Abstract
In the United States (US), immigrants constitute a considerable and growing proportion of the general population. Compared to the US-born, immigrants have differential health risks, and it is unclear if environmental exposures contribute. In this work, we estimated disparities between immigrants and the US-born in fine particulate matter (PM2.5) exposure and attributable premature mortality, including by region of origin and time since immigration. With PM2.5 estimates from a validated model at ~1 km2 spatial resolution and residential Census tract population data, we calculated the annual area-weighted average PM2.5 exposure for immigrants overall, the US-born, and immigrants separately by geographic region of origin and time since immigration. We then calculated the premature mortality attributed to PM2.5 for each population group, assessing disparities by immigrant status in PM2.5 exposures and attributable premature mortality for the US as a whole, and to assess spatial heterogeneity, in each US county. Overall, immigrants were exposed to slightly higher PM2.5 (0.36 μg/m3, 3.8%) than the US-born. This exposure difference translates to 2.11 more premature deaths attributable to PM2.5 per 100,000 in population for immigrants compared to the US-born in 2010. Immigrant – US-born disparities in PM2.5 and attributable premature mortality were more severe among immigrants originating from Asia, Africa, and Latin America than those from Europe, Oceania, and North America. Disparities between immigrant groups by time since immigration were comparatively small. Sensitivity analyses using 2000 data and a non-linear set of PM2.5 attributable mortality coefficients identified similar patterns. Our findings suggest that environmental exposure disparities, such as in PM2.5, may contribute to immigrant health disparities in the US.
Keywords: Air pollution, Health disparity, Immigrant health, PM2.5, Environmental justice
1. Introduction
Fine particulate air pollution, or particulate matter 2.5 μm or less in aerodynamic diameter (PM2.5), is a well-established environmental exposure associated with health detriments (Brook et al., 2010; Cohen et al., 2017). Prior research in clinical and experimental settings found that PM2.5 evokes detrimental bodily responses such as vascular dysfunction, heart arrhythmia, inflammatory cytokine release, impaired glucose metabolism, and neurohormonal imbalance (Franklin et al., 2015; Zhang et al., 2020). Long-term, yearly-averaged exposure to PM2.5 has been linked to increased risk for cardiovascular disease (Hayes et al., 2019), respiratory disorders (Pun et al., 2017), premature mortality (Di et al., 2017), and type 2 diabetes (Yang et al., 2020), among other adverse health endpoints (Ritz et al., 2019). Globally, PM2.5 ranks as the fifth highest contributor to mortality, with an estimated 4.2 million (95% confidence interval (CI): 3.7, 4.8 million) deaths in 2015 (Cohen et al., 2017). In the United States (US), an estimated 100,000 to 200,000 premature deaths per year are attributable to PM2.5 exposure (Fann et al., 2018).
Despite its importance as an exposure with high public health burden, little is known regarding disparities in PM2.5 exposure between immigrants and the US-born, and amongst immigrants. In the US, immigrants (i.e. foreign-born) exhibit different health risks compared to the US-born and amongst themselves depending on factors such as country of origin (Dupre et al., 2012; Mehta et al., 2016). For instance, while immigrants overall have been shown to have longer life expectancy than the US-born, immigrants from Asia exhibited lower life expectancy than Asians born in the US (Singh and Miller, 2004). Moreover, cause-specific mortality risks vary when comparing immigrants and the US-born with lower mortality risks from cardiovascular disease, but higher risks from some cancers for immigrants (Singh and Siahpush, 2001). Furthermore, within some racial/ethnic groups (e.g. East Asian) risks for morbidities such as hypertension, obesity, and diabetes are higher when comparing immigrants to their US-born counterparts (Horlyck-Romanovsky et al., 2019; Singh et al., 2013). Differences in health risks between immigrants and the US-born could be affected by variation in diet, linguistic and cultural barriers, and health care as a higher proportion of immigrants are without health insurance compared to the US-born (Arandia et al., 2012; Eamranond and Hu, 2008; Singh and Miller, 2004). Initial research in other countries such as Canada found that immigrants had higher PM2.5 exposures and were at higher risks for cardiovascular mortality attributable to PM2.5 exposure compared to the Canada-born (Erickson et al., 2020).
Evaluating environmental exposures of immigrants and the US-born, and among immigrants by region of origin or time since immigration, can help us gauge the impact of the environment on immigrant health disparities. Currently around 44 million people, or 14% of the total population, in the US are immigrants (Passel and Cohn, 2008; Vespa et al., 2018). This figure is expected to rise to 69 million, or 17% of the total population, by 2060 (Vespa et al., 2018). The extent to which environmental exposures such as PM2.5 contribute to health disparities between immigrants and the US-born, and among immigrants, is not well understood (Eamranond and Hu, 2008). Compared to other health determinants such as socioeconomic status, environmental exposures and their health effects comprise an understudied area. A better understanding of PM2.5 exposure disparities can lead to insights on how to reduce the health burden of PM2.5 on vulnerable immigrant population subgroups.
To address this research gap, we explore annual average PM2.5 exposure disparities between immigrants and the US-born. Among immigrants, we further calculate disparities by region of origin and time since immigration. To gauge the implications of PM2.5 exposure disparities, we conduct a health impact analysis and estimate the number of premature deaths attributable to PM2.5 in immigrants and the US-born.
2. Materials and Methods
2.1. PM2.5 Exposure Disparity by Immigrant Status
PM2.5 ambient monitoring networks do not provide the spatial coverage necessary to estimate exposure at all locations in the study area of the contiguous US. Therefore, we used monthly modelled estimates at 0.01° x 0.01° resolution, equivalent to around 1 km2 (van Donkelaar et al., 2019). These PM2.5 exposure surfaces were generated using geographically weighted regression with inputs from satellite observations of aerosol optical depth (AOD), PM2.5 composition estimates from a chemical transport model (GEOS-Chem), and ground-level observations from monitoring networks. Over its prediction period across North America, the PM2.5 estimation model achieved a cross-validation R2 of 0.70 for annual PM2.5 mass concentrations, indicating high prediction accuracy. There were spatial differences in PM2.5 model performance; its prediction accuracy, when compared to ground-level monitoring, was highest in the midwestern US, followed by the southwest, northeast, south, and northwest. In general, areas with higher PM2.5 had higher prediction accuracy. We estimated annual PM2.5 averages in 2010 for 72,539 contiguous US Census tracts via area weighting of gridded estimates.
We then calculated PM2.5 exposure by immigrant status using data from the decennial 2010 US Census (U.S. Census Bureau, 2019). The decennial Census has the most complete coverage of the US residential population and has lower sampling error compared to the American Community Survey (U.S. Census Bureau, 2018). We retrieved counts of the number of residents who were immigrants (i.e. foreign-born) and US-born for each of 72,539 Census tracts. Of these areas, 642 reported zero total population and an additional 2,533 had zero immigrant residents. Within the immigrant population, we collected data on resident counts by immigrants’ region of origin: Africa, Asia, Europe, Latin America, North America, and Oceania (Supplementary Material: Table S1). We additionally retrieved immigrant resident counts by time since immigration (< 10 years, 10 to 20 years, 20 to 30 years, and ≥ 30 years). Lastly, we assigned each Census tract resident to the corresponding Census tract average PM2.5 exposure estimate. With this data set, we calculated average yearly PM2.5 exposure by immigrant status (immigrant or US-born), immigrants by region of origin, and immigrants by time since immigration subgroups. Furthermore, we calculated the exposure disparity by immigrant status, estimating the difference in yearly average PM2.5 exposure between an immigrant and US-born resident at the national scale while accounting for overall PM2.5 prediction error. To evaluate possible spatial heterogeneity, we repeated these calculations of exposure disparities at the US county scale. We also generated annual estimates and corresponding US Census tract averages for 2000 for sensitivity analysis.
