Abstract
Background
Poly drug use is a public health threat causing morbidity and mortality all over the world. Combined use of licit and illicit drugs is among the possible causes of death. In this retrospective analytical study, we evaluated forensic toxicology analysis results from 2011 to 2016 in Tehran province, Iran.
Methods
All deaths related to poly drug use and referred to the Legal Medicine Organization, Tehran during the 6-year study period were evaluated. Postmortem samples were analyzed to detect alcohols, and prescription and illicit drugs using headspace gas chromatography (HSGC), high performance liquid chromatography (HPLC), and gas chromatography/mass spectrometry (GC/MS) in a forensic toxicology laboratory. Manner of death, demographic characteristics, and different drug categories in postmortem samples were analyzed.
Findings
A total of 1388 poly drug use-associated deaths were investigated during the 6-year study period. Overall, victims were mostly young men of 20-40 years of age (56.8%). The male to female ratio was 7:16. Methadone (n = 660; 47.6%) and amphetamine type stimulants (ATS) (n = 657; 47.3%) were in the highest category for poly drug use-associated deaths. Moreover, in some cases, opium (n = 458; 32.9%), tramadol (n = 389; 28.0%), and tricyclic antidepressants (n = 151; 10.9%) had been used with other drugs.
Conclusion
The present study provides information about poly drug use-associated deaths in Tehran and highlights the major role of substance abuse in death.
Keywords: Substance-related disorders, Forensic toxicology, Amphetamine, Methadone, Public health
Introduction
It has been acknowledged all around the world that use or abuse of drugs presents many health issues.1 Illicit drug use is rampant in the young population and has become one of the great conundrums for policy makers and health professionals.2 Poly drug use has been associated with accidental deaths in many cases. The adverse health consequences of poly drug use are often attributed to drug-drug interactions. Poly drug use is defined as the use of 2 or more psychoactive substances at the same time or sequentially to achieve particular effects.3 Some licit and illicit drugs are the cause of the majority of deaths due to intoxication;4,5 thus, it is crucial to get a better understanding of different drug classes that may be involved in death. While previous studies have evaluated different aspects of drug-associated deaths (suicidal poisoning, drug overdose, and specific drug-associated deaths),4,6-9 few have investigated poly drug use-associated deaths. The present study may contribute to filling such a gap in Iran. Physicians have anecdotally reported that many drug abusers show mixed side effects and toxicity due to drug abuse. These reports encourage and inspire forensic researchers to seek drug categories in postmortem samples of drug users. Many studies have consistently demonstrated an increased risk of poisoning with concomitant use of stimulants such as cocaine and methamphetamine.10,11
Coadministration of opioids and benzodiazepines can also confer an additional risk of death.12 Just like Iran, there has been a surge in opioid-associated death in other countries. There are reports that opioid-related overdose deaths have quadrupled since 1999 in the United States.13 In 2014, European opioid users were 5-10 times more likely to die in comparison to their peers of the same gender.14
Although poly drug use-associated deaths are increasingly recognized in Iran, knowledge of the trend and pattern of poly drug use remains insufficient and underdeveloped. This study was aimed at the identification of the various patterns and trends of poly drug use-associated deaths in Tehran, Iran, during a 6-year study period.
Methods
A retrospective analytical study was implemented to identify different drug categories in poly drug use-associated deaths in Tehran, over a period of 6 years (January 2011-December 2016). Autopsy reports and death certificates of all cases observed in the Legal Medicine Organization, Tehran, were obtained. This center serves about 13 million people, which equals 16.6% of the Iranian population. Autopsy is requested following jurisdictional claim to the legal medicine organization for conducting postmortem examinations, issuing death certificates, and determining causes and manner of death. About 10000 to 110000 cases are referred to the Legal Medicine Organization, Tehran, annually, 35% of which are examined in the forensic toxicology department. Forensic toxicology laboratories in Iran are centralized in a few accredited laboratories in some provinces such as Tehran. This laboratory uses a wide range of analytical instruments such as high performance liquid chromatography (HPLC), ultra-high performance liquid chromatography (UHPLC), gas chromatography/mass spectrometry (GC/MS), headspace gas chromatography (HSGC) with nitrogen phosphorous detector (NPD), HSGC, voltammetry working with the dropping mercury electrode (DME) for screening, verification, and qualitative and quantitative analysis of drugs in biologic and non-biologic matrices. The autopsy specimens are shipped to forensic laboratories from cities in Tehran Province in portable refrigerators (4 °C).
Postmortem samples collection: Routine postmortem and first choice specimens are urine, liver, blood, vitreous humor, bile, and stomach content. On arrival, all specimens are inspected and properly labeled with a unique identification code that is linked to the information of each case. Samples are stored in a refrigerator at 4 °C pending analysis. The cases selected were those whose manner of death was unnatural and drug-related, and those who had tested positive for at least 2 of the variables of psychoactive drugs, alcohol, and therapeutic medications.
Drug concentrations found in biological matrices obtained in autopsy examinations will not be discussed, because drugs alone could not necessarily contribute to the cause of death. Synergistic effects of drugs play an important role in death; moreover, the main focus of the present study was not to interpret postmortem drug concentration on a case by case basis.
