Abstract
We present a case of cecal bascule in a 60-year-old woman with abdominal pain and vomiting. Imaging tests revealed a cecal bascule causing mechanic obstruction of the stomach. Besides a small bowel dilatation was not seen, the distended cecum was extrinsically obstructing the antrum and therefore, the gastric outlet. Cecal bascule is a form of cecal volvulus without the axial twisted component. The cecum folds anterior or anteromedially on itself and, because of a valve mechanism, becomes distended. The pressure increases and it begins to compromise arterial blood flow so life-threatening complications, such as bowel ischemia and infarction can occur. Prompt diagnosis is therefore crucial and plain radiographs and computed tomography are the preferred imaging techniques for this purpose.
Keywords: Intestinal volvulus, Acute abdomen, Intestinal obstruction, Multidetector computed tomography, Diagnostic X-ray
Introduction
Cecal volvulus is a rare pathological condition and sometimes is misdiagnosed.
Prompt diagnosis is crucial to avoid life-threatening complications, such as bowel ischemia and infarction. Plain radiographs and computed tomography (CT) are the imaging techniques preferred for this purpose.
Specifically, cecal bascule is a kind of cecal volvulus without the axial mesenteric twisted component. Because of a valve mechanism, the cecum becomes distended until the increasing pressure begins to compromise perfusion.
Case report
A 60-year-old woman presented to the Emergency Services with abdominal epigastric pain and vomiting. Laboratory findings were irrelevant.
Plain radiographs (Fig. 1) showed a highly dilatated intestinal segment of over 10 cm, probably corresponding to the cecum, displaced upper and medially.
Fig. 1.
Plain X-ray of the abdomen. Severe dilatated viscus located at the epigastrium displacing the stomach laterally. Bowel distention in the lower abdomen.
A contrast enhanced abdominal CT with portal phase imaging acquisition was therefore performed, confirming a distended and mispositioned C-shaped cecum displaced to the epigastrium. Adjacent to the distended cecum, a vascular and bowel crossover was observed, involving the terminal ileum and the ascending colon itself, with their corresponding sheaths and vessels, describing a closed loop obstruction. No swirl image or torsion of the meso was identified (Figs. 2 and 3). In addition, an important dilatation of the stomach was seen, due to an extrinsic anterior compression of the antrum by the distended cecum (Figs. 2 and 4). Terminal ileum loops in the right flank were distended. Proximal ileum and jejunum were normal. The remaining large bowel appeared collapsed (Fig. 2). Minimal amount of free fluid around the gastric chamber was documented.
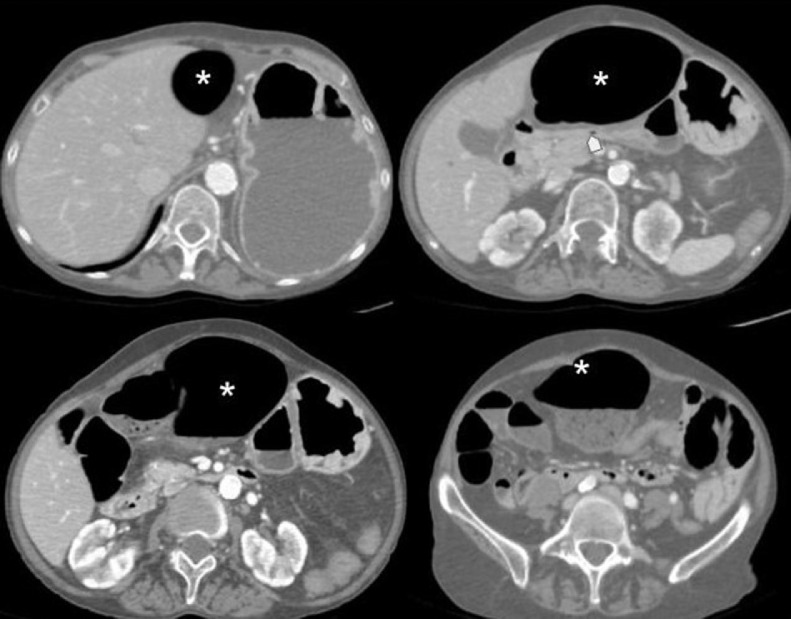
Fig. 2.