2.2. Estimating Premature Mortality Attributable to PM2.5
To assess the health burden associated with the PM2.5 exposure disparities between immigrants and the US-born, and among immigrants by region of origin, we applied a health impact function (Fann et al., 2018; Hubbell et al., 2009). For each population group, we estimated the number of premature deaths attributable to PM2.5 exposure in 2010 (and 2000 for sensitivity analysis) using the following formula:
| [1] |
where yijk is the total number of premature deaths in year i (i.e. 2000 or 2010), in Census tract j, of population group k (i.e. immigrants, US-born, immigrants from a specific region of origin, or immigrants of a certain time since immigration); m0 represents the baseline mortality rate in year i for group k; β is the mortality risk coefficient linking PM2.5 to mortality; Cij is the average yearly PM2.5 mass concentration for year i and tract j; and Pijk is the population count in year i for tract j and group k.
We obtained baseline yearly mortality rates (m0) from the US Census of Disease Control and Prevention (CDC) (Centers for Disease Control and Prevention, 2020). Mortality rates by immigrant status, and more specifically by region of origin or time since immigration were not available; we therefore retrieved adult (≥ 30 years old) mortality rates for the general population. Moreover, as data were not available at a spatial resolution as fine as Census tracts, we retrieved county-level rates and applied them to matching Census tracts using area-weighted averaging. Area-weighting is accomplished by computing the weighted mean of every PM2.5 estimate pixel overlapping a predefined Census tract based on the % overlap each pixel has with the Census tract. To account for temporal variability in mortality rates, we used yearly mortality rates for three-year periods around the year of interest (i.e. 2009-2011 for year 2010). Further details on these parameters are given in Supplementary Material: Equation S1.
The mortality risk coefficient (β) was based on results from a re-analysis study of the long-term effects of PM2.5 exposure in the American Cancer Society Cancer Prevention Study II cohort (Krewski et al., 2009). That study, which tracked a large national cohort of over 360,000 participants with over 12 years of follow-up, estimated a hazard ratio of 1.06 (95% CI: 1.04, 1.08) per 10 μg/m3 increase in annual average exposure to PM2.5. We derived the mortality risk coefficient from this study since it used a population representative of US demographics and has been used in other health impact analyses (Fann et al., 2017; Thind et al., 2019), allowing us to compare our results to existing literature. As a sensitivity analysis, we applied a set of mortality coefficients allowing for non-linearity in the PM2.5 concentration and attributable premature mortality relationship (Nasari et al., 2016; Pope et al., 2019).
We determined population counts (P) of residents in each group (immigrant, US born, immigrant group by region of origin) residing in each Census tract by year (from the US Census (U.S. Census Bureau, 2019). For each Census tract, we ascertained the number of US-born, total immigrants, immigrants from each of the regions of origin (Africa, Asia, Europe, Latin America, North America, and Oceania, and immigrants by time since immigration (< 10 years, 10 to 20 years, 20 to 30 years, and ≥ 30 years). Some Census tracts had no residents who were immigrants.
Finally, we summated the total number of estimated premature deaths associated with PM2.5 exposure in each year (2010, 2000 for sensitivity analysis) for each population group in all Census tracts nationally or by county to assess spatial heterogeneity:
| [2] |
We performed all analysis with the statistical programming language R (R Core Team, 2020). We evaluated statistical significance at an alpha level of 0.05; we used weighted two-sided t-tests to compare averages of two groups.
3. Results
3.1. PM2.5 Exposure of Population Groups
Overall, immigrants had slightly higher average annual PM2.5 exposure than the US-born at the national level. Table 1 summarizes the population and average annual PM2.5 exposure of US residents by immigrant status. On average, immigrants were exposed to annual average PM2.5 levels 0.36 (2.5th and 97.5th percentile: 0.19, 0.53) μg/m3 higher compared to the US-born. With respect to immigrants from different regions of origin, those originating from Asia, Africa, and Latin America had higher annual average exposures than those from Europe, Oceania, and North America. Differences in average PM2.5 exposure were smaller between immigrants by time since immigration than by region of origin; those who immigrated 20 to 30 years prior to 2010 had the highest exposure, followed by 10 to 20 years, < 10 years, and ≥ 30 years. Table S3 tested for statistically significant differences between average PM2.5 exposures between population subgroups. Most of the comparisons between population subgroups by region of origin were statistically significant while only immigrants who immigrated ≥ 30 years prior to 2010 had statistically lower exposure compared to those who immigrated 20 to 30 years prior to 2010.
Table 1:
Average Fine Particulate Air Pollution (PM2.5) Exposure for Those Born in the United States (US), Immigrants overall, Immigrants by Region of Origin, and by Time since Immigration in 2010. Values in parentheses indicate the 2.5th and 97.5th percentiles.
| Population (in millions) | Average PM2.5 (μg/m3) Exposure | |
|---|---|---|
| Total | 301.94 | 9.57 (5.39, 13.41) |
| US-born | 263.55 | 9.52 (5.28, 13.32) |
| Immigrants overall | 38.39 | 9.88 (6.10, 13.75) |
| by origin: | ||
| Africa | 1.46 | 9.99 (6.40, 13.40) |
| Asia | 10.54 | 10.02 (6.10, 13.80) |
| Europe | 4.83 | 9.49 (5.77, 13.24) |
| Latin America | 20.54 | 9.95 (6.17, 13.80) |
| North America | 0.83 | 8.78 (4.88, 13.10) |
| Oceania | 0.19 | 9.15 (5.10, 13.42) |
| by time since immigration: | ||
| < 10 years | 11.61 | 9.85 (6.10, 13.70) |
| 10 to 20 years | 10.97 | 9.89 (6.10, 13.70) |
| 20 to 30 years | 7.63 | 10.01 (6.11, 13.80) |
| ≥ 30 years | 8.18 | 9.79 (5.91, 13.75) |
We observed spatial heterogeneity in county-level annual average PM2.5 exposure (Figure 1A). The county-level annual average PM2.5 exposure for the total general population was highest in southern California at 14.96 μg/m3 (Supplementary Material: Table S2). Overall, counties in eastern US had higher PM2.5 than those in the west, with the lowest county averages east of the Rocky Mountains.
