Abstract
Background
Families with preterm infants find life after hospital discharge challenging and need tailored support to thrive. The “Transition to Home (TtH)”-model offers structured, individual support for families with preterm infants before and after hospital discharge. TtH improves parental mental health and competence, promotes child development and fosters interprofessional collaboration (IPC).
Aim
Evaluate the TtH-models’ structure and implementation process and its associated interprofessional collaboration from the healthcare professional’s (HCP) perspective.
Methods
This qualitative explorative study thematically analyzed four focus group interviews (n=28 HCP) and an open-ended questionnaire with general pediatricians (n=8).
Results
The main themes of the thematic analysis were the benefits of the TtH-model, tailored parental support, the challenges of changing interprofessional collaboration, facilitators and barriers to successfully implementing the model, and feasibility and health economic limits. HCP acknowledge that continuous family-centered care led by an advanced practice nurse (APN) supports, strengthens, and relieves families with preterm infants in the transition from hospital to home. Families in complex situations benefit most. The TtH-model incorporates key aspects of integrated care like shared decision-making, considering family preferences, and defining the APN as the family’s main contact. HCP want network collaboration but found communication, cooperation, and reorganization challenging in the new IPC process. IPC challenges and involving many HCP in family care can create parental oversupply, negatively affect treatment outcomes, and raise health care costs.
Conclusion
These challenges need to be addressed to ensure sustainable implementation of the model. The roles and tasks of HCP should be clearly distinguished from each other, and HCP must have time to learn this new form of IPC. Learning requires time, effective communication strategies, and leadership support. Political action is also required to implement new models of care, including regulating advanced practice roles and developing new financing models.
Keywords: interprofessional collaboration, transition from hospital to home, new model of care, advanced practice nurse, preterm birth, qualitative research
Introduction
After discharge from a neonatal intensive care unit (NICU), preterm infants and their families continue to be vulnerable.1 Although advances in medical and technical care ensure the survival of more preterm infants, there has not been a corresponding reduction in neonatal and long-term cognitive, motor and behavioral morbidities.2–4 Parents of these infants may have strong psycho-emotional reactions including depression, anxiety, posttraumatic stress disorder and parenting stress, lasting into the former preterm infants’ childhood.5–8 When parents suffer from these effects, their parenting competence declines and they may interact less with their child.9,10 Parents’ mental health and ability to cope with the consequences of premature birth and the home environment of the child have a significant effect on a child’s development.7,11 Interventions to improve child and parental outcomes must be well tailored; they should provide family-centered care, psychosocial support, continuity of care, and be based on smooth interprofessional collaboration (IPC) that begins in the antepartum period, continues throughout hospitalization, and makes the transition from hospital to home.10,12
Swiss hospitals do not offer continuous and coordinated support to help prevent developmental and emotional deterioration when preterm infants and their parents transition from hospital to home. Midwives, pediatric community health care nurses, and advisory services do make home visits, but they lack specific expertise in caring for preterm infants and their families at home. There is also a gap in transitional care between hospital and home, and no continuity in the specific care of families affected by preterm birth.1
The Transition to Home Model (TtH)
An academic-practice partnership between the University Children’s Hospital Bern and the Bern University of Applied Sciences was the basis for a new interprofessional model of transitional care. It was developed to support families with preterm infants, beginning at birth and ending six months after hospital discharge. The model adheres to principles of integrated care, including interventions and processes to improve interprofessional collaboration between stakeholders in the health care system and ensure that treatment and care of patients is coordinated optimally along the treatment continuum.13 The “Transition to Home (TtH)” model is designed to optimize transitional care of families with preterm infants between 24 and 35 weeks of gestational age by giving parents and infants structured, individual support, improving parental mental health and competence, promoting the child’s development, and optimizing interprofessional collaboration (IPC). This model is based on a German model that supports the families of chronically and severely ill children14 and on Naylor’s “Transitional Care Model” for hospitalized elders,15 which was developed in the US. Naylor’s model based on a model developed by Brooten et al, in which an Advanced Practice Nurse (APN) prepared very low birth weight infants for earlier discharge.16 To develop the model, we solicited the perspectives of users and health care professionals (HCP) with a range of expertise.
The APN plays a significant role in the TtH-model. The APN is an academically trained nurse with a master’s degree, specializing in care for a specific population. The APN’s competencies include clinical practice, ethical decision-making, counseling and support of other HCP, fostering IPC, research practice, and leadership tasks. An APN considers complex care processes as a part of integrated care and gives continuous support to affected parents where necessary.17 In Switzerland, APN roles are still emerging18,19 and there is still no legal framework in place.20 Internationally, APNs have improved patient outcomes and lowered health care costs, eg, by discharging patients earlier, delaying re-hospitalization, and shortening hospital stays.21–23 Comprehensive and personalized discharge planning and a continuum of care after discharge improved patient satisfaction.21,24
In the TtH-model, the academically trained APN heads a team of three specialized nurses in NICU. Table 1 shows the main components the interprofessional team offers, within the TtH-models.
Table 1.
