Abstract
Background
Despite the introduction of the concept known as “Chain of Survival” has significantly increased survival rates in patients with out-of-hospital cardiac arrest (OHCA), short-term mortality in this group of patients is still very high. Epidemiological data on OHCA in Poland are limited. The aim of this study was to create a prospective registry on OHCA covering a population of 2.7 million inhabitants of Upper Silesia in Poland. Presented herein is the study design and results of a 3-month pilot study.
Methods
The Silesian Registry of Out-of-Hospital Cardiac Arrest (SIL-OHCA) is a prospective, population-based registry of OHCA, of minimum duration which was planned for 12 months; from January 1st, 2018 to December 31st, 2018. The first 3 months of the study constituted the pilot phase. The inclusion criterion is the occurrence of OHCA in the course of activity of the Voivodeship Rescue Service in Katowice, Poland.
Results
During the 3-month pilot phase of the study there were 390 cases of OHCA in which cardiopulmonary resuscitation was undertaken. Estimated frequency of OHCA in the population analyzed was 57 per 100,000 population per year. Shockable rhythm was present in 25.8% of cases. Return of spontaneous circulation was achieved in 35.1% of the whole cohort. 28.7% of patients were admitted to the hospital, including 2.8% of patients, who were admitted during an ongoing cardiopulmonary resuscitation.
Conclusions
Prehospital survival of patients with OHCA in Poland is still unsatisfactory. It is believed that data collected in SIL-OHCA registry will allow identification factors, which require improvement in order to reduce short- and long-term mortality of patients with OHCA.
Keywords: out-of-hospital cardiac arrest, cardiopulmonary resuscitation, emergency medical services, registry
Introduction
Cardiovascular diseases are both the leading cause of death in adults of developed countries, and the most frequent cause of out-of-hospital cardiac arrest (OHCA) [1–5]. The introduction of the concept known as “chain of survival” has significantly increased the survival rate of patients with OHCA [4]. Nonetheless the mortality in this group of patients is still very high, and less than 10% of patients survive until hospital discharge [2]. Epidemiological data concerning OHCA in the European population is mainly provided from prospective registries, which number has increased over the last several years [3, 6–9]. Nonetheless, data on OHCA in Poland remains limited. The aim herein, therefore, was to create the Silesian Registry of Out-of-Hospital Cardiac Arrest (SIL-OHCA; ClinicalTrials.gov Identifier: NCT03654859) which covers a population of 2.7 million inhabitants of Upper Silesia. Main goals of SIL-OHCA are presented in Table 1. The study design of SIL-OHCA and the results of a 3-month pilot study are presented in this paper.
Table 1.
Questions to be answered by the results of Silesian Registry of Out-of-Hospital Cardiac Arrest.
| What is the frequency of OHCA in the Polish population? |
| What is the frequency of ROSC? |
| Which factors may affect the occurrence of ROSC? |
| What percentage of OHCA patients survive until admission to hospital? |
| What is the in-hospital/30-day mortality of patients with ROSC? |
| What percentage of patients who survive beyond 12 months after OHCA? |
| What factors affect the prognosis in patients with OHCA? |
| What is the percentage of OHCA patients whose primary cause of OHCA is cardiovascular disease? |
| What percentage of patients undergo coronary angiography/percutaneous coronary intervention during the first hospitalization after OHCA? |
| What percentage of patients with OHCA undergo implantable cardioverter-defibrillator implantation during the first year after OHCA? |
| What percentage of patients with OHCA undergo cardiological/neurological rehabilitation within a year after OHCA? |
OHCA — out-of-hospital cardiac arrest; ROSC — return of spontaneous circulation
Methods
SIL-OHCA is prospective, population-based registry of OHCA, a minimum duration was planned for 12 months, from January 1st, 2018 to December 31st, 2018 with the possibility of prolonging the study period. The first 3 months of the study (1st January 2018 to 30th March 2018) constituted the pilot phase. The area covered by the registry is a part of the Silesian Voivodeship (3883 km2, 1.2% of the total area of Poland), this corresponds to the region of activity of the Voivodeship Rescue Service in Katowice. There are 2,700,000 inhabitants in the area covered by this registry (7% of the population of Poland) and the mean population density is 695 persons per km2. Voivodeship Rescue Service in Katowice is the biggest public, emergency medical services (EMS) provider in Poland and is the sole EMS provider in the area covered by SIL-OHCA registry, excluding Polish Medical Air Rescue. There are 88 EMS ambulances in the structures of Voivodeship Rescue Service in Katowice, including 66 ambulances, consisting of two paramedics, and 22 ambulances, consisting of two paramedics and a physician. On average the number of EMS responses of Voivodeship Rescue Service in Katowice is 250,000 per year. Voivodeship Rescue Service in Katowice follows cardiopulmonary resuscitation (CPR) algorithms based on European Resuscitation Council guidelines [10, 11].