Figure 1:
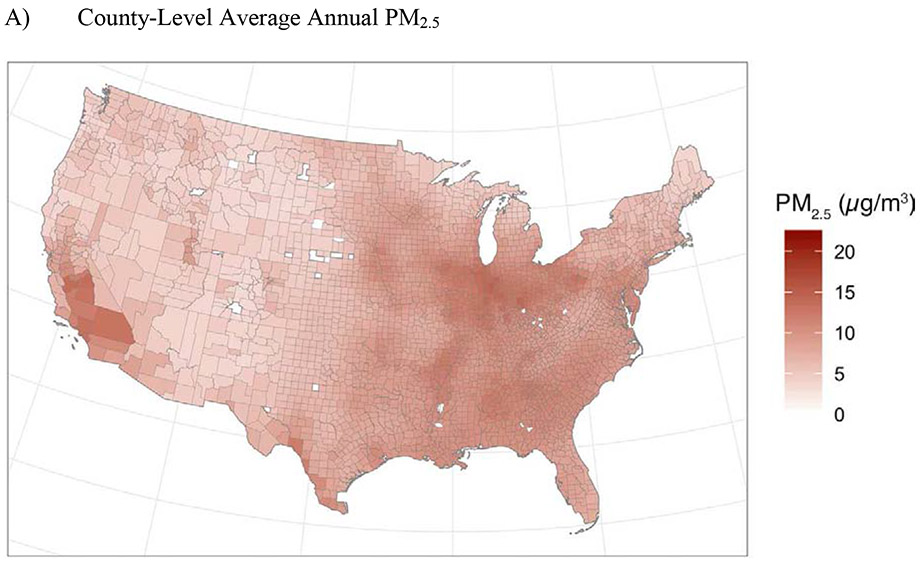
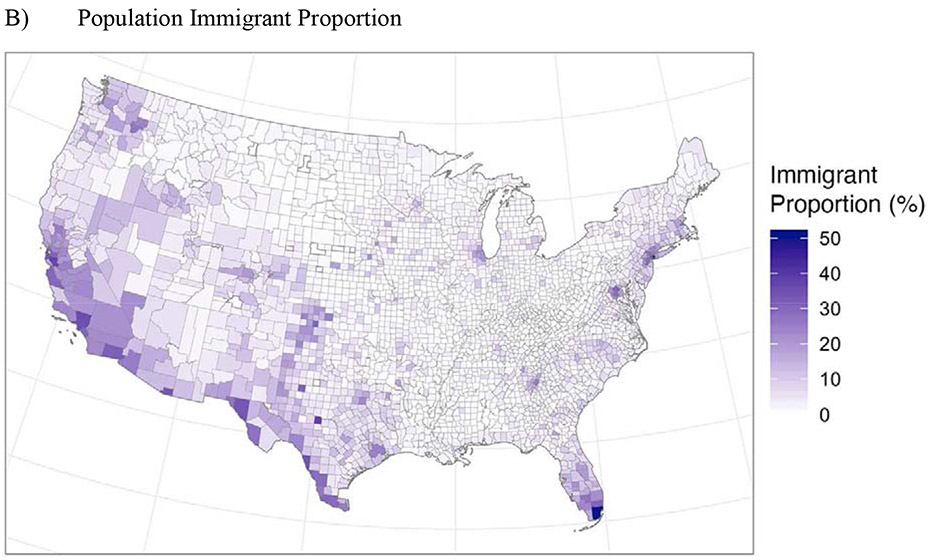
County-Level Average Annual PM2.5 and Population Immigrant Proportion (%) in United States Counties in 2010.
Note: Immigrant proportion refers to the percentage of the population that was not born in the US. Counties. Census tracts with zero immigrants were shaded in white.
3.2. Immigrant Proportion in General Population
On the national level, the proportion of the general population who were immigrants was 12.7% (Table 1). Of the 38.39 million immigrant residents in the US, the most populous group originated from Latin America (53.5% of total immigrant population), followed by Asia (27.5%).
We also observed spatial heterogeneity in the immigrant proportion by county (Figure 1B). Immigrant proportions by US counties were highest by the Californian coast, close to the US-Mexico border, and in Southern Florida. The percent of immigrants in each county ranged from 0.01% to 51.1% with an average of 4.34% and median of 2.39% (Supplementary Material: Table S2).
3.3. Disparity between Immigrants and US-born in Premature Deaths Attributable to PM2.5 Exposure
Table 2 summarizes the estimated number of premature deaths attributable to PM2.5 by population group for the US-born, immigrants to the US (overall), and immigrants by region of origin. In the general US population, we estimated 163,940 (2.5th and 97.5th percentiles: 31,140, 379,270) total deaths attributable to PM2.5 in 2010. We also calculated the number of premature deaths per 100,000 persons attributable to PM2.5 in each population group by immigrant status (US-born, immigrants overall, immigrants by region of origin, and immigrants by time since immigration). Based on higher exposures, immigrants overall had higher premature mortality attributable to PM2.5 than the US-born. In 2010, this immigrant – US-born disparity in premature mortality attributable to PM2.5 was 2.11 deaths per 100,000 in population.
Table 2:
Premature Deaths and Mortality Rate Attributable to Fine Particulate Air Pollution (PM2.5) for Those Born in the United States (US), Immigrants overall, Immigrants by Region of Origin, and Time since Immigration. Values in parentheses indicate the 2.5th and 97.5th percentiles and are reflective of variation in PM2.5 exposure exclusive of other uncertainties such as those in model predictions of PM2.5.
| Total Premature Deaths in Thousands |
Premature Mortality per 100,000 |
|
|---|---|---|
| Total | 163.94 (31.14, 379.27) | 54.30 (10.31, 125.61) |
| US-born | 142.39 (26.14, 329.09) | 54.03 (9.92, 124.87) |
| Immigrants overall | 21.55 (4.97, 49.30) | 56.14 (12.96, 128.42) |
| by origin: | ||
| Africa | 0.83 (0.21, 1.84) | 56.78 (14.08, 125.49) |
| Asia | 6.00 (1.37, 13.58) | 56.95 (12.96, 128.84) |
| Europe | 2.60 (0.57, 5.99) | 53.83 (11.75, 124.16) |
| Latin America | 11.61 (2.71, 26.47) | 56.51 (13.21, 128.84) |
| North America | 0.41 (0.07, 1.02) | 49.74 (8.42, 122.99) |
| Oceania | 0.10 (0.02, 0.24) | 51.87 (9.24, 125.70) |
| by time since immigration: | ||
| < 10 years | 6.49 (1.50, 14.86) | 55.94 (12.96, 128.00) |
| 10 to 20 years | 6.17 (1.42, 14.05) | 56.21 (12.96, 128.00) |
| 20 to 30 years | 4.34 (0.99, 9.83) | 56.91 (13.01, 128.84) |
| ≥ 30 years | 4.55 (1.00, 10.51) | 55.59 (12.23, 128.42) |
Based on exposure differences among immigrants, those originating from Asia, Africa, and Latin America had the highest premature mortality attributable to PM2.5 (Table 2). Immigrants from Europe and Oceania had lower-than-average premature mortality attributable to PM2.5 and immigrants from North America had the lowest. By time since immigration, premature mortality attributable to PM2.5 were similar between groups, with those in the 20 to 30 years since immigration having the highest mortality burden. In sensitivity analyses that applied a set of non-linear PM2.5 concentration and premature mortality coefficients, the attributable premature mortality from PM2.5 estimates were smaller overall compared to the main analysis (Supplementary Material: Table S4). Differences between population groups in premature mortality attributable to PM2.5 were in the same direction but larger in magnitude. We present results with a constant parameter for the PM2.5 concentration and premature mortality relationship as they are more comparable with prior studies, and that the differences between population groups were more conservative.
