Abstract
Ozone pollution is a known respiratory irritant, yet we do not fully understand the magnitude or timing of respiratory effects based on short-term exposure. We investigated the associations between ambient ozone concentrations and respiratory symptoms as measured by healthcare utilization events. We used comprehensive electronic health records to identify respiratory responses to changes in ambient ozone levels. We constructed a dataset from Kaiser Permanente Mid-Atlantic States (KPMAS) that included information on 2013 and 2014 daily utilization rates for a broad range of healthcare utilization – nurse calls/emails, provider visits, emergency department and urgent care visits (ED/UC) and hospital admissions – by census block. We used 8-hour average ozone concentrations collected from 48 air monitoring stations in the region via the Air Data database of the USEPA. We estimated the association between changes in ambient ozone (exposure windows of current day, 1-day lag and 3-day moving average) and changes in healthcare utilization using linear regression controlling for census tract-level socioeconomic indicators and temperature. Increases in ozone were associated with increases in three of the four utilization event types. A 10 ppb increase in 1-day ozone was associated with a 2.95% (95% CI: 1.93%, 3.96%) increase in calls/emails, a 1.56% (95% CI: 0.38%, 2.74%) increase in ED/UC visits and a 1.10% (95% CI: 0.48%, 1.73%) increase in provider visits. We did not find associations between ozone and hospital admissions. Proportionally, highest effects were found for nurse calls/emails possibly indicating a high number of mild effects that may be underreported in studies that examine only ED visits or hospital admissions.
Keywords: ozone, electronic health records, respiratory, healthcare, hospital, air pollution
1. INTRODUCTION
Respiratory disease is a common cause of morbidity across the globe (Forouzanfar et al., 2015). In a recent global burden of disease estimate for 2015, there were 3.6 million deaths and 90.1 million DALYs (disability-adjusted life years) attributable to asthma and chronic obstructive pulmonary disease (COPD). A percentage of this burden is explained by ambient levels of air pollution, including ozone (Soriano et al., 2017). The mechanism by which exposure to ozone can result in short-term respiratory effects and the development of chronic respiratory conditions is well established. Ozone is a potent oxidizer and pulmonary irritant causing an inflammatory response in the lungs as well as a cascade of subsequent responses (Arjomandi et al., 2018; Tager et al., 2005). Numerous epidemiological studies have identified associations between ozone exposure and the development of asthma, acute bronchitis and COPD) (Laumbach and Kipen, 2012; Magzamen et al., 2017; Strosnider et al., 2018; Viegi et al., 2006). Climate change is expected to increase ozone concentrations as well as the number of high ozone days in urban areas around the globe, potentially heightening adverse impacts on respiratory health (Fann et al., 2015; Wilson et al., 2017). Although researchers have measured adverse effects of ozone exposure, we do not fully understand the severity, magnitude or timing of impact in metropolitan areas. Preparation of local healthcare systems is necessary to provide adequate care now and into the future, especially for susceptible populations such as children and the elderly.
Much of the existing knowledge on ozone and short-term respiratory effects has been gained through studies using data from emergency department visits and hospital admissions (Slaughter et al., 2005; Winquist et al., 2012; Zheng et al., 2015). These studies are well designed to measure acute exacerbations that require emergency care but could miss milder effects that require non-urgent care. Evaluation of respiratory effects of ozone exposure through the lens of syndromic surveillance, instead of health endpoints, may allow us to understand the health burden more effectively.
Syndromic surveillance identifies changes in disease activity using either clinical features detected before disease diagnosis is confirmed or activities prompted by the onset of symptoms (Buehler et al., 2004). Surveillance uses data on healthcare care utilization such as hospital admissions; visits to the emergency department and urgent care facilities; healthcare provider visits; as well as nurse advice calls and emails. Both severe and minor respiratory effects can be captured using these data sources. The monitored data can help to understand multiple facets of health burden including the timing of a syndromic response; syndromic features; syndromic intensity; geographic location and spread.
KPMAS is one of eight regions of the Kaiser Permanente Medical Care Program, a federally qualified, prepaid group health maintenance organization (HMO) and the largest non-governmental health care provider in the world, making it a useful entity within which to explore these questions. KPMAS has approximately 700,000 members in northern Virginia, District of Columbia, suburban Maryland, and Baltimore (“DMV”). We collected data on environmental pollutants and irritants including nitrogen dioxide, particulate matter, ozone, grass pollen and tree pollen in order to explore associations with respiratory symptoms. Previous analysis of data in this cohort has revealed associations between ambient fine particle levels (particulate matter < 2.5 microns in aerodynamic diameter [PM2.5]) and healthcare utilization events. Current-day levels of PM2.5 were associated with increased emergency department (ED) and urgent care (UC) visits, provider visits, and nurse calls/emails (Fuller et al., 2019). In the current study, we investigated associations between short-term changes in ambient ozone concentrations and adverse respiratory symptoms. Our primary hypothesis was that increases in ozone concentrations would correspond to higher healthcare utilization events including nurse calls/emails, provider visits, ED/UC, visits and hospital admissions. Our secondary hypothesis was that the effect of ozone would be greatest for nurse calls/emails compared to other events such as emergency department visits.
