Abstract
Objectives
Recent rampant spread of COVID-19 cases in nursing homes has highlighted the concerns around nursing homes’ ability to contain the spread of infections. The ability of nursing homes to invest in quality improvement initiatives may depend on resource availability. In this study, we sought to examine whether lower profit margins, as a proxy for lack of resources, are associated with persistent infection control citations.
Design
We conducted a retrospective study.
Setting and Participants
Medicare-certified nursing homes in the US with financial and facility characteristics data (n = 12,194).
Methods
We combined facility-level data on nursing home profit margins from Medicare Cost Reports with deficiency citation data from Nursing Home Compare (2017-2019) and facility characteristics data from LTCFocus.org. We descriptively analyzed infection control citations by profit margins quintiles. We used logistic regressions to examine the relationship between profit margin quintiles and citations for infection prevention and control, adjusting for facility and market characteristics.
Results
About three-fourths of all facilities received deficiency citations for infection prevention and control during 1 or more years from 2017 to 2019 with about 10% of facilities cited in all 3 years. Facilities in the highest profit margin quintile had 7.6% of facilities with citations for infection prevention and control in each of the 3 years compared with 8.1%, 10.0%, 10.7%, and 13.7% for facilities in the fourth, third, second, and first quintiles of profit margins, respectively. Multivariable regressions showed that facilities with the lowest profit margins (first quintile) had 54.3% higher odds of being cited in at least 1 year and 87.6% higher odds of being cited in each of the 3 years compared with facilities with the highest profit margins (fifth quintile).
Conclusions and Implications
Our findings indicate that nursing homes may need more resources to prevent citations for infection prevention and control.
Keywords: nursing homes, deficiency citations, profit margins
Nursing home residents are vulnerable to infections because of lower immunity, higher comorbidities, and shared living arrangements.1 Every year, millions of serious infections occur in nursing homes2 , 3 leading to increased hospitalizations, health care costs, and mortality with thousands of deaths attributed to infections.4 Recent spread of COVID-19 cases in nursing homes has increased concerns around nursing homes’ ability to contain the spread of infections. In 2016, the Centers for Medicare & Medicaid Services (CMS) issued a final rule requiring nursing homes to develop a robust infection control program that includes antibiotic stewardship and employment of a trained infection preventionist.5
Despite the efforts from the CMS and other regulatory bodies to improve infection control in nursing homes over the years, more than 40% of nursing homes are cited for deficiency on infection prevention and control every year.6 These citations could be as simple as failure to follow proper hand hygiene by an individual staff to more widespread facility policies around screening for infectious diseases such as COVID-19. For instance, a failure to properly record and monitor COVID-19 symptoms can result in a citation. Citation for infection prevention and control is one of the most common types of deficiencies observed in nursing homes,7 and more than half of nursing homes are cited for infection prevention and control over multiple years between 2013 and 2017.8 More than 98% of infection control citations have “potential for more than minimal harm,” and about 46% of the citations are “patterns” and/or widespread across the facility.9
Several factors may explain why some facilities are cited repeatedly for infection prevention and control. Low staffing levels, higher older population, and low per capita income are associated with deficiency citations for infection control.10 In addition, facilities that are cited for infection controls had fewer experienced infection control professionals and also invested fewer resources on continuing education on infection control.11
Deficiency citations for infection-related issues could damage the reputation of nursing homes and impact finances either directly through fines or indirectly through lower consumer demand. Nursing homes are profit-maximizing firms12 that will invest resources to prevent citations for infection prevention and control if these quality improvements ultimately increase their profits. However, nursing homes may not respond to citations if the consumers do not respond to these citations or if the facilities do not have the resources to address citations. In a market with no competition, facilities may not lose consumers even if their reputation is damaged by citations; researchers often categorize market competition using the Herfindahl Hirschman Index.13 Other factors that may be associated with citations for infection prevention and control include the activities of daily living (ADL) index, race, age, gender, profit status, chain affiliation, payer mix, bed size, occupancy levels, staffing sizes, and rurality.10 , 14
Nursing home profit margins can be associated with citations for infection prevention and control in 2 distinct ways. First, there is an incentive for facilities to avoid citations to increase or maintain profits. It is difficult for facilities to increase profits in the long run by not investing resources in quality improvement because consumers may look for facilities without citations. There is evidence that improved performance on publicly reported quality measures leads to higher revenues and profit margins in nursing homes.15 Second, nursing homes with higher profit margins may have the resources to invest in quality improvement. A study found that profit margins are positively associated with quality.16
Existing studies have not explored whether nursing homes with fewer resources, as proxied by total profit margins, have higher likelihood of citations or persistent citation problems. When facilities with positive profit margins are cited for infection prevention and control, they may be able to tap into their profits to make the necessary improvements. However, facilities with losses may not have resources to address citation issues on a long-term basis.
