Abstract
Background
We redesigned the Schisto and Ladders health educational board game and evaluated its potential to encourage compliance to school-based mass drug administration with praziquantel.
Methods
Two hundred and seventy-five children from six schools who rejected praziquantel treatment were divided into intervention and control groups. Before the intervention, preassessment interviews were conducted on their knowledge about praziquantel treatment and schistosomiasis. The Schisto and Ladders version 2 game as an intervention, and the Snakes and Ladders game as a control, were played for 6 mo. Postassessment interviews, including focus group discussions, were conducted.
Results
At preassessment, 0/98 (0.0%) children in the intervention group had heard of praziquantel compared with 2/177 (1.1%) in the control group. Similarly, 0/98 (0.0%) children in the intervention group did not know that praziquantel does not kill compared with 4/177 (2.3%) in the control group. The postassessment showed that 53/78 (67.9%) in the intervention group were aware of praziquantel compared with 2/177 (1.1%) in the control group (p=0.000). Similarly, 53 (69.7%) in the intervention group knew about the safety of praziquantel compared with 0/177 (0.0%) in the control group (p=0.000). Sixty-four children (65.3%) from the intervention group sought praziquantel treatment after the trial.
Conclusions
Schisto and Ladders version 2 is a useful sensitisation tool with which to encourage compliance to praziquantel treatment in schools.
Keywords: health education, Nigeria, praziquantel, Schisto and Ladders version 2, schistosomiasis, school children
Introduction
The control of schistosomiasis in sub-Saharan Africa, including Nigeria, is mainly conducted through school-based mass drug administration (MDA) with praziquantel.1,2 Although praziquantel remains the drug of choice for reducing morbidity due to schistosomiasis, several studies have shown that treatment alone does not prevent reinfection, transmission or elimination of the disease.3,4 It has also been observed that rejection of MDA with praziquantel by school children has been attributed to the use of unskilled personnel for drug administration, a lack of proper health education to enable individuals to understand why they should take medicine, adverse side effects, bitter taste and even rumours of death.5,6 This has resulted in low treatment coverage, thus hampering the elimination of schistosomiasis as a public health problem in line with the Sustainable Developmental Goal (SDG) 3.3 by 2030. In Nigeria, an estimated 11.3 million school-aged children aged 5–14 y are infected with schistosomiasis and thus require praziquantel treatment.7 The Ogun State Neglected Tropical Diseases Control Programme commenced school-based MDA with praziquantel in 2017. However, the treatment coverage was low with a high rejection of praziquantel, a consequence of rumours about possible side effects and risk of death.8 Additional public health measures including novel health educational tools are required for more sustained control of schistosomiasis to sensitise and improve the knowledge of school children and their parents/caregivers on the importance of and compliance to school-based MDA with praziquantel. Health education is essential for the control of schistosomiasis.9,10 Innovative and novel health education tools such as the Juma na Kichocho comic-strip medical booklet for schistosomiasis have been used in Zanzibar, Tanzania11,12 and a cartoon video game was used for the control of intestinal helminths in China.13,14 Recently, we developed and tested a health education board game called Schisto and Ladders that improved the knowledge, attitudes and practices (KAP) about schistosomiasis among school children in Ogun State, Nigeria.15 Our study showed a 68.0% improvement in knowledge about urogenital schistosomiasis, its transmission and prevention demonstrating that a game-based health educational tool increases school children's knowledge of preventive measures against schistosomiasis.
To support compliance and uptake of school-based MDA with praziquantel, we have had to redesign the Schisto and Ladders game. Here, we report the redesigning of the Schisto and Ladders game to version 2 and the results of the evaluation of the game as a potential sensitisation tool during school-based MDA with praziquantel.
Materials and methods
Study site
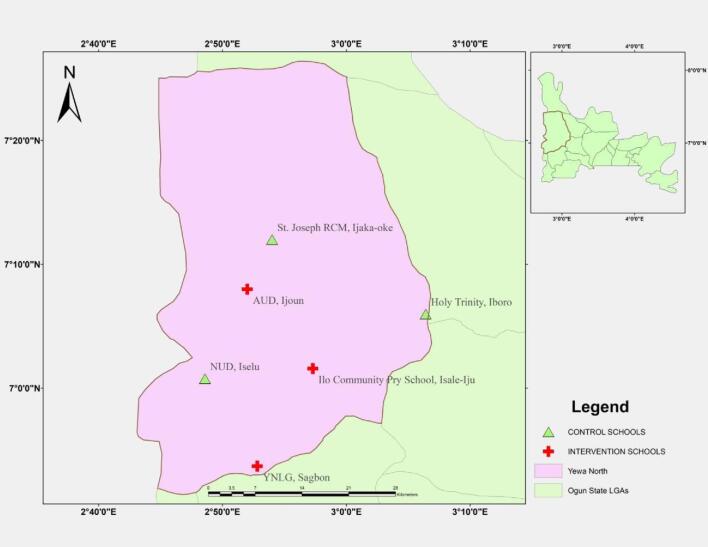
We conducted the study in Yewa North Local Government Area (LGA), a highly endemic LGA for urogenital schistosomiasis in Ogun State, Nigeria,16,17 where the rejection of school-based MDA with praziquantel in 2017 was reported.8 The LGA is about 77.8 km north of the capital city of Abeokuta. The primary sources of livelihood for inhabitants are farming and business. There are 132 public primary schools in the LGA, but only 57 (43.2%) participated in annual school-based MDA with praziquantel in 2017. The remaining 75 (56.8%) rejected school-based MDA with praziquantel in 2017 due to poor sensitisation, rumours of adverse side effects and death. Out of these 75 schools, 6 with wide travelling distances between them were selected to ensure there was no communication among the school children during the study. The schools were St Joseph RCM Primary School, Ijaka-Oke (7.20140°N, 3.36313°E), Holy Trinity Primary School, Iboro (7.09972°N, 3.10675°E), Nawairudeen Primary School, Iselu (7.0128°N, 2.80963°E), Ansar-Ud-Deen Primary School, Ijoun (7.22935°N, 3.43649°E), Ilo Community Primary school, Isale-Iju (7.02655°N, 2.95487°E) and Yewa North Local Government Primary School, Sagbon (6.895148°N, 2.880074°E). In each community, there is a river which is the transmission site for schistosomiasis. There is no public water supply or latrines or toilets. As such, the school children visit the river every day to play, swim, wash and fetch water for drinking and other domestic activities. The river also serves as a water source for the community's farming activities. Open defecation and urination are common practices in the surrounding bushes near the rivers. Figure 1 shows the locations of the intervention and control schools selected for the study.
