Abstract
Background
In geriatric age group, hip fractures tend to become a major public health hazard. Due to this high occurrence, there is a need to develop standardized, effective, and multidisciplinary management for treatment. These elderly patients have excessive mortality that can extend ahead of the time of recovery. Early surgery after hip fractures has lead to a notable reduction in mortality rates. Still, it is considerably high as compared to other fractures.
Methods
266 patients of >65 years who were operated within 72 h hours in a tertiary level health care centre for hip fractures were included. They were evaluated with X-rays and grade of Singh’s index was noted. Mortality rates and the factors associated with it such as age, sex, co morbidities (using Charlson’s co morbidity Index/CCI) were evaluated after 2 year follow up.
Results
The overall 2-year mortality reported in our study population was 11.2%. It was broadly lower as compared to most of the other studies. It was 6.3% in females as compared to 18.1% in males. While it was reported to be only 6% in 65–74 years of age, it was 25% in patients who were 85 years and above. 76.6% of the patients had Singh’s index of ≤ grade 3 showing osteoporosis. The patients with Low Charlson’s score showed only 4.2% mortality while those with high Charlson’s score showed 25.5% mortality.
Conclusion
It was concluded that Mortality among elderly patients after early surgery after osteoporotic hip fractures is quite significant. The factors for improvement in long term survival post-hip fracture may include changing treatment patterns, increasing life expectancy and early surgery. Increase in age, female sex, and high CCI Scores were major risk factors of mortality after hip fractures in a 2-year follow-up period.
Keywords: Hip fracture, Mortality, Early surgery, Co-morbidities, Elderly
1. Introduction
In geriatric age group, hip fractures tend to become a major public health hazard. It has a significant financial impact on the patients and health care systems. The number patients with hip fractures are known to vary by age and gender and are found more frequently in older people. Osteoporosis stands as most important independent cause of fractures in elderly especially in Low Income Asian countries like India.
Worldwide, it is estimated that 1 in 3 women and 1 in 5 men above the age of 50 will experience osteoporotic fractures in their lifetime.1 In 2013, it was indicated that 50 million people in India are either osteoporotic (T-score lower than-2.5) or have low bone mass (T-score between-1.0 and-2.5). Hip fractures reported in old osteoporotic individuals mostly result from trivial trauma like falling at home. The literature says that after surviving a hip fracture, the patients experience depletion in functional activity and social independence with an augmentation in psychological disorders like depression, anxiety and attention deficit episodes.2
Due to this high occurrence, there is an urgent need to develop standardized, effective, and multidisciplinary management approach for treatment and rehabilitation of patients. These elderly patients have reported excessive mortality that can continue beyond the period of recovery. Most of these patients are vulnerable and have multiple medical diseases that can hinder rehabilitation and make death non-preventable.
The mortality rates in the previous studies for patients with hip fractures are considerably high, ranging from 15% to 36%.3, 4, 5, 6, 7 Dubljanin-Raspopovic et al.8 reported the death rate among the elderly patients with hip fractures was 4 times as compared to general population.
Although early surgery has lead to a significant 19% reduction in mortality rates, it is still considerably high in comparison to other fractures.9 Increase in age, gender, ethnicity, medical co-morbidities, cognitive impairment, place of injury, time to surgery and rehabilitation protocols are known predictors of postoperative mortality in hip fracture patients.5,6,10, 11, 12, 13, 14, 15 Nearly 20% of patients with hip fractures are known to develop some complication during recovery period.16 Most common post-operative complications known include Lung infections (9%) and cardiac disorders (5%).15Other post-operative complications include prolonged immobilization leading to bedsores, failure in the union of bone, and re-fractures due to osteoporosis.
This study aims at predicting the mortality rates at 2 years follow up after early surgery (<72 h after injury) for hip fractures in the elderly.
