed] [Google Scholar]
Morgan 1998 {published data only}
- Morgan L, Allred E, Tavares M, Bellinger D, Needleman H. Investigation of the possible associations between fluorosis, fluoride exposure, and childhood behavior problems. Pediatric Dentistry 1998;20(4):244‐52. [PubMed] [Google Scholar]
Osuji 1988 {published data only}
- Osuji OO, Leake JL, Chipman ML, Nikiforuk G, Locker D, Levine N. Risk factors for dental fluorosis in a fluoridated community. Journal of Dental Research 1988;67(12):1488‐92. [DOI] [PubMed] [Google Scholar]
Pendrys 1989 {published data only}
- Pendrys DG. An Analytical Epidemiologic Study of the Association Between Enamel Fluorosis and a History of Fluoride Supplementation, Infant Formula Ingestion, and Fluoride Dentifrice Use by Young Children. Ann Arbor, MI: University Microfilms International, 1988. [Google Scholar]
- Pendrys DG, Katz RV. Risk of enamel fluorosis associated with fluoride supplementation, infant formula, and fluoride dentifrice use. American Journal of Epidemiology 1989;130(6):1199‐208. [DOI] [PubMed] [Google Scholar]
Pendrys 1994 {published data only}
- Pendrys DG, Katz RV, Morse DE. Risk factors for enamel fluorosis in a fluoridated population. American Journal of Epidemiology 1994;140(5):461‐71. [DOI] [PubMed] [Google Scholar]
Pendrys 1996 {published data only}
- Pendrys DG. Risk of enamel fluorosis in nonfluoridated and optimally fluoridated populations: considerations for the dental professional. Journal of the American Dental Association 2000;131(6):746‐55. [DOI] [PubMed] [Google Scholar]
- Pendrys DG, Katz RV, Morse DE. Risk factors for enamel fluorosis in a nonfluoridated population. American Journal of Epidemiology 1996;143(8):808‐15. [DOI] [PubMed] [Google Scholar]
Pendrys 1998 {published data only}
- Pendrys DG. Risk of enamel fluorosis in nonfluoridated and optimally fluoridated populations: considerations for the dental professional. Journal of the American Dental Association 2000;131(6):746‐55. [DOI] [PubMed] [Google Scholar]
- Pendrys DG, Katz RV. Risk factors for enamel fluorosis in optimally fluoridated children born after the US manufacturers' decision to reduce the fluoride concentration of infant formula. American Journal of Epidemiology 1998;148(10):967‐74. [DOI] [PubMed] [Google Scholar]
Pereira 2000 {published data only}
- Pereira AC, Cunha FL, Meneghim MdeC, Werner CW. Dental caries and fluorosis prevalence study in a nonfluoridated Brazilian community: trend analysis and toothpaste association. ASDC Journal of Dentistry for Children 2000;67(2):132‐5. [PubMed] [Google Scholar]
Riordan 1993 {published data only}
- Riordan PJ. Dental fluorosis, dental caries and fluoride exposure among 7‐year‐olds. Caries Research 1993;27(1):71‐7. [DOI] [PubMed] [Google Scholar]
Riordan 2002 {published data only}
- Riordan PJ. Dental fluorosis decline after changes to supplement and toothpaste regimens. Community Dentistry & Oral Epidemiology 2002;30(3):233‐40. [DOI] [PubMed] [Google Scholar]
Rock 1997 {published data only}
- Rock WP, Sabieha AM. The relationship between reported toothpaste usage in infancy and fluorosis of permanent incisors. British Dental Journal 1997;183(5):165‐70. [DOI] [PubMed] [Google Scholar]
Sagheri 2007 {published data only}
- Sagheri D, McLoughlin J, Clarkson JJ. The prevalence of dental fluorosis in relation to water or salt fluoridation and reported use of fluoride toothpaste in school‐age children. European Archives of Paediatric Dentistry 2007;8(1):62‐8. [DOI] [PubMed] [Google Scholar]
Skotowski 1995 {published data only}
