Abstract
[Purpose] This study aimed to investigate the relationships among the changes in iliopsoas muscle thickness, hip angle, and lower limb joint moment during squatting in different pelvic positions to help in performing hip-dominant squatting exercises. [Participants and Methods] The participants were seven healthy adult males. The measurement task consisted of squatting with 60 degrees of knee flexion in three positions: the anterior, neutral, and posterior pelvic tilt positions. The iliopsoas muscle thickness was measured in the center of the inguinal region using ultrasonography. A three-dimensional motion analysis system was used to measure the joint angles and joint moments. [Results] There were no significant differences in pelvic angles between the pelvic positions. The hip angle differences were significantly higher in the anterior and neutral pelvic tilt positions compared to those in the posterior tilt position. Only the anterior pelvic tilt position had a significantly positive correlation with iliopsoas muscle thickness and hip angle differences. [Conclusion] Squatting in the neutral or posterior pelvic tilt position was not associated with hip angle and iliopsoas muscle thickness changes, whereas squatting in an anterior pelvic tilt position was associated with changes in the iliopsoas muscle thickness and hip flexion angle. Our findings suggest that activation of the iliopsoas muscle might be necessary to promote hip-dominant squatting.
Key words: Squats, Iliopsoas muscle, Pelvic position
INTRODUCTION
Hip and lumbar movements are intimately interconnected and closely coordinated, and the association between hip and lumbar motion is widely known as the lumbopelvic rhythm1, 2) and pelvifemoral rhythm3) via the pelvis. Failure of the lumbopelvic rhythm or pelvifemoral rhythm results in excessive loading of the lumbar and hip joints, leading to injury4, 5). Individuals with a history of low back pain have been reported to have greater lumbar motion relative to the hip joint6, 7), and the evaluation and treatment of low back pain often focuses on lumbar and hip motion in terms of lumbar loading. “Waiters bow” and “Backwards rocking” are used not only as tests for observing lumbar and hip movement strategies but also as exercises to control excessive movement of the lumbar region and promote hip movement8). Squatting is widely used for lower extremity muscle strength training and serves similar purposes to “Waiters bow” and “Backwards rocking”9). Sitting, lifting, and other movements and postures similar to the squat are often used in daily life, and as such, the squat is often used as an exercise to improve activities of daily living. It has been reported that the squatting strategy differs between the lower back pain group and the non-lower back pain group10), and it is known that the load on the lumbar region varies with the squatting strategy11, 12). During the downward phase of the squat, the extensors of the lower extremities perform eccentric contractions, and during the upward phase, the extensors of the lower extremities perform concentric contractions to control the vertical movement of the center of gravity. Therefore, many studies have focused on the activity of the extensor muscles of the lower extremities; however, no studies have focused on the activity of the flexor muscles of the lower extremities. Hip flexor activity is critical when using the squat as an exercise to emphasize hip flexion for the purpose of controlling movement in the direction of trunk forward bending. The hip flexors are involved in adjusting the pelvic position, and it is considered that hip flexor activity allows the hip to squat with adequate hip flexion, although the relationship between changes in hip flexors and the joint angles and moments of the pelvis and hip joint during the squat has not been studied. The iliopsoas muscle is the main hip flexor and affects hip flexion and anterior pelvic tilt13, 14). As the iliopsoas muscle is relatively deep, wire electromyography and other techniques are used to capture its activity. However, wire electromyography and other measurement techniques make the execution of natural movements difficult due to pain and discomfort caused in the groin area. However, ultrasound techniques enable non-invasive measurement of muscle conditions and allow for measurement of the deeply-located iliopsoas muscle.
Therefore, the purpose of this study was to investigate the relationship between the changes in iliopsoas muscle thickness, pelvic tilt and hip angle, and lower limb joint moment during squatting in different pelvic positions.
PARTICIPANTS AND METHODS
The participants were seven healthy adult males (mean age: 25.4 ± 2.5 years, mean height: 175.0 ± 5.0 cm, mean body weight: 69.6 ± 6.2 kg) with no history of joint problems in the lower limbs or spine and no pain affecting their daily lives. The participants provided signed, written informed consent to participate in the study. The study was approved by the Ethics Committee of the Saisekai Kanazawa Hospital, Ishikawa Prefecture (Application No. 23 of the 2018 fiscal year).