2. Materials and methods
2.1. Data source
This was a retrospective study that was carried out in the Department of Orthopedics of a tertiary level health care centre. The patients were admitted either from OPD/Emergency rooms or referred from other health centers, identified clinically followed by X-rays’ (Anterio-posterior and lateral) and managed according to standard protocols. Singh’s index [17] was used to identify osteoporosis using the Hip x-rays. Informed consent was taken from all patients and were then planned for surgery once they were medically stable and fitness for surgery was obtained from the anesthesia department. The patients were operated according to the set protocols according to the type of fracture with the appropriate implant. Postoperative Rehabilitation and physiotherapy was started the next day of surgery while ambulation of the patient was decided according to the fracture fixation.
2.2. Data collection
Data was collected from the case records of Operation theatre for hip fracture surgery that were operated between April 15, 2017, and May 1, 2018 for CRIF/ORIF with PFN/DHS/Hemi-replacement arthroplasty/Total hip replacement after hip fractures after obtaining clearance from Institutional ethical committee. Admission tickets were then recruited for the cases and studied for diagnosis, timing of surgery, type of surgery, duration of stay, and co-morbid conditions such as DM, Hypertension, COPD or any chronic illness. The patients were then contacted telephonically and data was collected for mortality of all the cases.
2.3. Study group
Patients 65 years of age or older who sustained a hip fracture (including inter-trochanteric and neck of femur fractures) and were operated between April 15, 2017, and May 1, 2018, were included in the study for analysis. We excluded patients who had any pathological fracture, peri-prosthetic fracture, a previous hip fracture, or those who were treated conservatively.
2.4. Variables
We studied the mortality at 2-year follow up from the date of injury. Variables studied related to mortality included age, race, gender, postoperative complications, and any co morbidity associated with patients. We used Charlson co morbidity index (CCI)18 to study the role of co morbidities in mortality of hip fracture patients. It is a weighted score that takes various co morbid medical conditions into account. In the original study by Charlson, a patient with a CCI between 1 to 2 and 3 to 4 had mortality rates (after 1 year follow up)of 26% and 52%, respectively. Charlson co morbidity score was calculated using the medical history at the time of injury and classified into low (0 or 1), medium,2,3 and high (4 or more). Chi-Square tests and multiple logistic regression analysis were performed to determine statistical significance.
At the time of admission, all the patients were also screened for osteoporosis using Singh’s Index in standard hip x-rays. The patients diagnosed with osteoporosis were treated with Calcium and Vit D supplements and bisphosphonate drugs.
3. Results
We studied 312 patients operated for hip fracture (neck of femur, inter-trochanteric, and sub-trochanteric fractures) out of which we could not get data of 46 patients, and thus we included 266 patients in our study (Table 1). The mean age was 74.7 years. 58.6% of patients were females and 41.3%were males. 74% of patients presented with a history of fall at home while doing the household activity.
Table 1.
Characteristics of patients.
| Total (n) | 266 | |
|---|---|---|
| Gender, % | ||
| Female | 156 | 58.64% |
| Male | 110 | 41.36% |
| Age, y | ||
| Overall (mean) | 64.47 | |
| 65–75 | 133 | 50% |
| 76–85 | 95 | 35.71% |
| 85 and above | 35 | 14.29% |
| SINGH’S INDEX | ||
| >Grade 3 | 62 | 23.3% |
| <Grade 3 | 204 | 76.6% |
| <Grade 2 | 157 | 59% |
| Charlson score | ||
| Overall (mean) | 2.54 | |
| Low (0–1) | 94 | 35.3% |
| Medium (2–3) | 125 | 46.9% |
| High (3–4) | 47 | 17.66% |
Of the total 266 patients enrolled for study, 204 (76.6%) patients had Singh’s index of less than grade 3. Among these, 157 (59%) patients had it less than grade 2 thus establishing that osteoporosis is very prevalent in Old Indian population above 65 years of age. Among females, Osteoporosis was reported in 65% of the cases while 50% males had Singh’s index of less than grade 3.
