Abstract
Background
Public safety personnel and frontline healthcare professionals are at increased risk of exposure to potentially psychologically traumatic events (PPTE) and developing posttraumatic stress injuries (PTSI, e.g., depression, anxiety) by the nature of their work. PTSI are also linked to increased absenteeism, suicidality, and performance decrements, which compromise occupational and public health and safety in trauma-exposed workers. Evidence is lacking regarding the effectiveness of “prevention” programs designed to mitigate PTSI proactively. The purpose of this review is to measure the effectiveness of proactive PTSI mitigation programs among occupational groups exposed to PPTE on measures of PTSI symptoms, absenteeism, and psychological wellness.
Methods
Five electronic databases were searched per PRISMA guidelines for English or French peer-reviewed studies from 2008 to 2019 evaluating PTSI and psychological wellness in adults exposed to occupational PPTE. The risk of bias was assessed using the Newcastle-Ottawa Scale.
Results
We identified 42 studies evaluating 3182 public safety and frontline healthcare professionals, PPTE-exposed educational staff, and miners. Significant overlap was found across program themes that included mindfulness, psychoeducation, resilience promotion, and stress management strategies. Post-program effect sizes were small (SMD < 0.5) to moderate (SMD < 0.8) for reductions in PTSI symptoms and for promoting measures of well-being as indicated by a meta-analysis on 36 studies. There was no evidence for significant reductions in substance use, absenteeism, or biomarkers of distress except for heart rate. Subgroup analyses indicated that multimodal programs effectively improved general psychological health, while resilience programs improved measures of depression, burnout, coping, and resilience. Effect sizes for resilience, depression, and general psychological health improvements were greatest immediately or 1-month post-training, while improvements in PTSD symptoms and coping were larger at longer follow-up. Studies were of moderate quality and risk of bias.
Conclusions
The current results showcase modest evidence for time-limited reductions in PTSI following participation in holistic programs that promote resilience, stress, and emotion regulation among at-risk workers. Implications for organizational implementation of proactive PTSI mitigation programs and areas of future research are discussed.
Systematic review registration
PROSPERO (CRD42019133534)
Supplementary Information
The online version contains supplementary material available at 10.1186/s13643-021-01677-7.
Keywords: Posttraumatic stress injuries, Organizational stress, Mental health training, Occupational health, Resilience, Emergency personnel, Essential workers, Public safety, Healthcare, Meta-analysis
Background
Public safety personnel (PSP) serve to maintain public safety and well-being. Occupations included within the definition of PSP include, but are not limited to, border services officers, public safety communications officials (e.g., dispatch or 911 operators), correctional workers, firefighters (career and volunteer), paramedics, and police [1]. PSP and frontline healthcare personnel (FHP, e.g., nurses, physicians, social workers, counselors, and staff in emergency, trauma, surgical, psychiatric, geriatric, and/or intensive care units) are frequently and repeatedly exposed to potentially psychologically traumatic events (PPTEs) [1–3]. Consequently, PSP and FHP appear to be at increased risk for posttraumatic stress injuries (PTSIs) [4–7], which appears to be further exacerbated during the global COVID-19 pandemic [8–11].
PTSI typically include symptoms of major depressive disorder, panic disorder, generalized anxiety disorder, posttraumatic stress disorder, suicidal ideation and attempts, and substance abuse [1, 4, 12]. In a recent pan-Canadian survey of PSP, 44.5% of respondents screened positive for at least one occupationally mediated PTSI [4, 13]. Furthermore, PSP appear up to four times more likely than the general population to report suicidal behaviors (i.e., ideation, planning, attempts, deaths) [14, 15]. Recent evidence for PTSI prevalence among FHP is lacking; however, the Canadian Federation of Nurses Unions [16] reported that 61% of nurses had experienced abuse, harassment, or assault in the workplace. FHP also report high levels of occupationally mediated compassion fatigue and burnout [17]. The concept of burnout was first proposed in the early 1970s by psychologist Christina Maslach, who explored a phenomenon among care providers involving emotional exhaustion, depersonalization, and diminished personal achievement [18]. Over time, this tripartite construct has become known as burnout [19]. Burnout is currently not a diagnosable mental health disorder but has been formally included as a problematic syndrome in ICD-11 [20].
Evaluations of PPTEs among PSP and FHP have focused mainly on first responders and frontline workers; however, recent evidence indicates that the civilians who work alongside them (e.g., administrative staff, public service employees, victim services) are also frequently exposed to PPTE and report comparable levels of PTSI and suicidal behaviors [21]. The COVID-19 pandemic has also highlighted several less conventional “essential” occupational sectors at increased risk of occupational PPTEs, including public-facing personnel such as transportation workers, grocery clerks, and restaurant workers [22]. Workers in extractive sectors including miners and drillers also regularly face life-threatening operational conditions, increasing the risk for occupationally mediated PPTE [23]. While any study of the effectiveness of a proactive psychological program delivered in an occupational context will qualify for inclusion in the current work, we will focus on PSP and FHP (broadly defined) as the extant literature supports that these occupational groups are most frequently exposed to work-related PPTE.
PTSI symptoms may also negatively impact occupational performance quality, increase absenteeism, increase sleep difficulties, negatively impact interpersonal relationships, increase burnout, and increase early mortality [4, 12, 24, 25]. The economic burden of PTSI among Canadian PSP and FHP is unknown [26]; nevertheless, annual productivity losses from mental disorders experienced by Canadians are estimated to cost between $16.6 [27] and $21 billion [28]. In the USA, health care costs for treating a firefighter, paramedic, or police officer with PTSD are almost five times higher than one without PTSD (~ $10,000/year versus ~ $2000) [26]. The significant costs have prompted several stakeholder organizations and occupational health policymakers to seek proactive approaches, such as implementing psychological and mental health training programs to mitigate the impact of PPTE on workers [29]. Accordingly, psychological interventions that promote well-being have been shown to reduce absenteeism [30, 31]. Proactive measures to support mental health may be particularly relevant for PSP given evidence that stigma is substantially inhibiting care-seeking for mental health challenges [13].
Proactive psychological programs have occasionally been integrated into basic training as part of efforts to increase individual resilience before PPTE exposures, as demonstrated among paramedic [32, 33] and nursing students [34], as well as federal and special forces police in Canada and abroad [35–37]. Proactive psychological programs have been increasingly offered to experienced workers who have already been exposed to PPTE but are intended to “prevent” or mitigate the development of PTSI rather than treat them. The current systematic review and meta-analysis focuses on a broad variety of proactive psychological program types in order to investigate the degree to which various occupationally mediated PTSIs are impacted by different programming approaches. We are reticent to label “prevention” programs because of rampant misuses of the term in the existing literature and mental health programming. A program can only be deemed preventative with highly rigorous pre- and post-training PTSI clinical screenings among persons who do not already have a PTSI or mental disorder, which would confound the results. The extant literature indicates that any post-training gains (i.e., effect sizes) are small and very time-limited [13, 38]; also, the gains are expected to deteriorate like other learned skills [33, 39, 40], meaning refresher programs are likely critical for maintaining gains. Despite important efforts at summarizing the existing pre- and post-exposure programming options for first responders frequently exposed to PPTE [41–43], there are currently significant research gaps regarding the effectiveness of proactive programs designed to mitigate PTSI, especially among FHP.
Objectives
The current study was designed as a systematic literature review to identify published research on proactive PTSI mitigation programs tailored for PSP, FHP, and other workers exposed to PPTE. The effectiveness of such programs for improving outcomes related to PTSI and psychological health will be evaluated with a quantitative meta-analysis. Comparators will include controls in the waitlist, nil treatment, training as usual, or alternative programming groups, and baseline scores for within-subject studies. Results are presented to summarize the various training approaches, durations, and outcomes evaluated in empirical studies of program effectiveness. The current results can assist industrial, organizational, and occupational stakeholders in implementing evidence-based programming for mitigating PTSI among at-risk workers.
Methods
Protocol and registration
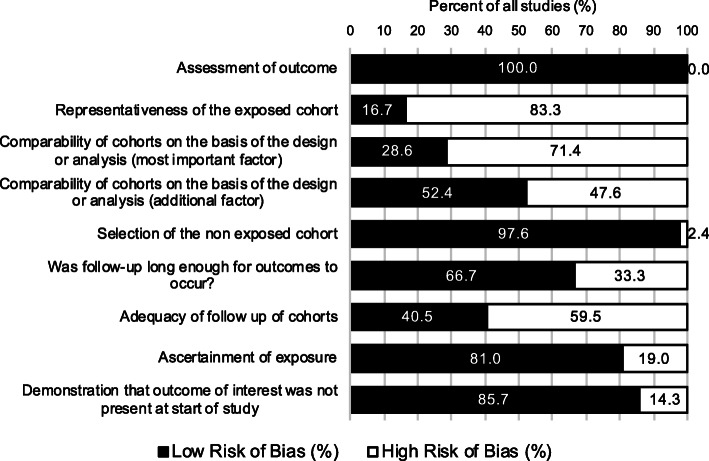
The current study was pre-registered with PROSPERO (CRD42019133534) [44]. Systematic literature review procedures followed PRISMA guidelines [45], as illustrated in Fig. 1 and in the PRISMA checklist in Additional File 1.
Fig. 1.
PRISMA flow diagram
Eligibility criteria
The current review was restricted to peer-reviewed English- or French-language studies assessing the impact of any mental health program designed to mitigate the impact of PPTE among adult (aged 18 and older) workers and published since January 1, 2008. To maximize yield, we extended eligibility to any PPTE-exposed group of workers, including counselors, correctional workers, dispatchers, emergency workers, firefighters, nurses, paramedics, police, rail transit operators, and social workers. Eligible study designs included randomized control trials (RCT) and quasi-experimental studies (e.g., pre-post studies). Studies involving participants with one or more identifiable mental disorders (e.g., clinician diagnosis or a positive screen on a validated psychological instrument), non-PPTE occupational stressors (e.g., work-related demands, organizational stress), or non-experimental designs (e.g., protocols, theses, qualitative studies) were excluded.
Information sources
A population-intervention-comparison-outcome (PICO) framework was used to define study variables of interest and keywords entered into our systematic literature searches, which are provided in Table 1. We searched EMBASE, MEDLINE, PsycINFO, PubMed, and Web of Science between 2008 and December 9, 2019. The database-facilitated searches were supplemented for additional studies with hand-searches of the reference lists from included studies, as well as previous review articles and reports. Following the searches, all citations were imported into Covidence—a web-based systematic review manager [46]. There were two independent reviewers who screened articles against the eligibility criteria: first by title/abstract and then in full. Initial screening was verified by having multiple reviewers screen 200 papers resulting in 99% agreement. All discrepancies were resolved by consensus between the two reviewers.
Table 1.
PICO literature search strategy
| Domain | Target | Search terms |
|---|---|---|
| Population | Public safety personnel |
Firefighters Police officers Law enforcement Dispatch Communication officers Paramedic Emergency medical technician Emergency medical service First responders Correctional officers Emergency workers Emergency response team Emergency room personnel Nurses Transit operators Transit workers Social workers Counselors |
| Intervention | Prevention training programs |
Prevention Resilience Coping (skills) Family coping Stress reduction Skill building Wellness capacity Capacity building Psychoeducation Mental health awareness (training) Stigma reduction |
| Comparison | Control group |
Waitlist control Randomized control trial |
| Outcome | Posttraumatic stress injuries |
Operational Stress Injury PTSD PTSI Occupational stress Trauma Trauma exposure (Major) depression Anxiety Substance use disorder Chronic pain Insomnia Stress |
Data extraction
There were two reviewers who extracted data independently from published full-text reports of eligible articles. Per the PICO framework (Table 1), population variables included sample size, age, sex, and years of employment. Intervention variables included the duration of the training program, as well as program themes and approaches reported by study authors. Comparison variables included the type and nature of the comparator group. Outcome variables included absenteeism, scores on validated psychological instruments (i.e., General Health Questionnaire [GHQ], Symptoms Checklist 90 [SCL-90], Depression Anxiety Stress Scale-21 [DASS-21], and physiological markers of stress (e.g., heart rate, blood pressure, salivary and plasma cortisol). Absenteeism did not include individuals already on medical leave at the time of the study. Absenteeism was measured for individuals participating in the PTSI mitigation program (versus annual reports of overall sickness absence). Missing data or outcomes reported in incompatible form for the meta-analysis (e.g., ranks, medians, regression results) were requested from corresponding authors. To maximize power for the meta-analysis, program types and outcome variables were categorized, and operational definitions are provided in Tables 2 and 3, respectively.
