Abstract
Opioids are commonly administered in the emergency department (ED) and prescribed for the treatment of back pain. It is important to understand the unintended consequences of this approach to inform treatment decisions and the consideration of alternative treatments. Recent evidence has shown that ED opioid prescriptions are associated with future opioid use. The objective of this study was to measure the association of opioid administration in the ED to patients treated for back pain with future opioid use.
Methods:
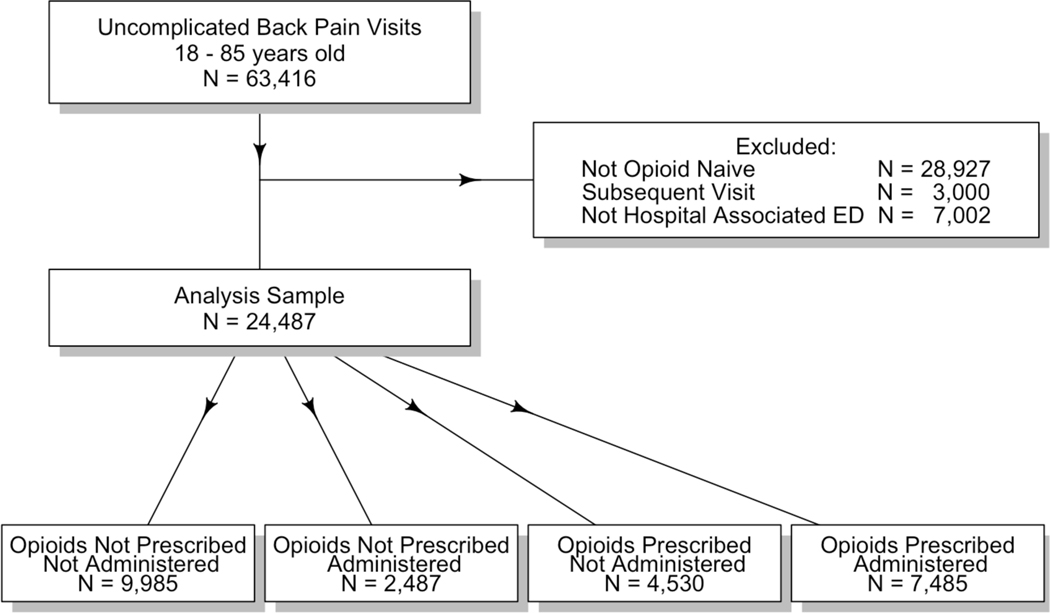
This is a retrospective study of opioid naïve adults discharged from the ED with a diagnosis of back pain. Patients were stratified by opioid therapy (none, ED administration only, prescription only, or ED administration + prescription). Relative risks of ongoing opioid use (filling >90-day supply in 180 days following ED visit as documented in the prescription drug monitoring program) were calculated for each opioid therapy group and compared to no the no opioid group.
Results:
We identified 24,487 opioid naïve back pain patients.. The median age was 38 years, 55% were female and 56% were non-Hispanic white. 41% received no opioid, 10% were only administered an ED opioid, 18% only received a prescription, and 31% received an ED opioid + prescription. The adjusted relative risks of ongoing use compared to the no opioid group were: ED only 1.9, prescription only 2.1, ED+ prescription 2.3. The increased risk persisted for other definitions of ongoing use and after adjustment for baseline pain scores.
Conclusions:
For opioid naïve patients with back pain, both ED opioid administration and opioid prescriptions are associated with a doubling of the risk of ongoing opioid use compared to patients not treated with opioids. This supports the consideration of minimizing exposure to opioids while treating back pain in the ED.
INTRODUCTION
Over 2.5 million patients are treated in U.S. Emergency Departments for back pain every year and approximately 60% of these will be treated with opioids. 1 The short-term safety and efficacy of parenteral 2–5 and oral opioids6–8 for treatment of acute pain (including back pain) in the ED are well established. However, recent studies have identified an association between ED opioid prescribing and long-term opioid use even with short-term prescriptions.9–12 This has led to an important reassessment of the long-term implications of exposing patients to opioids for the treatment of acute pain.
