Abstract
The aim of the study was to assess the short-term consequences of SARS-CoV-2-related pneumonia, also in relation to radiologic/laboratory/clinical indices of risk at baseline. This prospective follow-up cohort study included 94 patients with confirmed COVID-19 admitted to a medical ward at the Montichiari Hospital, Brescia, Italy from February 28th to April 30th, 2020. Patients had COVID-19 related pneumonia with respiratory failure. Ninety-four patients out of 193 survivors accepted to be re-evaluated after discharge, on average after 4 months. In ¼ of the patients an evidence of pulmonary fibrosis was detected, as indicated by an altered diffusing capacity of the lung for carbon monoxide (DLCO); in 6–7% of patients the alteration was classified as of moderate/severe degree. We also evaluated quality of life thorough a structured questionnaire: 52% of the patients still lamented fatigue, 36% effort dyspnea, 10% anorexia, 14% dysgeusia or anosmia, 31% insomnia and 21% anxiety. Finally, we evaluated three prognostic indices (the Brixia radiologic score, the Charlson Comorbidity Index and the 4C mortality score) in terms of prediction of the clinical consequences of the disease. All of them significantly predicted the extent of short-term lung involvement. In conclusion, our study demonstrated that SARS-CoV-2-related pneumonia is associated to relevant short-term clinical consequences, both in terms of persistence of symptoms and in terms of impairment of DLCO (indicator of a possible development of pulmonary fibrosis); some severity indices of the disease may predict short-term clinical outcome. Further studies are needed to ascertain whether such manifestations may persist long-term.
Keywords: COVID-19, SARS-CoV2, Lung fibrosis, Interstitial lung disease, Prognostic factors, Sequelae
Introduction
Coronavirus disease 2019 (COVID-19) pandemic represented, and still represents, a major clinical problem in Lombardy, one of the most affected Italian (and worldwide) regions; a high toll of victims was paid. In our clinical ward, a mortality rate of 25% was observed during the first pandemic outbreak (March–April 2020) [1].
However, a major issue is represented by the incidence of clinical sequelae of the disease, since it is not known which proportion of patients will develop pulmonary fibrosis (interstitial lung diseases, ILD). Available data are scarce [2, 3] or even anecdotal [4, 5].
Predicting factors determining outcome prognosis of patients that develop interstitial pneumonia with respiratory failure have been investigated; among them gender, hypertension, obesity, diabetes and other cardiovascular disorders seems be substantially associated with SARS-CoV-2 infection and with poor outcome [1, 6–9]. In fact, the severity of the primary respiratory syndrome is increased in patients with pre-existing cardiovascular disease [1, 6, 7, 10, 11], as also documented by the association of the Charlson Comorbidity Index with the clinical outcome [7] and with the chance of healing [9].
Also, the severity of the lung involvement may be relevant from a prognostic point of view. The Brixia score is a radiologic score proposed by Borghesi and Maroldi [12] to assess severity of SARS-CoV-2 pneumonia, whose prognostic meaning was clearly demonstrated [1, 13, 14].
Also, the “4C mortality score” was suggested to be useful for risk stratification of patients with COVID-19 [15]. This index predicts in-hospital mortality in patients admitted with COVID-19, and considers age, comorbidities, respiratory rate, peripheral oxygen saturation, Glasgow coma scale and other laboratory and clinical parameters [15].
It was also postulated that some clinical symptoms [16] and psychological involvement [17, 18] may persist after the resolution of the acute phase of the disease.
For all these reasons we considered worthwhile to assess, in a prospective follow-up cohort study, the short-term clinical consequences of SARS-CoV-2-related pneumonia, also in relation to radiologic/laboratory/clinical indices of risk at baseline in our population of survivors to COVID-19.
Methods
Patients
We conducted a prospective cohort study at the Montichiari Hospital, a tertiary health-care center in Brescia, Italy, which was designated as a COVID-19 hub by the Italian health authorities.
