Abstract
Complex bronchial ruptures are rare. Primary surgical repair is the preferred procedure. The aim of this retrospective case series was to study the clinical presentation of these complex bronchial injuries and their management and outcomes. Patients with injuries to the trachea or those who had simple single bronchial rupture and isolated lobar and segmental injuries were excluded. Twenty-one patients were operated for bronchial rupture due to blunt chest trauma. Seven patients had complex bronchial injuries and had right bronchial tree injury (n = 3), left bronchial tree injury (n = 3), and rupture of both right and left main bronchi (n = 1). Fibreoptic bronchoscopy established the diagnosis in all patients. Postoperative complications included atelectasis in four patients (57%) and left recurrent laryngeal nerve paralysis (n = 1; 14.3%), and one patient required tracheostomy (14.3%). All patients had follow-up bronchoscopy 2 months later, which showed no stenosis or scar formation in any of the patients. We concluded that primary repair of complex bronchial injuries, with preservation of the normal functioning lung, is the preferred option as it carries favorable immediate- and long-term results.
Keywords: Bronchial rupture, Bronchial injuries, Blunt thoracic trauma, Bronchial repair
Introduction
Bronchial injuries are rare. Although it was reported that their incidence declined following introduction of safety belts and airbags [1], they have become more common due to the increasing use of high-speed transportation [2]. The complex bronchial injuries are sometimes difficult to diagnose and treat. They usually require a highly specialized thoracic surgery center that manages such rare injuries. The priority in the management of patients with these injuries is to reconstruct the airway with maximal preservation of the normal functioning lung [3].
The aim of this study is to present our experience in the diagnosis, management, and outcome of these complex bronchial injuries.
Patients and methods
This is a retrospective clinical study that included the patients who had blunt thoracic trauma and admitted to the Thoracic Surgery Department, Chest Disease Hospital, Kuwait, with a diagnosis of a complex bronchial injuries during the period between January 1995 and December 2019. The study was conducted following the approval of the medical research ethics committee. Those patients, who had injuries to the trachea or simple single bronchial ruptures (within 2.5–3 cm from the carina on the left, and within 1 cm from the carina on the right side), as well as isolated lobar and segmental injuries, were excluded from the study. Right thoracotomy approach through the fourth intercostal space was used for the repair of the right-sided injuries and proximal left main bronchus injury in one patient, while left thoracotomy approach was used for the patients with left-sided injuries, except in one with bilateral bronchial injury (Table 1). The anastomosis was achieved using 4-0 vicryl sutures (Ethicon. Inc.) and was re-enforced with a pleural flap.
Table 1.
Site of complex tracheobronchial injury and type of surgery performed
| Serial | Site of tracheobronchial injury | Surgical procedure | Type of intubation | Period of postoperative ventilation in days | Postoperative complications |
|---|---|---|---|---|---|
| 1 | RMB + RUL + SSLL | Primary repair + sleeve upper lobectomy and re-implantation of SSLL | Single lumen | 14 | Tracheostomy |
| 2 | RIB + RUL | Primary repair + sleeve upper lobectomy | Single lumen | 1 | Atelectasis |
| 3 | RIB + RML + MBR | Primary repair + middle lobectomy | Double lumen | 2 | - |
| 4 | LMB + LUL | Primary repair + sleeve upper lobectomy | Double lumen | 2 | Atelectasis |
| 5 | MBR + LMB | Primary repair + anastomosis | Single lumen | 4 | Atelectasis + LLN paralysis |
| 6 | RMB + LMB | Primary repair + anastomosis | Double lumen | 3 | - |
| 7 | LMB + LUL + MBR | Primary repair + anastomosis + mobilization of aortic arch | Double lumen | 12 | Atelectasis |
RMB right main bronchus, RUL right upper lobe bronchus, RIB right intermedius bronchus, RML right middle lobe, MBR memberanous bronchial rupture, LMB left main bronchus, LUL left upper lobe bronchus, SSLL superior segment lower lobe, LLN left laryngeal nerve
Data collected included the age, sex, cause of the thoracic trauma, clinical presentation, operative findings, management, and outcome. Data was analyzed and was compared with that of the literature.
Results
Twenty-one patients were found to have bronchial injuries. Twenty of them (95.2%) had motor vehicle accidents (MVA), while one patient had a direct blow to the chest (4.8%). Age of patients ranged from 2½ to 49 years. Fourteen patients had “simple” bronchial injuries, i.e., short bronchial lesions located within 2.5–3 cm from the carina on the left and within 1 cm from the carina on the right side. Seven patients out of those twenty-one (33.3%) were found to have complex bronchial injuries and were included in this study. Six patients of the seven were involved in MVA, and one had a direct blow. Regarding those seven patients, three had rupture in the right bronchial tree (42.9%), three had rupture in the left bronchial tree (42.9%), and one had bilateral, right and left, main bronchial injury (14.2%).