The values of each parameter were measured at rest in a standing position and in the squatting position with 60° knee flexion. The knee joint angle was set at 60° knee flexion with the sensor in contact with the gluteal region. The participants were instructed to stop when the sensor made contact with the gluteal region (Fig. 1). The width between the feet was set at a position where the line connecting the greater trochanter and the lateral malleolus was perpendicular to the floor, and the foot angle was set at 10°. Squats were performed in the neutral position (NP), anterior tilt position (AP), and posterior tilt position (PP). The NP was defined as the participant’s natural pelvic position, and the AP and PP were defined as the anterior and posterior pelvic tilt, respectively, of the participant at maximum effort. The participants performed the NP, AP, and PP pelvic positions in a resting standing position, followed by squats while holding the pelvic position.
Fig. 1.
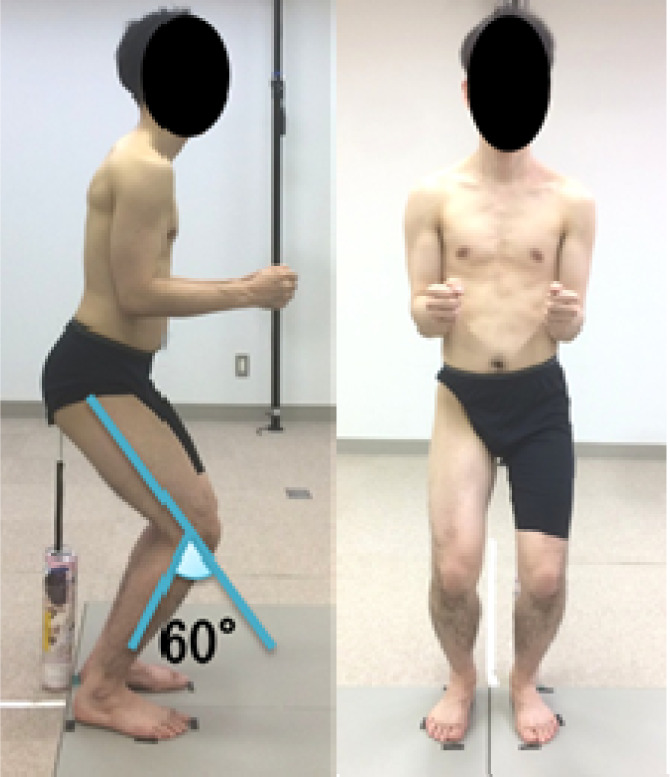
Squatting position.
The iliopsoas muscle was imaged using an ultrasound machine ((LOGIQ e, GE Healthcare Japan, Tokyo, Japan) with a linear probe (10 MHz) in B mode. The ultrasound probe was applied to measure the iliopsoas muscle according to the methodology of our previous study15), and the measurement area was the center of the inguinal region at the midpoint of the line connecting the anterior superior iliac spine to the pubic symphysis. Markings were applied to the pre-identified measurement areas to keep them constant, and the iliopsoas muscle was imaged by touching those areas with the probe (Fig. 2a). From the collected ultrasound images, the maximum length diameter of the iliopsoas muscle was measured based on the boundary of the fascia using the image analysis program Image J (Fig. 2b). The iliopsoas muscle thickness difference between the standing and squatting positions (ΔIT; iliopsoas muscle thickness in the squatting position − iliopsoas muscle thickness in the standing position) was then calculated. Measurements and image analysis were performed by the same examiner who was proficient in using and conducting analysis through the equipment.
Fig. 2.
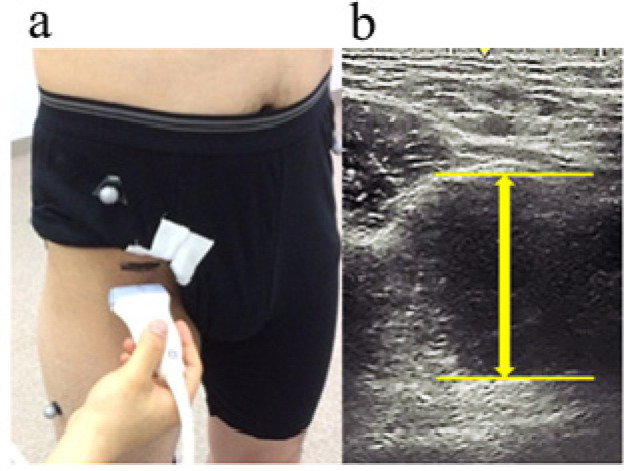
Measurement of iliopsoas muscle thickness using ultrasonography.
a: measurement area, b: region of interest.