Biological samples preparation: For analysis, all biological matrices were prepared to extract drugs. Liquid-liquid extraction (LLE) and dispersive liquid-liquid microextraction (DLLME) were used as sample preparation methods. Liver samples were first homogenized using a homogenizer (DIAX 900; Heidolph Instruments, Schwabach, Germany). PH adjustment was required to extract different drugs with various chemical structures from biological matrices. Weak acidic drugs such as phenytoin, phenobarbital, and valproic acid were extracted with a pH adjustment to 2. As many of the drugs that are important from the forensic point of view have basic structures, the pH of the experiment medium was adjusted to 12 for the extraction of antidepressants, benzodiazepines, narcotic analgesics, amphetamine type stimulants (ATS), and other drug classes. For the efficient extraction of morphine, the pH of the experiment medium was adjusted to its isoelectric point (pH = 9).15 For the separation of drugs and their metabolite conjugates, hydrochloric acid (pH = 1-2) was used for acid hydrolysis. After the adjustment of the pH of liver, stomach content, bile, and urine samples in aqueous media, a solvent extractant consisting of chloroform: isopropanol (80:20 v/v) was used to promote the partitioning of drugs and their metabolites into the organic phase and leaving waste materials in aqueous phase. In this phase, the organic layer that contained drugs was transferred to a clean tube and evaporated to dryness prior to analysis. For the extraction of drugs from urine samples, 2 mL of urine was diluted with 2 mL of 0.1 M borate buffer (pH = 9.2). The pH of the analysis medium was adjusted to 12 for the extraction of basic drugs. The extraction procedure was repeated in a pH of 2-3 and 8-9 for the extraction of acidic drugs and morphine, respectively. A mixture of 2.5 mL of methanol (dispersing solvent) and 300 µL of chloroform (extracting solvent) was pushed by force into 2 mL of prepared urine sample in borate buffer. The mixture was stirred and ultrasonicated for 5 min before centrifugation. After being centrifuged for 5 min at 3000 rpm, the chloroform layer was separated and evaporated to dryness under nitrogen stream. The extraction product was dissolved in 30 µL methanol pending instrumental analysis.
ATS such as amphetamine and methamphetamine were analyzed using a prevalidated specific method in urine samples.16 The pH of 1 mL of urine sample was alkalinized using potassium hydroxide (0.5 M) to pH = 12. Extraction was accomplished by adding 3 mLn-hexane to the mixture. After shaking the mixture, the organic layer was separated through the immersion of the mixture into the freezing bath. To achieve a complete derivatization reaction, heptafluorobutyric anhydride (HFBA) was added to the mixture. For the extraction of derivatized amphetamine and methamphetamine, 100 µL of n-heptane was used. The organic layer was evaporated and the extracted analytes were prepared for analysis.
Instrumental conditions: Forensic toxicology analysis of a wide range of drug categories and their metabolites was performed using well-established methods.4,7 Different analytical cut-off concentrations were applied to different licit and illicit drugs.
A gas chromatograph (model 7890; Agilent Technologies Inc., SdnBhd, Selangor, Malaysia) was used with a mass selective detector (model 5975 C; Agilent Technologies Inc., SdnBhd, Selangor, Malaysia) working with electron impact (70 ev) in full scan mode (50-550m/z) with a HP5-MS capillary column (cross-linked 5% methyl phenyl silicone, 30 m length, 0.25 mm ID, 0.25 µm film thickness) fitted with a split/splitless injector. The presence of drugs in biological matrices was confirmed using the National Institute of Standards and Technology (NIST), and Wiley libraries. The analytical protocol was prevalidated for the detection of methamphetamine in biological matrices using heptafluorobutyric acid (HFBA) as derivatization reagent and GC/MS instrumentation.16 Blood and vitreous humor samples were analyzed for alcohol according to national standards. A headspace gas chromatograph (model 6890 N; Agilent Technologies Inc., SdnBhd, Selangor, Malaysia) equipped with a flame ionization detector (FID) was used for quantitative analysis of alcohols in the blood and vitreous humor samples.17 Ethanol and methanol in blood and vitreous humor samples were quantitatively determined using HSGC with 0.1 and 1 mg/dl as limit of detection (LOD) and limit of quantitation (LOQ), respectively.
UHPLC was performed using a detector (KNAUER GmbH, Berlin, Germany) operated with a photodiode array (PDA) detector. The instrument was equipped with a cooling autosampler (PDA-1, 6 channels). A Eurospher II (100-3 C-18; KNAUER GmbH, Berlin, Germany) (100 mm × 3 mm) column was used for the separation of analytes.
SPSS software (version 17; SPSS Inc., Chicago, IL, USA) was used to carry out statistical analysis. Qualitative variables are presented as frequency (%) and number of events.
Chi-square test was used for the analysis of qualitative variables. For the analysis of quantitative variables (age and alcohol concentrations), mean values were used as central measures, and standard deviation (SD), and maximum and minimum values as measures of description. Student's t-test and Mann-Whitney test were used for quantitative variables with normal distribution and quantitative variables with non-normal distribution, respectively. The level of significance was considered as P < 0.05.
Results
To determine different drug categories in poly drug use-associated deaths in Tehran, Iran, we conducted a cross-sectional study based on forensic toxicology analysis results in cases with poly drug use pattern. About 63000 cases were autopsied during a 6-year study period. Approximately 22000 cases were analyzed in a forensic toxicology laboratory for the detection of drugs and poisons in postmortem samples. Results of the analytical toxicology examination displayed that 1388 (6.3% of cases referred to the forensic toxicology laboratory) cases were poly drug users. Different types of deaths occurred during the 6-year study period.