Of the 266 patients, 86 (32.3%) had a neck of femur fracture and the remaining 180 (67.7%) had a trochanteric fracture of femur. The patients had surgery under spinal (82.7%), general (5.6%), and combined spinal epidural (7.8%) anesthesia. The surgical techniques performed were hemiarthroplasty in 65 (24.4%), total arthroplasty in 21 (7.8%), intra-medullary nailing (IMN) in 160 (62.4%) cases and Dynamic Hip Screw in 14 (5.2%).
The overall 2-year mortality reported was 11.2% in our study population. It was 6.3% in females as compared to 18.1% in males (Table 2). The mortality rate was 1.7% for the initial inpatient hospital stay. The mortality rates saw a rise with increment in the age of the patient at time of injury. While it was reported to be only 6% in 65–74 years of age group, it was as high as 25% in patients who were 85 years and above.
Table 2.
–Factors associated with mortality.
| Characteristic | n | Mortality | Mortality Rate | Co-efficient | t-stat | p-value |
|---|---|---|---|---|---|---|
| Overall mortality | 266 | 30 | 11.2% | |||
| Age, y | 0.08 | 3.20 | 0.001 | |||
| 65-74 | 133 | 8 | 6.0% | |||
| 75-84 | 95 | 13 | 13.6% | |||
| 85-94 | 35 | 9 | 25.7% | |||
| Gender | 0.102 | 2.74 | 0.006 | |||
| Male | 110 | 20 | 18.1% | |||
| Female | 156 | 10 | 6.3% | |||
| Charlson Score | 0.09 | 3.74 | 0.0002 | |||
| Low (0–1) | 94 | 4 | 4.2% | |||
| Medium (2–3) | 125 | 14 | 11.2% | |||
| High (≥4) | 47 | 12 | 25.5% |
Mean Charlson score was 2.54 with 125 patients having medium score.2,3 Low CCI (0–1) was found in 94 patients and high (≥4) was reported in 47 patients. The patients with Low Charlson score showed only 4.2% mortality, with medium Charlson score showed 11.2% mortality and with high Charlson score showed 25.5% mortality.
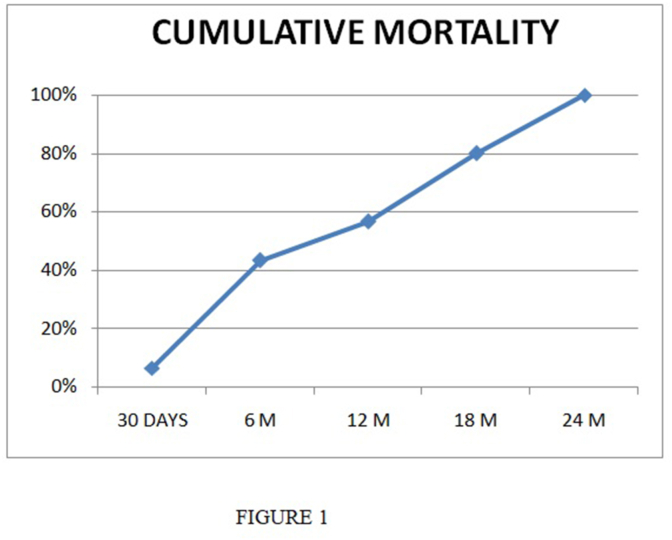
In Our study, Out of 30 patients who died, 17 died in the first year and 13 in the second year. 2 patients died during the hospital stay of initial seven days. Cause of death of both the cases was reported to be pulmonary embolism. 38 of the patients developed peri-implant re-fractures during the course of our study. Maximum mortality was reported to be in the initial 6 months (Fig. 1) and the most common cause of mortality was chest infections followed by cardiac failure. 38 of the patients developed peri-implant re-fractures during the course of our study.
Fig 1.
Cumulative Mortality over time.
