Abstract
Introduction
Pregnant women who disclose their HIV-positive status to their sexual partners have played an important role in reducing the risk of HIV/AIDS transmission to the baby during the antepartum, intrapartum, and postnatal periods. Studies are limited in the current study area in a similar arena. Therefore, this study aimed to assess the proportion of HIV-positive status disclosure and its associated factors among pregnant women.
Methods
A facility-based cross-sectional study was conducted among 156 HIV-positive pregnant women in Dire Dawa administrative from March 12th to May 10th, 2020. Data were generated using a pretested structured questionnaire through face-to-face interviews. Binary logistic regression analysis was employed to identify the predictor variables associated with the disclosure of HIV-positive status among pregnant women to their sexual partners. Finally, the adjusted odds ratio with 95% confidence intervals at P-value< 0.05 was considered statistically significant.
Results
Of the total, 135 (86.5%) of HIV-positive pregnant women disclosed their HIV status to their sexual partner. Christian followers (both Orthodox and Protestant) [AOR = 8.8, 95% CI: 2.3. 34] more likely to disclose HIV status to their sexual partner than those Muslims. Those participants who started practicing safer sex [AOR = 17.6, 95% CI: 4–77] and those women who had a smooth relationship before the HIV disclosure were [AOR = 14.7, 95% CI: 3–68.6] more likely to disclose HIV status to their sexual partner than their counterparts, respectively.
Conclusions
The proportion of HIV serostatus disclosure by HIV-positive pregnant women attending antenatal care services to their sexual partners was encouraging. However, this does not mean that there is no need for further awareness and intervention. Hence, interventions to boost and support women in safely disclosing their HIV-positive status are needed.
Introduction
Globally, in 2019, females accounted for 48% of all new HIV infections, and in sub-Saharan Africa, they accounted for 59% of all new HIV infections. Globally, 1.8 million and in Ethiopia, 44,000 children are living with HIV in the same year [1]. In Ethiopia, about 670,000 people were living with HIV in 2019, and women older than 15 years accounted for 390,000 (58.2%) of the total [2].
HIV-positive status disclosure to a sexual partner leads to safer sexual practices, prevention of re-infection, social and emotional, financial, and encourages partners to make informed reproductive health choices [3, 4]. It is also a crucial goal in HIV testing and counseling, and it increases the involvement of a woman partner in the prevention of mother-to-child transmission services [5–10]. However, disclosure remains a challenge for many pregnant women [9].
Also, disclosure enables HIV-positive pregnant women to understand HIV infection and make sense of their disease-related experiences and take part in healthcare decision-making for good or improved adherence to antiretroviral therapy [3]. It leads to positive health outcomes for both the patient and partner. It improved care-seeking behavior like condom use, partner testing that reduces the risk of HIV transmission, and social support, emotional well-being, improve long-term HIV care engagement among pregnant women, and an improved outlook for the future [11–14].
Despite this positive outcome, disclosure is a complex process that requires caution to prevent the occurrence of a bad outcome. It is a time of conflict with a partner, abuse, and withdrawal of finances [12, 15–18]. While HIV care engagement is vital during the antenatal period to PMTCT, it is a time of barriers to disclosure that happened [19]. To overcome these barriers, couple testing, advanced counseling, and overcoming the problem of stigma are the strategies for enhancing disclosure and prevention of HIV transmission [17].
Despite HIV-positive status, nondisclosure is the major challenge for HIV/AIDS care, a few studies have stated these issues in our country [20]. In 2020, the Global HIV Prevention Coalition has launched a program in 2017 to decrease new HIV infections by 75% [21]. Similarly, Ethiopia’s developed National HIV Prevention Road Map is aligned with the national HIV/AIDS strategic plan 2015–2020 [22]. National HIV strategies implemented specific interventions focused on the PMTCT of HIV. It includes HIV testing for all mothers during ANC and counseling for those who test positive emphasis on ART and its adherence and also to encourage them to tell the HIV status to their sexual partners.
Around the world, mother to child transmission is a significant cause of HIV-infections among children, especially in developing countries. Around 60% of HIV infections occur among women in most parts of Africa, and the rate is as high as 40% among antenatal care attendees in Sub Sahara Africa [23]. In a study conducted in Cameroon, the risk of HIV transmission from mother to baby is 30–45% in the absence of any intervention [24]. With no intervention, about 35% of children born to HIV-positive women are at risk of being infected with the virus [25].