Contrast enhanced abdominal CT. Distended mispositioned cecum at the epigastrium (*) conditioning an extrinsic compression of the gastric antrum that appears collapsed (arrowhead). Secondary severe dilatation of the gastric chamber, with surrounding free peritoneal fluid. Absence of the cecum and ascending colon in right hemiabdomen, which is occupied by small bowel dilatated loops . Remaining large bowel and jejunal loops appear collapsed.
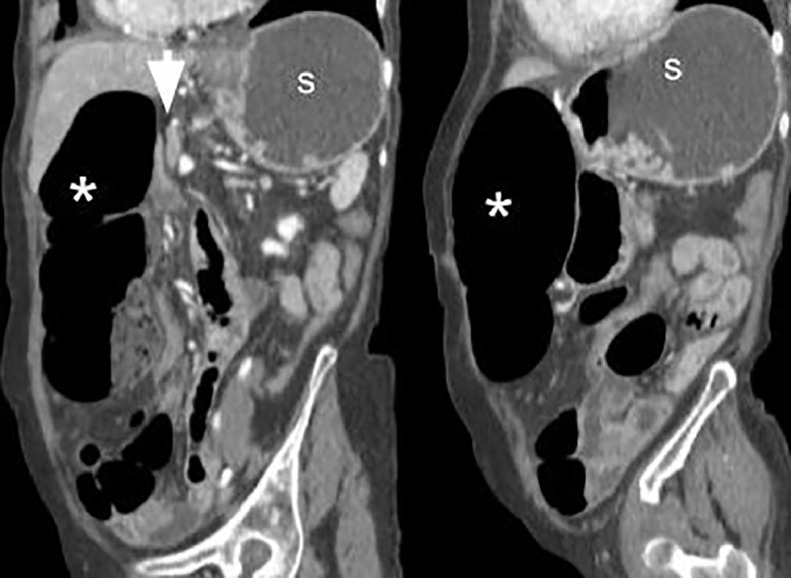
Fig. 3.
Contrast enhanced abdominal CT. Oblique coronal view. Markedly dilatated cecum and part of the ascending colon displaced upwards and medially to the epigastrium (*). Adjacent to the medial wall of this loop an image of vascular crossover is observed with sharped narrowing of the dragged intestinal loops (arrow).
Fig. 4.
Contrast enhanced abdominal CT. Sagittal view. Distended cecum (*) at epigastrium causes an anterior extrinsic compression of the antrum (↓). Secondary fluid-filled distended stomach (S).
The patient underwent emergency surgery with a midline laparotomy approach. Many fibrous adhesions were seen in the subhepatic region, conditioning a strongly fixation of the right colon. The free cecum was found upward and medially folded on itself, severely dilatated and with signs of hypoperfusion. Surgeons performed an adhesiotomy and release the cecum, but signs of hypoperfusion persisted, so a right colectomy with ileocolic anastomosis was finally necessary. The gastric obstruction was resolved before surgery, placing a nasogastric tube and obtaining more than one liter of gastric content.
Discussion
Cecal volvulus is a closed loop intestinal obstruction caused by an intestinal torsion that affects the cecum, the ascending colon and sometimes the terminal ileum.
It is more frequent in 30 to 60-year-old patients and accounts for 25%-40% of all cases of colonic volvulus and for 1%-3% of intestinal obstructions.
Predisposing factors that facilitate an abnormal mobility of the cecum such as long cecal mesentery, presence of scars and adhesions, neoplastic masses or lymph nodes are usually present [1].
We can classify cecal volvulus according to the torsion mechanism [2]:
-
-
Axialvolvulation: the cecum turns 180-360 degrees on its axis, remaining in the lower right quadrant of the abdomen.
