Abstract
Mobile mental health interventions have the potential to reduce barriers and increase engagement in psychotherapy. However, most current tools fail to meet evidence-based principles. In this paper, we describe data-driven design implications for translating evidence-based interventions into mobile apps. To develop these design implications, we analyzed data from a month-long field study of an app designed to support dialectical behavioral therapy, a psychotherapy that aims to teach concrete coping skills to help people better manage their mental health. We investigated whether particular skills are more or less effective in reducing distress or emotional intensity. We also characterized how an individual’s disorders, characteristics, and preferences may correlate with skill effectiveness, as well as how skill-level improvements correlate with study-wide changes in depressive symptoms. We then developed a model to predict skill effectiveness. Based on our findings, we present design implications that emphasize the importance of considering different environmental, emotional, and personal contexts. Finally, we discuss promising future opportunities for mobile apps to better support evidence-based psychotherapies, including using machine learning algorithms to develop personalized and context-aware skill recommendations.
Keywords: Mobile Health Interventions, Mental Health, Data Science, Dialectical Behavioral Therapy
1. INTRODUCTION
Mental health disorders are a leading cause of disability and death worldwide, with approximately 18% of US adults experiencing a mental illness in a given year [39]. Evidence-based psychotherapy is often effective for treating mental health conditions [56], as it can help people develop positive coping mechanisms to better manage their conditions. Unfortunately, people generally struggle to engage with psychotherapy, preventing them from managing their mental health disorders [40]. Increasing engagement with psychotherapy is therefore a top priority [4, 11, 12, 29, 30].
Technology-delivered mental health interventions have the potential to reduce barriers and increase engagement in psychotherapy, as they can reduce the financial and time burdens associated with attending in-person therapies [13] and increase comfort in providing honest disclosure [14, 15, 27]. Unfortunately, despite high interest in technology-delivered mental health interventions [47], commercially-available mental health apps often fall short of expectations; only 10% of apps aimed at supporting therapies for depression meet evidence-based principles [19], and many people view current digital psychotherapies as ineffective [44]. These challenges suggest a need for improved understanding of how to effectively translate evidence-based psychotherapies into technology-delivered interventions.
In this paper, we present data-driven design implications for such translations based on our examination of how people use Pocket Skills (Figure 1), a mobile web app designed to provide holistic support for Dialectical Behavioral Therapy (DBT). DBT is a skills-based therapy designed to support people with complex, difficult-to-treat disorders in developing concrete skills to help them solve problems, maintain positive relationships, and navigate negative events and emotions [24, 25]. Although research has shown that DBT can help people successfully manage a wide range of disorders [10, 26, 36], it has generally been difficult or impossible to quantitatively analyze the effectiveness of particular skills in real-world contexts. The translation of evidence-based interventions into mobile apps—and the collection of usage data within those apps—provides new opportunities to conduct such analyses, informing designs that help ensure people receive the best possible support. Similarly, comparing the effectiveness of different skills for different subgroups of people (e.g., those with particular disorders, demographics, or other characteristics) could reveal individuals that may need additional support.
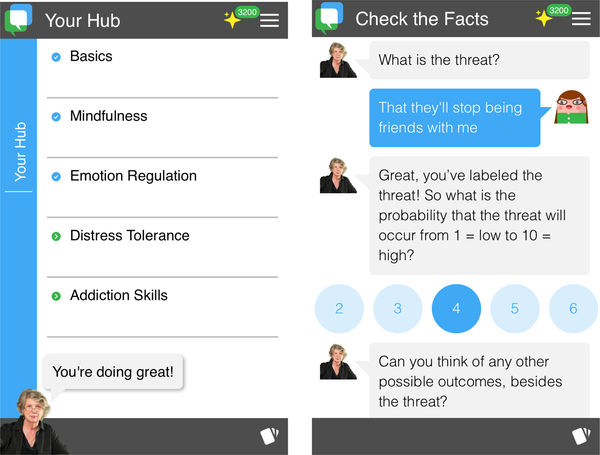
Figure 1:
Pocket Skills helps people learn and practice skills.
(a) Pocket Skills includes four modules, each focusing on different types of skills.
(b) Each skill walks people through DBT content via a conversational interface.
In this work, we therefore examined the effectiveness of individual DBT skills when translated into a mobile app, both overall and for different subgroups of people. The original month-long field study of Pocket Skills [51] collected: 1) survey data, including validated scales to assess progress, and 2) app usage data, including participant-reported skill effectiveness in terms of increasing mindfulness and reducing emotional distress. We analyzed this survey and usage data to investigate the following questions:
RQ1: When did study participants use the skills?
RQ2: Were particular skills more or less effective (e.g., in reducing emotional intensity and distress, in fostering mindfulness)?
RQ3: Were skills more or less effective for different subgroups of people (e.g., those with or without certain conditions)?
RQ4: Did skill-level effectiveness influence overall depression, anxiety, or skill use improvement throughout the study?
RQ5: Can we predict a particular skill’s effectiveness, given participant and skill characteristics?
We found that skills designed to help people regulate their emotions tended to be particularly helpful, while skills designed to help people manage distress were less effective (Section 4.1 and Section 4.2). We also found skill effectiveness differed among subgroups of people (Section 4.3), and that participants who reported higher skill effectiveness tended to report more improvement in depressive symptoms after the study (Section 4.4). We then developed a model to predict the effectiveness of specific skills (Section 4.5). Based on these findings, we developed data-driven design implications for translating evidence-based therapies into mobile applications (Section 5.1). Our design implications emphasize the importance of considering environmental contexts, emotional contexts, and personal contexts. Finally, we discuss important areas for future work, including opportunities for personalized and context-aware skill suggestions (Section 5.2).
2. BACKGROUND
In this section, we provide additional background on Dialectical Behavioral Therapy (DBT). We also describe prior work investigating the use of technology to monitor and predict mental health symptoms and to support positive coping skill use.
2.1. Dialectical Behavioral Therapy (DBT)
Dialectical Behavioral Therapy (DBT) was developed to treat complex behaviors associated with high emotional dysregulation [24]. DBT was originally designed as a treatment for borderline personality disorder (BPD) [26], but it has also been successfully applied to people with addictive behavior, eating disorders, and mood disorders [10]. The use of DBT skills as a whole has been shown to improve suicidal and self-injurious behavior, expressions of anger, and interpersonal problems [36].
DBT skills are traditionally separated into modules. Each module helps people learn specific types of skills. For example, the Mindfulness module contains skills dedicated to teaching people to accept the moment without judgment (e.g., by observing their breathing, by describing their thoughts). The Emotion Regulation module is designed to help people understand, manage, and adjust their emotional states. The Distress Tolerance module gives people specific healthy alternatives to unhealthy behaviors (e.g., instead of self-harming, people can take a cold shower or gently snap a rubber band on their wrist). By working through the modules and learning specific skills that can replace unhealthy behavior, people can start to apply those skills in their lives when they need them, helping them better navigate negative events and emotions as part of managing their mental illnesses [36].
2.2. Technological Support of Mental Health
Researchers have investigated technological support of mental health from a variety of perspectives. For example, research has investigated monitoring and predicting mental health symptoms through mobile phone sensors (e.g., [5, 57]) and social media posts (e.g., [2, 8, 9, 28, 58]). A large body of work has examined how machine learning techniques can support detection, diagnosis, and treatment of a myriad of mental health conditions (e.g., [52]). Researchers have also investigated personalizing mental health interventions (e.g., by recommending activities to manage stress [48] or prevent negative moods [18] based on an individual’s past sleep, diet, and activity data; by recommending interventions based on an individual’s personal characteristics and context [41]). Other work has examined evaluating counseling sessions through natural language processing and machine learning approaches to differentiate high-quality and low-quality counselors or counseling sessions (e.g, [1, 43, 54]). Similar to this prior work, we aim to quantitatively assess whether particular DBT skills may be particularly effective for different individuals.