Figure 1.
Map of Yewa North LGA, showing the six selected schools, with Ogun State inset.
Redesigning of the Schisto and Ladders board game
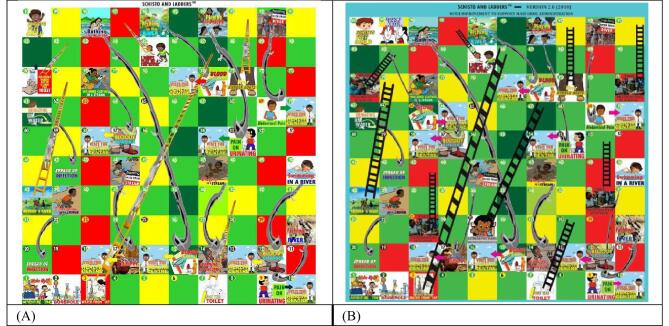
The name ‘Schisto and Ladders’ was coined from ‘Schistosomes and Ladders’. The game was designed using the children's game Snakes and Ladders as a template. A full description of the design of the first version of the game has been reported elsewhere.15 Briefly, the head of the Schistosoma worm was placed on squares inscribed with health education messages consisting of poor behavioural practices that are risk factors for schistosomiasis. The tail of the Schistosoma worm was placed on squares with health education messages warning about the consequences of these risky behaviours, adjacent to squares containing actions to be taken. Conversely, the feet of ladders were placed on squares inscribed with good behavioural practices that are preventative and control measures against schistosomiasis (Figure 2A).
Figure 2.
The Schisto and Ladders board game (A) version 1 and (B) version 2.
The computer design was created with Corel Draw computer software version x8, Corel Corporation, 1600 Carling Avenue, Ottawa ON K1Z 8R7, Canada. In the Schisto and Ladders board game version 2.0, health education messages to dispel rumours of possible risk of death resulting from taking praziquantel, encouraging praziquantel MDA and emphasising the need to eat before taking praziquantel to reduce incidences of side effects, were added. Necessary information for the modification and improvement of version 2 to support MDA was obtained by prestudy interactions with schistosomiasis control programme managers, parents, caregivers and pupils on why they rejected school-based praziquantel MDA. Additional information was derived from the literature and incorporated into the game to create version 2.5,6 On the game board, the health message ‘Take praziquantel in school’ was included on squares 23, 32, 71 and 80. On square 25, the message was ‘Eat before taking the drug (praziquantel)’. On square 99, accompanying the message of ‘Don't take the drug’, is a graphic picture of a child's peer group spreading rumours about praziquantel. On square 63, one consequence of not taking the treatment is depicted at the tail of a Schistosoma worm as ‘blood in urine’. There are health education messages on recommended actions if a child is experiencing any of the symptoms of schistosomiasis. On squares 9, 12, 16, 53, 57, 69 and 74, an arrow directs school children to go to the health centre to receive treatment with praziquantel. The length of each Schistosoma worm and ladder is proportional to the severity of the risk factor and behavioural change, respectively (Figure 2B). The aim of version 2 is to increase awareness and improve compliance of school children to school-based MDA with praziquantel. As in version 1, the game can be played by 2–4 children. The game starts when a player throws a 1 with a dice. A player moves up the board when they land at the foot of a ladder or downwards if they land on the head of a Schistosoma worm. Players are guided by the health messages on each square of the board. The players move the number of squares shown on the dice face when thrown and the first player to get to reach square 100 wins the game.15
Evaluation of Schisto and Ladders version 2
Study design and participation
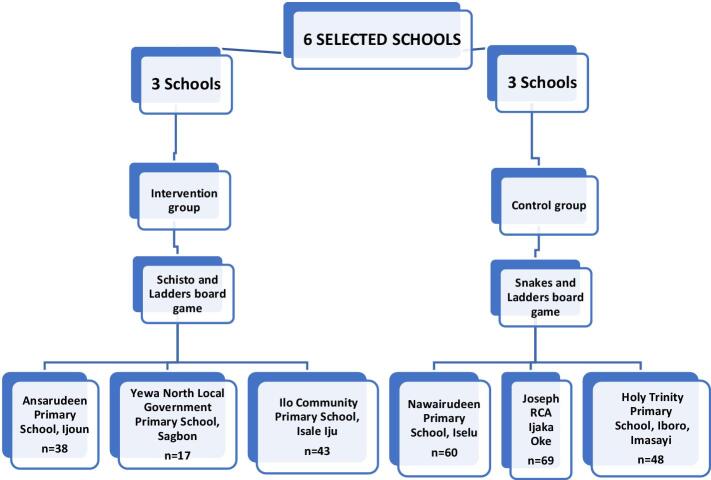
The study employed a single-blind, randomized controlled trial (RCT) setup among six selected public primary schools. The six selected schools were randomized into three intervention and three control schools by balloting. The intervention group played the Schisto and Ladders board game version 2 and the control group played the Snake and Ladders board game for 6 mo. The time for playing the games was set at 30 min every day during the school break period under the supervision of the school's headteacher. All the school children participating in the study played the games during break time. A roster was created by the head pupil appointed by the pupils in each school to ensure that each child played the game daily during break time. Each school received 15 board games and each game was played by 4 pupils. School children in both the intervention and control groups, including the teachers, were blinded to the study objectives to eliminate bias.