Main Components of the TtH-Model
| Components of Model | Description |
|---|---|
| Advanced Practice Nurse (APN) support | All team members comprehensively plan individual discharges, hold consultations, closely coordinate and collaborate with different HCP so information flows freely, and participate in regular interprofessional exchanges. The APN takes a family-centered approach to assessing the needs of the families and to making joint decisions. The APN regularly visits, consults and educates parents and acts as a continuous partner. After discharge, the APN offers three systematic follow-up calls, telephone support and up to nine follow-up home visits to assess the physical and mental health of parents and infants, to evaluate interventions and adapt the care. |
| Psychological support | Psychological support is provided to all families, comprising assessment and at least three follow-up consultations before the infant is discharged. Its goal is to re-establish emotional stability, improve parents’ ability to cope, prevent parents and family from developing adaptive disorders, and protect them from developmental disorders. |
| Lactation consultation | During hospitalization, the lactation consultant responds to the needs of the families, including fathers. Its aim is to strengthen parent-child bonds and show parents how to meet their child’s nutritional needs. |
| Physical therapy | The physical therapist provides treatment after an assessment. In a single consultation, the family learns how to handle their premature infant in everyday life, in a manner appropriate to the infant’s developmental stage. |
| Support by social worker | Social workers closely collaborate with the APN and are involved with every family. They help families cope with daily life after preterm birth, during and after hospitalization. |
| Music therapy | Music therapy is offered during hospitalization to stabilize the child, support its development, reduce parents’ anxiety and enhance their self-efficacy.25,26 |
| Interprofessional roundtable discussion | Interprofessional roundtable discussions with involved HCP and parents are held twice while the preterm infant is hospitalized and once three months after discharge. The meetings seek consensus on optimal support for families in care. |
Both the interprofessional roundtable discussions and the APN were designed to foster IPC in our model because effective IPC is a foundation for safe, high-quality patient care and a good work environment for HCP.27,28 Successful IPC depends on open communication, cooperation, trust, common goals, constructive debate that honors different opinions, mutual acceptance, and a willingness to take responsibility for processes.29,30
We pilot tested and implemented the TtH-model between February 2018 and March 2020 in the Neonatology of the University Children’s Hospital Bern. This study was an integral part of the pilot test because it solicited the HCP perspective to evaluate the structure and implementation of the TtH-model including the process of IPC. Results will help us adjust the model and our interprofessional approach to improve our implementation. We set out to identify and characterize the experiences of involved HCP a) in collaboration with parents; b) with IPC, and c) solicit their opinions on the implementation process and the intervention’s feasibility.
Methods
To evaluate the TtH-model, its structure, and the IPC from the HCP perspective, we designed a qualitative explorative study with focus group interviews. We also distributed a questionnaire containing open questions to the group of general pediatricians, most of whom could not attend the focus groups. We chose focus groups because they are particularly appropriate to investigating poorly understood phenomena, interrelated aspects, sources of complex behaviors and motivations, and the social reality of participants.31–33 Investigations took place between September 1st 2019 and July 31st 2020.
Sample
A total of 204 HCP were involved in implementing the TtH-model: APNs; registered nurses with expertise in neonatology and intensive care; pediatric community health care nurses; senior physicians in neonatology, neurorehabilitation, neuro- and pediatric surgery, pneumology and gastroenterology; music therapists; physical therapists; psychologists; speech therapists; health care chaplains; social workers; nutritionists; lactation consultants; experts from the family advisory service; midwives; and, general pediatricians. We included HCP who a) were involved in caring for one or more families in the pilot-study treated within the TtH-model; b) spoke and read German well; c) had worked at their profession for the previous two years.
We included 28 HCP and assigned them to one of four heterogeneous focus groups (6–8 participants per group). We wanted a good mix related of age, gender, and profession to enrich the discussion and elicit the challenges raised by ICP.34 According to Krueger and Casey,34 several small focus groups of participants can share opinions and discuss them, allowing researchers to identify up to 90% of relevant topics in their research area and to achieve data saturation.35
Ethical Considerations
We explained the study and the methods we used to the HCP, in detail, by mail and in team meetings. All participants received written information describing the study, data collection procedures, including audiotaping of the focus group interviews, privacy procedures, confidentiality, and their right to withdraw participation at any time during the study. Participants names were replaced by a code and all data that could have identified participants were removed from transcripts to guarantee anonymity. Participants could contact the responsible study coordinator at any time. All HCP consented to participate. All data is stored in a protected research server of the Bern University of Applied Sciences. The cantonal ethics committee in Bern, Switzerland approved the study (Project-ID: 2017–01249).
Data Collection
We used a semi-structured interview guide (see Supplementary Table 1) containing a thematically focused invitation to narrate or explain freely and discuss within the group. The guide helped us identify important topics and structure group discussions.36,37 We based the open-ended questionnaires on this interview guide. We tested the interview guide with two groups of HCP in a feasibility study; it helped us to improve the guide. We pre-tested the open-ended questionnaires with a general pediatrician who was not involved in the current study. We were able to assure questions are clearly articulated, understandable, suitable and to answer purposefully.
We held the focus groups in January and February 2020 in a neutral environment at Bern University of Applied Sciences, and they were guided by a trained moderator and facilitator. The last author moderated the first focus group interview and the second author was present. The second author led the remaining three interviews. The moderator led the process, raised key issues and encouraged all members to participate. They also observed the discussion, set up the equipment, and systematically summarized each interview. The focus groups lasted between 90 and 105 minutes, were audio recorded, and transcribed verbatim.
We anonymized the questionnaires returned by general pediatricians, extracted the data, and integrated it into our qualitative analysis.
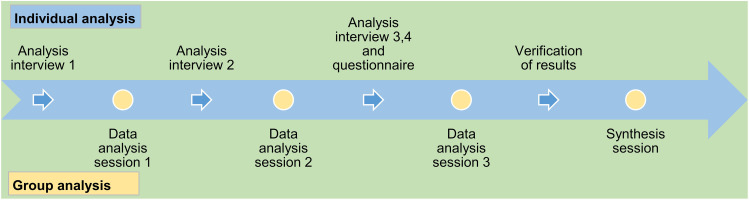
Data Analysis
We thematically analyzed (TA) the data from the focus group interviews and the questionnaires, based on the method described by Braun and Clarke.38 TA is flexible and adaptable, since its theoretical framework is not predefined. We used TA to identify, analyze and report patterns within data,38 and to assess the experiences, attitudes and perceptions shared by our focus group participants. TA allowed us to explore interprofessional perceptions of the TtH-model, differing realities, and specific incidents. Four methodologically trained researchers together conducted the analysis. Three are experts in prematurity and work in the NICU in the hospital where the study was conducted. We followed the six TA steps Brown and Clark38 described: (1) familiarize oneself with the data; (2) generate initial codes; (3) search for themes; (4) review themes; (5) define and name themes; and, (6) produce a report. Transcripts from each focus group were analyzed by individual team members and by the whole team, so we could compare and discuss emerging findings and come to consensus on final themes, so our results would be credible.39 Figure 1 shows the process of data analysis.
Figure 1.
Process of qualitative data analysis.