All the seven patients presented with respiratory distress on admission and required endotracheal intubation and mechanical ventilation. Dyspnea, subcutaneous emphysema, and mediastinal emphysema were the most common findings in these patients. Six patients out of the seven (85.7%) had pneumothorax on admission that was associated with persistent air leak following tube thoracostomy. Six patients (85.7%) had fractures of upper ribs; one had clavicular fracture (14.2%).
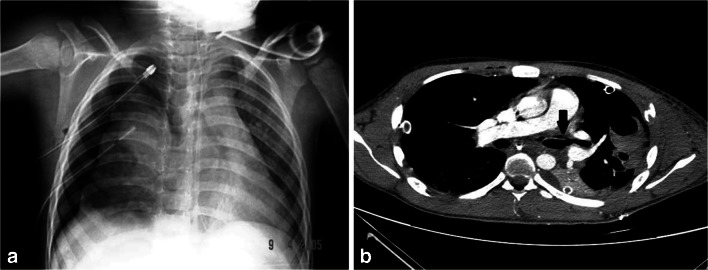
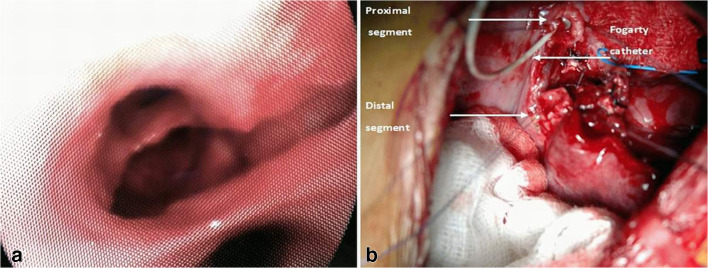
Chest X-ray (CXR) was done as the initial radiological investigation for all patients (Fig.1a). While an urgent computed chest tomography (CT-Chest) was performed in 3 patients, it did not provide any more information, except for the presence of associated lung contusion, massive pneumothorax, and surgical emphysema (Fig. 1b). Fiberoptic bronchoscopy was carried out in all patients and was diagnostic. Six patients had an urgent surgical procedure (within 2 h from the injury), and one had surgery 48 h after injury, due to delayed diagnosis (Fig. 2a). All of the seven patients required mechanical ventilation support following the surgery that ranged between 1 and 14 days (5.43 ± 5.28).
Fig. 1.
a Plain chest X-ray showing right-sided persistent pneumothorax with two inserted intercostal drains. b CT-Chest (mediastinal window) showing irregularity of the left upper lobe bronchus wall with two intercostal drains inserted in the left side and one intercostal drain inserted in the right side
Fig. 2.
a Pre-operative fibreoptic bronchoscopy showing intermedius and middle lobe bronchus rupture. b Intra-operative view: showing both the right main bronchus proximally with the Fogarty catheter introduced inside and the intermedius bronchus distally after sleeve upper lobectomy
The different types of the encountered complex bronchial injuries are listed in Table 1. Follow-up bronchoscopy was performed in all patients 2 months following the surgery and showed good results, with no stenosis or scar formations. Moreover, clinical follow-up for 5 years showed no complications in any of them. No perioperative mortality was recorded. The recorded postoperative complications were pulmonary atelectasis that required bronchoscopy for aspiration of secretions (n = 3), left recurrent laryngeal nerve paralysis (n = 1), and tracheostomy (n = 1).
Discussion
Complex bronchial ruptures due to blunt trauma are rare serious injuries, with a reported mortality up to 30% [2, 4]. Around 80% of the bronchial injuries due to blunt trauma are located within 2.5 cm of the carina [4]. Symbas et al. [5] have divided them into three types: transverse, longitudinal, and complex. Complex injuries were either combined transverse and longitudinal injuries or multiple ruptures. In their study, the complex injuries accounted for 8% of all airway injuries. However, in our study, their incidence was around 33.3%. On review of the literature, only few sporadic cases of complex bronchial injuries have been reported [3, 5].
Bronchial injuries are more common on the right side. The transverse bronchial ruptures are more frequent than longitudinal injuries. However, the longitudinal injuries are usually combined with the transverse ones [5]. Deslauriers et al. [6] noted that the bronchial rupture may be associated with a deep lobar lung laceration. This was encountered in four of our patients.
