Abstract
Symptomatic irreparable rotator cuff tears pose a challenge for shoulder surgeons. Whilst reverse polarity shoulder arthroplasty is an effective option for older symptomatic patients who have exhausted conservative management, the optimal treatment for younger patients remains controversial. In this article we outline the main tendon transfer options, including anatomical considerations, indications, contraindications, surgical technique, complications and a review of the evidence. Tendon transfers provide an alternative joint-preserving surgical option, but the evidence so far is limited, with a clear need for well-designed comparative studies to confirm their effectiveness.
Keywords: Tendon transfer, Management, Irreparable, Rotator cuff tears
1. Introduction
Rotator cuff disease is a common cause of shoulder pain and dysfunction. Rotator cuff tears are prevalent as often as one in five in the general population, with increasing age, history of trauma and dominant arm being risk factors.1 Advances in surgical techniques has allowed repair of large symptomatic tears but massive tears may not be amenable to repair, particularly when associated with retraction, muscle fatty infiltration and involvement of multiple tendons. Surgical procedures used for massive irreparable tears include cuff debridement, partial repair, tendon transfers, graft augmentation, superior capsular reconstruction, subacromial balloon spacer, bridging interposition graft and reverse polarity shoulder arthroplasty.2,3 Tendon transfers are an alternative for young, active patients with irreparable cuff tears. Latissimus dorsi (LD) transfer has been used more commonly, with other options being teres major (TM), lower trapezius (LT) and pectoralis major (PM) transfers.3,4 The tendon transfer aims to re-establish the centralising effect of the rotator cuff, improving the biomechanics of glenohumeral motion.5
2. Anatomical considerations
A good understanding of anatomical relationships of the neurovascular bundles is vital for safe and effective transfers. Despite a massive rotator cuff tear, normal shoulder function is possible when force-couples in two planes, one in the coronal plane and the other in the axial plane, are well balanced.6 The latissimus dorsi tendon (LDT) is well suited for transfers around the shoulder. The LD is a large, fan-shaped muscle with a broad origin from the iliac crest, thoracolumbar fascia, and spinous processes of lower thoracic and lumbar vertebrae. It inserts medial to the PM; and lateral and proximal to the TM on the humerus.7 It derives its neurovascular supply from the thoracodorsal nerve, a branch of the posterior cord of the brachial plexus and thoracodorsal artery, a branch of the subscapular artery.8 The axillary and radial nerves are closest to the LDT insertion when the arm is flexed, and farthest when the arm is internally rotated. The LDT transfer replaces the posterior cuff function, leading to a balance in the axial plane force-couple.3 Transfer of the LDT from the intertubercular groove on the anteromedial aspect to the posterosuperior greater tuberosity, converts the original internal rotation/extension action of LD to external rotation/flexion force. Once transferred, LD depresses and centralises the humeral head, thus helping the deltoid to elevate and abduct the arm.9 Overall, advantages of the transfer include a good line of pull, adequate strength, good amplitude and excellent excursion. However, a disadvantage is poor synergy.4,10
TM and supraspinatus are morphologically similar.11 The TM is a small, rectangular muscle originating from the posterior aspect of the inferior angle of the scapula and inserting medial to the LD insertion on the humerus.12 Its vascular supply is derived from the circumflex scapular artery, a branch of the subscapular artery and its nerve supply is from the lower subscapular nerve, a branch of the posterior cord of the brachial plexus.8 TM is an adductor and internal rotator. It has a mean length of about 13–14 cm and up to 47% of increased length may be required to reach the greater tuberosity. Hence problems with reattachment are more likely with the TM tendon when compared to LD.8 Combined transfer of TM and LD is considered stronger as TM is a bulky muscle with less risk of tendon rupture/necrosis.13 TM function changes from an adductor to an abductor and remains functionally activated after its transfer to the insertion of supraspinatus.14,15 LD used as a combined transfer with TM has been found to be more efficient in restoring active external rotation, active forward elevation and abduction strength.16,17,18 LD and TM tendon transfers were initially described for brachial plexus injuries by L’Episcopo in 1934.19 TM has also been used together with the split PM transfer for irreparable tears of both upper and lower portion of subscapularis.20
The LT muscle originates from T4 to T12 vertebrae and inserts into the medial portion of the scapular spine. It is supplied by the transverse cervical artery and innervated by the spinal accessory nerve.21 LT transfer is thought to provide a better anterior-posterior balancing force than LD. Unlike the LD tendon, which provides an internal rotation vector, the LT has a line of pull that is in the same direction as the infraspinatus, more closely resembling the posterosuperior musculature, making it biomechanically a better option.22,23
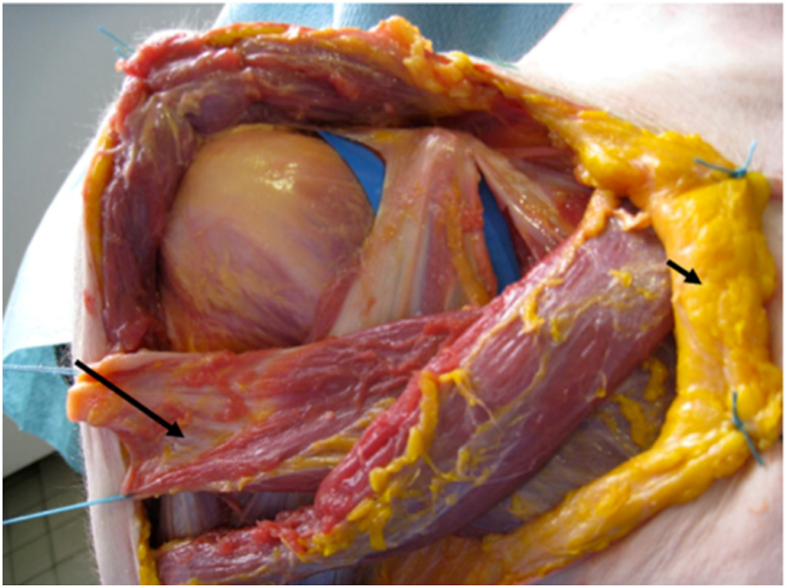
The PM muscle originates from the anterior aspect of the medial clavicle, the sternum, second to seventh ribs and the aponeurosis of the external oblique muscle. Its sternal and clavicular heads are separated by an intermuscular septum that is more apparent laterally.24 It inserts on the lateral lip of the bicipital groove of the humerus (Fig. 1). It is supplied by the pectoral branch of the thoracoacromial artery, with innervations from the lateral and medial pectoral nerves.5 Its function is to flex, internally rotate, and adduct the humerus.3 The PM tendon has a large potential excursion at 18.8 cm.25 Biomechanically, the clavicular portion provides a superior vector, with the sternal head providing an inferior vector.26
Fig. 1.