First, we read and reread the focus group transcripts to familiarize ourselves with the data. Second, we used an inductive approach to create codes, exploring and identifying latent themes in the data.37,38 We then added a deductive approach37 to deepen our structural evaluation: we used our inductive codes and research questions to create a structured list of codes that we continuously expanded and consolidated based on our continuing analysis. We used this deductive structure then build inductive themes and categories, in an iterative process in which we analyzed data and then coded extracts. We used ATLAS.ti. Version 8, a qualitative data management program, to support our analysis, and RStudio® to analyze the socio-demographic data describing our sample.
We ensured rigor39 by systematically summarizing and reflecting the content back to participants after the focus groups, to give them the opportunity to complete, correct, and confirm their statements. We addressed transferability by seeking to reach data saturation and thoroughly documenting and describing our research process and ensured confirmability by creating an electronic audit trail that includes our notes and coding rationale.
Results
Participants
The study sample consisted of N=36 HCP (n=28 focus group participants; n=8 questionnaires of general pediatricians), of whom 32 (88.8%) were women and four (11.1%) were men.
Table 2 shows the sociodemographic characteristics of our sample. The heterogeneous focus group mix included HCP of different ages, working experience, and profession, including three APN’s, two community health care nurses, one expert on family advisory service, two lactation consultants, two midwives, one music therapist, nine nurses (NICU and neonatal intermediate care), three physicians, two physical therapists, one psychologist and two social workers. Of those we invited, 82.3% (n=168) refused to participate. We received reasons for non-participation from 56.2% (n=94) of those who refused; reasons included little involvement in the project (56.2%), limited working experience (12.4%), no time (10.5%), no interest (3.8%), or other (17.1%), eg, maternity leave, illness, termination of employment or holidays.
Table 2.
Sociodemographic Characteristics of Involved HCP
| Sociodemographic Aspects | Mean | Range |
|---|---|---|
| Age in years | 49 | 28–70 |
| Working experience in years | 23 | 5–40 |
| Working experience in their specific role in years | 13 | 1–34 |
| Employment in % | 74 | 30–100 |
Qualitative Findings
The Benefits of the TtH-Model
HCP described the new model TtH as beneficial and useful for families with preterm infants, especially for families challenged by complex situations or those with infants treated by many HCP.
I see the need. This transition to home is not easy. We regularly hear that children who were discharged needed to be re-hospitalized three days later [...] #00:06:58-9#. [FG1]
HCP also said that the model was needed most by socially disadvantaged parents with limited resources, those with no supporting family system, or those unfamiliar with the Swiss health care system (eg, families with migration background or an ill parent). According to HCP, these families make the most unnecessary visits to the emergency department. HCP criticized the pilot-study for including mostly families with an intact family in a stable environment.
And those who were more in need of such a support were excluded from the project, although they could absolutely benefit of the services [...] Those who really have limited resources. #01:26:50-2#. [FG4]
HCP agreed that the model offers continuous support and smooths the transition to home, but said it needs to include the families who would most benefit.
Tailored Parental Support
HCP said that standard care usually places parents in the hospital into an unfamiliar and overwhelming situation, where they worry about the health condition and development of their child. They struggle with fears, feel guilt, and require intensive support and monitoring from HCP during hospitalization. After discharge, this intensive care-continuum is interrupted, and parents are left feeling alone, uncertain, and often overwhelmed by caring for their preterm infant.
In the hospital, the parents are protected. After discharge, the entire environment they have known falls apart. They fall into a deep crisis. #00:21:10-2#. [FG3]
HCP agreed that the new model could provide a continuum of care between the in- and outpatient setting by building a service bridge:
[...] it is a harsh break, and I was very pleased about that bridge from the medical to the home setting. #00:08:43-3#. [FG1]
When the TtH-model was introduced, HCP saw positive developments in parents; they could express how they felt, participated in decision-making processes, and seemed empowered and self-confident in caring for their preterm infant. HCP assumed this was associated with newly introduced structures, like the interprofessional roundtable discussions and APN support. The physical therapist thought parents’ self-efficacy improved because they were given more intensive instruction in infant handling. The music therapist emotionally supported parents and gave developmental support to preterm infants and the whole family. Physical and music therapists felt collaboration with parents improved.
HCP also had negative experiences. Some thought that parental oversupply was a risk, and that parents might be overwhelmed, and the TtH-model might cause learned helplessness because too many different HCP were caring for the baby. HCP wanted to optimally support families with their expertise, and engaged the parents in many discussions, several assessments, overlapping educational sessions, and flooded them with information.
Because many HCP were involved, it was difficult for some of them to have contact with parents. Since they were aware of these challenges, HCP suggested making the model more focused and letting parents decide the amount of support they need from each HCP. An HCP suggested a modular service:
It needs a system with different components from which the family can choose the ones they currently need. #01:25:02-7#. [FG3]
HCP agreed that the interventions in the model had positive effects for parents but that not all interventions needed to be delivered to each family. Transitional care should be tailored to the needs of the individual family and involve the right HCP.
The Challenges of Changing Interprofessional Collaboration
HCP agreed that optimal parental support depends on optimal IPC, especially in the three key areas of communicating, cooperating, and reorganizing the IPC.
Communication: HCP communicated quickly and were purposeful when they directly contacted each other, and when all HCP involved in the treatment process attended meetings and documented patient information accurately. HCP agreed that making the APN the key contact person improved the communication process. They organized meetings among HCP, contacted HCP who provided follow-up services, and consulted specialists to discuss specific health issues. But general pediatricians rarely interacted with the APN directly. They requested direct contact before the infant left the hospital to check on the infant’s health condition and determine the family’s need for support. HCP in the hospital found exchanges with external HCP proved especially challenging because there was no standardized cross-institutional information and documentation system: documentation overlapped and gathering information was time-consuming.
It is a tremendous effort to make sure that the important information gets to the right person. #01:01:54-7#. [FG4]
HCP thus asked for a single, cross-institutional information and documentation system that would save time and optimize communication.