HIV-positive disclosure to sexual partners reduces the risk of HIV transmission to the baby during the antenatal, intrapartum, and postnatal periods [4]. One study revealed that disclosing one’s serostatus for their sexual partner was predicted to decrease the risk of HIV transmission by between 17.9% and 40.6% relative to non-disclosed [26]. Another study showed that serostatus disclosure would contribute to minimizing HIV transmission to the child by 41% [9]. The studies conducted in sub-Saharan Africa showed that HIV-positive status disclosure to sexual partners among HIV-positive pregnant women was lower than the general population of people living with HIV [27].
Moreover, the studies were limited in the current study area. Therefore, this study aimed to determine the prevalence of HIV-positive status disclosure to sexual partners and its associated factors among HIV-positive pregnant women in Dire Dawa.
Methods and materials
Study setting and period
We conducted the study from 12th of March to 10th May 2020 in Dire Dawa. Dire Dawa is 515 km away from the center, Addis Ababa to the East. Dire Dawa is one of two chartered cities in Ethiopia with the other Addis Ababa. Dire Dawa had about 506,936 total population consists of 248,298 males and 258,638 females. About 162,220 (32%) rural and 344,716 urban residents with an average household size of 4.5, and 2.5 a population growth rate. Dire Dawa administrative had 38 rural and 9 urban Kebeles.
Dire Dawa Administration has two public hospitals, 15 health centers, and 34 health posts. Of these, ten public health facilities (two hospitals and eight health centers) are providing PMTCT services. According to Central Statistical Agency (CSA) and Inner city fund (ICF), in 2018, the Dire Dawa administration is the 3rd HIV prevalent region with the rate of 2.5% next to Gambella and Addis Ababa in Ethiopia. EDHS 2011 showed that 4.3% of reproductive-aged (15–49) women are living with HIV in Dire Dawa. We included all ten public health facilities (two hospitals and eight health centers) providing PMTCT in the Dire Dawa administrative. All ten public health facilities with a client flow of 5–18 HIV-positive pregnant women per month were included in the study. According to mini EDHS 2019, 83.8% of women are receiving antenatal care from a skilled provider in the Dire Dawa Administration.
Study design and population
A facility-based cross-sectional was conducted among selected HIV-positive pregnant women attending antenatal care services in the public health facilities of Dire Dawa administrative.
Sample size and sampling procedure
The sample size was obtained by single population proportion formula using the assumption, p-value from the previous study finding (89.7%) of pregnant women had disclosed HIV-positive to their sexual partner [10], 95% CI, and a margin of error-0.05. However, since the total number of HIV-positive pregnant women was 161, we included all of them in this study. Pregnant women who met the eligibility criteria were contacted through the midwives/nurses in charge of the maternal and child health units of the selected hospitals and health centers. They were informed about the study, including providing adequate information regarding the purpose, procedure, benefits, and risks of the study. Then, we used a consecutive sampling method to select the eligible participants. To be included in the study, the participants had to be women who had attended focused antenatal care (FANC) at least twice in the selected health facilities and tested positive for HIV infection, aged 15–49 years, could communicate well in Amharic (local working language) and had lived in the study area for at least 6 months. One hundred fifty-six (156) study participants who fulfilled the eligibility criteria were interviewed during their ANC visit.
Data collection tools and procedure
Data were collected through face-to-face interviews using structured and pre-tested tools. We have adapted it based on different literature which, includes socio-demographic characteristics, disclosure status and health service-related practice, and psychosocial characteristics among HIV-positive pregnant women [10, 28, 29]. The questionnaire was designed in English and translated into the local Amharic language and then translated back to English. We used ten trained health professionals who work in the same health facilities for the collection of data, and one MSc midwife supervises the data collection process.
The quality of data was assured by pre-testing of data collection tools on 10% (17 pregnant women) in Hiwot Fana Referral specialized Hospital from Jan 31th- February 10th, 2020, and necessary corrections on the instrument were incorporated. Data collectors took training on the purposes, the significance of the study, the art of interviewing, and meanings of each question, and the ethical issue. Every day, the supervisor and investigators reviewed each questionnaire for completeness, and we offered the orientation to data collectors every morning.