Table 2.
Proactive PTSI mitigation program categories and specific interventions included in the meta-analysis
| Intervention category | Specific programs included |
|---|---|
| Emotion Regulation | 1. Emotion Regulation Training |
| Mindfulness-based |
1. Yoga 2. Mindfulness-Based Resilience Training 3. Mindfulness-Based Stress Reduction |
| Resilience Promotion |
1. Resiliency Training Program 2. Online Resiliency Training 3. Imagery and Skills Training 4. Complementary Psychological Training 5. International Performance Resilience and Efficiency Program (iPREP) |
| Multimodal |
1. Relation, mindfulness, CISD 2. ERASE-Stress intervention 3. Work-related gratitude diary 4. Eclectic group counseling 5. Stress Management (multimodal) 6. Integrated Health Program |
| Stress Management | 1. Acceptance and Commitment Therapy |
| Web-based psychoeducation |
1. Online Workplace Mental Health Intervention 2. Web-based stress management program 3. Road to Mental Readiness 4. Stress Management Mobile App |
Table 3.
Outcome categories and specific measures included in the meta-analysis
| Outcome category | Specific measures included | Direction |
|---|---|---|
| Absenteeism |
1. Number of days on sick leave in previous 2 months 2. Number of weeks on full-time sick leave the preceding year 3. Number of days on sick leave |
Lower is better |
| Alcohol |
1. Patient Reported Outcomes Measurement Information System (PROMIS) Alcohol Use Subscale 2. Alcohol use disorders identification test (AUDIT) 3. Drank in the past 12 Months 4. Number of days having 5 or more drinks on one occasion in past 30 days 5. Number of drinks per drinking day in past 30 days 6. Using Alcohol to Relieve Stress |
Lower is better |
| Anger | 1. Personal and Organizational Quality Assessment: anger and resentment subscale | Lower is better |
| Antithrombin | 2. Serum antithrombin | Lower is better |
| Anxiety |
1. Patient Reported Outcomes Measurement Information System (PROMIS) Anxiety Subscale 2. Depression Anxiety Stress 21 Scale (Anxiety subscale) 3. State-Trait Anxiety Inventory (STAI) 4. Profile of Mood States Tension-Anxiety Subscale 5. Brief Symptom Inventory: Anxiety Subscale 6. Personal and Organizational Quality Assessment-Anxiety Subscale 7. General Health Questionnaire-Anxiety Subscale 8. Hospital Anxiety and Depression Scale-Anxiety Subscale 9. Symptoms Checklist (SCL-90)-Phobic Anxiety Subscale 10. Adult Manifest Anxiety Scale 11. DASS-21: Anxiety |
Lower is better |
| Blood pressure |
1. Diastolic blood pressure 2. Systolic blood pressure |
Lower is better |
| Burnout |
1. Maslach Burnout Inventory Depersonalization Domain 2. Maslach Burnout Inventory Emotional Exhaustion Domain 3. Maslach Burnout Inventory Personal Accomplishment Domain 4. Oldenburg Burnout Inventory 5. Professional QoL: Burnout 6. Professional Quality of Life Scale 7. Maslach Burnout Inventory Overall |
Lower is better |
| Coping |
1. Emotion-Regulation Skills Questionnaire 2. Brief-Coping Orientation to Problems Experienced (Brief-COPE) 3. Operationalized 3-item coping skills measure 4. Recovery Experiences Questionnaire-Global Score |
Higher is better |
| Cortisol |
1. Serum cortisol 2. Salivary cortisol |
Lower is better |
| Depression |
1. PANAS-Negative Affect Subscale 2. PANAS-Positive Affect Subscale* (higher is better) 3. DASS-21 Scale (Depression subscale) 4. Brief Symptom Inventory: Depression Subscale 5. Hospital Anxiety and Depression Scale-Depression subscale 6. Centre for Epidemiological Studies Depression Scale (CES-D) 7. Beck Depression Inventory II 8. Personal and Organizational Quality Assessment: anxiety and depression subscale 9. Profile of Mood States Negative Mood Composite |
Lower is better |
| DHEA |
1. Salivary dehydroepiandrosterone (DHEA) 2. Serum dehydroepiandrosterone-sulfate (DHEA-s) |
Lower is better |
| Drug Use |
1. Using prescription drugs as prescribed to relieve stress 2. Using prescription drugs not as prescribed to relieve stress |
Lower is better |
| General Symptoms |
1. General Health Questionnaire 2. Symptoms Checklist (SCL-90)-Overall |
Lower is better |
| Heart rate |
1. Average heart rate during scenarios 2. Average resting heart rate 3. High frequency (HF) heart rate variability (HRV) 4. Inter-beat Interval 5. Standard deviation of normal RR intervals 6. Maximum heart rate during scenarios 7. Heart rate recovery time |
Lower is better |
| Prolactin | 1. Serum prolactin | Lower is better |
| PTSD |
1. Professional QoL: secondary traumatic stress 2. Posttraumatic Check List 3. Impact of events scale: intrusive subscale 4. Impact of events scale: avoidance subscale 5. Response to stressful experiences scale 6. Posttraumatic Diagnostic Scale 7. Posttraumatic Check List for DSM-5 (PCL-5) |
Lower is better |
| Resilience |
1. Freiburg Mindfulness Inventory 2. Connor-Davidson Resilience Scale 3. Acceptance and Action Questionnaire II 4. Brief Resilience Scale 5. Self-Compassion Scale 6. Resilience Scale-global score |
Higher is better |
| Stress |
1. Police Stress Questionnaire Organizational Subscale 2. Police Stress Questionnaire Operational Subscale 3. Perceived Stress Scale 4. Depression Anxiety Stress 21 Scale (Stress subscale) 5. Professional Quality of Life Scale 6. Job stress 7. Self-reported stress 8. Coping with stress: Full Scale 9. Symptoms of Distress: Full Scale |
Lower is better |
| Suicidality | 1. Concise Health Risk Tracking Scale (suicidal ideation) | Lower is better |
| Well-being |
1. Health-Promoting Lifestyle Profile II 2. Patient-Reported Outcomes Measurement Information System (PROMIS) Global Scale 3. Professional QoL: Compassion satisfaction 4. Cognitive Fusion Questionnaire 5. Sources of support scale 6. Mental Health Continuum Short Form (MHC-SF): Overall 7. Performance-based self-esteem scale 8. Nurses Job Satisfaction |
Higher is better |
Quality assessment
Study quality was appraised using the Newcastle-Ottawa Scale [47], which evaluates nine items across three domains: outcome, selection, and comparability. Each item received a rating of high, low, or unclear risk of bias; each instance of a low risk of bias counted as one point, for a total possible score of nine. Overall study quality was operationalized using the total score: scores of 9 as “high quality,” scores of 7 or 8 as “moderate to high quality,” scores of 5 or 6 as “moderate to low quality,” and scores of 4 and below as “low quality.”
Synthesis of results
Eligible studies for the quantitative meta-analyses needed to report means and standard error or standard deviation values for study outcomes of interest (see Table 3). A random-effects model was applied to pool effect sizes across studies using standardized mean differences (SMD) and their corresponding 95% confidence intervals (CI). Cohen’s criteria [48, 49] were used to interpret an SMD of 0.2 as “small,” 0.5 as “medium,” and 0.8 or greater at “large.” SMDs were measured at all available post-training and follow-up timepoints.
Assessment of heterogeneity and additional analyses
Heterogeneity was quantified using the I2 statistic [50] and forest plots to graphically display summary effect sizes across studies [51]. Outcomes with at least ten studies were explored for sources using the following pre-specified subgroup analyses: occupation (e.g., firefighters, police officers), intervention (e.g., mindfulness-based, multimodal), and timeline (e.g., post-training, 1-month follow-up, 18-month follow-up). Sensitivity analyses included comparisons of random-effects and fixed-effects model effect sizes, as well as with the leave-out-one technique. For outcomes with at least ten studies, publication bias was assessed using funnel plots, the trim and fill method [52], and Egger’s test of funnel plot asymmetry [53, 54].
Results
Systematic literature review
The systematic review identified a total of 4154 studies. Among the identified studies, there were 224 removed as duplicates, leaving 3930 studies for the title and abstract screening. There were 3815 records removed, leaving 115 studies for full-text review. There were 73 studies excluded at the full-text stage: 25 had a wrong population (i.e., not PSP, FHP, or a PPTE-exposed occupational group), 23 had a wrong study design (i.e., not a pre-post evaluation of outcomes such as qualitative studies or protocols, or non-peer-reviewed dissertations, books, or reports), 20 had a wrong intervention (e.g., post-PPTE service, treatment, or therapeutic intervention), 4 had wrong outcomes (e.g., program acceptability or outcomes unrelated to mental health or wellness), and 1 was a duplicate title. The systematic review process resulted in 42 eligible studies that evaluated the effectiveness of a proactive PTSI mitigation program in workers exposed to PPTEs. Key study characteristics are described below and are summarized in Table 4, including participant summaries, study designs, PTSI mitigation program themes, primary outcomes, and results. A subsequent six studies were excluded from the meta-analysis for failing to report the means and/or standard deviations for their primary outcome measures [72, 86, 89], or reporting the means and/or standard deviations in formats that were incompatible for a quantitative meta-analysis; for example, reporting regression results [71], medians [81], or ranks [77]. All authors were contacted with data requests, but data were not yet provided at the time of submitting the current review. Ultimately, 36 studies were included in a quantitative meta-analysis (Fig. 1).
Table 4.
