Abstract
Background
Vaccination is crucial to limit the pandemic spread of SARS-CoV-2/COVID-19. Therefore, besides the development and supply of vaccines, it is essential that sufficient individuals are willing to get vaccinated, but concerning proportions of populations worldwide show vaccine hesitancy. This makes it important to determine factors that are associated with vaccine acceptance.
Methods
1779 adults of a non-probability convenience sample in Germany were assessed with an online survey in a cross-sectional survey period from 1st to 11th January 2021 (a few days after the beginning of vaccinations in Germany).
Results
64.5% of the sample stated that they absolutely would accept the vaccination, 13.8% would rather accept it, 10.4% were undecided, and 5.2% would rather not and 6.0% absolutely not get vaccinated. COVID-19-related anxiety, and fears of infection and health-related consequences correlated significantly positively with vaccine acceptance (all p < .001). In contrast, social (p = .006) and economic fears (p < .001) showed significant negative associations with vaccination willingness. The broader constructs of unspecific anxiety and depressive symptoms were not significantly associated with vaccine acceptance. Vaccine acceptance differed between users/non-users of social media and official websites to gain information about the pandemic (p < .001).
Conclusions
COVID-19-related anxiety and health-related fears were associated with higher vaccine acceptance, whereas the fear of social and economic consequences showed the contrary direction. These findings highlight the need to differentiate between several types of fears and anxiety to predict their influence on vaccine acceptance, and provide important information and an essential base for future studies and interventions.
Keywords: Vaccination, Vaccine acceptance, Corona, SARS-CoV-2, Pandemic
1. Introduction
Besides preventive protective measures and therapeutic approaches [1], vaccination is the key to limit the pandemic spread of SARS-CoV-2/COVID-19 [2], [3], [4], [5]. The development of vaccines against COVID-19 made rapid progress in the last year and to date, three different vaccines showed good efficacy against COVID-19 [6], [7]. In addition to the development and provision of vaccines, a central aspect is the willingness of the population to get vaccinated [5], [8]. Already before the pandemic, vaccine hesitancy was named as one of the top ten threats to global health in 2019 by the World Health Organization [9], and this issue grew further in light of the COVID-19 pandemic. While the development of a vaccine against COVID-19 was eagerly awaited by the majority of the communities at the beginning of the pandemic, skeptical voices are now becoming louder and rising evidence shows mixed patterns with a worldwide rather decreasing trend of acceptance [2], [5], [8], [10]. Therefore, identifying predictive factors for vaccination willingness is crucial to derive interventions to enhance the acceptance.
Several studies indicated the importance of sociodemographic factors (e.g., a lower vaccine acceptance in female and younger individuals) with regard to the acceptance of COVID-19 vaccine [2], [8], [11], [12], as well as for vaccines for other diseases in the past [13], [14]. Mistrust in research and the vaccines (e.g., with regard to the rapid development, negative side effects, and other adverse events) was a commonly reported reason for vaccine hesitancy [9], [15]. The lack of confidence in research was furthermore might related to the sometimes contradictory and rapidly evolving and changing research situation at the beginning of the pandemic [16]. In this context, media communication, particularly social media, seems to play an important role: In several studies, social media was associated with fears in context of the COVID-19 pandemic [17] and also with vaccine hesitancy and related conspiracy theories [18], [19]. Whereas previous research focuses on social media, the role of official media reporting (e.g., websites of the government and health authorities) with regard to vaccine acceptance was sparsely analyzed.
The subjective levels of anxiety, fear, and individual risk seem to be important predictors of vaccine acceptance in first studies: Individuals with higher risk perception and more anxiety showed significantly higher vaccine acceptance in Turkey, UK [2], and France [11]. Anxiety further was discussed as a functional fear which predicts public health compliance [20]. However, there were inconsistencies about this, highlighting the need to assess the role of fears and anxiety in detail. Therefore, we wanted to detangle different types of fears and anxiety with regard to vaccine acceptance.
Furthermore, most studies on vaccine acceptance took part before the actual availability of vaccines but this lack needs to be closed because there can be (in congruency with intention-behavior-models) expected a gap between the prospectively hypothetically reported willingness for a behavior (e.g., vaccination) and the attitude in the context of an actually possible vaccination [21]. This study aims to fill this gap with regard to vaccine acceptance in the general population and its relation to fears, media usage, and socio-demographic factors shortly after the beginning of vaccinations in Germany. This should provide a basis for subsequent longitudinal studies of vaccine acceptance as well as randomized-controlled trials with a focus on modifiable factors of the acceptance.