Measurement and definitions
HIV serostatus disclosure refers to the action of telling the status of the HIV-positive test result to a sexual partner and making it revealed and known by him. In this study, disclosure of HIV serostatus was measured by using the question "does your most recent sexual partner know your HIV status?" and answers are yes or no [10].
Sexual partner refers to a woman’s most recent male partner in marriage who is biologically responsible for her current pregnancy.
Data processing and analysis
We checked data for consistency and entered Epi Data version 4.2 and then exported it to the Statistical Package for Social Sciences (SPSS) version 24.0 software for analysis. Descriptive statistics like frequency, proportion, mean, and standard deviation computed to describe study variables about the population. Both bivariate and multivariate Logistic regressions analyses were used to determine the effect of independent variables on the outcome variables. Variables found to have a P-value <0.2 in the bivariate logistic regression entered/exported into multivariate analysis to identify the predictor variables. Then, the adjusted odds ratio with 95% CI at P-value< 0.05 was considered a statistically significant association with the outcome variable.
Ethical consideration
We obtained ethical clearance from the institutional review board of Addis Ababa University with approval protocol number: 051/20/SNM. Then, a support letter with Ethical clearance was offered to Dire Dawa administration Regional Health Bureaus, health facilities (hospital and health centers). Permission was obtained from each center’s administrative body. Participation of all respondents was voluntary and written informed consent was ensured before engaging in the study. Written consent was also obtained from parents and/or guardians of the minors included in the study. Measures were taken to assure the respect, norms, values, beliefs, culture, and freedom of each individual participating in the study. Information on the purpose and procedures of the study was explained; confidentiality was maintained by omitting their identifications such as names, and a great deal of care and information was assured verbally to all study participants. The interview was carried out in a private room.
Result
Sociodemographic characteristics of participants
A total of156 pregnant women were interviewed. The mean age of the participants was 30.69 (SD ±3.957) years. Of 156 respondents, 59 (37.8%) were housewives, and fifty-four (34.6%) of the participants attended primary school. More than half, 84 (53.8%) had established a sexual relationship for two years and below with their partner (Table 1).
Table 1. Sociodemographic characteristics of HIV-positive pregnant women attending ANC service in public health facilities in Dire Dawa, Ethiopia, 2020, (n = 156).
| Variables | Number | Percent (%) |
|---|---|---|
| Age (years) | ||
| 15–29 | 51 | 32.7 |
| 30 and above | 105 | 67.3 |
| Ethnicity | ||
| Oromo | 75 | 48.1 |
| Amhara | 57 | 36.5 |
| Tigre | 6 | 3.8 |
| Gurage | 9 | 5.8 |
| Somali | 6 | 3.8 |
| Others | 3 | 1.9 |
| Religion | ||
| Orthodox | 63 | 40.4 |
| Muslim | 69 | 44.2 |
| protestant | 24 | 15.4 |
| Marital status | ||
| Married | 101 | 64.7 |
| single | 17 | 10.9 |
| Divorced | 30 | 19.3 |
| Widowed | 8 | 5.1 |
| Educational level | ||
| No formal education | 36 | 23.1 |
| Primary (1–8) | 54 | 34.6 |
| Secondary and above | 66 | 42.3 |
| Occupation | ||
| Government employee | 15 | 9.6 |
| Private employee | 24 | 15.4 |
| Housewife | 59 | 37.8 |
| Daily labor | 27 | 17.3 |
| Merchant | 21 | 13.5 |
| Commercial sex worker | 3 | 1.9 |
| Others | 7 | 4.5 |
| Duration of relationship with partners (year) | ||
| Two years and below | 84 | 53.8 |
| Above two years | 72 | 46.2 |
*Hadiya, **Student, Jobless.