Cooperation: HCP cooperated best when they met regularly, and their areas of responsibility were clearly defined. When they failed to cooperate it created misunderstandings, treatment overlaps, and reduced quality of care. According to the HCP, two factors were key in improving inter-professional cooperation. First, the APN should take the lead and define its role and tasks clearly; otherwise, HCP might be unsure about the role of this additional stakeholder. Second, the number of primary caregivers must be clearly defined because the TtH-model may involve too many HCP in care, slowing down and complicating the IPC.
Reorganizing the IPC: We identified a strong preference for a collaboration network among HCP. The TtH-model established basic principles like roundtable discussions and HCP saw the potential advantages of cooperating in this fashion.
I am very happy the network exists because solutions can be found quicker if problems arise. [GP questionnaire]
HCP were frustrated with the internal hierarchical structures common in hospitals, where rapid changes in therapeutic agreements were made without discussions between professionals. Other characteristics of IPC included strains, ambiguities, and conflicts, especially in overlapping fields of activity. HCP feared losing competencies, responsibilities, and becoming superfluous. But their concerns disappeared if these negative feelings were addressed, or others’ work supported their own. To improve IPC and successfully implement the TtH-model, HCP thought existing structures would need to change, new roles and tasks should be clearly defined, and time should be allotted for interprofessional exchange among all HCP.
Facilitators and Barriers of a Successful Model Implementation
When they discussed how best to implement the model, HCP focused on (1) lack of clarity about the APN’s role, (2) the APN’s home visits, and (3) the usefulness and effectiveness of the interprofessional roundtable discussions.
The role of the APN: There was controversy over the APN’s role. On the one hand, the APN played a key role in supporting parents and ensuring continuity of care during the transition from hospital to home, bridging the care process. HCP described the APN as the key person parents trusted; the APN was responsible for their security, stability, and orientation. HCP saw the APN as an expert in neonatology, with a focus on family-centered care, and as a coordinator and translator in complex situations or when there was conflict. An APN stated:
I took up the family’s concerns and tried to find a solution together with the family. Particularly, if there were disagreements or difficult situations. I did like translational work, as a neutral person. #00:27:04-3#. [FG1]
The APN took the family’s medical, family, and social history, planned the discharge, and conducted clinical assessments at their home. The APN also organized interprofessional discussions. Some HCP thought the APN’s advanced competences could be further exploited, and that they could provide support for parent education, facilitate the transition from the NICU to the intermediate care unit, coach HCP in clinically complex situations, or improve the interprofessional roundtable discussions.
On the other hand, HCP — especially the APNs — felt insecure and confused about how to distribute tasks because their role was new and unclear, and this sometimes caused conflict. Nurses were most likely to question whether the APN was needed, because they believed they could take over the role themselves; sometimes they compared the APN to a case manager. The feeling of being superfluous and the perception that the APN role undermined their competencies were strongly evident in the professional relationship between nurses and APNs. APNs found it challenging to identify and implement their function because it was brand new and they had to find their place in the system. They constantly had to explain their areas of responsibility and activities to other HCP and HCP failed to inform them about the progress of health conditions or re-admissions of patients for whom they were responsible.
The home visits: The APN’s regular home visits were key because they benefitted parents shortly after hospital discharge. The APN monitored the premature infant and the family, highlighted the infant’s developmental progress and offered resource-oriented short- and long-term support to parents. They provided content and the number of home visits the family needed. Some midwives felt that the APN’s home visits reduced their workload and made it possible to focus on their specialty or to share responsibilities. The community health care nurses felt the APN’s home visits were detrimental because they delayed the family’s detachment from the hospital and posed a barrier to building the relationship between the community worker and the family, thus, these nurses recommended the APN make only one home visit after discharge.
The roundtable discussions: Roundtable discussions facilitated interprofessional exchange before discharge when patient situations were complex or if many medical disciplines and HCP were caring for the same patient.
In case of complex situations, I believe it is very important that all these disciplines come together. #00:22:31-8#. [FG2]
The HCP found that the most valuable benefits the roundtables provided were the ability to share important information about the preterm infant’s health condition, that HCP outside the hospital could initiate a relationship with parents, and that parents could share their opinions or ask questions. But the interprofessional roundtable discussions were challenged to organize; some of the HCP did not attend, and it was especially hard for external HCP and the APN to join the discussions. Since the discussions required so many human, time, and financial resources, HCP suggested shortening them and holding them only when they were needed to discuss complex situations; discussions should focus on therapeutic priorities and result in clear and binding therapeutic goals and procedures.
Feasibility and Health Economic Limits
HCP described their concerns about health economic factors that could affect model implementation. They critically discussed the possibility of reimbursing interprofessional services or services that had not yet been established, like participating in roundtable discussions, physical therapeutic handling instructions, and the APNs’ home visits. To improve the model’s sustainability and implement it successfully, they felt it urgent to obtain financial support from policymakers, insurers, and private foundations. They felt the model needed to be more deeply embedded into the institution. According to the HCP, they would need enough human resources to cope with the added workload resulting of intensified family support and ICP. HCP also recommended optimizing existing human resources and collaborating with general pediatricians, midwives, and advisory services for mothers and fathers in remote regions. The services the model provides could be enhanced by expanding telephone consultations and interprofessional consultation hours at the hospital. Despite health economic and political challenges, most of the HCP in our focus groups supported further developing and permanently implementing the TtH-model.
Discussion
The results of our study show the challenges of IPC within a new model of transitional care for families after preterm birth.
Experiences of IPC
The TtH-model is an integrated care model designed to foster IPC. We established structures enabling IPC in the in- and outpatient setting. Although HCP preferred to collaborate within a network collaboration, they trapped in hierarchical structures. HCP found it particularly hard to critically reflect on their own roles and attitudes and on the roles of others, and to figure out their place in the new system. They were caught in a paradigm shift from a multidisciplinary collaboration within hierarchical structures where HCP from different disciplines worked in parallel40 to a network IPC.41 This type of change can stress and irritate stakeholders, as Vahs and Weiand42 describe. The HCP in our focus groups were uncertain, especially about the role of the APN and the reallocation of tasks, and they feared their responsibilities and position would be diminished. Several studies found that role conflicts are common responses in those newly introduced to IPC, shifts in hierarchical structures, difficulties communicating, and silo thinking.17,43 Vahs and Weiand42 recommend setting specific targets for change, fostering open, confidential communication, supporting cultural change institutionally, and providing enough time for change.