Our objective in this study is to examine the relationship between profit margins, as a proxy for financial resources, and deficiency citations for infection prevention and control. First, are lower profit margins associated with deficiency citation for infection prevention and control? Second, are lower profit margins associated with persistent citation for infection prevention and control? These 2 questions will help us understand whether better-resourced facilities are less likely to be cited or less likely to be repeatedly cited for infection prevention and control. Our findings will also have implications for how we manage the spread of viruses such as COVID-19 in nursing homes.
Methods
Study Sample and Data Sources
We obtained general nursing home information and deficiency records from the CMS Nursing Home Compare Website (NHC) from 2017 to 2019. We used the provider ID to link these nursing homes to 2 other data sources: LTCfocus (2017) and CMS Cost Reports (2017). We used the resident characteristics aggregated at the facility level from LTCfocus data. NHC also has resident and nursing home characteristics. Using the LTCfocus and NHC data, we obtained resident- and facility-level characteristics, including resident demographic characteristics such as age, gender, and race; ADL index; RUG case mix index; number of beds; occupancy levels; payer mix (percentage of Medicaid residents and percentage of Medicare residents); staffing level for certified nursing assistant, licensed practical nurse, and registered nurse; profit status; chain membership; and a measure of market competition, the Herfindahl-Hirschman Index (HHI). We used CMS Cost Reports to obtain the total profit margins for nursing homes. Finally, we used Rural-Urban Commuting Area Codes to classify nursing homes into urban and rural areas.
Our initial study sample included all 15,540 nursing homes with health inspection records from 2017 to 2019. We excluded 750 hospital-based facilities since these facilities operate under a different environment than freestanding nursing homes. We excluded 1304 facilities without profit margins data and another 1044 facilities without some facility characteristics in 2017. Because financial data generally suffer from outlier issue, we excluded another 248 facilities with profit margins in the top and bottom 1 percentile. Our exclusion of outlier financial data is consistent with others that have used expenditure and cost data.17 , 18 Our final sample includes 12,194 nursing homes that had information on all key variables including profit margins, citation information, and facility characteristics.
Outcomes
Our outcome variable is a citation for infection prevention and control (citation tag: F880, Supplementary Table 3). As part of the regulations, facilities are required to establish and maintain programs and policies that provide an environment that prevents and controls communicable diseases and infections. Facilities should have a policy on how to identify, report, investigate, and control infections. Facilities also should ensure safe hand hygiene practices and handle linens in a way that prevents transmission of infections. We examined 2 key outcomes based on the pattern of infection prevention and control deficiency citation: (1) whether facilities received at least 1 deficiency citation for infection prevention and control from 2017 to 2019, and (2) whether facilities received deficiency citation for infection prevention and control in all 3 years from 2017 to 2019. Our goal in evaluating citations in all 3 years was to examine the persistency of citations. For descriptive analysis, we further created 4 mutually exclusive groups of facilities: (1) did not receive any deficiency citations; (2) received deficiency citations in only 1 year; (3) received deficiency citations in only 2 of the 3 years; and (4) received deficiency citations in all 3 years.
Key Independent Variable
Our key independent variable is the categorical variable indicating quintiles of total profit margins. We defined total profit margins as total revenues (Worksheet G3, line 3+25) minus total expenses (Worksheet G3, line 4+30) divided by total revenues.
Statistical Analyses
We conducted descriptive analyses to examine the infection prevention and control citation patterns from 2017 to 2019, overall and by profit margins group. Next, we used logistic regressions to examine the association between profit margins and deficiency citation patterns. We conducted separate regressions for the 2 outcomes: (1) whether facilities received at least 1 deficiency citation for infection prevention and control from 2017 to 2019 and (2) whether facilities received deficiency citation for infection prevention and control in all 3 years from 2017 to 2019. We control for several resident and facility characteristics associated with infection prevention and control citations including age, gender, race, ADL index and RUG case mix index, number of beds, occupancy, payer mix, staffing levels, profit status, chain membership, market competition, and urban-rural location.9 , 19 , 20 In a market with no competition, facilities may not lose consumers even if their reputation is damaged by citations; researchers often categorize market competition using Herfindahl Hirschman Index.13 We follow the literature and define a competitive market as one that has a Herfindahl Hirschman Index <0.15.21 In order to control for state-level differences in citation patterns, we also added state fixed effects in the regressions. We clustered standard errors at the state level.
We conducted several sensitivity analyses around the functional form and definition of our key independent variable—profit margins. First, we examined the relationship between profit margins and citations using a continuous measure of profit margins. Second, we dichotomize profit margins and examine citations between facilities with positive and negative profit margins. Finally, although total profit margins make the most sense when it comes to evaluation of resources available to nursing homes, we examined the relationship between operating profit margin quintiles and citations for infection prevention and controls.
