Scquizzato et al. [1] in their meta-analysis showed out-of-hospital cardiac arrest had worse short-term outcomes during the pandemic than a non-pandemic period, suggesting direct effects of COVID-19 infection and indirect effects from lockdown and disruption of healthcare systems. The American Heart Association (AHA) has issued an interim guideline on basic life support during COVID-19 [2, 3]. Since 2010, the AHA removed rescue breaths guidelines from the basic life support algorithm in favor of a hands-only approach for resuscitation performed by the public for individuals [4, 5]. As show by Rosell Ortiz et al. [6] the frequency of undertaking resuscitation by bystanders before the pandemic was 51.5% and during the pandemic it was 42.6%. Borkowska et al. [7] show the cardiopulmonary resuscitation (CPR) rapidity during the pandemic at the level of 10.1%. The reduction in the frequency of resuscitation by the witnesses of an incident in the Rosell Ortiz study [6] may be because of the increased level of fear of SARS-CoV-2 infection per person with cardiac arrest [8]. One might suppose that limitation of movement or lockdown also influenced such behavior, however, studies by Rosell Ortiz et al. [6] and Chan et al. [9] seem to contradict this thesis. In these studies, the witnessed cardiac arrest was at a comparable level both before the COVID-19 pandemic and during the pandemic. As showed by Jorge-Soto et al. [10] brief hands-on training supported by real-time feedback of CPR quality helps future schoolteachers improve their knowledge, self-confidence and CPR skills and build pro-health attitudes and increase the chances of undertaking CPR.
In order to verify the influence of COVID-19 on the frequency of resuscitation by witnesses of the event, a systematic review and meta-analysis were performed.
This review was performed according to the Cochrane Collaboration methodological guidelines. We conducted a literature search in the EMBASE, PubMed, Web of Science, Scopus and Cochrane Library databases, covering the publication period from databases inception to November 15, 2020. Two investigators (M.P. and S.B.) independently reviewed the articles obtained. Disagreements between the two investigators were resolved by a third reviewer (A.G. or L.S.).
All results are presented with a 95% confidence interval (CI). When the continuous outcome was reported in a study as median, range, and interquartile range, estimated means and standard deviations using the formula described by Hozo et al. [11] were used. Heterogeneity of the effect sizes was checked with the I2 index. If p > 0.1 and I2 < 50%, a fixed effect model was used, otherwise a random effect model was chosen. All statistical analyzes were carried out using RevMan 5.4 software (The Cochrane Collaboration, Oxford, Copenhagen, Denmark).
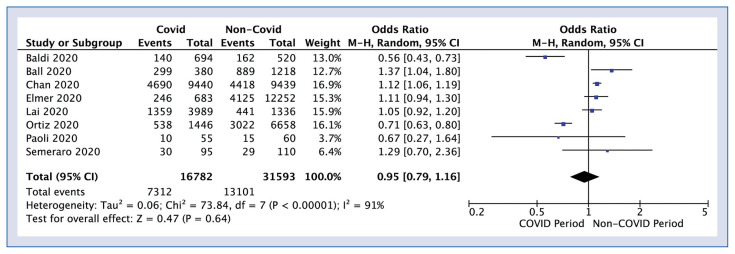
Eight studies reported bystander CPR ratio in COVID-19 and pre-COVID-19 periods. Bystander CPR rate in COVID-19 period was 43.6% vs. 41.5% for non-COVID-19 period (odds ratio: 0.95; 95% CI: 0.79–1.16; p = 0.64; I2: 91%; Fig. 1). Detailed characteristics of the studies included in the analysis are presented in Supplementary Table 1.
Figure 1.
Forest plot of bystander cardiopulmonary resuscitation rate in COVID-19 versus non-COVID-19 period. The center of each square represents the weighted odds ratios for individual trials, and the corresponding horizontal line stands for a 95% confidence interval (CI). The diamonds represent pooled results.
In summary, the meta-analysis performed showed a slightly higher frequency of CPR by witnesses during the COVID-19 pandemic compared to the periods preceding the pandemic. However, despite this fact, the effectiveness of resuscitation in out-of-hospital cardiac arrest is significantly lower than in the pre-pandemic period.
Supplementary Information
Footnotes
Conflict of interest: None declared
References
- 1.Scquizzato T, Landoni G, Paoli A, et al. Effects of COVID-19 pandemic on out-of-hospital cardiac arrests: A systematic review. Resuscitation. 2020 doi: 10.1016/j.resuscitation.2020.10.020. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Edelson DP, Sasson C, Chan PS, et al. Interim Guidance for Basic and Advanced Life Support in Adults, Children, and Neonates With Suspected or Confirmed COVID-19 From the Emergency Cardiovascular Care Committee and Get With The Guidelines-Resuscitation Adult and Pediatric Task Forces of the American Heart Association. Circulation. 2020;141(25):e933–e943. doi: 10.1161/CIRCULATIONAHA.120.047463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smereka J, Iskrzycki Ł, Makomaska-Szaroszyk E, et al. The effect of chest compression frequency on the quality of resuscitation by lifeguards. A prospective randomized crossover multicenter simulation trial. Cardiol J. 2019;26(6):769–776. doi: 10.5603/CJ.a2018.0121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Majer J, Jaguszewski MJ, Frass M, et al. Does the use of cardiopulmonary resuscitation feedback devices improve the quality of chest compressions performed by doctors? A prospective, randomized, cross-over simulation study. Cardiol J. 2019;26(5):529–535. doi: 10.5603/CJ.a2018.0091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abelsson A, Lundberg L. Prehospital CPR training performed with visual feedback. Disaster Emerg Med J. 2018;3(2):41–45. doi: 10.5603/demj.2018.0010.. [DOI] [Google Scholar]
- 6.Rosell Ortiz F, Fernández Del Valle P, Knox EC, et al. Influence of the Covid-19 pandemic on out-of-hospital cardiac arrest. A Spanish nationwide prospective cohort study. Resuscitation. 2020 doi: 10.1016/j.resuscitation.2020.09.037. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Borkowska MJ, Smereka J, Safiejko K, et al. Out-of-hospital cardiac arrest treated by emergency medical service teams during COVID-19 pandemic: A retrospective cohort study. Cardiol J. 2020 doi: 10.5603/CJ.a2020.0135. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perman SM. Overcoming fears to save lives: COVID-19 and the threat to bystander CPR in out-of-hospital cardiac arrest. Circulation. 2020;142(13):1233–1235. doi: 10.1161/CIRCULATIONAHA.120.048909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chan PS, Girotra S, Tang Y, et al. Outcomes for out-of-hospital cardiac arrest in the united states during the coronavirus disease 2019 pandemic. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.6210. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jorge-Soto C, Abilleira-González M, Otero-Agra M, et al. Schoolteachers as candidates to be basic life support trainers: a simulation trial. Cardiol J. 2019;26(5):536–542. doi: 10.5603/CJ.a2018.0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.