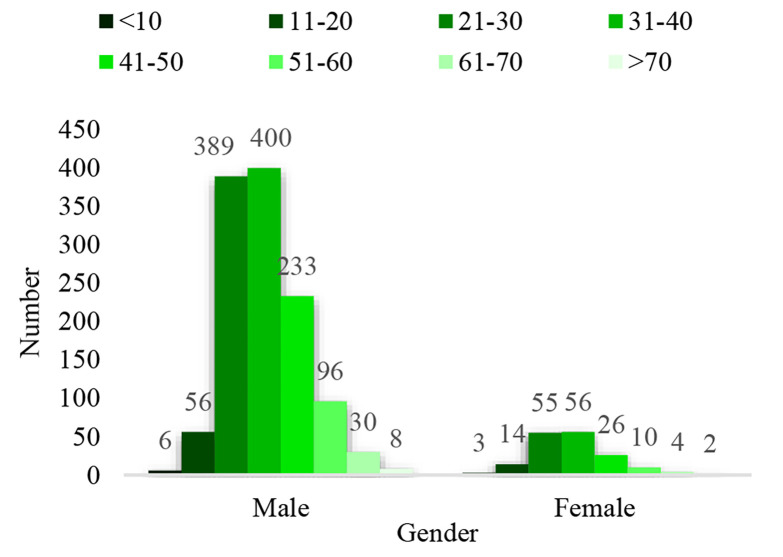
The manner of death was classified as accidental (75.2%), suicidal (19.0%), homicidal (2.3%), and undetermined (3.5%). The victims of deaths associated with a combination of illicit drugs were predominantly men with a mean age of 36.01 ± 11.58 years, and often had a history of drug abuse. A separate analysis examining poly drug use-associated deaths showed that their prevalence was higher in younger people (age ranges: 21-30 and 31-40 years) compared to the older population (P < 0.001). As shown in figure 1, men were more likely to use poly drugs than women (P < 0.050) in each year between 2011 and 2016. The ratio of men to women was 7.16, which is in accordance with the higher prevalence of men in poly drug use-associated deaths.
Figure 1.
Number of poly drug use-associated deaths in different age groups of men and women in Tehran, Iran, in 2011-2016
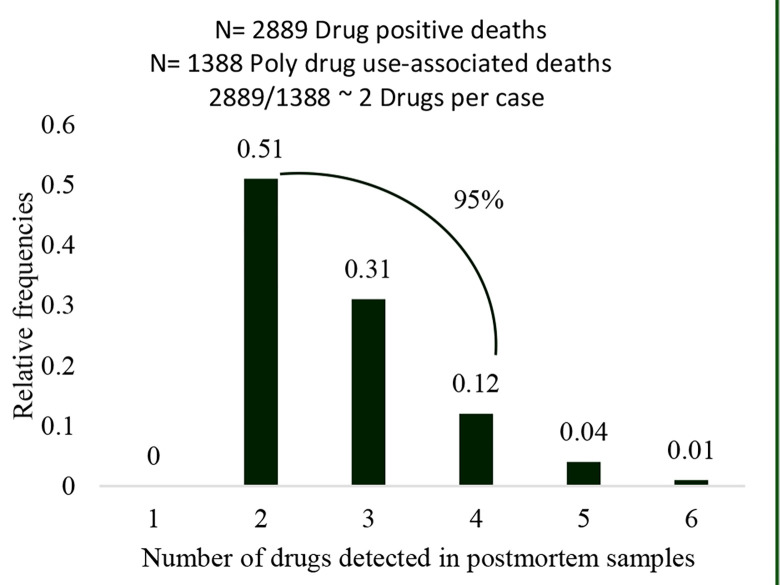
Deaths attributed to poly drug use increased 4.05 times in women compared to 3.17 times in men between 2011 and 2016. In all of the drug-associated death cases, at least 2 drug types were present in the victims' toxicology confirmatory tests (Figure 2).
Figure 2.