Summary characteristics of eligible studies (n = 42). Studies not included in meta-analyses (n = 6) are marked with an asterisk (*)
| Study (quality) | Sample size | Population (country) | Design | Program description | Program duration | Evaluation | Outcomes | Results |
|---|---|---|---|---|---|---|---|---|
| Alexander et al., 2015 [55] (Moderate-Low) | 40 | Nurses (USA) | RCT | Mindfulness-based stress management (Yoga) vs. Nil training | 1 session (time not provided) × 8 weeks | Pre-training, post-training | HPLP-II; FMI; MBI EE, DP, PA subscales | Significant post-training improvements in self-care (HPLP-II), EE and DP |
| Andersen et al., 2015 [35] (Moderate-Low) | 18 | Special forces (SWAT) police officers (Finland) | Prospective cohort study | Psycho-educational and physiological resilience promotion with HRV-BF (iPREP) | 5 days × 60 min sessions + 15 min daily breathing practice | Pre-training, post-training | HRmax; HRavg; respiratory achievement and coherence while listening to critical incident scenarios | Significant reductions in HRavg and improvement in respiratory achievement scores on Day 5 vs Day 1 of training, indicative of improved autonomic regulation under stress |
| Andersen & Gustafsberg, 2016 [36] (Moderate-High) | 12 | Special forces (SWAT) police officers (Finland) | RCT | Psycho-educational and physiological resilience promotion with HRV-BF (iPREP) vs. TAU | 5 days total: 2 pre-post evaluation days, 3 training days | Pre-training, post-training | HRmax; HRRec to HRBase; BP; self-reported stress | At post-training evaluations, the iPREP group had significantly lower HRMax (scenario 1 only) |
| Andersen et al., 2018 [40] (Moderate-low) | 57 | Police officers (Canada) | Prospective cohort study | Psycho-educational and physiological resilience promotion with HRV-BF (iPREP) | 4 days total: 1.5 days of pre and post-training evaluation, 2.5 days of training | Pre-training, post-training, 6, 12, and 18 months | HRMax and HRIndex during critical incident scenarios; HRRec | Significant reductions in HRIndex at 12 months follow-up, but not maintained at 18 months follow-up; HRRec faster at 12 and 18 months follow-up relative to pre- and post-training and 6 months follow-up |
| Anderson, Vaughan & Mills, 2017 [33] (Moderate-Low) | 138 | Primary care paramedical students performing a duty practicum (Canada) | RCT | Web-based psychoeducational resilience promotion vs. TAU | 6-8 hours | Pre-training, post-training | RS global score and subscales | Resilience training significantly improved all measures except meaningfulness subscale following in-field practicum. SD values obtained from authors. |
| Arble et al., 2017 [56] (Moderate-High) | 22 | Police officers (USA) | Prospective cohort study | Psychoeducational resilience promotion and coping skill building | 5 × 90 min group sessions | Pre-training, 12 months | COPE subscales; Sources of Support Scale; PCL; HADS; AUDIT | Following their first year in the field, officers appeared to report improved use of positive reframing and humor, and significant reductions in anxiety |
| Arnetz et al., 2009 [57] (Low) | 18 | Police officers (Sweden) | RCT | Psycho-educational and physiological resilience promotion and coping skill building vs. TAU | 2 h × 10 weeks | 12 months | Serum antithrombin and cortisol; mean change in HR; self-reported stress; POMS vigor-activity subscale and negative mood composite | Following their first year in the field, trained officers appeared to report less negative mood, smaller changes in mean HR and self-reported stress, and greater changes in antithrombin following a simulated critical incident |
| Arnetz et al., 2013 [58] (Moderate-High) | 75 | Police officers (Sweden) | RCT | Psycho-educational and physiological resilience promotion vs. TAU | 90 min × 10 weeks + homework 3× per week | Pre-training, 18 months | GHQ, serum cortisol; prolactin; DHEA | Statistically significant post-training improvement in GHQ only |
| Bademci et al., 2016 [59] (Moderate-Low) | 42 | Correctional officers (Turkey) | Prospective cohort study | Psychosocial support program | 75-min sessions, 3 times a week × 11 weeks (41.25 hs total) | Pre-training, post-training | PANAS; MBI EE, DP, PA subscales; BDI; BAI | Significant post-training improvements on all measures |
| Berger et al., 2016 [60] (Moderate-High) | 63 | Educational staff affected by the 2011 Christchurch earthquake (New Zealand) | RCT | Multimodal psychoeducational resilience promotion (EZ) vs. Critical incident management (METI) | 3 × 8 h sessions for both treatments | Pre-training, post-training, 8 months | PCL; ProQoL CF, burnout, CS subscales; CDRS | Resilience higher pre-training in EZ, significantly improved post-training for both groups. Greater improvements in PCL and ProQoL subscales for EZ compared with METI |
| Berking et al., 2010 [61] (Moderate-Low) | 31 | Police officers (Switzerland) | Crossover RCT | Psycho-educational and physiological emotion regulation, cognitive therapy, coping skill building (iTEC) vs. WLC | 12 × 45 min sessions delivered on 3 days over 4 weeks + at least 3 brief and one longer daily homework | Pre-training, post-training | ERSQ; PANAS | Statistically significant post-training increase in ERSQ scores and near-significant increase in positive affect scores |
| Bolier et al., 2014 [62] (Moderate-Low) | 366 | Allied health professionals (nurses, surgery assistants, physiotherapists, radiotherapists) (The Netherlands) | Cluster RCT | Web-based psychoeducation vs. Nil training | 4 to 8 weeks | Pre-training, 3 months, 6 months | MHC-SF global score + subscales; WHO-5 Well-being Scale; BSI depression and anxiety subscales | All measures except BSI depression improved post-training, 3 months and 6 months follow-up for both groups. Significant improvement in MHC-SF global and psychological well-being subscales for training group only. Very low uptake and compliance |
| Brinkborg et al., 2011 [63] (High) | 106 | Social workers (Sweden) | RCT | Psychoeducational stress management and cognitive therapy (ACT-SMI) in high stress (PSS ≥ 25) vs. ACT-SMI in low stress (PSS ≤ 24) vs. high-stress WLC vs. low-stress WLC | 4 × 3 h biweekly group sessions + homework (physical exercise, mindfulness) | Pre-training, post-training | PSS; MBI global, EE, DP, PA subscales; GHQ; Pbse | Significant reductions in all measures except Pbse for all ACT-SMI participants compared with WLC. High stress groups: significant reductions in PSS, MBI. Low stress groups: significant reductions in PSS, MBI global + PA subscale only |
| Brondolo et al., 2017 [64] (Moderate-Low) | 257 | ME’s, investigators, autopsy technicians, clerics/administrators, laboratory workers, clergy, legal staff, and facilities managers (USA) | Prospective cohort study | Web-based psychoeducation | 3 modules × 16 classes × 5-7 min each, mean completion = 10.69 classes (SD = 7.74, range 1-21) | 3 months and immediately pre-training, 1 month post-training | BDI; PDS | Of the 76 participants who completed at least 8 classes, post-training BDI scores were significantly lower than baseline or pre-training values, no changes in PDS values. Unadjusted M and SD values not reported in the text but provided by authors. |
| Carleton et al., 2018 [38] (Moderate-Low) | 133 | Police officers (Canada) | Prospective cohort study | Psychoeducational resilience promotion, stress management, coping skill building (R2MR) | 4-h group seminar | Pre-training, 6 months, 12 months | BRS; DASS subscales; PCL; AUDIT | No statistically significant changes in mental health or resilience post-training or at follow-up, but small significant post-training reductions in stigma |
| Cheng et al., 2015 [65] (Moderate-High) | 102 | Hospital workers (physicians, nurses, physiotherapists, and occupational therapists) (Hong Kong) | RCT | Emotion regulation | Gratitude journal (2 weekly entries × 4 weeks) vs. Hassle journal vs. Nil treatment | Pre-training, post-training, 3 months | CES-D, PSS |
Significant post-training reductions for the gratitude group only, further improved (CES-D) or maintained (PSS) at follow-up. M and SD values extracted from reported regression analyses, author contacted for raw data |
| Chongruksa et al., 2012 [66] (Moderate-High) | 42 | Police officers (Thailand) | Cluster RCT | Multimodal psychoeducation and counseling vs. Mental health psychoeducation control | 1.5–2 h/week × 12 weeks for both groups | Pre-training, mid-training, post-training, 1 month | BDI; GHQ global score + subscales; SCL-90 global score + subscales | Significant reductions in all measures mid- and post-training for the multimodal group only, and increased scores at 1-month follow-up |
| Christopher et al., 2016 [67] (Low) | 43 | Police officers (USA) | Prospective cohort study | Mindfulness-based resilience promotion | 2 h × 8 weeks + 6 h final lesson + daily homework (20 h total) | Pre-training, mid-training, post-training | BRS; OLBI; PSQ; PSS; PROMIS Global Mental Health Subscale; cortisol AUC | Significant post-training improvements on all measures, and significant increase in cortisol AUC predicted by change in PROMIS mental health score |
| Christopher et al., 2018 [68] (Moderate-Low) | 61 | Police officers (USA) | RCT | Mindfulness-based resilience promotion vs. Nil training | 2-h sessions × 8 weeks + 6-h session (20 h total) | Pre-training, post-training, 3 months | PROMIS subscales; Concise Health Risk Tracking Scale (suicidal ideation); PSQ; OLBI; CDRS; AUC cortisol | Significant post-training improvement in burnout and organizational stress only. Significant post-training reduction in cortisol AUC in males only. No differences at follow-up |
| Craigie et al., 2016 [69] (Moderate-High) | 20 | Nurses (Australia) | Prospective cohort study | Mindfulness-based resilience promotion | 12 h total + daily mindfulness homework practice | Pre-training, post-training, 1 month | DASS subscales; ProQoL subscales; STAI; CDRS | Significant post-training reductions in DASS depression, ProQoL burnout, and STAI, only the latter two remained significant at follow-up. Significant improvements in DASS Stress and ProQoL compassion satisfaction from pre-training to follow-up |
| Daigle et al., 2018 [70] (Moderate-Low) | 70 | Nurses (Canada) | RCT | Mindfulness-based stress management vs. WLC | 2.5 h × 8 weeks + full day retreat + recommended 45 min daily practice | Pre-training, post-training | POMS-TA | Significantly reduced POMS-TA post-training |
| Duarte et al., 2017 [71] (Low)* | 48 | Oncology nurses (Portugal) | Prospective cohort study | Mindfulness-based stress management | 2-h group sessions × 6 weeks + 15 min daily homework | Post-training | DASS subscales; ProQoL BO, CF subscales, SLS | Significant post-training reductions in DASS Stress, ProQoL, and SLS. Direct effects of regression analyses reported only, author contacted for M and SD values |
| Duchemin et al., 2015 [72] (Moderate-Low)* | 32 | SICU personnel (USA) | RCT | Multimodal mindfulness-based intervention vs. WLC | 9 × 1 h weekly sessions + recommended 20 min daily practice | Pre-training, post-training | PSS, DASS stress subscale, MBI EE, DP and PA subscales, ProQoL CS, BO STS subscales, self-report work stress |
Significant post-training reduction in DASS stress and proportion of participants with high (> 26) EE scores. M and SDs for primary outcome measures not provided, authors contacted. |
| Flarity et al., 2013 [73] (Moderate-Low) | 59 | Nurses (USA) | Prospective cohort study | Psychoeducational resilience promotion | 4-h group seminar | Pre-training, post-training | ProQoL CS, BO, STS subscales | Significant post-training improvements in all subscale scores and proportion in high/low cut-off ranges |
| Hersch et al., 2016 [74] (Moderate-Low) | 104 | Nurses (USA) | RCT | Web-based stress management (BREATHE) vs. WLC | 7 online modules (average time = 43 min) | Pre-training, 3 months post-training | Nursing Stress Scale; Symptoms of Distress (emotional symptoms subscale); Coping with Stress Scale | Significant post-training improvement in Nursing Stress Scale only. Low rates of participation |
| Joyce et al., 2018 [75] (Low) | 29 | Firefighters (Australia) | Prospective cohort study | Web-based, mindfulness-based resilience promotion (RAW) | 6 × 20–25 min sessions + optional practice | Pre-training, post-training | CDRS; CFQ; AAQ-II | Mean increase in resilience and reduction in cognitive fusion, psychological inflexibility, and avoidance, but not statistically significant |
| Joyce et al., 2019 [76] (Moderate-High) | 143 | Primary Fire and Rescue and Hazmat (Australia) | Cluster RCT | Web-based, mindfulness-based resilience promotion (RAW) vs. Healthy Living Program (control) | 6 × 20–25 min sessions + optional practice vs. 6 × 20 min modules | Pre-training, 6 weeks and 6 months post-training | CDRS; BRS; FMI; AAQ-II; SCS; LOT-R; COPE active coping, emotional support, instrumental support subscales; LET | Significantly higher resilience and active coping in RAW participants at 6 months follow-up compared with control but coping not sustained at follow-up. Improved mindfulness sustained in full but not partial program completers. Authors contacted for CDRS and BRS SD values. |
| Larijani et al., 2018 [77] (Low)* | 126 | Red Crescent Healthcare Centers (Iran) | Cluster RCT | Resilience promotion vs. Nil training | No description | Pre-training, post-training | GHQ physical symptoms, anxiety, social dysfunction, and depression subscales |