From 1st January to 30th June 2018 (including the pilot phase of the study) all cases of OHCA with CPR started or continued by EMS and cases with confirmed OHCA and the return of spontaneous circulation (ROSC) before EMS arrival have been included in the study (regardless of the cause of OHCA and age of patients). Additionally, starting from 1st July 2018 all OHCA cases where resuscitation was not attempted have been included as well.
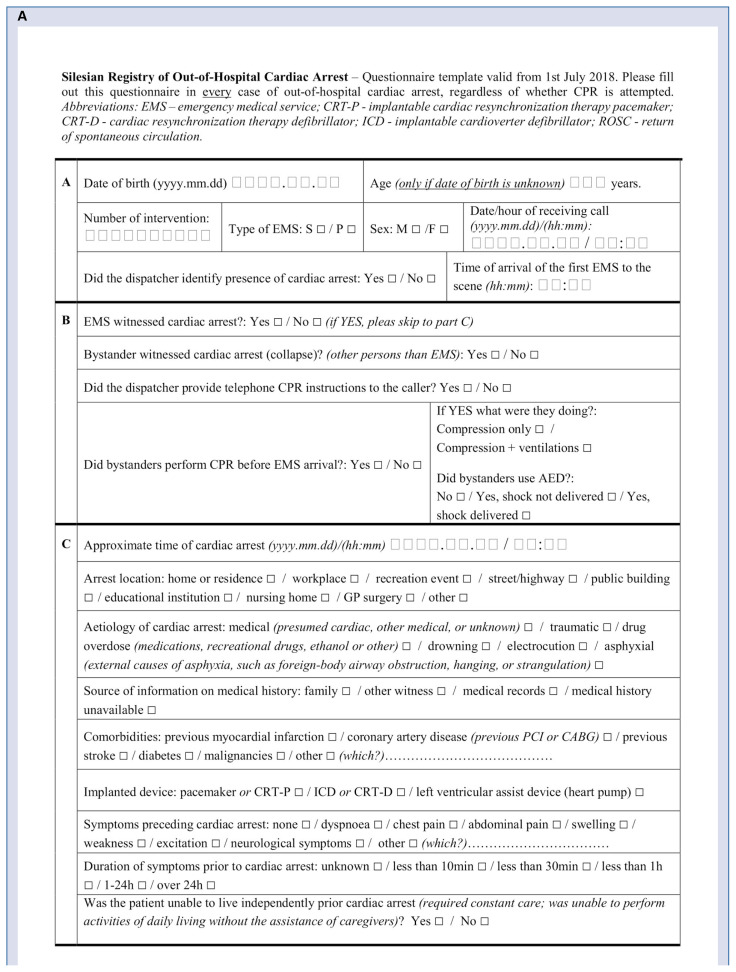
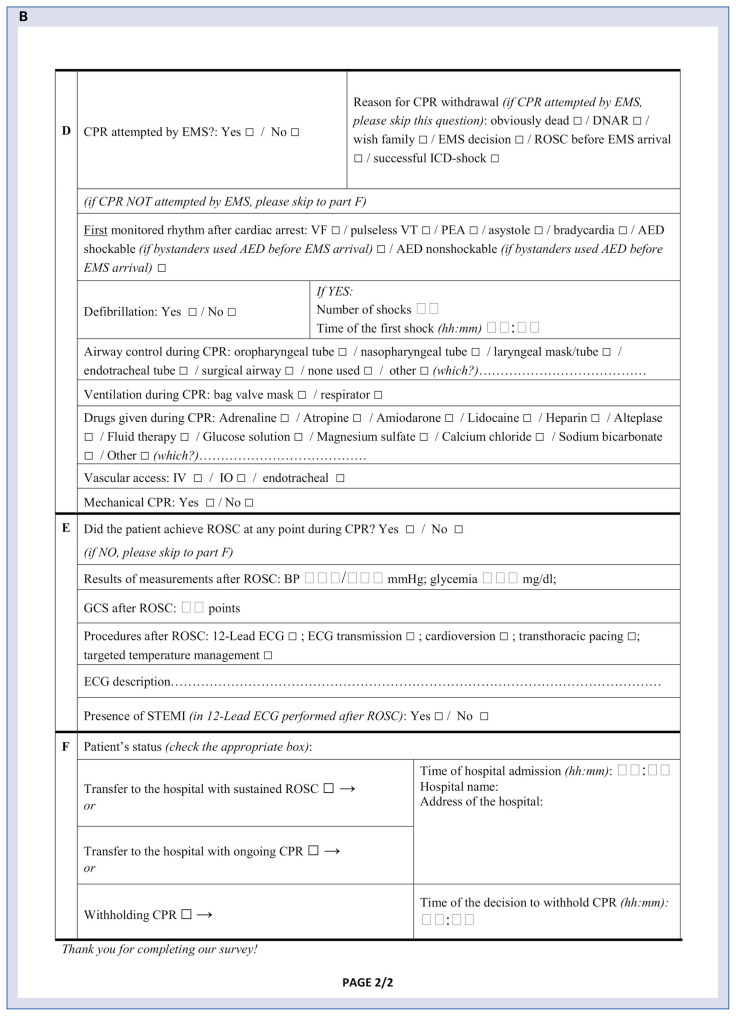
All EMS of Voivodeship Rescue Service in Katowice are required to fill out a standardized, paper-based questionnaire, immediately after completing medical activities. The questionnaire template is presented in Figure 1. In the case of intervention of more than one EMS, data provided by the EMS, that transferred the patient to the hospital or decided to stop CPR are taken into consideration. Subsequently, all questionnaires are transferred to the headquarters of Voivodeship Rescue Service, where they are archived digitally.
Figure 1.
Questionnaire template.
The questionnaire template, as well as all terms and definitions used in SIL-OHCA are based on the updated Utstein guidelines on reporting OHCA (2015) [1].
Follow-up
All patients transferred to the hospital by EMS are followed-up for a minimum of 1 year from the OHCA occurrence for all-cause mortality during initial hospitalization, within 30 days and at 12 months. The follow-up data will be sourced from the SILesian CARDiovascular (SILCARD) database, which is a joint initiative of the Silesian Center for Heart Diseases and the National Health Fund. SILCARD is a registry of administrative data, which comprises inter alia patients hospitalized due to OHCA within the Silesian Voivodeship area. Detailed information on the SILCARD registry have been published previously [12]. Data from the SILCARD registry enables to determine the etiology of OHCA (based on the final diagnosis during the first hospitalization after OHCA) to assess the percentage of patients who underwent procedures such as myocardial revascularization or cardioverter-defibrillator implantation, and to estimate the percentage of patients undergoing cardiac and neurological rehabilitation. Prehospital and follow-up data will be linked based on a patient’s date of birth, individual code of the unit (hospital, department) to which the patient was transferred and the date of admission to the unit. An estimated percentage of patients who survived beyond admission to hospital, and for whom follow-up was available in more than 99% of patients with available date of birth and admission status. The percentage of patients with accessible date of birth in the pilot study was 96.1% and admission status was available for all patients. In cases where data linking baseline characteristics with follow-up are ambiguous i.e. more than 1 patient born on the same day is admitted to a given unit on a given day then patient follow-up data will not be taken into consideration. Based on currently available SILCARD data, it was estimated that the percentage of these patients would not exceed 1%.
