The mortality of mechanically ventilated patients with COVID-19 in German intensive care units (ICUs) during the first wave of the pandemic was reported to be 53%.1 Several treatment options for patients with COVID-19 have been established since then. Corticosteroid treatment has been established for severely ill patients2, 3, 4 and in light of the ongoing RECOVERY trial (NCT04381936), IL-6 blockade might have an advantage in patients with organ failure, including the prevention of progression to mechanical ventilation in those receiving non-invasive respiratory support. It is, thus, suggested that this, as part of a bundle of different measures, may have impacted on the ICU admission rate and outcome. We, therefore, have analysed the data from the federal German hospital payment institute (Institut für das Entgeltsystem im Krankenhaus [InEK]) at the time of discharge of patients with COVID-19 from all hospitals in Germany in 2020, including data from both the first and second waves of the pandemic.
During 2020, the proportion of hospitalised patients requiring ICU treatment steadily dropped from 30% during the period of our previous analysis1 (ie, discharge up to week 23) to 14% in December (weeks 49–52), corresponding to a relative drop in ICU admissions of more than 50%. Additionally, the percentage of those being mechanically ventilated while in the ICU also dropped, from 64% up to week 23, to 54% in weeks 49–52 (ie, from 19% of all hospitalised patients with COVID-19 to less than 8%). However, the absolute number of patients requiring mechanical ventilation in the ICU steadily increased during the second wave (figure 1 ) and almost doubled compared with that of the first wave.
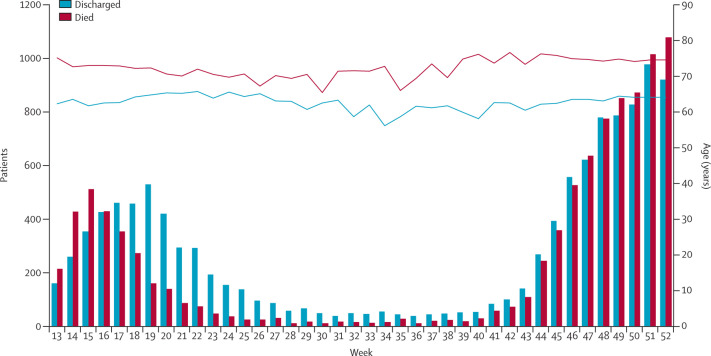
Figure 1.
Patients treated with mechanical ventilation (non-invasive and invasive) who were discharged from hospital or died
Lines show the corresponding mean age per week with COVID-19.
Mortality in patients being mechanically ventilated in the ICU remained unchanged at above 50% for the entire observational period (figure 1). We also found only minor changes in the mean age of survivors and non-survivors (figure 1). Although we cannot exclude that restrictions in ICU admission criteria might have occurred, resulting in these reduced ICU admission rates, the stable age distribution of ICU patients suggests that Germany did not experience a shortage of ICU capacity. This interpretation is supported by daily reports on nationwide ICU capacities, which allowed for optimal distribution of critically ill patients with COVID-19.
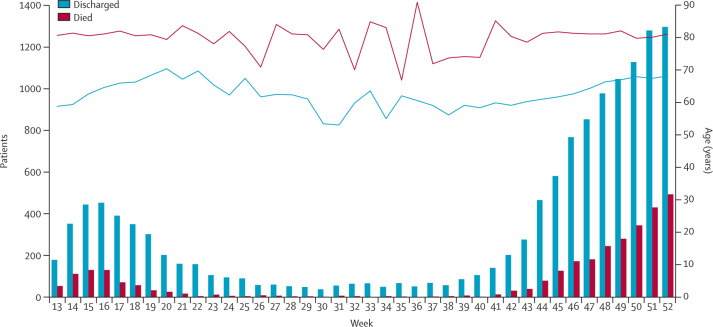
Finally, patients without mechanical ventilation requiring ICU treatment had a good prognosis, with a mortality rate of 10–38%, depending on the week of the second wave, almost similar to that of the first wave (figure 2 ).