Post-training improvements in physical symptoms, anxiety, and social dysfunction in experimental group only. Ranked data not useable for meta-analyses, authors contacted for unadjusted M and SD values. |
| Lin et al., 2019 [78] (Moderate-Low) | 90 | Nurses (China) | RCT | Multimodal mindfulness-based cognitive therapy vs. WLC | 8 × 2 h weekly group mindfulness sessions + recommended practice vs. nil | Pre-training, post-training, 3 months | PSS; PANAS; CDRS | Significant post-training improvements in perceived stress, positive affect, and negative affect maintained at follow up, improved resilience at follow-up compared with baseline |
| McCraty et al., 2009 [79] (Moderate-High) | 75 | Correctional officers (USA) | RCT | Psycho-educational and physiological stress management with HRV-BF (Power to Change Performance) vs. WLC | 2 days + 3mons recommended practice at work | Pre-training, 3 months post-training | Salivary cortisol and DHEA; BP; HRRest; HRV components (RMSSD, HF, LF, VLF, total power, LF/HF ratio); BSI subscales; POQA subscales | Significantly lower DHEA, BP, HR, anger and increased LF/HF HRV ratio post-training, no physiological changes, and increases in depressive symptoms in control group |
| McCraty & Atkinson, 2012 [80] (Moderate-Low) | 59 | Police officers (USA) | RCT | Psycho-educational and physiological resilience promotion stress management with HRV-BF (Coherence Advantage Program) vs. WLC | 3 × 4 h sessions | Pre-training, post-training | POQA subscales; BP and IBI during critical incident scenarios (n = 23, 12 exp, 11 ctrl) | Depression declined by 13% among trained officers while it increased by 17% in the control group. Significantly greater decrease in IBI during the post-training scenario in experimental group only. Authors contacted for HR data (SDs) and POQA baseline scores |
| Mealer et al., 2014 [81] (Moderate-Low)* | 27 | ICU nurses (USA) | RCT | Multimodal psychoeducation, mindfulness-based practice, emotional regulation vs. Nil training | 12 weeks total: 2-day workshop + 12 × 30 min weekly writing sessions + 15 min × 3/week mindfulness + 30–45min exercise × 3/week + 30–60 min counseling session | Pre-training, 1wk post-training | CDRS, PDS, HADS, MBI EE, DP, and PA subscales | Post-training reductions in depression symptoms in the experimental group. Both groups reported significant reductions in PTSD symptoms and improvements in resilience. |
| Molek-Winiarska & Żołnierczyk-Zreda, 2018 [82] (Moderate-High) | 66 | Miners (Poland) | RCT | Mindfulness-based stress management vs. Nil training | 8-h sessions × 5 weeks (40 h total) + optional homework | Pre-training, 3 months post-training | GHQ global score and anxiety and depression subscales | Significant post-training reduction in anxiety and depression scores |
| Oliver & Meier, 2009 [83] (Moderate-High) | 132 | Small-town and rural police officers and sheriffs (USA) | Prospective cohort study | Stress management | 8 h | Pre-training, post-training between 1-6mons, 7-12mons, or 13-18mons | Adult Manifest Anxiety Scale | No significant post-training reduction overall, but significant when analyzed according to post-test lag times (1-6mons, 7-12mons, 13-18mons) |
| Poulsen et al., 2015 [84] (Moderate-Low) | 70 | Radiation therapists and oncology nurses (Australia) | RCT | Stress management workshop vs. Written educational materials only | 1 day | Pre-training, 6 weeks post-training | Recovery experiences questionnaire global score and subscales | Workshop group global scores increased post-training, and 3 of 4 subscales were higher than the control group |
| Ramey et al., 2016 [85] (Moderate-Low) | 38 | Police officers (USA) | Prospective cohort study | Psycho-educational and physiological emotion regulation with HRV-BF | 2 × 2 h sessions held 2–3 weeks apart + 3mons practicing skills in the field | Pre-training, 3 months and 6 months post-training, but only a single post-training value is reported | BP; PSS; Impact of Events Scale total stress, intrusive and avoidance subscale scores; Response to Stressful Experience Scale; POQA subscales; on- and off-duty HR and HRV components (RMSSD, HF, LF, VLF, total power, LF/HF ratio), respiratory coherence on n = 26 | Below threshold (p > 0.05) improvements to anger and resentment but increases in intrusive and avoidance scores. Significant post-training changes to sympathetic (LF) and parasympathetic (HF) contributors of HRV on both work and off days, increased RMSSD on off days, and significantly increased respiratory coherence. Coherence values not reported and requested from the authors |
| Ranta, 2009 [86] (Low)* | 80 | Police officers (India) | RCT | Multimodal psychophysiological stress management vs. Relaxation only | 3 × 1 h sessions + brief home assignments vs. 1 × 1 h session | Pre-training, post-training | PSQ and CBQ global scores | Significant post-training improvements in both outcomes for the multimodal group only. SDs not provided, authors contacted. |
| Rø et al., 2010 [87] (Moderate-Low) | 153 | Nurses (Norway) | Prospective cohort study | Multimodal psychoeducational and psychophysiological retreat | 5 days | Pre-training, 12 months post-training | MBI EE, DP, and PA subscales; proportion on sick leave; preceding year number of weeks on sick leave; adverse life events | Significant reductions in MBI EE and DP 12-months post-training. Number of adverse life events not reported, authors contacted |
| Rodrigues et al., 2018 [88] (Moderate-Low) | 33 | Nurses (USA) | Prospective cohort study | Stress management coping skill building | Single 90-min group session | Pre-training, 3 months post-training | MBI EE and DP subscales | Significant reduction in EE and DP 3 months post-training |
| Steinberg et al., 2016 [89] (Moderate-Low)* | 32 | SICU personnel (USA) | RCT | Mindfulness-based intervention | 8 × 1 h weekly sessions + recommended 20-min practice × 5/week vs. Nil treatment | Pre-training, post-training | MBI EE, DP and PA subscales, ProQoL CS, BO, STS subscales, number of missed work days in past 2 months |
Work satisfaction measures were significantly correlated with some mental health subscales, but were not reported or analyzed separately in the study. M and SDs for primary outcome measures not provided, authors contacted. |
| Tveito & Eriksen, 2009 [90] (Moderate-Low) | 40 | Nursing home employees (Norway) | RCT | Multimodal stress management coping skill building (IHP) vs. WLC | 15 × 1 h weekly sessions and workplace assessment + 9 months physical exercise | Pre-training, post-training, 12 months | General Health Status Inventory SF-36 Mental Health subscale; Demand/Control Model subscales; number of days on sick leave; job stress (undefined) | No significant differences between groups post-training or 1-year follow-up |
| Villani et al., 2013 [91] (Moderate-Low) | 30 | Oncology nurses (Italy) | RCT | Web-based stress management coping skill building (M-SIT) vs. Neutral stimuli control group | 15-min video clips, 2×/week, 4 weeks (8 sessions, 2 h total) | Pre-training, post-training | STAI; COPE Active coping and Denial subscales | Significant post-training improvement on all measures for M-SIT group only |
AAQ-II Acceptance and Action Questionnaire II, ACT-SMI Acceptance and Commitment Therapy and Preventative Stress Management Intervention, AUC Area Under the Curve (Diurnal Cortisol), AUDIT Alcohol Use Disorders Identification Test, BAI Beck Anxiety Inventory, BDI Beck Depression Inventory, BO Burnout Subscale (ProQoL), BP blood pressure, BRS Brief Resilience Scale, BSI Brief Symptom Inventory, CBQ Coping Behaviour Questionnaire, CDRS Connor Davidson Resilience Scale, CES-D Center for Epidemiological Studies Depression Scale, CF Compassion Fatigue Subscale (ProQoL), CFQ Cognitive Fusion Questionnaire, COPE Brief Coping Orientation to Problems Experienced, CS Compassion Satisfaction Subscale (ProQoL), DASS Depression Anxiety Stress Scale-21, DHEA dehydroepiandrosterone-sulfate, DP Depersonalization Subscale (MBI), EE Emotional Exhaustion Subscale (MBI), ERSQ Emotion-Regulation Skills Questionnaire, EZ ERASE-Stress New Zealand, FMI Freiburg Mindfulness Inventory, GHQ General Health Questionnaire, HADS Hospital Anxiety and Depression Scale, HF high frequency, HPLP-II Health-Promoting Lifestyle Profile II, HR heart rate, HRAvg average heart rate, HRBase baseline resting heart rate, HRIndex maximum heart rate relative to resting heart rate, HRMax maximum heart rate, HRRec recovery time from maximum to resting heart rate, HRV heart rate variabilitym, HRV-BF heart rate variability biofeedback, IBI interbeat intervals, IHP Integrated Health Program, iTEC Integrative Training of Emotion-Regulation Competencies, LET Life Engagement Test, LF low frequency, LOT-R Life Orientation Test-Revised, M mean, MBI Maslach Burnout Inventory, ME medical examiner, METI Managing Emergencies and Traumatic Incidents Organizational Program, MHC-SF Mental Health Continuum Short Form, OLBI Oldenburg Burnout Inventory, PA Personal Accomplishment Subscale (MBI), PANAS Positive Affect Negative Affect Scale, Pbse Performance-based Self-esteem Scale, PCL Posttraumatic Checklist, PDS Posttraumatic Diagnostic Scale, POMS Profile of Mood States, POMS-TA POMS Tension-Anxiety Subscale, POQA Personal and Organizational Quality Assessment, PROMIS Patient Reported Outcomes Measurement Information System, ProQoL Professional Quality of Life Scale, PSQ Police Stress Questionnaire, PSS Perceived Stress Scale, RAW Resilience@Work, RCT randomized control trial, RMSSD root mean squared standard deviation, RS Resilience Scale, R2MR Road to Mental Readiness, SCL-90 Symptoms Checklist, SCS Self-Compassion Scale, SD Standard Deviation, SICU surgical intensive care unit, SLS Satisfaction with Life Scale, STAI State-Trait Anxiety Inventory, STS Secondary Traumatic Stress Subscale (ProQoL), TAU training as usual, VLF very low frequency, WLC waitlist control
Study characteristics
The 42 studies represented data from 3182 individuals. Police officers were the most common PSP group (n = 15), followed by correctional workers (n = 2), firefighters (n = 2), and paramedical students (n = 1). There were no eligible studies, including participants from other PSP sectors. FHP occupations represented included nurses (n = 11) and various groupings of FHP (n = 9), including social workers, radiologists, medical examiners, physicians, nursing home employees, Red Crescent/Red Cross personnel, physiotherapists, occupational therapists, and healthcare clerical and administrative staff. The systematic literature search also yielded two relevant studies on educational staff exposed to a PPTE [60] and on miners whose occupational roles pose a realistic and substantial life threat (e.g., workers, blasters, foremen at the mine face) [82].
PTSI mitigation program themes identified in the eligible studies overlapped heavily and are not mutually exclusive (i.e., one program may fall under multiple themes). The aggregation of programs into broader categories was conducted to perform the meta-analysis and are defined in Table 2. Program themes included mindfulness (n = 13), psychoeducation (n = 20), psychophysiology (n = 11), resilience promotion (n = 17), stress management (n = 15), building coping skills (n = 7), emotion regulation (n = 4), cognitive (behavior) therapy (n = 3), and psychosocial support or counseling (n = 2). There were 8 studies that evaluated the effectiveness of self-described “multimodal programs” that included multiple themes identified above. There were 6 studies that employed biofeedback with primary resilience promoting program types.
Study designs included RCTs (including cluster, parallel, and crossover RCTs) (n = 26) or prospective cohort studies (n = 15). Comparators included waitlist controls (i.e., offered the program at the end of the study) (n = 9), no training or occupational skills training (i.e., not mental health training) as usual (n = 11), psychoeducation only (n = 2), neutral or negatively valenced versions of the program (n = 2), or alternative control programs such as general wellness (n = 1) or Critical Incident Stress Management (n = 1). There were 7 studies that used online or web-based presentation of their programs, while 34 studies used in-person group sessions. Program durations ranged from a single 90 minute group session [88] or one-day workshop or equivalent (i.e., less than 8 hours) (n = 6) to 4- or 5-day workshops or retreats [35, 36, 40, 87]. Multiple training sessions were distributed over a minimum of two days [79] and a maximum of 9 months [90], which included 15 weeks of mental health programming within nine months of recommended physical exercise. Self-paced programs (n = 8) were predominantly web-based, and studies reported very low levels of program completion and/or adherence [62, 64, 74]. Several programs, predominantly mindfulness-based, also included optional or recommended daily practice, or “homework” (n = 19). Study duration for follow-up evaluations ranged from immediately following the training program (n = 25), 1 week to 3 months post-training (n = 16), 6 months (n = 6), 7 to 12 months (n = 8), and 13 to 18 months (n = 3). A single study with multiple follow-up durations would be included in more than one of the categories (e.g., Andersen et al. [40] conducted pre-, post-training, 6-, 12-, and 18-month evaluations).