The study conformed to the Declaration of Helsinki. Approval for research was waived by the Bioethics Committee of the Silesian Medical Chamber, given the observational nature of the study.
Statistical analysis
Dichotomous variables are presented as number of cases (percentage). Continuous variables are presented as median and (interquartile range [IQR]). Analysis of the pilot-study data was performed both for the whole cohort of EMS-treated patients, as well as the subgroup of patients with bystander witnessed cardiac arrest and an initial shockable rhythm (Utstein comparator group [1]). There were no prespecified analyses in the SIL-OHCA registry.
Results
Results of 3-month pilot study
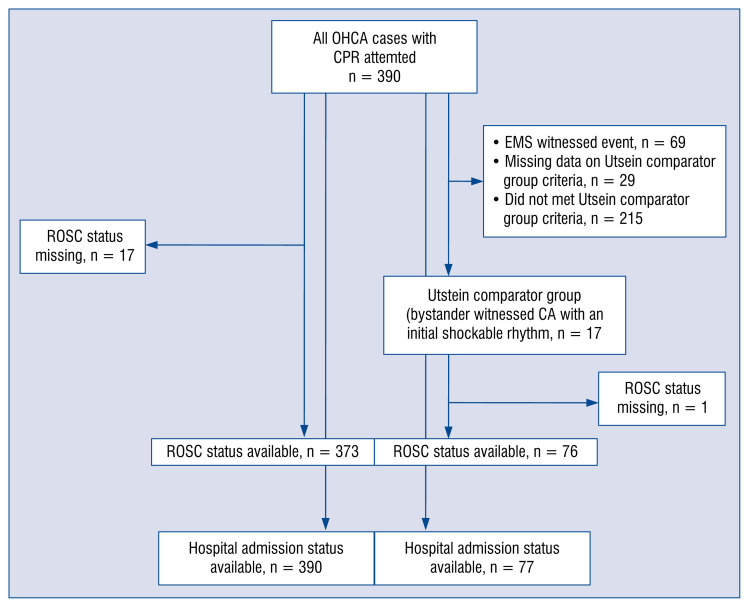
During the 3-month pilot phase of the study there were 390 cases of OHCA (128 women, 262 men), which is 0.6% of EMS responses during the period analyzed. A flow-chart of the pilot study population is presented in Figure 2. The median age of patients was 66 years (range 0–97 years; IQR 56–77 years). It was estimated that there are about 1560 cases of OHCA in the area covered per year, which corresponds with the 57 cases per 100,000 population per year. Baseline characteristics of the study population is shown in Table 2. The most frequent etiology of OHCA was medical. Asystole was the most common initial rhythm. Shockable rhythm was present in 25.8% of patients. The most frequent location of OHCA was home/residence, and 89.9% of events were witnessed. CPR was performed by bystander witnesses in 47.9% of OHCA cases. Automated external defibrillator (AED) was used by witnesses in 3 (0.8%) patients. ROSC occurred in 35.1% of the whole cohort, and in 51.3% of patients who met the Utstein comparator group criteria (bystander witnessed cardiac arrest with an initial shockable rhythm). In the whole study group, 28.7% of patients were admitted to hospital, including 2.8% of patients who were admitted during ongoing CPR. In the Utstein comparator group, 41.6% of patients were admitted to hospital, including 1.5% of patients during ongoing CPR.
Figure 2.
Flow-chart of the pilot study population; CA — cardiac arrest; CPR — cardiopulmonary resuscitation; EMS — emergency medical services; OHCA — out-of-hospital cardiac arrest; ROSC — return of spontaneous circulation.
Table 2.