HIV-positive status disclosure to a sexual partner
According to the finding, 135 (86.5%) pregnant women shared their HIV-positive status with their sexual partners. Following disclosure, 72 (46.2%) of the male sexual partners were supportive of their partners. Regarding the time of disclosure, 81 (51.9%) disclosed within the 1st month of diagnosis, and 87 (55.8%) of women known their HIV status during ANC. Nearly half 75 (48.1%) of the mothers had sex with a partner before disclosure, among those 48 (30%) of them used condoms. Over half, 90 (57.7%) of the study participants were given information about HIV before testing. Participants who disclose HIV status to others was 80 (51.9%) and started practicing safer sex was 133 (85.3%) (Table 2).
Table 2. Seropositive HIV status disclosure experience by HIV-positive pregnant women attendant ANC service in public health facilities in Dire Dawa, Ethiopia, 2020, (n = 156).
| Variables | Number | Percent (%) |
|---|---|---|
| Partner’s reaction to HIV status disclosure | ||
| Supportive | 72 | 46.2 |
| Worried about his own HIV status | 39 | 25.0 |
| Blamed me to infect him | 6 | 3.8 |
| Talked about divorcing me | 9 | 5.8 |
| Other | 9 | 5.8 |
| Duration of time for disclosure since diagnosed | ||
| Less than 1month | 81 | 51.9 |
| 1–2 month | 33 | 21.2 |
| 3–4 months | 15 | 9.6 |
| More than 4 months | 6 | 3.8 |
| Have you sex with your partner before disclosure | ||
| Yes | 75 | 48.1 |
| No | 60 | 38.5 |
| If yes, did you use a condom | ||
| Yes | 48 | 30.8 |
| No | 27 | 17.3 |
| Given any information about HIV before you tested | ||
| Yes | 90 | 57.7 |
| No | 66 | 42.3 |
| Information that was given by the health care worker | ||
| General about HIV | 33 | 21.2 |
| HIV transmission only | 27 | 17.3 |
| HIV prevention only | 21 | 13.5 |
| Positive living | 3 | 1.9 |
| Disclosure of HIV status to others | ||
| Yes | 81 | 51.9 |
| No | 75 | 48.1 |
| Started practicing safer sex | ||
| Yes | 133 | 85.3 |
| No | 23 | 14.7 |
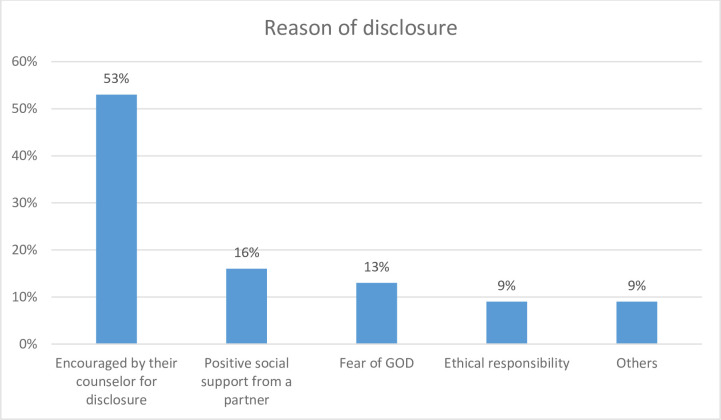
Reason for disclosure HIV status to a partner
The reason for the disclosure, 83 (53%) of pregnant women were reported encouragement from their counselors about disclosure, followed by having positive social support from a partner (Fig 1).
Fig 1. Participants’ reasons for disclosure of their HIV-positive status to a partner.
Psychosocial factors of HIV-positive pregnant women
Of the total, 72 (46.2%) of them had challenges of telling their HIV test result to their sexual partners; of these 30 (19.2%) of them reported fear of lack of support from their partner. Over half, 83 (53.2%) of participants have self-stigma, and 72 (46.2%) of the women have also shared their HIV-positive test results with their families. Regarding the relationship of participants with their partner before the HIV test, 138 (88.5%) of the participants have a smooth relationship (Table 3)
Table 3. Psychosocial factors among HIV-positive pregnant women attending ANC service in selected public health facilities in Dire Dawa, Ethiopia, 2020 (n = 156).