- Skotowski MC, Hunt RJ, Levy SM. Risk factors for dental fluorosis in pediatric dental patients. Journal of Public Health Dentistry 1995;55(3):154‐9. [DOI] [PubMed] [Google Scholar]
Szpunar 1988 {published data only}
- Szpunar SM, Burt BA. Dental caries, fluorosis, and fluoride exposure in Michigan schoolchildren. Journal of Dental Research 1988;67(5):802‐6. [DOI] [PubMed] [Google Scholar]
Tabari 2000 {published data only}
- Tabari ED, Ellwood R, Rugg‐Gunn AJ, Evans DJ, Davies RM. Dental fluorosis in permanent incisor teeth in relation to water fluoridation, social deprivation and toothpaste use in infancy. British Dental Journal 2000;189(4):216‐20. [DOI] [PubMed] [Google Scholar]
Tavener 2006 {published data only}
- Tavener A, Davies GM, Davies RM, Ellwood RP. The prevalence and severity of fluorosis in children who received toothpaste containing either 440 or 1,450 ppm F from the age of 12 months in deprived and less deprived communities. Caries Research 2006;40(1):66‐72. [DOI] [PubMed] [Google Scholar]
Wang 1997 {published data only}
- Wang NJ, Gropen AM, Ogaard B. Risk factors associated with fluorosis in a non‐fluoridated population in Norway. Community Dentistry & Oral Epidemiology 1997;25(6):396‐401. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Alonge 2000 {published data only}
- Alonge OK, Williamson DD, Narendran S. Dental fluorosis among third graders in Harris County, Texas‐‐1998 study findings. Texas Dental Journal 2000;117(9):22‐9. [PubMed] [Google Scholar]
Bohaty 1989 {published data only}
- Bohaty BS, Parker WA, Seale NS, Zimmerman ER. The prevalence of fluorosis‐like lesions associated with topical and systemic fluoride usage in an area of optimal water fluoridation. Pediatric Dentistry 1989;11(2):125‐8. [PubMed] [Google Scholar]
Burgstahler 2008 {published data only}
- Burgstahler AW, Spittle B. XVIIITH conference of the International Society for Fluoride Research. Fluoride: bone and brain effects. Fluoride 2008;41(3):173‐5. [Google Scholar]
Clark 1994 {published data only}
- Clark DC, Hann HJ, Williamson MF, Berkowitz J. Influence of exposure to various fluoride technologies on the prevalence of dental fluorosis. Community Dentistry & Oral Epidemiology 1994;22(6):461‐4. [DOI] [PubMed] [Google Scholar]
Connett 2008 {published data only}
- Connett P. 3rd citizens conference of the Fluoride Action Network. Fluoride 2008;41(3):175. [Google Scholar]
D'Hoore 1992 {published data only}
- D'Hoore W, Nieuwenhuysen JP. Benefits and risks of fluoride supplementation: caries prevention versus dental fluorosis. European Journal of Pediatrics 1992;151(8):613‐6. [DOI] [PubMed] [Google Scholar]
Disney 1992 {published data only}
- Disney J, Cutress T, Bohannan H, Graves R, Zack D. Fluorosis experience of children enrolled in a caries risk study. Journal of Dental Research 1992;71(Spec Issue):749. [Google Scholar]
Ellwood 1992 {published data only}
- Ellwood RP, O'Mullane DM. Enamel opacities and brushing frequency in non‐fluoridated and fluoridated areas. Journal of Dental Research 1992;71(Spec Issue):612. [Google Scholar]
Ellwood 1994 {published data only}
- Ellwood RP, O'Mullane DM. Tooth brushing behaviour in twelve year old children and dental enamel. Journal of the Irish Dental Association 1994;40(1):12‐5. [PubMed] [Google Scholar]
Evans 1991 {published data only}
- Evans DJ. A study of developmental defects in enamel in 10‐year‐old high social class children residing in a non‐fluoridated area. Community Dental Health 1991;8(1):31‐8. [PubMed] [Google Scholar]
Gomez‐Santos 2008 {published data only}