4. Discussion
Osteoporosis is one of the major causes of fractures in the elderly population and currently leads to approximately 9 million fractures annually around the world.19 Also, these are increasing with an excess of 6 million added per year. 59% patients in our study has Singh’s Index of less than grade 2 thus establishing that osteoporosis is very prevalent in Old Indian population above 65 years of age. We found that Osteoporosis was reported in 65% females and 50% males with hip fractures. It is highly prevalent in females because of marked increase in bone loss during peri-menopause and post-menopause. While men experience only Age related linear bone loss, women in addition to age-related bone loss also experience menopausal bone loss.
The greatest increment of osteoporosis is predicted to be in Asian countries like India and China.20 So, there is an urgent need for a plan for optimization of this expected rise. Extensive studies are required to examine the patterns for mortality and morbidity among elderly to bear with an impending surge of hip fractures.
The overall mortality rate observed in our study (11.2%) was broadly lower as compared to most of the older studies, but only slightly lower when compared to latest studies. [3, 4, 5, 6, 7, 8,13,.21, 22, 23, 24, 25 Mortality rates and variables considered for various studies are mentioned in the table (Table 3).
Table 3.
Changes in mortality rates over time.
| YEAR OF STUDY | AUTHOR | TYPE OF STUDY | VARIABLES WITH INCREASED MORTALITY | FOLLOW UP | MORTALITY RATE |
|---|---|---|---|---|---|
| 2005 | Christopher G Moran et al.22 | Prospective | Delay in surgery (>4 days) | 1 year | 30% |
| 2010 | Scott Shnell23 | Retrospective | High CCI score (>4), Male, Increased Age | 1 year | 21.2% |
| 2019 | Eric Wei LiangCher24 | Prospective | High CCI score | 1 year | 13.3% |
| 2020 | Toshihiro Higashikawa et al.25 | Retrospective | Age, Sex, Albumin levels | 1 year | 12.2% |
The factors for improvement in long term survival post-hip fracture may include the ethnicity of population, changing treatment patterns, increasing life expectancy, early surgery, and adoption of secondary prevention and current best practices for care of patients. The mortality rates after one year follow up of hip fractures has traditionally been reported in literature as 30%.22 Various studies states that this mortality was 23.3% in Europe and 17.9% in Asia.26 In a study by Dhanwal DK27 in New Delhi, India, it was reported to be 30.4% after 1 year follow up. Oya kilci28 in 2016, reported mortality in 36.7% after 3 year study period.
Our study reports positive co-relation between mortality rates and increase in age of patient. While the patients of the age group 65–75 years reported only 6.03% mortality, those with age more than 85 years reported it as 25.7%. Various other studies in the literature have also shown the same, Aharonoff29 in a study of 612 patients found >85 years age as a significant predictor of mortality in hip fracture patients. Scott schnell23 proved mortality of 27% for >90 years and only 2% in patients less than 70 years of age. Berry et al.30 also reported that there was a 30% increase in mortality with every 5 years of advancing age after hip fractures. Bolton31 in a very recent study evaluated hip injuries in the individuals over 90 years of age and found 38.1% mortality among them, which is close to 25.7% reported by our study (>85 years of age). All these findings are conclusive with the regular trends of increase in mortality with increasing age.
Various studies have tried to establish a relationship with mortality rates and gender and the results are varied. Most studies claim that men have higher death rate after hip fractures. We also found that men have a higher mortality rate (18.1%) in comparison to women (6.3%) at our 2 year follow up. The study done by Endo et al.32 in 983 patients with hip fractures (206 men) found that men had an increased postoperative complication risk and almost double 1-year mortality as compared to women. No significant difference was determined between the genders in respect of mortality rates by Oya kilci (28) in his study. The reason for this disparity in mortality between the sexes is unclear and warrants further studies.