Prior work has also examined how technology could support skills practice for a range of skill-based psychotherapies. For example, a suite of skills-based apps has been shown to reduce depression and anxiety [32]. The DBT Coach is designed to provide constantly-available, interactive walkthroughs of DBT skills [45, 46]. Similarly, the Virtual Hope Box includes analogous skills to the mindfulness and distress tolerance skills found in DBT, emphasizing support, comfort, distraction, and relaxation [7]. Participants in the Pocket Skills feasibility study reported improvements in depression, anxiety, and DBT skills use, describing increased engagement with DBT that helped them learn skills and ultimately apply them to their daily lives [51]. The concept of suggesting specific interventions when people need them, known as “just in time interventions” [34], has been pursued in other health contexts (e.g., promoting physical activity [17], stress management [20], and weight management [53]), with recent interest in applying them to positive coping skill use [21]. We build on this prior work and advance this opportunity by quantitatively determining which skills may be more or less effective, and whether skill effectiveness varies for different subgroups of people.
3. DATASET
To examine our research questions, we reanalyzed data from a previous field deployment of Pocket Skills [51]. These data required additional processing and have associated limitations.
3.1. Original Data Collection
The Pocket Skills deployment consisted of a 4-week field study [51]. 100 people were recruited; 27 dropped out over the course of the study, resulting in 73 total participants. The app included modules for Mindfulness, Emotion Regulation, Distress Tolerance, and Addiction Skills adapted from the DBT Skills Training Manual and Workbooks [25]. Each module contained module-specific skills presented via a conversational interface (see Figure 1). Some of these skills contained subskills, or different options for completing the skill (e.g., the Mindfulness skill of Observing included subskills for observing breathing, sounds, visuals, and everyday life).
Throughout the study, Schroeder et al. collected data on participant characteristics via surveys, including demographic information (e.g., gender, age); their anxiety, depression, and coping skill use (measured with the OASIS [38], PHQ-9 [23], and DBT Ways of Coping Checklist [37]); and other characteristics (e.g., what disorders they have been diagnosed with, whether they take medication, what modules they preferred). They also collected app usage data throughout the study, including app navigation and participant inputs for the skills. Many skills included Likert-scale ratings of how a participant felt before and/or after completing the skill, which we refer to in this paper as pre- and post-ratings. For example, Mindfulness skills often asked people to rate how mindful they felt after completing the skill; Emotion Regulation skills often asked people to rate their emotional intensity before and after completing the skill; and Distress Tolerance skills asked people to rate their level of distress before and/or after completing the skill.
3.2. Data Processing
To process the Pocket Skills study data, we first reviewed the app content to examine the skills themselves. We identified 11 skills that had pre- and post-ratings and 26 skills that had only post-ratings: 18 distinct Mindfulness skills (all with post-ratings only); 5 distinct Emotion Regulation skills (all with post- and pre-ratings); and 14 distinct Distress Tolerance skills (9 with post-ratings only and 5 with post- and pre-ratings). We excluded from our analyses any skill that did not include any Likert-scale ratings. No participant completed the Emotion Regulation skill Cope Ahead; all other skills were practiced at least once by at least one participant. No Addiction skills had Likert-scale ratings, so the module was excluded. Supplementary Table 1 shows our final list of modules, skills, and subskills. Four participants did not complete any of the included skills over the course of the study, and were therefore excluded from the dataset.
After we identified the skills to include, we extracted each distinct use of a specific skill from the usage log data and derived metadata (e.g., the ratings, the first use of a skill, the total order of practiced skills). Each interaction with the app (e.g., enter/exit skill screen, rate mindfulness) was logged with a local timestamp from each participant’s device, from which we derived temporal metadata (e.g., skill rating time of day, day of week). Because participants were able to access the app even after the study was completed, we filtered the data to only include skills practiced between the study intake (July 19th, 2017) and the last submitted exit survey (August 23rd, 2017). We then standardized the ratings: some had Likert-scales from 1–10, some from 1–5, and some binary (yes/no). Mindfulness scores were better if higher (i.e., a higher score indicated more mindfulness), but lower scores were better for all other modules (e.g., lower Distress Tolerance scores indicated lower distress). We therefore shifted everything to a 5-point scale, and reversed Mindfulness ratings so lower ratings were better (i.e., higher mindfulness). Finally, we computed the difference between pre- and post-ratings to characterize improvement before and after completing a skill, referred throughout the paper as skill improvement. Because lower numbers indicate better ratings, negative numbers indicate more improvement.
We grouped participants within categories for analysis based on their survey responses (see Table 1 for the categories and distributions). Categories included education; age; gender; intake survey scores on the PHQ-9 and OASIS; the number of family members living close (within a 50-mile radius); whether they were on any mental health related medication; and any mental health disorders they were diagnosed with. For age, close family, and education, we defined buckets to better balance the groups. Because participants had been diagnosed with a wide range of disorders, we grouped disorders by category based on the Diagnostic and Statistical Manual of Mental Disorders (DSM) [3]. Categories included neurodevelopmental disorders, mood disorders, anxiety disorders, personality disorders, eating disorders, and no diagnosed disorder. Each participant was then categorized as having or not having each disorder type, based on their reported disorders. Diagnosed disorders were all self-reported; the original study did not include clinical diagnostic interviews.
Table 1:
Participant categories. Many categories were biased towards particular subgroups, necessitating the bucketing.
| Gender | 62 female, 6 male, 1 Genderqueer/androgynous |
| Age | 18–63 (=37.3) |
| Age Buckets | <25 (12), 25–35 (17), 35–45 (21), >45 (19) |
| Education | High school (7), Some college (16), 2-year degree (5), 4-year degree (21), Professional degree (2), Master’s degree (14), Doctorate (4) |
| Education Buckets | <4 year degree (28), 4 year degree (21), >4 year degree (20) |
| Depression at Intake (Via PHQ-9) | Minimal or None (6), Mild (17), Moderate (18), Moderately Severe (16), Severe (12) |
| Anxiety at Intake (Via OASIS) | No anxiety disorder (12), Anxiety disorder (57) |
| On Related Medication | 12 no, 54 yes, 3 declined to answer |
| Types of Disorders | Mood (42), Anxiety (43), Personality (27), Neurodevelopmental (8), Eating (3) |
| Close Family Member Buckets | 0 (13), 1–2 (24), 3–4 (20), >4 (12) |
3.3. Limitations
Our dataset has a several associated limitations. First, we found evidence of incomplete data logging: one datapoint had a post-skill rating without a pre-skill rating, which should not have been possible given the app design. We excluded that data point, but its existence proves that our skill practice data is not complete. Second, we cannot say how many skills people practiced or applied in their daily lives without explicitly using the app. Participants reported that having the app reminded them to use skills in the moment, sometimes without the app; although the app included self-tracking of moods and behaviors, it did not allow users to log skills practiced outside of the app. Third, for many skills, participants may not have actually completed the skill at the time it was suggested. For example, some Distress Tolerance skills suggest activities such as taking a walk or a cold shower; the app did not support indication of whether or when participants actually completed those activities. Future tools designed to support DBT could include ways to report these aspects of DBT skill practice, which would allow further research and development of intelligent support for skill practice.
The study methods also introduced some biases. For ethical reasons, all participants were enrolled in therapy at the time of the study; we therefore cannot characterize what positive effects may be due to their therapy, rather than the app itself, beyond self-report by the participants. We also can only comment on the usefulness of the skills as they were translated in the app, which may be different than the usefulness of skills more traditionally taught and practiced. The majority of the study participants were female, possibly because women are more likely to be diagnosed with borderline personality disorder (BPD) (although prevalence is thought to be approximately equal [49]) and are more likely to seek therapy for BPD [16] and in general [55]. The role of gender on skill effectiveness should therefore be examined in future studies.
Finally, the clinical psychologists on the team ordered the modules based on traditional DBT practices, but that ordering may have encouraged more use of skills with only post-ratings. Additionally, at the beginning of the study, participants could not access the Emotion Regulation module until they had gone through the entire Mindfulness module. Based on participant feedback, all modules were unlocked after the second week; however, this initial limitation encouraged more use of Mindfulness skills, which lacked the pre-ratings needed to observe skill improvements. The Distress Tolerance: Self-Soothe skills were also added halfway through the study, limiting the amount of time participants were able to use them. Future studies investigating relative skill effectiveness should consider designs that collect pre- and post-ratings for every skill and should examine possible ordering effects.