Due to the wide variety and limited consistency in PTSI mitigation program types, outcome variables, occupational groups, and follow-up durations across studies, the meta-analysis results will be presented by outcome categories (defined in Table 3) and are summarized in Table 5. Below, we report on the effectiveness of PTSI mitigation programs on reducing symptoms of PTSI and improving general measures of psychological health and wellness. Effect sizes (SMD) and confidence intervals (CIs) will be reported for specific outcomes. Any statistically significant differences in outcomes by program type, follow-up duration, and/or occupational group will then be presented where subgroup analyses were performed. Supporting figures can be found in Additional File 2.
Table 5.
Summary of meta-analytic results, subgroup analyses, and publication biases
| Outcome | Studies | Meta-analytic results | Subgroup analyses | Publication biases | |||
|---|---|---|---|---|---|---|---|
| SMD [95% CI] | Timepoint | Program type | Occupation | Study design | Linear regression test of funnel plot asymmetry | ||
| Absenteeism | 4 | 0.01 [− 0.19; 0.21] | – | – | – | – | – |
| Alcohol | 10 | − 0.08 [− 0.21; 0.06] | – | – | – | – | – |
| Antithrombin | 1 | 0.49 [− 0.45; 1.44] | – | – | – | – | – |
| Anxiety | 21 | − 0.20 [− 0.31; − 0.10] | 0.61 | 0.31 | 0.76 | – | − 0.10 [− 0.23; 0.02], p < 0.01 * |
| Blood pressure | 8 | − 0.17 [− 0.38; 0.04] | – | – | – | – | – |
| Burnout | 15 | − 0.45 [− 0.64; − 0.26] * | 0.15 | 0.04* | 0.46 | – | − 0.28 [− 0.47; − 0.09], p = 0.07 |
| Coping | 5 | 0.41 [0.02; 0.80] * | < 0.01* | < 0.01* | < 0.01* | – | – |
| Cortisol | 6 | − 0.20 [− 0.44; 0.04] | – | – | – | – | – |
| Depression | 18 | − 0.46 [− 0.71; − 0.21] * | 0.05* | < 0.01* | 0.80 | 0.88 | − 0.17 [− 0.47; 0.12], p = 0.03 * |
| DHEA | 2 | − 0.29 [− 0.80; 0.21] | – | – | – | – | – |
| Drug use | 2 | − 0.05 [− 0.35; 0.24] | – | – | – | – | – |
| General symptoms | 7 | − 0.70 [− 1.14; − 0.26] * | < 0.01* | < 0.01* | 0.46 | – | – |
| Heart rate | 21 | − 0.27 [− 0.40; − 0.14] | 0.04* | 0.01* | 0.04* | – | − 0.23 [− 0.37; − 0.09], p = 0.10 |
| Prolactin | 1 | − 0.07 [− 0.56; 0.41] | – | – | – | – | – |
| PTSD | 9 | − 0.33 [− 0.55; − 0.11] * | < 0.01* | 0.10 | 0.03* | – | – |
| Resilience | 22 | 0.27 [0.13; 0.42] * | 0.02* | < 0.01* | 0.29 | 0.78 | 0.27 [0.13; 0.42], p = 0.62 |
| Stress | 25 | − 0.35 [− 0.51; − 0.20] * | 0.49 | 0.14 | 0.02* | 0.80 | − 0.21 [− 0.37; − 0.05], p = 0.55 |
| Suicidality | 2 | 0.33 [− 0.07; 0.73] | – | – | – | – | – |
| Well-being | 20 | 0.46 [0.26; 0.66] * | 0.63 | 0.24 | < 0.01* | 0.45 | 0.46 [0.26; 0.66], p = 0.16 |
The standardized mean difference (SMD) is a method of pooling continuous outcomes (i.e., scores on rating scales) in meta-analysis. It is preferred over mean differences when there are differences in how the outcome is measured across studies. The asterisk (*) indicates that the pooled estimate is statistically significant at p < 0.05 (i.e., the confidence interval (CI) does not overlap with the null). Subgroup analyses were only performed where at least ten studies were included. Statistically significant subgroup analyses (p < 0.05) are marked with an asterisk (*). The linear regression test of funnel plot asymmetry is used to appraise publication bias in the pooled estimate for any individual outcome in the meta-analysis. p values smaller than 0.05 (marked with an asterisk) are considered statistically significant and indicate evidence of publication bias in that outcome’s pooled estimate. DHEA, dehydroepiandrosterone; PTSD, posttraumatic stress disorder
Mental disorder symptoms and absenteeism
Depression
Significant reductions in mental disorder symptoms were observed for depression, with an SMD of − 0.46 [ − 0.71; − 0.21]. Depression effect sizes were largest for resilience promotion programs (SMD = − 1.05; p < 0.01) and immediately post-training (− 0.78) compared with follow-up (p = 0.05) (Figure 2.1 in Additional File 2).
Burnout
Moderate reductions in symptom burden were also observed for burnout (SMD = − 0.45 [− 0.64; − 0.26]), with larger effect sizes observed in resilience promotion versus multimodal programs (− 0.90 vs. − 0.24; p = 0.04) (Figure 2.2 in Additional File 2).
PTSD
Medium reductions were observed for PTSD symptoms with an SMD of − 0.33 [− 0.55; − 0.11]. Significant subgroup analyses evidenced the largest effect sizes at 8-month follow-up (− 1.22; p < 0.01), and among PPTE-exposed educators (− 0.86; p = 0.03) (Figure 2.3 in Additional File 2).
Anxiety
Small reductions were observed across all studies for anxiety symptoms, with an SMD of − 0.20 [− 0.31; − 0.10].
Suicidality
Suicidality was not significantly reduced with the programs considered (SMD = 0.33 [− 0.07; 0.73]).
Substance use
For alcohol, the overall reduction in weekly alcoholic drinks was small and not statistically significant, with an SMD of − 0.08 [− 0.21; 0.06]. The effect was even smaller for other substance use, with an SMD of − 0.05 [− 0.35; 0.24]. Given the small study yield for either outcome (Table 5), subgroup analyses were not conducted.
Absenteeism
There was no significant improvement in absenteeism—defined as the number of sick days taken by employees in the study—with an SMD of 0.01 [− 0.19; 0.21].
General measures of general psychological health, stress, resilience, and well-being
General psychological health
There was a significant medium reduction in general psychological symptom burden across studies, with an SMD of − 0.70 [− 1.14; − 0.26] (Figure 2.4 in Additional File 2). There were significant differences in effect sizes across timepoints (p < 0.01) – with small positive effects (i.e., increases in general psychological symptoms relative to pre-training) noted at 18-month follow-up (0.34) relative to large decreases in symptoms (reflected by negative effect sizes) at 1-month (− 0.95) and immediate post-training (− 0.91) timepoints—and by program type (p < 0.01), with the larger reductions associated with multimodal programs (− 1.09) relative to resilience promotion programs (0.34).
Stress
Stress symptoms were associated with small-to-medium reductions in symptom burden overall, with an SMD of − 0.35 [− 0.51; − 0.20] and larger effects among hospital staff (− 0.84) compared with police officers (− 0.29; p = 0.02).
Well-being
Among measures of broader mental health status, effect sizes were largest for well-being with a medium SMD of 0.46 [0.26; 0.66]; larger effects were observed among educators (1.95) compared with other occupational categories (p < 0.01).
Coping
There was evidence of a medium SMD of 0.41 [0.02; 0.80], with larger effect sizes at 18-months (0.93) versus other timepoints (p < 0.01), with resilience promotion programs (0.93) relative to other program themes (p < 0.01), and among police officers (0.73) and radiation therapists and nurses (0.70) relative to paramedical staff (− 0.01; p < 0.01) (Figure 2.5 in Additional File 2).
Resilience: Overall improvement in resilience was small, with an SMD of 0.27 [0.13; 0.42] (Figure 2.6 in Additional File 2). Effect sizes were largest at immediate post-test (− 0.46; p = 0.02) and larger with resilience-promoting strategies (0.98) relative to other modalities (p < 0.01).
Biological measures of stress
There was no evidence that the investigated programs reduced serum biomarkers of stress, such as cortisol, antithrombin, dehydroepiandrosterone (DHEA), and prolactin (Table 5). While there were no significant reductions in blood pressure across studies, there were significant improvements in overall and average measures of heart rate, with a small SMD of − 0.27 [− 0.40; − 0.14]. The greatest reductions in heart rate were seen at 12-months of follow-up (− 1.52, p = 0.04), with resilience promotion programs (− 1.00; p < 0.01), and among nurses (− 0.55) and police officers (− 0.45) compared with correctional officers (− 0.15; p = 0.04).
Publication bias
There was evidence of a publication bias for anxiety (p = 0.0061) and depression (p = 0.03) (Figure 2.7 in Additional File 2). The trim-and-fill method was used to account for potential outcome effect size estimate inflation (Table 5). For anxiety, the effect size changed from an SMD of − 0.20 to − 0.10 [− 0.23; 0.02]. For depression, the effect size changed from an SMD of − 0.46 to − 0.17 [− 0.47; 0.12]. For each outcome, correction for publication bias significantly reduced the effect size, meaning that anxiety and depression outcomes are likely associated with publication bias.
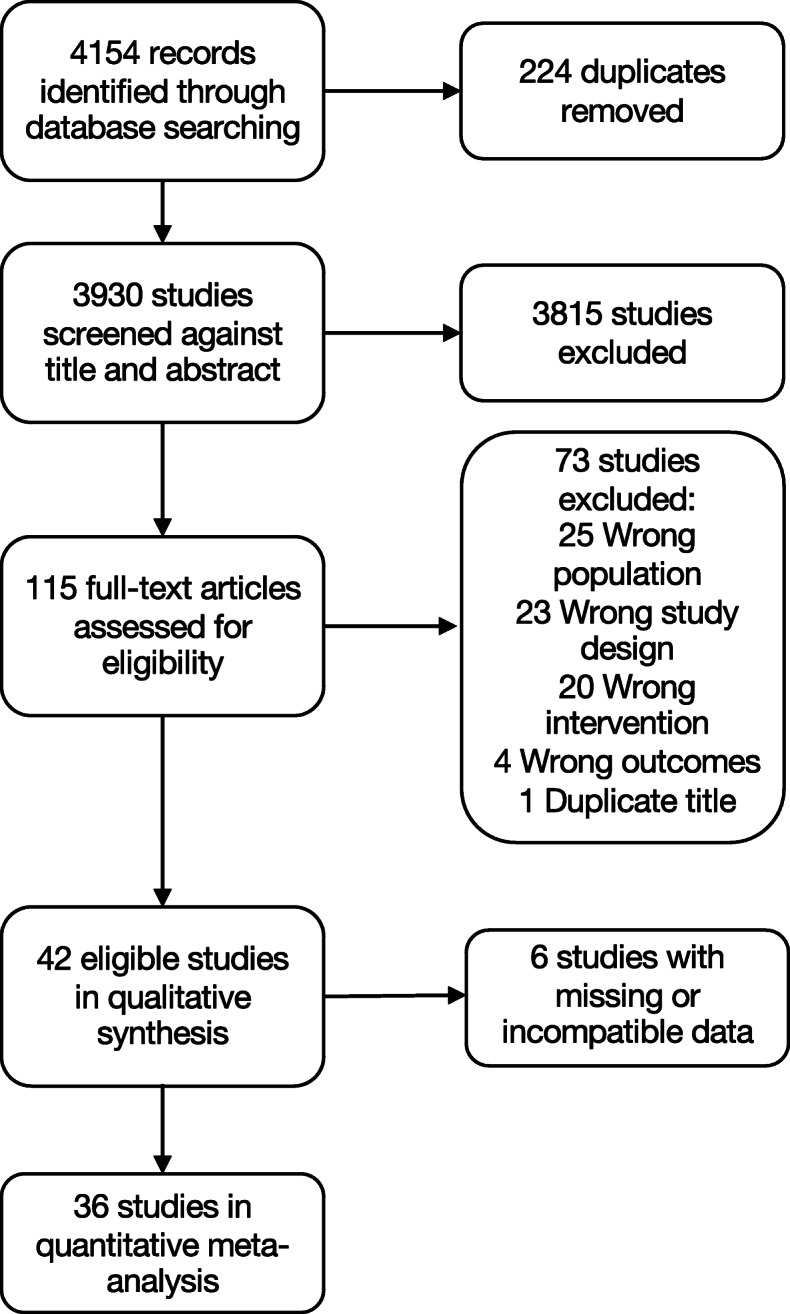
Quality assessment
Quality assessment ratings for all studies in the current systematic review are illustrated in Fig. 2. Individual study ratings are reported in Table 4, and detailed study ratings are presented in Table 3.1 in Additional File 3. Overall, only one study was of “high quality” [63], 11 were “moderate to high quality,” 24 were of “moderate to low quality,” and six were of “low quality.”