Results
Of the 12,194 facilities in our final analytical sample, average profit margin ranged from negative 14.5% for the first quintile to positive 11.2% for the fifth quintile. We summarize the descriptive characteristics by profit margin quintiles in Table 1 . Most of the characteristics of facilities across profit margins quintiles are qualitatively similar. However, facilities in the lower profit margins quintiles have lower occupancy levels, higher proportion of Medicaid residents, and lower proportion of Medicare residents.
Table 1.
Descriptive Statistics of Nursing Homes (2017)
| All Nursing Homes | Total Profit Margin Quintiles |
|||||
|---|---|---|---|---|---|---|
| First Quintile | Second Quintile | Third Quintile | Fourth Quintile | Fifth Quintile | ||
| ADL index, mean (SD) | 16.70 (2.45) | 16.50 (2.30) | 16.63 (2.40) | 16.73 (2.43) | 16.77 (2.52) | 16.88 (2.57) |
| RUG case mix index, mean (SD) | 1.18 (0.15) | 1.17 (0.14) | 1.17 (0.14) | 1.18 (0.15) | 1.18 (0.14) | 1.19 (0.17) |
| Facility total beds, mean (SD) | 112.28 (57.73) | 109.77 (52.55) | 114.16 (61.05) | 115.64 (58.34) | 113.22 (58.19) | 108.60 (57.91) |
| Occupancy %, mean (SD) | 80.99 (14.01) | 74.49 (15.81) | 79.98 (13.65) | 82.55 (12.88) | 83.55 (12.54) | 84.38 (12.56) |
| Medicaid, mean (SD) | 60.38 (21.45) | 62.07 (21.94) | 61.49 (20.14) | 60.90 (20.74) | 60.01 (20.25) | 57.41 (23.71) |
| Medicare, mean (SD) | 13.62 (11.42) | 12.63 (10.94) | 12.87 (10.20) | 13.42 (11.19) | 13.96 (11.11) | 15.23 (13.23) |
| Age, mean (SD) | 79.57 (6.15) | 78.58 (5.92) | 79.47 (5.82) | 79.77 (6.09) | 79.97 (5.97) | 80.04 (6.78) |
| Female %, mean (SD) | 66.48 (11.50) | 65.30 (10.86) | 66.59 (11.06) | 66.73 (11.88) | 67.00 (11.59) | 66.77 (12.00) |
| White %, mean (SD) | 79.77 (21.90) | 79.69 (20.93) | 80.11 (21.69) | 79.34 (22.22) | 79.89 (22.27) | 79.84 (22.38) |
| Staffing hours per resident day, mean (SD) | ||||||
| CNA | 2.44 (0.59) | 2.39 (0.58) | 2.42 (0.59) | 2.48 (0.59) | 2.49 (0.57) | 2.44 (0.61) |
| LPN | 1.07 (0.42) | 1.08 (0.45) | 1.07 (0.40) | 1.08 (0.44) | 1.06 (0.40) | 1.06 (0.42) |
| RN | 0.53 (0.23) | 0.55 (0.24) | 0.53 (0.23) | 0.53 (0.22) | 0.53 (0.24) | 0.51 (0.23) |
| Urban or rural, n (%) | ||||||
| Urban | 8159 (67) | 1668 (68) | 1623 (67) | 1647 (68) | 1601 (66) | 1620 (66) |
| Large rural town | 1709 (14) | 315 (13) | 360 (15) | 341 (14) | 355 (15) | 338 (14) |
| Small rural town | 1336 (11) | 269 (11) | 263 (11) | 269 (11) | 261 (11) | 274 (11) |
| Isolated rural | 990 (8) | 187 (8) | 193 (8) | 182 (7) | 222 (9) | 206 (8) |
| Profit margin %, mean (SD) | −0.36 (9.39) | −14.49 (7.30) | −3.65 (1.57) | 0.68 (1.03) | 4.45 (1.23) | 11.20 (3.76) |
| For-profit, n (%) | 9036 (74%) | 1834 (75%) | 1798 (74%) | 1778 (73%) | 1818 (75%) | 1808 (74%) |
| Multi-facility organization, n (%) | 7373 (60%) | 1702 (70%) | 1462 (60%) | 1386 (57%) | 1402 (57%) | 1421 (58%) |
| Competitive market, n (%) | 7097 (58%) | 1498 (61%) | 1427 (59%) | 1432 (59%) | 1366 (56%) | 1374 (56%) |
| Number of observations, n | 12,194 | 2439 | 2439 | 2439 | 2439 | 2438 |
ADL, activities of daily living; CNA, certified nursing assistant; LPN, licensed practical nurse; RN, registered nurse; RUG, resource utilization groups.