Demographic data, baseline characteristics and outcome of patients with OHCA included in Silesian Registry of Out-of-Hospital Cardiac Arrest.
| Variable | Whole population (n = 390) | Percentage of cases with missing data |
|---|---|---|
| Age [years] | 66 [56–77] | 3.8 |
| Sex: | 0 | |
| Male | 262 (67.2) | |
| Female | 128 (32.8) | |
| OHCA etiology: | 1.5 | |
| Medical | 299 (77.9) | |
| Asphyxial | 44 (11.5) | |
| Traumatic | 9 (2.3) | |
| Other | 32 (8.3) | |
| Location of OHCA: | 0.2 | |
| Home/residence | 282 (72.5) | |
| Public space | 64 (16.5) | |
| Other | 43 (11.1) | |
| Response time [min] | 8 [6–11] | 1.3 |
| EMS witnessed OHCA | 69 (17.9) | 0 |
| Bystander CPR | 186 (47.9) | 0.5 |
| Comorbidities: | 0 | |
| Previous MI | 51 (13.1) | |
| Previous stroke | 37 (9.5) | |
| Malignancies | 27 (6.9) | |
| Previously implanted cardioverter-defibrillator | 4 (1.0) | 0 |
| First monitored rhythm: | 4.6 | |
| VF/pulseless VT | 96 (25.8) | |
| Asystole/PEA | 276 (74.2) | |
| 12-lead ECG performed after ROSC | 54 (41.2) | 0 |
| Presence of STEMI | 16 (29.6) | 58.8 |
| Patients who met the Utstein comparator group criteria (bystander witnessed CA with an initial shockable rhythm) | 77 (19.7) | 7.4 |
| ROSC (whole population) | 131 (35.1) | 4.4 |
| Status of patients on hospital admission (whole population): | 0 | |
| Died before hospital admission | 278 (71.3) | |
| Admission to hospital with ROSC | 101 (25.9) | |
| Admission to hospital during ongoing CPR | 11 (2.8) | |
| ROSC (Utstein comparator group) | 39 (51.3) | 1.3 |
| Status of patients on hospital admission (Utstein comparator group): | 0 | |
| Died before hospital admission | 45 (58.4) | |
| Admission to hospital with ROSC | 31 (40.3) | |
| Admission to hospital during ongoing CPR | 1 (1.3) |
Dichotomous variables are presented as number of cases (percentage). Continous variables are presented as median (intequartile range); CA — cardiac arrest; CPR — cardiopulmonary resuscitation; ECG — electrocardiography; OHCA — out-of-hospital cardiac arrest; MI — myocardial infarction; PEA — pulseless electrical activity; ROSC — return of spontaneous circulation; STEMI — ST-elevation myocardial infarction; VF — ventricular fibrillation; VT — ventricular tachycardia
Discussion
Large-scale medical registries are the primary source of information on the epidemiology of OHCA [2, 13, 14]. They enable analyzing trends in the occurrence, treatment approaches and prognosis in OHCA [15, 16]. International EuReCa One study encompassing 10,682 OHCA cases in 27 European countries have indicated substantial differences in the frequency of OHCA and survival to hospital discharge among participating countries [2]. In this registry 275 patients with OHCA from Poland were included, and inhabited only small cities (< 100,000 inhabitants) or villages [2]. The biggest prospective registry of OHCA in the Polish population was described by Cebula et al. [8], who provided a lot of valuable information on epidemiology of OHCA, however it did not include long-term follow-up. Aforementioned limitations of the previous studies provided reasons to introduce SIL-OHCA covering a population of 2.7 million inhabitants, residing in the highly urbanized region of Upper Silesia.
To the best of our knowledge, there have been published results in one prospective and three retrospective registries encompassing the Polish population to date [8, 17–19], as well as data from Poland which was reported in the international EuReCa ONE study [2]. The frequency of OHCA with attempted CPR was 70–128 cases per 100,000 population per year in these registries. The incidence of OHCA in the Upper Silesian population was estimated on the basis of the present 3-month pilot study when there were 57 cases per 100,000 inhabitants per year, which was close to the mean frequency in the European population (49 cases/100,000 inhabitants per year) [2]. Approximately two-thirds of patients with OHCA included in the examined registry were male, this finding was similar to other studies [8, 18]. ROSC in the present population was achieved in 35.1% of patients, which confirms previously published data from Poland, where ROSC occurred in 30.5–31.2% of cases [8, 18]. In addition, in a homogeneous sub-population meeting Utstein comparator group criteria, the ROSC frequency was 51.3%, which corresponds to data from European registries and is slightly lower than that reported on average in Europe (56.8%) [2]. Finally, of all patients with OHCA included in the pilot study, 25.9% survived the event (were transferred to the hospital with sustained ROSC). This finding is also very similar to the results of EuReCa ONE, where the event survival rate was 25.2% [2].