The joint angles and joint moments were measured with a three-dimensional motion analysis system (VICON NEXUS, Vicon Motion Systems, Oxford, UK) with eight MX cameras and two force plates (AMTI, Watertown, MA, USA). For motion analysis, the sampling frequency was set at 100 Hz, and the participants were given a total of 35 infrared reflective markers of 14 mm in diameter to be placed at predetermined positions based on a plug-in gait full body model. The force plate was set at a sampling frequency of 1,000 Hz, and the left and right lower limbs were positioned on each of the two force plates. The pelvic tilt angle was defined as anterior pelvic tilt in the positive direction and posterior tilt in the negative direction, and the hip angle was defined as flexion in the positive direction and extension in the negative direction. The positive direction of the joint moment was the external flexion moment, and the negative direction was the external extension moment. Joint angles were calculated as the difference in pelvic and hip angles between the resting standing and squatting positions (ΔJA; joint angles in the squatting position − joint angles in the standing position).
Squats were performed twice in each position, and the mean of both measurements were used for statistical analysis. Statistical analysis was performed using SPSS version 24 (SPSS Statistics, Japan IBM, Tokyo, Japan). Repeated analysis of variance and Bonferroni tests were used to compare each value at the pelvic position, and Pearson’s product-rate correlation coefficient was used to determine the values correlation. The significance level was set at 0.05. All continuous data are presented as mean ± standard error.
RESULTS
The joint angles, joint moments, and ΔIT for each pelvic position are shown in Table 1. The anterior pelvic tilt and hip flexion angles in the squatting position were significantly higher for AP, NP, and PP, in that order. For ΔJA, the pelvic angle did not differ significantly between pelvic positions. However, the hip angle was significantly higher in AP and NP than in PP. There was no significant difference in joint moments between the hip and knee joints due to differences in the pelvic position. The ΔIT was significantly higher for AP than for PP.
Table 1. Values of the lower limb parameters in each pelvic position.
| NP | AP | PP | |
| Pelvic tilt angle in squatting position (°) | 12.9 ± 4.8 | 23.8 ± 4.1* | −0.6 ± 6.0*† |
| Hip joint angle in squatting position (°) | 41.3 ± 4.7 | 52.0 ± 4.2* | 25.4 ± 6.5*† |
| ΔJA of pelvic tilt (°) | 0.5 ± 2.1 | 3.5 ± 1.9 | −2.9 ± 3.7 |
| ΔJA of hip joint (°) | 34.2 ± 2.1 | 36.0 ± 2.3 | 22.0 ± 5.0*† |
| Hip joint moment (Nm) | 0.3 ± 0.1 | 0.3 ± 0.1 | 0.1 ± 0.1 |
| Knee joint moment (Nm) | 0.4 ± 0.1 | 0.4 ± 0.1 | 0.5 ± 0.1 |
| ΔIT (mm) | 9.3 ± 2.4 | 10.6 ± 1.7 | 3.6 ± 1.2† |
Data are presented as the mean ± standard error.
NP: neutral position; AP: anterior tilt position; PP: posterior tilt position; ΔJA: the angle difference between the resting standing and squatting positions; ΔIT: the iliopsoas thickness difference between the standing and squatting positions.
*Significant difference compared to NP (p<0.05).
†Significant difference compared to AP (p<0.05).
The correlation coefficients between the ΔIT and ΔJA and the joint moments are shown in Table 2. There was no significant correlation between ΔIT and pelvic ΔJA for all pelvic positions. For ΔIT and hip ΔJA, only AP had a significant positive correlation (p=0.03, r=0.82). In terms of joint moments, ΔIT and hip joint moments were not significantly correlated in all pelvic positions. Only PP had a significant positive correlation between ΔIT and knee joint moment (p=0.04, r=0.77).
Table 2. Correlation coefficients of joint angle and joint moment with iliopsoas muscle thickness.
| NP | AP | PP | |
| ΔJA of pelvic tilt | 0.21 | 0.12 | −0.27 |
| ΔJA of hip joint (°) | 0.57 | 0.82* | −0.25 |
| Hip joint moment | 0.18 | −0.3 | −0.65 |
| Knee joint moment | −0.15 | −0.07 | 0.77* |
NP: neutral position; AP: anterior tilt position; PP: posterior tilt position; ΔJA: the angle difference between the resting standing and squatting positions; ΔIT: the iliopsoas thickness difference between the standing and squatting positions.
*Significant correlation (p<0.05).
DISCUSSION
This study investigated the relationship between iliopsoas muscle thickness, pelvic and hip joint angles, and lower limb joint moments in squats in different pelvic positions and provides insight into the involvement of the iliopsoas muscle in lumbar and hip motor control in the squat, which could assist in exercise selection.