- Gomez‐Santos G, Gonzalez‐Sierra MA, Vazquez‐Garcia‐Machinena J. Evolution of caries and fluorosis in schoolchildren of the Canary Islands (Spain): 1991, 1998, 2006. Medicina Oral, Patologia Oral y Cirugia Bucal 2008;13(9):E599‐608. [PubMed] [Google Scholar]
Gopalakrishnan 1999 {published data only}
- Gopalakrishnan P, Vasan RS, Sarma PS, Nair KS, Thankappan KR. Prevalence of dental fluorosis and associated risk factors in Alappuzha district, Kerala. National Medical Journal of India 1999;12(3):99‐103. [PubMed] [Google Scholar]
Heller 1996 {published data only}
- Heller KE. Risk Factors for Dental Fluorosis Prevalence and Severity in US Schoolchildren, 1986‐1987. Ann Arbor, MI: University of Michigan, 1996. [Google Scholar]
Hong 2006a {published data only}
- Hong L, Levy SM, Warren JJ, Broffitt B, Cavanaugh J. Fluoride intake levels in relation to fluorosis development in permanent maxillary central incisors and first molars. Caries Research 2006;40(6):494‐500. [DOI] [PubMed] [Google Scholar]
Hong 2006b {published data only}
- Hong L, Levy SM, Broffitt B, Warren JJ, Kanellis MJ, Wefel JS, et al. Timing of fluoride intake in relation to development of fluorosis on maxillary central incisors. Community Dentistry & Oral Epidemiology 2006;34(4):299‐309. [DOI] [PubMed] [Google Scholar]
Houwink 1979 {published data only}
- Houwink B, Wagg BJ. Effect of fluoride dentifrice usage during infancy upon enamel mottling of the permanent teeth. Caries Research 1979;13(4):231‐7. [DOI] [PubMed] [Google Scholar]
Kumar 2000 {published data only}
- Kumar J, Swango P, Haley V, Green E. Intra‐oral distribution of dental fluorosis in Newburgh and Kingston, New York. Journal of Dental Research 2000;79(7):1508‐13. [DOI] [PubMed] [Google Scholar]
Larsen 1985a {published data only}
- Larsen MJ, Kirkegard E, Fejerskov O, Poulsen S. Prevalence of dental fluorosis after fluoride‐gel treatments in a low‐fluoride area. Journal of Dental Research 1985;64(8):1076‐9. [DOI] [PubMed] [Google Scholar]
Larsen 1985b {published data only}
- Larsen MJ, Richards A, Fejerskov O. Development of dental fluorosis according to age at start of fluoride administration. Caries Research 1985;19(6):519‐27. [DOI] [PubMed] [Google Scholar]
Levy 1991 {published data only}
- Levy SM, Zarei‐M Z. Evaluation of fluoride exposures in children. ASDC Journal of Dentistry for Children 1991;58(6):467‐73. [PubMed] [Google Scholar]
Machado 2008 {published data only}
- Machado MAdeAM, Silva TCdaS, Silva SMBda, Oliveira TM. Critical analysis of the use of fluoride in pediatric dentistry [Abordagem critica do uso do fluoreto em odontopediatria]. In: Buzalaf MAR editor(s). Fluoretos e Saude Bucal. Sao Paulo, Brazil: Editora Santos, 2008:271‐95. [Google Scholar]
Martignon 2000 {published data only}
- Martignon S, Granados OL. Prevalence of dental fluorosis and association to risk factors in schoolchildren in Santafe de Bogota, Colombia. Caries Research 2000;34(4):352‐3. [Google Scholar]
Martins 2008 {published data only}
- Martins CC, Paiva SM, Lima‐Arsati YB, Ramos‐Jorge ML, Cury JA. Prospective study of the association between fluoride intake and dental fluorosis in permanent teeth. Caries Research 2008;42(2):125‐33. [DOI] [PubMed] [Google Scholar]
Momeni 2007 {published data only}
- Momeni A, Neuhaeuser A, Renner N, Heinzel‐Gutenbrunner M, Abou‐Fidah J, Rasch K, et al. Prevalence of dental fluorosis in German schoolchildren in areas with different preventive programmes. Caries Research 2007;41(6):437‐44. [DOI] [PubMed] [Google Scholar]
Nowjack‐Raymer 1995 {published data only}