| Variables | Number | Percent (%) |
|---|---|---|
| Have you had challenges telling your sexual partner about your HIV + status? | ||
| Yes | 72 | 46.2 |
| No | 84 | 53.8 |
| What are the challenges? | ||
| Fear of lack of support from their partner | 30 | 19.2 |
| Fear of the spread of information | 12 | 7.7 |
| Fear of abandonment | 12 | 7.7 |
| Fear of deterioration in the relationship with a partner | 6 | 3.8 |
| Fear of discrimination by family and community | 6 | 3.8 |
| Fear of violence | 6 | 3.8 |
| Do the participants have self-stigma? | ||
| Yes | 83 | 53.2 |
| No | 73 | 46.8 |
| Family know that you are HIV-positive | ||
| Yes | 72 | 46.2 |
| No | 84 | 53.8 |
| If yes, who are they | ||
| Parents | 39 | 25.0 |
| Siblings | 18 | 11.6 |
| Children | 6 | 3.8 |
| All of them | 9 | 5.8 |
| How they get to know about your HIV-positive status | ||
| I told them myself | 36 | 23.1 |
| They escorted me to get results | 33 | 21.2 |
| They got information from other people | 3 | 1.9 |
| Relationship with your partner before the HIV test | ||
| Smooth relationship | 138 | 88.5 |
| With disagreement | 18 | 11.5 |
| Relationship with your partner after disclosure of HIV test results | ||
| Smooth relationship | 81 | 51.9 |
| With disagreement | 75 | 48.1 |
Associated factors of HIV-positive status disclosure to sexual partners among HIV-infected pregnant women
In multivariate analysis, three factors are significantly associated, such as the religion of mothers, who started practicing safer sex, and relationships with a partner before the HIV test.
Those Christian followers “Orthodox and Protestants” were approximately 9 [AOR = 8.8, 95% CI, 2.3–34] times more likely to disclose HIV status to their sexual partner than those Muslim. Participants who started practicing safer sex were [AOR = 17.6, 95% CI, 4–77] times more likely to disclose HIV-positive to their sexual partner than those who did not practice. Another, those mothers who had a smooth relationship with their partner before the HIV test were 14.7 [AOR = 14.7 95% CI, 3–68.6] times more likely to tell HIV status to their partner than those mothers with a disagreement with their partners (Table 4).
Table 4. Factors associated with HIV-positive status disclosure to sexual partner among PMTCT attendees women in public health facilities in Dire Dawa, 2020, (n = 156).
| Variables | Disclosure status (N = 156) | COR (95% CI) | AOR (95% CI) | P-value | |
|---|---|---|---|---|---|
| Yes (N = 135) | No (N = 21) | ||||
| Marital Status (currently) | |||||
| Married | 91 | 10 | 2.27 (0.9–5.7) | 1.045 (0.3–3.6) | 0. 944 |
| Not | 44 | 11 | 1 | 1 | |
| Religion of women | |||||
| Christian | 81 | 6 | 3.75 (1.4–10.3) | 8.8 (2.3–34) | 0.002* |
| Muslim | 54 | 15 | 1 | 1 | |
| Duration of relationship with partners (year) | |||||
| 0–2 year | 69 | 15 | 1 | 1 | |
| Above two years | 66 | 6 | 2.4 (0.87–6.5) | 3.78 (0.9–15.8) | 0. 069 |
| HIV status of partner | |||||
| Positive | 63 | 6 | 1 | 1 | |
| Negative | 72 | 15 | 2.2 (0.8–5.9) | 1.2(0.34–4.2) | 0. 769 |
| Started practicing safer sex | |||||
| Yes | 123 | 12 | 7.7 (2.7–21.9) | 17.6 (4–77) | 0.000* |
| No | 12 | 9 | 1 | 1 | |
| Relationship with a partner before the HIV test | |||||
| Smooth relationship | 123 | 12 | 7.6 (2.7–21.9) | 14.7 (3–68.6) | 0.001* |
| With disagreement | 12 | 9 | 1 | 1 | |
*Statistically significant at p-value <0.05 in multivariate logistic regression analysis.
Discussion
In this study, the overall prevalence of disclosure of HIV status to sexual partners among pregnant women LHIV+ was 86.5%. This was similar to that of studies from Nigeria (88%) [30], Uganda (85.4%) [16]. It is also comparable to the studies conducted in Gondar and Addis Ababa (2019), which was 89.7% and 80.6%, respectively [10, 31].