The results showed that the anterior pelvic tilt and hip flexion angle during squatting were increasingly higher in the anterior, middle, and posterior pelvic tilt positions suggesting that the anterior and posterior pelvic tilt movements caused sufficient pelvic tilt causing a concomitant change in the hip flexion angle. With respect to the angular difference between squatting and resting standing positions, there was no difference in the pelvic angle in the pelvic position. Therefore, the pelvic angle remains constant during the standing pelvic position, and no changes are expected to occur during the squat. The hip joint, on the other hand, had less movement in the direction of hip flexion in PP compared to AP and NP. Low hip mobility during squatting is known to increase the shear force on the spine, which can lead to injury9), and squatting in a posterior pelvic tilt position with low hip motion may increase stress on the spine. Therefore, if the squat is used for the purpose of facilitating hip movement, squatting in the posterior pelvic tilt position may not be appropriate in terms of causing excessive load on the spine. However, since the posterior pelvic tilt in this study was caused by active movement, the effect of different alignments needs to be further investigated.
The ΔIT was significantly higher for AP than for PP. This suggests that the change in the iliopsoas muscle due to squatting is greater in the anterior pelvic tilt position than in the posterior pelvic tilt position. Kinugasa16) reported that the cross-sectional area of the muscle decreases with muscle elongation because the muscle has a constant volume; conversely, the cross-sectional area of the muscle is likely to increase as the muscle adopts a shortened position. In our previous study15), it was also shown that increasing the hip angle passively between 0 and 60° increased the muscle thickness of the iliopsoas muscle. The angle of hip flexion during squatting in the present study was within the range of our previous study15), which might have resulted in changes in muscle thickness due to the shortening limb position of the iliopsoas muscle. However, in the present study, the correlation between ΔIT and ΔJA of the hip joint was not observed in NP and PP, but only in AP. Therefore, in addition to the increase in the cross-sectional area due to passive muscle shortening, other factors may be involved in AP. There are scattered reports linking changes in muscle thickness to muscle activity under isometric contraction17, 18). The correlation between ΔIT and ΔJA of the hip joint could be the effect of muscle thickness change due to muscle contraction. This suggests that the iliopsoas muscle might need to be active to hold the anterior pelvic tilt in AP and be more active in the squatting position. Based on our findings, it seems that the activity of the iliopsoas muscle is important for the achievement of hip-based movements in the direction of forward trunk flexion.
Regarding joint moments, there was no correlation between hip and knee moments and ΔIT for AP and NP, but only PP had a positive correlation with ΔIT for knee joint moments. The greater anterior tilt of the trunk results in a greater hip extension moment and a smaller knee extension moment9). In the present study, the pelvic angle in the squatting position of the PP was negative, which suggests that the trunk tilt posteriorly with the posterior tilt of the pelvis caused an increase in the knee joint moment. At the same time, with the posterior tilt of the trunk, the iliopsoas muscle might have been active in order to maintain balance.
A limitation of this study is that we focused solely on iliopsoas muscle measurements as the hip flexor. However, other hip flexors, such as the rectus femoris muscle, were not considered and should be included in future studies. In addition, the present study only specified the pelvic position, not the trunk position, and it is unclear how the trunk limb positions were related to each other. Furthermore, because the pelvic position is the maximal position, the pelvic angle differs among individuals. Moreover, although the probe angle was kept constant during the measurement of iliopsoas muscle thickness, it was difficult to determine whether the probe was perpendicular to the iliopsoas muscle. Additionally, as mentioned above, ultrasonic muscle thickness measurements do not directly reflect muscle activity; therefore, the present study can only describe the possibility that muscle activity occurred in relation to muscle thickness changes and joint angle changes. It has been reported that changes in muscle thickness do not necessarily reflect muscle activity and that muscle thickness is influenced by myofascial extensibility19), the region measured20), and the strength of contraction21). Thus, caution should be observed while interpretating the results of this study with respect to increase in muscle thickness and muscle activity. Future studies with larger samples are needed to validate other indices of direct muscle activity using wire electromyography and other measurement tools such as MRI.
In conclusion, squatting in the neutral or posterior pelvic tilt position was not associated with hip angle and iliopsoas muscle thickness changes, whereas squatting in an anterior pelvic tilt position was associated with changes in the iliopsoas muscle thickness and hip flexion angle. It is suggested that the activity of the iliopsoas muscle might be necessary to promote hip-dominant squatting.
Funding
This work was supported by JSPS KAKENHI Grant Number JP19K24181.
Conflict of interest
The authors declare no conflict of interest.