Cadaveric view of the clavicular and sternal heads of the pectoralis major tendon. Reprinted by permission from Springer Nature, International Orthopaedics, Transfer of the clavicular or sternocostal portion of the pectoralis major muscle for irreparable tears of the subscapularis, Valenti. P et al., Volume 39, Issue 3, p. 477–483. Copyright © 2014.55
3. General prerequisites for tendon transfers, indications and contraindications
3.1. Prerequisites for tendon transfers4,5,27
-
1.
Tissue equilibrium should have occurred (i.e. maturation of the tissue bed before tendon transfer so as not to hinder tendon gliding via scarring or oedema)
-
2.
The tendon should function across a passively mobile and stable joint
-
3.
The transferred muscle should have a similar excursion and tension to the recipient muscle
-
4.
The transferred tendon should be synergistic with a similar line of pull to the recipient tendon
-
5.
The transferred muscle should be expendable without compromising the donor site
-
6.
The transferred muscle should have adequate strength and be used to replace one function of the recipient muscle
-
7.
Accurate positioning of the transferred tendon reimplantation site
-
8.
Physiological tensioning of the transferred muscle-tendon unit
-
9.
Strong osseous fixation of the implanted tendon
-
10.
Meticulous technique to reduce muscle scarring (hence to not hinder the excursion of the transfer)
3.2. Indications21,28,29
-
•
Massive irreparable cuff tear, with significant fatty infiltration of muscle
-
•
Functional deficit
-
•
Young/active patient
3.3. Contraindications23,28,29,30
-
•
Advanced glenohumeral arthritis
-
•
Stiff shoulder
-
•
Deltoid dysfunction
-
•
Brachial plexus injury/dysfunction of intended donor muscle
-
•
Infection
-
•
Inability to comply with post-operative protocol
-
•
Posterosuperior cuff tears with a concurrent subscapularis tear
-
•
A subscapularis tear with a concurrent irreparable supraspinatus tear i.e. Supraspinatus should not be retracted to the glenoid and the fatty infiltration should not exceed grade II. However, subscapularis retraction to the glenoid is acceptable for transfer with fatty degeneration of the torn Subscapularis of grade III or IV.
4. Specific tendon transfers
The surgical technique for each tendon transfer will be discussed below, including specific complications. Note potential complications common to all tendon transfer procedures include neurovascular injury, infection and tendon transfer rupture.
4.1. Latissimus dorsi tendon transfer (LDTT)
Although this tendon transfer is utilised for massive posterosuperior cuff tears, it can also be used for irreparable subscapularis tears, as its direction of pull and function is synergistic to subscapularis.31,32,33
Surgical technique
Gerber et al.34 described the transfer using a two-incision open technique (Posterior and Transdeltoid)4,35 which is a modification of Hoffer technique36 originally described for Erb’s palsy. Later Boileau et al.37 used a single incision Deltopectoral approach to harvest the LD & TM tendons. These tendons are rerouted deep to the Deltoid and anchored to the greater tuberosity.
Arthroscopic assisted LDTT transfer has the advantage of not violating the integrity of the deltoid attachment. An all arthroscopic technique38 and various modifications including mini-invasive axillary approach and arthroscopic humeral head fixation of the graft have been described.39,40
If a tenodesis effect is desired, a more anterior attachment to the front of greater tuberosity or subscapularis is performed. It also provides better humeral head coverage.10,41,42 If Improved external rotation and forward elevation of the arm is desired, LDTT to the infraspinatus attachment is performed.14
Reported complications
Neurovascular injury, failure of the deltoid repair and high rupture rates of 38–43% of the transfer are reported.43,44 The risk of rupture is higher with trans-osseous tunnels or “over the top” fixation to the footprint of the supraspinatus, than posteriorly to the infraspinatus insertion.45
4.2. Teres major tendon transfer
This tendon transfer is utilised for irreparable posterosuperior cuff tears.
Surgical technique
The tendon is usually harvested through a posterior incision proximal to the axilla, safeguarding the neurovascular bundle in the quadrangular space. The tendon is tunnelled underneath the deltoid to the subacromial space and attached to the footprint of supraspinatus.46 Combined (LD&TM) fully arthroscopic techniques have also been described.13
Reported complications
Rupture of the transfer and persistent pseudo paralysis are reported complications. A disadvantage is a need for a broader tunnel, since TM is a short and bulky tendon.46
4.3. Lower trapezius tendon transfer
The LT tendon transfer was first described for the management of paralytic shoulders following brachial plexus injuries in order to restore external rotation.23 This tendon transfer is now also utilised for irreparable posterosuperior cuff tears.
Surgical technique
The LT tendon is harvested and rerouted, with an Achilles tendon allograft, deep to the posterior deltoid and inserted onto the supraspinatus footprint via open47 or arthroscopic methods (Fig. 2).48
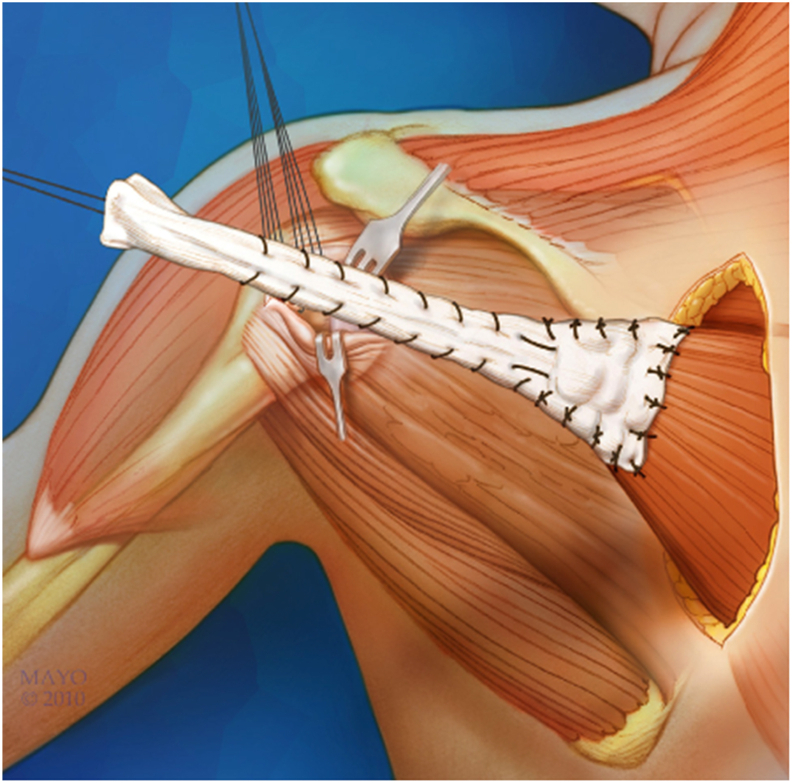
Fig. 2.