4. METHODS AND RESULTS
In this section, we describe our methods and results from the statistical analyses and modeling we conducted to answer our research questions. This paper focuses on our quantitative analyses of skill usage and participant characteristics; a previous publication presents qualitative and quantitative descriptions of participant experiences while using Pocket Skills [51].
We address RQ1–RQ4 by examining the data along different individual dimensions through stratification and statistical tests. In Section 4.1 and Section 4.2, we describe overall skill use throughout the study, as well as skill effectiveness (e.g., how much participant emotional intensity or distress improved after using the skill, how mindful participants felt after using the skill) both in general and between different subgroups of participants. We examine how these participant and skill-level characteristics correlated with mental health improvements over the course of the study (i.e., improvements in anxiety, depression, and skill use) in Section 4.4. We used Python to clean and process the data and calculate group averages, then used R for our statistical analyses.
Finally, we address RQ5 by consolidating our findings and explorations in a machine-learning (ML) model that jointly uses the variables and leverages interactions between variables. In Section 4.5, we developed a model to predict skill improvement given participant and skill characteristics and to demonstrate the incremental value of additional information. We used scikit-learn, a Python machine learning package [42], to develop these models.
4.1. RQ1: Skill Use
We first examined overall skill use throughout the study.
4.1.1. Methods
To investigate overall skill use, we visualized the data and computed basic sums and averages.
4.1.2. Results
We found 1483 total skills practiced by 69 participants: 974 Mindfulness skills (all with post-only ratings); 127 Emotion
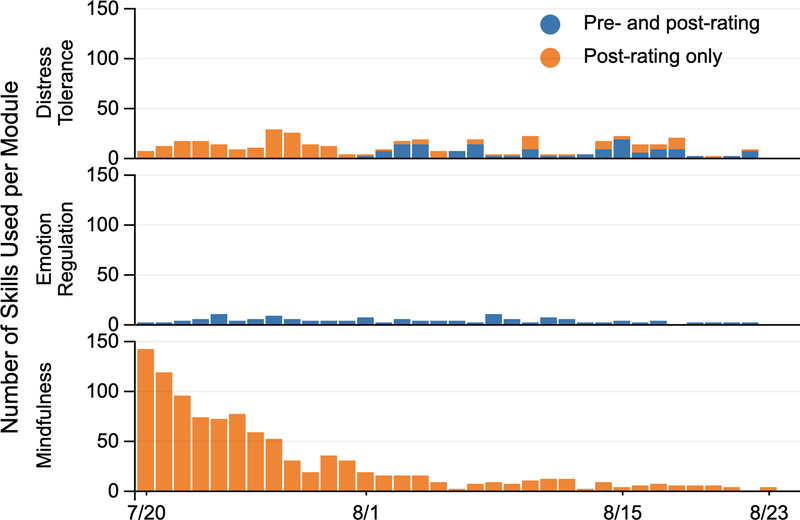
Regulation skills (all with pre- and post-ratings); and 382 Distress Tolerance skills (131 with pre- and post-ratings and 258 with post-ratings only). Mindfulness skills were most often used at the beginning of the study, with Emotion Regulation and Distress Tolerance skills more evenly distributed throughout (see Figure 2). Between July and August, Mindfulness skill use went from 78% of total usage to 37%, while Distress Tolerance went from 16% to 47%, perhaps because Distress Tolerance: Self-Soothe skills were added on August 1st. In the same time period, Emotion Regulation skill usage increased from 5% to 16%, perhaps because the Emotion Regulation module was universally unlocked (i.e., no longer depended on the completion of the Mindfulness module) on the same date. Usage patterns may also be partially due to an ordering effect (i.e., because the Mindfulness module was presented first in the app). Total usage of the skills dropped by more than half between July and August, indicating that skills were used less overall as the study progressed.
Figure 2:
Distribution of the total number of skills practiced over the course of the Pocket Skills feasibility study, showing skills with pre- and post-ratings and skills with only post-ratings.
Each participant completed an average of 21.5 skills throughout the study (min=1, max=93, stdev=20.57). On average, participants completed 14.1 Mindfulness skills (min=0, max=70, stdev=15.6), 1.84 Emotion Regulation skills (min=0, max=10, stdev=2.15), and 5.54 Distress Tolerance skills (min=0, max=42, stdev=7.00). Of the 69 participants, 51 practiced at least one skill more than once. Of the skills practiced with pre- and post-ratings, 213 (82.6%) had pre-ratings of ≥ 3 (i.e., indicated high levels of emotional intensity or distress before completing the skill).
4.2. RQ2: Overall Skill Effectiveness
We next compared overall skill effectiveness for the different modules and skills across all participants.
4.2.1. Methods
After standardizing skill ratings (see Section 3.2), our data included skills with only pre-ratings, skills with only post-ratings, and skills with both pre- and post-ratings. To investigate improvement trends, we examined skills with both pre- and post-ratings; similarly, to investigate post-rating trends, we examined skills with only post-ratings. For overall skill use, we examined skills at both the module and subskill granularities (see Supplementary Table 1). We used t-tests to analyze effectiveness by module: one to examine differences in skill improvement between the Emotion Regulation and Distress Tolerance skills (the only modules with skills that had pre- and post-ratings) and another to examine differences in post-ratings between Distress Tolerance and Mindfulness (the only modules with skills that had only post-ratings).
For our subskill-level analyses, we used one-way analysis of variance (ANOVA) tests to examine differences in 1) skill improvement and 2) post-ratings by subskill. When we found significant results, we then investigated pairwise differences, employing Tukey’s HSD procedure to correct for the increased risk of Type I error due to unplanned comparisons.
4.2.2. Results
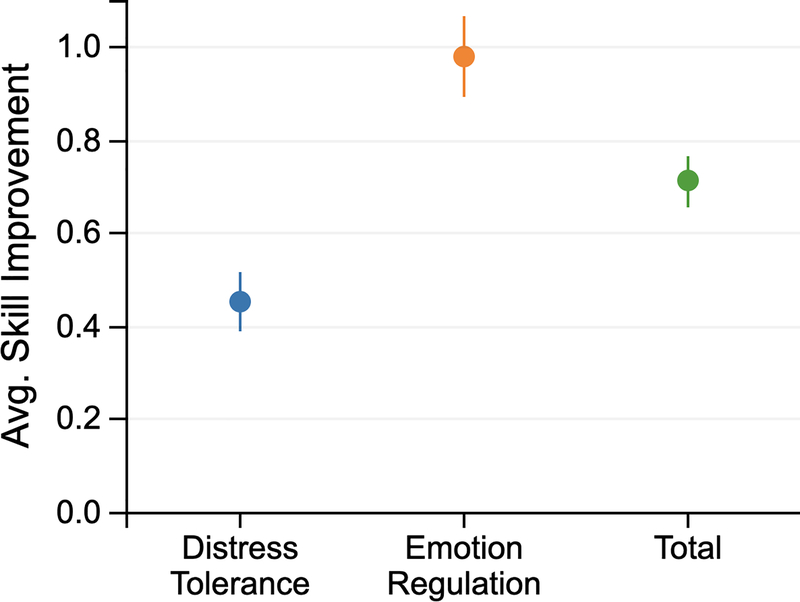
For skills with pre- and post-ratings, we found a significant effect of module on skill improvement (t(233.16) = 4.956, p<0.001). Emotion Regulation skills correlated with more than half a point more improvement on our 5-point scale (X̄=−0.98) than Distress Tolerance skills (X̄=−0.45). Figure 3 illustrates the overall average skill improvements across different modules. We also found a significant effect of the specific subskills (F(9, 248) = 3.901, p<0.001). Our Tukey HSD test accounting for unplanned comparisons revealed Emotion Regulation skills, particularly the Problem Solve skill, generally correlated with significantly greater improvement than Distress Tolerance skills of Self-Soothe (see Supplementary Section S.2).
Figure 3:
Average skill improvement on the 5-point scales of all skill uses (purple), Emotion Regulation skills (blue), and Distress Tolerance skills (red), with standard error bars. People improved more using Emotion Regulation skills than Distress Tolerance skills.