Frequency distribution of number of drugs detected in postmortem samples of poly drug use-associated death cases in Tehran, Iran, in 2011-2016
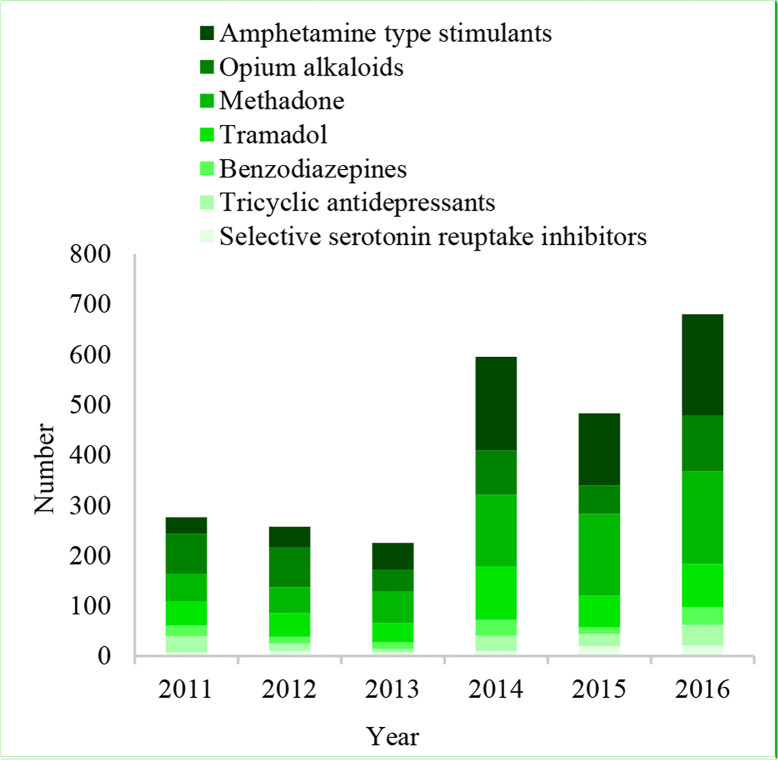
A significantly higher proportion of poly drug use-associated deaths were investigated in 2016 (n = 469; 33.79%) compared to other years of the study (P < 0.050). From 2011 to 2016, poly drug use-associated deaths increased 330.28% (P < 0.001). It should be noted that the role of ATS in poly drug use-associated deaths increased from 33 cases in 2011 to 210 cases in 2016 (P < 0.050). Moreover, the role of methadone in poly drug use-associated deaths showed a significant increase (55 cases in 2011 compared to 184 cases in 2016) (P < 0.050). Findings of the present study indicate that opium alkaloids, tramadol, amitriptyline, and nortriptyline were found in postmortem samples of poly drug use-associated deaths in combination with methadone and ATS (Figure 3). Methadone (n = 660, 47.6%) and amphetamine type stimulants (n = 657, 47.3%) were in the highest category for poly drug use-associated deaths. Also cases had used opium (n = 458, 32.9%), tramadol (n = 389, 28%) and tricyclic antidepressants (n = 151, 10.9%) with other drugs.
Figure 3.
The most common prescription and illicit drugs detected in postmortem samples of 1388 cases of poly drug use-associated deaths in Tehran, Iran, in 2011-2016
Ethanol was detected in 16 out of 1388 cases, with mean positive vitreous humor and blood alcohol concentrations of 94.44 ± 89.41 and 63.11 ± 37.53 mg/dL, respectively. Table 1 shows the rate of poly drug use-associated deaths per 1000000 in the population of Tehran from 2011 to 2016. The growth rate in mortality due to poly drug use for the entire 6 years of the study was 20.3% per 1000000 population, calculated using the following formula:
Table 1.
Numbers and rates of poly drug use-associated deaths per one million of the population of Tehran, Iran, during 2011-2016
| Year | Number of drug associated deaths | Tehran population (million) | Rate of drug associated death per one million of the population of Tehran |
|---|---|---|---|
| 2011 | 142 | 12183391 | 11.66 |
| 2012 | 144 | 12358831 | 11.65 |
| 2013 | 108 | 12413461 | 8.70 |
| 2014 | 288 | 12550000 | 22.95 |
| 2015 | 237 | 12720950 | 18.63 |
| 2016 | 469 | 12267637 | 35.35 |
Discussion
This study contributes to the body of research on poly drug use-associated deaths in Tehran, Iran. Overall, trends in the poly drug use-associated deaths in Tehran are characterized by an increase in methadone and ATS use over the years 2011-2016. Our assumption prior to the performance of the study and data analysis was that, consistent with the results of previous studies, poly drug use is associated with fatal consequences among poly substance users.18 Results of the present study indicated that most of the deaths due to poly drug use were accidental. These results are in line with those reported by Wang et al. from China.19 They showed that the majority of poisoning deaths were accidental. They also indicated that the pattern of drug poisoning varies in different countries based on the availability of drugs.19 Easy access to different types of illegal drugs have been increasing in recent years, thus paving the way for the use or abuse of multiple drugs by an individual in Iran.20,21 These findings are consistent with the results of similar studies in other cultures that showed that some factors can increase an individual's risk of being a drug user including easy access to licit or illicit drugs.3 Toxicological analysis by manner of death in the study by Paul et al. revealed that accidental poisoning was the most prevalent manner of death in adolescents in Clark County, Nevada, USA, from 2005 to 2015.2
Considering the age of the decedents, our results were confirmed by previous studies. Ghane et al., in their study on lead poisoning outbreak due to contaminated opium use, concluded that the average age of opioid dependence was 32 years.6 It is worth noting that over 64% (900 cases) of poly drug use-associated deaths occurred in young individuals aged 21-40 years.
As other studies have suggested, drug abuse is more prevalent in young individuals. Young populations, as valuable assets of the country, are more likely to engage in risky behaviors such as addiction and illicit drug use.4,7
Results of the present study showed that the difference between men and women was statistically significant. In agreement with the results of the present study, Grigsby and Howard showed that men were more likely than women to report prescription opioids and poly drug use.22 Moreover, our findings support those of Hassan and Le Foll in that poly drug use is associated with certain demographic features such as the male gender.23 Titidezh et al., in their survey on deaths due to drugs and chemicals toxicity in Tehran, concluded that the highest rate of mortality due to poisoning was seen in male subjects.9 There is evidence that the prescription opioids-related death rate showed a significant increase in women aged 55-64 years during 1999-2017 in the US,24 our findings support this finding in showing a significant increase in this regard in the young female population in Iran.
The majority of cases in the present study (95%) consumed 2 to 4 drugs. Additionally, in more than 40% of the study population, methadone, ATS, and crude opium were detected in combination with each other. Natural and synthetic opioids can act synergistically with each other in depressing the respiratory function and inducing death.18 Most of the obtained results in the present study are in concordance with data previously reported. Heightened levels of risk are associated with abuse or non-medical use of opioid drugs that are prescribed as substitution medications such as methadone.25 It must be noted that the majority of deaths involved the simultaneous use of drugs with different pharmacologic properties. Most of the deaths were linked to the use of methadone. ATS (amphetamine and methamphetamine) were the second leading cause of drugs-induced deaths followed by opium alkaloids.