Before the trial, a baseline assessment of the prevalence and intensity of urogenital schistosomiasis was carried out, after which preassessment questionnaires were administered to collect quantitative data on knowledge, attitudes and practices (KAP) on schistosomiasis transmission, control and school-based MDA with praziquantel. A postassessment was conducted at 6 mo to re-evaluate KAP regarding schistosomiasis transmission and school-based MDA with praziquantel. Qualitative data were collected through focus group discussions (FGDs) among children, parents and caregivers from the intervention group. Treatment-seeking behaviour was determined by counting the number of children that requested praziquantel treatment in the intervention group. A flowchart of the RCT study design is shown in Figure 3. The trial was carried out from October 2018 to March 2019.
Figure 3.
Flowchart randomising the selected schools into the intervention and control groups.
Ethical aspects
The study was approved by the ethical committee of the Ogun State Ministry of Health, Abeokuta (HPRS/3817275) and permission to conduct the research was obtained from community leaders, parents, caregivers, teachers and headteachers of the selected schools. Only children who returned signed or thumb- printed informed consent forms were included in the study.
Statistical analysis
Data were analysed using IBM SPSS Statistics for Windows version 20.0 (IBM, Armonk, NY, USA). Analyses were performed to determine the differences in proportions between pre- and postassessment KAP using χ2, either for trend or independence, as appropriate. Data from FGDs were recorded, transcribed and analysed accordingly.
Results
The total number of pupils that participated in the study was 275. The participants comprised 98 children in the intervention group and 177 in the control group. The prevalence of urogenital schistosomiasis was 37 (37.8%) in the intervention group and 76 (42.9%) in the control group, while the mean intensity of infection was 29.06±7.99 and 47.91±10.49 in the intervention and control groups, respectively. There were no significant differences in gender (p=0.180), age group (p=0.340), prevalence (p=0.403) or mean intensity of infection (p=0.219) in both the intervention and control groups. The main characteristics of the study participants are summarised in Table 1.
Table 1.
Prevalence, mean intensity and characteristics of participants
| Variables | Int. (%) | Cont. (%) | Total (%) | p-value (Int. vs Cont.) |
|---|---|---|---|---|
| Gender | n=98 | n=177 | n=275 | |
| Male | 46 (46.9) | 98 (55.4) | 131 (47.6) | 0.180 |
| Female | 52 (53.1) | 79 (44.6) | 144 (52.4) | |
| Total | 98 (100) | 177 (100) | 275 (100) | |
| Age group, y | n=98 | n=177 | n=275 | |
| 5–9 | 29 (29.6) | 42 (23.7) | 71 (25.8) | 0.340 |
| 10–14 | 43 (43.9) | 74 (41.8) | 117 (42.5) | |
| 15–19 | 26 (26.5) | 61 (34.5) | 87 (31.6) | |
| Total | 98 (100) | 177(100) | 275 (100) | |
| Prevalence | ||||
| Male | 21 (45.7) | 39 (39.8) | 60 (41.7) | |
| Female | 16 (30.8) | 37 (46.8) | 53 (40.5) | 0.403 |
| Total | 37 (37.8) | 76 (42.9) | 113 (41.1) | |
| Mean intensity | 29.06±7.996 | 47.91±10.493 | 41.19±7.340 | 0.219 |
Abbreviations: Int., intervention schools; Cont., control schools
Knowledge of praziquantel and schistosomiasis
During the preassessment test, only two pupils (1.1%) in the control group had heard about praziquantel and none in the intervention group. By contrast, during the postassessment test, 53 (67.9%) in the intervention group now knew about the drug and 53 (67.9%) stated that praziquantel does not kill compared with 2 (1.1%) and 4 (2.3%) in the control group, respectively. There was a significant difference (p=0.000) in knowledge about the praziquantel drug and its safety in the intervention group compared with the control group. Similarly, knowledge about schistosomiasis among pupils, such as the symptom of ‘blood in urine’ (56 [71.8%]), mode of transmission, such as bathing and washing in the river (38 [48.7%]), avoiding going to the river as a preventive measure (30 [38.5%]) and going to the hospital for treatment if infected (56 [71.8%]), improved in the intervention group at postassessment compared with no improvement in the control group. There was a significant difference (p=0.000) in the knowledge of schistosomiasis in the intervention group compared with the control group (Table 2).