2. METHODS
2.1. Study Design
We collected information from Kaiser Permanente Mid-Atlantic States (KPMAS) databases on routine care of its members for two years: January 1 2013 through December 31 2014. We restricted our analysis to KPMAS members who resided in the greater Washington, DC area including the counties of Montgomery, Prince George’s, Arlington, Fairfax, Loudon, Alexandria, Fairfax, Falls Church, Fredericksburg, and the District of Columbia. All data were de-identified, and therefore, informed consent was not required. Institutional review boards from KPMAS and Georgia State University approved the study.
2.2. Healthcare utilization data
We focused our analysis on utilization events associated with ICD-9-CM diagnosis codes for likely respiratory issues. These codes are based on the symptoms that are clearly linked to a respiratory condition when a member interacts with his/her provider. These included 102 unique codes such as 460 acute nasopharyngitis, 466.0 acute bronchitis, and 493.82 cough variant asthma. We categorized utilization events into four event types that represented different points of contact with the healthcare system. The event types were nurse calls/emails, provider visits, ED/UC visits and hospital admissions. In the case of multiple visits, a patient was counted only once per event type on a single day. This outcome occurred rarely in our dataset. Descriptions of each of the event types are given below:
Nurse calls/emails:
Many participants choose to access assistance through nurse calls or email. These services are available 24 hours per day, 7 days per week. We combine these two utilization events into this event type, because they provide similar levels of support and are utilized to address similar symptoms.
Provider visits:
This category specifies outpatient provider face-to-face visits with a nurse or physician that is not an ED/UC visit. This service is available at all KPMAS facilities, which are generally accessible Monday through Friday from 8 am to 6 pm.
Emergency department/ urgent care (ED/UC):
These two visit types are grouped together for our analysis due to the similarity among conditions treated. Emergency department care is provided through contracts with 11 hospitals in the region and is available 24 hours a day/ 7 days per week. Urgent care is available after hours (generally after 6 pm on weekdays) and on weekends at 10 of the 29 primary care medical offices.
Hospital admissions:
In-patient services are provided by the same 11 hospitals in the region that also provide ED care and reflects the most severe health events.
2.3. Data aggregation
Each utilization event was assigned to a census block from the 2010 U.S. Census based on the member’s residence and a day in the sample period. The denominator for event rate was defined by the number of KPMAS members with residence in a particular census block as of December 31, 2013. Our unit of analysis was the census block for which we calculated the number of KPMAS beneficiaries with a healthcare utilization event per 100,000 KPMAS beneficiaries per day (henceforth referred to as the utilization rate). In order to protect the privacy of KPMAS members, any census block with 5 or fewer total members during the sample period was censored from the dataset. There were separate counts for each of the four event types by day.
2.4. Ozone concentrations and temperature
Data on ambient ozone concentrations were obtained from 48 air monitoring stations in the region via the Air Data database within the Air Quality System (AQS) of the USEPA (US Environmental Protection Agency, 2019). We restricted our analysis to the months April through September, when there is the greatest variation in ambient ozone levels. Concentrations during the other months of the year are typically low, with little variation, making it difficult to see any effects (Babin et al., 2008; Vingarzan, 2004). The data represented 8-hr maximum concentrations for each date and location following USEPA guidance (US Environmental Protection Agency, 1998). Some monitors did not collect data each day; therefore, we assigned a measurement from the closest station with a non-missing measurement. We restricted the assignment of ozone measurements within 10 km of each block to reduce exposure misclassification (Jiang and Yoo, 2018; Punger and West, 2013).
We considered daily temperature as a potential confounder in our models. Daily average temperature data was collected from 16 weather monitors in Virginia and Maryland from the National Oceanic and Atmospheric Administration Climate Data Online system (National Oceanic and Atmospheric Association, 2019). As with the EPA monitors, weather monitors have missing measurements for some days in our sample period, so census blocks may use measurements from different weather stations on different days within the study period. We assigned the temperature from the closest weather monitor with a non-missing measurement on each day.
2.5. Statistical Analysis
We evaluated the association between changes in ambient pollutants and the utilization rate using linear regression. We first created unadjusted models including only ozone as the independent variable and then built adjusted models that included significant predictors and potential confounders. We evaluated temperature and 2010 U.S. Census tract-level socioeconomic status (SES) indicators as potential confounders. SES indicators included: percent of households below the poverty level; percent of households receiving public assistance; percent of households with annual income below $30,000; percent of working age adults not in the labor force; percent of adults with a high school education or less; median household income; and median home value. We evaluated the potential for lagged effects of ambient ozone concentrations by devising three model specifications including current-day ozone concentration, 1-day lag and 3-day moving average (MA). The 3-day MA is the average of day lags 0, 1 and 2.