The results of the present 3-month pilot study have indicated an inadequate participation of bystanders in CPR before the arrival of EMS, which has a significant impact on the percentage of cases with shockable rhythm, and long-term outcome [20–22]. Hasselqvist-Ax et al. [20] reported, based on data from nationwide Swedish registry of OHCA, that CPR performed by bystanders was associated with 30-day survival, which is more than twice as high as that associated with no CPR before EMS arrival. A high percentage of cases with CPR performed before EMS arrival in Sweden is probably due to the fact that almost one third of the Swedish population have undergone CPR training during the past three decades [20, 23]. In this context Sweden is a role model for other nations [23]. In addition, Nakahara et al. [21] reported that in Japan, between 2005 and 2012, increase in neurologically intact survival in patients with OHCA was observed, which was associated with an increased rate of bystander CPR. Another critical element of the “chain of survival”, besides CPR, is rapid defibrillation [24]. Hansen et al. [25] showed that over 30% of patients with OHCA, who were defibrillated by bystanders, survived to hospital discharge. The AED was used by bystanders in less than 1% of cases included in SIL-OHCA, which may have been be due to the low availability of AED, as well as insufficient knowledge of society about the possibility of using the device. The use of AED by bystanders in the present population was over five times lower than reported in the United States, according to study by van Diepen et al. [26]. Aforementioned factors affect an unsatisfactory percentage of ROSC, as well as the percentage of patients admitted to the hospital with sustained ROSC, which, despite being close to the outcomes reported on average in the European population, is lower than results achieved in some Western European countries [2, 27, 28]. There is a critical need for interventions to increase the frequency of bystander CPR and AED use in the Polish population to improve survival rate in patients with OHCA.
The SIL-OHCA registry, which is an initiative of the Voivodeship Rescue Service in Katowice in cooperation with the Silesian Center for Heart Diseases in Zabrze, is, to the best of our knowledge, the first prospective OHCA registry which aims to assess long-term prognosis for this group of patients in Poland. Results of the 3-month pilot study confirmed the possibility of creating registry which covers all patients with OHCA in the region of activity of Voivodeship Rescue Service in Katowice. In the pilot phase of the study, the percentage of missing data was low, and results presented were comparable to previous studies. We believe that the SIL-OHCA registry will provide reliable epidemiological data on OHCA, including the prehospital data and long-term follow-up. Owing to the data collected, it will be possible to identify factors that need improvement in order to increase both the short- and long-term survival rates of patients with OHCA.
Conclusions
Short-term results of OHCA patients in Poland are still unsatisfactory. It is believed that owing to the prospective registry, medical practitioners will be able to identify factors that require modification in order to improve short- and long-term prognosis in patients with OHCA.