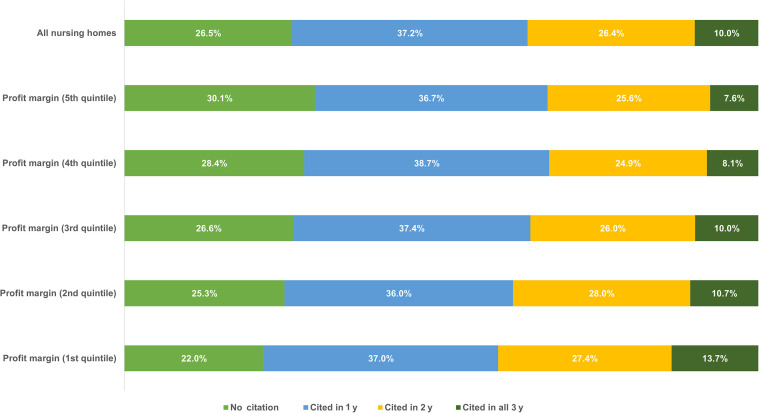
We report the infection prevention and control citation patterns by profit margins quintiles in Figure 1 . During the 2017 to 2019 period, 26.5% of facilities had no citations, 10% were cited for in each of the 3 years, and 64% were cited once or twice during the 3-year period. Compared with facilities in the higher profit margin quintiles, facilities in the lower profit margin quintiles have a higher proportion of facilities that are cited for all 3 years. For instance, only 7.6% of facilities in the highest profit margin quintile (fifth quintile) are cited for infection prevention and control in all 3 years compared with 13.7% of facilities in the lowest profit margin quintile (first quintile).
Fig. 1.
Citation pattern between 2017 and 2019 for infection prevention and control by profit margin quintiles.
We present the results from the multivariable logistic regressions in Table 2 . Profit margins ranged from 6.7% to 23.4% for facilities in the fifth quintile to −6.7% to −43.2% for facilities in the first quintile. The facilities in the first profit margin quintile have 54.3% (OR 1.543, 95% CI 1.29, 1.85) higher odds of receiving deficiency citation in at least 1 year compared with facilities in the fifth profit margin quintile. Furthermore, the odds of receiving deficiency citations for 3 consecutive years are 87.6% (OR 1.876, 95% CI 1.61, 2.19) higher for facilities in the first profit margin quintile when compared to facilities in the fifth profit margin quintile. Among the control variables, higher occupancy percentages and higher RN hours per resident day were associated with lower odds of deficiency citations. We did not find any relationship between competition and citation for infection prevention and control.
Table 2.
Association Between Profit Margins and Citation for Infection Prevention and Control
| Cited in At Least 1 y, OR (95% CI) | Cited in All 3 y, OR (95% CI) | |
|---|---|---|
| Profit margin % quintile categories [reference: fifth quintile (6.7-23.4)] |
||
| First quintile (−43.2 to −6.7) | 1.543 (1.290, 1.847) | 1.876 (1.608, 2.187) |
| Second quintile (−6.7 to −1.1) | 1.352 (1.173, 1.559) | 1.586 (1.239, 2.030) |
| Third quintile (−1.1 to 2.5) | 1.244 (1.057, 1.464) | 1.443 (1.213, 1.718) |
| Fourth quintile (2.5-6.7) | 1.131 (0.981, 1.305) | 1.147 (0.959, 1.373) |
| ADL index | 0.980 (0.950, 1.010) | 0.999 (0.955, 1.046) |
| RUG case mix index | 1.072 (0.590, 1.946) | 1.673 (0.930, 3.010) |
| Facility total beds | 1.003 (1.001, 1.005) | 1.003 (1.001, 1.005) |
| Occupancy % | 0.999 (0.995, 1.002) | 0.990 (0.983, 0.998) |
| Medicaid | 1.000 (0.997, 1.004) | 0.997 (0.993, 1.001) |
| Medicare | 1.004 (0.997, 1.011) | 0.995 (0.989, 1.002) |
| Age | 0.973 (0.959, 0.988) | 0.978 (0.956, 1.001) |
| Female % | 1.004 (0.996, 1.012) | 1.000 (0.989, 1.011) |
| White % | 0.997 (0.992, 1.002) | 0.997 (0.993, 1.001) |
| Staffing hours per resident day | ||
| CNA | 0.861 (0.767, 0.967) | 0.954 (0.855, 1.064) |
| LPN | 1.151 (0.976, 1.358) | 1.074 (0.877, 1.315) |
| RN | 0.648 (0.492, 0.854) | 0.660 (0.456, 0.955) |
| Urban or rural | ||
| Large rural town | 0.972 (0.857, 1.102) | 0.935 (0.736, 1.187) |
| Small rural town | 0.848 (0.695, 1.036) | 0.849 (0.606, 1.191) |
| Isolated rural | 0.771 (0.571, 1.041) | 0.775 (0.510, 1.177) |
| For-profit | 1.129 (0.992, 1.284) | 1.371 (1.076, 1.747) |
| Multifacility organization | 0.936 (0.839, 1.044) | 0.883 (0.756, 1.031) |
| Competitive market | 0.945 (0.783, 1.141) | 1.107 (0.841, 1.457) |
| Number of observations | 12,176 | 12,027 |
ADL, activities of daily living; CNA, certified nursing assistant; LPN, licensed practical nurse; RN, registered nurse; RUG, resource utilization groups.