Charlson’s co morbidity index (CCI) was used to assess role of co-morbidities in mortality among hip fracture patients. Various studies have previously used the CCI to assess risk and predict 1-year mortality [28–30]. Charlson’s Index uses a cumulative score of co morbidities to provide prognostic data for the survival of patients after hip fractures.18 Patients with low CCI (0–1) had only 4.2% mortality rates while patients having high CCI (4 or more) had 5 times more (25%) mortality rates. This shows that co-morbid conditions (CCI) continue to be the most significant factor for hindering the recovery of the patient and leading to mortality after hip region surgery. Various other authors have found similar results. Roche et al.15 in their study of 2448 hip fractures found that higher complication rate and mortality were found in patients having 3 or more medical co morbidities. Bentler et al.[30] replicated his results where he reported that patients with 3 or more co morbid conditions were 65% more likely to die than those with fewer conditions. Scott Schnell23 found an average CCI Score of 2.7 and reported that segment of the population who may have severe or multiple medical co morbidities presumed a higher 1-year mortality rate.
The timing of surgery, type of fractures, route of anesthe31sia administered, and type of surgical technique were not found significant for mortality rates observed after hip fractures. Allen Tenner II et al.33 in his 3 year retrospective cohort study recently evaluated if earlier intervention is associated with improved mortality, hospital length of stay or cost of treatment after hip fractures. Similar to our study, they found that surgery within 24 h of admission was not associated with lower odds of death when compared to surgery after 24 h of admission. However, a significant decrease in cost and length of hospital stay was observed for early surgery.
In Our study, Out of 30 patients who died, 17 died in the first year and 13 in the second year. 2 patients died due to post-operative complications during the hospital stay of initial seven days. Cause of death of both the cases was reported to be pulmonary embolism. In a recent systematic review by Istianiah [34] it was concluded that at 30 days after hip surgery, complications of chest infection were 9% while complications of UTI were 4% and wound infection or deep infection were 1.1% and 1% respectively.
This study was not without limitations. We lost follow up of 46 patients during our study and could not evaluate their mortality status in results. This could have affected our mortality rates leading to lower or higher mortality rates. Since 32 of these patients were from age group 65–74 with average CCI score of 2 among these patients, we can assume that they also must have followed the same trend as the mortality rates exhibited by others. Also, we analyzed short term results and thus longer duration studies are required in future.
5. Conclusion
Hip fracture among elderly is a major public health concern and needs attention for proper management and early rehabilitation as there is quite significant mortality associated. It was concluded that increasing age, female sex, and high CCI Scores due to comorbidities were major risk factors of mortality after hip fractures.
Funding
Not required.
Availability of data and material- from OPD/IPD at associated hospital statement
The manuscript has been read and approved by all the authors and that each author believes that the manuscript represents honest work.
Declaration of competing interest
None.
References
- 1.Kanis J.A., Johnell O., Oden A. Long-term risk of osteoporotic fracture in Malmö. Osteoporos Int. 2000;11(8):669–674. doi: 10.1007/s001980070064. [DOI] [PubMed] [Google Scholar]
- 2.Moore D.P., Quinlan W. Mortality and morbidity associated with hip fractures. Ir J Med Sci. 1989;158:40–42. doi: 10.1007/BF02942060. [DOI] [PubMed] [Google Scholar]