The lower trapezius muscle prepared with Achilles tendon allograft. Reprinted from: Operative Techniques in Orthopaedics, Volume 25, Issue 1, B. Schoch; E.Wagner and B. Elhassan, Tendon Transfers for Massive Irreparable Rotator Cuff Tear, p. 57–75, Copyright © 2015, with permission from Elsevier.5
Reported complications
These include seroma formation and distal upper limb sensory deficit.49 With the open method, around 25% of patients had non-union of their acromial osteotomy, but this did not affect their outcomes.47
4.4. Pectoralis major tendon transfer
The PM transfer can be utilised for irreparable anterosuperior cuff tears or isolated subscapularis tears.3
Surgical technique
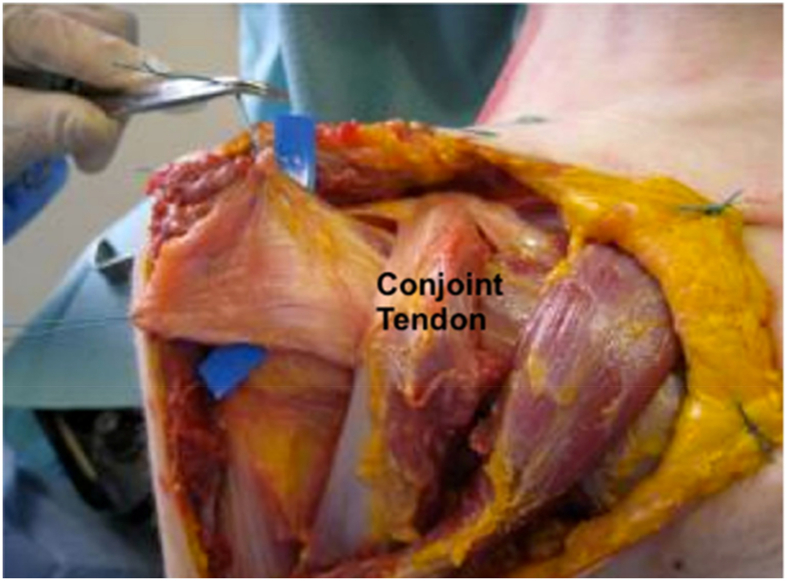
There have been multiple described techniques for PM transfer. In 1997, Wirth and Rockwood50 published their technique for PM tendon transfer, where the superior 2.5–3 cm is transferred into the greater tuberosity. In 2000, Resch et al.51 described a modified technique, whereby the superior one-half to two-thirds of the PM tendon was transferred into the lesser tuberosity, with rerouting behind the conjoint tendon (Fig. 3, Fig. 4). Warner52 described transfer of the sternal portion of the tendon only, deep to the clavicular portion, onto the greater tuberosity. Klepps et al.53 described transferring part or all of the PM tendon beneath the conjoint tendon into the greater tuberosity. Depending on the chosen technique, one or both of the lamina can be used and are passed either anterior or posterior to the conjoint tendon, with the latter providing a ‘pulley’ effect before inserting onto the tuberosity.54 Note that if the tendon is transferred subconjoint, it should remain anterior to the musculocutaneous nerve.
Fig. 3.
Harvesting of the sternal head. Reprinted by permission from Springer Nature, International Orthopaedics, Transfer of the clavicular or sternocostal portion of the pectoralis major muscle for irreparable tears of the subscapularis, Valenti. P et al., Volume 39, Issue 3, p. 477–483. Copyright © 2014.55
Fig. 4.
Transfer of the harvested tendon underneath the conjoint tendon. Reprinted by permission from Springer Nature, International Orthopaedics, Transfer of the clavicular or sternocostal portion of the pectoralis major muscle for irreparable tears of the subscapularis, Valenti. P et al., Volume 39, Issue 3, p. 477–483. Copyright © 2014.55
Reported complications
Jost and Gerber30 reported an overall complication rate of 10% for this procedure. Complications include axillary deep vein thrombosis, residual pain at the PM insertion site, anterior humeral head subluxation and musculocutaneous/axillary nerve dysfunction (note the musculocutaneous nerve is most at risk when the tendon is transferred beneath the conjoint tendon).30,56
5. Rehabilitation
5.1. Lower trapezius and latissimus dorsi transfer
Several studies exploring the use of LD or LT transfers have suggested using the same post-operative protocol for both surgical methods. This involves using a custom brace to immobilise the shoulder in 30–40° of external rotation and 30–40° of abduction. From weeks 6–8 patients can start passive mobilisation of the glenohumeral joint progressing to active-assisted followed by active movement. Elhassan et al.48 allow pool-based exercises to commence at this stage. To avoid stretching of the graft, internal rotation is limited to 0° from weeks 6–12. From 12 weeks there is no restriction to the range of motion and patients can return to most activities of daily living. Strengthening can start from four months.47,57, 58, 59 Moursy et al.60 suggested a shorter period of immobilisation following LD transfer. The shoulder was immobilised in 30° of external rotation and 45° of abduction before active exercises commenced at four weeks, avoiding pain provoking movements. At twelve weeks, full shoulder range of motion was permitted, and patients were allowed to return to light manual work and sports activities.
5.2. Teres major
Management following TM tendon transfer also includes a period of immobilisation. This varied between resting the shoulder in 0° of abduction and 0° of external rotation for six weeks61 or in 0° of abduction and 0–20° of internal rotation.46 Active movement started at six weeks with increasing mobilisation and strengthening from 12 weeks.46,61
5.3. Pectoralis major
Shin at al.56 reviewed eight studies utilising PM tendon transfer for subscapularis tears. They found that the majority of studies used a period of immobilisation in a sling for six weeks and commenced passive motion between days 1 and 3. Gavriilidis et al.62 reported three weeks of immobilisation in a 15-degree abduction pillow, with progressive passive ROM for flexion and internal rotation from day 3. Jost et al.63 allowed passive range of motion within a safe zone identified intraoperatively. Both Elhassan et al.64 and Galatz et al.65 did not allow any movement during the six week immobilisation period. Elhassan permitted passive and active movement following this period whereas Galatz initiated active movement from 12 weeks following a period of passive movement. The majority of studies allowed active range of motion between 6 and 8 weeks post-operatively, with strengthening commenced from 12 to 16 weeks.56,62, 63, 64, 65
Post-operative protocols are described within studies exploring surgical outcomes for each of the tendon transfers. However, currently there is no research comparing rehabilitation methods.
6. Current evidence
6.1. Overview
Tendon transfers for irreparable rotator cuff tears are relatively uncommon procedures and are typically reserved for younger patients with an irreparable cuff tear whose principal symptom is weakness. The majority of evidence in the literature is based on case series, with a lack of comparative studies. Below, we discuss the evidence available for each tendon transfer.