The functional form of the final adjusted model is:
| (1) |
Where Y is the utilization event for census block “i” on day “j” in the study sample. Ozone is the ambient concentration in the selected time window (i.e. current day, 1-day lag, 3-day MA). The primary effect estimate of interest is b(1) – the association of exposure with response. SESi is the array of census tract socioeconomic indicators described above (e.g. median household income). SES indicators differ across census blocks but are invariant by day. Included also are sets of indicators for DOW (day of the week), Month, and Year, as well as variables for Temp and Temp2 (temperature and temperature squared). DOW, month, and year vary by date. The letter eij is an error term representing random variation for each of the Census blocks “i” on day “j”. The number of KPMAS members varied substantially by census block; thus, observations were weighted by the mid-year KPMAS member count in each census block.
We conducted additional analyses exploring the sensitivity to model specification and categorization of the outcome. First, we ran a distributed lag model including current-day, one-day and two-day lags. Second, we ran adjusted models including a more comprehensive definition of respiratory events that included both likely and possibly respiratory events. Possibly respiratory events included any code that identifies a possible response that may be linked to a respiratory condition or event in a secondary way, such as an ophthalmic or dermatologic response. These included 182 unique codes, in addition to the 102 previously identified codes.
3. RESULTS
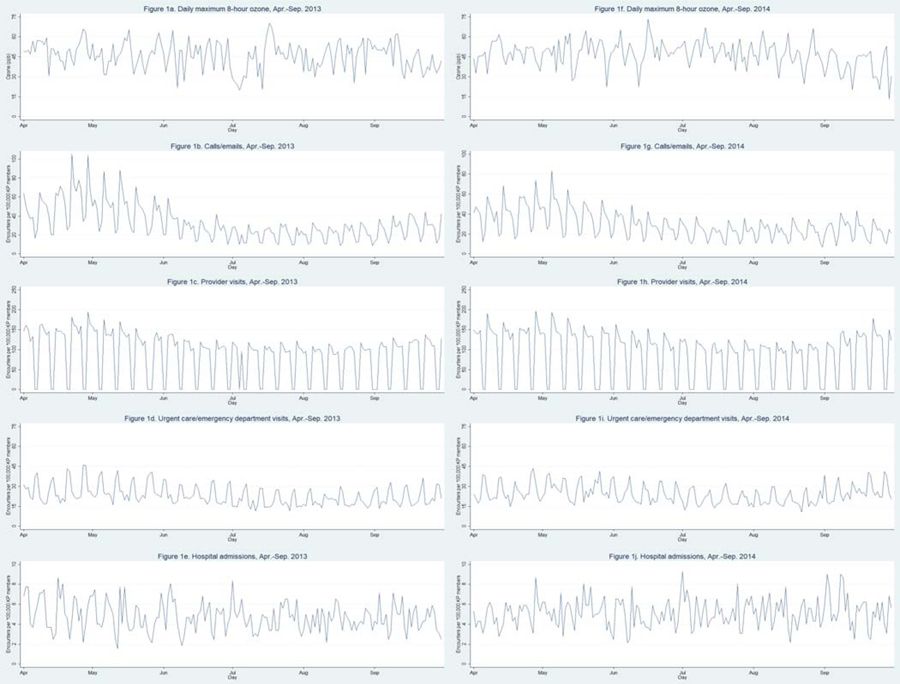
Mean ozone levels were comparable to those reported by Babin et al. (Babin et al., 2008; Babin et al., 2007) in a study of the DMV area. Mean ozone concentration during the study period was 46.1 ppb (SD: 1.1 ppb). The mean distance of members to ozone monitors was 7.4 km (SD: 4.0 km). Figure 1 is a collection of time-series plots of daily ozone and utilization events for 2013 and 2014. There was weekly variation in calls/emails and provider visits with higher rates during the week compared to weekends, while the opposite is generally true for ED/UC visits. The dataset including the months of April through September 2013 and 2014 contained 6,182,104 member-days and 173,527 respiratory events (Table 1). The mean utilization rates 31.0 (SD: 29.9) for calls/emails, 87.4 (SD: 59.8) for provider visits, 23.7 (SD: 25.5) for ED/UC visits, and 4.9 (SD: 16.3) for hospital admissions.
Figure 1:
Time-series plots of daily 8-hr ambient ozone concentrations and healthcare utilization event rates in the Kaiser Permanente Mid-Atlantic States (KPMAS) for April through September 2013 and 2014.
Table 1.