Table 2.
Knowledge about the praziquantel drug and schistosomiasis before and after the trial in intervention (Int.) and control (Cont.) schools
| Int. (%) | Cont. (%) | p-value | Int. (%) | Cont .(%) | p-value | Source of information | |
|---|---|---|---|---|---|---|---|
| Number of participants | 98 | 177 | 78 | 177 | |||
| Knowledge of schistosomiasis | |||||||
| No | 93 (94.9) | 167 (94.4) | 1.000 | 0 | 158 (89.3) | 0.000 | Playing Schisto and Ladders board game |
| Yes | 5 (5.1) | 10 (5.6) | 78 (100) | 19 (10.7) | |||
| Source of information | Playing Schisto and Ladders board game | ||||||
| Health worker | 0 | 3 (1.7) | 0.419 | 0 | 2 (1.1) | 0.000 | |
| Parent | 1 (1.0) | 4 (2.3) | 0 | 14 (7.9) | |||
| Radio | 0 | 1 (0.5) | 0 | 0 | |||
| Schisto and Ladders | 0 | 0 | 78 (100) | 0 | |||
| No response | 97 (99.0) | 169 (95.5) | 0 | 161 (91.0) | |||
| Symptoms | Messages on squares 12, 15, 57, 63 and 74 | ||||||
| Blood in urine | 1 (1.0) | 1 (0.6) | 0.178 | 56 (71.8) | 3 (1.7) | 0.000 | |
| Blood in faeces | 0 | 0 | 4 (5.1) | 0 | |||
| Blood in urine and faeces | 0 | 0 | 5 (6.4) | 0 | |||
| No response | 97 (99.0) | 176 (99.4) | 13 (16.7) | 174 (98.3) | |||
| Transmission | Messages on squares 30, 39, 47, 50, 61, 78, 92, 94, 96 and 98 | ||||||
| Bathing, washing, and fetching in river | 1 (1.0) | 0 | 0.178 | 38 (48.7) | 0 | 0.000 | |
| Fishing in river | 0 | 0 | 5 (6.4) | 0 | |||
| Playing | 0 | 0 | 1 (1.3) | 0 | |||
| No response | 97 (99.0) | 177 (100) | 34 (43.6) | 177 (100) | |||
| Where to seek treatment | Messages on squares 10, 16, 18, 54, 58, 64, 70 and 75 | ||||||
| Hospital | 1 (1.0) | 2 (1.1) | 0.933 | 56 (71.8) | 2 (1.1) | 0.000 | |
| No response | 97 (99.0) | 175 (98.9) | 22 (28.2) | 175 (98.9) | |||
| Preventive measure | Messages on squares 3, 10, 16, 18, 23, 30, 32, 39, 45, 47, 50, 54, 58, 61, 64, 70, 71, 73, 75, 78, 80, 85, 92, 94, 96 and 98 | ||||||
| Avoid bathing in the river | 0 | 0 | 0.178 | 10 (12.8) | 0 | 0.000 | |
| Avoid defecating in river | 0 | 0 | 1 (1.3) | 0 | |||
| Avoid fetching water from the river | 0 | 0 | 1 (1.3) | 0 | |||
| Avoid fishing | 0 | 0 | 1 (1.3) | 0 | |||
| Avoid playing | 0 | 0 | 1 (1.3) | 0 | |||
| Avoid going to the river | 1 (1.0) | 0 | 30 (38.5) | 0 | |||
| Avoid urinating in the river | 0 | 0 | 5 (6.4) | 0 | |||
| Avoid washing in the river | 0 | 0 | 1 (1.3) | 0 | |||
| Take praziquantel/visit the hospital | 0 | 0 | 1 (1.3) | 0 | |||
| Wearing rubber boots | 0 | 0 | 3 (3.8) | 0 | |||
| No response | 97 (99.0) | 177 (100) | 24 (30.7) | 177 (100) | |||
| Have you heard of praziquantel? | Messages on squares 22, 32, 71 and 80 | ||||||
| Yes | 0 | 2 (1.1) | 0.047 | 53 (67.9) | 2 (1.1) | 0.000 | |
| No | 74 (75.5) | 109 (61.6) | 0 | 109 (61.6) | |||
| No response | 24 (24.5) | 66 (37.3) | 25 (32.1) | 66 (37.3) | |||
| Will Praziquantel kill you? | Message on square 99 | ||||||
| Yes | 0 (0.0) | 0 (0.0) | 0.134 | 0 (0.0) | 0 (0.0) | 0.000 | |
| No | 0 (0.0) | 4 (2.3) | 53 (67.9) | 4 (2.3) | |||
| No response | 98 (100) | 173 (97.7) | 25 (32.1) | 173 (97.7) |
Attitudes regarding schistosomiasis and school-based MDA with praziquantel
The attitude of school children in the intervention group about any required behavioural changes concerning water contact increased significantly (p=0.000) after playing the board game compared with their preassessment attitude. Of the 78 pupils in the intervention group, 18 (23.1%) indicated that they had experienced changes in their attitude compared with 0 (0.0%) in the control group. The behavioural changes in attitude experienced in the intervention group were ‘I do not bathe in the river’, ‘I do not defecate in the river’, ‘I do not urinate in the river, ‘I do not visit the river’, ‘I make fewer trips to the river’ and ‘I wash with well water’ (Table 3).