Bronchial rupture may be diagnosed immediately in 25–60% of patients. The left-sided bronchial ruptures usually take longer time to be diagnosed, as explained by Taskinen et al. [2]. The usual clinical presentation of bronchial ruptures includes dyspnea (90%), subcutaneous and mediastinal emphysema (65%), pneumothorax (66%), and less frequently hemoptysis [2, 5, 6]. A diagnosis of bronchial rupture should be considered in all patients with thoracic trauma, especially when there is mediastinal emphysema or continuous air leak. The CXR usually demonstrates pneumothorax, pneumomediastinum, or subcutaneous emphysema (90%) [1, 2, 6]. The fallen lung sign is specific for bronchial rupture [6]. The routine use of CT-Chest in blunt trauma is controversial, although its accuracy in detection of the site of injury reaches 94% especially with the use of the multi-detector computed tomogram (MDCT) [7]. Bronchoscopy is important to establish the diagnosis and to evaluate the extent of injury. It should be performed inside the operating room with a full anesthetic backup, so that endotracheal tube can be passed distally to the rupture site, or the lung can be isolated with a double lumen.
The patients included in this study presented with severe dyspnea that mandated endotracheal intubation. All had moderate to mild surgical emphysema. CXR was performed for all patients as initial screening and revealed subcutaneous emphysema and massive pneumothorax, either on the right or the left side. CT-Chest was performed for 3 patients after endotracheal intubation. We depend mainly on bronchoscopy for the diagnosis and evaluation of such bronchial injuries, as it can accurately delineate the site and extent of the lesion. Moreover, this policy avoids losing time taken for performing CT-Chest, as these patients usually have severe air leak with border line oxygen saturation. Furthermore, CT-Chest do not add any further details, except for associated small pulmonary contusions.
Complex bronchial ruptures should be diagnosed and treated early to prevent complications like airway stenosis, respiratory infection, and bronchiectasis. Immediate management is directed to securing the airway. Endotracheal tube can be placed into the uninjured bronchus providing single lung ventilation. However, it should be kept in mind that the tube can slip out of the bronchus during positioning of the patient, or may cause future narrowing by an over-inflated cuff in a relatively small bronchus. The double-lumen endotracheal tube is the best standard for isolation, but its large size and rigidity can cause further airway injury, especially when the rupture is located at carina or at a proximal bronchus [8]. This was seen in one of our patients.
Right thoracotomy approach is used for all injuries of the trachea, carina, and right main bronchus. It is also recommended for the repair of injuries involving the first 2–3 cm of the left main bronchus [5]. Left thoracotomy approach is indicated for the repair of all injuries of the left main bronchus [4, 5]. We do not recommend right thoracotomy for the repair of the proximal left main bronchus in a case of complex bronchial injury, as there is always lung contusion, and during dissection to access the site of the left bronchial rupture, the lung has to be compressed for long time, which may lead to ventilation problems and desaturation.
Regarding injuries of the left main bronchus that are close to the carina, the aortic arch can be mobilized and repair performed. The surgeon should be ready to manage the airway once the mediastinum is entered, as the ventilation may be inadequate. A separate endotracheal tube (crossing the field) and manual ventilation using bag mask valve system or using another ventilator is necessary [9]. In the case of distal injury of the main bronchi, intra-operative Fogarty catheter can be introduced proximally into the main bronchus (Fig.2b), thus preventing the transient compression of the lumen during the surgical manipulation [10]. If oxygen saturation falls to a critical level, temporary clamping of the left or right pulmonary artery is indicated with the use of low tidal volume and low positive end-expiratory pressure (PEEP) [9, 10]. Extensive complex bilateral injuries, associated with difficulties in ventilation during the procedures, may be repaired using cardiopulmonary bypass (CPB) [5], although we did not use it in any of our patients. A successful repair requires sharp dissection, saving the vascular supply, especially at the proximal end, removing all devitalized tissues and performing precise anastomosis with minimal tension at the suture line. The anastomosis should be achieved with an absorbable vicryl 4-0 (Ethicon. Inc.) to avoid granuloma formation and should be re-enforced with a pleural flap. If the damage of pulmonary parenchyma or the bronchial injuries are extensive, then lung resection may be necessary [1]. In cases with lobar bronchial rupture and lung damage beyond the bronchial repair, primary repair of the bronchial rupture with sleeve lung resection should be tried. This was done in four (57%) of our cases, thus preserving most of the functioning lung parenchyma.