-
-
Horizontalvolvulation: turning on its horizontal axis, the cecum and ileum migrate to the upper left quadrant.
-
-
Cecal torsion (bascule type): Associated with adhesions. The cecum, ascending colon and ileum fold forward without twisting. The cecal loop appears dilatated in the epigastrium. A valve mechanism determines cecal occlusion and dilation [2] (Fig. 4).
Clinically non-specific, the diagnosis is based on radiological findings. Conventional abdominal radiography is usually the initial imaging test. A dilatated and with air-fluid level cecum mispositioned in the left upper quadrant can be sufficient for diagnosis. However, the cecum can be located anywhere in the abdomen depending on the volvulus type, so further test will be needed. Small bowel dilatation may also appear, depending on the time of onset [1], [3], [4], [5].
Diagnose is confirmed with multidetector computed tomography . Locating the terminal ileum loop, the ileocecal valve, and the appendix can help identifying the ectopic cecum. It is important to watch out for the “whirlpool sign”, conformed by collapsed bowel loops, mesenteric fat and congestive mesenteric vessels. This sign appears when the bowel rotates around its mesentery, leading to whirls of the mesenteric vessels. Associated with an enlarged cecum, is diagnostic for cecum volvulus, axial if the cecum remains in its normal position, horizontal if the cecum becomes displaced to the left upper abdominal quadrant [2]. The absence of it do not dismiss the diagnose, because the “whirlpool” sign does not appear in the cecal bascule, where the cecum folds forward to the epigastric region without twisting. Even though there is no mesenteric torsion, a valve mechanism occurs, and the cecum becomes either way distended until the pressure begins to compromise perfusion [2], [5] (Figs. 3.and 5). Determining the absence or presence of this sign is therefore the key to make a correct diagnosis. So, the presence of an enlarged cecum located in the epigastrium without a whirl sign, as in our case, suggests a cecal bascule [4,5]. Another element for diagnosis is the detection of the point of torsion, following the dilatated bowel loops gradual narrowing up to one single level of obstruction (“bird's beak sign”) (Fig. 3) [6], [7]. Multiplanar and 3D Volume reconstructions (Figs. 3-5) still fundamental to make the diagnosis, allowing the identification of the “whirlpool sign” or the crossover site usually not visible on axial examinations according to the torsion plane [7].
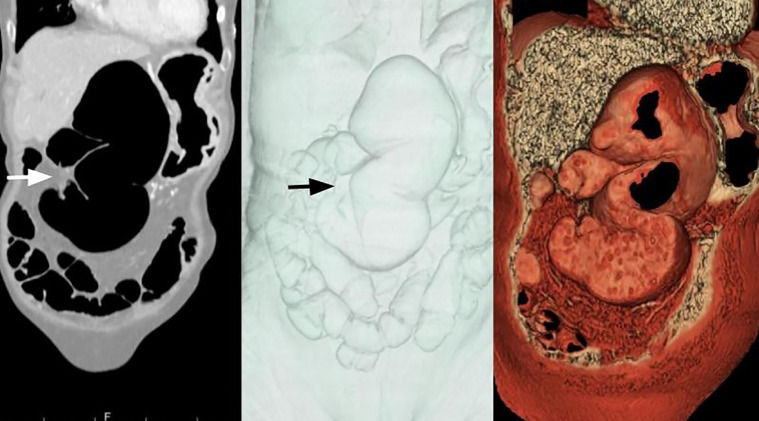
Fig. 5.
Contrast enhanced abdominal CT. Coronal MPR and volume reformations. Closed loop obstruction features. A dilatated cecum is seen, fold over the ascending colon and located at the epigastrium, fixed on its lateral aspect, where a change in caliber is appreciated (→). No “whirlpool sign” is appreciated. Findings consistent with a cecal bascule.