2. Methods
2.1. Design
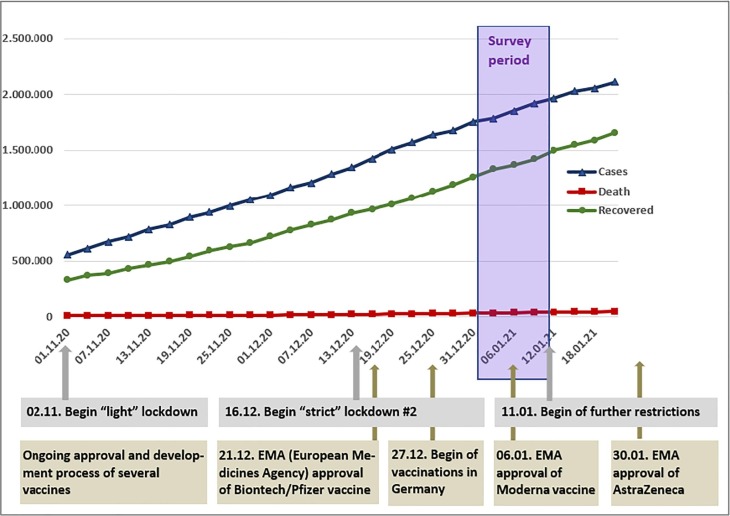
We analyzed cross-sectional data of one survey period from 1st to 11th January 2021 as part of a longitudinal online survey of a non-probability sample of the adult general population in Germany with to date seven data collection waves [22]. The assessment period (of this 7th assessment) took part a few days after the beginning of vaccinations in Germany (see Fig. 1 ).
Fig. 1.
The situation regarding COVID-19 (cases, deaths, recovered), political measures, and the progress of vaccines in Germany in temporal proximity with the survey period [7].
The study was approved by the ethics committee of the Charité – Universitätsmedizin Berlin (EA1/071/20) and registered at clinicaltrials.gov (NCT04331106). Recruitment of the convenience sample was primarily done via social media platforms (Twitter, Facebook, Instagram), news portals, the homepage of the Charité – Universitätsmedizin Berlin, and the kbo-Inn-Salzach-Klinikum. Participants who gave their email-addresses and consent at a prior assessment wave were contacted for the subsequent periods via e-mail. 1779 (37.8%) of the 4704 contacted individuals participated in this 7th assessment period.
The survey was carried out online via SoSci-Survey and, on average, 12 min (SD = 5 min; range: 5–36 min) were required to complete the survey. No incentives were given to the participants. Mandatory for participation were the minimum age of 18 years, the ability to complete the survey in German language, and the current place of residency in Germany.
2.2. Assessment
Vaccination willingness was assessed by the item (“If you were offered the COVID-19-vaccination now, would you accept it?”) on a five-point Likert scale from −2 (“absolutely not”) to + 2 (“absolutely”).
COVID-19-related anxiety was recorded with the COVID-19-Anxiety Questionnaire (C-19-A) [23]. The C-19-A is a modification of the validated DSM-5 Severity Measure for Specific-Phobia Adult Scale that comprises 10 items that assess the appearance of phobic anxiety symptoms related to the COVID-19 pandemic. The items are rated on a 5-point Likert scale ranging from 0 (“never”) to 4 (“all the time”) and sum up to the scale score (0 – 40). The score classifies the severity of the specific anxiety symptoms in none (0–4) mild (5–14), moderate (15–24), severe (25–34), and extreme (35–40). The Patient Health Questionnaire-4 (PHQ-4) was used to assess depressive and “unspecific” anxiety symptoms (“unspecific” in this context means that the anxiety is not specific regarding the COVID-19 pandemic) [24]. The PHQ-4 is an ultra-brief screening instrument that includes two items that examine core criteria of depressive disorders/symptomatology (subscale: PHQ-2) and two items indicating key criteria for generalized anxiety disorder (subscale: GAD-2) that are validated as well for other anxiety disorders and unspecific anxiety symptoms in general. The intensity of each item was evaluated on a 4-point scale from 0 (“not at all”) to 3 (“nearly every day”) and sum up to the subscale scores (0–6) and the total PHQ-4 score (0–12). Higher values represent higher symptom burden and a score of 3 on the subscales, respectively 6 on the total score represents the cutoff for severe symptoms. Furthermore, different aspects of fears with regard to the COVID-19 pandemic were obtained with six separate items on 6-point Likert scales from 1 (“not true at all”) to 6 (“totally true”); higher scores indicated stronger fear [22], [25]. Additionally, the subjective risk perception was assessed with one item (“how likely will you become infected with COVID-19 within the next month?” from 0 to 100%) [25].