The regressions show ORs from logistic regressions after adjusting for state fixed effects.
The findings from our sensitivity analyses are consistent with our main findings (Table 3 ). When we use profit margins as a continuous variable, we find that as profit margins increase by a percentage point, the odds of getting cited for infection prevention and control deficiency decrease by about 1.4% (OR 0.986, 95% CI 0.98, 0.99). Similarly, we find that facilities with negative profit margins have 30.8% (OR 1.308, 95% CI 1.2, 1.4) higher odds of being cited at least once during the 3-year period, and 44.6% (OR 1.446, 95% CI 1.26, 1.66) higher odds of being cited in all 3 years. The findings are consistent when we examine the relationship between operating profit margin quintiles and infection control citations (Supplementary Table 1).
Table 3.
Sensitivity Analyses
| Cited in At Least 1 y | Cited in All 3 y | |
|---|---|---|
| Profit margin %, OR (95% CI) | 0.986 (0.980, 0.991) | 0.979 (0.974, 0.984) |
| Number of observations | 12,176 | 12,027 |
| Negative profit margin, OR (95% CI) | 1.308 (1.198, 1.427) | 1.446 (1.256, 1.664) |
| Number of observations | 12,176 | 12,027 |
The regressions show ORs from logistic regressions after adjusting for state fixed effects.
Discussion
We examined the relationship between profit margins and infection prevention and control deficiency citations to explore how resource availability affects deficiency citations. We find that facilities with lower profit margins have higher odds of getting citations for infection prevention and control even after controlling for resident and facility characteristics. Furthermore, we find that facilities with lower profit margins have higher odds of persistent citations.
Our findings are consistent with the literature on infection control citations in nursing homes. A recent study found that 15% of facilities were cited for infection control at least twice during a 2-year period.9 In our study, we examined citations during a 3-year period and found that 10% of the facilities were cited in all 3 years. Researchers found that 57% of facilities received at least 1 infection prevention and control citation during a 2-year period, whereas we find that more than 74% of facilities were cited at least once during a 3-year period.9
Our findings are also broadly consistent with existing evidence on nursing home finances and quality. A study found that better financial performance was associated with higher quality in a broad range of nursing home quality measures.16 Another study found that investing in quality is profitable for nursing homes.22 There is also evidence that nursing homes that perform better in terms of health outcomes such as pressure ulcers are able to lower costs and ultimately improve their profit margins.23
Our findings have important implications for policy. First, managing the spread of infections such as COVID-19 is challenging and enforcing existing regulations or imposing new regulations is not enough. Our findings suggest that simply citing facilities for infection prevention and control will not result in improved quality because more than one-third of facilities are cited at least twice in 3 years. In fact, 10% of the facilities were cited in all 3 years of our study. Second, emphasizing on staffing alone is not going to prevent deficiency citations. Although we find that higher RN staffing is associated with lower odds of being cited for infection prevention and control, a finding consistent with a previous study,8 resource availability is another important factor that determines whether a facility is cited or is cited repeatedly for infection prevention and control. A previous study suggested the need for training and support of infection preventionists in nursing homes;24 additional resources may help facilities with training and support for staff engaged in infection prevention and control.
Our findings also have implications for disparities in nursing home quality. Nursing homes serving high proportions of minorities tend to perform poorly in quality and finances, and can contribute to growing inequities.25 Similarly, Medicaid reimbursement rates are far lower than Medicare and/or private payer rates. Fewer resources mean limited ability to invest in quality improvements. These reimbursement differences may continue to increase the growing disparity in financial performance and quality of nursing homes serving underserved populations.