We evaluated spatial heterogeneity of the overall immigrant vs. US-born disparities in premature mortality attributable to PM2.5 exposure. Figure 2 maps the county-level disparity between an immigrant group by region of origin and US-born in premature mortality attributable to PM2.5. A density plot shows a slight skew towards higher premature mortality attributable to PM2.5 among immigrants than in the US-born, which we identify as a positive immigrant – US-born premature mortality disparity. We found that there was a higher premature mortality attributable to PM2.5 for immigrants than the US-born in 58.9% of US counties. There was no clear geographic pattern for where counties with immigrant – US-born premature mortality disparity are located, although there are some areas in the US with clusters of immigrant – US-born premature mortality disparity (e.g. coastal California, southern Florida, and along the US-Mexico border). We visualized the error in the estimated premature mortality attributable to PM2.5 exposure, noting slightly higher errors in the western parts of the US (Supplementary Material: Figure S1). Figure 2 also visualizes the county-level immigrant proportion in the total general population, and shows whether or not a county is below or above the national median. We observed that the proportion of the population that is immigrants in a county was higher along the coasts and in the Southwest; most counties in the northern Midwest and in the inland areas of the eastern US had a county immigrant proportion lower than the median. We also identified counties at the extreme ends of premature mortality disparity attributable to PM2.5 and immigrant population proportion (Supplementary Material: Figure S2). Counties with high immigrant – US-born disparity and high immigrant population proportion (i.e. top 10% of each measure) were in northern Washington, southern California, and southeastern New York. Counties with lower immigrant – US-born disparity and low immigrant proportion (i.e. lowest 10% of each measure) were mostly scattered throughout the mid-eastern half of the US.
Figure 2:
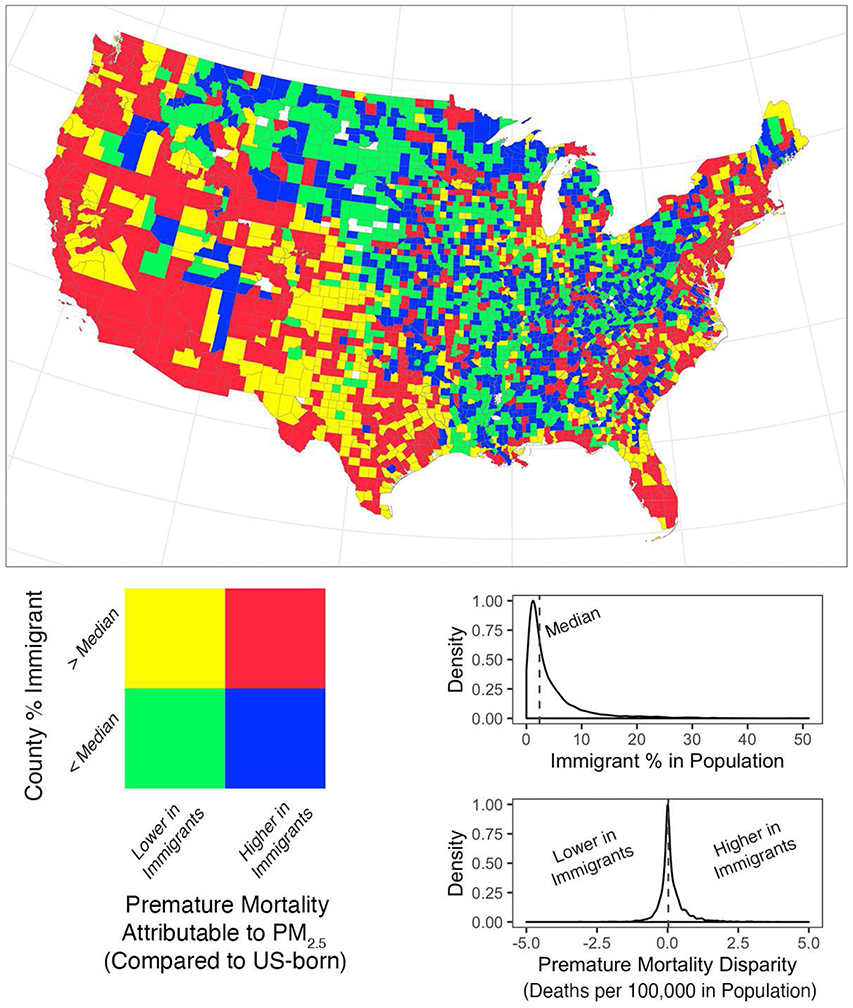
Disparity between Immigrants and the US-Born in Premature Mortality Attributable to PM2.5 Exposure in 2010. The coloring scheme indicates whether a county had higher or lower estimated premature deaths attributable to PM2.5 in immigrants compared to the US-born (positive or negative premature mortality disparity) and whether the county was in the upper or lower half of county immigrant population proportions nationally. Counties with any Census tracts with zero immigrants were shaded in white. Density plots for each measure with its median value (dotted line) are also shown.
We also investigated the disparities in PM2.5-attributable premature mortality among immigrants from specific regions of origin and the US-born (Figure 3). For immigrants from some regions (i.e. Africa and Oceania), there were many counties for which no immigrants who originated from these regions resided. Thus, the immigrant – US-born disparity for these groups of immigrants, especially in central US, could not be calculated and are thus displayed as white in the maps. In the remaining counties with a non-zero number of immigrants from Africa or Oceania, the spatial pattern of immigrant – US-born disparities in premature mortality attributable to PM2.5 appears similar to that of the overall immigrant – US-born disparities (Figure 2). Comparing the spatial patterns for immigrants from Asia, Europe, Latin America, and North America, differences depending on region of origin are more apparent. The region of origin whose spatial pattern most resembles that of the overall immigrant population is Latin America, followed by Asia (Figure 3). This is expected since among immigrants, the most populous group comes from Latin America then Asia (Table 1). Counties along the northern US border had the highest percentages of immigrants from North America (i.e. Canada). Counties in New York and along the Northeast Corridor had the highest proportions of immigrants from Europe. Some inland counties of California had high immigrant proportion from Europe, North America, or Latin America and lower immigrant – US-born disparity, indicating a higher premature mortality burden from PM2.5 in the US-born than in the immigrant group.
Figure 3:
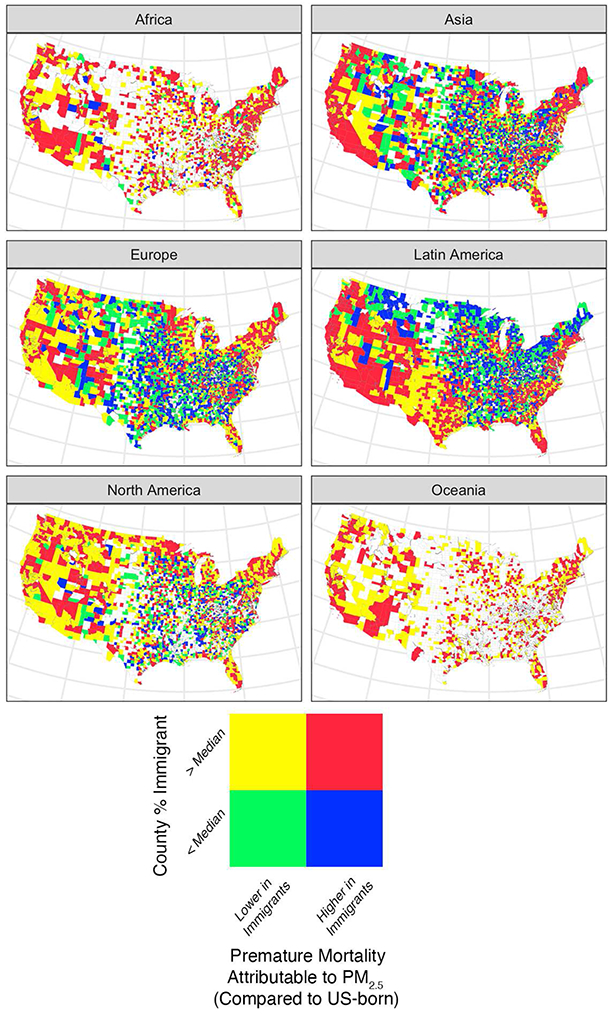
Disparity between Immigrants and the US-Born in Premature Mortality Attributable to PM2.5 Exposure by Immigrants’ Region of Origin in 2010. The coloring scheme indicates whether a county had higher or lower estimated premature deaths attributable to PM2.5 in immigrants of the specified region of origin compared to the US-born and whether the county was above or below the national median for county immigrant population from the specified region of origin proportions.