Footnotes
Conflict of interest: None declared
References
- 1.Perkins G, Jacobs I, Nadkarni V, et al. Cardiac Arrest and Cardiopulmonary Resuscitation Outcome Reports: Update of the Utstein Resuscitation Registry Templates for Out-of-Hospital Cardiac Arrest. Resuscitation. 2015;96:328–340. doi: 10.1016/j.resuscitation.2014.11.002.. [DOI] [PubMed] [Google Scholar]
- 2.Gräsner JT, Lefering R, Koster RW, et al. EuReCa ONE-27 Nations, ONE Europe, ONE Registry: A prospective one month analysis of out-of-hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation. 2016;105:188–195. doi: 10.1016/j.resuscitation.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 3.Masterson S, Wright P, O’Donnell C, et al. Urban and rural differences in out-of-hospital cardiac arrest in Ireland. Resuscitation. 2015;91:42–47. doi: 10.1016/j.resuscitation.2015.03.012. [DOI] [PubMed] [Google Scholar]
- 4.Iwami T, Nichol G, Hiraide A, et al. Continuous improvements in “chain of survival” increased survival after out-of-hospital cardiac arrests: a large-scale population-based study. Circulation. 2009;119(5):728–734. doi: 10.1161/CIRCULATIONAHA.108.802058. [DOI] [PubMed] [Google Scholar]
- 5.Freund B, Kaplan PW. A review of the utility of a hypothermia protocol in cardiac arrests due to non-shockable rhythms. Cardiol J. 2017;24(3):324–333. doi: 10.5603/CJ.a2017.0016. [DOI] [PubMed] [Google Scholar]
- 6.Hubert H, Tazarourte K, Wiel E, et al. Rationale, methodology, implementation, and first results of the French out-of-hospital cardiac arrest registry. Prehosp Emerg Care. 2014;18(4):511–519. doi: 10.3109/10903127.2014.916024. [DOI] [PubMed] [Google Scholar]
- 7.Strömsöe A, Svensson L, Axelsson ÅB, et al. Improved outcome in Sweden after out-of-hospital cardiac arrest and possible association with improvements in every link in the chain of survival. Eur Heart J. 2015;36(14):863–871. doi: 10.1093/eurheartj/ehu240. [DOI] [PubMed] [Google Scholar]
- 8.Cebula GM, Osadnik S, Wysocki M, et al. Comparison of the early effects of out-of-hospital resuscitation in selected urban and rural areas in Poland. A preliminary report from the Polish Cardiac Arrest Registry by the Polish Resuscitation Council. Kardiol Pol. 2016;74(4):356–361. doi: 10.5603/KP.a2016.0001. [DOI] [PubMed] [Google Scholar]
- 9.Ristagno G, Semeraro F, Radeschi G, et al. The “Italian Registry of Cardiac Arrest - RIAC”, a National achievement to portrait the Italian reality and to contribute to the wider European vision by “EuReCa”. Resuscitation. 2014;85(12):e193–e194. doi: 10.1016/j.resuscitation.2014.09.015. [DOI] [PubMed] [Google Scholar]
- 10.Perkins GD, Olasveengen TM, Maconochie I, et al. European Resuscitation Council. European Resuscitation Council Guidelines for Resuscitation: 2017 update. Resuscitation. 2018;123:43–50. doi: 10.1016/j.resuscitation.2017.12.007. [DOI] [PubMed] [Google Scholar]
- 11.Monsieurs KG, Nolan JP, Bossaert LL, et al. ERC Guidelines 2015 Writing Group. European Resuscitation Council Guidelines for Resuscitation 2015: Section 1. Executive summary. Resuscitation. 2015;95:1–80. doi: 10.1016/j.resuscitation.2015.07.038. [DOI] [PubMed] [Google Scholar]
- 12.Gąsior M, Pres D, Wojakowski W, et al. Causes of hospitalization and prognosis in patients with cardiovascular diseases. Secular trends in the years 2006–2014 according to the SILesian CARDiovascular (SILCARD) database. Pol Arch Med Wewn. 2016;126(10):754–762. doi: 10.20452/pamw.3557. [DOI] [PubMed] [Google Scholar]
- 13.van Diepen S, Abella BS, Bobrow BJ, et al. Multistate implementation of guideline-based cardiac resuscitation systems of care: description of the HeartRescue project. Am Heart J. 2013;166(4):647–653.e2. doi: 10.1016/j.ahj.2013.05.022. [DOI] [PubMed] [Google Scholar]