Fig. 2.
Quality assessment using Newcastle-Ottawa Scale. Full sample (n = 36 studies) summary of strength of evidence from systematic review and meta-analysis
Outcome
All studies were rated at low risk of bias because all used empirically validated self-report mental disorder screening tools or objective physiological data. There were 14 studies that were rated at high risk of bias for follow-up periods; outcomes were only assessed immediately after program delivery, prohibiting evaluations of program effectiveness following subsequent occupational exposures to PPTE. Concerning adequacy of follow-up, more than half of all studies (n = 25) received high risk of bias ratings for either failing to report post-training sample sizes and any possible participant attrition and/or failing to provide analyses of retained participants to those lost at follow-up.
Selection
All but seven studies were rated at a high risk of selection bias for failing to demonstrate sample representativeness, limiting results’ generalizability. All studies were rated at a low risk of bias due to clear selection criteria for control groups except for one sample from a different police district [85]. Most studies adequately ascertained participation in the programming being assessed (n = 34); however, three studies were either unclear about program completion or participation [68, 77, 86] and five studies of self-paced online programs reported very low participation or completion [62, 64, 74–76].
Comparability
The purpose of the current systematic review was to identify the effectiveness of proactive psychological programs designed to mitigate PTSI and limit the decline of psychological symptoms among workers at high risk of exposure to a PPTE. Therefore, studies that included individuals with diagnosed PTSI or mental health disorders were excluded at the title and abstract screening phase, as these would be considered PTSI treatments or services. Accordingly, the comparability criterion pertains to controlling for the most important factor in the study design, which in the case of the current review is the presence of a pre-existing PTSI (i.e., before program onset) and/or exposure to a PPTE following program onset, both of which would significantly confound investigations of program effectiveness. Only 12 of the included studies received a low risk of bias rating for the comparability criterion, either reporting or controlling for mental disorder symptom severity at baseline or pre-training measures, or by reporting PPTE exposures following program onset and before any follow-up evaluations. All remaining studies (n = 25) were at a high risk of bias.
Conversely, all but five studies received a low-risk rating for demonstrating that the outcome of interest was not present at the start of the study by providing pre-training baseline measures for reported outcomes. Roughly half of the eligible studies (n = 22) controlled an additional factor in the study design or analysis, including age or years of service/employment, which are known correlates of mental health among PSP and FHP [4, 14, 92].
Discussion
The effectiveness of various organizational programs designed to “prevent”—or more accurately to proactively mitigate—PTSI and improve psychological health indicators among PPTE-exposed occupational groups remains unclear. The current systematic review identified 42 empirical research studies measuring the effectiveness of organizational training programs designed to proactively mitigate PTSI among PSP, FHP, and other workers exposed to PPTEs (Table 4). A great deal of heterogeneity was indicated across program themes and durations and study designs, durations, and follow-up periods. Self-directed or web-based programs also suffered from poor participant adherence and completion. The quality assessment indicated a high risk of reporting bias for several study elements (Fig. 2), including failure to demonstrate sample representativeness (83% of studies), evaluate or report on the presence of a PTSI and/or mental disorder before the study and program onset, and/or participant exposure to PPTEs before follow-up evaluations (71%). The identified factors would significantly confound investigations of program effectiveness and limit the generalizability of results. Most studies also reported high attrition rates at follow-up evaluations (60%), and several collected post-training measures before the newly acquired skills could be practiced or applied in work conditions (33%).
Evaluation of 36 study outcomes with a quantitative meta-analysis provide evidence that all programs (i.e., collapsed across program type) resulted in statistically significant reductions in PTSI after training (Table 5), including symptoms of general psychological health, depression, burnout, stress, PTSD, and anxiety, as well as significant improvements in measures of well-being, coping, and resilience (see Tables 2 and 3 for operational definitions of program types and outcomes, respectively). Consistent with previous literature [13, 41, 42], post-training improvements are of a medium (SMD < 0.8) or small (SMD < 0.5) effects in magnitude and time-limited. Subgroup analyses indicated large (SMD > 0.8) effect sizes for sustained improvements in PTSD symptoms and coping for up to 18 months. Resilience promotion programs appeared to reduce symptoms of depression and burnout and improved coping and resilience measures. Multimodal programs that combined therapeutic approaches (e.g., mindfulness, stress management, emotion regulation, resilience promotion) appeared to improve measures of general psychological health. Police appeared to report the greatest improvement in coping measures, likely due to the overrepresentation of this population across studies (n = 15). In contrast, combined groups of FHP indicated the greatest reduction in stress symptoms, and PPTE-exposed educational staff indicated the greatest decrease in PTSI symptoms [61]. Significant and sustained improvements in coping may be promising, but coping is not yet a clinically validated construct for PTSI. Similarly, wellness and resilience are general health indicators that vary in operational and theoretical definitions between individual studies. Substantial barriers to evaluating program effectiveness identified in the current review include inconsistency in outcome measures, outcome reporting (i.e., mean and standard deviation values required for meta-analysis), and follow-up durations across studies. The limitations precluded more detailed subgroup analyses and data synthesis for the current meta-analysis.
Despite claims for reduced absenteeism as a justification for funding and implementation of mental disorder “prevention” programs, evidence provided by the current meta-analysis does not support reduced absenteeism due to inconsistent or insufficient reporting, and especially for distinguishing missed work as a result of a psychological injury sustained at work or due to physical illness. Similarly, the results did not evidence statistically significant reductions in substance use or suicidality, both of which are prevalent among PSP [4, 14, 21] but remain under-investigated among FHP and other at-risk workers. There was also no evidence for post-training improvements in physiological biomarkers of stress except for heart rate (Table 5), which was the third most common outcome measure and included several studies that condition adaptive through heart rate variability biofeedback training (HRV-BF). Despite the limited evidence supporting the effectiveness of HRV-BF as a possible tool for modulating stress physiology, doing so requires substantial resources such as medical-grade cardiovascular equipment, software, repeated training sessions, and qualified personnel psychophysiology to guide psychoeducational modules [35, 36, 40, 79, 80].
The studies identified by the current systematic literature review provide modest evidence for very time-limited improvements in several PTSI symptoms. Variability in program types and durations also represents variability in organizational cost and feasibility, which place limitations on implementing and repeated investigation of PTSI mitigation program effectiveness either separate from or part of a longitudinal research study (see also [93]). Web-based or self-directed programs may be considered more cost-effective to implement than multiple in-person group sessions; however, the current systematic review results demonstrate a critical and substantial lack of adherence, as well as very low completion rates for several online program protocols [62, 64, 74–76]. Inconsistent and poor-quality study designs precluded more conclusive recommendations directed at organizational stakeholders to inform PTSI mitigation programming or training tailored to PSP and FHP.
Limitations
Despite a relatively high number of eligible studies (n = 42), the main limitation of the current systematic review is the high heterogeneity across studies, which precluded the inclusion of six studies in a quantitative meta-analysis and more detailed subgroup analyses. The quality of available studies was also highly variable (Fig. 2 and Table 3.1 in Additional File 3), with 71% (30 of 42) of studies scoring moderate to low quality (≤ 6 out of 9). The geographical variability of participants also makes generalizability difficult because an effective program in one political, cultural, social, economic, and epidemiological context may not be relevant, applicable, or effective elsewhere. Nevertheless, the substantial impact of PPTE exposures on the mental health of PSP and FHP appears broadly accepted, as does the need to develop effective evidence-based PTSI mitigation programming for all at-risk workers to minimize personal, social, and economic costs [26, 29].
Publication bias was high for studies with outcome measures assessing anxiety and depression, and adjustments for methods biases rendered the results no longer statistically significant (Table 5). As smaller trials are generally analyzed with less methodological rigor than larger ones, the resulting asymmetrical funnel plot suggested that selective reporting may have led to an overestimation of effect sizes in smaller trials (Figure 2.7 in Additional File 2). Other limitations included the search strategy and criteria process (Table 1), which was restricted to English- and French-language studies published after 2008 from five indexed electronic databases.
Conclusions
Especially during the current global coronavirus pandemic, there is an urgent need to identify effective organizational training tailored for PSP and FHP and designed to mitigate the psychological impact of PTSI that can result from occupational PPTE exposures [26, 29]. The extant literature identified by the current systematic literature review indicates broad variety in sampled occupational populations, implemented programming approaches, and measured outcome variables. Heterogeneity across studies precludes identifying a proactive PTSI mitigation program type that is superior to others and effective for diverse PSP, FHP, and other at-risk workers exposed to PPTE. Nonetheless, we have synthesized the available evidence on proactive programming effectiveness in reducing specific PTSI symptoms. Based on our meta-analytic results, resilience promotion and multimodal programs that combine a variety of therapeutic and skill-building approaches appear to produce modest time-limited reductions in symptoms of general psychological health, depression, burnout, stress, PTSD, and anxiety, as well as promoting well-being, adaptive coping, and resilience. By identifying significant research gaps and practical study limitations, we intend to help inform future high-quality research evaluating program effectiveness within the context of PSP and FHP working environments. The current results provide organizational stakeholders and policymakers with numerous options for developing innovative mental health solutions tailored to the unique occupational challenges faced by those who serve to maintain and protect public health and safety.
Supplementary Information
Acknowledgements
The authors would like to acknowledge Dr. Vivien Lee, Dr. Don McCreary, and Dr. Dan Bilsker for their thoughtful reviews on early versions of the current manuscript.
Abbreviations
- DHEA
Dehydroepiandrosterone
- FHP
Frontline healthcare professional
- HRV-BF
Heart rate variability biofeedback
- PPTE
Potentially psychologically traumatic event
- PSP
Public safety personnel
- PTSD
Posttraumatic stress disorder
- PTSI
Posttraumatic stress injury
- SMD
Standardized mean difference
Authors’ contributions
PMD conducted the systematic literature reviews, data extraction for meta-analytic data, quality assessment, and was the primary contributor in writing the manuscript; AB registered the systematic review, performed the meta-analyses, provided major contributions to the methods and results sections, and data interpretation; DG and RNC contributed significantly to the theoretical definitions and literature in the introduction, methods, and discussion, and to data interpretation; GSA is responsible for study conception and design, and contributed significantly to verification of extracted data, quality assessment, and all sections of the manuscript. All authors read and approved the final manuscript.