However, this finding is higher than the studies conducted in Uganda and Tanzania were 69% and 41%, respectively [9, 26]. Similarly, this higher than the studies conducted in a different place of Ethiopia in southwest Ethiopia, Addis Ababa (2013), and Mekelle which was 69%, 72.9%, and 57.4%, respectively [28, 29, 32]. This difference might be because of variations in the study population difference since the current study included specifically only HIV-positive pregnant women while the studies conducted in Uganda, Mekelle, and Southwest Ethiopia included all mothers, sampling size among others. The other reason may be the elapsed study period that leads there is encouraging disclosure by a health care professional, and improvement issues related to stigma, and there is access to PMTCT services with partner joint in the current study.
In this study, participants who started practicing safer sex were 17 times more likely to disclose HIV-positive to their sexual partner than those who did not practice. Studies do not support this finding. This might because starting or need to use a condom as unusual leads to questioning the sexual partner. This repeated question may lead to the disclosure of HIV test status.
Another, participants who had a smooth relationship with their partner before the HIV test were 14.7 times more likely to disclose HIV status to a sexual partner than those compared with have not. This finding agrees with many other studies conducted in Ethiopia [10, 28, 29]. The justification might be because the couple’s prior smooth relation leads to better communication, and also it avoids the secret between couples and avoids the fear of women to disclose.
Conclusion
The proportion of HIV serostatus disclosure by HIV-positive pregnant women attending antenatal care services to their sexual partners was encouraging. However, this doesn’t mean that there will be no need for further awareness and intervention. Hence, interventions to boost and support women in safely disclosing their HIV + status are compulsory.
Limitations
We should interpret the findings of this study considering its limitations. The result of this study depended on self-report of a sensitive topic disclosure of HIV status. As in all cross-sectional studies, we can infer association but not causation from our results. The findings of this study were limited to the study setting. The information obtained from women could also be subject to recall bias. Besides, not interviewing health workers and exclusion of HIV-positive pregnant women missing visits or whose follow-up visits not within the study period might affect the results of the study.
Supporting information
(DOCX)
(DOCX)
Acknowledgments
We acknowledge the Addis Ababa University institutional review board for giving us ethical clearance and advising us to do this study. We are thankful to the Dire Dawa administrative Regional Health Bureau for providing us permission to conduct the study in public health facilities. Finally, the authors are also grateful to the data Collectors and the study participants.
Abbreviations and acronyms
- AIDS
Acquired Immune Deficiency Syndrome
- ANC
Antenatal Care
- ART
Antiretroviral Therapy
- CSA
Central Statistical Agency
- ANC
Antenatal Care
- FANC
Focused Antenatal Care
- ICF
Inner city fund
- HIV
Human Immunodeficiency Virus
- PMTCT
Prevention of Mother to child transmission of HIV
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
Addis Ababa University has supported the study with grant number: AAUMF 03-008/2020 (Recipient: Mulusew Ambissa). The funders had no role in study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Global, HIV Statistics, AIDS statistics-2019 fact sheet. 2020. https://scholar.google.com/scholar?hl=en&as_sdt=0%2C5&q=Global+HIV+%26+AIDS+statistics+%E2%80%94+2020+fact+sheet&btnG.
- 2.UNAIDS. 2019. https://www.unaids.org/en/regionscountries/countries/ethiopia.
- 3.Bajunirwe F, Arts EJ, Tisch DJ, King CH, Debanne SM, Sethi AK. Adherence and treatment response among HIV-1-infected adults receiving antiretroviral therapy in a rural government hospital in Southwestern Uganda. Journal of the International Association of Physicians in AIDS Care. 2009. March; 8(2):139–47. 10.1177/1545109709332470 [DOI] [PubMed] [Google Scholar]
- 4.Shiyoleni MN. Non-disclosure of HIV serostatus to partners among HIV positive pregnant women enrolled in the prevention of mother to child transmission (PMTCT) program at Katutura Antenatal Clinic, Windhoek, Namibia (Doctoral dissertation, Stellenbosch: Stellenbosch University). http://hdl.handle.net/10019.1/79858.