In contrast to the results of the present study that showed a high prevalence of pharmaceutical opioid-associated fatalities, Clinton et al. showed that this issue has a low rate in Connecticut, USA.26 Fentanyl and 3-methylfentanyl ranked the highest in drug-related deaths in Estonia in 2000-2009.27 Researchers, policy makers, and clinicians are concerned with the high prevalence of opium and opioids abuse and point to the high prevalence of opioid-associated deaths in Iran.28 Non-natural deaths associated with drug use is an important and preventable issue. Therefore, it is important to investigate trends of drug use and its profile. In a study conducted in 2000-2009 in Norway, it was concluded that the number of various legal and illegal substances has increased in toxicological analysis.29 Results of the present study indicate that the increasing trend in drug consumption seams to continue. Our findings vary considerably from findings observed in other countries. Tetrahydrocannabinol (THC) was the most prevalent substance detected in postmortem samples of adolescents in Clark County, Nevada, in 2005-2015.2 In contrast to some other countries such as Germany and France,30 tramadol is regarded to have high potential for abuse in Iran. As a result of many reports indicating tramadol misuse among the young population, tramadol has been classified as a “controlled drug” in Iran since April 2007.30 Access to tramadol and methadone is limited to medical settings and is not freely available to patients. Previous studies in the United States indicated that, following the implementation of interventions for prescription opioids use and decreasing their supply, the rate of heroin use increased 63% from 2002-2013.31
The results of the present study are in keeping with that of previous studies about the role of tramadol in fatal intoxication, especially when used in combination with other licit and illicit drugs.30 Fischer et al., in their study on drug overdose-related deaths, indicated that overdose involving opioids have been dramatically increasing in North America.32 Other studies confirmed the association of poly drug use with a higher risk of overdose. Results of previous studies showed that over half of prescription opioid-related poisoning involved more than 1 type of drug category.31,33 Our results are consistent with that of prior studies demonstrating that the use of a combination of different types of drugs in drug-associated deaths is a common occurrence in the US.26
Multiple drug use is often involved in overdose deaths. In the present study, the opioids most commonly involved in poly drug use-associated deaths were methadone, opium, and tramadol; however, Hedegaard et al. stated that heroin, oxycodone, methadone, morphine, hydrocodone, and fentanyl were the most commonly used opioids.34 The Substance Abuse and Mental Health Services Administration (SAMHSA) reported that only 17.9% of people who needed substance use treatment received treatment in 2016.35 According to the United Nations Office on Drugs and Crime (UNODC), the use of illicit psychoactive substances showed a prevalence of about 5% among individuals of 15-64 years of age all over the world in 2017.36 Although cannabis is the most commonly used illicit drug in the world, opiates such as methadone rank alongside ATS as the drugs most commonly detected in postmortem samples of poly drug use-associated deaths in Tehran, Iran. An evident shift from traditional opium use to crystal methamphetamine use has been reported in Iran. Expensive methamphetamine was first imported to Iran from Southeast Asian countries. Expensive methamphetamine use was uncommon in Iran before 2005.37 Soon after, illegal production of methamphetamine was initiated using inexpensive precursors in clandestine laboratories.37 The rise in methamphetamine production is one of the main reasons for its use in Persian society. It is a misconception that methamphetamine use can relieve methadone side effects such as depression, poor sexual activity, and loss of energy and attention.38 Opioid substitution treatment with oral methadone is among the maintenance interventions used to relieve opioid use.39 Iran, the most populated Persian Gulf country, struggles with methamphetamine use as a health concern. In recent years, Iran has witnessed major challenges in the pattern of substance use. We observed a steep increase in the number of cases of methadone use after its introduction as opioid substitution therapy.40 Methadone was the most detected drug in combination with other drugs or substances (660 cases). Our survey showed that the number of people who died of methadone use in combination with other drugs in 2016 was 3 times that in 2010. As previous studies have indicated, increased tendency for opiate substitution therapy, leakage of drug from legitimate centers to drug gray or black market, steep increase in the number of clients who abuse methadone, and sharing the drug with each other are among the important factors that play a key role in the increase in the number of deaths associated with poly drug use.40-42
According to the UNODC report in 2011, Iran has the highest number of heroin and opium users per capita all over the world.43 Although it is indicated that opium and its residue are the most commonly used drugs in Iran,6 our study confirms the presence of methadone and ATS as the drugs most commonly detected in poly drug use-associated deaths. According to the Iran Drug Central Headquarters report, the number of illicit drugs dependent individuals of 15-64 years of age was 2.8 million in 2015.6 As confirmed by previous studies, we noticed a steep increase in opium consumption in 2016. Iran has a long and porous border with Afghanistan and this can facilitate opium trafficking to Iran.44
Barzegar et al., in their study on the mortality rate of illicit drug use, observed that opium and its extract (Shire) were the most commonly used drugs in Iran.8 However, results of the present study showed that methadone ranks first in poly drug use-associated deaths. Furthermore, ATS were the second drugs attributed to poly drug use with a slight difference. The discrepancy may be due to several factors such as study period, geographic region, and results based on laboratory analysis or relatives’ declaration.