Finally, we explored disparities in PM2.5-attributable premature mortality among immigrants by times since immigration (Figure 4). The spatial pattern of immigrant – US-born disparities in premature mortality attributable to PM2.5 was similar to the overall immigrant – US-born map (Figure 2). There were some spatial differences in immigrant proportion by times since immigration. Recent (< 10 years) immigrants’ proportion of the total population were low in northern areas compared to the rest of the country. In contrast, the proportion of the total population for immigrants who immigrated ≥ 30 years prior to 2010 was high in northern areas compared to other parts of the country, relative to the immigrant proportion of the total population patterns for those with shorter times since immigration. In summary, spatial patterns in PM2.5 mortality disparities between immigrants and the US-born, when comparing immigrant groups with different times since immigration to the US-born were similar to spatial patterns comparing immigrants overall to the US-born. When comparing between immigrant subgroups by time since immigration, there were some minor differences in immigrant proportion of the total population when comparing the map for those who immigrated ≥ 30 years prior to 2010 to more recent immigrants.
Figure 4:
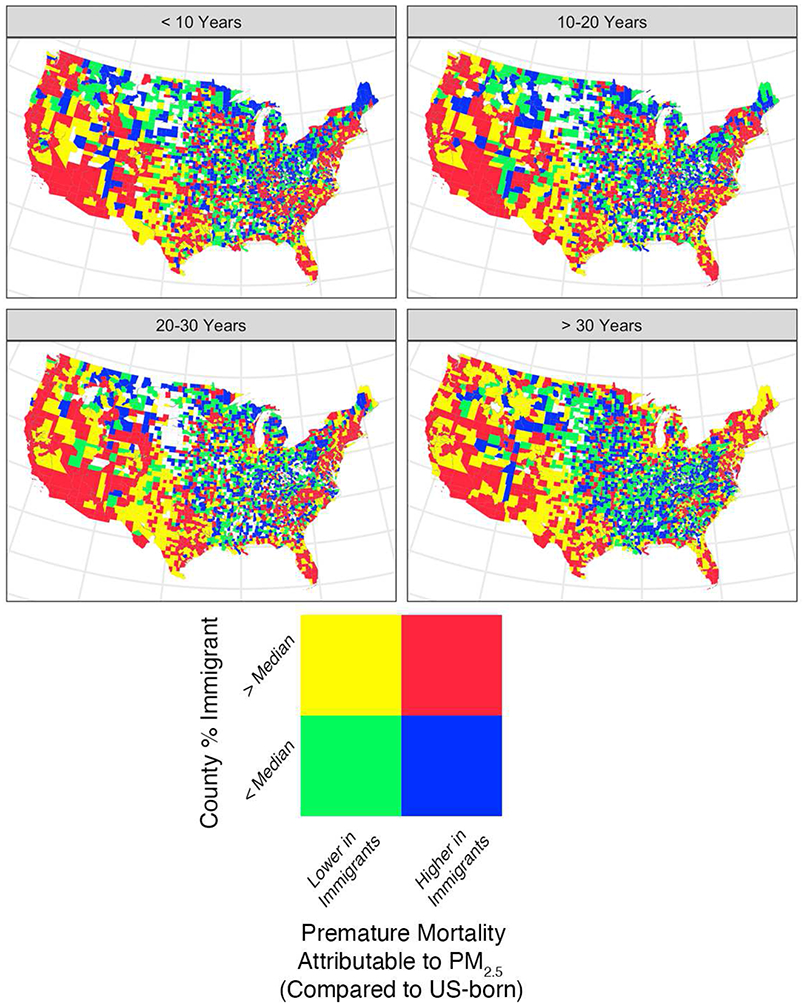
Disparity between Immigrants and the US-Born in Premature Mortality Attributable to PM2.5 Exposure by Immigrants’ Time since Immigration in 2010. The coloring scheme indicates whether a county had higher or lower estimated premature deaths attributable to PM2.5 in immigrants of certain time periods since immigration compared to the US-born and whether the county was above or below the national median for county immigrant population of a certain time since immigration proportions.
3.4. Sensitivity Analysis with 2000 Data
We repeated our analysis using 2000 data as sensitivity analysis. We found similar patterns of spatial heterogeneity in county-level annual average PM2.5 and immigrant proportion in total population (Supplementary Material: Figure S3). Overall, there were fewer immigrants living in the US in 2000 than in 2010 (Supplementary Material: Table S5). The US-born population outnumbered immigrants overall 8-to-1 in 2000 and just under 7-to-1 in 2010. The annual average PM2.5 was higher in 2000 than 2010. The immigrant – US-born disparity in average annual PM2.5 exposure was larger in 2000 at 1.25 μg/m3. Compared to 2010, county-specific average annual PM2.5 was higher while immigrant, overall and by region of origin, proportion in the total population was lower in 2000 (Supplementary Material: Table S8)
PM2.5 and attributable premature mortality disparities overall, by immigrants’ region of origin, by immigrants’ times since immigration, and their respective spatial patterns by county in 2000 were similar to those of 2010. As PM2.5 exposure disparities were larger in 2000, the overall immigrant – US-born disparity in premature mortality attributable to PM2.5 was also larger at 7.59 deaths per 100,000 in population. By region of origin, those who immigrated from Asia, Latin America, and Africa, as in 2010, had the highest PM2.5 exposure and premature mortality burden from PM2.5 in 2000 compared to immigrants from Europe, Oceania, and North America (Supplementary Material: Tables S5 and S6). In contrast to 2010, PM2.5 exposure and attributable premature mortality in 2000 were higher among immigrants from Europe or Oceania compared to the US-born (Supplementary Material: Tables S6 and S9). When comparing subgroups by time since immigration, those who immigrated 10 to 20 years prior to 2000 (20 to 30 years prior to 2010) had the highest PM2.5 exposure and attributable premature mortality. Although the differences between subgroups by times since immigration in PM2.5 exposure were larger in 2000, similar to 2010, those who had the longest time since immigration (≥ 30 years) were the least exposed followed by the most recent immigrants (< 10 years since immigration). Applying a set of non-linear PM2.5 and attributable premature mortality coefficients found, in contrast to 2010, larger premature mortality attributable to PM2.5 in the total population, US-born, and immigrants overall, compared to the main analysis (Supplementary Material: Tables S6 and S7). Similar to 2010 results, the differences in premature mortality attributable to PM2.5 between subgroups by immigrants’ region of origin or time since immigration were more conservative in the main analysis compared to the sensitivity analysis with non-linear premature mortality coefficients. Inspecting county-specific premature mortality disparities between immigrants and the US-born, or immigrants from specific regions of origin or of a specific time period since immigration and the US-born, the spatial patterns across the US were similar to those in 2010 (Supplementary Material: Figures S4 to S7). A slightly higher majority of US counties (60.0%) had a higher premature mortality burden attributable to PM2.5 for immigrants overall than the US-born in 2000 than in 2010.