Two hundred and fifty-eight patients admitted to General Medicine ward (COVID-19 M unit) of the Montichiari Hospital from February 28th to April 30th, 2020 were included in the study if they met the following inclusion criteria: (1) confirmed COVID-19 infection as determined by a positive reverse-transcriptase-polymerase-chain-reaction (RT-PCR) assay of a specimen collected on a nasopharyngeal swab; (2) bilateral pulmonary interstitial opacities on chest imaging that were not fully explained by congestive heart failure or other forms of volume overload; (3) an acute respiratory distress syndrome showing at least one of the following conditions: respiratory rate ≥ 30 breaths/min; peripheral capillary oxygen saturation (SpO2) ≤ 93% while breathing ambient air or ratio of the partial pressure of oxygen in arterial blood to the fractional concentration of oxygen in inspired air (PaO2/FiO2) ≤ 300 mmHg. Sixty-five of them died during or after the admission to the hospital. All 193 surviving patients were invited to participate to a follow up program that included: a clinical assessment, standard laboratory testing, a chest X-ray, lung function tests with an evaluation of the diffusing capacity of the lung for carbon monoxide (DLCO), and, in case of the presence of alterations in such a test, a computed tomography (CT) scan of the chest. In addition, to assess the persistence/new onset of symptoms and/or psychological distress, a structured questionnaire was administered. The following items were investigated: presence/absence of fatigue, effort dyspnea, anorexia, dysgeusia, insomnia and anxiety.
Ninety-four patients out of 193 survivors accepted to be re-evaluated after discharge, on average after 4 months. The follow-up ended in August 2020.
The following laboratory parameters were evaluated at hospital admission, at the time of discharge and at the time of follow up: circulating white blood cells, granulocytes, monocytes, lymphocytes, and hemoglobin, c-reactive protein (CRP), procalcitonin, ferritin, D-dimer, international normalised ratio (INR) and activated partial thromboplastin time (aPTT), plasma creatinine and electrolytes, aspartate aminotransferase (AST), alanine aminotransferase (ALT), gamma glutamyl transferase (γGT) and urinalysis. This study has been conducted in accordance with the declaration of Helsinki and was approved by the Ethical Committee of the Spedali Civili of Brescia.
Drug treatment during admission Patients admitted to our Division of Medicine underwent standard therapy (hydroxychloroquine 400 mg daily, lopinavir 800 mg daily plus ritonavir 200 mg per day) [17–19], according to indications of our Institution at that time based on available information [19]. Some patients could not be treated with antiviral agents or antimalarial agents because such drugs were not always available due to the excessive requests from hospitals. In a subgroup of patients with severe respiratory distress intravenous corticosteroids (dexamethasone 20 mg intravenously per day for 5 days and then 10 mg i.v. per day for 5 days) were used, while another subgroup of patients received off-label a single low dose administration of the anti-interleukin-6 monoclonal antibody Tocilizumab (8 mg/kg i.v.- or 324 mg subcutaneous -s.c.- depending on the drug availability) in addition to standard therapy [20, 21]. During hospitalization, patients in both groups were assisted with non-invasive (i.e. low flow nasal cannula; high flow mask; Continuous Positive Airway Pressure –CPAP-) or invasive (i.e. mechanical ventilation) oxygen therapy, according to their needs. For further clinical information see reference [1].
Prognostic indices In 64 patients the Brixia radiologic score was evaluated at hospital admission and at follow up, according to Borghesi and Maroldi [12]. Briefly, a score (from 0 to 3) is assigned to each of previously defined pulmonary zones based on the lung abnormalities detected on frontal chest projection as follows: score 0 (zero) no lung abnormalities; score 1 interstitial infiltrates, score 2 interstitial and alveolar infiltrates (interstitial predominance), score 3 interstitial and alveolar infiltrates (alveolar predominance). The scores of the six lung zones are then added to obtain an overall score ranging from 0 to 18.
For each patient, we calculated the Charlson Comorbidity Index (CCI) based on the available data [22]. This index takes into account age and coexisting conditions, in an algorithm used also to predict 10-year mortality. The percentage of COVID-19 related deaths increases with the Charlson Index [7]; this index was a logarithmic multiplier when the risk of death was assessed by increasing by one point the score, starting from the score of 2 [7, 22]. It was previously demonstrated, in a similar population, that such an index predicts mortality with an exponential increase in the odds ratio by each point. The Charlson index was calculated as absolute values and as predicted mortality at 10 years [22]. In addition, we calculated also the 4 C mortality score for COVID-19, according to Knight et al. [15].
Statistical Analyses
Data were analyzed with SPSS version 25.0 (Chicago, IL, USA). We report categorical variables as number (%) and continuous variables as mean (standard deviation) when data were normally distributed, and as median and interquartile range when data were not normally distributed (lymphocytes, procalcitonin, ferritin, D-dimer). Statistical significance between groups was assessed by means of Chi-square test for dichotomous variables, or by means of one-way analysis of variance (ANOVA) or by Mann–Whitney U test when appropriate. A multivariate Cox regression analysis was also performed considering the whole period of observation (from hospital admission to follow up) and the outcome in terms of normal or altered DLCO (% of predicted).