For skills with only post-ratings, we found no significant difference between modules. We did find a significant effect of the subskills (F(25, 1199) = 4.461, p<0.001). Our Tukey HSD test accounting for unplanned comparisons revealed 14 significant pairwise differences (see Supplementary Table 2). Generally, Mindfulness skills of Observing, Describing, and Participating correlated with better post-ratings than Mindfulness skills of Non-Judgementality. Distress Tolerance skills of Distracting also correlated with better post-ratings than Mindfulness skills of Non-Judgementality.
4.3. RQ3: Skill Effectiveness Across Subgroups
After examining overall skill effectiveness, we investigated whether different subgroups of people reported different skill effectiveness.
4.3.1. Methods
We first separated participants into the subgroups described in Section 3.2 and Table 1. We ran t-tests on categories with two groups (i.e., whether or not the participant completing the skill: took medications to manage their mental health; had anxiety disorder at the intake survey based on their OASIS results; had a mood, anxiety, eating, personality, neurodevelopmental, or no disorder diagnosed) to investigate differences between subgroups for each type of skill effectiveness (i.e., skill improvement, post-ratings). For each type of skill effectiveness, we then used the Benjamini-Hochberg procedure [6] on the t-test results to correct for multiple comparisons. Our results report these adjusted p-values.
For groups with three or more subgroups (i.e., initial PHQ-9 class; gender; close family, age, and education buckets), we ran one-way ANOVA tests to investigate subgroup differences in each type of skill effectiveness measure. When we found significant results, we again investigated pairwise differences using Tukey’s HSD procedure to account for unplanned comparisons.
4.3.2. Results
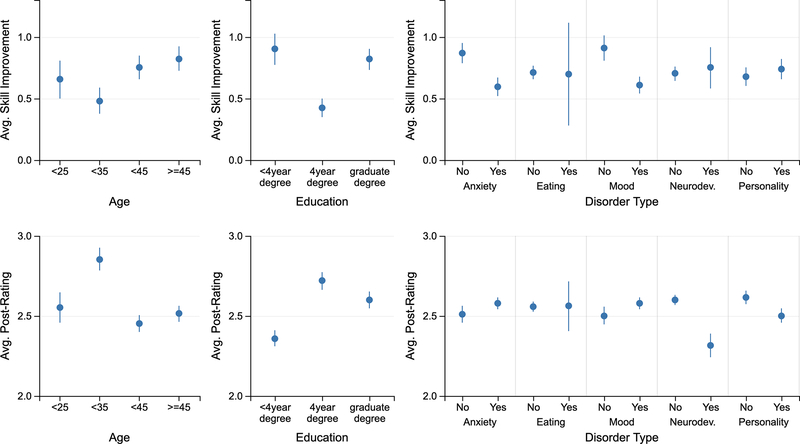
Figure 4 illustrates the differences in average skill improvements and post-ratings across various participant subgroups. For skill improvement, Education had a significant effect (F(2, 255)=7.068, p<0.01), with having <4 year degree correlating with 0.48 points more improvement than having a 4-year degree (t=3.404, p<0.01) and having a graduate degree correlating with 0.4 points more improvement than having a 4-year degree (t=−3.081, p<0.01). We found no significant differences in skill improvements between subgroups in any other categories.
Figure 4:
Average skill improvement (top) and post-ratings (bottom) across age subgroups (left), education subgroups (middle), and disorder types (right), with standard error bars. Higher improvement indicates more improvement (i.e., is better), while lower post-ratings indicate more positive ratings (i.e., is better). Some subgroups varied more, on average, than others. Section 4.3.2 discusses significant differences between subgroups.
For skill post-ratings, we found a significant difference depending on whether people had a personality disorder (t(1220.7)=2.533, p<0.05): people who had a personality disorder rated skills slightly more positively (X̄=2.40) than those who did not (X̄=2.56). We similarly found a significant effect of neurodevelopmental disorder (t(252.68)=2.580, p<0.05), with people who had a neurodevelopmental disorder rating skills slightly more positively (X̄=2.28) than those who did not (X̄=2.52). We also found a significant difference in post-rating given medication use (t(214.39)=3.1043, p<0.05), with people who took medication rating skills slightly more positively (X̄=2.43) than people who did not take medication (X̄=2.75). Education also significantly correlated with post-rating (F(2, 1222)=6.27, p<0.01), where a <4 year degree correlated with slightly better post-ratings than having a 4-year degree (by 0.28 points; t=3.384, p<0.01) or a graduate degree (by 0.20 points; t=2.561, p<0.05). Number of family members close also had a significant effect (F(3, 1221)=3.36, p<0.05), with having no family close correlating with less positive ratings than having 1–2 (by 0.38 points; t=−2.90, p<0.05) or 3–4 (by 0.42 points; t=−3.10, p<0.05). Finally, we found a significant effect of age (F(3, 1221)=4.19, p<0.01); being 25–35 years old correlated with more negative ratings than either being between 35–45 years old (by 0.34 points; t=−3.502, p<0.01) or being greater than 45 years old (by 0.25 points; t=−2.651, p<0.05). We found no significant differences in post-ratings between any other subgroups.
4.4. RQ4: Skill vs. Validated Scale Improvement
We next investigated whether participant and skill characteristics correlated with overall improvements in the clinically validated scales that participants in the feasibility study [51] completed for anxiety (OASIS [38]), depression (PHQ-9 [23]), and skill use (DBT Ways of Coping Checklist [37]) throughout the study.
4.4.1. Methods
We first calculated score differences between the intake and exit surveys for the PHQ-9, OASIS, and DBT Ways of Coping Checklist scales. We then extracted additional participant characteristics, including: their favorite and least favorite module; how much they felt Pocket Skills helped their goals and skill use; and whether they felt they practiced more skills with Pocket Skills than they would have practiced without it. We also examined participant skill use patterns, including total skills practiced in each module; whether they repeated any skills; their average, best, and worse skill improvement and post-rating; and the proportion of unique skills they practiced (i.e., an individual’s number of unique skills over the number of total skills practiced).
We performed mixed model analyses of variance for each scale, treating the characteristics described above as well as medication use and demographics (i.e., age, education, and close family member buckets) as fixed effects and the specific disorder types (i.e., whether they reported any disorders within each disorder category) as random effects to account for any heterogeneity within the overarching disorder types. We again investigated pairwise differences using Tukey’s HSD procedure to adjust for repeated testing.
4.4.2. Results
For depression improvement, we found significant main effects of age bucket (F(3, 9.3811)=4.5852, p<0.05); family bucket (F(3, 9.6203)=4.3922, p<0.05); education bucket (F(2, 9.5581)=5.0718, p<0.05); favorite module (F(3, 9.1457)=4.5373, p<0.05); best skill improvement (F(1, 9.3973)=5.3843, p<0.05); and best skill post-rating (F(1, 9.6632)=8.5388, p<0.05). Participants with larger best skill improvements and more positive best post-skill ratings tended to improve more on their PHQ-9 score. Pairwise analyses revealed that being 35 or younger generally correlated with more improvement than being older than 35, and that having zero family members close correlated with more improvement than having any number greater than zero. Having a <4 year degree correlated with more improvement than having a graduate degree (z=−3.161, p<0.01). Finally, people who preferred the Addiction Skills module improved more than those who preferred any other module. See Supplementary Section S.3 for Tukey test details.
For anxiety improvement, we found a significant main effect of age bucket, with participants who were older than 35 again improving less than those who were 25–35 (see Supplementary Section S.3). The skill use model yielded no significant results.
4.5. RQ5: Predictability of Skill Effectiveness
Finally, we examined the feasibility of predicting skill effectiveness for particular participants and skills. Given participant and skill use characteristics and each participant’s historical skill usage and rating data, we built four different machine learning classifiers to predict whether a specific skill would result in a skill improvement for that participant (i.e., lower emotional intensity or distress after skill use).
4.5.1. Methods
To predict whether using a skill would lead to a skill-level improvement for a participant, we used the subset of data (N=258) that included pre- and post-ratings to train binary classification models with positive prediction corresponding to skill improvement. We used participant and skill use characteristics as features, including contextual information (e.g., time of day, day of week, emotional intensity or distress rating prior to skill use); usage patterns (e.g., consecutive use of a skill within 15 minutes); historical skill improvement (e.g., cumulative average of skill improvements, skill improvement from the last skill use); and preferences (e.g., favorite module). All categorical features were one-hot encoded to transform each category into a binary representation necessary for model construction.