With regard to the media exposure was ascertained which media formats the participants used as primary source to obtain information about the pandemic. The selection of multiple formats was possible. In the analysis we focused on the both most divergent types of media: social media (as a rather emotionally loaded and unfiltered source of information) and official websites of the government and health authorities (probably providing the comparatively highest amount of reliable information) [17].
2.3. Data analysis
IBM SPSS Statistics Version 26 was used for analyses. Due to ordinal-scaled and non-normal distributed data, we used non-parametric Spearman rank correlations and Kruskal-Wallis-tests. We controlled for age and educational level as covariates in the correlative analyses because those variables showed (in accordance with previous studies) statistically significant correlations with vaccine acceptance in our sample. The significance-level was set to 0.05 (two-tailed) and Bonferroni Holm method was used to counteract the problem of multiple testing.
3. Results
3.1. Sample characteristics
The sample (N = 1779) included 1380 women, 389 men, and 10 diverse individuals. Mean age was 41.33 years (SD = 12.62; Range 18–84). 14.7% reported an intermediate or lower secondary school degree, 25.2% a higher education entrance qualification, and 59.8% a university degree. For cross tabulations of gender, age, and education see Table S1a, S1b, and S1c in the supplement.
3.2. Vaccine acceptance, sociodemographic characteristics, and media usage
64.5% (N = 1146) stated that they absolutely would accept the vaccination, 13.8% (N = 246) would rather accept it, 10.4% (N = 185) were undecided, and 5.2% (N = 93) would rather not or absolutely not 6.0% (N = 107) get vaccinated.
Males reported on average higher willingness than females, but gender differences were not significant (χ2(2) = 4.261, p = .119). Age (rS(1777) = 0.70, p = .003**) and educational level (rS(1777 = 0.117, p < .001***) showed significant positive correlations with vaccination acceptance (see Table S1a, S1b, and S1c in the supplement for the means by gender, age, and educational level).
The usage of social media and/or official websites to gain information about the pandemic was significantly associated with the levels of vaccine acceptance (χ2(3) = 28.783, p < .001***). The group of individuals which reported to use neither official websites nor social media reported the lowest acceptance level (M = 0.96, SD = 1.37, N = 297), followed by individuals that used only social media (M = 1.16, SD = 1.32, N = 116). Participants that only reported the usage of official websites were on average more willing to get vaccinated (M = 1.33, SD = 1.12, N = 827) and those who used both formats had the highest acceptance scores (M = 1.38, SD = 1.13, N = 490).
3.3. Vaccine acceptance, fears, anxiety, and stress-related variables
Table 1 shows the rank correlations of vaccine acceptance with COVID-19-related anxiety, distinct fears, unspecific anxiety, depressive symptoms, and the subjective risk perception. COVID-19-related anxiety and fears of infection and health-related consequences correlated significantly positively with the vaccine acceptance. In contrast, social and economic fears were significantly negatively associated with the willingness to get vaccinated. The broader constructs (unspecific anxiety and depressive symptoms) showed no significant association with vaccine acceptance, and the correlation with the subjective risk perception did not reach statistically significance after correction for multiple testing with Bonferroni-Holm correction.
Table 1.
Associations of anxiety and fear with vaccination willingness (partial Spearman rank correlation coefficients rS with partialization of age and educational level; N = 1730).