Results of the present study showed that the majority of cases of opioid-associated deaths were due to concomitant non-medical use of opioid agonist medications, such as methadone and tramadol, with crude opium. A drug-related or associated death occurs when the underlying cause of death is drug abuse, drug dependence, or overdose. The term overdose has not been used to describe drug-associated death, because all study cases had used at least 2 drugs, it would be possible that blood drug concentrations were within therapeutic ranges. It is assumed that drug-drug interactions accounted for the person's demise. However, the role of ethanol in poly drug use-associated deaths is not so important in competition to other countries due to cultural and religious beliefs and ban on ethanol use in Iran.4 Nonetheless ethanol topped the list of most commonly identified drugs in postmortem femoral blood in fatal poisoning in Sweden.33 In the study by Mohanty et al. in a Southern town in India, more than 50% of professional college students took alcohol.45
Conclusion
Fatalities due to poly drug use signals an important area for further exploration into how drug combinations are being prescribed, used, and produced in the drug black market as street drugs. Poly drug use-associated death rates continue to increase. The rise in non-medical prescription opioids use and abuse triggered the implementation of various interventions in order to reduce availability to these drugs. This analysis documents gender and age differences in trends of poly drug use-associated deaths in Tehran during the 6 years of the study. Evidence of the increasing rate of poly drug use-associated deaths points to the need for information propagation regarding health risks attributed to drugs used in combination. Raising awareness and the provision of information about the risk of overdose in cases with poly drug use or misuse are important measures in preventing drug related harms.
Limitations: There is increasing evidence that new psychoactive substances can cause severe side effects that can even result in death. One of the limitations that we encountered in the present study was that we were unable to detect new psychoactive substances (NPS) due to limitations in drug testing panels that are targeted at the detection of relevant compounds. These limitations were further compounded by the lack of access to analytical grade standards as reference materials.
Acknowledgments
The authors would like to acknowledge the Legal Medicine Research Center, Legal Medicine Organization, Tehran, Iran, that made the present research possible.
The study protocol was in conformity with the ethical guidelines of the 1975 Declaration of Helsinki, as revised in 1983. Private information, name, surname, and burial permit were removed from datasheets to comply with ethical concern. Moreover, this study was conducted under the supervision of the Legal Medicine Research Center, Legal Medicine Organization, Tehran, Iran, and the protocol was approved by the Legal Medicine Ethics Committee and was registered under the registration number IR.LMO.REC.1397.70.
Conflicts of Interest
The Authors have no conflict of interest.
Authors’ Contribution
Contribution to the conception of the research idea, design, paper drafting, and revision for important intellectual content: MA; providing the legal framework, data collection, and statistical analysis: FSI; contribution to the design, data analysis, and interpretation. All authors have read and approved the final manuscript and have agreed to be accountable for all aspects of the work: MG.
REFERENCES
- 1.Auckloo M, Davies BB. Post-mortem toxicology in violent fatalities in Cape Town, South Africa: A preliminary investigation. J Forensic Leg Med. 2019;63:18–25. doi: 10.1016/j.jflm.2019.02.005. [DOI] [PubMed] [Google Scholar]
- 2.Paul ABM, Simms L, Mahesan AA, Belanger EC. Teens, Drugs, and Vegas: Toxicological surveillance of illicit prescription and illegal drug abuse in adolescents (12-17 years) using post-mortem data in Clark County, Nevada from 2005 to 2015. J Forensic Leg Med. 2018;58:20–4. doi: 10.1016/j.jflm.2018.04.002. [DOI] [PubMed] [Google Scholar]
- 3.Rigg KK, Sharp A. Nonmedical prescription drug use among African Americans who use MDMA (ecstasy/molly): Implications for risk reduction. Addict Behav. 2018;79:159–65. doi: 10.1016/j.addbeh.2017.12.024. [DOI] [PubMed] [Google Scholar]
- 4.Akhgari M, Kahfi MS, Akha HS. Analysis of intoxication deaths: Causes and manners of death. ndian J Pharm Sci. 2019;81(1):32–8. [Google Scholar]