One approach to acute pain is the administration of opioids in the ED for symptom control to facilitate the evaluation of the etiology, and then discharge without a prescription as an attempt to mitigate the risk associated with prescription. The safety and effectiveness of this approach is not known. In addition, there has been a recent push for EDs to use alternatives to opioids whenever possible and even “opioid free EDs”13. To date there are no studies that quantify the future risk of ongoing use after a brief exposure to opioids in the ED. To address this knowledge gap, we measure the association between opioid administration in the ED to opioid naïve patients with back pain and ongoing opioid use in the 6 months following their ED visit.
METHODS
Design
This is a retrospective cohort study of patients discharged from the ED with a diagnosis of back pain.
Setting
We studied a university–associated healthcare system in the Rocky Mountain Region. The system included an urban-academic hospital, an urban community hospital and three suburban community hospitals. The total number of ED visits in the system is approximately 500,000 annually.
Participants
We included adults aged 18–85 years discharged from a hospital-associated ED between October 1, 2013 and September 30, 2015 for back pain based on ICD-9 codes.14 Specific ICD-9 codes are included in Online Table 1. We did not include patients treated in freestanding EDs as opioid administration as prescribing was rare (<1%) suggesting that this population was substantially different from those seen in hospital associated EDs. As we were primarily interested in patients who began using opioids following their ED visit, we only included opioid-naïve patients (no opioid prescriptions in our state prescription drug monitoring program (PDMP) in the 6 months preceding their index ED visit).15 For patients with multiple ED visits during the study timeframe we only considered their first visit.
Variables
We collected the following clinical information: age, sex, race (American Indian and Alaska Native, Asian, Black or African American, Native Hawaiian and Other Pacific Islander, White or Caucasian, multiple race, other), ethnicity (Hispanic or non-Hispanic), ED where the visit occurred, insurance, length of stay, triage category defined as Emergency Severity Index (ESI) and pain scores. Race/ethnicity was dichotomized to Non-Hispanic White vs. other for analysis. Insurance was categorized as Medicaid, Medicare, private, uninsured and other, and ESI as 1–2, 3, and 4–5. We had four levels of our exposure variable: 1) No opioid administered in the ED and no opioid prescription at discharge(No opioid), 2) opioids administered in the ED but no prescription (ED opioid)n, 3) no opioids administered in the ED but patient given an opioid prescription (Prescription opioid) and 4) opioids given in the ED and an opioid prescription provided at discharge (ED+ prescription opioid). The no opioids group served as the primary comparator.
Data sources and measurements
We collected clinical information from the system-wide electronic health record (EHR; epic Madison, WI). Patient histories for filled controlled medication prescriptions in the PDMP were obtained from the State Department of Public Health and linked to the clinical information by an honest broker to produce a de-identified limited dataset that was used for all analysis. A description of the linking process is included in Appendix 2
Study size
A sample size of 1,774 subjects treated with opioids and 1,774 subjects not treated with opioids has 80% power to detect a 30% increased risk for ongoing opioid use assuming a risk of 10% for patients not treated with opioids. Our data abstraction team requested to pull data using a timeframe rather than number; based on prior work we estimated that 2 years would provide an adequate sample.
Quantitative variables
We defined ongoing opioid use as filled prescriptions in the PDMP representing a >90-day supply in the 180 days post ED index visit. This definition was modified from Barnett et al. [14] as we only had prescription histories for the 6 months following the ED visit. We also examined an alternative definition of >4 prescriptions in the 6 months following the ED visit.16 A history concerning for aberrant use was defined as opioid prescriptions filled from five or more prescribers and five or more pharmacies in a six-month period. 17
Statistical Methods
We used relative risk regression (general linear model with a binomial log link function) to examine the risk associated with each level of exposure to opioid (none, ED only, prescription only, and in ED + prescription) and ongoing opioid use. All models were adjusted for age, sex, and race/ethnicity of the patient and the hospital were the patient was seen. Data were collected using REDCAP (Nashville, TN) and all analyses were performed in R version 3.5.2 (2018–12-20). The stats package v.3.5.2 was used for all general linear regression.