| Vaccination willingness | ||
|---|---|---|
| Anxiety and stress-related variables | Correlation coefficient rS (p) | 95% confidence interval of rS |
| C-19-A (COVID-19-related anxiety) | 0.156 (<0.001***) | [0.110; 0.201] |
| PHQ-4 (unspecific anxiety and depressive symptoms) | 0.030 (0.208) | [−0.017; 0.077] |
| GAD-2 (unspecific anxiety symptoms) | 0.031 (0.198) | [−0.016; 0.078] |
| PHQ-2 (depressive symptoms) | 0.024 (0.320) | [−0.023; 0.071] |
| Several aspects of fear regarding the COVID-19 pandemic | ||
| Fear of the consequences of the pandemic in general | 0.009 (0.715) | [−0.038; 0.056] |
| Fear of infection with COVID-19 | 0.238 (<0.001***) | [0.194; 0.281] |
| Fear of the health-related consequences for oneself | 0.178 (<0.001***) | [0.132; 0.223] |
| Fear of the health-related consequences for loved ones | 0.166 (<0.001***) | [0.120; 0.211] |
| Fear of the social consequences of the pandemic | −0.066 (0.006*) | [−0.112; −0.019] |
| Fear of the economic consequences of the pandemic | −0.098 (<0.001***) | [−0.144; −0.052] |
| Risk perception | ||
| Subjective risk perception to get infected | 0.055 (0.023) | [0.008; 0.101] |
Note. Significance levels: *** p < 0.001, ** p < 0.01, * p < 0.05. Significance levels relate to Bonferroni-Holm corrected p-values; in the table the uncorrected original p-values are displayed.
4. Discussion
4.1. Summary and interpretation of the results
The vaccination acceptance in our sample was relatively high and comparable with results from UK [8] and France [11]. Compared to findings from the US [26], the acceptance was higher in our sample, but lower than in a survey from China [27]. Congruent with other countries [2], [8], [11], [12], age and educational level correlated positively with acceptance. In contrast to those previous studies [2], [8], no significant effect was found for gender and risk perception. When comparing vaccination acceptance and its associations with sociodemographic factors it is relevant to consider that the different studies used different sample designs and compositions (e.g., regarding gender, age, and educational level) and a comparison is therefore only possible to a limited extent.
As an extension to previous studies [18], [19], we analyzed in our study not only the association of vaccine acceptance with the consumption of social media but also with the usage of official websites to gain information about the pandemic. In comparison to the usage of none of those information sources, the exploitation of social media was associated with a slightly higher vaccine acceptance. In addition, using official websites seemed to have a supportive effect. These results are in contrast to previous findings [18], [19] and may give a hint that the role of social media is more complex and not always maladaptive with regard to vaccine acceptance. Future studies need to further detangle the role of different social and other media formats and interconnect those analyses with different fears in context of the COVID-19 pandemic.
It is remarkable that COVID-19-related anxiety and health-related fears were associated with a higher willingness, whereas the fear of social and economic consequences showed the contrary direction. It seems plausible that fears that are directly related to the physical health of oneself or loved ones are associated with a higher acceptance of a vaccination that promises to reduce the probability of those negative outcomes. This partially supports the discussion of anxiety as a functional fear which predicts public health compliance [20]. In contrast, social and economic fears seem to be dysfunctional fears with regard to the adherence to public health measurements in the pandemic context. A lack of adaptive internal coping and external measures to buffer negative social and economic consequences and frustration towards the government (which is in turn associated with less vaccine acceptance [9], [15]) might be factors that partially explain those findings. Future studies need to clarify those potential explanations empirically.
The broader constructs of unspecific anxiety and depressive symptoms seem to be neglectable with regard to vaccine acceptance. In summary, these findings highlight the need to differentiate between types of fears and anxiety to predict their influence on vaccine acceptance.
Furthermore, it is essential not to misunderstand the positive correlation of vaccine acceptance with COVID-19 related anxiety and health-related fears with the interpretation that it would be helpful to enhance those fears in the general population to promote a further increase in the vaccine acceptance. An overly pronounced fear respectively an emotionally loaded attitude towards the pandemic is, in contrast, a risk factor for severe mental health issues due to the pandemic and may leads chronically to an inability to correctly and adaptively engage in preventive measures [28], [29]. Therefore, our results rather enlighten the need to improve risk communication strategies and to promote a better preventive and therapeutic coping with several fears in the context of the pandemic.
To reduce vaccine hesitancy, it seems to be important to give credible and reliable information about the safety of vaccines and to eradicate misinformation [26]. Concerns should always be taken seriously and addressed with appropriate measures. Information should be transported on different levels: e.g., from personal conversations with professionals in the medical context (e.g., physicians) up to information via several media formats on institutional level – ideally communicated by trusted individuals/institutions [26], [30]. Our data suggest that, for example, social media may be used for this purpose in addition to official websites (ideally if appropriate conditions are given to stop rumours and emotionally overloaded content). On individual level strategies such as motivational interviewing techniques are potential approaches to solve uncertainties and to enhance vaccine acceptance [26], [31]. At society level measures should possibly be taken to reduce social and economic fears (e.g., by providing opportunities of social contact and financial support).