Distribution of healthcare utilization events for respiratory symptoms in the Kaiser Permanente Mid-Atlantic States (KPMAS): April through September, 2013 and 2014
| Event type | No. of events | Events per day/100,000 members Mean (SD) |
|---|---|---|
| Calls/Emails | 36,601 | 31.0 (29.9) |
| Provider Visits | 103,104 | 87.4 (59.8) |
| ED/UC visits | 28,008 | 23.7 (25.5) |
| Hospital Admissions | 5,814 | 4.9 (16.3) |
Table 2 and Figure 2 display O3 level effect estimates on the utilization rates of the 4 healthcare utilization event types and for each of the 3 model specifications. The changes according to healthcare utilization event type are given for each of the selected exposure periods: current-day lag (Model A); 1-day lag (Model B) and 3-day MA (Model C). Models are adjusted for potential confounders including day of the week, month, year, percent of adults with a high school education or less, median household income, temperature, and temperature squared. A 1-day lag in exposure was associated with a statistically significant (p < 0.05) increase in utilization rate for calls/emails (0.09 [95% CI: 0.06 – 0.12]), provider visits (0.10 [95% CI: 0.04 – 0.15]), and ED/UC visits (0.04 [95% CI: 0.01 – 0.06]), but not hospital admissions. Also, a 3-day MA was associated with increases in utilization rates of calls/emails (0.11 [95% CI: 0.06, 0.15]) and provider visits (0.13 [95% CI: 0.06, 0.21]).
Table 2:
Difference in daily event rates for likely respiratory symptoms per 100,000 members associated with selected ozone metrics within the Kaiser Permanente Mid-Atlantic States (KPMAS), 2013 and 2014
| Calls/Emails | Provider Visits | ED/UC Visits | Hospital admissions | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model A | Model B | Model C | Model A | Model B | Model C | Model A | Model B | Model C | Model A | Model B | Model C | |
| Current day | 0.011 | -- | -- | –0.029 | -- | -- | 0.005 | -- | -- | –0.005 | -- | -- |
| 95% CI | (–0.020, 0.042) | -- | -- | (–0.084, 0.026) | -- | -- | (–0.023, 0.033) | -- | -- | (–0.018, 0.007) | -- | -- |
| 1-day lag | -- | 0.091 | -- | -- | 0.096 | -- | -- | 0.037 | -- | -- | –0.01 | -- |
| 95% CI | -- | (0.060, 0.123) | -- | -- | (0.042, 0.151) | -- | -- | (0.009, 0.065) | -- | -- | (–0.023, 0.002) | -- |
| 3-day MA | -- | -- | 0.108 | -- | -- | 0.134 | -- | -- | 0.038 | -- | -- | –0.009 |
| 95% CI | -- | -- | (0.065, 0.152) | -- | -- | (0.058, 0.209) | -- | -- | (–0.002, 0.078) | -- | -- | (–0.027, 0.009) |
Notes: Bold font represents statistically significant effect estimates; MA, moving average; CI, confidence interval
Models are adjusted for potential confounders including day of the week, month, year, percent of adults with a high school education or less, median household income, temperature and temperature-squared.
Figure 2:
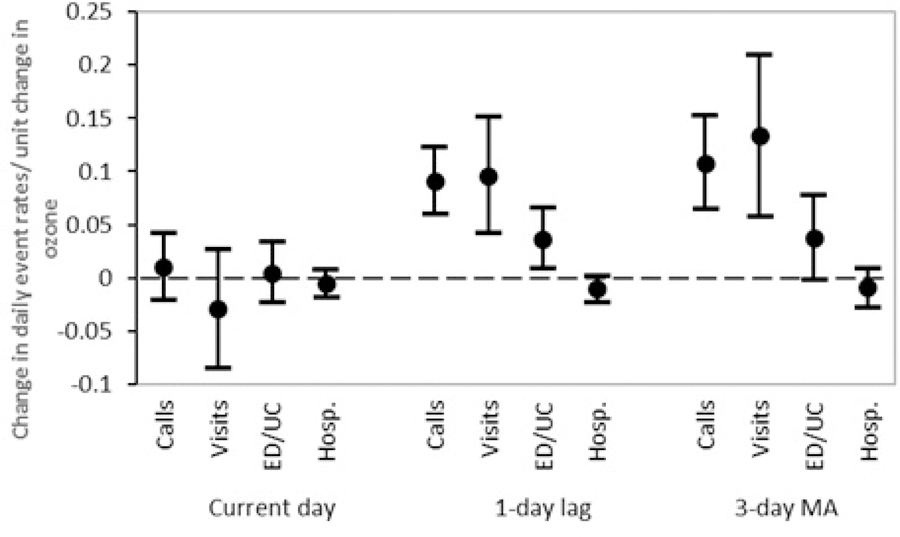
Change in healthcare utilization event rate per unit change in ambient 8-hour ozone concentration within the Kaiser Permanente Mid-Atlantic States (KPMAS), 2013 and 2014
Given that a 1-unit change in ozone is small and may be difficult to interpret, we scaled the results. Table 3 shows the absolute and percent change in utilization rates based on an interquartile range increase, a 5 ppb increase, and a 10 ppb increase in 1-day lag and 3-day MA ozone. The relationship between absolute and percent increase relies on the underlying utilization event rate, which varies by type. For example, a small absolute difference may be a large relative difference if the average event rate is low. A 10 ppb increase in 1-day ozone was associated with utilization rate increases of 2.95% (95% CI: 1.93%, 3.96%) in calls/emails, 1.56% (95% CI: 0.38%, 2.74%) in ED/UC visits and 1.10% (95% CI: 0.48%, 1.73%) in provider visits. Associations for a 10 ppb increase in 3-day MA ozone were 3.495% (95% CI: 2.079%, 4.910%) for calls/emails and 1.529% (95% CI: 0.667%, 2.391%) for provider visits. The same change in 3-day MA ozone results in a 1.605% (95% CI: −0.088%, 3.298%) increase in ED/UC, however, the confidence intervals include zero.