We performed two exploratory analyses. First, severity of pain is one potential confounder of the association of ED opioid administration, prescriptions at discharge and ongoing opioid use. Pain scores were not universally measured in our cohort. Given this limitation, we examined ongoing use adjusted for baseline pain scores in the subset of patients with pain scores. We also re-examined the entire data set using imputed pain scores. Random forests were utilized to impute missing data using multiple (m=5) imputation by chained equations and analyses were repeated and pooled across all imputed data sets.18 Second, we examined if the association of opioid administration in the ED with ongoing opioid use was different for oral and parenteral opioids.
To determine the potential for residual confounding, we calculated E values for our primary outcomes. The E-value is defined as “as the minimum strength of association, on the risk ratio scale, that an unmeasured confounder would need to have with both the treatment and the outcome to fully explain away a specific treatment-outcome association, conditional on the measured covariates” 18
Ethical review
Our Institutional Review Board (IRB) reviewed and approved the study. The study was conducted under a waiver of informed consent given the retrospective nature of data collection and no greater than minimal risk determination by IRB.
RESULTS
We identified 63,416 back pain visits throughout our system during the study period. The stratification of patients is show in Figure 1. Our final sample included 24,487 opioid naïve patients discharged from a hospital-associated ED following a back pain-related visit. Our sample had a median age of 38 years, a slight female predominance and was largely non-Hispanic White (Table 1). Just over half of patients were in the no opioid group, while the remaining patients were roughly evenly split between the ED opioid, prescription opioid and ED+prescription opioid group. (Table 1). In the ED, 5,193 (21%) patients received only oral opioids and 4,779 (20%) patients received parenteral opioids. The distribution of use of each opioid was: oral oxycodone 36.1%, oral hydrocodone 17.3%, oral hydromorphone 0.7%, oral morphine 0.2%, injected morphine 34.6% and injected hydromorphone 18.8% (note: patients may have received more than 1 medication). At discharge the opioids prescribed were oxycodone 47%, hydrocodone 40%, and tramadol 11%. The median number of morphine milligram equivalent/day was 30 with a range of 2 to 250 and an IQR of 20 to 40. 89% of prescriptions were for 50 or less MME/day.
Figure 1.
Stratification of cases identified by our ICD-9 search.
Table 1.
Characteristics of opioid-naïve patients discharged from the ED with a diagnosis of back pain by opioid administration.
| All N = 24,487 | Not Prescribed/ Not Administered N = 9,985 | Not Prescribed/ Administered N = 2,487 | Prescribed/ Not Administered N = 4,530 | Prescribed/ Administered N = 7,485 | ||
|---|---|---|---|---|---|---|
| Gender | Female | 13,460(55) | 5,582(56) | 1,449(58) | 2,378(52) | 4,051(54) |
| Male | 11,027(45) | 4,403(44) | 1,038(42) | 2,152(48) | 3,434(46) | |
| Race/Ethnicity | Hispanic | 5,080(21) | 2,120(21) | 616(25) | 897(20) | 1,447(19) |
| Non-Hispanic Black | 4,047(17) | 2,021(20) | 463(19) | 675(15) | 888(12) | |
| Non-Hispanic White | 13,605(56) | 4,981(50) | 1,220(49) | 2,688(59) | 4,716(63) | |
| Other | 1,468(6) | 738(7) | 175(7) | 209(5) | 346(5) | |
| Missing | 287(1) | 125(1) | 13(1) | 61(1) | 88(1) | |
| Emergency Severity Index | 4–5 | 3,125(13) | 1,681(17) | 411(17) | 381(8) | 652(9) |
| 3 | 20,770(85) | 7,997(80) | 1,943(78) | 4,123(91) | 6,707(90) | |