A P value < 0.05 was considered as statistically significant.
Results
A total of 94 patients were included in the current study. Baseline demographic and clinical characteristics of patients are similar to those observed in the general population of 258 patients admitted to our medical ward in that period and described elsewhere [1]. In particular, no major difference in risk factors or other clinical parameters was present between those who did or did not respond to our follow up call.
Lung function tests Parameter obtained through the evaluation of DLCO are detailed in reference [23] and criteria for definition of normalcy and/or extent of the impairment are detailed in reference [24]. Briefly, a DLCO (% of predicted) ≥ 80% was considered as normal; < 80% and ≥ 60%: mild impairment; < 60% and ≥ 40%: moderate impairment; < 40%: severe impairment. Similar cutpoints were adopted for DLCO/VA (alveolar volume) = transfer coefficient of the lung for carbon monoxide (KCO) (% of predicted). Data are reported in Table 1.
Table 1.
Lung function tests
| Population: n = 94 | DLCO (% of predicted) | DLCO/VA (KCO) (% of predicted) |
|---|---|---|
| Normal (n, %) | 57 (60.6%) | 71 (75.5%) |
| Altered (n, %) (any alteration) | 37 (39.3%) | 23 (24.5%) |
| Mild alteration (n, %) | 30 (31.9%) | 17 (18.1%) |
| Moderate alteration (n, %) | 4 (4.26%) | 5 (5.32%) |
| Severe alteration (n, %) | 3 (3.19%) | 1 (1.06%) |
| Moderate + severe alteration (n, %) | 7 (7.45%) | 6 (6.38%) |
In ¼ of the patients an evidence of pulmonary fibrosis was detected, as indicated by an altered diffusing capacity of the lung for carbon monoxide (DLCO); in 6–7% of the patients the alteration was classified as of moderate/severe degree. In all these cases the chest CT scan confirmed the presence of indices of pulmonary fibrosis. Those patients that were ventilated with CPAP or that have needed high oxygen flow (> than the median oxygen flow—FiO2 value) had a worse DLCO pattern compared with those needing lower oxygen flows according to a Chi-square tests (Table 2). This is further confirmed by the observation of a significant inverse correlation between FiO2 and DLCO (% of predicted): r = − 0.224, p = 0.003. There was also an association between days on oxygen supplementation during the acute phase of COVID-19 and DLCO (% predicted) r = − 0.186; p = 0.010. Laboratory parameters of the patients with normal or altered lung function tests as well as values of parameter measured with lung function test are reported in Tables 3, 4.
Table 2.
Lung function tests in ventilated/high FiO2 patients vs. not ventilated/low FiO2 patients
| DLCO (% of predicted) | DLCO/VA (KCO) (% of predicted) | |
|---|---|---|
| Ventilated or high FiO2 (≥ 28%): n = 47 | 81.2 ± 18.3 | 89.5 ± 20.5 |
| Normal (n, %) | 23 (48.9%) | 35 (74.5%) |
| Altered (n, %) (any alteration) | 24 (51.1%) | 12 (25.5%) |
| Mild alteration (n, %) | 19 (40.4%) | 8 (17.0%) |
| Moderate alteration (n, %) | 4 (8.51%) | 4 (8.512%) |
| Severe alteration (n, %) | 1 (2.13%) | 0 (0%) |
| Moderate + severe alteration (n, %) | 5 (10.6%) | 4 (8.51%) |
| Not ventilated and low FiO2 (< 28%): n = 47 | 87.3 ± 18.3 | 93.1 ± 2.5 |
| Normal (n, %) | 34 (72.3%) | 36 (76.6%) |
| Altered (n,%) (any alteration) | 13 (27.7%) | 11 (23.4%) |
| Mild alteration (n, %) | 11 (23.4%) | 9 (19.1%) |
| Moderate alteration (n, %) | 0 (0%) | 1 (2.13%) |
| Severe alteration (n, %) | 2 (4.25%) | 1 (2.13%) |
| Moderate + severe alteration (n, %) | 2 (4.25%) | 2 (4.25%) |
DLCO (% of predicted): Chi square test (Normal/altered − Ventilated or high FiO2/Not ventilated and low FiO2): p = 0.003
DLCO/VA (KCO) (% of predicted): Chi square test (Normal/altered − Ventilated or high FiO2/Not ventilated and low FiO2): p = 0.33 (NS)
Table 3.