Our study adds to the growing literature examining nursing home quality. Several recent studies have examined the characteristics of nursing homes with infection prevention and control citations including the characteristics of facilities with COVID-19 infections. A recent study found that for-profit facilities, facilities serving higher proportion of Medicaid residents, and facilities with sicker individuals are likely to be cited for infection prevention and control.9 Several studies have highlighted community transmission rates, facility location, as well as facility size as being important determinants of COVID-19 infections.19 , 20 Given the high transmission rate of COVID-19, it is difficult to assess whether these findings will remain valid in other diseases with lower transmission rates. Our findings add to the existing literature by incorporating the role of nursing home financial resources in deficiency citations.
Our findings are subject to several limitations. First, although we made every effort to include potentially confounding variables, we may still have confounding from unobserved variables on resident-level case mix. Nevertheless, we do incorporate facility-level ADL index and RUG case mix index to proxy for resident acuity. Similarly, we do not have data on education and training of staff working in these facilities. Instead, we include nurse hours per resident day by the type of nurses. Second, the profit margins calculated in this study are based on CMS Cost Reports and may be subject to errors. We tried to address this issue by excluding outliers from the study. Third, we do not distinguish between citations in different years as we are evaluating the relationship between profit margins in 2017 and citations in subsequent years. However, as profit margin data become available for 2018-2019, it would be important to look at the dynamic relationship between profit margins and citations. Fourth, we focused on profit margins, but facilities may respond to quality issues in different ways depending on liquidity and cash flows. For example, a recent study found that nursing homes with less liquidity and those with cash flow problems had a higher likelihood of COVID-19 transmission.26 In addition, about a quarter of facilities in our data are nonprofit organizations, that may not necessarily be trying to maximize profits. However, even these facilities need to generate enough revenue to sustain operations. Finally, we did not account for the severity of deficiency citations in our analysis. There is little variation in the severity of citations for infection prevention and control and, thus, our approach to including all types of deficiency citations is justified.
Conclusions and Implications
Although some existing studies have examined the relationship between several resident- and facility-level factors and deficiency citations for infection prevention and control, our study fills an important gap by looking at financial resources and deficiency citations for infection prevention and control. Our finding that nursing homes with fewer resources, as characterized by lower profit margins, are substantially more likely to have repeated deficiency citations for infection prevention and control is worth emphasizing. If we want nursing homes to improve quality, we should enforce regulations by citing facilities for substandard care but also need to provide nursing homes with the resources to improve quality.
Supplementary Data
Supplementary Table 1.
Association Between Operating Margins and Citation for Infection Prevention and Control
| Cited in At Least 1 y, OR (95% CI) | Cited in All 3 y, OR (95% CI) | |
|---|---|---|
| Operating margin % quintile categories [reference group: fifth quintile (5.1-18.3)] |
||
| First quintile (−184.9 to −10.9) | 1.400 (1.178, 1.664) | 1.739 (1.464, 2.067) |
| Second quintile (−10.9 to −3.7) | 1.253 (1.093, 1.437) | 1.613 (1.342, 1.939) |
| Third quintile (−3.7 to 0.5) | 1.277 (1.097, 1.485) | 1.518 (1.242, 1.855) |
| Fourth quintile (0.5-5.1) | 1.118 (0.966, 1.293) | 1.208 (1.039, 1.404) |
| ADL index | 0.983 (0.955, 1.013) | 0.999 (0.959, 1.040) |
| RUG case mix index | 1.017 (0.585, 1.768) | 1.585 (0.904, 2.781) |
| Facility total beds | 1.003 (1.000, 1.005) | 1.003 (1.001, 1.005) |
| Occupancy % | 0.998 (0.994, 1.003) | 0.990 (0.983, 0.998) |
| Medicaid | 1.001 (0.998, 1.004) | 0.998 (0.994, 1.002) |
| Medicare | 1.004 (0.996, 1.012) | 0.995 (0.989, 1.002) |
| Age | 0.972 (0.959, 0.986) | 0.977 (0.957, 0.997) |
| Female % | 1.004 (0.997, 1.011) | 1.001 (0.990, 1.012) |
| White % | 0.997 (0.993, 1.002) | 0.997 (0.994, 1.001) |
| Staffing hours per resident day | ||
| CNA | 0.860 (0.768, 0.962) | 0.940 (0.842, 1.049) |
| LPN | 1.151 (0.971, 1.363) | 1.069 (0.877, 1.303) |
| RN | 0.638 (0.490, 0.831) | 0.667 (0.453, 0.982) |
| Urban or rural | ||
| Large rural town | 0.980 (0.861, 1.117) | 0.923 (0.737, 1.156) |
| Small rural town | 0.846 (0.695, 1.030) | 0.824 (0.592, 1.148) |
| Isolated rural | 0.765 (0.572, 1.023) | 0.750 (0.494, 1.139) |
| For-profit | 1.168 (1.027, 1.328) | 1.442 (1.127, 1.846) |
| Multifacility organization | 0.947 (0.850, 1.055) | 0.915 (0.787, 1.064) |
| Competitive market | 0.946 (0.794, 1.127) | 1.101 (0.840, 1.444) |
| Number of observations | 12,175 | 12,023 |
ADL, activities of daily living; CNA, certified nursing assistant; LPN, licensed practical nurse; RN, registered nurse; RUG, resource utilization groups.
