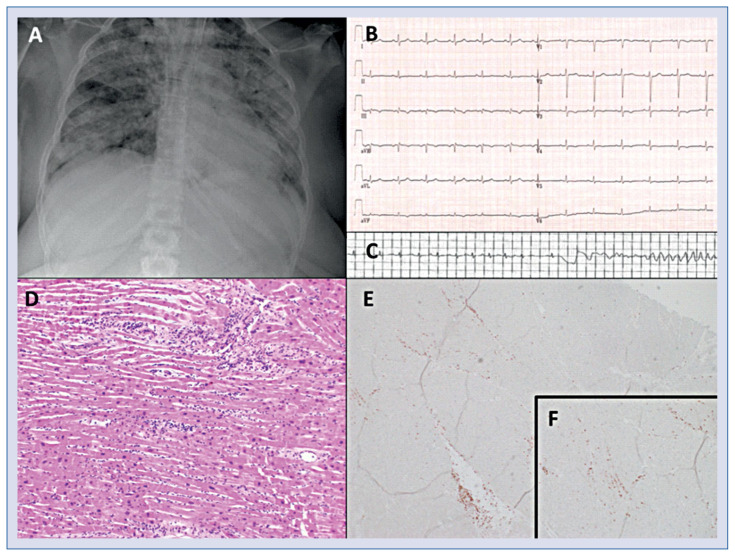
A 42-year-old female patient was admitted for shortness of breath during the COVID-19 pandemic. She had been tested positive for SARS-CoV-2 5 days before hospital admission. Medical history included bariatric surgery for morbid obesity 6 years prior and elevated blood pressure at occasional measurements. Admission heart rate was 75 bpm and blood pressure was 109/62 mmHg. Body mass index was 42 kg/m2. C-reactive protein was 54.3 mg/L (0–5 mg/L), high-sensitivity cardiac troponin I level was 12.3 ng/L (< 16 ng/L), lactate dehydrogenase was 464 U/L (120–240 U/L), and N-terminal-pro-B-type natriuretic peptide was 150 pg/mL (< 125 pg/mL). Peripheral oxygen saturation was 82% and increased to 89% with oxygen supply (4 L/min by nasal cannula). Transthoracic echocardiography showed normal systolic left ventricular function. Chest radiography showed bilateral pulmonary infiltrates (Fig. 1A). Electrocardiography revealed T-wave inversion in leads III and aVF and repolarization irregularities in left precordial leads (Fig. 1B). The patient required mechanical ventilation for progressive respiratory failure 6 hours after admission. High-sensitivity troponin I and N-terminal-pro-B-type natriuretic peptide increased to a peak of 28.1 ng/L (< 16 ng/L) and 636.8 pg/mL (< 125 pg/mL), respectively. On day 9 after admission, sudden onset ventricular fibrillation occured (Fig. 1C) and resuscitation was unsucessful. Autopsy revealed lymphocytic infiltates of the myocardium (Fig. 1D) and positive staining with anti-CD3 antibody characterizing T cells (Fig. 1E, F).
Figure 1.
Chest radiography with bilateral pulmonary infiltrates (A). Electrocardiography reveals T-wave inversion in leads III and aVF and repolarization irregularities in left precordial leads (B). Monitor electrocardiogram with sudden onset ventricular fibrillation (C). Hematoxylin-eosin staining of myocardium reveals lmphocytic infiltates (D) with positive staining with anti-CD3 antibody characterizing T cells (E, F).
Footnotes
Conflict of interest: None declared