Difficulties with interprofessional communication and breakdowns in cooperation between HCP are common problems that Tracy and O’Grady17 describe as “parallel communication” and “parallel functioning”. This means that HCP support patients and families optimal. But HCP fail coordinating patient treatment with other HCP. The HCP in our focus group attributed the risk of parental oversupply these two major problems. Several studies indicate that deficits in interprofessional communication lead to misunderstanding and treatment mistakes; successful communication and maintaining the information flow among HCP is crucial.44 Weller et al44 recommend training HCP to communicate effectively through strategies like structured information transfer, and supporting interprofessional exchange with standardized protocols, checklists, and technical informatic solutions; for example, an electronic patient record shares the patient’s health data safely and consistently across institutions.45 Using checklists and standardized protocols can also improve roundtable discussions by giving them structure and defining consistent goals.46 Verhaegh et al46 recommend setting time limits for the discussion and documenting short and long-term goals at the end. We also found that “parallel functioning” and difficult IPC can be avoided by clarifying the tasks and roles of individual stakeholders, especially the APN.
The APN and the Introduction of New Roles
Our results show that APNs eased the work of other HCP because they shared professional responsibilities. Studies by Gysin et al19 and Josi et al47 support these findings: APNs who worked in Swiss primary care reduced the workload of other HCP, saving them time and demonstrating alternate approaches to patient care, improving task-sharing, raising the quality of care and making it more flexible.
But in the TtH-model we studied, the tasks of HCPs were not well-differentiated, and the APN’s role was not clear to either HCPs or the APNs. The APNs had difficulty familiarizing themselves with their new role, implementing it successfully, and finding their place in the system. Two recent studies show that Swiss HCP do not know much about APN roles19 and underline that role clarification is necessary for effective IPC.47 Casey et al48 identified facilitators and barriers to implementing advanced practice roles and highlighted the importance of leadership support, mutually supportive relationships between HCP, HCPs’ and the public’s clear understanding of the APNs’ role, and legal relation of APN roles.48 In Switzerland, APN roles are yet not sufficiently described or regulated by law, impeding development of the APN role and defining its scope of practice.19,47 Currently, there is a strong ongoing professional policy debate about the APNs’ educational prerequisites, professional regulations and policies including reimbursement options and professional autonomy. Regulation is essential to clarifying APN roles and overcoming political and legal obstacles to implementing them.19 Bryant-Lukosius und DiCenso18 recommend that stakeholders help defining the APN’s role and the APN must be integrated sustainably into the model of care. This approach helps improving interprofessional relationships, patient-focused care and accepting the APN role. APNs must obtain at least a master’s degree and be well-trained in their core competencies if other HCP are to accept their roles.17–19 In the TtH-model, an APN with a master’s led a team of three specialized nurses. To support parents, they primarily focused on the core competencies “direct care” and “counselling” and coordinated the IPC. Their scope of practice differed only slightly from the one of hospital’s internal and external nurses, which may make the division of tasks less clear and caused the role conflicts. To distinguish the role of the APN more clearly from that of other HCP, the APN should be demonstrably competent in leadership and coaching and lead IPC. Ideally, the APN would take a transformational leadership approach which, according to Pelz,49,50 would allow the APN to actively integrate the abilities of all HCP, promote their independence, and foster open communication between HCP. If the APN accomplished this, trust would be established, and the team’s performance would improve.
Parental Support
From the HCP perspective, APN-led, continuous, and family-centered care can support, strengthen and relieve families with preterm infants during their transition from hospital to home, a finding that affirms the assumptions of Schuetz Haemmerli et al.1 But there is also a risk of parental oversupply that could lead to them being overwhelmed. The literature and our findings suggest that this could be caused by interruptions in interprofessional communication and cooperation.17,43
HCP have different opinions on the optimal time to initiate and maintain an interprofessional relationship, but recommendations do exist. Rothe et al51 recommend initial prenatal contact between the caregiver and the parents and a prenatal consultation to help parents feel secure and reduce their concerns. Bornhorst et al52 showed that involving parents in prenatal decision-making increased their feeling of involvement in the postnatal treatment of their child, and concluded that the course of a trusting relationship between parents and HCP is set before birth.52 Studies on transitional care found that an intensive relationship between the APN and those in care can improve patient outcomes, significantly increase the chances patients will survive, and reduce rehospitalizations.17 In the TtH-model, APN support includes intensive, long-term parental support.
Health Economic Barriers
In the Swiss healthcare system, where care is highly specialized and fragmented, an increasing number of HCP are caring for each patient. Coordinating this treatment is challenging and it increases the risk of multiple treatments, complications, and overprovision, which have a negative effect on treatment outcomes and patient safety and increase healthcare costs.53 We found HCP needed more human resources to intensively support parents and the changes in IPC, and they thought it might be difficult to implement the model so it is financially sustainable. A recent Swiss study13 found that financial barriers hindered IPC within integrated care. The current reimbursement system is not designed for integrated care and serves as a macro level barrier. We need new fee-for-service models that lengthen the treatment continuum and support multiple actors working in cooperation.53
There is potential for meso-level improvement: tasks should be specific and clearly allocated among HCP; internal and external stakeholders should be more effectively integrated into the model; and, resources should be coordinated and bundled. Sottas and Kissmann28 found that bundling and use of existing resources increases benefits across the whole spectrum of expertise, skills, and experience within a team. They can better share the workload and realize a more holistic vision of the team and of patient treatment, which improves quality of care. Specific allocation of tasks also allows the HCP to focus more on their core competencies.
Strengths and Limitations
We generated rich data from our four focus groups and had already reached data saturation after we analyzed the second focus group. Though the group of experts conducting the qualitative analysis had broad evidence-based knowledge of neonatology, we may have been biased by our direct involvement in our field of research. To prevent possible biases from influencing our results, we constantly reflected and discussed questions by critically comparing expert opinion to the opinion of our one researcher without neonatal background.