- Nowjack‐Raymer RE, Selwitz RH, Kingman A, Driscoll WS. The prevalence of dental fluorosis in a school‐based program of fluoride mouthrinsing, fluoride tablets, and both procedures combined. Journal of Public Health Dentistry 1995;55(3):165‐70. [DOI] [PubMed] [Google Scholar]
Toassi 2005 {published data only}
- Toassi RFC, Abegg C. Dental fluorosis in schoolchildren in a county in the mountainous region of Rio Grande do Sul State, Brazil. Cadernos de Saude Publica 2005;21(2):652‐5. [DOI] [PubMed] [Google Scholar]
van der Hoek 2003 {published data only}
- Hoek W, Ekanayake L, Rajasooriyar L, Karunaratne R. Source of drinking water and other risk factors for dental fluorosis in Sri Lanka. International Journal of Environmental Health Research 2003;13(3):285‐93. [DOI] [PubMed] [Google Scholar]
Wetzel 1989 {published data only}
- Wetzel WE. Dental fluorosis from repeated fluoride use. Die Quintessenz 1989;40(10):1799‐807. [PubMed] [Google Scholar]
Wotlgens 1989 {published data only}
- Woltgens JHM, Etty WJ, Nieuwland WMD, Lyaruu DM. Use of fluoride by young children and prevalence of mottled enamel. Advances in Dental Research 1989;3(2):177‐82. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Larsen 1987 {published data only}
- Larsen MJ, Kirkegaard E, Poulsen S, Fejerskov O. Dental fluorosis in Denmark. II. Large single doses of fluoride and dental fluorosis. Tandlaegebladet 1987;91(18):761‐4. [PubMed] [Google Scholar]
Additional references
Alvarez 2009
- Alvarez JA, Rezende K, Marocho SMS, Alves FBT, Celiberti P, Ciamponi AL. Dental fluorosis: Exposure, prevention and management. Medicina Oral, Patologia Oral y Cirugia Bucal 2009;14(2):E103‐7. [PubMed] [Google Scholar]
Barnhart 1974
- Barnhart WE, Hiller LK, Leonard GJ, Michaels SE. Dentifrice usage and ingestion among four age groups. Journal of Dental Research 1974;53(6):1317‐22. [DOI] [PubMed] [Google Scholar]
Chen 2006
- Chen H, Czajka‐Jakubowska A, Spencer NJ, Mansfield JF, Robinson C, Clarkson BH. Effects of systemic fluoride and in vitro fluoride treatment on enamel crystals. Journal of Dental Research 2006;85(11):1042‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Clark 1993
- Clark DC. Appropriate uses of fluorides for children: guidelines from the Canadian Workshop on the Evaluation of Current Recommendations Concerning Fluorides. Canadian Medical Association Journal 1993;149(12):1787‐93. [PMC free article] [PubMed] [Google Scholar]
Cunha 2006
- Cunha LF, Tomita NE. Dental fluorosis in Brazil: a systematic review from 1993 to 2004. Cadernos de Saude Publica 2006;22(9):1809‐16. [DOI] [PubMed] [Google Scholar]
Do 2007
- Do LG, Spencer AJ. Risk‐benefit balance in the use of fluoride among young children. Journal of Dental Research 2007;86(8):723‐8. [DOI] [PubMed] [Google Scholar]
Ekstrand 1987
- Ekstrand J. Pharmacokinetic aspects of topical fluorides. Journal of Dental Research 1987;66(5):1061‐5. [DOI] [PubMed] [Google Scholar]
Ekstrand 1996
- Ekstrand J. Fluoride metabolism. In: Fejerskov O, Ekstrand J, Burt BA editor(s). Fluoride in Dentistry. 2nd Edition. Copenhagen: Munksgaard, 1996:50‐68. [Google Scholar]
Gillcrist 1996
- Gillcrist JA. Fluoridation status of Tennesseans, declining caries prevalence rates, increasing fluorosis, and a review of the appropriate use of fluoride products. Journal of Tennessee Dental Association 1996;76(3):12‐7. [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions version 5.0.1 (updated September 2008). The Cochrane Collaboration, 2008. Available from www.cochrane‐handbook.org.