Table 3.
Attitudes about schistosomiasis and MDA with praziquantel before and after the trial in intervention (Int.) and control (Cont.) schools
| Pretest assessment test | Post-test assessment test | ||||||
|---|---|---|---|---|---|---|---|
| Attitude questions | Int. (%) | Cont. (%) | p-value | Int. (%) | Cont. (%) | p-value | Source of attitudinal change |
| Number of participants | 98 | 177 | 78 | 177 | |||
| Experience of any river behavioural change | |||||||
| Yes | 0 (0.0) | 0 (0.0) | - | 18 (23.1) | 0 (0.0) | 0.000 | |
| No | 0 (0.0) | 0 (0.0) | 54 (69.2) | 0 (0.0) | |||
| No response | 0 (0.0) | 0 (0.0) | 6 (7.7) | 0 (0.0) | |||
| Behavioural change experienced | |||||||
| I do not bathe in the river | 0 (0.0) | 0 (0.0) | - | 2 (2.6) | 0 (0.0) | 0.000 | Playing of Schisto and Ladders board game |
| I do not defecate in the river | 0 (0.0) | 0 (0.0) | 1 (1.3) | 0 (0.0) | |||
| I do not urinate in the river | 0 (0.0) | 0 (0.0) | 5 (6.4) | 0 (0.0) | |||
| I do not visit the river | 0 (0.0) | 0 (0.0) | 2 (2.6) | 0 (0.0) | |||
| I make fewer trips to the river | 0 (0.0) | 0 (0.0) | 3 (3.8) | 0 (0.0) | |||
| I wash with well water | 0 (0.0) | 0 (0.0) | 5 (6.4) | 0 (0.0) | |||
| No response | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| 98 (100) | 177 (100) | 60 (76.9) | 177 (100) | ||||
Practices regarding schistosomiasis and school-based MDA with praziquantel
The frequency of practices which enhance schistosomiasis transmission reduced significantly in the intervention group compared with the control group postassessment. These included washing in the river (p=0.019), fetching water from the river (p=0.001) and urinating into the river (p=0.001). However, there was no significant difference between the two groups in the frequency of other practices which enhance schistosomiasis transmission, such as fishing (p=0.880), bathing in the river (p=0.085) and defecating in the river (p=0.0105) (Table 4).
Table 4.
Practices regarding schistosomiasis and MDA with praziquantel before and after the trial in intervention (Int.) and control (Cont.) schools
| Pretest assessment test | Post-test assessment test | |||||
|---|---|---|---|---|---|---|
| Practices questions | Int. (%) | Cont. (%) | p-value | Int. (%) | Cont. (%) | p-value |
| Number of participants | 98 | 177 | 78 | 177 | ||
| Do you wear rubber boots? | ||||||
| Yes | 3 (3.1) | 8 (4.5) | 0.343 | 7 (9.0) | 8 (4.5) | 0.000 |
| No | 94 (95.9) | 169 (95.5) | 29 (37.2) | 169 (95.5) | ||
| No response | 0 (0.0) | 0 (0.0) | 42 (53.8) | 0 (0.0) | ||
| Fishing | ||||||
| Once | 3 (37.5) | 1 (33.3) | 2 (66.7) | 1 (33.3) | 0.880 | |
| Twice | 4 (50.0) | 2 (66.7) | 0.780 | 5 (71.4) | 2 (66.7) | |
| Thrice | 1 (12.5) | - | 0 (0.0) | 0 (0.0) | ||
| Numerous | 0 (0.0) | - | 0 (0.0) | 0 (0.0) | ||
| Total | 8 (8.2) | 3 (1.7) | 7 (9.0) | 3 (1.7) | ||
| Washing | ||||||
| Once | 43 (50.0) | 96 (56.1) | 0.172 | 40 (76.9) | 95 (55.6) | 0.019 |
| Twice | 25 (29.1) | 38 (22.2) | 9 (17.3) | 39 (22.8) | ||
| Thrice | 14 (16.3) | 35 (20.5) | 2 (3.8) | 34 (19.9) | ||
| Numerous | 4 (4.6) | 2 (1.2) | 1 (1.9) | 3 (1.7) | ||
| Total | 86 (87.8) | 171 (96.6) | 52 (66.7) | 171 (96.6) | ||
| Fetching | ||||||
| Once | 12 (15.6) | 27 (16.9) | 0.008 | 21 (40.4) | 26 (16.2) | 0.001 |
| Twice | 30 (38.9) | 31 (19.4) | 12 (23.1) | 27 (16.9) | ||
| Thrice | 17 (22.1) | 60 (37.5) | 12 (23.1) | 63 (39.4) | ||
| Numerous | 18 (23.4) | 42 (26.2) | 7 (13.4) | 44 (27.5) | ||
| Total | 77 (78.6) | 160 (90.4) | 52 (66.7) | 160 (90.4) | ||
| Bathing | ||||||
| Once | 34 (38.6) | 66 (38.2) | 0.709 | 30 (60.0) | 69 (40.0) | 0.085 |
| Twice | 29 (33.0) | 49 (28.3) | 9 (18.0) | 47 (27.1) | ||
| Thrice | 19 (21.6) | 48 (27.7) | 10 (20.0) | 48 (27.7) | ||
| Numerous | 6 (6.8) | 10 (5.8) | 1 (2.0) | 9 (5.2) | ||
| Total | 88 (89.8) | 173 (97.7) | 50 (64.1) | 173 (97.7) | ||
| Urinating | ||||||
| Once | 32 (40.5) | 64 (57.1) | 0.024 | 41 (87.2) | 63 (56.2) | 0.001 |
| Twice | 31 (39.2) | 28 (25.0) | 1 (2.1) | 29 (25.9) | ||
| Thrice | 8 (10.1) | 16 (14.3) | 3 (6.4) | 16 (14.3) | ||
| Numerous | 8 (10.1) | 4 (3.6) | 2 (4.3) | 4 (3.6) | ||
| Total | 79 (80.6) | 112 (63.3) | 47 (60.3) | 112 (63.3) | ||
| Defecating | ||||||
| Once | 5 (45.4) | 30 (50.8) | 0.017 | 7 (100.0) | 30 (50.9) | 0.105 |
| Twice | 3 (27.3) | 13 (22.0) | 0 (0.0) | 13 (22.0) | ||
| Thrice | 0 (0.0) | 14 (23.8) | 0 (0.0) | 14 (23.7) | ||
| Numerous | 3 (27.3) | 2 (3.4) | 0 (0.0) | 2 (3.4) | ||
| Total | 11 (11.2) | 59 (33.3) | 7 (9.0) | 59 (33.3) | ||
Treatment-seeking behaviour