- 3.Tarazona-Santabalbina F.J., Belenguer-Varea Á., Rovira-Daudi E. Early interdisciplinary hospital intervention for elderly patients with hip fractures – functional outcome and mortality. Clinics. 2012 Jun;67(6):547–555. doi: 10.6061/clinics/2012(06)02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Civinini R., Paoli T., Cianferotti L. Functional outcomes and mortality in geriatric and fragility hip fractures—results of an integrated, multidisciplinary model experienced by the “Florence hip fracture unit. Int Orthop. 2019 Jan 1;43(1):187–192. doi: 10.1007/s00264-018-4132-3. [DOI] [PubMed] [Google Scholar]
- 5.Pioli G., Lauretani F., Davoli M.L. Older people with hip fracture and IADL disability require earlier surgery. J Gerontol A Biol Sci Med Sci. 2012 Nov;67(11):1272–1277. doi: 10.1093/gerona/gls097. [DOI] [PubMed] [Google Scholar]
- 6.Mariconda M., Costa G.G., Cerbasi S. The determinants of mortality and morbidity during the year following fracture of the hip: a prospective study. Bone Joint Lett J. 2015 Mar;97-B(3):383–390. doi: 10.1302/0301-620X.97B3.34504. [DOI] [PubMed] [Google Scholar]
- 7.Lee T.-C., Ho P.-S., Lin H.-T., Ho M.-L., Huang H.-T., Chang J.-K. One-year readmission risk and mortality after hip fracture surgery: a national population-based study in taiwan. Aging Dis. 2017 Jul;8(4):402–409. doi: 10.14336/AD.2016.1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dubljanin-Raspopović E., Marković-Denić L., Marinković J., Nedeljković U., Bumbaširević M. Does early functional outcome predict 1-year mortality in elderly patients with hip fracture? Clin Orthop Relat Res. 2013 Aug;471(8):2703–2710. doi: 10.1007/s11999-013-2955-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ravindrarajah R., Hazra N.C., Charlton J., Jackson S.H.D., Dregan A., Gulliford M.C. Incidence and mortality of fractures by frailty level over 80 years of age: cohort study using UK electronic health records. BMJ Open. 2018 Jan 1;8(1) doi: 10.1136/bmjopen-2017-018836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim S.-M., Moon Y.-W., Lim S.-J. Prediction of survival, second fracture, and functional recovery following the first hip fracture surgery in elderly patients. Bone. 2012 Jun;50(6):1343–1350. doi: 10.1016/j.bone.2012.02.633. [DOI] [PubMed] [Google Scholar]
- 11.Smith T., Pelpola K., Ball M., Ong A., Myint P.K. Pre-operative indicators for mortality following hip fracture surgery: a systematic review and meta-analysis. Age Ageing. 2014 Jul;43(4):464–471. doi: 10.1093/ageing/afu065. [DOI] [PubMed] [Google Scholar]
- 12.Brown K., Cameron I.D., Keay L., Coxon K., Ivers R. Functioning and health-related quality of life following injury in older people: a systematic review. Inj Prev. 2017 Dec;23(6):403–411. doi: 10.1136/injuryprev-2016-042192. [DOI] [PubMed] [Google Scholar]
- 13.Haentjens P., Magaziner J., Colón-Emeric C.S. Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med. 2010 Mar 16;152(6):380–390. doi: 10.1059/0003-4819-152-6-201003160-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chang W., Lv H., Feng C. Preventable risk factors of mortality after hip fracture surgery: systematic review and meta-analysis. Int J Surg. 2018 Apr;52:320–328. doi: 10.1016/j.ijsu.2018.02.061. [DOI] [PubMed] [Google Scholar]
- 15.Roche J.J.W., Wenn R.T., Sahota O., Moran C.G. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005 Dec 10;331(7529):1374. doi: 10.1136/bmj.38643.663843.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carpintero Pedro, Caeiro Jose Ramón, Carpintero Rocío, Morales Angela, Silva Samuel, Mesa Manuel. Complications of hip fractures: a review - PubMed [Internet] https://pubmed.ncbi.nlm.nih.gov/25232517/ [cited 2021 Apr 4]. Available from: [DOI] [PMC free article] [PubMed]
- 17.Singh M., Nagrath A.R., Maini P.S. Changes in trabecular pattern of the upper end of the femur as an index of osteoporosis. J Bone Joint Surg Am. 1970 Apr;52(3):457–467. [PubMed] [Google Scholar]