Since we conducted our study in only one hospital, we cannot argue that our findings are generalizable to other settings or contexts. Bauer and Kirchner54 recommend analyzing the context, including affected individuals, HCP, the organization itself and other affected stakeholder groups before implementing the TtH-model in another hospital. The analysis identifies barriers and facilitating aspects of the context which must be addressed when implementing the model of care.
Implications for Further Research and Practice
We established a list (see Supplementary Table 2) that summarizes our recommendations for permanently implementing the TtH-model in the hospital setting we investigated.
Within the implementation of the TtH-model and the pilot-study we supported mostly stable families with an intact environment and missed families with a migrant background. This might have been influenced by the inclusion criteria set. According to the currents study participants, these families could have benefited most from the transitional care model. All families that need enhanced support should be able to benefit from future care within the TtH-model, including families who are socially disadvantaged or have limited knowledge of the national health care system.
Our study highlighted HCPs’ perspective on collaboration and building and maintaining relationships with parents. Parents may have different opinions, so we recommend future studies evaluate the parents’ perspective to determine their support needs and barriers and facilitators to using and benefitting from this program. After the TtH-model is adapted and implemented in its final form, we recommend re-evaluating the program to study the development of the IPC, the changing APN role over time, and the sustainability of the model.
Conclusions
From the HCPs’ perspective, the TtH-model and its services benefit families with preterm infants, especially families in complex situations. But the model of care needs to be adapted to ensure implementation is sustainable. To help HCP cope with a paradigm shift from traditional care to networked care, the APN’s scope of practice needs to be clarified, as do the roles and tasks of the HCP who work together. New ways of collaboration must be learned, and adapting to the new system will take time, new communication strategies that foster trust, and substantial leadership support. When implementing new models of care, sufficient time should always be allocated for learning and evaluation. Political action is also required to successfully implement the TtH-model, including drafting regulations for advanced practice roles, and implementing new financing models that support integrated care.
Acknowledgments
This study is funded by the following foundations: Foundation Anna Mueller-Grocholski; Zuerich, Switzerland; Foundation Gottfried & Julia Bangerter-Rhyner, Bern, Switzerland; Stiftung Lindenhof, Bern, Switzerland; Stiftung Pflegewissenschaft Schweiz, Basel, Switzerland. The authors are grateful to all HCP who participated in the focus group and the questionnaire for their open and honest engagement. We also thank Kali Tal for her editorial suggestions.
Disclosure
Mrs Natascha Schuetz Haemmerli reports grants from Foundation Anna Mueller-Grocholski; Zuerich, Switzerland, grants from Foundation Gottfried & Julia Bangerter-Rhyner, Bern, Switzerland, grants from Stiftung Lindenhof, Bern, Switzerland, and grants from Stiftung Pflegewissenschaft Schweiz, Basel, Switzerland, during the conduct of the study. Mrs Geraldine von Gunten reports grants from Foundation Anna Mueller-Grocholski; Zuerich, Switzerland, grants from Foundation Gottfried & Julia Bangerter-Rhyner, Bern, Switzerland, grants from Stiftung Lindenhof, Bern, Switzerland, and grants from Stiftung Pflegewissenschaft Schweiz, Basel, Switzerland, during the conduct of the study. Dr Jeannine Khan reports grants from Foundation Anna Mueller-Grocholski; Zuerich, Switzerland, grants from Foundation Gottfried & Julia Bangerter-Rhyner, Bern, Switzerland, grants from Stiftung Lindenhof, Bern, Switzerland, and grants from Stiftung Pflegewissenschaft Schweiz, Basel, Switzerland, during the conduct of the study. Mrs Liliane Stoffel reports grants from Foundation Anna Mueller-Grocholski; Zuerich, Switzerland; grants from Foundation Gottfried & Julia Bangerter-Rhyner, Bern, Switzerland; Stiftung Lindenhof, Bern, Switzerland; and Stiftung Pflegewissenschaft Schweiz, Basel, Switzerland., during the conduct of the study. The authors report no other conflicts of interest in this work.
References
- 1.Schuetz Haemmerli N, Lemola S, Holditch-Davis D, Cignacco E. Comparative evaluation of parental stress experiences up to 2 to 3 years after preterm and term birth. Adv Neonatal Care. 2020;20(4):301–313. doi: 10.1097/ANC.0000000000000714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stoll BJ, Hansen NI, Bell EF, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993–2012. JAMA. 2015;314(10):1039–1051. doi: 10.1001/jama.2015.10244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Latal B. Prediction of neurodevelopmental outcome after preterm birth. Pediatr Neurol. 2009;40(6):413–419. doi: 10.1016/j.pediatrneurol.2009.01.008 [DOI] [PubMed] [Google Scholar]
- 4.Chen F, Bajwa NM, Rimensberger PC, Posfay-Barbe KM, Pfister RE, Swiss Neonatal N. Thirteen-year mortality and morbidity in preterm infants in Switzerland. Arch Dis Child Fetal Neonatal Ed. 2016;101(5):F377–F383. doi: 10.1136/archdischild-2015-308579 [DOI] [PubMed] [Google Scholar]
- 5.Roque ATF, Lasiuk GC, Radünz V, Hegadoren K. Scoping review of the mental health of parents of infants in the NICU. J Obstet Gynecol Neonatal Nurs. 2017;46(4):576–587. doi: 10.1016/j.jogn.2017.02.005 [DOI] [PubMed] [Google Scholar]