Table 3:
Change in daily utilization events for likely respiratory symptoms associated with increased in 1-day lag and 3-day moving average (MA) ozone concentration within the Kaiser Permanente Mid-Atlantic States (KPMAS) membership, 2013 and 2014
| Change in ozone | Calls/Emails | 95% CI | Provider Visits | 95% CI | ED/UC Visits | 95% CI | Hospital Admissions | 95% CI |
|---|---|---|---|---|---|---|---|---|
| 1-day Lag Ozone | ||||||||
| Absolute change in daily event rates per 100,000 Patients | ||||||||
| 0.98 ppb (IQR) | 0.09 | (0.06,0.12) | 0.09 | (0.04,0.15) | 0.04 | (0.01,0.06) | −0.01 | (−0.02,0.00) |
| 5.00 ppb | 0.46 | (0.30,0.61) | 0.48 | (0.21,0.75) | 0.18 | (0.04,0.32) | −0.05 | (−0.11,0.01) |
| 10.0 ppb | 0.91 | (0.60,1.23) | 0.96 | (0.42,1.51) | 0.37 | (0.09,0.65) | −0.10 | (−0.23,0.02) |
| Percent change in daily event rates per 100,000 Patients | ||||||||
| 0.98 ppb (IQR) | 0.29% | (0.19%,0.39%) | 0.11% | (0.05%,0.17%) | 0.15% | (0.04%,0.27%) | −0.20% | (−0.47%,0.04%) |
| 5.00 ppb | 1.47% | (0.97%,1.98%) | 0.55% | (0.24%,0.86%) | 0.78% | (0.19%,1.37%) | −1.05% | (−2.35%,0.24%) |
| 10.0 ppb | 2.95% | (1.93%,3.96%) | 1.10% | (0.48%,1.73%) | 1.56% | (0.38%,2.74%) | −2.13% | (−4.73%,0.47%) |
| 3-day MA Ozone | ||||||||
| Absolute change in daily event rates per 100,000 Patients | ||||||||
| 0.98 ppb (IQR) | 0.11 | (0.06,0.15) | 0.13 | (0.06,0.20) | 0.04 | (−0.01,088) | −0.01 | (−0.03,0.01) |
| 5.00 ppb | 0.54 | (0.323,0.762) | 0.67 | (0.29,1.04) | 0.19 | (−0.00,0.39) | −0.05 | (−0.14,0.04) |
| 10.0 ppb | 1.08 | (0.64,1.52) | 1.34 | (0.58,2.09) | 0.38 | (−0.02,0.78) | −0.09 | (−0.27,0.09) |
| Percent change in daily event rates per 100,000 Patients | ||||||||
| 0.98 ppb (IQR) | 0.34% | (0.20%,0.48%) | 0.15% | (0.06%,0.23%) | 0.16% | (−0.01%,0.32%) | −0.18% | (−0.55%,0.18%) |
| 5.00 ppb | 1.75% | (1.04%,2.46%) | 0.76% | (0.33%,1.20%) | 0.80% | (−0.04%,1.65%) | −0.93% | (−2.76%,0.91%) |
| 10.0 ppb | 3.49% | (2.08%,4.91%) | 1.53% | (0.67%,2.39%) | 1.60% | (−0.09%,3.30%) | −1.85% | (−5.54%,1.85%) |
Notes: Bold font represents statistically significant effect estimates; MA, moving average; CI, confidence interval
Models are adjusted for potential confounders including day of the week, month, year, percent of adults with a high school education or less, median household income, temperature and temperature-squared.