We defined operating margins as net patient income (net patient revenues minus total operating expenses) divided by net patient revenues. The regressions show odds ratios from logistic regressions after adjusting for state fixed effects. We excluded 249 facilities with operating margins in the top and bottom 1 percentile.
Supplementary Table 2.
Characteristics of Excluded Sample
| Excluded Nursing Homes (n=2596) | |
|---|---|
| ADL index, mean (SD) | 16.02 (3.85) |
| RUG case mix index, mean (SD) | 1.15 (0.25) |
| Facility total beds, mean (SD) | 93.07 (63.36) |
| Occupancy %, mean (SD) | 78.59 (17.13) |
| Medicaid, mean (SD) | 60.61 (28.69) |
| Medicare, mean (SD) | 12.65 (16.92) |
| Age, mean (SD) | 77.08 (10.92) |
| Female %, mean (SD) | 63.10 (14.70) |
| White %, mean (SD) | 79.49 (22.60) |
| Staffing hours per resident day, mean (SD) | |
| CNA | 2.62 (0.78) |
| LPN | 1.10 (0.54) |
| RN | 0.63 (0.37) |
| Urban or rural, n (%) | |
| Urban | 1723 (67) |
| Large rural town | 327 (13) |
| Small rural town | 264 (10) |
| Isolated rural | 243 (10) |
| For-profit, n (%) | 1320 (64) |
| Multifacility organization, n (%) | 1075 (52) |
| Competitive market, n (%) | 1572 (61) |
ADL, activities of daily living; CNA, certified nursing assistant; LPN, licensed practical nurse; RN, registered nurse; RUG, resource utilization groups.
Supplementary Table 3.
F880: Infection Prevention and Control Regulation
| §483.80 Infection Control |
| The facility must establish and maintain an infection prevention and control program designed to provide a safe, sanitary and comfortable environment and to help prevent the development and transmission of communicable diseases and infections. |
| §483.80(a) Infection prevention and control program. |
| The facility must establish an infection prevention and control program (IPCP) that must include, at a minimum, the following elements: |
| §483.80(a)(1) A system for preventing, identifying, reporting, investigating, and controlling infections and communicable diseases for all residents, staff, volunteers, visitors, and other individuals providing services under a contractual arrangement based on the facility assessment conducted according to §483.70(e) and following accepted national standards; |
| §483.80(a)(2) Written standards, policies, and procedures for the program, which must include, but are not limited to: |
| (i) A system of surveillance designed to identify possible communicable diseases or infections before they can spread to other persons in the facility; |
| (ii) When and to whom possible incidents of communicable disease or infections should be reported; |
| (iii) Standard and transmission-based precautions to be followed to prevent spread of infections; |
| (iv) When and how isolation should be used for a resident; including but not limited to: |
| (A) The type and duration of the isolation, depending on the infectious agent or organism involved, and |
| (B) A requirement that the isolation should be the least restrictive possible for the resident under the circumstances. |
| (v) The circumstances under which the facility must prohibit employees with a communicable disease or infected skin lesions from direct contact with residents or their food, if direct contact will transmit the disease; and |
| (vi) The hand hygiene procedures to be followed by staff involved in direct resident contact. |
| §483.80(a)(4) A system for recording incidents identified under the facility’s IPCP and the corrective actions taken by the facility. |
| §483.80(e) Linens. |
| Personnel must handle, store, process, and transport linens so as to prevent the spread of infection. |
| §483.80(f) Annual review. |
| The facility will conduct an annual review of its IPCP and update their program, as necessary. |
References
- 1.High K.P., Juthani-Mehta M., Quagliarello V.J. Infectious diseases in the nursing home setting: Challenges and opportunities for clinical investigation. Clin Infect Dis. 2010;51:931–936. doi: 10.1086/656411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dwyer L.L., Harris-Kojetin L.D., Valverde R.H., et al. Infections in long-term care populations in the United States. J Am Geriatr Soc. 2013;61:341–349. doi: 10.1111/jgs.12153. [DOI] [PubMed] [Google Scholar]
- 3.Herzig C.T., Dick A.W., Sorbero M., et al. Infection trends in US nursing homes, 2006-2013. J Am Med Dir Assoc. 2017;18:635.e9–635.e20. doi: 10.1016/j.jamda.2017.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Strausbaugh L.J., Joseph C.L. The burden of infection in long-term care. Infect Control Hosp Epidemiol. 2000;21:674–679. doi: 10.1086/501712. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Medicare & Medicaid Services Medicare and Medicaid programs; reform of requirements for long-term care facilities. Final rule. Fed Regist. 2016;81(192):68688–68872. [PubMed] [Google Scholar]