Authors’ information
PMD was a postdoctoral fellow in the Office of Applied Research and Graduate Studies at the Justice Institute of British Columbia at the time of this work.
Funding
This research is supported by funds awarded to G. Anderson from WorkSafeBC (RS2019-SP13), who was Dean of Applied Research and Graduate Studies at the Justice Institute of British Columbia at the time of receiving funding. WorkSafeBC had no role in the design of the study, collection, analysis, and interpretation of data, nor in writing the manuscript. The views, results, opinions, and conclusions expressed herein do not necessarily represent the views of WorkSafeBC.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Paula M. Di Nota, Email: paula.dinota@utoronto.ca
Anees Bahji, Email: anees.bahji1@ucalgary.ca.
Dianne Groll, Email: grolld@queensu.ca.
R. Nicholas Carleton, Email: nick.carleton@uregina.ca.
Gregory S. Anderson, Email: ganderson@tru.ca
References
- 1.Canadian Institute for Public Safety Research and Treatment (CIPSRT): Glossary of terms: a shared understanding of the common terms used to describe psychological trauma (version 2.0). http://hdl.handle.net/10294/9055 (2019). Accessed 23 October 2020.
- 2.Carleton RN, Afifi TO, Taillieu T, et al. Exposures to potentially traumatic events among public safety personnel in Canada. Can J Behav Sci. 2019;51(1):37–52. https://doi.org/10.1037/cbs0000115.
- 3.Shi L, Wang L, Jia X, Li Z, Mu H, Liu X, et al. Prevalence and correlates of symptoms of post-traumatic stress disorder among Chinese healthcare workers exposed to physical violence: a cross-sectional study. BMJ Open. 2017;7(7):e016810. doi: 10.1136/bmjopen-2017-016810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carleton RN, Afifi TO, Turner S, et al. Mental disorder symptoms among public safety personnel in Canada. Can J Psychiatry Rev Can Psychiatr. 2018;63(1):54–64. https://doi.org/10.1177/0706743717723825. [DOI] [PMC free article] [PubMed]
- 5.Robertson N, Perry A. Institutionally based health care workers’ exposure to traumatogenic events: systematic review of PTSD presentation. J Trauma Stress. 2010;23(3):417–420. https://doi.org/10.1002/jts.20537. [DOI] [PubMed]
- 6.Dragano N, Lunau T, Eikemo TA, Toch-Marquardt M, van der Wel KA, Bambra C. Who knows the risk? A multilevel study of systematic variations in work-related safety knowledge in the European workforce. Occup Environ Med. 2015;72(8):553–559. doi: 10.1136/oemed-2014-102402. [DOI] [PubMed] [Google Scholar]
- 7.Tamers SL, Chosewood LC, Childress A, Hudson H, Nigam J, Chang CC. Total worker health® 2014–2018: the novel approach to worker safety, health, and well-being evolves. Int J Environ Res Public Health. 2019;16(3):321. doi: 10.3390/ijerph16030321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chirico F, Heponiemi T, Pavlova M, Zaffina S, Magnavita N. Psychosocial risk prevention in a global occupational health perspective. A descriptive analysis. International journal of environmental research and public health. 2019 16(14):2470. doi: 10.3390/ijerph16142470. [DOI] [PMC free article] [PubMed]
- 9.Chirico F, Nucera G, Magnavita N. Protecting the mental health of healthcare workers during the COVID-19 emergency. BJPsych International. 2021 18(1). doi: 10.1192/bji.2020.39
- 10.Spoorthy MS, Pratapa SK, Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic–a review. Asian J Psychiatr. 2020;51:102119. https://doi.org/10.1016/j.ajp.2020.102119. [DOI] [PMC free article] [PubMed]
- 11.Vujanovic AA, Lebeaut A, Leonard S. Exploring the impact of the COVID-19 pandemic on the mental health of first responders. Cogn Behav Ther. 2021;19:1–6. https://doi.org/10.1080/16506073.2021.1874506. [DOI] [PubMed]
- 12.Carleton RN, Afifi TO, Taillieu T, et al. Assessing the relative impact of diverse stressors among public safety personnel. Int J Environ Res Public Health 2020; https://doi.org/10.3390/ijerph17041234, 17, 4. [DOI] [PMC free article] [PubMed]
- 13.Carleton RN, Afifi TO, Turner S, et al. Mental health training, attitudes toward support, and screening positive for mental disorders. Cogn Behav Ther. 2019:1–19. [DOI] [PubMed]
- 14.Carleton RN, Afifi TO, Turner S, et al. Suicidal ideation, plans, and attempts among public safety personnel in Canada. Can Psy. 2018;59(3):220–231. http://dx.doi.org/10.1037/cap0000136.
- 15.Stanley IH, Hom MA, Joiner TE. A systematic review of suicidal thoughts and behaviors among police officers, firefighters, EMTs, and paramedics. Clin Psychol Rev. 2016:4425–44. [DOI] [PubMed]
- 16.Canadian Federation of Nurses Unions. Enough is enough: putting a stop to violence in the health care sector. https://nursesunions.ca/research/enough-is-enough-safe-workplaces-for-all/. 2017. Accessed 23 October 2020.
- 17.Mealer M, Burnham EL, Goode CJ, Rothbaum B, Moss M. The prevalence and impact of post traumatic stress disorder and burnout syndrome in nurses. Depression and Anxiety. 2009;26(12):1118–1126. doi: 10.1002/da.20631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pines A, Maslach C. Characteristics of staff burnout in mental health settings. Psychiatr Serv. 1978;29(4):233–237. doi: 10.1176/ps.29.4.233. [DOI] [PubMed] [Google Scholar]
- 19.Chirico F. Is burnout a syndrome or an occupational disease? Instructions for occupational physicians. Epidemiologia e prevenzione. 2017 Sep 1;41(5-6):294-8. doi: 10.19191/EP17.5-6.P294.089. [DOI] [PubMed]
- 20.World Health Organization. International classification of diseases for mortality and morbidity statistics (11th Revision). 2018.
- 21.Di Nota PM, Anderson GS, Ricciardelli R, et al. Mental disorder symptoms and suicidal ideation among police in Canada. Occup Med. 2020;70(3):183–190. https://doi.org/10.1093/occmed/kqaa026. [DOI] [PMC free article] [PubMed]
- 22.The Lancet The plight of essential workers during the COVID-19 pandemic. Lancet. 2020;395(10237):1587. doi: 10.1016/S0140-6736(20)31200-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Donoghue AM. Occupational health hazards in mining: an overview. Occup Med. 2004;54(5):283–289. https://doi.org/10.1093/occmed/kqh072. [DOI] [PubMed]
- 24.Anderson GS, Litzenberger R, Plecas D. Physical evidence of police officer stress. Polic Int J Police Strateg Manag. 2002;25(2):399–420. doi: 10.1108/13639510210429437. [DOI] [Google Scholar]
- 25.Iacobucci F. Police encounters with people in crisis: an independent review conducted by the Honourable Frank Iacobucci for Chief of Police William Blair. Toronto Police Service. 2014. https://www.torontopolice.on.ca/publications/files/reports/police_encounters_with_people_in_crisis_2014.pdf. Accessed 23 October 2020.
- 26.Oliphant R. Healthy minds, safe communities: supporting our public safety officers through a national strategy for operational stress injuries. Canadian House of Commons. 2016; https://www.ourcommons.ca/Content/Committee/421/SECU/Reports/RP8457704/securp05/securp05-e.pdf. .
- 27.Mercer: How much are you losing to absenteeism? https://www.mercer.ca/en/our-thinking/how-much-are-you-losing-to-absenteeism.html (2018) Accessed 23 October 2020.
- 28.Wilson S, Guliani H, Boichev G. On the economics of post-traumatic stress disorder among first responders in Canada. J Community Saf Well-Being. 2016;1(2):26–31. doi: 10.35502/jcswb.6. [DOI] [Google Scholar]
- 29.Weiss S. Update on post-traumatic stress research. Canadian Institutes for Health Research. https://cihr-irsc.gc.ca/e/51386.html. 2019. Accessed 23 October 2020.
- 30.Gimeno D, Benavides FG, Amick BC, Benach J, Martínez JM. Psychosocial factors and work related sickness absence among permanent and non-permanent employees. J Epidemiol Community Health. 2004;58(10):870–876. doi: 10.1136/jech.2003.016634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ho JT. Corporate wellness programmes in Singapore: effect on stress, satisfaction and absenteeism. J Manag Psychol. 1997;12(3):177–189. doi: 10.1108/02683949710174801. [DOI] [Google Scholar]
- 32.Anderson GS, Vaughan AD, Mills S. Building personal resilience in paramedic students. J Community Saf Well-Being. 2017;2(2):51–54. doi: 10.35502/jcswb.44. [DOI] [Google Scholar]
- 33.Vaughan AD, Stoliker BE, Anderson GS. Building personal resilience in primary care paramedic students, and subsequent skill decay. Aust J Paramedicine. 2020;16:17(1). [Google Scholar]
- 34.Anderson GS, Black J, Vaughan AD. Researching resilience in bachelor of science in nursing (BScN) students. Int J Cross-Discip Subj Educ. 2019;10(3):4098–4102. [Google Scholar]
- 35.Andersen JP, Papazoglou K, Koskelainen M, et al. Applying resilience promotion training among special forces police officers. SAGE Open. 2015;5(2):2158244015590446. doi: 10.1177/2158244015590446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Andersen JP, Gustafsberg H. A training method to improve police use of force decision making: a randomized controlled trial. SAGE Open. 2016:1–13.
- 37.Fikretoglu D, Liu A, Nazarov A, Blackler K. A group randomized control trial to test the efficacy of the road to mental readiness (R2MR) program among Canadian military recruits. BMC Psychiatry. 2019;19(1):326. doi: 10.1186/s12888-019-2287-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Carleton RN, Korol S, Mason JE, Hozempa K, Anderson GS, Jones NA, et al. A longitudinal assessment of the road to mental readiness training among municipal police. Cogn Behav Ther. 2018;47(6):508–528. doi: 10.1080/16506073.2018.1475504. [DOI] [PubMed] [Google Scholar]
- 39.Anderson GS, Di Nota PM, Metz GA, Andersen JP. The impact of acute stress physiology on skilled motor performance: implications for policing. Front Psychol. 2019;10:2501. doi: 10.3389/fpsyg.2019.02501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Andersen JP, Di Nota PM, Beston B, et al. Reducing lethal force errors by modulating police physiology. J Occup Environ Med. 2018;60(10):867–874. doi: 10.1097/JOM.0000000000001401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Anderson GS, Di Nota PM, Groll D, et al. Peer support and crisis-focused psychological interventions designed to mitigate post-traumatic stress injuries among public safety and frontline healthcare personnel: a systematic review. Int J Environ Res Public Health. 2020;17(20). 10.3390/ijerph17207645. [DOI] [PMC free article] [PubMed]
- 42.Beshai S, Carleton RN. Peer Support and crisis-focused psychological intervention programs in Canadian first responders: blue paper. Regina: University of Regina. 2016. https://www.justiceandsafety.ca/rsu_docs/blue_paper_full_web_final_production_aug_16_2016.pdf. Accessed 23 October 2020.
- 43.McCreary D. Veteran and first responder mental ill health and suicide prevention: a scoping review of prevention and early intervention programs used in Canada, Australia, New Zealand, Ireland, and the United Kingdom. Donald McCreary Scientific Consulting: Canada; 2019. [Google Scholar]
- 44.National Institute for Health Research. PROSPERO international prospective register of systematic reviews. 2019. https://www.crd.york.ac.uk/prospero/. Accessed 23 October 2020.
- 45.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 46.Veritas Health Innovation. Covidence systematic review software. Melbourne, Australia. 2019. https://www.covidence.org/. Accessed 23 October 2020.
- 47.Wells G, Shea B, O’Connell D, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Canada: the Ottawa Hospital Research Institute 2019. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. .