- 5.Barocas JA, Wang J, Marshall BDL, LaRochelle MR, Bettano A, Bernson D, et al. Sociodemographic factors and social determinants associated with toxicology confirmed polysubstance opioid-related deaths. Drug Alcohol Depend. 2019;200:59–63. doi: 10.1016/j.drugalcdep.2019.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ghane T, Zamani N, Hassanian-Moghaddam H, Beyrami A, Noroozi A. Lead poisoning outbreak among opium users in the Islamic Republic of Iran, 2016-2017. Bull World Health Organ. 2018;96(3):165–72. doi: 10.2471/BLT.17.196287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kordrostami R, Akhgari M, Ameri M, Ghadipasha M, Aghakhani K. Forensic toxicology analysis of self-poisoning suicidal deaths in Tehran, Iran; trends between 2011-2015. Daru. 2017;25(1):15. doi: 10.1186/s40199-017-0181-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barzegar A, Shahbazi F, Mirtorabi D, Ghadirzadeh MR, Shojaei A, Hashemi Nazari SS. Quantification of mortality rate from illicitsubstance abuse in Iran in 2016. International Journal of Medical Toxicology and Forensic Medicine. 2018;8(4):123–30. [Google Scholar]
- 9.Titidezh V, Arefi M, Taghaddosinejad F, Behnoush B, Akbar PS, Mahboobi M. Epidemiologic profile of deaths due to drug and chemical poisoning in patients referred to Baharloo Hospital of Tehran, 2011 to 2014. J Forensic Leg Med. 2019;64:31–3. doi: 10.1016/j.jflm.2019.02.009. [DOI] [PubMed] [Google Scholar]
- 10.Turner C, Chandrakumar D, Rowe C, Santos GM, Riley ED, Coffin PO. Cross-sectional cause of death comparisons for stimulant and opioid mortality in San Francisco, 2005-2015. Drug Alcohol Depend. 2018;185:305–12. doi: 10.1016/j.drugalcdep.2017.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Seth P, Scholl L, Rudd RA, Bacon S. Overdose deaths involving opioids, cocaine, and psychostimulants - United States, 2015-2016. MMWR Morb Mortal Wkly Rep. 2018;67(12):349–58. doi: 10.15585/mmwr.mm6712a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hernandez I, He M, Brooks MM, Zhang Y. Exposure-response association between concurrent opioid and benzodiazepine use and risk of opioid-related overdose in medicare part D beneficiaries. JAMA Netw Open. 2018;1(2):e180919. doi: 10.1001/jamanetworkopen.2018.0919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Metz VE, Brown QL, Martins SS, Palamar JJ. Characteristics of drug use among pregnant women in the United States: Opioid and non-opioid illegal drug use. Drug Alcohol Depend. 2018;183:261–6. doi: 10.1016/j.drugalcdep.2017.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The European Monitoring Centre for Drugs and Drug Addiction (EMCDDA). [cited 2017 Jun]; Available from: URL: https://www.emcdda.europa. European Drug Report 2017: Trends and Developments [Online]. 2017. Available from: URL: https://www.emcdda.europa.eu/publications/edr/trends-developments/2017_en.
- 15.Mazak K, Noszal B, Hosztafi S. Advances in the physicochemical profiling of opioid compounds of therapeutic interest. ChemistryOpen. 2019;8(7):879–87. doi: 10.1002/open.201900115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bahmanabadi L, Akhgari M, Jokar F, Sadeghi HB. Quantitative determination of methamphetamine in oral fluid by liquid-liquid extraction and gas chromatography/mass spectrometry. Hum Exp Toxicol. 2017;36(2):195–202. doi: 10.1177/0960327116638728. [DOI] [PubMed] [Google Scholar]
- 17.Behnoush B, Bazmi E, Akhgari M, Hashemi Nazari SS, Sardari Iravani F. Evaluation of ethanol and N-propanol in victims. Iran J Toxicol. 2010;3(3):311–6. [Google Scholar]
- 18.Handanagic S, Bozicevic I, Sekerija M, Rutherford GW, Begovac J. Overdose mortality rates in Croatia and factors associated with self-reported drug overdose among persons who inject drugs in three Croatian cities. Int J Drug Policy. 2019;64:95–102. doi: 10.1016/j.drugpo.2018.11.017. [DOI] [PubMed] [Google Scholar]
- 19.Wang LL, Zhang M, Zhang W, Li BX, Li RB, Zhu BL, et al. A retrospective study of poisoning deaths from forensic autopsy cases in northeast China (Liaoning). J Forensic Leg Med. 2019;63:7–10. doi: 10.1016/j.jflm.2019.02.008. [DOI] [PubMed] [Google Scholar]
- 20.Shahraki G, Sedaghat Z, Fararouei M. Withdrawing attempt and its related factors among Iranian substance users: A case-control study. Subst Abuse Treat Prev Policy. 2018;13(1):45. doi: 10.1186/s13011-018-0184-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taremian F, Yaghubi H, Pairavi H, Hosseini SR, Zafar M, Moloodi R. Risk and protective factors for substance use among Iranian university students: A national study. Subst Abuse Treat Prev Policy. 2018;13(1):46. doi: 10.1186/s13011-018-0181-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grigsby TJ, Howard JT. Prescription opioid misuse and comorbid substance use: Past 30-day prevalence, correlates and co-occurring behavioral indicators in the 2016 National Survey on Drug Use and Health. Am J Addict. 2019;28(2):111–8. doi: 10.1111/ajad.12866. [DOI] [PubMed] [Google Scholar]
- 23.Hassan AN, Le Foll B. Polydrug use disorders in individuals with opioid use disorder. Drug Alcohol Depend. 2019;198:28–33. doi: 10.1016/j.drugalcdep.2019.01.031. [DOI] [PubMed] [Google Scholar]
- 24.VanHouten J, Rudd R, Ballesteros M, Mack K. Drug overdose deaths among women aged 30-64 years - United States, 1999-2017. MMWR Morb Mortal Wkly Rep. 2019;68(1):1–5. doi: 10.15585/mmwr.mm6801a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Anzillotti L, Marezza F, Calo L, Cucurachi N, Veronesi L, Cecchi R. Toxicological findings: A retrospective overview of medico-legal investigations in Parma (Italy). J Forensic Leg Med. 2019;62:92–6. doi: 10.1016/j.jflm.2019.01.011. [DOI] [PubMed] [Google Scholar]