| 1–2 | 592(2) | 307(3) | 133(5) | 26(1) | 126(2) | |
| Insurance | Medicaid | 7,215(29) | 3,093(31) | 760(31) | 1,324(29) | 2,038(27) |
| Private | 3,588(15) | 1,378(14) | 289(12) | 739(16) | 1,182(16) | |
| Uninsured | 5,326(22) | 2,289(23) | 593(24) | 982(22) | 1,462(20) | |
| Other | 5,124(21) | 1,954(20) | 488(20) | 941(21) | 1,741(23) | |
| Medicare | 3,233(13) | 1,270(13) | 357(14) | 544(12) | 1,062(14) | |
| Missing | 1(0) | 1(0) | 0(0) | 0(0) | 0(0) | |
| Age at index visit | Median (IQR) | 38(28.0–52.0) | 37.0(26.0–52.0) | 38.0(28.0–52.0) | 38.0(29.0–52.0) | 40.0(29.0–54.0) |
Using our primary outcome definition (>90-day supply in the 180 days post ED index visit) 15 575 (2%) patients went on to ongoing opioid use. The unadjusted absolute proportion of ongoing opioid use among patients with each level of exposure is shown in Table 2. Using our secondary definition (> 4 prescriptions in 6 months) the rate of ongoing use was high (4%)16, but the increased risk associated with each level of exposure was similar (Table 2). Only 148 (1%) of patients in our cohort met our definition of aberrant use 17. The number of subjects with aberrant use for each level of exposure is shown in Table 2.
Table 2.
The unadjusted absolute proportion of ongoing opioid use among patients with each level of exposure to opioids.
| Opioid Exposure | Aberrant Usea | >90 Day Supplyb | Four or More Rxc |
|---|---|---|---|
| All | 148 (1%) | 575 (2%) | 1,086 (4%) |
| Not Prescribed/ Not Administered | 13 (0%) | 130 (1%) | 260 (3%) |
| Not Prescribed/ Administered | 12 (0%) | 63 (3%) | 129 (5%) |
| Prescribed/ Not Administered | 49 (1%) | 132 (3%) | 243 (5%) |
| Prescribed/ Administered | 74 (1%) | 250 (3%) | 454 (6%) |
Aberrant use = Filled opioid prescriptions from five or more prescribers and pharmacies in a six-month period post visit.
> 90 day supply= Filled more than a 90 days supply in the 180 days post visit.
Four or more Rx = Filled four or more opioid prescriptions in the 30 to 180 days post ED visit.
Patients in the ED opioid and prescription opioid groups were both associated with an increased risk of ongoing opioid use (Table 3), and this risk persisted after adjustment for age, race and triage category (ESI). Given the small number of patients who went on to aberrant use, we were unable to perform an adjusted analysis for this outcome.
Table 3.
Association of department opioid administration and prescribing of opioids with ongoing use compared to patients who received no opioids. Adjusted for age, sex, race/ethnicity and emergency severity index of patient
| Crudeb | Adjustedab | |||||
|---|---|---|---|---|---|---|
| Exposure | RR | LCI | UCI | RR | LCI | UCI |
| Not Prescribed/Administered | 1.9 | 1.4 | 2.6 | 1.9 | 1.4 | 2.5 |
| Prescribed/Not Administered | 2.2 | 1.8 | 2.9 | 2.1 | 1.7 | 2.7 |
| Prescribed/Administered | 2.6 | 2.1 | 3.2 | 2.3 | 1.9 | 2.9 |
A total of 14,901 (58%) of patients had pain scores recorded. The majority of patients had pain scores six or greater (online appendix Figure 1). Patients with an ESI of 4 or 5 were less likely to have pain scores recorded while a higher proportion of non-Hispanic white patients had pain scores recorded (Online appendix Table 1). Among the subset of patients with pain scores recorded, the adjusted strength of the association between ED opioid and prescribed opioid and increased risk of ongoing use compared to no opioid was relatively unchanged compared to the entire data set: ED administration only 2.0 (95% CI 1.4 to 3.2), prescription only 1.8 (95% CI 1.2 to 2.6), ED administration and prescription 2.5 (95% CI 1.9 to 3.5).