3.1. Sensitivity Analysis
We conducted two sensitivity analyses, the first of which was specifying a distributed lag model for each utilization event type. Results are given in the supplementary material (Supplementary Table 1). The distributed lag models combine current-day, 1-day lag and 2-day lags together. In distributed lag models, 1-day lag ozone concentration was a consistent predictor of changes in calls/emails (0.085 [95% CI: 0.049, 0.120]), provider visits (0.086 [95% CI: 0.024, 0.149]) and ED/UC visits (0.038 [95% CI: 0.007, 0.070]) when controlling for the other exposure periods. The 1-day lag in ozone was also associated with the largest magnitude of effect for calls/emails and ED/UC visits. However, a 2-day lag in ozone (0.107 [95% CI: 0.052, 0.163]) was the greatest effect seen for provider visits. There were no statistically significant associations with hospital admissions.
The second sensitivity analysis added possibly respiratory events to the models (Supplementary Table 2). Effect estimates for 1-day lag and 3-day MA increase in ozone for calls/emails increased in magnitude and the current day lag became significant. Provider visits also increased for a 1-day lag and 3-day MA. However, the opposite effect was seen for ED/UC visits for which the effect estimates were smaller than in the main analysis.
4. DISCUSSION
The overall objective of our study was to measure the relationship between short-term changes in ambient ozone concentrations and respiratory symptoms as represented by respiratory-related healthcare utilization in a comprehensive electronic medical record system. We believe that our study is the first to address a wide range of utilization events linked to respiratory symptoms in this way. We identified associations between ambient ozone and increases in calls/emails, provider visits and ED/UC visits associated with respiratory symptoms. A 10 ppb change in 1-day lag ozone was associated with an approximately 3% change in utilization rate for calls/emails, 1.6 % for ED/UC visits, and a 1.1% for provider visits. Across all 700,000 KPMAS beneficiaries this equates to an increase of approximately 6.4 calls/emails (from 217.0 to 223.4), 2.6 ED/UC visits (from 165.9 to 168.5), and 6.7 provider visits (from 611.8 to 618.5) per day. The highest effect was a 3.5% change in calls/emails corresponding to a 3-day MA ozone increase of 10 ppb. This equates to an additional 7.6 calls/email per day (from 217.0 to 224.6) for KPMAS beneficiaries. The largest changes were seen in calls/emails compared to ED/UC visits, which are more widely studied. We did not find evidence of associations between ozone and respiratory-related hospital admissions. A distributed lag analysis revealed that the timing associated with the highest magnitude of effect was a 1-day lag for both calls/emails and ED/UC visits, which indicates that high exposure the previous day (perhaps in the evening) may lead to adverse respiratory symptoms and healthcare contact the following day. Provider visits are highest for a 2-day lag, which may incorporate a delay in scheduling an appointment with a nurse or physician.
We can compare our findings to other similar studies which overwhelmingly focus on emergency room visits and hospital admissions. Some incorporate all respiratory disease while others focus on asthma-related diagnoses exclusively. A comprehensive study of the association between daily changes in ambient ozone on ED visits across the U.S. found statistically significant associations. A review and meta-analysis of 71 studies identified a small risk ratio of 1.009 (95%CI: 1.006, 1.011) and a population attributable fraction of 0.8 (95%CI: 0.6, 1.1) of ambient ozone levels on increased asthma ED visits and hospital admissions. Specifically, the rate ratio for an interquartile change in ozone (16.54 ppb) was 1.039 (95%CI: 1.036, 1.042) (Strosnider et al., 2018). A separate study identified associations between ozone and respiratory hospital admissions for a 3-day lag exposure, but not for lags between 0 and 2 days in 3 counties in Washington State (Magzamen et al., 2017). The relative risks for the counties were 1.04 (95% CI: 1.02, 1.07), 1.03 (95% CI: 1.01, 1.05) and 1.02 (95% CI: 1.01, 1.03) for Clark, Spokane and King Counties, respectively. We failed to find any association between 0–2 day lags or a 3-day moving average of ozone with hospital admissions. It is possible that an effect of ozone on hospital admissions is not evident until later time periods.
Fewer studies evaluate provider visits. Babin et al. investigated the effect of ozone on Medicaid-related acute care visits in the metropolitan DC area (2008). They identified a statistically significant 0.9% (95%CI: 0.2, 1.7) increase in acute care visits for respiratory events for each 10 ppb increase in ozone among all participants and a borderline significant 1.9% (95%CI: 0, 2.4) increase for persons aged 21–49. The majority, but not all studies identified positive associations, as is evident from a recent study in Shanghai, China, in which researchers found no relationship between ozone and respiratory outpatient visits during warm periods, but an inverse association during cool periods (Wang et al., 2018). It may be possible that these associations are confounded by co-pollutants that display the opposite temporal variation as ozone. It is important to note that the studies listed here vary in terms of the time period included in analyses, modeling approaches and ambient levels of ozone.