Holloway 1997
- Holloway PJ, Ellwood RP. The prevalence, causes and cosmetic importance of dental fluorosis in the United Kingdom: a review. Community Dental Health 1997;14(3):148‐55. [PubMed] [Google Scholar]
Ismail 2008
- Ismail AI, Hasson H. Fluoride supplements, dental caries and fluorosis: a systematic review. Journal of the American Dental Association 2008;139(11):1457‐68. [DOI] [PubMed] [Google Scholar]
Kargul 2003
- Kargul B, Caglar E, Tanboga I. History of water fluoridation. Journal of Clinical Pediatric Dentistry 2003;27(3):213‐7. [DOI] [PubMed] [Google Scholar]
Kubota 2005
- Kubota K, Lee DH, Tsuchiya M, Young CS, Everett ET, Martinez‐Mier EA, et al. Fluoride induces endoplasmic reticulum stress in ameloblasts responsible for dental enamel formation. Journal of Biological Chemistry 2005;280(24):23194‐202. [DOI] [PubMed] [Google Scholar]
Lecompte 1987
- Lecompte EJ. Clinical application of topical fluoride products: risks, benefits and recommendations. Journal of Dental Research 1987;66(5):1066‐71. [DOI] [PubMed] [Google Scholar]
Levy 1994
- Levy SM. Review of fluoride exposures and ingestion. Community Dentistry & Oral Epidemiology 1994;22(3):173‐80. [DOI] [PubMed] [Google Scholar]
Loke 2007
- Loke YK, Price D, Herxheimer A, Cochrane Adverse Effects Methods Group. Systematic reviews of adverse effects: framework for a structured approach. BMC Medical Research Methodology 2007;7:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Manji 1986
- Manji F, Kapila S. Fluorides and fluorosis in Kenya. Part III: Fluorides, fluorosis and dental caries. Odonto‐Stomatologie Tropicale 1986;9(3):135‐9. [PubMed] [Google Scholar]
Marinho 2002
- Marinho VCC, Higgins JPT, Logan S, Sheiham A. Fluoride gels for preventing dental caries in children and adolescents. Cochrane Database of Systematic Reviews 2002, Issue 1. [Art. No.: CD002280. DOI: 10.1002/14651858.CD002280] [DOI] [PubMed] [Google Scholar]
Marinho 2002b
- Marinho VCC, Higgins JPT, Logan S, Sheiham A. Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database of Systematic Reviews 2002, Issue 1. [Art. No.: CD002279. DOI: 10.1002/14651858.CD002279] [DOI] [PubMed] [Google Scholar]
Marinho 2003
- Marinho VCC, Higgins JPT, Logan S, Sheiham A. Topical fluoride (toothpastes, mouthrinses, gels or varnishes) for preventing dental caries in children and adolescents. Cochrane Database of Systematic Reviews 2003, Issue 4. [Art. No.: CD002782. DOI: 10.1002/14651858.CD002782] [DOI] [PMC free article] [PubMed] [Google Scholar]
Marinho 2003b
- Marinho VCC, Higgins JPT, Logan S, Sheiham A. Fluoride toothpastes for preventing dental caries in children and adolescents. Cochrane Database of Systematic Reviews 2003, Issue 1. [Art. No.: CD002278. DOI: 10.1002/14651858.CD002278] [DOI] [PMC free article] [PubMed] [Google Scholar]
Marinho 2003c
- Marinho VCC, Higgins JPT, Logan S, Sheiham A. Fluoride mouthrinses for preventing dental caries in children and adolescents. Cochrane Database of Systematic Reviews 2003, Issue 3. [Art. No.: CD002284. DOI: 10.1002/14651858.CD002284] [DOI] [PubMed] [Google Scholar]
Marinho 2004