6.2. Latissimus dorsi transfer
The clinical outcomes are better when LDTT is performed as a primary procedure for massive irreparable rotator cuff tear rather than as a salvage procedure.66 Gerber et al. showed substantial and durable improvements in shoulder function and pain relief at a mean follow-up of 147 months.67,68 Another long-term follow-up with radiographic and clinical reviews on 115 shoulders with LDTT revealed that pain relief and improved shoulder function were maintained at 9.3 years. Younger patients had better outcomes.69
A recent systematic review of arthroscopic assisted LDTT72 noted that they had no cases of deltoid dysfunction as deltoid integrity was not violated. This led to a larger improvement in abduction as compared to the systematic review of open LDTT.73
The long-term review of LDTTs after failed cuff repairs have shown poor results. Castricini et al.74 in their series of eighty-six patients with three-year follow-up noted less favourable outcomes of arthroscopic assisted LDTT in patients who had lower pre-operative Constant scores and failed cuff repairs. Grimberg et al.75 showed similar findings of inferior scores for failed cuff repairs.
There is growing evidence on EMG that the functional improvement after the LDTT is due to strong muscle activity. 70, 71 Calvert et al.71 in their 4.7 years follow-up, showed good outcomes along with evidence of LDTT working as an active muscle unit rather than just interposition or tenodesis effect on the humeral head. They noted the improvement in ROM was mainly in abduction and external rotation. In a 3D Motion analysis, the proprioceptive ability was similar to the non-operated side.76
Short term reviews of arthroscopic assisted LDTT showed promising results. A systematic review in 2018 concluded that arthroscopic-assisted LDTT provides a marked improvement in shoulder pain, strength and function. Furthermore, there is a low risk of complications but further high-quality comparative studies are required.72
LDTT can also be considered for irreparable subscapularis tears as an effective option as its direction of pull and function is relatively similar to Subscapularis. Mun et al.31 found this resulted in pain relief, improved shoulder function and outcome scores. Elhassan et al.32 showed the potential of LDTT as an option for irreparable subscapular tear. Their series of fifty-four patients (fourteen open and forty-two arthroscopic) showed good outcomes. Kany et al.33 also showed good outcomes with arthroscopic-assisted LDTT for subscapularis tear.
6.3. Teres major transfer
Literature for an isolated TM transfer is scarce. Short term and midterm results reveal that it effectively restores function and relieves pain with overall clinical improvement for irreparable posterosuperior cuff tears.46,77 Long-term review with a mean follow-up of 10 years, performed for similar indications to LDTT, shows comparable outcomes, suggesting TM as an effective alternative transfer to LD.61 Lafosse et al.78 demonstrated in a cadaveric study that bipolar TM transfer is anatomically feasible for an irreparable subscapularis tear. Longo et al.79 in a systematic review reported restoration of anterior elevation, along with external rotation of the shoulder, when combined TM & LD transfers were done.
6.4. Lower trapezius transfer
Clouette et al.80 published a systematic review of LT transfers. With regards to clinical outcomes, two studies were included which revealed an improvement of both forward elevation and external rotation by greater than 30°. One of these studies47 utilised an open technique with an Achilles tendon allograft. They reported a 34 point improvement in the Disabilities of the Arm, Shoulder and Hand (DASH) score. Furthermore, they found an improvement of the shoulder subjective value (SSV) from 54% pre-operatively to 78% post-operatively. The second study58 describes an arthroscopic-assisted LT tendon transfer, using a semitendinosus tendon autograft for augmentation. Fourteen patients underwent the procedure, with a mean follow-up of two years. They found an improvement in range of motion, with SSV increasing from 40 to 70% and the Constant score improving from 35 to 60.
In 2020, the largest study to date evaluating the arthroscopically-assisted LT tendon transfer was published by Elhassan et al.49 Forty-one patients underwent this procedure, of which two-thirds had had a previous failed rotator cuff repair. The average follow-up was 14 months. Thirty-seven patients (90%) had significant improvement in all outcome scores: Visual analogue scale (VAS), SSV and DASH. Overall, a good improvement was seen in the range of motion. Of note, three patients with pre-operative features of cuff arthropathy had persistent pain and stiffness following surgery, with two going on to have a reverse shoulder arthroplasty. Furthermore, two patients had traumatic ruptures of the tendon transfers following a fall. One of these underwent revision repair surgery.
Woodmass et al.81 carried out a multicentre retrospective analysis comparing the outcomes of open and arthroscopic-assisted LD transfer and arthroscopic-assisted LT transfer. Ten patients underwent open LD transfer, sixteen arthroscopic-assisted LD transfer and eight arthroscopic-assisted LT transfers, with a mean follow-up of 22 months. The arthroscopic-assisted LD and LT transfers resulted in improvement in pain and function at 2-years follow-up. Furthermore, arthroscopic-assisted LD provided significantly improved outcomes when compared to the open LD transfer, at 2-years follow-up. In total, there were six complications: two axillary nerve injuries, two infections, adhesive capsulitis and complex regional pain syndrome. Overall, they concluded that the arthroscopic-assisted LT transfer was a safe and effective alternative to the arthroscopic-assisted LD transfer.
6.5. Pectoralis major transfer
In 2003, Jost et al.63 published on the outcomes of PM transfer for irreparable subscapularis tears. Twenty transfers in twenty-eight patients were carried out. The mean Constant score increased from 47% preoperatively to 70% post-operatively. The mean SSV increased from 23% preoperatively to 55% post-operatively. There was an improvement in forward flexion and abduction, with loss of external rotation. Overall, five patients were disappointed or dissatisfied with the outcome. A key finding was that if an irreparable subscapularis tear was associated with an irreparable supraspinatus tear, the results were less favourable. The authors concluded that in this scenario, a pectoralis transfer may not be warranted.
Shin et al.56 published a systematic review on PM transfers for the treatment of irreparable subscapularis tears. Eight studies were included with a total of 195 shoulders. Mean follow-up was 33.4 months. Constant scores improved from a mean pre-operative score of 37.8 to a mean post-operative score of 61.3. The scores were significantly higher in patients who received a subcoracoid transfer. Pain scores could not be pooled as the studies used different scales for assessment. Functional outcomes were not as positive for massive rotator cuff tears. From all the cases, there was one report of a transient musculocutaneous nerve palsy and one axillary nerve dysfunction.
In 2017, Moroder82 reported their outcomes for twenty-seven consecutive patients who were treated with partial subcoracoid PM tendon transfers. Twenty-two patients had long-term follow-up with a mean of 10 years and 77% were very satisfied at the final follow-up. The improvement in pain was maintained at final follow-up. The internal rotation strength increased at short-term follow-up but returned to the pre-operative level at the long-term follow-up. Furthermore, the improvement in range of motion declined over time, although it remained improved compared to the pre-operative baseline. One patient underwent revision surgery to a reverse shoulder arthroplasty, due to persistent pain.
In 2019, Ernstbrunner et al.83 published their long-term outcomes of PM transfer, for the treatment of irreparable subscapularis tears, with a mean follow-up of 20 years. Their operative technique was a complete release of the PM tendon, with transfer over the conjoined tendon, to the medial aspect of the greater tuberosity. The mean relative Constant score and SSV both improved significantly from preoperatively to post-operatively, with all patients rating their results as good or excellent. However, active internal and external rotation had declined significantly by final follow-up. Four out of twenty-one shoulders showed evidence of glenohumeral arthropathy but were mildly symptomatic or asymptomatic at final follow-up. Six shoulders underwent re-operation, and one shoulder underwent a reverse shoulder arthroplasty.