Laboratory parameters and lung function tests in the two groups of patients (normal or altered DLCO % of predicted)
| Normal lung function tests (n = 57) | Abnormal lung function tests (n = 37) | All patients (n = 94) | |
|---|---|---|---|
|
Humoral parameters: White blood cells (#/mm3) |
6000 ± 2600 | 6380 ± 2920 | 6170 ± 2730 |
| Granulocytes (#/mm3) | 4400 ± 2600 | 4860 ± 2650 | 4590 ± 2590 |
| Monocytes (#/mm3) | 429 ± 376 | 485 ± 578 | 410 ± 210 |
| Lymphocytes (#/mm3) | 1940 (950) | 2120 (1200) | 2014 (980) |
| Hemoglobin (g/dL) | 13.3 ± 1.6 | 12.3 ± 1.77 ** | 12.9 ± 1.64 |
| Platelets (# × 103/mm3) | 205 ± 72 | 229 ± 99 | 215 ± 84 |
| CRP (mg/L) | 76.1 ± 61.5 | 115.9 ± 94.9 * | 91.8 ± 78.4 |
| Ferritin (µg/L) | 148 (115) | 113 (161) | 141 (142) |
| D-dimer (ng/mL) | 220 ± 80.4 | 398 ± 485 * | 297 ± 332 |
| Creatinine (mg/dL) | 0.94 ± 0.26 | 0.99 ± 0.45 | 0.96 ± 0.35 |
| AST | 52 ± 52 | 44 ± 29 | 49 ± 40 |
| ALT | 43 ± 46 | 32 ± 25 | 39 ± 39 |
| INR | 1.2 ± 0.2 | 1.3 ± 0.3 | 1.3 ± 0.3 |
| aPTT (s) | 33.1 ± 4.3 | 33.0 ± 4.3 | 33.1 ± 4.3 |
| Lung function test | |||
| FVC (L) | 4.1 ± 1.0 | 3.3 ± 0.8*** | 3.8 ± 1.0 |
| FEV1 (L) | 3.2 ± 0.7 | 2.6 ± 0.7*** | 3.0 ± 0.8 |
| DLCO (mL/min/mmHg) | 23.5 ± 5.7 | 15.5 ± 2.8*** | 20.4 ± 6.2 |
| VA (mL/min) | 5.5 ± 1.0 | 4.4 ± 0.9*** | 5.1 ± 1.1 |
| VA % predicted. | 89.5% ± 10.9% | 78.5% ± 15.9%*** | 84.8% ± 14.2% |
| DLCO % predicted | 94.9 ± 14.2 | 66.8 ± 8.6*** | 84.2 ± 18.4 |
| DLCO/VA% predicted (= KCO) | 97.0 ± 20.1 | 82.2 ± 19.3*** | 91.2 ± 21.0 |
| FEV1/FVC | 78.7% ± 7.2% | 78.5% ± 10.9% | 78.6% ± 8.8% |
| DLCO/VA | 4.3 ± 0.6 | 3.6 ± 0.8*** | 4.03 ± 0.8 |
Table 4.