Figure 2.
Patients treated in ICUs without mechanical ventilation who were discharged from hospital or died
Lines show the corresponding mean age per week with COVID-19 in the ICU. ICU=intensive care unit.
Overall, our analysis clearly suggests a dramatic improvement in the management of patients with COVID-19. Compared with in the first wave, 50% less of all hospitalised patients were admitted to the ICU during the second wave of the pandemic. By contrast, the analysis also clearly shows that the prognosis of ICU patients, those requiring mechanical ventilation and those not, remained unimproved. This finding advocates for the importance of optimal COVID-19 treatment before the necessity of ICU treatment, especially mechanical ventilation. Several potential explanations for the reduced incidence of mechanical ventilation on the ICU are plausible. First, changes in the use of high-flow oxygen treatment and non-invasive ventilation with more clearly defined algorithms being available when these treatment strategies need to be escalated to invasive mechanical ventilation.5 Second, the establishment of pharmacological treatments, with the greatest treatment success most likely to be achieved by the early administration of dexamethasone in patients with severe COVID-19.2 One limitation of these data is that there was no information on comorbidities. In conclusion, given that approximately 5700 patients with COVID-19 were in German ICUs at the end of December 2020, the profound decrease in ICU admissions was a key factor in avoiding unmanageable ICU shortages.
For ICU capacities in Germany see www.intensivregister.de
Acknowledgments
CK reports personal fees from Maquet, Xenios, and Bayer; non-financial support from Speaker of the German register of ICUs; and grants from the German Ministry of Research and Education, during the conduct of the study. WW reports grants from Weinmann, Vivisol, Löwenstein Medical, VitalAire, and Philips/Respironics, during the conduct of the study; and personal fees from companies dealing with mechanical ventilation, outside of the submitted work. RB reports grants from Berlin University Alliance; and being a member of the COVID-19 Hospital Exoneration Committee for the German Federal Ministry of Health, during the conduct of the study. TW reports grants from the German Ministry of Research and Education, during the conduct of the study. DFM reports personal fees from consultancy for GlaxoSmithKline, Boehringer Ingelheim, Bayer, Novartis, and Eli Lilly, and from sitting on a data safety monitoring board for a trial undertaken by Vir Biotechnology, outside of the submitted work. DFM's institution has received funds from grants from the UK National Institute for Health Research (NIHR), Wellcome Trust, Innovate UK. DFM is one of four named inventors on a patent (US8962032) covering the use of sialic acid-bearing nanoparticles as anti-inflammatory agents issued to his institution, The Queen's University of Belfast, which has no direct effect on the contents of the manuscript. DFM is a director of research for the Intensive Care Society and NIHR Efficacy and Mechanism Evaluation programme director.
References
- 1.Karagiannidis C, Mostert C, Hentschker C, et al. Case characteristics, resource use, and outcomes of 10 021 patients with COVID-19 admitted to 920 German hospitals: an observational study. Lancet Respir Med. 2020;8:853–862. doi: 10.1016/S2213-2600(20)30316-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Group RC, Horby P, Lim WS, et al. Dexamethasone in hospitalized patients with COVID-19—preliminary report. N Engl J Med. 2020 doi: 10.1056/NEJMoa2021436. published online July 17. [DOI] [Google Scholar]
- 3.Sterne JAC, Murthy S, Diaz JV, et al. Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: a meta-analysis. JAMA. 2020;324:1330–1341. doi: 10.1001/jama.2020.17023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Angus DC, Derde L, Al-Beidh F, et al. Effect of hydrocortisone on mortality and organ support in patients with severe COVID-19: the REMAP-CAP COVID-19 corticosteroid domain randomized clinical trial. JAMA. 2020;324:1317–1329. doi: 10.1001/jama.2020.17022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kluge S, Janssens U, Spinner CD, Pfeifer M, Marx G, Karagiannidis CM. Recommendations on inpatient treatment of patients with COVID-19. Dtsch Arztebl Int (in press). [DOI] [PMC free article] [PubMed]