We trained binary classifiers using four different learning algorithms (i.e., decision tree, gradient boosting, random forest, logistic regression). We trained and evaluated each model using leave-one-participant-out cross validation. We used the average model accuracy and AUC on the hold-out participants as our metric to prevent overfitting and tune hyper-parameters of the learning algorithm (e.g., depth of the tree, max feature count, number of estimators, minimum samples for splitting nodes and leaf nodes, regularization strength, penalty). Because results from both test accuracy and test AUC were qualitatively similar, we report only test accuracy (see Supplementary Section S.4 for AUC results).
Finally, we performed a feature ablation study by training independent classifiers using all except one feature in order to understand the informativeness of each feature. We specifically focused on the set of features or variables that we found to have significant effect on the skill improvement in our statistical analyses (see Supplementary Section S.4).
4.5.2. Results
Given all features, the decision tree classifier yielded the best test accuracy (72.1%). All classifiers performed better than the base rate of the majority class (57.4%, or 148 out of 258 skill uses, were reported to have improved ratings). Our feature ablation study revealed that skill ID was the most impactful feature for the decision tree, gradient boosting, and logistic regression classifiers, leading to a drop of 17.1%, 13.4%, and 4.9% respectively in accuracy when removed. On the other hand, mood disorder was the most impactful feature for the random forest classifier, leading to a drop of 1.1% in accuracy when removed.
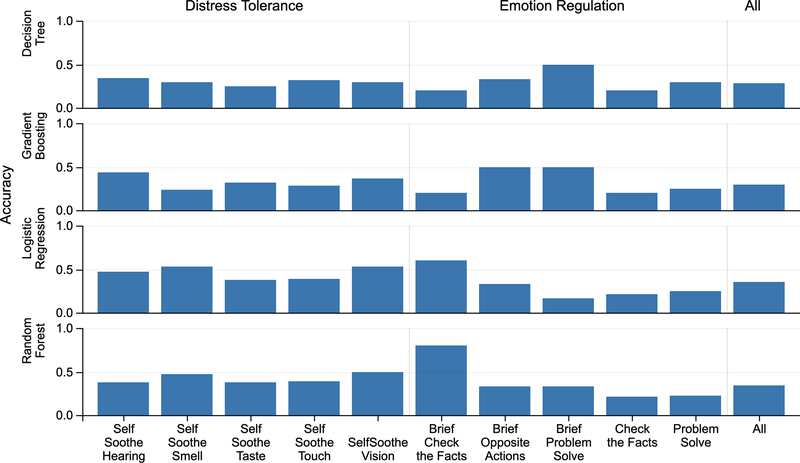
We further found that different classifiers perform better or worse on individual skills. For example, Figure 5 shows that the accuracy ranges from 20% for a random forest classifier to 80% for gradient boosting and decision tree classifiers for the Brief Check the Facts skill. Similarly, accuracy varied dramatically within specific classifiers for different skills. For example, for the logistic regression classifier, the accuracy for Distress Tolerance skills (54.2%) is lower than the accuracy for Emotion Regulation skills (68.8%).
Figure 5:
Accuracy of model prediction across individual skills, with accuracy of a single model across all skills displayed on the right. The varying accuracy of different models for different skills, together with an ablation study highlighting the importance of skill ID, reveals a need for skill-specific models that can account for different context relevant to each skill.
5. DISCUSSION
In this paper, we analyzed data from a month-long field study of Pocket Skills, a mobile web application designed to provide holistic support for dialectical behavioral therapy (DBT). Based on our findings, we present design implications for future translations of evidence-based therapies into mobile apps, including the importance of designing for environmental context, emotional context, and personal context. We also discuss the promise for future work in personalized and context-aware recommendations for skill-based mental health interventions. These design implications and opportunities can inform future designs for the increasingly-prevalent mobile app interventions aimed to help people better manage their mental health.
5.1. Data-Driven Design Implications
Our findings highlight a range of contextual information that can influence skill effectiveness for an individual using a mobile app to identify and implement a positive coping skill.
5.1.1. Designing for Environmental Context
Overall, we found that participants consistently reported specific skills to be more effective than others. In Section 4.2, we described how participants generally improved more using Emotion Regulation skills and less using Distress Tolerance: Self-Soothe skills. This difference may be due to the immediate feasibility of the activities suggested in the respective skills. Emotion Regulation skills generally walk people through considering and solving the problem they have, and can therefore be completed in most contexts. In contrast, the included Distress Tolerance: Self-Soothe skills suggest specific methods to distract people from distress that may be difficult to complete at certain times (e.g., eating something spicy, taking a cold shower). These activities are helpful when one has the ability to complete them, and are therefore useful in certain environmental contexts. However, they often cannot be immediately performed (e.g., when the person using the app is not at home). The post-ratings we collected therefore may not always reflect how people felt after completing the activity, as they may have been unable to do so when the post-ratings were solicited. Skills that suggest activities that may be infeasible in certain contexts should therefore be designed differently than those that can be done anywhere at anytime, perhaps by asking the person if they are able to immediately complete the skill and enabling them to explicitly schedule the skill for a future time if they cannot.
5.1.2. Designing for Emotional Context
In addition to enabling people to indicate later uses of a skill, apps designed to support skill-based interventions should recognize emotional circumstances in which it may be inappropriate to suggest skills that cannot be immediately completed. As we reported in Section 4.2, the majority of people using skills with pre- and post-ratings reported high distress or emotional intensity in the pre-rating of the skill: they were using the app in the moment, rather than practicing the skill so they could use it during future times of distress. Although all skills were directly adapted from the DBT Skills Training and Workbooks [51], Pocket Skills is a constantly-available resource and may therefore be used much differently than a traditional DBT skills worksheet. Instead of directly translating content, designers of tools to support skill-based interventions must consider how to best adapt skill-related materials to consider these different use cases. For example, a tool could differentiate between people practicing skills versus people who are currently in distress and attempting to use a skill in the moment. When a person indicates they are in distress, such a tool could focus on guiding them towards skills that are most likely to be feasible and useful in their current context. A tool could even sense emotional state (e.g., using sensing techniques such as those described in [22, 33]) and send push notifications during times of distress to directly suggest an appropriate skill. Such just-in-time interventions have been shown to support health behavior change (e.g., in promoting physical activity [17], in stress management [20], in weight management [53], in smoking cessation [35]). Our results both support emerging interest in applying such techniques to positive coping skill use (e.g., [21]) and differentiate the additional need to support skill development when people are not distressed. For example, a tool could then focus on supporting discovery of new skills, so people can continue to expand their positive coping skill “toolbox” and identify the practices that work best for them.
5.1.3. Designing for Personal Context
In addition to the trends we found in overall skill use, we also found that individual characteristics were often correlated with different levels of effectiveness, both in terms of individual skills and overall improvement throughout the study. As we discussed in Section 4.3, the type of disorder an individual had sometimes correlated with different levels of skill effectiveness, as did their education level, age, medication use, and the number of physically close family members. Section 4.4 revealed that many of those characteristics also correlated with differences in depressive symptom improvement throughout the study. Our investigations in Section 4.4 additionally revealed that people who had larger best improvements and post-ratings in individual skills tended to improve more in depressive symptoms, so helping people find skills that are effective for them could also help them improve their mental health overall.
Our preliminary results also indicate that individual preferences may influence effectiveness: as we detailed in Section 4.4, participants who preferred the Addiction Skills module reported higher improvements in depression after the study that those who preferred other modules. However, we cannot confirm whether practicing those skills leads to better skill-level improvements because the module did not include any Likert-scale ratings.
Given these differences between subgroups of people, future designs should account for individual characteristics and preferences in intervention activities. Future studies should also investigate how to better understand, acknowledge, and counteract any disparities or detrimental effects that could result from an individual’s characteristics and preferences.