- 5.Alemayehu M, Yohannes G, Damte A, Fantahun A, Gebrekirstos K, Tsegay R, et al. Prevalence and predictors of sexual violence among commercial sex workers in Northern Ethiopia. Reproductive health. 2015. December; 12 (1):1–7. 10.1186/s12978-015-0036-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Antelman G, Fawzi MC, Kaaya S, Mbwambo J, Msamanga GI, et al. Predictors of HIV-1 serostatus disclosure: a prospective study among HIV-infected pregnant women in Dar es Salaam, Tanzania. AIDS (London, England). 2001. September 28; 15 (14):1865. 10.1097/00002030-200109280-00017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ethiopian Federal Ministry of Health. Tuberculosis, Leprosy, and TB/HIV Prevention and Control Program Manual. Addis Ababa, Ethiopia. 2008. [Google Scholar]
- 8.Geremew D, Tajebe F, Ambachew S, Endalamaw A, Eshetie S. Seroprevalence of HIV among pregnant women in Ethiopia: a systematic review and meta-analysis. BMC research notes. 2018. December; 11(1):1–7. 10.1186/s13104-017-3088-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kiula ES, Damian DJ, Msuya SE. Predictors of HIV serostatus disclosure to partners among HIV-positive pregnant women in Morogoro, Tanzania. BMC public health. 2013. December 1; 13 (1):433. 10.1186/1471-2458-13-433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alemayehu D, Tadesse S, Adefris M, Birhanu Z. HIV serostatus disclosure and associated factors among HIV positive pregnant women attending antenatal care services in northwest Ethiopia. International Journal of Infection Control. 2014; 10 (4):10–3396. 10.3396/IJICv10i4.028.14 [DOI] [Google Scholar]
- 11.Evangeli M, Wroe AL. HIV disclosure anxiety: A systematic review and theoretical synthesis. AIDS and Behavior. 2017. January 1; 21 (1): 1–1. 10.1007/s10461-016-1453-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lugalla J, Yoder S, Sigalla H, Madihi C. Social context of disclosing HIV test results in Tanzania. Culture, health & sexuality. 2012. November 1; 14 (sup1):S53–66. 10.1080/13691058.2011.615413 [DOI] [PubMed] [Google Scholar]
- 13.Naigino R, Makumbi F, Mukose A, Buregyeya E, Arinaitwe J, Musinguzi J, et al. HIV status disclosure and associated outcomes among pregnant women enrolled in antiretroviral therapy in Uganda: a mixed-methods study. Reproductive Health. 2017. December 1; 14 (1):107. 10.1186/s12978-017-0367-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization. Gender dimensions of HIV status disclosure to sexual partners: rates, barriers, and outcomes. https://scholar.google.com/scholar.
- 15.Poku RA, Owusu AY, Mullen PD, Markham C, McCurdy SA. Considerations for purposeful HIV status disclosure among women living with HIV in Ghana. AIDS Care. 2017. May 4; 29 (5):541–4. 10.1080/09540121.2016.1255711 [DOI] [PubMed] [Google Scholar]
- 16.Ngonzi J, Mugyenyi G, Kivunike M, Mugisha J, Salongo W, Masembe S, et al. Frequency of HIV status disclosure, associated factors and outcomes among HIV positive pregnant women at Mbarara Regional Referral Hospital, southwestern Uganda. The Pan African Medical Journal. 2019; 32. 10.11604/pamj.2019.32.200.12541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chan B, Tsai A. Trends in HIV-related stigma in the general population during the era of antiretroviral treatment expansion: An analysis of 31 Sub-Saharan African Countries. In Open Forum Infectious Diseases 2015. (Vol. 2, No. suppl_1, p. 404). Infectious Diseases Society of America. 10.1093/ofid/ofv133.280. [DOI] [Google Scholar]
- 18.Sowell RL, Seals BF, Phillips KD, Julious CH. Disclosure of HIV infection: how do women decide to tell? Health Education Research. 2003. February 1; 18 (1):32–44. 10.1093/her/18.1.32 [DOI] [PubMed] [Google Scholar]
- 19.Tam M, Amzel A, Phelps BR. Disclosure of HIV serostatus among pregnant and postpartum women in sub-Saharan Africa: a systematic review. AIDS Care. 2015. April 3; 27 (4):436–50. 10.1080/09540121.2014.997662 [DOI] [PubMed] [Google Scholar]
- 20.Malaju TM, Alene DJ. Women’s expectation of partner’s violence on HIV disclosure for prevention of mother to child transmission of HIV in North West Ethiopia. BMC Research Notes 2013, 6: 96. 10.1186/1756-0500-6-96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dehne KL, Dallabetta G, Wilson D, Garnett GP, Laga M, Benomar E, et al. HIV Prevention 2020: a framework for delivery and a call for action. The Lancet HIV. 2016. July 1; 3 (7):e323–32. http://www.unaids.org/en/resources/documents/2017/hiv-prevention-2020-road-map. 10.1016/S2352-3018(16)30035-2 [DOI] [PubMed] [Google Scholar]
- 22.Federal HIV/AIDS Prevention and Control Office 2018. HIV Prevention in Ethiopia National Road Map 2018–2020.