- 18.Charlson M.E., Pompei P., Ales K.L., MacKenzie C.R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 19.Cooper C., Campion G., Melton L.J. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992 Nov;2(6):285–289. doi: 10.1007/BF01623184. [DOI] [PubMed] [Google Scholar]
- 20.Cenzer I.S., Tang V., Boscardin W.J. One-year mortality after hip fracture: development and validation of a prognostic index. J Am Geriatr Soc. 2016 Sep;64(9):1863–1868. doi: 10.1111/jgs.14237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mitchell R., Harvey L., Brodaty H., Draper B., Close J. One-year mortality after hip fracture in older individuals: the effects of delirium and dementia. Arch Gerontol Geriatr. 2017 Sep;72:135–141. doi: 10.1016/j.archger.2017.06.006. [DOI] [PubMed] [Google Scholar]
- 22.Moran C.G., Wenn R.T., Sikand M., Taylor A.M. Early mortality after hip fracture: is delay before surgery important? J Bone Joint Surg Am. 2005 Mar;87(3):483–489. doi: 10.2106/JBJS.D.01796. [DOI] [PubMed] [Google Scholar]
- 23.Schnell S., Friedman S.M., Mendelson D.A., Bingham K.W., Kates S.L. The 1-year mortality of patients treated in a hip fracture program for elders. Geriatr Orthop Surg Rehabil. 2010 Sep;1(1):6–14. doi: 10.1177/2151458510378105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cher E.W.L., Allen J.C., Howe T.S., Koh J.S.B. Comorbidity as the dominant predictor of mortality after hip fracture surgeries. Osteoporos Int. 2019 Dec;30(12):2477–2483. doi: 10.1007/s00198-019-05139-8. [DOI] [PubMed] [Google Scholar]
- 25.Higashikawa T., Shigemoto K., Goshima K. Mortality and the risk factors in elderly female patients with femoral neck and trochanteric fractures. J Clin Med Res. 2020 Oct;12(10):668–673. doi: 10.14740/jocmr4292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Downey C., Kelly M., Quinlan J.F. Changing trends in the mortality rate at 1-year post hip fracture - a systematic review. World J Orthoped. 2019 Mar 18;10(3):166–175. doi: 10.5312/wjo.v10.i3.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dhanwal D.K. ESCE013-IOF Congress; April 18 2013. 2013. Mortality and functional impairment after hip fracture - a prospective study in Indian population. Rome, Italy. [Google Scholar]
- 28.Kilci O., Un C., Sacan O. Postoperative mortality after hip fracture surgery: a 3 Years follow up. PloS One. 2016;11(10) doi: 10.1371/journal.pone.0162097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aharonoff G.B., Koval K.J., Skovron M.L., Zuckerman J.D. Hip fractures in the elderly: predictors of one year mortality. J Orthop Trauma. 1997 Apr;11(3):162–165. doi: 10.1097/00005131-199704000-00004. [DOI] [PubMed] [Google Scholar]
- 30.Berry S.D., Samelson E.J., Bordes M., Broe K., Kiel D.P. Survival of aged nursing home residents with hip fracture. J Gerontol A Biol Sci Med Sci. 2009 Jul;64(7):771–777. doi: 10.1093/gerona/glp019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.D B., C B., Mt W. Nonagenarian hip fractures: morbidity and mortality at a single institution. J Clin Orthop Trauma. 2020 Sep 22;14:69–73. doi: 10.1016/j.jcot.2020.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Endo Y., Aharonoff G.B., Zuckerman J.D., Egol K.A., Koval K.J. Gender differences in patients with hip fracture: a greater risk of morbidity and mortality in men. J Orthop Trauma. 2005 Jan;19(1):29–35. doi: 10.1097/00005131-200501000-00006. [DOI] [PubMed] [Google Scholar]
- 33.Tanner Ii A., Jarvis S., Orlando A. A three-year retrospective multi-center study on time to surgery and mortality for isolated geriatric hip fractures. J Clin Orthop Trauma. 2020 Feb;11(Suppl 1):S56–S61. doi: 10.1016/j.jcot.2019.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Istianah U., Nurjannah I., Magetsari R. Post-discharge complications in postoperative patients with hip fracture. Journal of Clinical Orthopaedics & Trauma. 2021 Mar 1;14:8–13. doi: 10.1016/j.jcot.2020.10.045. [DOI] [PMC free article] [PubMed] [Google Scholar]