5.2. Opportunities for Intelligent Support
Researchers have investigated how technology could use predictive models to identify and support people with mental health conditions (see Section 2.2). Machine learning has also been used to match stress relief interventions to particular individuals and contexts (e.g., [41, 48]). Mohr et al. recently examined a recommender system that identified skills an individual was particularly likely to use, finding that such recommendations resulted in improved depressive symptoms [31]. Preliminary evidence therefore suggests that incorporating such models into technology-delivered mental health interventions could better support people in engaging with psychotherapy.
People using Pocket Skills must currently discover which skills are most helpful to them on their own and must remember to use those skills during times of distress. However, our preliminary modeling results indicate promise for predicting whether a skill would yield improvement based on participant and skill use characteristics, indicating a potential to intelligently identify effective skills (see Section 4.5). Future studies with more participants, as well as skills designed to consistently include and elicit appropriate pre- and post-ratings, could generate data for more advanced modeling and prediction of skill effectiveness.
Predictive models would enable apps to generate skill recommendations, better supporting people in discovering and using effective skills. Our analyses suggested that some skills may be more effective than others, and our feature ablation study similarly revealed that the skill itself was consistently an important feature for predicting skill improvement. As we describe in Section 5.1.1, these differences in effectiveness may be due to the translation of the skill into app content rather than the skill itself. However, if certain skills do tend to be more effective than others, an app could suggest that people generally focus on those skills. Our results suggested that without such recommendations, people tend to go through the modules and skills in the order the app presents (see Section 4.1). Even with advanced predictive modeling techniques, people who are new to an app would lack necessary data for personalized recommendations. This common “cold-start problem” of recommender systems [50] can be alleviated through general recommendations based on someone’s demographics or other static features. Expert advice could also inform recommendations based on specific conditions and characteristics (e.g., by working with a psychologist to develop general recommendations). Such recommendations would enable even new users to discover skills that are more likely to help them in a given moment.
In this paper, we explored a one-size-fits-all predictive model, in which a single model is used to generate all predictions (see Section 4.5). We found that models trained on our current set of features can predict individual improvements more successfully (73.1%) compared to the base rate of the majority class (57.4%). In addition to demonstrating this potential for modeling approaches, we also revealed opportunities for future work to improve predictions. For example, we found that certain learning algorithms performed better at predicting skill improvements for different individual skills (see Figure 5). Future approaches could include an ensemble of models to further improve skill recommendations, leveraging: 1) different learning algorithms, to account for any differences in model performance for different skill or participant characteristics, and 2) different models, to account for any differences in data needs for individual skills (e.g., a model for Distress Tolerance: Self-Soothe skill could leverage location data).
Our modeling approach was also limited by a lack of richer contextual information. Given more complete data, a predictive model could allow personalized recommendations based on the contexts described above (e.g., in-the-moment environment and emotions, preferences and goals, personal characteristics). For example, during times of emotional distress, a recommender system could examine the individual’s preferences, current context, and historical app use to suggest skills that are most likely to result in improvements for that person. The same system could help people diversify their skill portfolio by recommending they practice new skills that were helpful to similar individuals. Recommendations could also depend on the individual’s environmental context, suggesting different skills when a person is at home, in transit, or on the bus. Such recommendations could further support people in identifying positive coping skills that work for them and implementing those skills in their lives when they need them.
6. CONCLUSION
Mobile mental health interventions are becoming increasingly ubiquitous, prompting a need for improved understanding to help designers more consistently base these interventions on evidence-based principles. We analyzed data from a month-long field study of Pocket Skills, a mobile web app designed to provide holistic support for dialectical behavioral therapy (DBT) to help people develop positive coping skills. We identified several factors that contribute to skill effectiveness, including the skill itself and participant characteristics and preferences. We also developed machine learning models to predict skill-based improvements. Based on our findings, we presented design implications for translating evidence-based psychotherapies into application content, including the need to consider different environmental, emotional, and personal contexts. Finally, we discussed opportunities to use machine learning techniques for better mental health support by producing personalized and context-aware skill recommendations based on an individual’s personal characteristics, preferences, past application use, and in-the-moment emotions and environmental factors.
Supplementary Material
ACKNOWLEDGMENTS
The authors would like to acknowledge Ran Gilad-Bachrach, Javier Hernandez, Daniel McDuff, and Kael Rowan for their advice on data analysis and their insights and feedback on this work as well as Microsoft Research for providing the data used in this research. Research was supported in part by the National Science Foundation under awards DGE-1256082, IIS-1553167, IIS-1813675, and IIS-1901386, the National Institutes of Health under awards R01LM012810 and P50MH115837, an Adobe Data Science Research Award, Supportiv, and the Allen Institute for Artificial Intelligence (AI2). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the National Science Foundation.
Footnotes
CCS CONCEPTS
• Human-Centered Computing → Human Computer Interaction.
ACM Reference Format:
Jessica Schroeder, Jina Suh, Chelsey Wilks, Mary Czerwinski, Sean A. Munson, James Fogarty, and Tim Althoff. 2020 (To Appear). Data-Driven Implications for Translating Evidence-Based Psychotherapies into Technology-Delivered Interventions. In Proceedings of PervasiveHealth 2020: 14th EAI International Conference on Pervasive Computing Technologies for Healthcare (PervasiveHealth 2020). ACM, New York, NY, USA, 14 pages.
Contributor Information
Jessica Schroeder, University of Washington.
Jina Suh, University of Washington, Microsoft Research.
Chelsey Wilks, Harvard University.
Mary Czerwinski, Microsoft Research.
Sean A. Munson, University of Washington
James Fogarty, University of Washington.
Tim Althoff, University of Washington.
REFERENCES
- [1].Althoff Tim, Clark Kevin, and Leskovec Jure. 2016. Large-Scale Analysis of Counseling Conversations: An Application of Natural Language Processing to Mental Health. Transactions of the Association for Computational Linguistics 4 (2016), 463–476. [PMC free article] [PubMed] [Google Scholar]
- [2].Andalibi Nazanin, Oxturk Pinar, and Forte Andrea. 2017. Sensitive Self-Disclosures, Responses, and Social Support On Instagram: The Case of #Depression. In Proceedings of the ACM Conference on Computer-Supported Cooperative Work and Social Computing. 10.1145/2998181.2998243 [DOI] [Google Scholar]
- [3].America Psychiatric Association. 1994. Diagnostic and Statistical Manual of Mental Disorders.
