Dear Editor,
Since the beginning of the COVID-19 pandemic, radiologists have been working at the forefront of patient care. Computed tomography (CT) is a pivotal imaging essential modality by contributing to diagnosis and differentials as well as for the follow-up and management of complications [1], [2], [3]. Recently, a large vaccination campaign has been set up and very rare thrombotic complications have been reported in patients who have been vaccinated. We report a patient who developed hypercoagulable state after receiving COVID-19 vaccine (Oxford-AstraZeneca®).
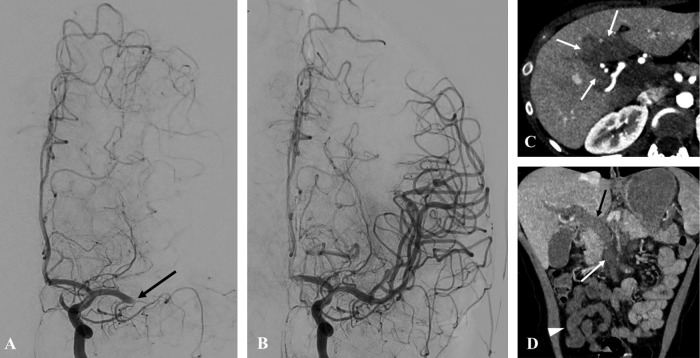
A 26-year-old woman was admitted for acute stroke 8 days after administration of COVID-19 vaccine (Oxford-AstraZeneca®). Right hemiplegia and aphasia (Score of 8 using the National Institute of Health Stroke Scale) occurred rapidly while the patient was hospitalized for persistent nausea and headache that had started shortly after vaccination. Initial angiography revealed a proximal left middle cerebral artery occlusion. Dual thrombo-aspiration using the direct aspiration first pass technique (ADAPT technique, i.e., without stent retriever) performed 3.5 hours after the onset of symptoms led to recanalization of left middle cerebral artery after a first pass (Fig. 1 A). Final angiography showed a 2C recanalization based on thrombolysis in cerebral infarction scale (Fig. 1B). Laboratory tests revealed major thrombocytopenia, hypofibrinogenemia and inflammation (C-reactive protein 158 mg/L). Disseminated intravascular coagulation or catastrophic antiphospholipid syndrome were initially considered. However, high titre anti-platelet factor 4 antibodies (Lifecodes PF4 IgG Assay, Immucor®) and positive result of functional platelet activation testing were consistent with vaccine-induced immune thrombotic thrombocytopenia [4], [5]. CT examination revealed segmental pulmonary embolism and portal thrombosis extending to the splenomesenteric trunk and ileal veins while the patient was eupneic and had no abdominal pain. On arterial phase, CT showed global arterialization of the liver parenchyma with central hypoattenuating areas, that became isoattenuating on portal venous phase. These findings consistent with transient hepatic attenuation differences due to hepatic blood flow alterations (Fig. 1C). In addition, mesenteric venous enlargement and intraluminal filling defects, bowel wall edema and decreased ileal wall enhancement suggested venous mesenteric ischemia (Fig. 1D). The patient was given corticosteroids, plasmatic exchange and anticoagulants. Magnetic resonance imaging of the brain 14 days later showed minor sylvian and border zone infarcts, with mild hemorrhagic changes. At day 15, only gripping difficulties and minor phasic troubles were remaining.
Fig. 1.
26-year-old woman was admitted for acute stroke 8 days after administration of COVID-19 vaccine. A: Digital subtracted angiography of the left internal carotid artery in anteroposterior projection shows occlusion of the M1 segment (arrow) of the left middle cerebral artery and absence of opacification of the Sylvian network. National Institute of Health Stroke Scale score was 8. B: Cerebral digital subtracted angiography after double thrombo-aspiration (ADAPT technique) shows 2C recanalization of left middle cerebral artery after a first pass based on thrombolysis in cerebral infarction scale. Immediate clinical follow up was favorable. Fifteen days later, National Institute of Health Stroke Scale score was 2. C: CT image of the liver in axial plane obtained during the arterial phase of enhancement shows global arterialization of the liver parenchyma with central and perihilar perfusion defects anomalies (arrow) due to portal trunk thrombosis. Central areas became isoattenuating on portal venous phase. D: CT image of the abdomen in the coronal plane obtained during the portal venous phase demonstrates portal (black arrow) and superior and inferior mesenteric vein (white arrow) thrombosis. Decreased ileal wall enhancement (arrowhead) consistent with venous mesenteric ischemia is also present.
As observed in COVID-19 [6], Oxford/AstraZeneca vaccine may induce hypercoagulable state that could lead to concomitant venous and arterial thromboses. In our patient, immunoassay and confirmatory functional assay for PF4 antibodies were positive and consistent with vaccine-induced immune thrombotic thrombocytopenia, a disease that resembles heparin-induced thrombocytopenia. Post-vaccination thrombosis has been recently described, but imaging findings have rarely been reported. Although very rare, occurrence of multiple thrombosis in the days following Covid-19 vaccine should urge extensive evaluation in order to approach the diagnosis. Multimodality imaging has a pivotal role in the diagnosis and treatment of such condition.
Human rights
The authors declare that the work described has been carried out in accordance with the Declaration of Helsinki of the World Medical Association revised in 2013 for experiments involving humans.
Informed consent and patient details
The authors declare that this report does not contain any personal information that could lead to the identification of the patients. The authors also confirm that the personal details of the patients have been removed.
Disclosure of interest
The authors declare that they have no competing interest.
Funding
This work did not receive any grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
All authors attest that they meet the current International Committee of Medical Journal Editors (ICMJE) criteria for Authorship.
References
- 1.Hani C., Trieu N.H., Saab I., Dangeard S., Bennani S., Chassagnon G., et al. COVID-19 pneumonia: a review of typical CT findings and differential diagnosis. Diagn Interv Imaging. 2020;101:263–268. doi: 10.1016/j.diii.2020.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ammar A., Drapé J.-L., Revel M.-P. Lung cavitation in COVID-19 pneumonia. Diagn Interv Imaging. 2021;102:117–118. doi: 10.1016/j.diii.2020.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cellina M., Oliva G. Acute pulmonary embolism in a patient with COVID-19 pneumonia. Diagn Interv Imaging. 2020;101:325–326. doi: 10.1016/j.diii.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Greinacher A., Thiele T., Warkentin T.E., Weisser K., Kyrle P.A., Eichinger S. Thrombotic thrombocytopenia after ChAdOx1 nCov-19 vaccination. N Engl J Med. 2021 doi: 10.1056/NEJMoa2104840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oldenburg J., Klamroth R., Langer F., Albisetti M., von Auer C., Ay C., et al. Diagnosis and management of vaccine-related thrombosis following AstraZeneca COVID-19 vaccination: guidance statement from the GTH. Hamostaseologie. 2021 doi: 10.1055/a-1469-7481. [DOI] [PubMed] [Google Scholar]
- 6.Le Berre A., Marteau V., Emmerich J., Zins M. Concomitant acute aortic thrombosis and pulmonary embolism complicating COVID-19 pneumonia. Diagn Interv Imaging. 2020;101:321–322. doi: 10.1016/j.diii.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]