- 6.Treyvaud K, Lee KJ, Doyle LW, Anderson PJ. Very preterm birth influences parental mental health and family outcomes seven years after birth. J Pediatr. 2014;164(3):515–521. doi: 10.1016/j.jpeds.2013.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Treyvaud K. Parent and family outcomes following very preterm or very low birth weight birth: a review. Semin Fetal Neonatal Med. 2014;19(2):131–135. doi: 10.1016/j.siny.2013.10.008 [DOI] [PubMed] [Google Scholar]
- 8.Kantrowitz-Gordon I, Altman MR, Vandermause R. Prolonged distress of parents after early preterm birth. J Obstet Gynecol Neonatal Nurs. 2016;45(2):196–209. doi: 10.1016/j.jogn.2015.12.004 [DOI] [PubMed] [Google Scholar]
- 9.Thomas J, Feeley N, Grier P. The perceived parenting self-efficacy of first-time fathers caring for very-low-birth-weight infants. Issues Compr Pediatr Nurs. 2009;32(4):180–199. doi: 10.3109/01460860903281366 [DOI] [PubMed] [Google Scholar]
- 10.Hynan MT, Mounts KO, Vanderbilt DL. Screening parents of high-risk infants for emotional distress: rationale and recommendations. J Perinatol. 2013;33(10):748–753. doi: 10.1038/jp.2013.72 [DOI] [PubMed] [Google Scholar]
- 11.Lean RE, Paul RA, Smyser TA, Smyser CD, Rogers CE. Social adversity and cognitive, language, and motor development of very preterm children from 2 to 5 years of age. J Pediatr. 2018;203:177–184 e171. doi: 10.1016/j.jpeds.2018.07.110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Purdy IB, Craig JW, Zeanah P. NICU discharge planning and beyond: recommendations for parent psychosocial support. J Perinatol. 2015;35(Suppl S1):24–28. doi: 10.1038/jp.2015.146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gilles I, Filliettaz SS, Berchtold P, Peytremann-Bridevaux I. Financial barriers decrease benefits of interprofessional collaboration within integrated care programs: results of a nationwide survey. Int J Integr Care. 2020;20(1):10. doi: 10.5334/ijic.4649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Porz F, Podeswik A. Case Management in der Kinder- und Jugendmedizin. Qualitätsmanagement beim Aufbau und in der Begleitung von Nachsorgeeinrichtungen für schwer und chronisch kranke Kinder und Jugendliche am Beispiel des Bunten Kreises. In: Brinkmann V, editor. Case Management Organisationsentwicklung und Change Management im Gesundheits- und Sozialunternehmen. 2 ed. Wiesbaden: Gabler Fachverlag GmbH; 2010. [Google Scholar]
- 15.Naylor MD, Brooten D, Campbell R, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. JAMA. 1999;281(7):613–620. doi: 10.1001/jama.281.7.613 [DOI] [PubMed] [Google Scholar]
- 16.Brooten D, Kumar S, Brown LP, et al. A randomized clinical trial of early hospital discharge and home follow-up of very-low-birth-weight infants. N Engl J Med. 1986;315(15):934–939. doi: 10.1056/NEJM198610093151505 [DOI] [PubMed] [Google Scholar]
- 17.Tracy MF, O’Grady ET. Hamric and Hanson’s Advanced Practice Nursing: An Integrative Approach. 6 ed. St. Louis: Elsevier; 2019. [Google Scholar]
- 18.Bryant-Lukosius D, Spichiger E, Martin J, et al. Framework for evaluating the impact of advanced practice nursing roles. J Nurs Scholarsh. 2016;48(2):201–209. doi: 10.1111/jnu.12199 [DOI] [PubMed] [Google Scholar]
- 19.Gysin S, Sottas B, Odermatt M, Essig S. Advanced practice nurses’ and general practitioners’ first experiences with introducing the advanced practice nurse role to Swiss primary care: a qualitative study. BMC Fam Pract. 2019;20(1):163. doi: 10.1186/s12875-019-1055-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morin D, Ramelet A-S, Shaha M. Advanced nursing practice:vision in Switzerland. Rech Soins Infirm. 2013;N° 115(115):49–58. doi: 10.3917/rsi.115.0049 [DOI] [PubMed] [Google Scholar]
- 21.Bryant-Lukosius D, Carter N, Reid K, et al. The clinical effectiveness and cost-effectiveness of clinical nurse specialist-led hospital to home transitional care: a systematic review. J Eval Clin Pract. 2015;21(5):763–781. doi: 10.1111/jep.12401 [DOI] [PubMed] [Google Scholar]
- 22.Brooten D, Naylor MD, York R, et al. Lessons learned from testing the quality cost model of Advanced Practice Nursing (APN) transitional care. J Nurs Scholarsh. 2002;34(4):369–375. doi: 10.1111/j.1547-5069.2002.00369.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mackavey C. Advanced practice nurse transitional care model promotes healing in wound care. Care Manage J. 2016;17(3):140–149. doi: 10.1891/1521-0987.17.3.140 [DOI] [PubMed] [Google Scholar]
- 24.Tsiachristas A, Wallenburg I, Bond CM, et al. Costs and effects of new professional roles: evidence from a literature review. Health Policy (New York). 2015;119(9):1176–1187. doi: 10.1016/j.healthpol.2015.04.001 [DOI] [PubMed] [Google Scholar]
- 25.Haslbeck FB. Music therapy for premature infants and their parents: an integrative review. Nord J Music Ther. 2012;21(3):203–226. doi: 10.1080/08098131.2011.648653 [DOI] [Google Scholar]
- 26.Bieleninik Ł, Ghetti C, Gold C. Music therapy for preterm infants and their parents: a meta-analysis. Pediatrics. 2016;138(3):e20160971. doi: 10.1542/peds.2016-0971 [DOI] [PubMed] [Google Scholar]
- 27.Reeves S, Pelone F, Harrison R, Goldman J, Zwarenstein M. Interprofessional collaboration to improve professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2017;6:CD000072. doi: 10.1002/14651858.CD000072.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sottas B, Kissmann S. Übersichtsstudie zu Nutzen und Wirksamkeit der interprofessionellen Praxis (IPP) Expertenbericht für das Bundesamt für Gesundheit. Teilbericht 1. Bundesamt für Gesundheit; 2015:1–26. [Google Scholar]
- 29.Bridges DR, Davidson RA, Odegard PS, Maki IV, Tomkowiak J. Interprofessional collaboration: three best practice models of interprofessional education. Med Educ Online. 2011;16(1):1–10. doi: 10.3402/meo.v16i0.6035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Canadian Interprofessional Health Collaborative (CIHC). A national interprofessional competency framework. 2010; Available from: https://drive.google.com/file/d/1Des_mznc7Rr8stsEhHxl8XMjgiYWzRIn/view. Accessed November30, 2020.