Laboratory parameters and lung function tests in the two groups of patients (normal or altered DLCO/VA % of predicted)
| Normal Lung function tests (n = 71) | Abnormal Lung function tests (n = 23) | All patients (n = 94) | |
|---|---|---|---|
| Humoral parameters: White blood cells (#/mm3) | 6200 ± 2600 | 6000 ± 3100 | 6170 ± 2730 |
| Granulocytes (#/mm3) | 4700 ± 2500 | 4400 ± 2900 | 4590 ± 2590 |
| Monocytes (#/mm3) | 410 ± 220 | 430 ± 210 | 410 ± 210 |
| Lymphocytes (#/mm3) | 2010 (980) | 2320 (1140) | 2014 (980) |
| Hemoglobin (g/dl) | 13.0 ± 1.5 | 12.7 ± 2.1 | 12.9 ± 1.64 |
| Platelets (# × 103/mm3) | 216 ± 87 | 211 ± 78 | 215 ± 84 |
| CRP (mg/L) | 93.8 ± 74.2 | 85.5 ± 91.7 | 91.8 ± 78.4 |
| Ferritin (µg/L) | 147 (140) | 119 (125) | 141 (142) |
| D-dimer (ng/ml) | 270 ± 325 | 384 ± 350* | 297 ± 332 |
| Creatinine (mg/dl) | 0.96 ± 0.27 | 0.97 ± 0.53 | 0.96 ± 0.35 |
| AST | 53 ± 44 | 36 ± 20* | 49 ± 40 |
| ALT | 42 ± 43 | 29 ± 22 | 39 ± 39 |
| INR | 1.26 ± 0.26 | 1.32 ± 0.40 | 1.3 ± 0.3 |
| aPTT (s) | 32.5 ± 3.5 | 35.0 ± 5.8 | 33.1 ± 4.3 |
| Lung function test | |||
| FVC (L) | 3.88 ± 1.04 | 3.48 ± 081 | 3.8 ± 1.0 |
| FEV1 (L) | 3.04 ± 0.76 | 2.71 ± 0.72 | 3.0 ± 0.8 |
| DLCO (mL/min/mmHg) | 21.3 ± 6.4 | 17.8 ± 4.3** | 20.4 ± 6.2 |
| VA (ml/min) | 5.1 ± 1.2 | 5.1 ± 0.9 | 5.1 ± 1.1 |
| VA % predicted | 83.9% ± 14.0% | 93.7% ± 14.8% | 84.8% ± 14.2% |
| DLCO % predicted | 87.2 ± 18.2 | 74.7 ± 13.6** | 84.2 ± 18.4 |
| DLCO/VA% predicted (= KCO) | 98.8 ± 17.9 | 66.8 ± 6.5*** | 91.2 ± 21.0 |
| FEV1/FVC | 79.1% ± 9.1% | 77.0% ± 7.94% | 78.6% ± 8.8% |
| DLCO/VA | 4.2 ± 0.7 | 3.5 ± 0.6*** | 4.03 ± 0.8 |
CRP C-reactive protein, AST aspartate transaminase, ALT alanine aminotransferase, INR international normalized ratio, aPTT activated partial thromboplastin time, FVC forced vital capacity, FEV1 forced expiratory volume in one second, DLCO diffusing capacity of lung for carbon monoxide, VA alveolar volume, pred predicted
One-way ANOVA: *p < 0.05, **0 < 0.01, ***p < 0.001 vs. normal
There were no differences between patients previously treated or not with antiviral agents, steroids, antimalaric agents or tocilizumab in terms of DLCO.
We observed some correlations between parameters derived from arterial blood sample and lung function test. In particular, a significant correlation was observed between PaO2/FiO2 (a reliable index of blood perfusion) and FVC (r = 0.30, p = 0.005), FEV1 (r = 0.33, p = 0.002), DLCO (r = 0.29, p = 0.006), % of predicted DLCO (r = 0.37, p < 0.001), probably due to the fact that patients with lower PaO2/FiO2 at the time of admission had a more severe COVID-19. In addition, a correlation was observed between duration of the hospitalization and % of predicted DLCO (r = − 0.31, p = 0.002).
Quality of life questionnaire As mentioned, we also evaluated the quality of life thorough a structured questionnaire: 52% of the patients still lamented fatigue, 36% effort dyspnea, 10% anorexia, 14% dysgeusia, 31% insomnia and 21% anxiety. Data are reported in Table 5.
Table 5.