4. Discussion
Using US Census data and air pollution modeling predictions, we found that PM2.5 exposures were 3.8% higher in immigrants to the US than the US-born. Consequently, premature mortality attributable to PM2.5 was estimated to be higher in immigrants compared to the US-born. Across the US, there was spatial heterogeneity in the immigrant – US-born disparity in PM2.5 exposure and its attributable premature mortality. Furthermore, there were differences in disparities depending on the immigrants’ region of origin.
Higher PM2.5 exposures and attributable premature mortality in immigrants overall compared to the US-born, and in immigrants originating in some world regions compared to others, may be explained by differences in immigrant settlement patterns and socioeconomic status (SES). Historically, immigrants to the US settle in more urban areas, usually in select gateway cities (Hempstead, 2007). Immigrant settlement patterns show a preference for existing immigrant communities, where there may be existing family and cultural ties (National Academies of Sciences, 2015). As urban areas tend to have higher PM2.5 levels compared to rural areas, immigrant settlement preferences may explain the immigrant – US-born disparity in PM2.5 exposure. SES differences between immigrants and the US-born, and among immigrant groups, may influence some immigrants’ residence in areas with higher PM2.5, and may contribute to other disparities, although other factors could also play a role. On average, immigrants had lower household income compared to the US-born (Singh and Hiatt, 2006). Among immigrant groups by region of origin, those from Latin America had lower SES compared to those from other regions (National Academies of Sciences, 2015). Prior research found that metropolitan areas with lower costs of living had the largest increases in immigrants from 1990 to 2000 (Baird et al., 2008). Since areas with lower SES had higher levels of PM2.5 (Hajat et al., 2015), links between immigration migration and SES likely contribute to our finding of higher PM2.5 exposures and premature mortality burden in immigrants overall compared to the US-born, and in some immigrant groups (i.e. from Latin America) compared to others (i.e. Europe).
To our knowledge, no study to date has investigated air pollution exposure disparities between immigrants and the US-born on the national scale. Existing research on environmental exposures and immigrants has been in occupational settings (Gany et al., 2017; Moyce and Schenker, 2017; Pappalardo and Mosnaim, 2018). These studies are limited in informing PM2.5 exposure disparities by foreign-born status in the general population. Questionnaire-based studies have assessed immigrants’ perception of air pollution. Hispanic immigrants interviewed in Spanish expressed lower concern for air pollution as a health concern compared to those interviewed in English (Johnson, 2011). On the other hand, residents of a neighborhood with predominantly Chinese immigrant population in Boston expressed high concern for health effects from traffic exhaust exposure (Brugge et al., 2000). These questionnaire-based studies did not quantify PM2.5 exposure disparities between immigrants and the US-born.
A study using Census data and modeled air pollution, similar to our study, found that in 2006, immigrants to Canada were exposed to 1.55 μg/m3 higher PM2.5 than the Canada-born (Pinault et al., 2017). The magnitude of this exposure disparity in Canada is larger than the overall national disparity we found between immigrants and the US-born (Table 1).
We can also draw comparisons to prior US-based studies that investigated PM2.5 exposure disparities by race/ethnicity, although not by immigrant status. A recent study using Census data found that average annual PM2.5 exposures between 1990 and 2010 were highest for non-Hispanic African Americans, followed by Asians and Hispanics (Woo et al., 2019). These disparities by race/ethnicity were estimated to be between 1 to 2 μg/m3 in PM2.5, which are similar to the magnitude of PM2.5 exposure disparities by immigrant status in our study. Other studies using cohort and administrative data also documented racial/ethnic differences in exposure to air pollution, with higher exposure for minorities compared to whites (Parker et al., 2018). Although results from these prior studies cannot be directly compared to those in this study, almost all immigrants from Asia, Africa, and Latin America are racial/ethnic minorities in the US while the majority of immigrants from Europe, North America, and Oceania are white. In this way, our finding of higher PM2.5 exposures in immigrants overall compared to the US-born, and higher exposures in immigrants from Asia, Africa, and Latin America compared to those from Europe, North America, and Oceania are consistent with results from prior studies on exposure disparities by race/ethnicity.
We did not find convincing evidence of differences in PM2.5 exposure and attributable premature mortality by time since immigration (Tables 1 and 2). Although the immigrant subgroup with the longest time since immigration (≥ 30 years) was the least exposed to PM2.5 in both 2010 and 2000, there was no clear pattern of increased or decreased exposures by time since immigration. We are not aware of existing studies that evaluated PM2.5 exposure differences by immigrant time since immigration, which limits our ability to compare our results to prior work.
Our estimates of premature deaths attributable to PM2.5 are similar with those from recent studies. In the total US population, we estimated 163,940 (2.5th and 97.5th percentiles: 31,140, 379,270) premature deaths attributable to PM2.5 in 2010 (Table 1). An US EPA study that employed a similar methodology but with a different set of PM2.5 data estimated 120,000 (95% CI: 83,000, 160,000) premature deaths from PM2.5 in 2010 (Fann et al., 2017). Other recent studies employing a health impact analysis approach on other years between 2005 and 2014 also estimated a similar number of premature deaths attributable to PM2.5., with lower estimates in later years (Fann et al., 2018; Thind et al., 2019).
Consistent with the lack of studies on immigrant – US-born disparities in PM2.5 exposure, we are unaware of a national analysis on immigrant – US-born disparities in premature mortality attributable to PM2.5. Regarding disparities in air pollution-related mortality between immigrants and the US-born, one study found that, in 2005, high Latino immigrant population and economic deprivation was the strongest predictor of a Census tract being a spatial cluster of high lifetime cancer risk from air toxic exposures (Lievanos, 2015). Absent previous estimates of the disparities between immigrants and the US-born in premature mortality attributable to PM2.5, we make comparisons to disparities by other demographic factors and to premature mortality attributable to other causes. When estimating premature deaths attributable to PM2.5 generated from electricity generation in 2014, researchers found disparities by race/ethnicity with African Americans having the highest mortality burden followed by whites, Asians, then Latinos (Thind et al., 2019). The disparity between African Americans and Latinos, the racial/ethnic groups with the largest disparity, was about 3.0 deaths per 100,000 population. This is almost 0.9 larger than the disparity between immigrants and the US-born, which in 2010 was 2.11 deaths per 100,000 population. To put our estimates into perspective with other causes of premature mortality, we note that the overall disparity between immigrants and the US-born in premature mortality attributable to PM2.5 was around one-fifth of premature mortality attributable to motor vehicle accidents, which was 11.3 deaths per 100,000 population (2010), or to drug poisonings, which was 12.3 deaths per 100,000 population (2010) (Johnson et al., 2014).