- 31.Polit DF, Beck CT, Hungler BP. Lehrbuch Pflegeforschung: Methodik, Beurteilung Und Anwendung. In: Bartholomeyczik S, Trans. 2 ed. Bern: Hans Huber; 2012. [Google Scholar]
- 32.Flick U, von Kardorff E, Steinke I. Was ist qualitative Forschung? Einleitung und Überblick. In: Flick U, von Kardorff E, Steinke I, editors. Qualitative Forschung: Ein Handbuch. 10th ed. Reinbek bei Hamburg: Rowohlt Taschenbuch Verlag; 2013:13–29. [Google Scholar]
- 33.Jayasekara RS. Focus groups in nursing research: methodological perspectives. Nurs Outlook. 2012;60(6):411–416. doi: 10.1016/j.outlook.2012.02.001 [DOI] [PubMed] [Google Scholar]
- 34.Krueger RA, Casey MA. Focus Groups: A Practical Guide for Applied Research. 5 ed. Thousand Oaks, California: SAGE Publications; 2015. [Google Scholar]
- 35.Guest G, Namey E, McKenna K. How many focus groups are enough? Building an evidence base for nonprobability sample sizes. Field Method. 2016;29(1):3–22. doi: 10.1177/1525822X16639015 [DOI] [Google Scholar]
- 36.Schweizerische Akademie der Medizinischen Wissenschaften (SAMW). Forschung mit Menschen. Ein Leitfaden für die Praxis. Bern: Schweizerische Akadmie der Medizinischen Wissenschaften (SAMW); 2015. [Google Scholar]
- 37.Kruse J. Qualitative Interviewforschung. Ein Integrativer Ansatz. 2 ed. Weinheim: Beltz Juventa; 2015. [Google Scholar]
- 38.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 39.Lincoln YS, Guba EG. Naturalistic Inquiry. Beverly Hills, CA: Sage Publications, Inc.; 1985. [Google Scholar]
- 40.Baird J, Ashland M, Rosenbluth G. Interprofessional teams: current trends and future directions. Pediatr Clin North Am. 2019;66(4):739–750. doi: 10.1016/j.pcl.2019.03.003 [DOI] [PubMed] [Google Scholar]
- 41.Schmitz C, Atzeni G, Berchtold P. Challenges in interprofessionalism in Swiss health care: the practice of successful interprofessional collaboration as experienced by professionals. Swiss Med Wkly. 2017. doi: 10.4414/smw.2017.14525 [DOI] [PubMed] [Google Scholar]
- 42.Vahs D, Weiand A. Workbook Change Management: Methoden Und Techniken. 3 ed. Deutschland: Schäffer-Poeschel Verlag für Wirtschaft; 2020. [Google Scholar]
- 43.Sottas B, Kissmann S, Brügger S. Interprofessionelle Ausbildung (IPE): Erfolgsfaktoren – Messinstrument – Best Practice Beispiele. Expertenbericht für das Bundesamt für Gesundheit. Teilbericht 2. Bundesamt für Gesundheit; 2016. [Google Scholar]
- 44.Weller J, Boyd M, Cumin D. Teams, tribes and patient safety: overcoming barriers to effective teamwork in healthcare. Postgrad Med J. 2014;90:149–154. doi: 10.1136/postgradmedj-2012-131168 [DOI] [PubMed] [Google Scholar]
- 45.eHealth Suisse: Kompetenz- und Koordinationsstelle von Bund und Kantonen. Elektronisches patientendossier. 2020; Available from: www.patientendossier.ch. Accessed November30, 2020.
- 46.Verhaegh KJ, Seller-Boersma A, Simons R, et al. An exploratory study of healthcare professionals’ perceptions of interprofessional communication and collaboration. J Interprof Care. 2017;31(3):397–400. doi: 10.1080/13561820.2017.1289158 [DOI] [PubMed] [Google Scholar]
- 47.Josi R, Bianchi M, Brandt SK. Advanced practice nurses in primary care in Switzerland: an analysis of interprofessional collaboration. BMC Nurs. 2020;19(1):1. doi: 10.1186/s12912-019-0393-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Casey M, O’Connor L, Cashin A, et al. Enablers and challenges to advanced nursing and midwifery practice roles. J Nurs Manag. 2019;27:271–277. doi: 10.1111/jonm.12697 [DOI] [PubMed] [Google Scholar]
- 49.Pelz W. Transformationale Führung: Forschungsstand und Umsetzung in der Praxis. In: von Au C, editor. Wirksame und nachhaltige Führungsansätze: System, Beziehung, Haltung und Individualität. Wiesbaden: Springer Fachmedien; 2016:93–110. [Google Scholar]
- 50.Pelz W. Transformationale Führung in der unternehmerischen Praxis. 2020; Available from: http://www.transformationale-fuehrung.com/. Accessed December1, 2020.
- 51.Rothe F, Gebauer C, Pulzer F, Bläser A, Robel-Tillig E, Knüpfer M. Pränatale Elternbegleitung bei drohender Frühgeburt. Kinder- und Jugendmedizin. 2009;09(06):362–366. doi: 10.1055/s-0038-1629055 [DOI] [Google Scholar]
- 52.Bohnhorst B, Ahl T, Peter C, Pirr S. Parents‘ prenatal, onward, and postdischarge experiences in case of extreme prematurity: when to set the course for a trusting relationship between parents and medical staff. Am J Perinatol. 2015;32(13):1191–1197. doi: 10.1055/s-0035-1551672 [DOI] [PubMed] [Google Scholar]
- 53.Schweizerische Konferenz der kantonalen Gesundheitsdirektorinnen und -direktoren GDK. Impulse für die Integrierte Versorgung in den Kantonen: ein Leitfaden. 2019; Available from: https://www.gdk-cds.ch/fileadmin/docs/public/gdk/themen/integrierte_versorgung/GDK_Leitfaden_DE_def.pdf. Accessed April7, 2021.
- 54.Bauer MS, Kirchner J. Implementation science: what is it and why should I care? Psychiatry Res. 2020;283:112376. doi: 10.1016/j.psychres.2019.04.025 [DOI] [PubMed] [Google Scholar]