7. Conclusion
Management of irreparable rotator cuff tears in younger patients remains a difficult clinical challenge. Although tendon transfers have been used, the evidence so far is limited, and more comparative studies are needed to inform future clinical decision making. For posterosuperior rotator cuff tears, the LD transfer is the most commonly used, with the LT tendon transfer providing a surgical alternative. For the management of irreparable subscapularis tears, there is controversy about whether PM or LD provides the best tendon transfer option, with the latter having a more comparable line of pull to subscapularis. Again, more evidence is required before any conclusions can be drawn.
Funding
Nil.
Declaration of competing interest
Nil.
Acknowledgements for illustrations
Valenti et al. Transfer of the clavicular or sternocostal portion of the pectoralis major muscle for irreparable tears of the subscapularis. International Orthopaedics (Springer Nature).
B. Schoch, E. Wagner and B. Elhassan. Tendon transfers for massive irreparable rotator cuff tear. Operative Techniques in Orthopaedics (Elsevier).
References
- 1.Yamamoto A., Takagishi K., Osawa T. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010;19(1):116–120. doi: 10.1016/j.jse.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 2.Cvetanovich G.L., Waterman B.R., Verma N.N., Romeo A.A. Management of the irreparable rotator cuff tear. J Am Acad Orthop Surg. 2019;27(24):909–917. doi: 10.5435/JAAOS-D-18-00199. [DOI] [PubMed] [Google Scholar]
- 3.Omid R., Lee B. Tendon transfers for irreparable rotator cuff tears. J Am Acad Orthop Surg. 2013;21(8):492–501. doi: 10.5435/JAAOS-21-08-492. [DOI] [PubMed] [Google Scholar]
- 4.Checchia C., Domos P., Grimberg J., Kany J. Current options in tendon transfers for irreparable rotator cuff tears. JBJS Rev. 2019;7(2):e6. doi: 10.2106/JBJS.RVW.18.00044. [DOI] [PubMed] [Google Scholar]
- 5.Schoch B., Wagner E., Elhassan B. Tendon transfers for massive irreparable rotator cuff tear. Operat Tech Orthop. 2015;25(1):57–75. doi: 10.1053/j.oto.2014.11.001. [DOI] [Google Scholar]
- 6.Burkhart S.S. Arthroscopic treatment of massive rotator cuff tears: clinical results and biomechanical rationale. Clin Orthop Relat Res. 1991;267:45–56. doi: 10.1097/00003086-199106000-00006. [DOI] [PubMed] [Google Scholar]
- 7.George M.S., Khazzam M. Latissimus dorsi tendon rupture. J Am Acad Orthop Surg. 2019;27(4):113–118. doi: 10.5435/JAAOS-D-17-00581. [DOI] [PubMed] [Google Scholar]
- 8.Buijze G.A., Keereweer S., Jennings G., Vorster W., Debeer J. Musculotendinous transfer as a treatment option for irreparable posterosuperior rotator cuff tears: teres major or latissimus dorsi? Clin Anat. 2007;20(8):919–923. doi: 10.1002/ca.20547. [DOI] [PubMed] [Google Scholar]
- 9.Galasso O., Mantovani M., Muraccini M. The latissimus dorsi tendon functions as an external rotator after arthroscopic-assisted transfer for massive irreparable posterosuperior rotator cuff tears. Knee Surgery. Sport Traumatol Arthrosc. 2020;28:2367–2376. doi: 10.1007/s00167-019-05819-2. [DOI] [PubMed] [Google Scholar]
- 10.Burnier M., Elhassan B.T., Sanchez-Sotelo J. Surgical management of irreparable rotator cuff tears: what works, what does not, and what is coming. J Bone Jt Surg Am. 2019;101(17):1603–1612. doi: 10.2106/JBJS.18.01392. [DOI] [PubMed] [Google Scholar]
- 11.Hernández-Cortés P., Rivadeneira-Ruiz M., O’Valle F., Sánchez-Montesinos I., Roda O. Anatomic study of pedicled bipolar teres major transfer for irreparable posterosuperior rotator cuff tears. J Shoulder Elbow Surg. 2018;27(10):1740–1747. doi: 10.1016/j.jse.2018.04.008. [DOI] [PubMed] [Google Scholar]
- 12.Donohue B.F., Lubitz M.G., Kremchek T.E. Sports injuries to the latissimus dorsi and teres major. Am J Sports Med. 2017;45(10):2428–2435. doi: 10.1177/0363546516676062. [DOI] [PubMed] [Google Scholar]
- 13.Kany J., Selim H.A. Combined fully arthroscopic transfer of latissimus dorsi and teres major for treatment of irreparable posterosuperior rotator cuff tears. Arthrosc Tech. 2020;9(1):E147–E157. doi: 10.1016/j.eats.2019.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Magermans D.J., Chadwick E.K.J., Veeger H.E.J., Van Der Helm F.C.T., Rozing P.M. Biomechanical analysis of tendon transfers for massive rotator cuff tears. Clin Biomech. 2004;19(4):350–357. doi: 10.1016/j.clinbiomech.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 15.Steenbrink F., Nelissen R.G.H.H., Meskers C.G.M., van de Sande M.A.J., Rozing P.M., de Groot J.H. Teres major muscle activation relates to clinical outcome in tendon transfer surgery. Clin Biomech. 2010;25(3):187–193. doi: 10.1016/j.clinbiomech.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 16.Gerhardt C., Lehmann L., Lichtenberg S., Magosch P., Habermeyer P. Modified L’Episcopo tendon transfers for irreparable rotator cuff tears: 5-year follow-up. Clin Orthop Relat Res. 2010;468(6):1572–1577. doi: 10.1007/s11999-009-1030-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lichtenberg S., Magosch P., Habermeyer P. Are there advantages of the combined latissimus-dorsi transfer according to L’Episcopo compared to the isolated latissimus-dorsi transfer according to Herzberg after a mean follow-up of 6 years? A matched-pair analysis. J Shoulder Elbow Surg. 2012;21(11):1499–1507. doi: 10.1016/j.jse.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 18.Henseler J.F., Kolk A., Zondag B., Nagels J., de Groot J.H., Nelissen R.G.H.H. Three-dimensional shoulder motion after teres major or latissimus dorsi tendon transfer for posterosuperior rotator cuff tears. J Shoulder Elbow Surg. 2017;26(11):1955–1963. doi: 10.1016/j.jse.2017.03.023. [DOI] [PubMed] [Google Scholar]