REFERENCES
- 1.Vazirian M, Van Dillen L, Bazrgari B: Lumbopelvic rhythm during trunk motion in the sagittal plane: a review of the kinematic measurement methods and characterization approaches. Phys Ther Rehabil, 2016, 3: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vazirian M, Van Dillen LR, Bazrgari B: Lumbopelvic rhythm in the sagittal plane: a review of the effects of participants and task characteristics. Int Musculoskelet Med, 2016, 38: 51–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bohannon RW, Bass A: Research describing pelvifemoral rhythm: a systematic review. J Phys Ther Sci, 2017, 29: 2039–2043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pierannunzii L: Pelvic posture and kinematics in femoroacetabular impingement: a systematic review. J Orthop Traumatol, 2017, 18: 187–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prather H, van Dillen L: Links between the hip and the lumbar spine (hip spine syndrome) as they relate to clinical decision making for patients with lumbopelvic pain. PM R, 2019, 11: S64–S72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Scholtes SA, Gombatto SP, Van Dillen LR: Differences in lumbopelvic motion between people with and people without low back pain during two lower limb movement tests. Clin Biomech (Bristol, Avon), 2009, 24: 7–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Esola MA, McClure PW, Fitzgerald GK, et al. : Analysis of lumbar spine and hip motion during forward bending in subjects with and without a history of low back pain. Spine, 1996, 21: 71–78. [DOI] [PubMed] [Google Scholar]
- 8.Luomajoki H, Kool J, de Bruin ED, et al. : Movement control tests of the low back; evaluation of the difference between patients with low back pain and healthy controls. BMC Musculoskelet Disord, 2008, 9: 170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schoenfeld BJ: Squatting kinematics and kinetics and their application to exercise performance. J Strength Cond Res, 2010, 24: 3497–3506. [DOI] [PubMed] [Google Scholar]
- 10.Lui TK, Tsang SM, Kwok AW: Changes in lumbopelvic movement and muscle recruitment associated with prolonged deep squatting: a pilot study. Int J Environ Res Public Health, 2018, 15: 1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.List R, Gülay T, Stoop M, et al. : Kinematics of the trunk and the lower extremities during restricted and unrestricted squats. J Strength Cond Res, 2013, 27: 1529–1538. [DOI] [PubMed] [Google Scholar]
- 12.Fry AC, Smith JC, Schilling BK: Effect of knee position on hip and knee torques during the barbell squat. J Strength Cond Res, 2003, 17: 629–633. [DOI] [PubMed] [Google Scholar]
- 13.Blemker SS, Delp SL: Three-dimensional representation of complex muscle architectures and geometries. Ann Biomed Eng, 2005, 33: 661–673. [DOI] [PubMed] [Google Scholar]
- 14.Andersson E, Oddsson L, Grundström H, et al. : The role of the psoas and iliacus muscles for stability and movement of the lumbar spine, pelvis and hip. Scand J Med Sci Sports, 1995, 5: 10–16. [DOI] [PubMed] [Google Scholar]
- 15.Miyachi R, Deguchi M, Hara J, et al. : Intra- and inter-rater reliabilities of measurements of iliopsoas thickness in hip flexion. Rigakuryoho Kagaku, 2019, 34: 523–527. [Google Scholar]
- 16.Kinugasa R, Hodgson JA, Edgerton VR, et al. : Asymmetric deformation of contracting human gastrocnemius muscle. J Appl Physiol 1985, 2012, 112: 463–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blanchard TW, Smith C, Grenier SG: In a dynamic lifting task, the relationship between cross-sectional abdominal muscle thickness and the corresponding muscle activity is affected by the combined use of a weightlifting belt and the Valsalva maneuver. J Electromyogr Kinesiol, 2016, 28: 99–103. [DOI] [PubMed] [Google Scholar]
- 18.Hodges PW, Pengel LH, Herbert RD, et al. : Measurement of muscle contraction with ultrasound imaging. Muscle Nerve, 2003, 27: 682–692. [DOI] [PubMed] [Google Scholar]
- 19.Whittaker JL, Stokes M: Ultrasound imaging and muscle function. J Orthop Sports Phys Ther, 2011, 41: 572–580. [DOI] [PubMed] [Google Scholar]
- 20.Miyachi R, Mori K, Yonekura S, et al. : Change in muscle thickness during exercise to stabilize the hip joint against a load in the ventral direction of the femoral head. J Phys Ther Sci, 2019, 31: 935–938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pappas GP, Asakawa DS, Delp SL, et al. : Nonuniform shortening in the biceps brachii during elbow flexion. J Appl Physiol 1985, 2002, 92: 2381–2389. [DOI] [PubMed] [Google Scholar]