- [4].Bardram Jakob E, Frost Mads, Szántó Károly, Faurholt-Jepsen Maria, Vinberg Maj, and Kessing Lars Vedel. 2013. Designing Mobile Health Technology for Bipolar Disorder: A Field Trial of the Monarca System. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems. ACM, 2627–2636. 10.1145/2470654.2481364 [DOI] [Google Scholar]
- [5].Ben-Zeev Dror, Scherer Emily A, Wang Rui, Xiev Haiyi, and Campbell Andrew T. 2015. Next-Generation Psychiatric Assessment: Using Smartphone Sensors to Monitor Behavior and Mental Health. Psychiatric Rehabilitation Journal 38, 4 (2015), 313–313. 10.1037/prj0000130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Benjamini Yoav and Hochberg Yosef. 1995. Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal statistical society: series B (Methodological) 57, 1 (1995), 289–300. [Google Scholar]
- [7].Bush Nigel E, Dobscha Steven K, Crumpton Rosa, Denneson Lauren M, Hoffman Julia E, Crain Aysha, Cromer Risa, and Kinn Julie T. 2015. A Virtual Hope Box Smartphone App as an Accessory to Therapy: Proof-of-Concept in a Clinical Sample of Veterans. Suicide & Life-Threatening Behavior 45, 1 (2015), 1–9. 10.1111/sltb.12103 [DOI] [PubMed] [Google Scholar]
- [8].Munmun De Choudhury Emre Kiciman, Dredze Mark, Coppersmith Glen, and Kumar Mrinal. 2016. Discovering Shifts to Suicidal Ideation From Mental Health Content in Social Media. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems. 10.1145/2858036.2858207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Munmun De Choudhury Michael Gamon, Counts Scott, and Horvitz Eric. 2013. Predicting Depression Via Social Media. ICWSM 13 (2013), 1–10. [Google Scholar]
- [10].Dimeff Linda and Linehan Marsha M. 2001. Dialectical Behavior Therapy in a Nutshell. The California Psychologist 34, 3 (2001), 10–13. [Google Scholar]
- [11].Doherty Gavin, Coyle David, and Sharry John. 2012. Engagement With Online Mental Health Interventions: An Exploratory Clinical Study of a Treatment for Depression. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems. 10.1145/2207676.2208602 [DOI] [Google Scholar]
- [12].Stefan Rennick Egglestone Sarah Knowles, Toms Gill, Bee Penny, Lovell Karina, and Bower Peter. 2016. Health Technologies ‘In the Wild’: Experiences of Engagement With Computerised CBT. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems. 10.1145/2858036.2858128 [DOI] [Google Scholar]
- [13].National Institute for Clinical Excellence and Great Britain. 2002. Guidance on the Use of Computerised Cognitive Behavioural Therapy for Anxiety and Depression. National Institute for Clinical Excellence. [Google Scholar]
- [14].Gega Lina, Marks Isaac, and Mataix-Cols David. 2004. Computer-Aided CBT Self-help for Anxiety and Depressive Disorders: Experience of a London Clinic and Future Directions. Journal of Clinical Psychology 60, 2 (2004), 147–57. 10.1002/jclp.10241 [DOI] [PubMed] [Google Scholar]
- [15].Gilat Itzhak, Tobin Yishai, and Shahar Golan. 2011. Offering Support to Suicidal Individuals in An Online Support Group. Archives of Suicide Research : Official Journal of the International Academy for Suicide Research 15, 3 (2011), 195–206. 10.1080/13811118.2011.589675 [DOI] [PubMed] [Google Scholar]
- [16].Goodman Marianne, Patil Uday, Steffel Lauren, Avedon Jennifer, Sasso Scott, Triebwasser Joseph, and Stanley Barbara. 2010. Treatment Utilization By Gender in Patients With Borderline Personality Disorder. Journal of Psychiatric Practice 16, 3 (2010), 155–63. 10.1097/01.pra.0000375711.47337.27 [DOI] [PubMed] [Google Scholar]
- [17].Hardeman Wendy, Houghton Julie, Lane Kathleen, Jones Andy, and Naughton Felix. 2019. A Systematic Review of Just-In-Time Adaptive Interventions (JITAIs) to Promote Physical Activity. International Journal of Behavioral Nutrition and Physical Activity 16, 1 (2019), 31. 10.1186/s12966-019-0792-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Hollis Victoria, Konrad Artie, Springer Aaron, Antoun Matthew, Antoun Christopher, Martin Rob, and Whittaker Steve. 2017. What does all this data mean for my future mood? Actionable Analytics and Targeted Reflection for Emotional Well-Being. Human–Computer Interaction 32, 5–6 (2017), 208–267. 10.1080/07370024.2016.1277724 [DOI] [Google Scholar]
- [19].Huguet Anna, Rao Sanjay, Patrick J Mcgrath Lori Wozney, Wheaton Mike, Conrod Jill, and Rozario Sharlene. 2016. A Systematic Review of Cognitive Behavioral Therapy and Behavioral Activation Apps for Depression. PLOS One 11, 5 (2016), E0154248. 10.1371/journal.pone.0154248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Jaimes Luis G, Llofriu Martin, and Raij Andrew. 2015. Preventer, A Selection Mechanism for Just-In-Time Preventive Interventions. IEEE Transactions on Affective Computing 7, 3 (2015), 243–257. 10.1109/TAFFC.2015.2490062 [DOI] [Google Scholar]
- [21].Juarascio Adrienne S, Parker Megan N, Lagacey Madeline A, and Godfrey Kathryn M. 2018. Just-In-Time Adaptive Interventions: A novel Approach for Enhancing Skill Utilization and Acquisition in Cognitive Behavioral Therapy for Eating Disorders. International Journal of Eating Disorders 51, 8 (2018), 826–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Kanjo Eiman, Al-Husain Luluah, and Chamberlain Alan. 2015. Emotions in context: examining pervasive affective sensing systems, applications, and analyses. Personal and Ubiquitous Computing 19, 7 (2015), 1197–1212. [Google Scholar]
- [23].K Kroenke R Spitzer L, and Williams JB. 2001. The PHQ-9: Validity of a Brief Depression Severity Measure. Journal of General Internal Medicine 16, 9 (2001), 606–13. https://www.ncbi.nlm.nih.gov/pubmed/11556941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Linehan Marsha. 1993. Cognitive-Behavioral Treatment of Borderline Personality Disorder. Guilford Press. [Google Scholar]
- [25].Linehan Marsha. 2014. DBT Skills Training Manual. Guilford Publications. [Google Scholar]
- [26].Linehan MM,Heard HL, and Armstrong HE. 1993. Naturalistic Follow-Up of a Behavioral Treatment for Chronically Parasuicidal Borderline Patients. Archives of General Psychiatry 50, 12 (1993), 971–4. https://www.ncbi.nlm.nih.gov/pubmed/8250683 [DOI] [PubMed] [Google Scholar]
- [27].Lucas Gale M., Gratch Jonathan, King Aisha, and Morency Louis-Philippe. 2014. It’s Only A Computer: Virtual Humans Increase Willingness to Disclose. Computers in Human Behavior 37 (2014), 94–100. 10.1016/j.chb.2014.04.043 [DOI] [Google Scholar]
- [28].Manikonda Lydia and De Choudhury Munmun. 2017. Modeling and Understanding Visual Attributes of Mental Health Disclosures in Social Media. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems. 10.1145/3025453.3025932 [DOI] [Google Scholar]
- [29].Matthews Mark, Doherty Gavin, Coyle David, and Sharry John. 2008. Designing Mobile Applications to Support Mental Health Interventions. In Handbook of research on user interface design and evaluation for mobile technology. IGI Global, 635–656. 10.4018/978-1-59904-871-0.ch038 [DOI] [Google Scholar]
- [30].David C Mohr Michelle Nicole Burns, Stephen M Schueller Gregory Clarke, and Klinkman Michael. 2013. Behavioral Intervention Technologies: Evidence Review and Recommendations for Future ResearchÆŠMental Health. General Hospital Psychiatry 35, 4 (2013), 332–338. 10.1016/j.genhosppsych.2013.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Mohr David C, Schueller Stephen M, Tomasino Kathryn Noth, Kaiser Susan M, Alam Nameyeh, Karr Chris, Vergara Jessica L, Gray Elizabeth L, Kwasny Mary J, and Lattie Emily G. 2019. Comparison of the Effects of Coaching and Receipt of App Recommendations on Depression, Anxiety, and Engagement in the IntelliCare Platform: Factorial Randomized Controlled Trial. Journal of Medical Internet Research (JMIR) 21, 8 (2019), e13609. 10.2196/13609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].David C Mohr Kathryn Noth Tomasino, Lattie Emily G, Palac Hannah L, Kwasny Mary J, Weingardt Kenneth, Karr Chris J, Kaiser Susan M, Rossom Rebecca C, Bardsley Leland R, Caccamo Lauren, Stiles-Shields Colleen, and Schueller Stephen M. 2017. IntelliCare: An Eclectic, Skills-Based App Suite for The Treatment of Depression and Anxiety. Journal of Medical Internet Research 19, 1 (2017). https://dx.doi.org/10.2196%2Fjmir.6645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Morris Margaret E and Aguilera Adrian. 2012. Mobile, social, and wearable computing and the evolution of psychological practice. Professional Psychology: Research and Practice 43, 6 (2012), 622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Nahum-Shani Inbal, Smith Shawna N, Tewari Ambuj, Witkiewitz Katie, Collins Linda M, Spring Bonnie, and Murphy S. 2014. Just In Time Adaptive Interventions (JITAIs): An Organizing Framework for Ongoing Health Behavior Support. Methodology Center technical report 2014 (2014), 14–126. 10.1007/s12160-016-9830-8 [DOI] [Google Scholar]