4.2. Strengths and limitations
The nuanced examination of different types of anxiety and fears, using well-established scales, considering the role of media usage, and the time period a few days after the first vaccinations add to the advantages of our study. On the one hand, the short period of data collection (ten days) is beneficial because it allows a clear allocation in the temporal context. On the other hand, it limits the generalizability of our results because controversies about vaccination have changed (and potentially increased) over time. As a further limitation, our sample is a repeatedly online measured self-selected convenience sample and not representative of the general population: e.g., due to the high proportion of females and high educational levels in the sample and an underrepresentation of elderly individuals. Media- and topic-affine individuals, as well as more conscientious persons and those with easier internet-access, might have had a higher probability to participate (repeatedly) in the survey. This potential lack of representativeness limits the accurate explanatory power of our results to individuals with those specific characteristics. The substantial sample size is not able to compensate for potential limitations in representativeness and generalizability. For subsequent studies, a larger sample size and random/probability sampling techniques would be desirable.
The cross-sectional observational data of our study does not allow any causal conclusions nor the identification of the temporal sequences and interconnections of different variables. In addition, it cannot be ruled out that further covariates modified the results of this study. Furthermore, the generalizability and the statistical power of our study are limited due to one-sided range restriction of the dependent variable because most participants had a rather positive attitude towards vaccination. Future studies should focus particularly on those individuals which are undecided or have only a slightly negative opinion towards the vaccination because they might have the best potential to change their beliefs regarding the vaccination [26].
Our study tried to reduce the gap between the vaccination acceptance before the actual supply of vaccines and the future behavior with the period of assessment shortly after the beginning of vaccinations in Germany. Nevertheless, our study still relies on self-reported hypothetical data which needs to be amended with the data as soon as most parts of the population were actually offered a vaccination. Anyhow, it is essential to address this issue already now in order to ensure that the future vaccination and the containment of the pandemic will be as successful as possible.
Future studies should assess the connection of several vaccine-related fears and beliefs with the different types of pandemic-related fears to further elucidate and complement the findings and questions raised in this study in more detail.
4.3. Conclusions
In summary, our results provide important up-to-date information and an essential base for future studies and interventions. It is remarkable that different types of pandemic-related fears show the contrary associations with vaccine acceptance. This highlights the need to differentiate between several types of fears and anxiety to predict their influence on vaccine acceptance. Furthermore, our findings emphasize that the concepts of public health and related programs need to have a broader, more holistic focus beyond just developing and providing vaccines; e.g., including the consideration of the beliefs, worries, fears, and other emotions of the target populations. In addition, associations between vaccine acceptance and different fears should be longitudinally analyzed and interventions, from a scientific perspective ideally randomized-controlled trials, should target fears with the aim of increasing the willingness for vaccination.
Funding/Support: This work was supported by the Sonnenfeld-Stiftung (grant for Antonia Bendau).
Role of the Funder/Sponsor: The Sonnenfeld-Stiftung had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Ethical Standards: The authors assert that all procedures contributing to this work have been approved by the appropriate ethics committee (ethics committee of Charité Universitätsmedizin Berlin: EA1/071/20) and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Additional Contributions: We would thank Sarah Wyka, Stefanie Kunas, Lena Pyrkosch, Julia Große, Dr. Lea Mascarell Maricic, Janina Rogoll, Dr. Felix Betzler, Dr. Katharina Feldker-Kasparek, and Prof. Dr. Peter Zwanzger for their support in conceptualizing and realizing the project. None of these individuals received compensation for their contribution. Furthermore, many thanks to the Sonnenfeld-Stiftung for supporting our efforts.