Our study had limitations. For PM2.5 exposure assessment and calculation of disparities by immigrant status, we relied on US Census data with estimated counts of each population group in each Census tract. Exposure assessment based on residential Census tract might not accurately represent each person’s annual average PM2.5 exposure due to PM2.5 prediction model error, mobility patterns away from place of residence, and possible misreporting of immigrant population counts. Additionally, the Census data do not differentiate between documented and undocumented immigrants, and it was likely that those who were undocumented were not counted. Despite these limitations, Census data represent the largest source of residential information of US residents by immigrant status (U.S. Census Bureau, 2018). Furthermore, we expect that possible errors from our PM2.5 exposure assessment and calculations of disparities are non-differential and random, although future research could investigate this issue. Moving to our calculation of premature mortality attributable to PM2.5, we were limited by the unavailability of population subgroup specific mortality rates. Ideally, we would employ a different baseline mortality rate specific to the US-born, immigrants overall, and immigrant subgroups by region of origin or time since immigration. If baseline mortality rates were higher in immigrants compared to the US-born overall, we would have found larger immigrant – US-born disparities in premature mortality attributable to PM2.5. The all-cause mortality risk coefficient is another component of our calculations that could potentially differ by population subgroups. Our main analysis based this coefficient on a hazard ratio of 1.06 (95% CI: 1.04, 1.08) per 10 μg/m3 in PM2.5 (Krewski et al., 2009), which is commonly used in other recent health impact analyses on premature mortality attributable to PM2.5 (Fann et al., 2018; Fann et al., 2017; Thind et al., 2019). We assumed a mortality coefficient for the general population due to the lack of PM2.5 mortality hazard ratios by immigrant status and by immigrant region of origin. A recent Canadian study suggests that the PM2.5 mortality hazard ratio may be higher among immigrants to Canada than those born in Canada (Erickson et al., 2020). This study estimated slightly higher all-cause mortality risk attributable to PM2.5 exposure among immigrants than those born in Canada, although the difference was not statistically significant. As the general population in the US is different than that in Canada, the estimation of hazard ratios by immigrant status, further divided by region of origin and time since immigration, should be an aim of future environment health disparities research. If the premature mortality coefficient due to PM2.5 exposure were higher among immigrant residents in the US than the US-born, then our estimates of premature mortality differences between immigrants overall and the US-born would have been conservative. Adding to this, our estimates of premature mortality attributable to PM2.5 could be conservative since the mortality coefficient we applied was lower relative to those found in other studies, such as that from a reanalysis of the Harvard Six Cities Study data, where the estimated mortality hazard ratio was 1.14 (95% CI: 1.07, 1.22) per 10 μg/m3 in PM2.5 (Lepeule et al., 2012). With a higher PM2.5 all-cause mortality hazard ratio, our estimates of premature mortality attributable to PM2.5 in all groups would have been larger, as would have been estimated disparities between groups. An important future direction would be a cohort study estimating the hazard ratios from PM2.5 exposure by immigrant status, including region of origin and time since immigration. Furthermore, understanding of PM2.5 exposure and attributable health disparities can advance via research into the contribution of factors such as age at the time of immigration or combinations of race/ethnicity with immigrant status, should such data be available. In summary, our estimates of disparities between immigrants and the US-born, and among immigrant groups by region of origin, in premature mortality attributable to PM2.5 were likely to be conservative and biased towards the null due to limited data that impacted our analytical choices, although further research is needed.
Our study led to novel insights on PM2.5 exposure and attributable premature mortality disparities between immigrants and the US-born, and among immigrant subgroups by region of origin or by time since immigration. Compared to prior work that estimated premature mortality attributable to PM2.5 nationally, we used PM2.5 exposure predictions with higher spatial resolution (~1 km2 vs. 144 km2) (Fann et al., 2018; Fann et al., 2017). The increased spatial resolution likely decreased PM2.5 exposure assessment error. Our study also had almost complete spatial coverage of the contiguous US and high sample size. We were able to generate a national estimate of immigrant – US-born disparities in PM2.5 exposure and attributable premature mortality in the general population. At the same time, we also considered results by US county to highlight spatial heterogeneity. We found that the spatial heterogeneity in immigrant – US-born disparities in PM2.5 exposure was most likely driven by the sizable immigrant population from Latin America. Finally, although there have been prior studies on immigrant mortality disparities using US national data (Argeseanu Cunningham et al., 2008; Mehta et al., 2016; Singh and Siahpush, 2002), PM2.5 exposure disparities and their contribution to these health disparities were previously unexplored. Our findings motivate more research into immigrant – US-born disparities in other environmental exposures as well as the differences in health response to exposures by immigrant status.
5. Conclusion
Environmental health disparities among immigrants of the general US population is an understudied area. In this paper, we showed that average annual PM2.5 exposure was 0.36 (2.5th and 97.5th percentile: 0.19, 0.53) μg/m3 or 3.8% higher among immigrants than the US-born, which led to higher premature mortality from PM2.5 among immigrants overall and some immigrant subgroups. Between groups of immigrants by region of origin, we found higher exposures and premature mortality attributable to PM2.5 in those who immigrated from Africa, Asia, and Latin America than those who immigrated from Europe, North America, and Oceania, which provides further insight into US racial/ethnic disparities. We did not find large differences by immigrants’ time since immigration. Our results demonstrated spatial heterogeneity by county across the contiguous US, with the highest immigrant population proportion and immigrant – US-born disparities in southern California, northern Washington, and southeastern New York. This study represents an important step towards a better understanding of environmental health disparities between immigrants and the US-born, as well as among immigrant groups by region of origin. As immigrants are an increasing part of the US population, and many immigrants are entering old age, public health planning would benefit from further research on how environmental exposures contribute to immigrant health disparities.
Supplementary Material
Highlights.
Contributions of the environment to immigrant health disparities are understudied.
Immigrants had higher fine particulate air pollution exposure than US native-born.
Immigrants from Asia, Africa, and Latin America had the highest exposures.
Air pollution exposure differences may lead to disparities in premature mortality.
Disparities in air pollution and attributable premature mortality varied spatially.
Acknowledgements
We acknowledge the funding support from the National Institutes of Health and the Environmental Protection Agency. We thank the peer reviewers for their helpful input on this manuscript.
Funding Sources
This publication was developed under Assistance Agreement No. RD835871 awarded by the U.S. Environmental Protection Agency to Yale University. It has not been formally reviewed by EPA. The views expressed in this document are solely those of the authors and do not necessarily reflect those of the Agency. EPA does not endorse any products or commercial services mentioned in this publication. Research reported in this publication was also supported by the National Institute On Minority Health And Health Disparities of the National Institutes of Health under Award Number R01MD012769. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Human Subjects or Experimental Animals
This paper does not deal with research on human subjects or experimental animals.
Data Statement
All data used in this study are publicly-available. Please refer to the methods and references to access these data.