The symptomatology in colon volvulus is due to the cecum distention, consisting of abdominal pain and distension followed by signs of peritonitis if complications like bowel ischemia, infarction and ultimately perforation occur. It usually has a rapid evolution, so patients rarely have time to develop symptoms derived from intestinal obstruction such as nausea and vomiting. When present, there are usually secondary to the peritoneal reaction [7], [8]. However, in our case, in addition to abdominal pain, the dominant symptom was precisely intense vomiting. What was special in our case was that this was because the distended and displaced cecum was extrinsically compressing the antrum causing a mechanical gastric outlet obstruction, leading to a severe dilatation of the stomach (Figs. 2 and 4). In the previous literature, no cases of gastric outlet obstruction secondary to a cecal volvulus have been reported.
CT is also useful detecting signs of bowel ischemia like mesenteric fat stranding, bowel wall thickening or diminished or absent enhancement. Pneumatosis intestinalis, mesenteric or portal, and pneumoperitoneum represents and advanced irreversible stage. Free intraperitoneal fluid is a frequent and unspecific sign[4], [7], [8].
Surgery is the treatment of choice. Endoscopic approach is not recommended for the management of cecal volvulus because there is a low rate of success and a high rate in recurrence, leading to delay surgical approach and worsening the prognosis.
Surgery offers several options: manual detorsion, cecopexy, cecostomy and open or laparoscopic colectomy. Obviously, in case of life-threatening complications surgical resection must be performed [3], [8].
In our case, besides signs of hypoperfusion were documented during the surgery, there were not present at the time when CT was performed. The 5-hour delay between each other may explain the different findings.
Patient consent
The patient has been informed that his clinical case was going to be sent for publication in a scientific journal and that the clinical data and some images of the radiological studies carried out would be sent.
In no case the patient will be identified nor will there be any data that violates confidentiality, remaining anonymous anywere.
We have in custody the copy of the consent at your disposal if necessary.
REFERENCES
- 1.Peterson CM, Anderson JS, Hara AK, Carenza JW, Menias CO. Volvulus of the gastrointestinal tract: appearances at multimodality imaging. Radiographics. 2009;29:1281–1293. doi: 10.1148/rg.295095011. [DOI] [PubMed] [Google Scholar]
- 2.Delabrousse E, Sarliève P, Sailley N, Aubry S, Kastler BA. Cecal volvulus: CT findings and correlation with pathophysiology. EmergRadiol. 2007;14(6):411–415. doi: 10.1007/s10140-007-0647-4. [DOI] [PubMed] [Google Scholar]; Epub 2007 Jul 6. PMID: 17618472.
- 3.Consorti E, Liu T. Diagnosis and treatment of cecal volvulus. Postgrad Med J. 2005;81:772–776. doi: 10.1136/pgmj.2005.035311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moore CJ, Corl FM, Fishman EK. CT of cecal volvulus: unraveling the image. AJR Am J Roentgenol. 2001;177:95–98. doi: 10.2214/ajr.177.1.1770095. [DOI] [PubMed] [Google Scholar]
- 5.Frank AJ, Goffner LB, Fruauff AA, Losada RA. Cecal volvulus: the CT whirl sign. Abdom Imaging. 1993;18:288–289. doi: 10.1007/BF00198126. [DOI] [PubMed] [Google Scholar]
- 6.Vandendries C, Jullès MC, Boulay-Coletta I, Loriau J, Zins M. Diagnosis of colonic volvulus: findings on multidetector CT with three-dimensional reconstructions. Br J Radiol. 2010;83:983–990. doi: 10.1259/bjr/35714052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosenblat JM, Rozenblit AM, Wolf EL, DuBrow RA, Den EI, Levsky JM. Findings of cecal volvulus at CT. Radiology. 2010;256(1):169–175. doi: 10.1148/radiol.10092112. [DOI] [PubMed] [Google Scholar]; PMID: 20574094.
- 8.Tonerini M, Pancrazi F, Lorenzi S, Pacciardi F, Ruschi F, Turturici L. Cecal volvulus: what the radiologist needs to know. Glob Surg. 2015;1 doi: 10.15761/GOS.1000106. [DOI] [Google Scholar]