CRediT authorship contribution statement
Antonia Bendau: Conceptualization, Methodology, Formal analysis, Writing - original draft, Writing - review & editing. Jens Plag: Conceptualization, Writing - review & editing. Moritz Bruno Petzold: Conceptualization, Writing - original draft, Writing - review & editing. Andreas Ströhle: Conceptualization, Writing - review & editing, Supervision, Project administration.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.intimp.2021.107724.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Kumar V. Understanding the complexities of SARS-CoV2 infection and its immunology: a road to immune-based therapeutics. Int. Immunopharmacol. 2020;88:106980. doi: 10.1016/j.intimp.2020.106980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Salali G.D., Uysal M.S. COVID-19 vaccine hesitancy is associated with beliefs on the origin of the novel coronavirus in the UK and Turkey. Psychol. Med. 2020;1–3 doi: 10.1017/S0033291720004067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Molaei S., Dadkhah M., Asghariazar V., Karami C., Safarzadeh E. The immune response and immune evasion characteristics in SARS-CoV, MERS-CoV, and SARS-CoV-2: vaccine design strategies. Int. Immunopharmacol. 2021;92:107051. doi: 10.1016/j.intimp.2020.107051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mohammad M.H.S. Immune response scenario and vaccine development for SARS-CoV-2 infection. Int. Immunopharmacol. 2021;94:107439. doi: 10.1016/j.intimp.2021.107439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hotez P.J., Cooney R.E., Benjamin R.M., Brewer N.T., Buttenheim A.M., Callaghan T., Caplan A., Carpiano R.M., Clinton C., DiResta R., Elharake J.A., Flowers L.C., Galvani A.P., Lakshmanan R., Maldonado Y.A., McFadden S.M., Mello M.M., Opel D.J., Reiss D.R., Salmon D.A., Schwartz J.L., Sharfstein J.M., Omer S.B. Announcing the lancet commission on vaccine refusal, acceptance, and demand in the USA. The Lancet. 2021 doi: 10.1016/S0140-6736(21)00372-X. [DOI] [PubMed] [Google Scholar]
- 6.Gupta T., Gupta S.K. Potential adjuvants for the development of a SARS-CoV-2 vaccine based on experimental results from similar coronaviruses. Int. Immunopharmacol. 2020;86:106717. doi: 10.1016/j.intimp.2020.106717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Robert Koch Institut, COVID-19: Fallzahlen in Deutschland und weltweit, 2020. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Fallzahlen.html.
- 8.Freeman D., Loe B.S., Chadwick A., Vaccari C., Waite F., Rosebrock L., Jenner L., Petit A., Lewandowsky S., Vanderslott S. COVID-19 vaccine hesitancy in the UK: the Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol. Med. 2020;1–15 doi: 10.1017/S0033291720005188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Geoghegan S., O’Callaghan K.P., Offit P.A. Vaccine safety: myths and misinformation. Front. Microbiol. 2020;11:372. doi: 10.3389/fmicb.2020.00372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harrison E.A., Wu J.W. Vaccine confidence in the time of COVID-19. Eur. J. Epidemiol. 2020;35:325–330. doi: 10.1007/s10654-020-00634-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Detoc M., Bruel S., Frappe P., Tardy B., Botelho-Nevers E., Gagneux-Brunon A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine. 2020;38:7002–7006. doi: 10.1016/j.vaccine.2020.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malik A.A., McFadden S.M., Elharake J., Omer S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26:100495. doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schmid P., Rauber D., Betsch C., Lidolt G., Denker M.-L. Barriers of influenza vaccination intention and behavior - a systematic review of influenza vaccine hesitancy, 2005–2016. PLoS ONE. 2017;12:e0170550. doi: 10.1371/journal.pone.0170550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.M. Bults, D.J.M.A. Beaujean, J.H. Richardus, H.A.C.M. Voeten, Perceptions and behavioral responses of the general public during the 2009 influenza A (H1N1) pandemic: a systematic review, Disaster Medicine and Public Health Preparedness 9 (2015) 207–219. 10.1017/dmp.2014.160. [DOI] [PubMed]