- 19.L’Episcopo J.B. Tendon transplantation in obstetrical paralysis. Am J Surg. 1934;25(1):122–125. doi: 10.1016/S0002-9610(34)90143-4. [DOI] [Google Scholar]
- 20.Gerber A., Clavert P., Millett P.J., Holovacs T.F., Warner J.J.P. Split pectoralis major and teres major tendon transfers for reconstruction of irreparable tears of the subscapularis. Tech Shoulder Elbow Surg. 2004;5(1):5–12. doi: 10.1097/00132589-200403000-00002. [DOI] [Google Scholar]
- 21.Stoll L.E., Codding J.L. Lower trapezius tendon transfer for massive irreparable rotator cuff tears. Orthop Clin N Am. 2019;50(3):375–382. doi: 10.1016/j.ocl.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 22.Omid R., Heckmann N., Wang L., McGarry M.H., Vangsness C.T., Lee T.Q. Biomechanical comparison between the trapezius transfer and latissimus transfer for irreparable posterosuperior rotator cuff tears. J Shoulder Elbow Surg. 2015;24(10):1635–1643. doi: 10.1016/j.jse.2015.02.008. [DOI] [PubMed] [Google Scholar]
- 23.Aibinder W.R., Elhassan B.T. Arthroscopic lower trapezial transfer for irreparable rotator cuff tears. Operat Tech Orthop. 2018;28(4):217–225. doi: 10.1053/j.oto.2018.08.006. [DOI] [Google Scholar]
- 24.Nelson G.N., Namdari S., Galatz L., Keener J.D. Pectoralis major tendon transfer for irreparable subscapularis tears. J Shoulder Elbow Surg. 2014;23(6):909–918. doi: 10.1016/j.jse.2013.12.035. [DOI] [PubMed] [Google Scholar]
- 25.Herzberg G., Urien J.P., Dimnet J., Lyon F. Potential excursion and relative tension of muscles in the shoulder girdle: relevance to tendon transfers r. JSES. 1999;8(5):430–437. doi: 10.1016/S1058-2746(99)90072-1. [DOI] [PubMed] [Google Scholar]
- 26.Jennings G.J., Keereweer S., Buijze G.A., De Beer J., DuToit D. Transfer of segmentally split pectoralis major for the treatment of irreparable rupture of the subscapularis tendon. J Shoulder Elbow Surg. 2007;16(6):837–842. doi: 10.1016/j.jse.2007.03.030. [DOI] [PubMed] [Google Scholar]
- 27.Wilbur D., Hammert W.C. Principles of tendon transfer. Hand Clin. 2016;32(3):283–289. doi: 10.1016/j.hcl.2016.03.001. [DOI] [PubMed] [Google Scholar]
- 28.Pagani N.R., Cusano A., Li X. Latissimus dorsi tendon transfer with acromial osteotomy for massive irreparable rotator cuff tear. Arthrosc Tech. 2018;7(2):E105–E112. doi: 10.1016/j.eats.2017.08.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Talbot J.C., Watts A.C., Grimberg J., Funk L. Shoulder tendon transfers for rotator cuff deficiency. Shoulder Elbow. 2013;5(1):1–11. doi: 10.1111/j.1758-5740.2012.00224.x. [DOI] [Google Scholar]
- 30.Jost B., Gerber C. Pectoralis major transfer for subscapularis insufficiency. Tech Shoulder Elbow Surg. 2004;5(3):157–164. doi: 10.1097/01.bte.0000135966.61724.1f. [DOI] [Google Scholar]
- 31.Mun S.W., Kim J.Y., Yi S.H., Baek C.H. Latissimus dorsi transfer for irreparable subscapularis tendon tears. J Shoulder Elbow Surg. 2018;27(6):1057–1064. doi: 10.1016/j.jse.2017.11.022. [DOI] [PubMed] [Google Scholar]
- 32.Elhassan B.T., Wagner E.R., Kany J. Latissimus dorsi transfer for irreparable subscapularis tear. J Shoulder Elbow Surg. 2020;29(10):2128–2134. doi: 10.1016/j.jse.2020.02.019. [DOI] [PubMed] [Google Scholar]
- 33.Kany J., Guinand R., Croutzet P., Valenti P., Werthel J.D., Grimberg J. Arthroscopic-assisted latissimus dorsi transfer for subscapularis deficiency. Eur J Orthop Surg Traumatol. 2016;26(3):329–334. doi: 10.1007/s00590-016-1753-3. [DOI] [PubMed] [Google Scholar]
- 34.Gerber C., Vinh T., Hertel R., Hess C. Latissimus dorsi transfer for the treatment of massive tears of the rotator cuff A preliminary report. Clin Orthop Relat Res. 1988;232:51–61. [PubMed] [Google Scholar]
- 35.Wagner E.R., Elhassan B.T. Tendon transfers for rotator cuff pathologies. Curr Orthop Pract. 2019;30(3):192–199. doi: 10.1097/BCO.0000000000000757. [DOI] [Google Scholar]
- 36.Hoffer M.M., Wickenden R., Roper B. Brachial plexus birth palsies. Results of tendon transfers to the rotator cuff. J Bone Jt Surg Am. 1978;60:691–695. doi: 10.2106/00004623-197860050-00019. [DOI] [PubMed] [Google Scholar]
- 37.Boileau P., Chuinard C., Roussanne Y., Neyton L., Trojani C. Modified latissimus dorsi and teres major transfer through a single delto-pectoral approach for external rotation deficit of the shoulder: as an isolated procedure or with a reverse arthroplasty. J Shoulder Elbow Surg. 2007;16(6):671–682. doi: 10.1016/j.jse.2007.02.127. [DOI] [PubMed] [Google Scholar]
- 38.Cutbush K., Peter N.A., Hirpara K. All-arthroscopic latissimus dorsi transfer. Arthrosc Tech. 2016;5(3):e607–e613. doi: 10.1016/j.eats.2016.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kany J., Kumar H.A., Chang V.K., Grimberg J., Garret J., Valenti P. Mini invasive axillary approach and arthroscopic humeral head interference screw fixation for latissimus dorsi transfer in massive and irreparable posterosuperior rotator cuff tears. Tech Shoulder Elbow Surg. 2010;11(1):8–14. doi: 10.1097/BTE.0b013e3181cabdab. [DOI] [Google Scholar]
- 40.Goldstein Y., Grimberg J., Valenti P., Chechik O., Drexler M., Kany J. Arthroscopic fixation with a minimally invasive axillary approach for latissimus dorsi transfer using an endobutton in massive and irreparable postero-superior cuff tears. Int J Shoulder Surg. 2013;7(2):79–82. doi: 10.4103/0973-6042.114223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Codsi M.J., Hennigan S., Herzog R. Latissimus dorsi tendon transfer for irreparable posterosuperior rotator cuff tears. Surgical technique. J Bone Jt Surg Am. 2007;89(2):1–9. doi: 10.2106/00004623-200703001-00001. [DOI] [PubMed] [Google Scholar]