As a secondary analysis, we explored potential differences in the risk of ongoing use between oral and parenteral opioids. Because filling a prescription at discharge was strongy associated with ongoing use, we measured the risk of ongoing use for oral and parenteral opioid administration during the ED visit in two strata: patients who filled an opioid prescription and patients who did not fill a prescription. Among patients who filled an opioid prescription, parenteral opioid administration (adjusted RR 1.1, 95% CI 0.9 to 1.4) and oral ED administration (adjusted RR 1.1, 95% CI 0.8 to 1.4) were similarly associated with ongoing use compared to the no opioid group.. If the patient did not receive a prescription, risks were also similar (adjusted RR 1.9, 95% CI 1.3 to 2.8 and adjusted RR 1.8, 95% CI 1.2 to 2.6 for oral and parenteral respectively vs. the no opioid group).
The calculated E values for the crude and adjusted associations between the administration of parenteral and oral opioid administration in the ED and ongoing opioid use were >3 for all levels of exposure and both outcome definitions suggesting that residual confounding is unlikely to account for the observed associations.
DISCUSSION
We found that both opioids administered in the ED and/or by prescription were associated with an increased risk of ongoing of opioid use among opioid naïve patients with back pain. This provides the first evidence that even a single dose of opioids in the ED may have downstream ramifications for our patients. By focusing on an opioid naïve population these results reinforce the importance of primary prevention, supporting a reduction in opioid exposures in the ED in addition to limiting the use of prescription opioids. Further, this identifies the need for future systematic evaluations of alternative nonopioid modalities for back pain in the ED.
Our findings are consistent with prior work demonstrating that opioid prescriptions for the short-term treatment of pain are associated with an increased risk of long-term opioid use. Prior studies have identified unexpectedly high rates of ongoing opioid use following prescription opioids for acute pain from minor surgical procedures 9, dental procedures 12, and orthopedic procedures 10. The absolute rate of ongoing use reported in these studies varies; this may be due to differences in the definition of ongoing use or differences in the conditions. Still these studies consistently identify an increased risk of long-term opioid use amongst patients treated with opioids for an acutely painful condition.
Specific to emergency medicine, the association of ED opioid prescribing and ongoing opioid use has been reported previously. Hoppe et al. studied multiple painful conditions 11 and Delgado et al. studied ankle sprains.16 The rate of opioid prescribing at discharge in the current study was similar to the overall rate reported for multiple ED painful conditions (47%) 11 and higher than that reported for ankle sprains (25%).16 The rate of long-term use in the current study using the definition of filling a greater than 90 day supply in the six months following the visit was much lower than that reported by Hoppe (12%) although this comparison is limited by different definitions of ongoing use (an opioid prescription within +/− 30 days of the 1 year anniversary of the ED visit). When we used the definition suggested by Delgado (> 4 scripts filled more than 30 and less than 180 days following the ED visit), we found a rate much higher than the 0.7% identified among patients treated for ankle sprain. The relative risk for ongoing opioid use when opioids were prescribed versus not prescribed was similar to that reported by Hoppe for a variety of painful conditions (OR 1.8). Interestingly both the Delgado and the current study found a surprisingly high rate of ongoing opioid use (approximately 1%) among patients who did not receive opioids for what are considered to be self-limited conditions. A recent study found a much lower rate of ongoing use (1%) using a definition of six prescriptions in 6 months. 19 However, this study suffers from a low enrollment rate (approximately 66%) and only 85% follow-up. Finally, a Canadian study found approximately 9% of patients had ongoing use at 2 months but they reported low rates of misuse,20 with many patients taking opioids for the pain that led to their ED visit. When considered in total, these studies suggest that an ED visit is a risk factor for long-term opioid use.