References
- Arandia G, et al. , 2012. Diet and acculturation among Hispanic/Latino older adults in the United States: a review of literature and recommendations. J Nutr Gerontol Geriatr. 31, 16–37. [DOI] [PubMed] [Google Scholar]
- Argeseanu Cunningham S, et al. , 2008. Health of foreign-born people in the United States: a review. Health Place. 14, 623–35. [DOI] [PubMed] [Google Scholar]
- Baird J, et al. , 2008. Immigrant Settlement Patterns: The Role of Metropolitan Characteristics. Sociological Inquiry. 78, 310–334. [Google Scholar]
- Brook RD, et al. , 2010. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation. 121, 2331–78. [DOI] [PubMed] [Google Scholar]
- Brugge D, et al. , 2000. An environmental health survey of residents in Boston Chinatown. J Immigr Health. 2, 97–111. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, Centers for Disease Control and Prevention (CDC) Wide-ranging Online Data for Epidemiologic Research (WONDER) - Mortality Data. Vol. 2020, 2020. [Google Scholar]
- Cohen AJ, et al. , 2017. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet. 389, 1907–1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Q, et al. , Air Pollution and Mortality in the Medicare Population. N Engl J Med, United States, 2017, pp. 1498–9. [DOI] [PubMed] [Google Scholar]
- Dupre ME, et al. , Survival Differences among Native-Born and Foreign-Born Older Adults in the United States. PLoS One, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eamranond PP, Hu H, 2008. Environmental and occupational exposures in immigrant health. Environ Health Insights. 1, 45–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erickson AC, et al. , 2020. Disease assimilation: The mortality impacts of fine particulate matter on immigrants to Canada. Health Rep. 31, 14–26. [DOI] [PubMed] [Google Scholar]
- Fann N, et al. , 2018. The estimated change in the level and distribution of PM2.5-attributable health impacts in the United States: 2005-2014. Environ Res. 167, 506–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fann N, et al. , 2017. Estimated Changes in Life Expectancy and Adult Mortality Resulting from Declining PM2.5 Exposures in the Contiguous United States: 1980-2010. Environ Health Perspect. 125, 097003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franklin BA, et al. , 2015. Air pollution and cardiovascular disease. Curr Probl Cardiol. 40, 207–38. [DOI] [PubMed] [Google Scholar]
- Gany F, et al. , 2017. Perception and reality of particulate matter exposure in New York City taxi drivers. J Expo Sci Environ Epidemiol. 27, 221–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajat A, et al. , 2015. Socioeconomic Disparities and Air Pollution Exposure: a Global Review. Curr Environ Health Rep. 2, 440–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes RB, et al. , 2019. PM2.5 air pollution and cause-specific cardiovascular disease mortality. Int J Epidemiol. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hempstead K, 2007. Mobility of the foreign-born population in the United States, 1995-2000: The role of gateway states. International Migration Review. 41, 466–479. [Google Scholar]
- Horlyck-Romanovsky MF, et al. , 2019. Foreign-Born Blacks Experience Lower Odds of Obesity but Higher Odds of Diabetes than US-Born Blacks in New York City. J Immigr Minor Health. 21, 47–55. [DOI] [PubMed] [Google Scholar]
- Hubbell B, et al. , 2009. Methodological considerations in developing local-scale health impact assessments: balancing national, regional, and local data. Air Qual Atmos Health. 99–110. [Google Scholar]
- Johnson BB, 2011. Acculturation, ethnicity, and air pollution perceptions. Risk Anal. 31, 984–99. [DOI] [PubMed] [Google Scholar]
- Johnson NB, et al. , 2014. CDC National Health Report: leading causes of morbidity and mortality and associated behavioral risk and protective factors--United States, 2005-2013. MMWR Suppl. 63, 3–27. [PubMed] [Google Scholar]
- Krewski D, et al. , 2009. Extended follow-up and spatial analysis of the American Cancer Society study linking particulate air pollution and mortality. Res Rep Health Eff Inst. 5–114; discussion 115-36. [PubMed] [Google Scholar]
- Lepeule J, et al. , 2012. Chronic exposure to fine particles and mortality: an extended follow-up of the Harvard Six Cities study from 1974 to 2009. Environ Health Perspect. 120, 965–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lievanos RS, 2015. Race, deprivation, and immigrant isolation: The spatial demography of air-toxic clusters in the continental United States. Soc Sci Res. 54, 50–67. [DOI] [PubMed] [Google Scholar]
- Mehta NK, et al. , 2016. Life Expectancy Among U.S.-born and Foreign-born Older Adults in the United States: Estimates From Linked Social Security and Medicare Data. Demography. 53, 1109–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyce SC, Schenker M, 2017. Occupational Exposures and Health Outcomes Among Immigrants in the USA. Curr Environ Health Rep. 4, 349–354. [DOI] [PubMed] [Google Scholar]
- Nasari MM, et al. , 2016. A class of non-linear exposure-response models suitable for health impact assessment applicable to large cohort studies of ambient air pollution. Air Qual Atmos Health. 9, 961–972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, E., and Medicine, 2015. The Integration of Immigrants into American Society. The National Academies Press, Washington, DC. [Google Scholar]
- Pappalardo AA, Mosnaim G, 2018. Immigrant Respiratory Health: a Diverse Perspective in Environmental Influences on Respiratory Health. Curr Allergy Asthma Rep. 18, 21. [DOI] [PubMed] [Google Scholar]
- Parker JD, et al. , 2018. Particulate Matter Air Pollution Exposure and Heart Disease Mortality Risks by Race and Ethnicity in the United States: 1997 to 2009 National Health Interview Survey With Mortality Follow-Up Through 2011. Circulation. 137, 1688–1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Passel J, Cohn D, 2008. U.S. population projections: 2005-2050.
- Pinault L, et al. , 2017. Exposure to fine particulate matter air pollution in Canada. Health Rep. 28, 9–16. [PubMed] [Google Scholar]
- Pope CA 3rd, et al. , 2019. Mortality Risk and Fine Particulate Air Pollution in a Large, Representative Cohort of U.S. Adults. Environ Health Perspect. 127, 77007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pun VC, et al. , 2017. Long-Term PM2.5 Exposure and Respiratory, Cancer, and Cardiovascular Mortality in Older US Adults. Am J Epidemiol. 186, 961–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria, 2020. [Google Scholar]
- Ritz B, et al. , 2019. The Effects of Fine Dust, Ozone, and Nitrogen Dioxide on Health. Dtsch Arztebl Int. 51-52, 881–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh GK, Hiatt RA, 2006. Trends and disparities in socioeconomic and behavioural characteristics, life expectancy, and cause-specific mortality of native-born and foreign-born populations in the United States, 1979-2003. Int J Epidemiol. 35, 903–19. [DOI] [PubMed] [Google Scholar]
- Singh GK, Miller BA, 2004. Health, life expectancy, and mortality patterns among immigrant populations in the United States. Can J Public Health. 95, I14–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh GK, et al. , 2013. Immigrant health inequalities in the United States: use of eight major national data systems. ScientificWorldJournal. 2013, 512313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh GK, Siahpush M, 2001. All-cause and cause-specific mortality of immigrants and native born in the United States. Am J Public Health. 91, 392–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh GK, Siahpush M, 2002. Ethnic-immigrant differentials in health behaviors, morbidity, and cause-specific mortality in the United States: an analysis of two national data bases. Hum Biol. 74, 83–109. [DOI] [PubMed] [Google Scholar]
- Thind MPS, et al. , 2019. Fine Particulate Air Pollution from Electricity Generation in the US: Health Impacts by Race, Income, and Geography. Environ Sci Technol. 53, 14010–14019. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau, Differences between the ACS and the Decennial Census. Understanding and Using American Community Survey Data. U.S. Government Printing Office, Washington, DC, 2018. [Google Scholar]
- U.S. Census Bureau, American FactFinder. 2019. [Google Scholar]
- van Donkelaar A, et al. , 2019. Regional Estimates of Chemical Composition of Fine Particulate Matter Using a Combined Geoscience-Statistical Method with Information from Satellites, Models, and Monitors. Environ Sci Technol. 53, 2595–2611. [DOI] [PubMed] [Google Scholar]
- Vespa J, et al. , Demographic Turning Points for the United States: Population Projections for 2020 to 2060. Current Population Reports, Vol. 2018. United States Census Bureau, 2018. [Google Scholar]
- Woo B, et al. , 2019. Residential Segregation and Racial/Ethnic Disparities in Ambient Air Pollution. Race Soc Probl. 11, 60–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang M, et al. , 2020. Effects of long-term exposure to air pollution on the incidence of type 2 diabetes mellitus: a meta-analysis of cohort studies. Environ Sci Pollut Res Int. 27, 798–811. [DOI] [PubMed] [Google Scholar]
- Zhang H, et al. , 2020. Ambient air pollution and gestational diabetes mellitus: A review of evidence from biological mechanisms to population epidemiology. Sci Total Environ. 719, 137349. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