- 42.Herzberg G., Urien J.P., Dimnet J. Potential excursion and relative tension of muscles in the shoulder girdle: relevance to tendon transfers. J Shoulder Elbow Surg. 1999;8(5):430–437. doi: 10.1016/S1058-2746(99)90072-1. [DOI] [PubMed] [Google Scholar]
- 43.Kany J., Grimberg J., Amaravathi R.S., Sekaran P., Scorpie D., Werthel J.D. Arthroscopically-assisted latissimus dorsi transfer for irreparable rotator cuff insufficiency: modes of failure and clinical correlation. Arthrosc J Arthrosc Relat Surg. 2018;34(4):1139–1150. doi: 10.1016/j.arthro.2017.10.052. [DOI] [PubMed] [Google Scholar]
- 44.Muench L.N., Kia C., Williams A.A. High clinical failure rate after latissimus dorsi transfer for revision massive rotator cuff tears. Arthrosc J Arthrosc Relat Surg. 2020;36(1):88–94. doi: 10.1016/j.arthro.2019.07.034. [DOI] [PubMed] [Google Scholar]
- 45.Kany J., Sekaran P., Grimberg J. Risk of latissimus dorsi tendon rupture after arthroscopic transfer for posterior superior rotator cuff tear: a comparative analysis of 3 humeral head fixation techniques. J Shoulder Elbow Surg. 2020;29(2):282–290. doi: 10.1016/j.jse.2019.06.019. [DOI] [PubMed] [Google Scholar]
- 46.Henseler J.F., Nagels J., Van Der Zwaal P., Nelissen R.G.H.H. Teres major tendon transfer for patients with massive irreparable posterosuperior rotator cuff tears: short-term clinical results. Bone Jt J. 2013;95-B(4):523–529. doi: 10.1302/0301-620X.95B4.30390. [DOI] [PubMed] [Google Scholar]
- 47.Elhassan B.T., Wagner E.R., Werthel J.D. Outcome of lower trapezius transfer to reconstruct massive irreparable posterior-superior rotator cuff tear. J Shoulder Elbow Surg. 2016;25(8):1346–1353. doi: 10.1016/j.jse.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 48.Elhassan B.T., Alentorn-Geli E., Assenmacher A.T., Wagner E.R. Arthroscopic-assisted lower trapezius tendon transfer for massive irreparable posterior-superior rotator cuff tears: surgical technique. Arthrosc Tech. 2016;5(5):e981–e988. doi: 10.1016/j.eats.2016.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Elhassan B.T., Sanchez-Sotelo J., Wagner E.R. Outcome of arthroscopically assisted lower trapezius transfer to reconstruct massive irreparable posterior-superior rotator cuff tears. J Shoulder Elbow Surg. 2020;29(10):2135–2142. doi: 10.1016/j.jse.2020.02.018. [DOI] [PubMed] [Google Scholar]
- 50.Wirth M.A., Rockwood C.A. Operative treatment of irreparable rupture of the subscapularis. J Bone Jt Surg Am. 1997;79(5):722–731. doi: 10.2106/00004623-199705000-00012. [DOI] [PubMed] [Google Scholar]
- 51.Resch H., Povacz P., Ritter E., Matschi W. Transfer of the pectoralis major muscle for the treatment of irreparable rupture of the subscapularis tendon. J Bone Jt Surg Am. 2000;82(3):372–382. doi: 10.2106/00004623-200003000-00008. [DOI] [PubMed] [Google Scholar]
- 52.Warner J.J.P. Management of massive irreparable rotator cuff tears: the role of tendon transfer. J Bone Jt Surg Am. 2000;82-A(6):878–887. [PubMed] [Google Scholar]
- 53.Klepps S., Galatz L., Yamaguchi K. Subcoracoid pectoralis major transfer: a salvage procedure for irreparable subscapularis deficiency. Tech Shoulder Elbow Surg. 2001;2(2):85–91. doi: 10.1097/00132589-200106000-00003. [DOI] [PubMed] [Google Scholar]
- 54.Kany J. Tendon transfer for anterosuperior cuff: the pectoralis major transfer. In: Gomes N.S., Kovačič L., Martetschläger F., Milano G., editors. Massive and Irreparable Rotator Cuff Tears. Springer; Berlin, Heidelberg: 2020. pp. 237–243. [DOI] [Google Scholar]
- 55.Valenti P., Boughebri O., Moraiti C. Transfer of the clavicular or sternocostal portion of the pectoralis major muscle for irreparable tears of the subscapularis. Technique and clinical results. Int Orthop. 2015;39(3):477–483. doi: 10.1007/s00264-014-2566-9. [DOI] [PubMed] [Google Scholar]
- 56.Shin J.J., Saccomanno M.F., Cole B.J., Romeo A.A., Nicholson G.P., Verma N.N. Pectoralis major transfer for treatment of irreparable subscapularis tear: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2016;24(6):1951–1960. doi: 10.1007/s00167-014-3229-5. [DOI] [PubMed] [Google Scholar]
- 57.Wagner E.R., Woodmass J.M., Welp K.M. Novel arthroscopic tendon transfers for posterosuperior rotator cuff tears latissimus dorsi and lower trapezius transfers. JBJS Essent Surg Tech. 2018;8(2):e12. doi: 10.2106/JBJS.ST.17.00062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Valenti P., Werthel J.D. Lower trapezius transfer with semitendinosus tendon augmentation: indication, technique, results. Obere Extrem. 2018;13(4):261–268. doi: 10.1007/s11678-018-0495-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wagner E.R., Elhassan B.T. Surgical management of massive irreparable posterosuperior rotator cuff tears: arthroscopic-assisted lower trapezius transfer. Curr Rev Musculoskelet Med. 2020;13(5):592–604. doi: 10.1007/s12178-020-09657-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Moursy M., Schmalzl J., Kadavkolan A.S., Bartels N., Lehmann L.J. Latissimus dorsi transfer for massive posterosuperior rotator cuff tears: what affects the postoperative outcome? J Shoulder Elbow Surg. 2019;28(11):2191–2197. doi: 10.1016/j.jse.2019.03.028. [DOI] [PubMed] [Google Scholar]
- 61.Kolk A., Henseler J.F., Overes F.J., Nagels J., Nelissen R.G.H.H. Teres major tendon transfer in the treatment of irreparable posterosuperior rotator cuff tears. Bone Jt J. 2018;100-B(3):309–317. doi: 10.1302/0301-620X.100B3.BJJ-2017-0920.R1. [DOI] [PubMed] [Google Scholar]
- 62.Gavriilidis I., Kircher J., Magosch P., Lichtenberg S., Habermeyer P. Pectoralis major transfer for the treatment of irreparable anterosuperior rotator cuff tears. Int Orthop. 2010;34(5):689–694. doi: 10.1007/s00264-009-0799-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jost B., Puskas G.J., Lustenberger A., Gerber C. Outcome of pectoralis major transfer for the treatment of irreparable subscapularis tears. J Bone Jt Surg Am. 2003;85(10):1944–1951. doi: 10.2106/00004623-200310000-00012. [DOI] [PubMed] [Google Scholar]