- 14.Berger S. Survival from out-of-hospital cardiac arrest: are we beginning to see progress? J Am Heart Assoc. 2017;6(9) doi: 10.1161/JAHA.117.007469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Okubo M, Kiyohara K, Iwami T, et al. Nationwide and regional trends in survival from out-of-hospital cardiac arrest in Japan: a 10-year cohort study from 2005 to 2014. Resuscitation. 2017;115:120–128. doi: 10.1016/j.resuscitation.2017.03.036. [DOI] [PubMed] [Google Scholar]
- 16.Ro YS, Shin SDo, Kitamura T, et al. Temporal trends in out-of-hospital cardiac arrest survival outcomes between two metropolitan communities: Seoul-Osaka resuscitation study. BMJ Open. 2015;5(6):e007626. doi: 10.1136/bmjopen-2015-007626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kłosiewicz T, Skitek-Adamczak I, Zieliński M. Emergency medical system response time does not affect incidence of return of spontaneous circulation after prehospital resuscitation in one million central European agglomeration residents. Kardiol Pol. 2017;75(3):240–246. doi: 10.5603/KP.a2016.0181. [DOI] [PubMed] [Google Scholar]
- 18.Gach D, Nowak JU, Krzych ŁJ. Epidemiology of out-of-hospital cardiac arrest in the Bielsko-Biala district: a 12-month analysis. Kardiol Pol. 2016;74(10):1180–1187. doi: 10.5603/KP.a2016.0086. [DOI] [PubMed] [Google Scholar]
- 19.Szczerbinski S, Ratajczak J, Lach P, et al. Epidemiology and chronobiology of out-of-hospital cardiac arrest in a subpopulation of southern Poland: A two-year observation. Cardiol J. 2020;27(1):16–24. doi: 10.5603/CJ.a2018.0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hasselqvist-Ax I, Riva G, Herlitz J, et al. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med. 2015;372(24):2307–2315. doi: 10.1056/NEJMoa1405796. [DOI] [PubMed] [Google Scholar]
- 21.Nakahara S, Tomio J, Ichikawa M, et al. Association of Bystander Interventions With Neurologically Intact Survival Among Patients With Bystander-Witnessed Out-of-Hospital Cardiac Arrest in Japan. JAMA. 2015;314(3):247–254. doi: 10.1001/jama.2015.8068. [DOI] [PubMed] [Google Scholar]
- 22.Jorge-Soto C, Abilleira-González M, Otero-Agra M, et al. Schoolteachers as candidates to be basic life support trainers: A simulation trial. Cardiol J. 2018 doi: 10.5603/CJ.a2018.0073. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Strömsöe A, Andersson B, Ekström L, et al. Education in cardiopulmonary resuscitation in Sweden and its clinical consequences. Resuscitation. 2010;81(2):211–216. doi: 10.1016/j.resuscitation.2009.10.014. [DOI] [PubMed] [Google Scholar]
- 24.Krammel M, Schnaubelt S, Weidenauer D, et al. Gender and age-specific aspects of awareness and knowledge in basic life support. PLoS One. 2018;13(6):e0198918. doi: 10.1371/journal.pone.0198918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hansen CM, Kragholm K, Granger CB, et al. The role of bystanders, first responders, and emergency medical service providers in timely defibrillation and related outcomes after out-of-hospital cardiac arrest: Results from a statewide registry. Resuscitation. 2015;96:303–309. doi: 10.1016/j.resuscitation.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 26.van Diepen S, Girotra S, Abella BS, et al. Multistate 5-Year Initiative to Improve Care for Out-of-Hospital Cardiac Arrest: Primary Results From the HeartRescue Project. J Am Heart Assoc. 2017;6(9) doi: 10.1161/JAHA.117.005716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gräsner JT, Meybohm P, Fischer M, et al. A national resuscitation registry of out-of-hospital cardiac arrest in Germany-a pilot study. Resuscitation. 2009;80(2):199–203. doi: 10.1016/j.resuscitation.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 28.Blom MT, Beesems SG, Homma PCM, et al. Improved survival after out-of-hospital cardiac arrest and use of automated external defibrillators. Circulation. 2014;130(21):1868–1875. doi: 10.1161/CIRCULATIONAHA.114.010905. [DOI] [PubMed] [Google Scholar]