There is little information regarding the administration of opioids in the ED for the treatment of back pain. While the exact proportion of ED patients with back pain treated with parenteral opioids is not well quantified in the literature, a review of the most commonly used opioids suggests that the percentage is greater than 10%.1 This is consistent with the 20% observed in our study. Parenteral opioids offer several potential advantages over oral medications including more rapid onset and ease of titration. However, rapid increases in brain concentrations may increase the reinforcing effects that lead to long-term opioid use and abuse. 21 While we did not assess abuse, we found the risk of ongoing use among patients treated with parenteral opioids was similar when compared to patients given oral opioids in the ED. This suggests that when providers believe opioids are necessary, they can choose between oral and parenteral opioids based on clinical circumstances without being overly concerned about additional risk of ongoing use.
The long-term adverse effects of opioid use are well described. In addition to the well-publicized issues of overdose and opioid use disorder, long-term use is associated with increased risks of depression, hyperalgesia and decreased overall function.22 These long-term risks carry a significant personal and societal burden and discontinuing chronic opioid use is difficult. More than 50% of patients who received more than a 90-day supply will go on to continued use at 3 years.23 Therefore some have argued that the best course of action primary prevention by avoiding the initial exposure to opioids that can trigger the progression to long-term use. 24 This can be challenging for emergency providers caring for patients who present in acute pain and distress requesting relief, with limited time and resources. Opioids have historically been the standard of care for acute pain, but providers have not had the information necessary to appropriately assess the risks and benefits of their use. This project provides additional risk information that may assist in both shared decision-making and the development of ED analgesia protocols. While the absolute risk is small, patients should understand that what they expect to be a short-term treatment could progress to long-term use and the attendant risks of misuse, abuse and overdose. 23
As evidence of ongoing harm following an opioid exposure from an ED visit continues to emerge, there is need for the specialty of emergency medicine to reassess our reliance on opioids. As part of a responsible response to the opioid crisis, we need to continually systematically evaluate the impact of or ED opioids when compared to analgesic alternatives. This includes research on the efficacy and safety of non-opioid medications as well as addressing barriers to implementation of other treatments as emergency medicine shifts away from an opioid-centric paradigm. 13,25
LIMITATIONS
The retrospective design of our study introduces several limitations. We used data collected for clinical purposes that can increase the risk of misclassification. However, there is no reason to suspect any misclassification to systematically differ between groups. We only considered prescription opioids captured by our state PDMP. Patients who used opioids obtained without a prescription written in our state or who went on to use illicit opioids would be misclassified.
Finally, while we believe that the causal link between opioid exposure and future opioid use has face validity, we recognize that the lack of random treatment assignment has the potential for residual confounding. We explored this possibility using E-values and found that any potential confounder would need to have a very strong relationship (relative risk >3) to both our exposure and outcome. One potential confounder that might meet this threshold is severity of pain. While we cannot exclude severity of pain rather than opioid exposure as the causal factor, it is important to note that all subjects in our cohort were discharged from the ED suggesting that while severity may be a factor in determining if opioids were administered, none of the patients was felt to have pain severe enough to warrant admission. In addition, our limited scale analysis of patients for whom a pain score was recorded, the relative risk of ongoing use was not significantly associated with higher pain score.
There are also limitations to the external validity of our study. Our findings may not generalize to other types of pain. It is possible that other hospital systems may provide patients with different adjunct treatments (such as physical therapy in the ED or at follow-up) and these interventions may change the rate of ongoing opioid use. Finally, we found a substantial variation in the rates of opioid prescribing between our academic and community sites. There may also be differences between our hospital system and other systems.
CONCLUSION
For patients treated for back pain in the ED, both ED opioid administration and opioid prescriptions at discharge are associated with increased risks of ongoing opioid use, with the highest risk seen in the group of patients provided the combination of opioids in the ED and by prescription at discharge. Providers should consider this when providing analgesia in the ED and discuss this risk with patients when they are considering opioids for treatment of back pain.
Supplementary Material
Online Figure 1. Distribution of pain scores
Online Table 1. ICD-9 codes used to identify back pain subjects.