Our findings may reflect the way we identified respiratory events and how we classified them into 4 categories. The results suggest a greater sensitivity of calls/emails as an indicator of respiratory symptoms due to ambient ozone concentrations. Calls/emails are typically utilized more frequently for mild symptoms, which may often be missed in studies that include only ED/UC visits and hospital admissions. Although symptoms may be mild, it is possible that they can have broader effects such as lost school and work days (Fann et al., 2015). Our investigation focused on short-term effects within a few days of change in ambient ozone concentration. The main results and sensitivity analyses showed the greatest effects for a 1-day lag in exposure for two of the utilization events, revealing its importance relative to other exposure periods. It is possible that an effect on the other utilization events may not emerge until later.
Research has shown that background ozone levels have increased over the past 100 years and are expected to continue on this path (Vingarzan, 2004). Local anthropogenic inputs of precursor pollutants heighten ozone concentrations even further, especially in urban areas. Health effects are also expected to increase in the future causing greater pressures on the healthcare system. Thus, the ozone related healthcare impacts explored in this study will have economic impacts as well. It is estimated that future ozone levels will result in between $320 million and $15 billion in additional costs to address the associated morbidity and mortality in the U.S. (Fann et al., 2015).
A strength of this study is the assessment of effect over a major metropolitan region of the United States. However, there is the possibility for exposure misclassification using central site data to approximate personal exposure. Evidence has shown that this methodology is appropriate given that ozone is a regional pollutant with similar concentrations within a region (Punger and West, 2013). We restricted our analysis to Census blocks within 10 km (6.2 miles) of a monitor to reduce exposure misclassification.
Several studies of healthcare utilization have noted different effect sizes based on age, with higher effects typically among younger populations (Babin et al., 2008; Babin et al., 2007; Wang et al., 2018; Zheng et al., 2015). We were unable to fully explore potentially susceptible sub-populations such as children or adults with chronic conductions due to use of an aggregated dataset. We found that data aggregation and IRB requirements of nullifying cells with five or fewer patients (which for these analyses would be five or fewer patients with the specific condition) removed many census blocks – creating potential bias in analyses. Future research can investigate possible strategies to address this issue such as aggregating data by adjacent census blocks. Therefore, we suspect that our present analysis should be viewed as a conservative estimate of the impact of ozone on utilization events, given that we were unable to assess potentially susceptible subpopulations.
This study is ecological in nature and therefore we sought to address potential confounders at the group level. The existence of co-pollutants is a limitation that we explored. Co-pollutants including particulate matter, nitrogen dioxide, tree and grass pollen, could confound associations between ozone and respiratory events. In order to evaluate this possibility, we measured the daily variation between these variables and ozone (analyses not shown); however, we did not identify significant correlations. Therefore, we conclude that any potential effect of the other pollutants on our results would be small. With regards to outcome measurement, we are confident that the lists of nurse protocol numbers and ICD-9-CM codes defining a respiratory-related event are adequate based on prior literature and established assignment in the healthcare field. However, we did not ascertain if the coding was sensitive and specific and there remains the possibility of misclassification of our outcome variables. There is also the possibility of residual confounding by unmeasured variables; however, we believe that we have captured the most important confounders. Another potential confounder is the availability of services that define a specific event type. KPMAS, as with most healthcare systems, limits provider visits to Monday through Friday, typically between 8 am and 6 pm. For this reason, we included fixed effects for day of the week into the model specifications. This helped to account for the possibility that in the event of a spike in an allergen on a weekend, there could be no increase in provider visits since that service was not available at the time of a spike.
Another important confounder, which we did not measure, is patient preference for alternative services. Preferences might be informed by insurance status, access to services, perceptions of urgency or severity, and perceptions of the value of alternative service options. For example, rather than calling an advice nurse when experiencing symptoms, selected patient subgroups might prefer booking a same day appointment with a provider because they have an established relationship with their primary care provider, prefer a face-to-face visit, or have a low office visit copayment. We have accounted for several community-level socioeconomic variables that may drive some measure of these preferences.
5. CONCLUSIONS
In summary, we used a comprehensive electronic health record system to evaluate associations between ambient ozone pollution and respiratory effects across a broad range of healthcare utilization types. Our results show associations between ambient ozone levels and increases in calls/emails, provider visits and emergency department visits for adverse respiratory symptoms among patients of a large healthcare program. We found the highest effects between ambient ozone levels and nurse calls/emails, revealing the importance of future assessment of this type of utilization event. Our findings indicate the usefulness of utilizing previously little-studied data to understand relationships between air pollution and respiratory health.
Supplementary Material
Highlights.