- 15.Palamenghi L., Barello S., Boccia S., Graffigna G. Mistrust in biomedical research and vaccine hesitancy: the forefront challenge in the battle against COVID-19 in Italy. Eur. J. Epidemiol. 2020;35:785–788. doi: 10.1007/s10654-020-00675-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rzymski P., Nowicki M., Mullin G.E., Abraham A., Rodríguez-Román E., Petzold M.B., Bendau A., Sahu K.K., Ather A., Naviaux A.-F., Janne P., Gourdin M., Delanghe J.R., Ochs H.D., Talmadge J.E., Garg M., Hamblin M.R., Rezaei N. Quantity does not equal quality: scientific principles cannot be sacrificed. Int. Immunopharmacol. 2020;86:106711. doi: 10.1016/j.intimp.2020.106711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bendau A., Petzold M.B., Pyrkosch L., Mascarell Maricic L., Betzler F., Rogoll J., Große J., Ströhle A., Plag J. Associations between COVID-19 related media consumption and symptoms of anxiety, depression and COVID-19 related fear in the general population in Germany. Eur. Arch. Psychiatry Clin. Neurosci. 2020 doi: 10.1007/s00406-020-01171-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kennedy J. Vaccine hesitancy: a growing concern. Pediatric Drugs. 2020;22:105–111. doi: 10.1007/s40272-020-00385-4. [DOI] [PubMed] [Google Scholar]
- 19.Wilson S.L., Wiysonge C. Social media and vaccine hesitancy. BMJ Glob. Health. 2020;5 doi: 10.1136/bmjgh-2020-004206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harper C.A., Satchell L.P., Fido D., Latzman R.D. Functional fear predicts public health compliance in the COVID-19 pandemic. Int. J. Ment. Health Addict. 2020:1–14. doi: 10.1007/s11469-020-00281-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.French J., Deshpande S., Evans W., Obregon R. Key Guidelines in developing a pre-emptive COVID-19 vaccination uptake promotion strategy. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17165893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bendau A., Plag J., Kunas S., Wyka S., Ströhle A., Petzold M.B. Longitudinal changes in anxiety and psychological distress, and associated risk and protective factors during the first three months of the COVID-19 pandemic in Germany. Brain and Behavior. 2020:e01964. doi: 10.1002/brb3.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Petzold M.B., Bendau A., Plag J., Pyrkosch L., Maricic L.M., Rogoll J., Betzler F., Große J., Ströhle A. Development of the COVID-19-Anxiety Questionnaire and first psychometric testing. BJPsych Open. 2020;6:e91. doi: 10.1192/bjo.2020.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Löwe B., Wahl I., Rose M., Spitzer C., Glaesmer H., Wingenfeld K., Schneider A., Brähler E. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J. Affective Disorders. 2010;122:86–95. doi: 10.1016/j.jad.2009.06.019. [DOI] [PubMed] [Google Scholar]
- 25.Petzold M.B., Bendau A., Plag J., Pyrkosch L., Mascarell Maricic L., Betzler F., Rogoll J., Große J., Ströhle A. Risk, resilience, psychological distress, and anxiety at the beginning of the COVID-19 pandemic in Germany. Brain Behav. 2020 doi: 10.1002/brb3.1745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fisher K.A., Bloomstone S.J., Walder J., Crawford S., Fouayzi H., Mazor K.M. Attitudes Toward a Potential SARS-CoV-2 Vaccine A Survey of U.S. Adults. Ann. Internal Med. 2020;173:964–973. doi: 10.7326/M20-3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang J., Jing R., Lai X., Zhang H., Lyu Y., Knoll M.D., Fang H. Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. Vaccines (Basel) 2020;8 doi: 10.3390/vaccines8030482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bendau A., Kunas S.L., Wyka S., Petzold M.B., Plag J., Asselmann E., Ströhle A. Longitudinal changes of anxiety and depressive symptoms during the COVID-19 pandemic in Germany: the role of pre-existing anxiety, depressive, and other mental disorders. J. Anxiety Disorders. 2021:102377. doi: 10.1016/j.janxdis.2021.102377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chou W.-Y.-S., Budenz A. Considering emotion in COVID-19 vaccine communication: addressing vaccine hesitancy and fostering vaccine confidence. Health Commun. 2020;35:1718–1722. doi: 10.1080/10410236.2020.1838096. [DOI] [PubMed] [Google Scholar]
- 30.Lu P.-J., Srivastav A., Amaya A., Dever J.A., Roycroft J., Kurtz M.S., O'Halloran A., Williams W.W. Association of provider recommendation and offer and influenza vaccination among adults aged ≥18 years - United States. Vaccine. 2018;36:890–898. doi: 10.1016/j.vaccine.2017.12.016. [DOI] [PubMed] [Google Scholar]
- 31.Lemaitre T., Carrier N., Farrands A., Gosselin V., Petit G., Gagneur A. Impact of a vaccination promotion intervention using motivational interview techniques on long-term vaccine coverage: the PromoVac strategy. Hum. Vaccin. Immunother. 2019;15:732–739. doi: 10.1080/21645515.2018.1549451. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.