- Marinho VCC, Higgins JPT, Sheiham A, Logan S. One topical fluoride (toothpastes, or mouthrinses, or gels, or varnishes) versus another for preventing dental caries in children and adolescents. Cochrane Database of Systematic Reviews 2004, Issue 1. [Art. No.: CD002780. DOI: 10.1002/14651858.CD002780.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Marinho 2004b
- Marinho VCC, Higgins JPT, Sheiham A, Logan S. Combinations of topical fluoride (toothpastes, mouthrinses, gels, varnishes) versus single topical fluoride for preventing dental caries in children and adolescents. Cochrane Database of Systematic Reviews 2004, Issue 1. [Art. No.: CD002781. DOI: 10.1002/14651858.CD002781.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mascarenhas 2000
- Mascarenhas AK. Risk factors for dental fluorosis: a review of the recent literature. Pediatric Dentistry 2000;22(4):269‐77. [PubMed] [Google Scholar]
Pendrys 1990
- Pendrys DG, Stamm JW. Relationship of total fluoride intake to beneficial effects and enamel fluorosis. Journal of Dental Research 1990;69 Spec No:529‐38. [DOI] [PubMed] [Google Scholar]
Pendrys 2000
- Pendrys DG. Risk of enamel fluorosis in nonfluoridated and optimally fluoridated populations: considerations for the dental professional. Journal of the American Dental Association 2000;131(6):746‐55. [DOI] [PubMed] [Google Scholar]
Ripa 1991
- Ripa LW. A critique of topical fluoride methods (dentifrices, mouthrinses, operator‐, and self‐applied gels) in an era of decreased caries and increased fluorosis prevalence. Journal of Public Health Dentistry 1991;51(1):23‐41. [DOI] [PubMed] [Google Scholar]
Rozier 1994
- Rozier RG. Epidemiologic indices for measuring the clinical manifestations of dental fluorosis: overview and critique. Advances in Dental Research 1994;8(1):39‐55. [DOI] [PubMed] [Google Scholar]
Steiner 2004
- Steiner M, Helfenstein U, Menghini G. Effect of 1000 ppm relative to 250 ppm fluoride toothpaste. A meta‐analysis. American Journal of Dentistry 2004;17(2):85‐8. [PubMed] [Google Scholar]
Stookey 1994
- Stookey GK. Review of fluorosis risk of self‐applied topical fluorides: dentifrices, mouthrinses and gels. Community Dentistry & Oral Epidemiology 1994;22(3):181‐6. [DOI] [PubMed] [Google Scholar]
Tobin 1988
- Tobin EA. Dental fluorosis in children in the 1980s. A review of the literature. Dental Hygiene 1988;62(8):380‐4. [PubMed] [Google Scholar]
Walsh 2010
- Walsh T, Worthington HV, Glenny A‐M, Appelbe P, Marinho VCC, Shi X. Fluoride toothpastes of different concentrations for preventing dental caries in children and adolescents. Cochrane Database of Systematic Reviews 2010, Issue 1. [DOI: 10.1002/14651858.CD007868.pub2] [DOI] [PubMed] [Google Scholar]
Warren 1999
- Warren JJ, Levy SM. A review of fluoride dentifrice related to dental fluorosis. Pediatric Dentistry 1999;21(4):265‐71. [PubMed] [Google Scholar]
Wells 2008
- Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle‐Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta‐analyses. Available from: www.ohri.ca/programs/clinical_epidemiology/oxford.htm (accessed 1 January 2008).
Whelton 2004
- Whelton HP, Ketley CE, McSweeney F, O'Mullane DM. A review of fluorosis in the European Union: prevalence, risk factors and aesthetic issues. Community Dentistry & Oral Epidemiology 2004;32 Suppl 1:9‐18. [DOI] [PubMed] [Google Scholar]