Ozone is a respiratory irritant, but we don’t understand the full scope of effects
We estimated the association between changes in ozone and healthcare utilization
An increase in calls/emails, provider visits and emergency care were linked to ozone
Highest percent effects were found for calls/emails, an understudied data source
Acknowledgements
Funding was provided by the Atlanta Clinical Trials and Science Institute” (ACTSI), Health Innovations Program, Preliminary Study Grant through the National Center for Advancing Translational Sciences of the National Institutes of Health under award number UL1TR002378. We would also like to thank Nolan Johnson, Alphonse Derus and Suma Vupputuri for their input at the beginning of the project and Dr. Howard Burkom and Dr. Steven Babin for feedback on the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
REFERENCES
- Arjomandi M, et al. , 2018. Respiratory Responses to Ozone Exposure. MOSES (The Multicenter Ozone Study in Older Subjects). Am J Respir Crit Care Med. 197, 1319–1327. [DOI] [PubMed] [Google Scholar]
- Babin S, et al. , 2008. Medicaid patient asthma-related acute care visits and their associations with ozone and particulates in Washington, DC, from 1994–2005. Int J Environ Health Res. 18, 209–21. [DOI] [PubMed] [Google Scholar]
- Babin SM, et al. , 2007. Pediatric patient asthma-related emergency department visits and admissions in Washington, DC, from 2001–2004, and associations with air quality, socio-economic status and age group. Environmental Health: A Global Access Science Source. 6, 9–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buehler JW, et al. , 2004. Framework for evaluating public health surveillance systems for early detection of outbreaks: recommendations from the CDC Working Group. MMWR Recomm Rep. 53, 1–11. [PubMed] [Google Scholar]
- Fann N, et al. , 2015. The geographic distribution and economic value of climate change-related ozone health impacts in the United States in 2030. J Air Waste Manag Assoc. 65, 570–80. [DOI] [PubMed] [Google Scholar]
- Forouzanfar MH, et al. , 2015. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet. 386, 2287–2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller CH, et al. , 2019. Utilizing Syndromic Surveillance to Evaluate the Respiratory Effects of Fine Particulate Matter. Ann Am Thorac Soc. [DOI] [PMC free article] [PubMed]
- Jiang XY, Yoo EH, 2018. The importance of spatial resolutions of Community Multiscale Air Quality (CMAQ) models on health impact assessment. Science of the Total Environment. 627, 1528–1543. [DOI] [PubMed] [Google Scholar]
- Laumbach RJ, Kipen HM, 2012. Respiratory health effects of air pollution: update on biomass smoke and traffic pollution. J Allergy Clin Immunol. 129, 3–11; quiz 12–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magzamen S, et al. , 2017. Ozone-Related Respiratory Morbidity in a Low-Pollution Region. J Occup Environ Med. 59, 624–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Oceanic and Atmospheric Association, Climate Data Online. National Oceanic and Atmospheric Association, 2019.
- Punger EM, West JJ, 2013. The effect of grid resolution on estimates of the burden of ozone and fine particulate matter on premature mortality in the USA. Air Quality Atmosphere and Health. 6, 563–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slaughter JC, et al. , 2005. Association between particulate matter and emergency room visits, hospital admissions and mortality in Spokane, Washington. J Expo Anal Environ Epidemiol. 15, 153–9. [DOI] [PubMed] [Google Scholar]
- Soriano JB, et al. , 2017. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet Respiratory Medicine. 5, 691–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strosnider HM, et al. , 2018. Age-Specific Associations of Ozone and PM2.5 with Respiratory Emergency Department Visits in the US. Am J Respir Crit Care Med. [DOI] [PubMed]
- Tager IB, et al. , 2005. Chronic exposure to ambient ozone and lung function in young adults. Epidemiology. 16, 751–9. [DOI] [PubMed] [Google Scholar]
- US Environmental Protection Agency, GUIDELINE ON DATA HANDLING CONVENTIONS FOR THE 8-HOUR OZONE NAAQS. In: O. o. A. Q. P. a. Standards, (Ed.), Research Triangle Park, North Carolina: 27711, 1998. [Google Scholar]
- US Environmental Protection Agency, Air Data: Air Quality Data Collected at Outdoor Monitors Across the US. 2019.
- Viegi G, et al. , 2006. Epidemiology of chronic obstructive pulmonary disease: health effects of air pollution. Respirology. 11, 523–32. [DOI] [PubMed] [Google Scholar]
- Vingarzan R, 2004. A review of surface ozone background levels and trends. Atmospheric Environment. 38, 3431–3442. [Google Scholar]
- Wang Y, et al. , 2018. Associations between daily outpatient visits for respiratory diseases and ambient fine particulate matter and ozone levels in Shanghai, China. Environ Pollut. 240, 754–763. [DOI] [PubMed] [Google Scholar]
- Wilson A, et al. , 2017. Climate change impacts on projections of excess mortality at 2030 using spatially varying ozone-temperature risk surfaces. J Expo Sci Environ Epidemiol. 27, 118–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winquist A, et al. , 2012. Comparison of emergency department and hospital admissions data for air pollution time-series studies. Environ Health. 11, 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng XY, et al. , 2015. Association between Air Pollutants and Asthma Emergency Room Visits and Hospital Admissions in Time Series Studies: A Systematic Review and Meta-Analysis. PLoS One. 10, e0138146. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.