- 64.Elhassan B., Ozbaydar M., Massimini D., Diller D., Higgins L., Warner J.J.P. Transfer of pectoralis major for the treatment of irreparable tears of subscapularis: does it work? J Bone Jt Surg Br. 2008;90-B(8):1059–1065. doi: 10.1302/0301-620X.90B8.20659. [DOI] [PubMed] [Google Scholar]
- 65.Galatz L.M., Connor P.M., Calfee R.P., Hsu J.C., Yamaguchi K. Pectoralis major transfer for anterior-superior subluxation in massive rotator cuff insufficiency. J Shoulder Elbow Surg. 2003;12(1):1–5. doi: 10.1067/mse.2003.128137. [DOI] [PubMed] [Google Scholar]
- 66.Warner J.J.P., Parsons I.V.I.M. Latissimus dorsi tendon transfer: a comparative analysis of primary and salvage reconstruction of massive, irreparable rotator cuff tears. J Shoulder Elbow Surg. 2001;10(6):514–521. doi: 10.1067/mse.2001.118629. [DOI] [PubMed] [Google Scholar]
- 67.Ebert-Fillmer S., Bloos U.T., El Masri S., Stangl R. Latissimus-dorsi-Transfer bei irreparablen posterior-superioren Rotatorenmanschettendefekten bei älteren Patienten. Unfallchirurg. 2019;122(7):544–554. doi: 10.1007/s00113-018-0557-9. [DOI] [PubMed] [Google Scholar]
- 68.Gerber C., Rahm S.A., Catanzaro S., Farshad M., Moor B.K. Latissimus dorsi tendon transfer for treatment of irreparable posterosuperior rotator cuff tears: long-term results at a minimum follow-up of ten years. J Bone Jt Surg Am. 2013;95(21):1920–1926. doi: 10.2106/JBJS.M.00122. [DOI] [PubMed] [Google Scholar]
- 69.El-Azab H.M., Rott O., Irlenbusch U. Long-term follow-up after latissimus dorsi transfer for irreparable posterosuperior rotator cuff tears. J Bone Jt Surg Am. 2015;97(6):462–469. doi: 10.2106/JBJS.M.00235. [DOI] [PubMed] [Google Scholar]
- 70.Irlenbusch U., Bernsdorf M., Born S., Gansen H.K., Lorenz U. Electromyographic analysis of muscle function after latissimus dorsi tendon transfer. J Shoulder Elbow Surg. 2008;17(3):492–499. doi: 10.1016/j.jse.2007.11.012. [DOI] [PubMed] [Google Scholar]
- 71.Clavert P., Arndt J., Daemgen F., Kempf J.F. Long-term outcomes of latissimus dorsi transfer for irreparable rotator cuff tears. Int Orthop. 2020;44(5):905–910. doi: 10.1007/s00264-020-04540-x. [DOI] [PubMed] [Google Scholar]
- 72.Memon M., Kay J., Quick E. Arthroscopic-assisted latissimus dorsi tendon transfer for massive rotator cuff tears: a systematic review. Orthop J Sport Med. 2018;6(6) doi: 10.1177/2325967118777735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Namdari S., Voleti P., Baldwin K., Glaser D., Huffman G.R. Latissimus dorsi tendon transfer for irreparable rotator cuff tears: a systematic review. J Bone Jt Surg Am. 2012;94(10):891–898. doi: 10.2106/JBJS.K.00841. [DOI] [PubMed] [Google Scholar]
- 74.Castricini R., De Benedetto M., Familiari F. Functional status and failed rotator cuff repair predict outcomes after arthroscopic-assisted latissimus dorsi transfer for irreparable massive rotator cuff tears. J Shoulder Elbow Surg. 2016;25(4):658–665. doi: 10.1016/j.jse.2015.08.043. [DOI] [PubMed] [Google Scholar]
- 75.Grimberg J., Kany J., Valenti P., Amaravathi R., Ramalingam A.T. Arthroscopic-assisted latissimus dorsi tendon transfer for irreparable posterosuperior cuff tears. Arthrosc J Arthrosc Relat Surg. 2015;31(4):599–607. doi: 10.1016/j.arthro.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 76.Hetto P., Erhard S., Thielen M. 3D motion analysis of latissimus dorsi tendon transfer in patients with posterosuperior rotator cuff tears: analysis of proprioception and the ability to perform ADLS. Orthop Traumatol Surg Res. 2020;106(1):39–44. doi: 10.1016/j.otsr.2019.10.018. [DOI] [PubMed] [Google Scholar]
- 77.Celli A., Marongiu M.C., Rovesta C., Celli L. Transplant of the teres major in the treatment of irreparable injuries of the rotator cuff (long-term analysis of results) Chir Organi Mov. 2005;90(2):121–132. [PubMed] [Google Scholar]
- 78.Lafosse T., Le Hanneur M., Lee J., Elhassan B. Bipolar pedicled teres major transfer for irreparable subscapularis tendon tears: an anatomic feasibility study. J Shoulder Elbow Surg. 2018;27(5):931–939. doi: 10.1016/j.jse.2017.11.024. [DOI] [PubMed] [Google Scholar]
- 79.Longo U.G., Franceschetti E., Petrillo S., Maffulli N., Denaro V. Latissimus dorsi tendon transfer for massive irreparable rotator cuff tears: a systematic review. Sports Med Arthrosc. 2011;19(4):428–437. doi: 10.1097/JSA.0b013e3182390639. [DOI] [PubMed] [Google Scholar]
- 80.Clouette J., Leroux T., Shanmugaraj A. The lower trapezius transfer: a systematic review of biomechanical data, techniques, and clinical outcomes. J Shoulder Elbow Surg. 2020;29(7):1505–1512. doi: 10.1016/j.jse.2019.12.019. [DOI] [PubMed] [Google Scholar]
- 81.Woodmass J.M., Wagner E.R., Chang M.J. Arthroscopic lower trapezius tendon transfer provides equivalent outcomes to latissimus dorsi transfer in the treatment of massive posterosuperior rotator cuff tears. J ISAKOS. 2020;5(5):269–274. doi: 10.1136/jisakos-2019-000341. [DOI] [Google Scholar]
- 82.Moroder P., Schulz E., Mitterer M., Plachel F., Resch H., Lederer S. Long-term outcome after pectoralis major transfer. J Bone Jt Surg Am. 2017;99(3):239–245. doi: 10.2106/JBJS.16.00485. [DOI] [PubMed] [Google Scholar]
- 83.Ernstbrunner L., Wieser K., Catanzaro S. Long-term outcome of pectoralis major transfer for the treatment of irreparable subscapularis tears: an update 20 years postoperatively. J Bone Jt Surg Am. 2019;101(23):2091–2100. doi: 10.2106/JBJS.19.00172. [DOI] [PubMed] [Google Scholar]