Online Table 2. Demographics of patients with and without pain score.
Online appendix 2. Linkage process for PDMP to patients.
Acknowledgements:
We would also like to acknowledge the Colorado Department of Public Health and Environment, The University of Colorado Health Data Compass and NIH/NCRR Colorado CTSI Grant Number UL1 TR002535.
Presented at SAEM Annual Meeting. Las Vegas, May 2019.
Funding: This project was funded by the U.S. Department of Defense- AFRL-RQKHC FA8650–17-2–6777. The content is the responsibility of the authors and do not necessarily reflect the official views or policy of the Colorado Department of Public Health and Environment, the Department of Defense or its Components, or the National Institute of Health.
Footnotes
COI: None
REFERENCES
- 1.Friedman BW, Chilstrom M, Bijur PE and Gallagher EJ, Diagnostic testing and treatment of low back pain in United States emergency departments: a national perspective, Spine (Phila Pa 1976), 2010, 35(24):E1406–1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chang AK, Bijur PE, Lupow JB and Gallagher EJ, Randomized clinical trial of the 2 mg hydromorphone bolus protocol versus the “1+1” hydromorphone titration protocol in treatment of acute, severe pain in the first hour of emergency department presentation, Ann Emerg Med, 2013, 62(4):304–310. [DOI] [PubMed] [Google Scholar]
- 3.Chang AK, Bijur PE, Meyer RH, Kenny MK, Solorzano C and Gallagher EJ, Safety and efficacy of hydromorphone as an analgesic alternative to morphine in acute pain: a randomized clinical trial, Ann Emerg Med, 2006, 48(2):164–172. [DOI] [PubMed] [Google Scholar]
- 4.Chang AK, Bijur PE, Campbell CM, Murphy MK and Gallagher EJ, Safety and efficacy of rapid titration using 1mg doses of intravenous hydromorphone in emergency department patients with acute severe pain: the “1+1” protocol, Ann Emerg Med, 2009, 54(2):221–225. [DOI] [PubMed] [Google Scholar]
- 5.Chang AK, Bijur PE and Gallagher EJ, Randomized clinical trial comparing the safety and efficacy of a hydromorphone titration protocol to usual care in the management of adult emergency department patients with acute severe pain, Ann Emerg Med, 2011, 58(4):352–359. [DOI] [PubMed] [Google Scholar]
- 6.Hewitt DJ, Todd KH, Xiang J, Jordan DM, Rosenthal NR and Investigators C-S, Tramadol/acetaminophen or hydrocodone/acetaminophen for the treatment of ankle sprain: a randomized, placebo-controlled trial, Ann Emerg Med, 2007, 49(4):468–480, 480 e461–462. [DOI] [PubMed] [Google Scholar]
- 7.Marco CA, Plewa MC, Buderer N, Black C and Roberts A, Comparison of oxycodone and hydrocodone for the treatment of acute pain associated with fractures: a double-blind, randomized, controlled trial, Acad Emerg Med, 2005, 12(4):282–288. [DOI] [PubMed] [Google Scholar]
- 8.Turturro MA, Paris PM and Larkin GL, Tramadol versus hydrocodone-acetaminophen in acute musculoskeletal pain: a randomized, double-blind clinical trial, Ann Emerg Med, 1998, 32(2):139–143. [DOI] [PubMed] [Google Scholar]
- 9.Alam A, Gomes T, Zheng H, Mamdani MM, Juurlink DN and Bell CM, Long-term analgesic use after low-risk surgery: a retrospective cohort study, Arch Intern Med, 2012, 172(5):425–430. [DOI] [PubMed] [Google Scholar]
- 10.Goesling J, Moser SE, Zaidi B, Hassett AL, Hilliard P, Hallstrom B, Clauw DJ, et al. , Trends and predictors of opioid use after total knee and total hip arthroplasty, Pain, 2016, 157(6):1259–1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hoppe JA, Kim H and Heard K, Association of emergency department opioid initiation with recurrent opioid use, Ann Emerg Med, 2015, 65(5):493–499 e494. [DOI] [PubMed] [Google Scholar]