- [35].Naughton Felix. 2017. Delivering âĂIJJust-In-TimeâĂİ smoking cessation support via mobile phones: current knowledge and future directions. Nicotine & Tobacco Research 19, 3 (2017), 379–383. 10.1093/ntr/ntw143 [DOI] [PubMed] [Google Scholar]
- [36].Neacsiu Andrada D, Rizvi Shireen L, and Linehan Marsha M. 2010. Dialectical Behavior Therapy Skills Use as a Mediator and Outcome of Treatment for Borderline Personality Disorder. Behaviour Research and Therapy 48, 9 (2010), 832–9. 10.1016/j.brat.2010.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Neacsiu Andrada D, Rizvi Shireen L, Vitaliano Peter P, Lynch Thomas R, and Linehan Marsha M. 2010. The Dialectical Behavior Therapy Ways of Coping Checklist: Development and Psychometric Properties. Journal of clinical psychology 66, 6 (2010), 563–582. 10.1002/jclp.20685 [DOI] [PubMed] [Google Scholar]
- [38].Norman Sonya B, Cissell Shadha Hami, Means-Christensen Adrienne J, and Stein Murray B. 2006. Development and Validation of an Overall Anxiety Severity and Impairment Scale (OASIS). Depression and Anxiety 23, 4 (2006), 245–9. https://www.ncbi.nlm.nih.gov/pubmed/16688739 [DOI] [PubMed] [Google Scholar]
- [39].National Institutes of Health: National Institute of Mental Health. 2015. Any Mental Illness (AMI) Among U.S. Adults https://www.nimh.nih.gov/health/statistics/prevalence/any-mental-illness-ami-among-us-adults.shtml
- [40].Olfson Mark, Mojtabai Ramin, Sampson Nancy A, Hwang Irving, Druss Benjamin, Wang Philip S, Wells Kenneth B, Pincus Harold Alan, and Kessler Ronald C. 2009. Dropout From Outpatient Mental Health Care in the United States. Psychiatric Services 60, 7 (2009), 898–907. 10.1176/ps.2009.60.7.898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Paredes Pablo, Ran Gilad-Bachrach Mary Czerwinski, Roseway Asta, Rowan Kael, and Hernandez Javier. 2014. PopTherapy: Coping with Stress Through Pop-culture. In Proceedings of the 8th International Conference on Pervasive Computing Technologies for Healthcare (Oldenburg, Germany) (PervasiveHealth ‘14). ICST (Institute for Computer Sciences, Social-Informatics and Telecommunications Engineering), ICST, Brussels, Belgium, Belgium, 109–117. 10.4108/icst.pervasivehealth.2014.255070 [DOI] [Google Scholar]
- [42].Pedregosa F, Varoquaux G, Gramfort A, Michel V, Thirion B, Grisel O, Blondel M, Prettenhofer P, Weiss R, Dubourg V, Vanderplas J, Passos A, Cournapeau D, Brucher M, Perrot M, and Duchesnay E. 2011. Scikit-learn: Machine Learning in Python. Journal of Machine Learning Research 12 (2011), 2825–2830. [Google Scholar]
- [43].Pérez-Rosas Verónica, Sun Xuetong, Li Christy, Wang Yuchen, Resnicow Kenneth, and Mihalcea Rada. 2018. Analyzing the Quality of Counseling Conversations: the Tell-Tale Signs of High-quality Counseling. In Proceedings of the Eleventh International Conference on Language Resources and Evaluation (LREC-2018). [Google Scholar]
- [44].Renn Brenna N, Hoeft Theresa J, Sophia Lee Heather, Bauer Amy M, and Areán Patricia A. 2019. Preference for in-person psychotherapy versus digital psychotherapy options for depression: survey of adults in the US. npj Digital Medicine 2, 1 (2019), 6. 10.1038/s41746-019-0077-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Rizvi Shireen L, Dimeff Linda A, Skutch Julie, Carroll David, and Linehan Marsha M. 2011. A Pilot Study of the DBT Coach: An Interactive Mobile Phone Application for Individuals With Borderline Personality Disorder and Substance Use Disorder. Behavior Therapy 42, 4 (2011), 589–600. 10.1016/j.beth.2011.01.003 [DOI] [PubMed] [Google Scholar]
- [46].Rizvi Shireen L, Hughes Christopher D, and Thomas Marget C. 2016. The DBT Coach Mobile Application as an Adjunct to Treatment for Suicidal and Self-Injuring Individuals With Borderline Personality Disorder: A Preliminary Evaluation and Challenges to Client Utilization. Psychological Services 13, 4 (2016), 380–388. 10.1037/ser0000100 [DOI] [PubMed] [Google Scholar]
- [47].Rubanovich Caryn Kseniya, Mohr David C, and Schueller Stephen M. 2017. Health App Use Among Individuals With Symptoms of Depression and Anxiety: A Survey Study With Thematic Coding. In JMIR Mental Health. 10.2196/mental.7603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Sano Akane, Johns Paul, and Czerwinski Mary. 2015. HealthAware: An Advice System for Stress, Sleep, Diet and Exercise. In 2015 International Conference on Affective Computing and Intelligent Interaction (ACII). IEEE, 546–552. 10.1109/ACII.2015.7344623 [DOI] [Google Scholar]
- [49].Sansone Randy A and Sansone Lori A. 2011. Gender Patterns in Borderline Personality Disorder. Innovations in Clinical Neuroscience 8, 5 (2011), 16–20. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3115767/ [PMC free article] [PubMed] [Google Scholar]
- [50].Schein Andrew I, Popescul Alexandrin, Ungar Lyle H, and Pennock David M. 2002. Methods and Metrics for Cold-Start Recommendations. In Proceedings of the International ACM SIGIR Conference on Research and Development in Information Retrieval. ACM, 253–260. 10.1145/564376.564421 [DOI] [Google Scholar]
- [51].Schroeder Jessica, Wilks Chelsey, Rowan Kael, Toledo Arturo, Paradiso Ann, Czerwinski Mary, Mark Gloria, and Linehan Marsha M.. 2018. Pocket Skills: A Conversational Mobile Web App To Support Dialectical Behavioral Therapy. In Proceedings of the ACM Conference on Human Factors in Computing Systems. 398. 10.1145/3173574.3173972 [DOI] [Google Scholar]
- [52].Shatte Adrian BR, Hutchinson Delyse M, and Teague Samantha J. 2019. Machine Learning in Mental Health: A Scoping Review of Methods and Applications. Psychological Medicine 49, 9 (2019), 1426–1448. 10.1017/S0033291719000151 [DOI] [PubMed] [Google Scholar]
- [53].Spruijt-Metz Donna, Wen Cheng KF, OâĂŹReilly Gillian, Li Ming, Lee Sangwon, Emken BA, Mitra Urbashi, Annavaram Murali, Ragusa Gisele, and Narayanan Shrikanth. 2015. Innovations in the use of interactive technology to support weight management. Current obesity reports 4, 4 (2015), 510–519. https://dx.doi.org/10.1007%2Fs13679-015-0183-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Tanana Michael, Hallgren Kevin A, Imel Zac E, Atkins David C, and Srikumar Vivek. 2016. A Comparison of Natural Language Processing Methods For Automated Coding Of Motivational Interviewing. Journal of Substance Abuse Treatment 65 (2016), 43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Vessey John T and Howard Kenneth I. 1993. Who Seeks Psychotherapy? Psychotherapy: Theory, Research, Practice, Training 30, 4 (1993), 546. 10.1037/0033-3204.30.4.546 [DOI] [Google Scholar]
- [56].Wampold Bruce E and Imel Zac E. 2015. The Great Psychotherapy Debate: The Evidence for What Makes Psychotherapy Work. Routledge. [Google Scholar]
- [57].Wang Rui, Campbell Andrew T, and Zhou Xia. 2015. Using Opportunistic Face Logging from Smartphone to Infer Mental Health: Challenges and Future Directions. In Adjunct Proceedings of the 2015 ACM International Joint Conference on Pervasive and Ubiquitous Computing and Proceedings of the 2015 ACM International Symposium on Wearable Computers. ACM, 683–692. 10.1145/2800835.2804391 [DOI] [Google Scholar]
- [58].Yates Andrew, Cohan Arman, and Goharian Nazli. 2017. Depression and Self-Harm Risk Assessment in Online Forums. Proceedings of the Conference on Empirical Methods in Natural Language Processing. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.