- 26.Clinton HA, Hunter AA, Logan SB, Lapidus GD. Evaluating opioid overdose using the National Violent Death Reporting System, 2016. Drug Alcohol Depend. 2019;194:371–6. doi: 10.1016/j.drugalcdep.2018.11.002. [DOI] [PubMed] [Google Scholar]
- 27.Tuusov J, Vals K, Tonisson M, Riikoja A, Denissov G, Vali M. Fatal poisoning in Estonia 2000-2009. Trends in illegal drug-related deaths. J Forensic Leg Med. 2013;20(1):51–6. doi: 10.1016/j.jflm.2012.04.023. [DOI] [PubMed] [Google Scholar]
- 28.Alam-Mehrjerdi Z, Abdollahi M, Higgs P, Dolan K. Drug use treatment and harm reduction programs in Iran: A unique model of health in the most populated Persian Gulf country. Asian J Psychiatr. 2015;16:78–83. doi: 10.1016/j.ajp.2015.06.002. [DOI] [PubMed] [Google Scholar]
- 29.Konstantinova-Larsen SV, Normann PT, Arnestad M, Karinen R, Christophersen AS, Morland J. Surveillance of abused drugs in forensic autopsy cases in Norway. Nor J Epidemiol. 2011;21(1):43–8. [Google Scholar]
- 30.Hedenmalm K, Slattery J, Skibicka-Stepien I, Kurz X, Morales D. Prescribing patterns of tramadol in adults in IMS(R) primary care databases in France and Germany between 1 January 2006 and 30 June 2016. Eur J Clin Pharmacol. 2019;75(5):707–16. doi: 10.1007/s00228-018-02622-9. [DOI] [PubMed] [Google Scholar]
- 31.Mital S, Windle M, Cooper HL, Crawford ND. Trends in non-medical prescription opioids and heroin co-use among adults, 2003-2014. Addict Behav. 2018;86:17–23. doi: 10.1016/j.addbeh.2018.05.005. [DOI] [PubMed] [Google Scholar]
- 32.Fischer B, Patra J, Cruz MF, Gittins J, Rehm J. Comparing heroin users and prescription opioid users in a Canadian multi-site population of illicit opioid users. Drug Alcohol Rev. 2008;27(6):625–32. doi: 10.1080/09595230801956124. [DOI] [PubMed] [Google Scholar]
- 33.Jones AW, Holmgren A, Ahlner J. Post-mortem concentrations of drugs determined in femoral blood in single-drug fatalities compared with multi-drug poisoning deaths. Forensic Sci Int. 2016;267:96–103. doi: 10.1016/j.forsciint.2016.08.015. [DOI] [PubMed] [Google Scholar]
- 34.Hedegaard H, Warner M, Minino AM. Drug overdose deaths in the United States, 1999-2015. NCHS data brief, no 273. Hyattsville, MD: National Center for Health Statistics; 2017. [Google Scholar]
- 35.Substance Abuse. Key substance use and mental health indicators in the United States: Results from the 2017 National Survey on Drug Use and Health (HHS Publication No. SMA 18-5068, NSDUH Series H-53). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2018. [Google Scholar]
- 36.United Nations Office on Drugs and Crime (UNODC). World Drug Report 2017. Vienna, Austria: United Nations Publication; 2017. [Google Scholar]
- 37.Alam-Mehrjerdi Z, Abdollahi M. The Persian methamphetamine use in methadone treatment in Iran: Implication for prevention and treatment in an upper-middle income country. Daru. 2015;23:51. doi: 10.1186/s40199-015-0134-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shariatirad S, Maarefvand M, Ekhtiari H. Methamphetamine use and methadone maintenance treatment: An emerging problem in the drug addiction treatment network in Iran. Int J Drug Policy. 2013;24(6):e115–6. doi: 10.1016/j.drugpo.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 39.Eastwood B, Strang J, Marsden J. Change in alcohol and other drug use during five years of continuous opioid substitution treatment. Drug Alcohol Depend. 2019;194:438–46. doi: 10.1016/j.drugalcdep.2018.11.008. [DOI] [PubMed] [Google Scholar]
- 40.Akhgari M, Amini-Shirazi N, Iravani FS. Forensic toxicology perspectives of methadone-associated deaths in Tehran, Iran, a 7-year overview. Basic Clin Pharmacol Toxicol. 2018;122(4):436–41. doi: 10.1111/bcpt.12930. [DOI] [PubMed] [Google Scholar]
- 41.Argo A, Spatola GF, Zerbo S, Sortino C, Lanzarone A, Uzzo ML, et al. A possible biomarker for methadone related deaths. J Forensic Leg Med. 2017;49:8–14. doi: 10.1016/j.jflm.2017.05.010. [DOI] [PubMed] [Google Scholar]
- 42.Gharehdaghi J, Takalloo-Bakhtiari A, Hassanian-Moghaddam H, Zamani N, Hedayatshode MJ. Suspected methadone toxicity: From hospital to autopsy bed. Basic Clin Pharmacol Toxicol. 2017;121(6):531–9. doi: 10.1111/bcpt.12831. [DOI] [PubMed] [Google Scholar]
- 43.United Nations Office on Drugs and Crime (UNODC). World Drug Report 2011. Vienna, Austria: United Nations Publication; 2011. [Google Scholar]
- 44.United Nations Office on Drugs and Crime (UNODC). Afghan opiate trafficking along the northern route. Vienna, Austria: United Nations Office on Drugs and Crime; 2018. [Google Scholar]
- 45.Mohanty S, Tripathy R, Palo SK, Jena D. Socioeconomic, demographic study on substance abuse among students of professional college in a southern town, Berhampur of Odisha state (India). J Forensic Leg Med. 2013;20(8):1057–62. doi: 10.1016/j.jflm.2013.09.018. [DOI] [PubMed] [Google Scholar]