Follow-up for a period of 5 years revealed a favorable outcome without development of bronchial stenosis or granuloma formation. No mortality was recorded in our patients. This could be attributed to the rapid transfer of the patients from the scene of the accident to the hospital and rapid management without full radiological investigations in such risky patients.
Conclusion
In conclusion, complex bronchial injuries are rare. The definitive diagnosis of these injuries can be made by bronchoscopy. Surgery for reconstruction of such injuries can be challenging and requires an experienced surgeon, who is familiar with the lung-sparing surgical techniques and airway repair. The ipsilateral postero-lateral thoracotomy is the incision of choice for the repair of such injuries, with as limited as possible lung resection.
Funding
None
Availability of data and material
Non-applicable.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of Human and animal rights Ethical approval
was waived by the Research Ethics Committee at the Chest Diseases Hospital, Kuwait in view of the retrospective nature of the study and all the procedures being performed were part of the routine care.
Ethics approval
Study was approved by the research ethical committee.
Consent for publication
The authors affirm that human research participants provided informed consent for publication of the images.
Footnotes
Meeting Presentation
The preliminary work was presented as an oral presentation at the annual meeting of the World Society of Cardiovascular and Thoracic Surgery (WSCTS2015) that was held at Edinburgh, Scotland, during 19–22 September 2015. The abstract including the preliminary work was published on-line by the Journal of Cardiovascular Surgery under the title (Management of Complex Bronchial Ruptures in Blunt Trauma).
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Schneider T, Volz K, Dienemann H, Hoffmann H. Incidence and treatment modalities of tracheobronchial injuries in Germany. Interact Cardiovasc Thorac Surg. 2009;8:571–576. doi: 10.1510/icvts.2008.196790. [DOI] [PubMed] [Google Scholar]
- 2.Taskinen SO, Salo JA, Halttunen PE, Sovijärvi AR. Tracheobronchial rupture due to blunt chest trauma: a follow-up study. Ann Thorac Surg. 1989;48:846–849. doi: 10.1016/0003-4975(89)90683-8. [DOI] [PubMed] [Google Scholar]
- 3.Wandling MW, Hoel AW, Meyerson SL, et al. Complex intrathoracic tracheal injury. Am J Respir Crit Care Med. 2015;192:e20–1. [DOI] [PMC free article] [PubMed]
- 4.Rossbach MM, Johnson SB, Gomez MA, Sako EY, Miller OL, Calhoon JH. Management of major tracheobronchial injuries: a 28-year experience. Ann Thorac Surg. 1998;65:182–186. doi: 10.1016/S0003-4975(97)01001-1. [DOI] [PubMed] [Google Scholar]
- 5.Symbas PN, Justicz AG, Ricketts RR. Rupture of the airways from blunt trauma: treatment of complex injuries. Ann Thorac Surg. 1992;54:177–183. doi: 10.1016/0003-4975(92)91177-B. [DOI] [PubMed] [Google Scholar]
- 6.Deslauriers J, Beaulieu M, Archambault G, LaForge J, Bernier R. Diagnosis and long-term follow-up of major bronchial disruptions due to nonpenetrating trauma. Ann Thorac Surg. 1982;33:32–39. doi: 10.1016/S0003-4975(10)63195-5. [DOI] [PubMed] [Google Scholar]
- 7.Scaglione M, Romano S, Pinto A, Sparano A, Scialpi M, Rotondo A. Acute tracheobronchial injuries: impact of imaging on diagnosis and management implications. Eur J Radiol. 2006;59:336–343. doi: 10.1016/j.ejrad.2006.04.026. [DOI] [PubMed] [Google Scholar]
- 8.Conti M, Pougeoise M, Wurtz A, Porte H, Fourrier F, Ramon P, Marquette CH. Management of postintubation tracheobronchial ruptures. Chest. 2006;130:412–418. doi: 10.1378/chest.130.2.412. [DOI] [PubMed] [Google Scholar]
- 9.Gwely NN. Blunt traumatic bronchial rupture in patients younger than 18 years. Asian Cardiovasc Thorac Ann. 2009;17:598–603. doi: 10.1177/0218492309349067. [DOI] [PubMed] [Google Scholar]
- 10.Jamal-Eddine H, Ayed AK, Perić M, Ben-Nakih ME. Injuries to the major airway after blunt thoracic trauma in children: review of 2 cases. J Pediatr Surg. 2007;42:719–721. doi: 10.1016/j.jpedsurg.2006.12.043. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Non-applicable.