Before the beginning of the trial, all the school children in the intervention group had rejected praziquantel MDA. However, at the end of the trial, a total of 64 out of 98 school children (65.3%) who played the Schisto and Ladders board game version 2 significantly (p=0.001) sought praziquantel treatment from their headteacher by putting down their names for treatment (Table 5). Those who did not seek treatment stated that they needed to obtain permission from their parent or caregiver before putting their name down for treatment.
Table 5.
Assessment of the impact of the Schisto and Ladders board game on the health-seeking behaviour of school children in intervention schools
| Name of school | Number of pupils | Those seeking praziquantel treatment | p-value |
|---|---|---|---|
| Ansar-Ud-Deen Primary School, Ijoun | 38 | 29 (76.3) | 0.000 |
| Ilo Community Primary school, Isale Iju | 43 | 18 (41.9) | |
| Yewa North Local Government Primary School, Sagbon | 17 | 17 (100) | |
| Total | 98 | 64 (65.3%) |
FGDs with school children in the intervention group
After playing the Schisto and Ladders board game version 2 for 6 mo, at the FGDs, children in the intervention group stated that the game had taught them to stop visiting the river to wash, urinate, defecate, play, fish or bathe and to take praziquantel when given. One pupil from the Ilo Community Primary School said, ‘It taught us to stop defecating in the river.’ A pupil from Ansar-Ud-Deen Primary School said, ‘It taught me to go to the hospital when I have schistosomiasis and to take praziquantel when given.’ The consequence of refusing MDA with praziquantel was noted as wrong and that an individual will continue to have schistosomiasis or could die, as expressed by a schoolboy from Ansar-Ud-Deen Primary School, who said, ‘The individual that rejects praziquantel may die.’ All the school children in the intervention group mentioned the common symptoms of schistosomiasis infection, the passing of ‘blood in urine’ and ‘blood in faeces’, as knowledge they had gained by playing Schisto and Ladders version 2. The children in the intervention group stated that not bathing, washing, playing or urinating into the river are ways of preventing the transmission of schistosomiasis. They quoted the health education messages in the game such as ‘Fetching water from the tap’, ‘Taking praziquantel’, ‘Going to the hospital when infected’, ‘Wearing rubber boots to the river’ and ‘Not defecating in the river’ with regard to preventing schistosomiasis.
The FGDs also showed that from playing the game, school children learned they must eat before taking praziquantel to minimise the side effects of the drug and that praziquantel was safe. When asked about the safety of praziquantel and necessary measures to minimise side effects when taking praziquantel, one pupil responded that ‘Praziquantel is safe, and that food should be eaten before taking praziquantel.’ Reasons for rejecting school-based MDA with praziquantel were attributed to instructions issued by parents and caregivers. One pupil from Ansar-Ud-Deen Primary School said, ‘I wasn't allowed to come to school on the day the drug was given.’ A pupil from the Ilo Community Primary School said, ‘Our parents said we should not take drugs in school.’
FGDs with parents and caregivers of children in the intervention group
Parents and caregivers of school children in the intervention group provided various reasons for their rejection of MDA with praziquantel, including fear of possible side effects of the drug, such as vomiting, fainting observed after taking praziquantel, as well as a risk of death. One parent of a pupil at Ilo Community Primary School said, ‘Treatment was rejected because of rumours of death and fainting of children after taking praziquantel.’ The parents and caregivers suggested that children should be diagnosed as infected before being given any treatment and that parents should be informed about school-based MDA with praziquantel prior to treatment. For instance, one parent of a pupil at Ansar-Ud-Deen Primary School said, ‘I will accept the treatment of my child after examination and if my child is found to be infected with the disease.’ Similarly, a female parent of another pupil at Ansar-Ud-Deen Primary School said, ‘Parents should be called and be informed about MDA before the commencement of treatment by the government.’ The parents expressed their support for their children playing the Schisto and Ladders board game, provided it did not interfere with their academic activities.