- 48.Cohen J. Statistical power analysis for the behavioural sciences. 2. L. Erlbaum Associates: Hillsdale, NJ; 1988. [Google Scholar]
- 49.Faraone SV. Interpreting estimates of treatment effects. Pharm Ther. 2008;33(12):700–711. [PMC free article] [PubMed] [Google Scholar]
- 50.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 51.Kang EY, Park Y, Li X, et al. ForestPMPlot: A flexible tool for visualizing heterogeneity between studies in meta-analysis. G3 Bethesda Md 2016;6(7):1793–1798. [DOI] [PMC free article] [PubMed]
- 52.Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–463. doi: 10.1111/j.0006-341X.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 53.Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–1101. doi: 10.2307/2533446. [DOI] [PubMed] [Google Scholar]
- 55.Alexander GK, Rollins K, Walker D, Wong L, Pennings J. Yoga for self-care and burnout prevention among nurses. Workplace Health Saf. 2015;63(10):462–471. doi: 10.1177/2165079915596102. [DOI] [PubMed] [Google Scholar]
- 56.Arble E, Lumley MA, Pole N, Blessman J, Arnetz BB. Refinement and preliminary testing of an imagery-based program to improve coping and performance and prevent trauma among urban police officers. J Police Crim Psychol. 2017;32(1):1–10. doi: 10.1007/s11896-016-9191-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Arnetz BB, Nevedal DC, Lumley MA, Backman L, Lublin A. Trauma resilience training for police: psychophysiological and performance effects. J Police Crim Psychol. 2009;24(1):1–9. doi: 10.1007/s11896-008-9030-y. [DOI] [Google Scholar]
- 58.Arnetz BB, Arble E, Backman L, Lynch A, Lublin A. Assessment of a prevention program for work-related stress among urban police officers. Int Arch Occup Environ Health. 2013;86(1):79–88. doi: 10.1007/s00420-012-0748-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bademci HO, Karadayi EF, Pur Karabulut IG, et al. Who is the helper? Who is being helped? The benefits of psychosocial support to correctional officers in Turkey. Psychodyn Pract Individ Groups Organ. 2016;22(4):351–365. [Google Scholar]
- 60.Berger R, Abu-Raiya H, Benatov J. Reducing primary and secondary traumatic stress symptoms among educators by training them to deliver a resiliency program (ERASE-stress) following the Christchurch earthquake in New Zealand. Am J Orthop. 2016;86(2):236–251. doi: 10.1037/ort0000153. [DOI] [PubMed] [Google Scholar]
- 61.Berking M, Meier C, Wupperman P. Enhancing emotion-regulation skills in police officers: results of a pilot controlled study. Behav Ther. 2010;41(3):329–339. doi: 10.1016/j.beth.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 62.Bolier L, Ketelaar SM, Nieuwenhuijsen K, Smeets O, Gärtner FR, Sluiter JK. Workplace mental health promotion online to enhance well-being of nurses and allied health professionals: a cluster-randomized controlled trial. Internet Interv. 2014;1(4):196–204. doi: 10.1016/j.invent.2014.10.002. [DOI] [Google Scholar]
- 63.Brinkborg H, Michanek J, Hesser H, Berglund G. Acceptance and commitment therapy for the treatment of stress among social workers: a randomized controlled trial. Behav Res Ther. 2011;49(6–7):389–398. doi: 10.1016/j.brat.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 64.Brondolo E, Kaur A, Brondolo TJ, et al. Development of a web-based scalable intervention to reduce mental health risks in medical examiner personnel. TPM-Test Psychom Methodol Appl Psychol. 2017;24(3):409–421. [Google Scholar]
- 65.Cheng S-T, Tsui PK, Lam JHM. Improving mental health in health care practitioners: randomized controlled trial of a gratitude intervention. J Consult Clin Psychol. 2015;83(1):177–186. doi: 10.1037/a0037895. [DOI] [PubMed] [Google Scholar]
- 66.Chongruksa D, Parinyapol P, Sawatsri S, Pansomboon C. Efficacy of eclectic group counseling in addressing stress among Thai police officers in terrorist situations. Couns Psychol Q. 2012;25(1):83–96. doi: 10.1080/09515070.2012.666424. [DOI] [Google Scholar]
- 67.Christopher MS, Goerling RJ, Rogers BS, Hunsinger M, Baron G, Bergman AL, et al. A pilot study evaluating the effectiveness of a mindfulness-based intervention on cortisol awakening response and health outcomes among law enforcement officers. J Police Crim Psychol. 2016;31(1):15–28. doi: 10.1007/s11896-015-9161-x. [DOI] [Google Scholar]
- 68.Christopher MS, Hunsinger M, Goerling LRJ, et al. Mindfulness-based resilience training to reduce health risk, stress reactivity, and aggression among law enforcement officers: a feasibility and preliminary efficacy trial. Psychiatry Res. 2018:264104–15. [DOI] [PMC free article] [PubMed]
- 69.Craigie M, Slatyer S, Hegney D, Osseiran-Moisson R, Gentry E, Davis S, et al. A pilot evaluation of a mindful self-care and resiliency (MSCR) intervention for nurses. Mindfulness. 2016;7(3):764–774. doi: 10.1007/s12671-016-0516-x. [DOI] [Google Scholar]
- 70.Daigle S, Talbot F, French DJ. Mindfulness-based stress reduction training yields improvements in well-being and rates of perceived nursing errors among hospital nurses. J Adv Nurs. 2018;74(10):2427–2430. doi: 10.1111/jan.13729. [DOI] [PubMed] [Google Scholar]
- 71.Duarte J, Pinto-Gouveia J. Mindfulness, self-compassion and psychological inflexibility mediate the effects of a mindfulness-based intervention in a sample of oncology nurses. J Context Behav Sci. 2017;6(2):125–133. doi: 10.1016/j.jcbs.2017.03.002. [DOI] [Google Scholar]
- 72.Duchemin AM, Steinberg BA, Marks DR, Vanover K, Klatt M. A small randomized pilot study of a workplace mindfulness-based intervention for surgical intensive care unit personnel: effects on salivary α-amylase levels. J Occup Environ Med. 2015;57(4):393–399. doi: 10.1097/JOM.0000000000000371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Flarity K, Gentry JE, Mesnikoff N. The effectiveness of an educational program on preventing and treating compassion fatigue in emergency nurses. Adv Emerg Nursing J. 2013;35(3):247–258. doi: 10.1097/TME.0b013e31829b726f. [DOI] [PubMed] [Google Scholar]
- 74.Hersch RK, Cook RF, Deitz DK, et al. Reducing nurses’ stress: a randomized controlled trial of a web-based stress management program for nurses. Appl Nurs Res. 2016:3218–25. [DOI] [PMC free article] [PubMed]
- 75.Joyce S, Shand F, Bryant RA, Lal TJ, Harvey SB. Mindfulness-based resilience training in the workplace: pilot study of the internet-based resilience@work (RAW) mindfulness program. J Med Int Res. 2018;20(9):e10326. doi: 10.2196/10326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Joyce S, Shand F, Lal TJ, Mott B, Bryant RA, Harvey SB. Resilience at work mindfulness program: results from a cluster randomized controlled trial with first responders. J Med Int Res. 2019;21(2):e12894. doi: 10.2196/12894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Larijani HA, Garmaroudi G. Effectiveness of resiliency training the mental health of the red crescent health care teams. Rev Romaneasca Pentru Educ Multidimens. 2018;10(1):64–83. [Google Scholar]
- 78.Lin L, He G, Yan J, Gu C, Xie J. The effects of a modified mindfulness-based stress reduction program for nurses: a randomized controlled trial. Workplace Health Saf. 2019;67(3):111–122. doi: 10.1177/2165079918801633. [DOI] [PubMed] [Google Scholar]
- 79.McCraty R, Atkinson M, Lipsenthal L, Arguelles L. New hope for correctional officers: an innovative program for reducing stress and health risks. Appl Psychophysiol Biofeedback. 2009;34(4):251–272. doi: 10.1007/s10484-009-9087-0. [DOI] [PubMed] [Google Scholar]
- 80.McCraty R, Atkinson M. Resilience training program reduces physiological and psychological stress in police officers. Glob Adv Health Med. 2012;1(5):42–64. doi: 10.7453/gahmj.2012.1.5.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mealer M, Conrad D, Evans J, Jooste K, Solyntjes J, Rothbaum B, et al. Feasibility and acceptability of a resilience training program for intensive care unit nurses. Am J Crit Care. 2014;23(6):e97–e105. doi: 10.4037/ajcc2014747. [DOI] [PubMed] [Google Scholar]
- 82.Molek-Winiarska D, Żołnierczyk-Zreda D. Application of mindfulness-based stress reduction to a stress management intervention in a study of a mining sector company. Int J Occup Saf Ergon. 2018;24(4):546–556. doi: 10.1080/10803548.2018.1452843. [DOI] [PubMed] [Google Scholar]
- 83.Oliver WM, Meier C. Considering the efficacy of stress management education on small-town and rural police. Applied Psychology in Criminal Justice. 2009;1:5(1). [Google Scholar]
- 84.Poulsen AA, Sharpley CF, Baumann KC, Henderson J, Poulsen MG. Evaluation of the effect of a 1-day interventional workshop on recovery from job stress for radiation therapists and oncology nurses: a randomised trial. J Med Imaging Radiat Oncol. 2015;59(4):491–498. doi: 10.1111/1754-9485.12322. [DOI] [PubMed] [Google Scholar]
- 85.Ramey SL, Perkhounkova Y, Hein M, Chung S, Franke WD, Anderson AA. Building resilience in an urban police department. J Occup Env Med. 2016;58(8):796–804. doi: 10.1097/JOM.0000000000000791. [DOI] [PubMed] [Google Scholar]
- 86.Ranta RS. Management of stress and coping behaviour of police personnel through Indian psychological techniques. J Indian Acad Appl Psychol. 2009;35(1):47–53. [Google Scholar]
- 87.Rø KEI, Gude T, Tyssen R, et al. A self-referral preventive intervention for burnout among Norwegian nurses: one-year follow-up study. Patient Educ Couns. 2010;78(2):191–197. doi: 10.1016/j.pec.2009.07.008. [DOI] [PubMed] [Google Scholar]
- 88.Rodrigues NP, Cohen LL, McQuarrie SC, et al. Burnout in nurses working with youth with chronic pain: a pilot intervention. J Pediatr Psychol. 2018;43(4):382–391. doi: 10.1093/jpepsy/jsx132. [DOI] [PubMed] [Google Scholar]
- 89.Steinberg BA, Klatt M, Duchemin AM. Feasibility of a mindfulness-based intervention for surgical intensive care unit personnel. Am J Crit Care Off Publ Am Assoc Crit-Care Nurses. 2016;26(1):10–18. doi: 10.4037/ajcc2017444. [DOI] [PubMed] [Google Scholar]
- 90.Tveito TH, Eriksen HR. Integrated health programme: a workplace randomized controlled trial. J Adv Nurs. 2009;65(1):110–119. doi: 10.1111/j.1365-2648.2008.04846.x. [DOI] [PubMed] [Google Scholar]
- 91.Villani D, Grassi A, Cognetta C, Toniolo D, Cipresso P, Riva G. Self-help stress management training through mobile phones: an experience with oncology nurses. Psychol Serv. 2013;10(3):315–322. doi: 10.1037/a0026459. [DOI] [PubMed] [Google Scholar]
- 92.Humpel N, Caputi P. Exploring the relationship between work stress, years of experience and emotional competency using a sample of Australian mental health nurses. J Psychiatr Ment Health Nurs. 2001;8(5):399–403. doi: 10.1046/j.1365-2850.2001.00409.x. [DOI] [PubMed] [Google Scholar]
- 93.Andersen J, Collins P. A longitudinal, within-subjects intervention study to reduce lethal force errors: psychophysiological research with police officers. SAGE Research Methods Cases Part 2. 2020; DOI: 10.4135/9781529715415.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.