- 12.Schroeder AR, Dehghan M, Newman TB, Bentley JP and Park KT, Association of Opioid Prescriptions From Dental Clinicians for US Adolescents and Young Adults With Subsequent Opioid Use and Abuse, JAMA Intern Med, 2019, 179(2):145–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goett R, Todd KH and Nelson LS, Addressing the Challenge of Emergency Department Analgesia: Innovation in the Use of Opioid Alternatives, J Pain Palliat Care Pharmacother, 2016, 30(3):225–227. [DOI] [PubMed] [Google Scholar]
- 14.Lisi AJ, Burgo-Black AL, Kawecki T, Brandt CA and Goulet JL, Use of Department of Veterans Affairs administrative data to identify veterans with acute low back pain: a pilot study, Spine (Phila Pa 1976), 2014, 39(14):1151–1156. [DOI] [PubMed] [Google Scholar]
- 15.Barnett ML, Olenksi AR and Jena AB, Opioid Prescribing by Emergency Physicians and Risk of Long-Term Use, N Engl J Med, 2017, 376(19):1896. [DOI] [PubMed] [Google Scholar]
- 16.Delgado MK, Huang Y, Meisel Z, Hennessy S, Yokell M, Polsky D and Perrone J, National Variation in Opioid Prescribing and Risk of Prolonged Use for Opioid-Naive Patients Treated in the Emergency Department for Ankle Sprains, Ann Emerg Med, 2018, 72(4):389–400 e381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Katz N, Panas L, Kim M, Audet AD, Bilansky A, Eadie J, Kreiner P, et al. , Usefulness of prescription monitoring programs for surveillance--analysis of Schedule II opioid prescription data in Massachusetts, 1996–2006, Pharmacoepidemiol Drug Saf, 2010, 19(2):115–123. [DOI] [PubMed] [Google Scholar]
- 18.VanderWeele TJ and Ding P, Sensitivity Analysis in Observational Research: Introducing the E-Value, Ann Intern Med, 2017, 167(4):268–274. [DOI] [PubMed] [Google Scholar]
- 19.Friedman BW, Ochoa LA, Naeem F, Perez HR, Starrels JL, Irizarry E, Chertoff A, et al. , Opioid Use During the Six Months After an Emergency Department Visit for Acute Pain: A Prospective Cohort Study, Ann Emerg Med, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Daoust R, Paquet J, Gosselin S, Lavigne G, Cournoyer A, Piette E, Morris J, et al. , Opioid Use and Misuse Three Months After Emergency Department Visit for Acute Pain, Acad Emerg Med, 2019, 26(8):847–855. [DOI] [PubMed] [Google Scholar]
- 21.Bioavailability of drugs to the brain and the blood brain barrier, NIDA Res Monogr, 1992, 120:1–258. [PubMed] [Google Scholar]
- 22.Deyo RA, Von Korff M and Duhrkoop D, Opioids for low back pain, BMJ, 2015, 350:g6380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martin BC, Fan MY, Edlund MJ, Devries A, Braden JB and Sullivan MD, Long-term chronic opioid therapy discontinuation rates from the TROUP study, J Gen Intern Med, 2011, 26(12):1450–1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Duncan RW, Smith KL, Maguire M and Stader DE 3rd, Alternatives to opioids for pain management in the emergency department decreases opioid usage and maintains patient satisfaction, Am J Emerg Med, 2019, 37(1):38–44. [DOI] [PubMed] [Google Scholar]
- 25.Todd KH, A Review of Current and Emerging Approaches to Pain Management in the Emergency Department, Pain Ther, 2017, 6(2):193–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Online Figure 1. Distribution of pain scores
Online Table 1. ICD-9 codes used to identify back pain subjects.
Online Table 2. Demographics of patients with and without pain score.
Online appendix 2. Linkage process for PDMP to patients.