- 6.Chidambaram P. Key questions about the impact of coronavirus on long-term care facilities over time. https://www.kff.org/coronavirus-covid-19/issue-brief/key-questions-about-the-impact-of-coronavirus-on-long-term-care-facilities-over-time/ Available at:
- 7.Office of the Inspector General . 2008. Trends in Nursing Home Deficiencies and Complaints. [Google Scholar]
- 8.US Government Accountability Office . US Government Accountability Office; Washington, DC: 2020. Infection Control Deficiencies Were Widespread and Persistent in Nursing Homes Prior to COVID-19 Pandemic. [Google Scholar]
- 9.Jester D.J., Peterson L.J., Dosa D.M., Hyer K. Infection control citations in nursing homes: Compliance and geographic variability. J Am Med Dir Assoc. 2020 doi: 10.1016/j.jamda.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Castle N.G., Wagner L.M., Ferguson-Rome J.C., et al. Nursing home deficiency citations for infection control. Am J Infect Control. 2011;39:263–269. doi: 10.1016/j.ajic.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 11.Herzig C.T., Stone P.W., Castle N., et al. Infection prevention and control programs in US nursing homes: Results of a national survey. J Am Med Dir Assoc. 2016;17:85–88. doi: 10.1016/j.jamda.2015.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Konetzka R.T., Sharma H., Park J. Malpractice environment vs direct litigation: What drives nursing home exit? Inquiry. 2018:55. doi: 10.1177/0046958018787995. 0046958018787995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rhoades S.A. Herfindahl-Hirschman Index. 79 Fed Res Bull. 1993:188. [Google Scholar]
- 14.Loomer L., Grabowski D.C., Gandhi A. 2020. Association between nursing home staff turnover and infection control citations. SSRN 3766377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Park J., Konetzka R.T., Werner R.M. Performing well on nursing home report cards: Does it pay off? Health Serv Res. 2011;46:531–554. doi: 10.1111/j.1475-6773.2010.01197.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Park J., Werner R.M. Changes in the relationship between nursing home financial performance and quality of care under public reporting. Health Econ. 2011;20:783–801. doi: 10.1002/hec.1632. [DOI] [PubMed] [Google Scholar]
- 17.Sharma H., Konetzka R.T., Smieliauskas F. The relationship between reported staffing and expenditures in nursing homes. Medical Care Res Rev. 2019;76:758–783. doi: 10.1177/1077558717739214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Doyle J.J., Jr., Graves J.A., Gruber J. Uncovering waste in US healthcare: Evidence from ambulance referral patterns. J Health Econ. 2017;54:25–39. doi: 10.1016/j.jhealeco.2017.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gorges R.J., Konetzka R.T. Staffing levels and COVID-19 cases and outbreaks in U.S. nursing homes. J Am Geriatr Soc. 2020;68:2462–2466. doi: 10.1111/jgs.16787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abrams H.R., Loomer L., Gandhi A., Grabowski D.C. Characteristics of U.S. nursing homes with COVID-19 cases. J Am Geriatr Soc. 2020;68:1653–1656. doi: 10.1111/jgs.16661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Huang S.S., Hirth R.A. Quality rating and private-prices: Evidence from the nursing home industry. J Health Econ. 2016;50:59–70. doi: 10.1016/j.jhealeco.2016.08.007. [DOI] [PubMed] [Google Scholar]
- 22.Weech-Maldonado R., Pradhan R., Dayama N., et al. Nursing home quality and financial performance: Is there a business case for quality? Inquiry. 2019:56. doi: 10.1177/0046958018825191. 0046958018825191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weech-Maldonado R., Neff G., Mor V. Does quality of care lead to better financial performance?: The case of the nursing home industry. Health Care Manage Rev. 2003;28:201–216. doi: 10.1097/00004010-200307000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Stone P.W., Herzig C.T.A., Agarwal M., et al. Nursing home infection control program characteristics, CMS citations, and implementation of antibiotic stewardship policies: A national study. Inquiry. 2018;55 doi: 10.1177/0046958018778636. 46958018778636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chisholm L., Weech-Maldonado R., Laberge A., et al. Nursing home quality and financial performance: Does the racial composition of residents matter? Health Serv Res. 2013;48:2060–2080. doi: 10.1111/1475-6773.12079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Begley T.A., Weagley D. Firm finances and the spread of COVID-19: Evidence from nursing homes. SSRN. 2020 [Google Scholar]