- 23.UNICEF: Prevention of Mother to Child Transmission (PMTCT) in Ethiopia. http://www.unicef.org/supply/index_428555.html/2016.
- 24.Ngemu EK, Khayeka-Wandabwa C, Kweka EJ, Choge JK, Anino E, Oyoo-Okoth E. Effectiveness of option B highly active antiretroviral therapy (HAART) prevention of mother-to-child transmission (PMTCT) in pregnant HIV women. BMC research notes. 2014. December; 7(1):1–7. http://bmcresnotes.biomedcentral.com/articles/10.1186/1756-0500-7-868. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 25.Medley A, Garcia-Moreno C, McGill S, Maman S. Rates, barriers and outcomes of HIV serostatus disclosure among women in developing countries: implications for prevention of mother-to-child transmission programs. Bulletin of the World Health Organization. 2004; 82:299–307. [PMC free article] [PubMed] [Google Scholar]
- 26.King R, Katuntu D, Lifshay J, Packel L, Batamwita R, Nakayiwa S, et al. Processes and outcomes of HIV serostatus disclosure to sexual partners among people living with HIV in Uganda. AIDS and Behavior. 2008. March 1; 12 (2):232–43. https://link.springer.com/article/10.1007/s10461-007-9307-7. 10.1007/s10461-007-9307-7 [DOI] [PubMed] [Google Scholar]
- 27.Knettel BA, Minja L, Chumba LN, Oshosen M, Cichowitz C, Mmbaga BT, et al. Serostatus disclosure among a cohort of HIV-infected pregnant women enrolled in HIV care in Moshi, Tanzania: a mixed-methods study. SSM-population health. 2019; 7: 100323. 10.1016/j.ssmph.2018.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sendo EG, Cherie A, Erku TA. Disclosure experience to partner and its effect on the intention to utilize prevention of mother to child transmission service among HIV positive pregnant women attending antenatal care in Addis Ababa, Ethiopia. BMC public health. 2013. December 1; 13 (1):765. http://www.biomedcentral.com/1471-2458/13/765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kassaye KD, Lingerh W, Dejene Y. Determinants and outcomes of disclosing HIV-seropositive status to sexual partners among women in Mettu and Gore towns, Illubabor Zone southwest Ethiopia. Ethiopian Journal of health development. 2005; 19 (2): 126–31. 10.4314/ejhd.v19i2.9981. [DOI] [Google Scholar]
- 30.Olagbuji BN, Ezeanochie MC, Agholor KN, Olagbuji YW, Ande AB, Okonofua FE. Spousal disclosure of HIV serostatus among women attending antenatal care in urban Nigeria. Journal of Obstetrics and Gynecology. 2011. August 1; 31 (6): 486–8. 10.3109/01443615.2011.563637 [DOI] [PubMed] [Google Scholar]
- 31.Meseret Y, Dulla D, Nega B. Prevalence and factors affecting disclosure of HIV status among pregnant women attending antenatal care in Addis Ababa public health centers: a cross-sectional survey. Obstet Gynecol Int J. 2019; 10 (4):317–24. [Google Scholar]
- 32.Gultie T, Genet M, Sebsibie G. Disclosure of HIV-positive status to a sexual partner and associated factors among ART users in Mekelle Hospital. HIV/AIDS (Auckland, NZ). 2015; 7: 209. 10.2147/HIV.S84341 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.