Discussion
Rejection of school-based MDA with praziquantel is a significant issue that has resulted in low coverage of treatment for schistosomiasis control in school-aged children.5,6,9 Therefore, the instances of drug rejection in Ogun State, where MDA with praziquantel started in 2017, was not a surprise.8 Fears related to praziquantel can be quelled using effective health education as a sensitisation tool both before and during school-based MDA. The Schisto and Ladders board game version 2 encourages the uptake of praziquantel among school children. New health education messages were added in version 2 to dispel the rumours of risk of death and possible side effects caused by taking praziquantel, and also that school children should eat at home or in school before taking praziquantel, to reduce the occurrence of potential drug-related side effects. The Schisto and Ladders board game version 2 addresses the problem of drug rejection and promotes an acceptance of and compliance to school-based MDA with praziquantel.
The significant changes in the knowledge of pupils concerning schistosomiasis and the safety of praziquantel from the pre- and postassessment tests suggest that the Schisto and Ladders board game version 2 can deliver specific educational messages to rapidly induce behavioural changes in a target population. These results are similar to those obtained by use of the Juma no Kichocho comic-strip medical booklet in Zanzibar.11 The behavioural changes expressed by the school children, such as wearing rubber boots, avoiding the river, not bathing in the river and avoiding urinating and defecating in the river, demonstrate the potential effectiveness of educational games in changing behavioural practices. However, without the provision of safe water and sanitation, it is difficult, if not impossible, for this knowledge to be translated into sustainable practices with which to reduce morbidity, hence the need for a novel health education tool such as Schisto and Ladders version 2 to support compliance to school-based MDA with praziquantel. Educational games should be investigated for delivering health education messages as part of behavioural change intervention programmes. There are several children's and adult's games that could be adapted to deliver health education messages rather than the use of posters and flyers, which are currently popular in many disease control programmes. However, it is vital that when considering any children's game for modification, a participatory community approach involving parents, caregivers and teachers is employed when identifying which game(s) should be adapted, which in turn strengthens community engagement and participation in disease control.18 The adaption of the Snakes and Ladders game to Schisto and Ladders arose because of the popularity of the original game among children.15 The acceptance of the Schisto and Ladders board game version 2 by children shows that they welcomed the modification of the Snakes and Ladders game. Including health education messages captivated the children and they enjoyed learning while playing the game. The inscription of health education messages on the board of the game made it more appealing for playing and learning among school children. The innovative use of an existing children's board game is an excellent idea. It guarantees its adaptability and applicability, especially in those low- and middle-income countries endemic with schistosomiasis, where the applicability of electronic games such as computer and video games may be subject to resource constraints.
The Schisto and Ladders board game version 2 had a positive impact on the treatment-seeking behaviour of children: 65.3% of pupils in the intervention group who had earlier rejected treatment put down their names for treatment after playing the game, indicating that the board game had a positive influence on children, encouraging them to accept treatment against the wishes of their parents and caregivers. The potential of the Schisto and Ladders board game version 2 to significantly improve awareness of and knowledge about schistosomiasis control, including school-based MDA with praziquantel, has been demonstrated in this RCT. The game can be used as a health education and sensitisation tool by schistosomiasis control programme managers to support compliance with school-based MDA with praziquantel.
Acknowledgements
The authors are grateful to parents, headteachers, staff and pupils at Ansar-Ud-Deen Primary School, Ijoun, Yewa North Local Government Primary School, Sagbon and Ilo Community Primary School, Isale Iju, all in Yewa North LGA, Ogun State, for their cooperation, support and valuable contribution to the animated pictures used in the game. We thank the Baales of Isale-Iju and Sagbon communities for their support in the mobilisation of their communities. We appreciate the support of Ogun State Universal Basic Education Board (SUBEB) for granting permission to use their school system for the study. Finally, we thank Dave Melkman of Manta Ray Media, United Kingdom for digital media support.
Contributor Information
Cynthia Uchechukwu Ejike, Department of Pure and Applied Zoology, Federal University of Agriculture, Abeokuta, Nigeria.
Akinola Stephen Oluwole, COUNTDOWN implementation research Consortium, Ogun State; Sightsavers Nigeria Country Office, 1 Golf Course Road, PO Box 503, Kaduna State, Nigeria.
Olaitan Olamide Omitola, Department of Pure and Applied Zoology, Federal University of Agriculture, Abeokuta, Nigeria.
Adedotun Ayodeji Bayegun, Department of Pure and Applied Zoology, Federal University of Agriculture, Abeokuta, Nigeria.
Islamiat Yetunde Shoneye, Neglected Tropical Diseases Unit, Ogun State Ministry of Health, Oke-Mosan, Abeokuta, Nigeria.
Bolanle Idowu Akeredolu-Ale, Department of Communication and General Studies, Federal University of Agriculture, Abeokuta, Nigeria.
Oluwafunmilayo Aduke Idowu, Department of Pure and Applied Zoology, Federal University of Agriculture, Abeokuta, Nigeria.
Chiedu Felix Mafiana, Research Administration and Advancement, National Open University of Nigeria, Abuja, Nigeria.
Uwem Friday Ekpo, Department of Pure and Applied Zoology, Federal University of Agriculture, Abeokuta, Nigeria.
Authors’ contributions
UFE, CUE, OAI, ASO and BIA designed the game and developed the study protocol for its evaluation. CUE, OOO and AAB participated in data collection, CUE and OOO conducted the analysis and wrote the first draft of the manuscript, which UFE, ASO and IYS reviewed before finalising it. UFE, CUE, OAI, BIA, AAB, ASO, IYS and CFM approved the final draft.
Funding
This study was supported by the Stephen Oluwole Awokoya Foundation for Science Education, M.Sc. Scholarship awarded to CUE.
Competing interests
None declared.
Ethical approval
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Data availability
The data underlying this article will be shared upon reasonable request to the corresponding author.
References
- 1. World Health Organization . Preventive Chemotherapy in human helminthiasis. Coordinated Use of Anthelminthic Drugs in Control Interventions: a Manual for Health Professionals and Programme Managers, 2006.http://apps.who.int/iris/bitstream/10665/43545/1/9241547103_eng.pdf [accessed December 22, 2019]. [Google Scholar]
- 2. Fenwick AO. Praziquantel: do we need another antischistosoma treatment? Future Med Chem. 2015;7(6):677–80. [DOI] [PubMed] [Google Scholar]
- 3. Landouré A, Dembélé R, Goita Set al. Significantly reduced intensity of infection but persistent prevalence of schistosomiasis in a highly endemic region in Mali after repeated treatment. PLoS Negl Trop Dis. 2012;6(7):e1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lelo AE, Mburu DN, Magoma GNet al. No apparent reduction in schistosome burden or genetic diversity following 4 years of school-based mass drug administration in Mwea, Central Kenya, a heavy transmission area. PLoS Negl Trop Dis. 2014;8(10):e3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hastings J. Rumours, riots, and the rejection of Mass Drug Administration for the treatment of Schistosomiasis in Morogoro, Tanzania. J Biosoc Sci. 2016;48:16–39. [DOI] [PubMed] [Google Scholar]
- 6. Muhumuza S, Olsen A, Katahoire A, et al. Uptake of preventive treatment for intestinal schistosomiasis among school children in Jinja District, Uganda: a cross-sectional study. PLoS One. 2013;8(5):634–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ekpo UF, Hurlimann E, Schur N, et al. Mapping and prediction of schistosomiasis in Nigeria using compiled survey data and Bayesian geospatial modelling. Geospat Health. 2013;7(2):355–66. [DOI] [PubMed] [Google Scholar]
- 8. Olukoya O. Panic In Ogun Schools Over Deworm Exercise. Nigerian Tribune Newspaper, 2017. http://tribuneonlineng.com/panic-ogun-schools-deworm-exercise/ [accessed March 30, 2020]. [Google Scholar]
- 9. Parker M, Allen T. Does mass drug administration for the integrated treatment of neglected tropical diseases really work? Assessing evidence for the control of schistosomiasis and soil-transmitted helminths in Uganda. Health Res Policy Syst. 2011;9:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Guanghan H, Dandan L, Shaoji Z, et al. The Role of Health Education for Schistosomiasis Control in Heavy Endemic Area of Poyang Lake Region, People's Republic of China. Southeast Asian J Trop Med Public Health. 2000;31(3):467–72. [PubMed] [Google Scholar]
- 11. Stothard JR, Mook P, Mgeni AF, et al. Control of urinary schistosomiasis on Zanzibar (Unguja Island): a pilot evaluation of the educational impact of the Juma na Kichocho health booklet within primary schools. Mem Inst Oswaldo Cruz. 2006;101(1):119–24. [DOI] [PubMed] [Google Scholar]
- 12. Stothard JR, Khamis AN, Khamis IS, et al. Health Education and the control of urogenital schistosomiasis: Assessing the impact of the Juma na Kichocho comic-strip medical booklet in Zanzibar. J Biosoc Sci. 2016;48:40–55. [DOI] [PubMed] [Google Scholar]
- 13. Bieri FA, Gray DJ, Williams GM, et al. Health-education package to prevent worm infections in Chinese schoolchildren. N Engl J Med. 2013;368:1603–12. [DOI] [PubMed] [Google Scholar]
- 14. Bieri FA, Yuan L, Li Y, et al. Development of an educational cartoon to prevent worm infections in Chinese schoolchildren. Infect Dis Poverty. 2013;2:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ejike CU, Oluwole AS, Mogaji HO, et al. Development and testing of Schisto and Ladders™, an innovative health educational game for control of schistosomiasis in schoolchildren. BMC Res Notes. 2017;10:236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ekpo UF, Mafiana CF. Epidemiological studies of urinary schistosomiasis in Ogun State, Nigeria: identification of high-risk communities. Nig J Parasitol. 2004;25:111–9. [Google Scholar]
- 17. Ekpo UF, Mafiana CF, Adeofun CO, et al. Geographical information system and predictive risk maps of urinary schistosomiasis in Ogun State, Nigeria. BMC Infect Dis. 2008;8:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Oluwole AS, Dean L, Lar L, et al. Optimising the performance of frontline implementers engaged in the NTD programme in Nigeria: lessons for strengthening community health systems for universal health coverage. Hum Resour Health. 2019;17:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article will be shared upon reasonable request to the corresponding author.