Quality of life questionnaire
| Population: n = 91 | Yes | No |
|---|---|---|
| Fever (n, %) | 0 (0%) | 91 (100%) |
| Fatigue (n, %) | 47 (52%) | 44 (485%) |
| Effort dyspnea (n, %) | 33 (36%) | 58 (64%) |
| Anorexia (n, %) | 9 (10%) | 82 (90%) |
| Insomnia (n, %) | 28 (31%) | 63 (61%) |
| Anxiety (n, %) | 19 (21%) | 71 (78%) |
| Dysgeusia or anosmia (n, %) | 13 (14%) | 78 (86%) |
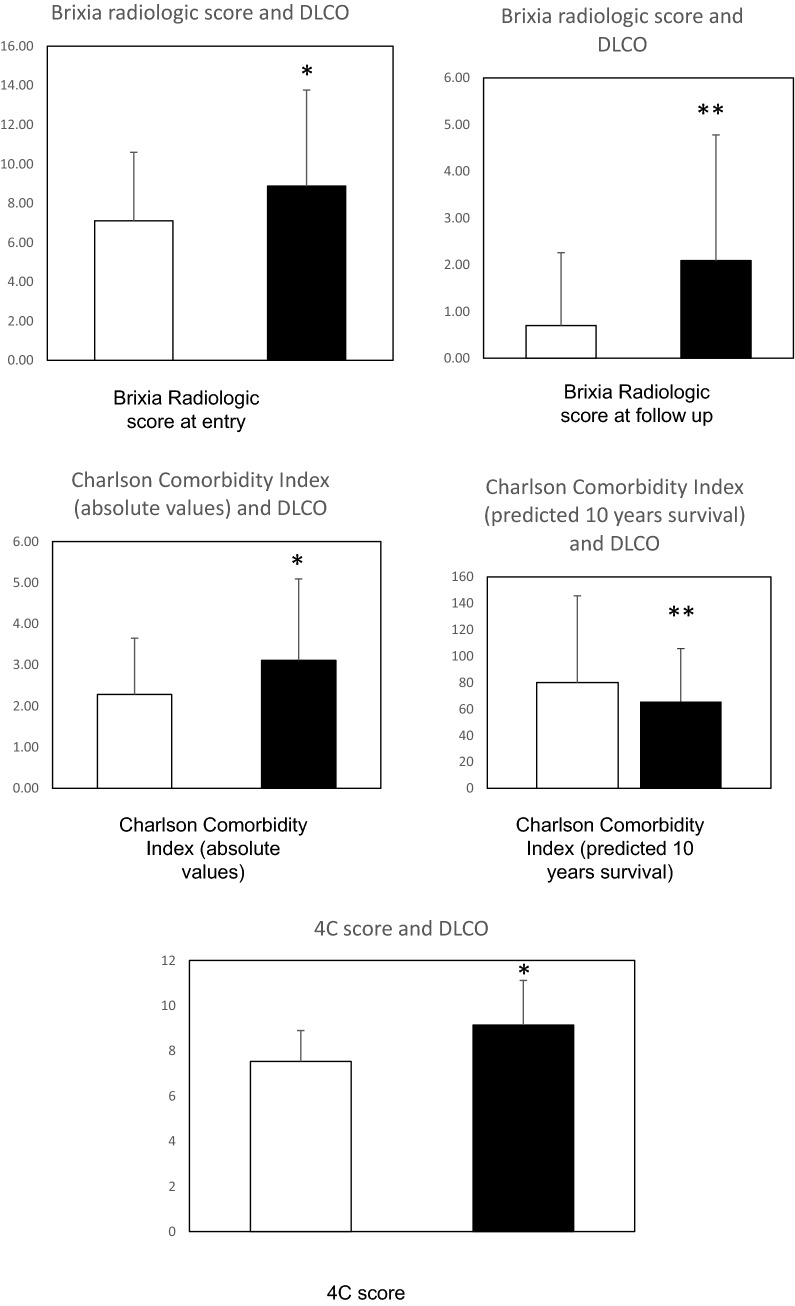
Prognostic indices The Brixia radiologic score both calculated at hospital admission and at follow up was significantly correlated with predicted DLCO but not with predicted DLCO/VA (Table 6). When patients were subdivided according to the presence of a normal or altered predicted DLCO (any alteration), the Brixia radiologic score was significantly higher in patients with altered DLCO at follow up (Fig. 1).
Table 6.
Correlations between Brixia radiologic score, Charlson Comorbidity Index and 4C Mortality Score and lung function tests
| r | P | |
|---|---|---|
| Brixia score at entry and predicted DLCO | − 0.245 | 0.05 |
| Brixia score at entry and predicted DLCO/VA | 0.045 | NS |
| Brixia score at follow up and predicted DLCO | − 0.376 | < 0.001 |
| Brixia score at follow up and predicted DLCO/VA | − 0.095 | NS |
| Charlson Comorbidity Index (absolute values) and | ||
| Predicted DLCO | − 0.229 | 0.028 |
| Predicted DLCO/VA | − 0.091 | NS |
| Charlson Comorbidity Index (survival at 10 years) and | ||
| Predicted DLCO | − 0.242 | 0.020 |
| Predicted DLCO/VA | 0.144 | NS |
| 4C Mortality Score and | ||
| Predicted DLCO | − 0.213 | 0.042 |
| Predicted DLCO/VA | 0.147 | NS |
Fig. 1.
Brixia radiologic score (at hospital admission and at follow up, top panel), Charlson Comorbidity Index (absolute values and predicted 10 years survival: middle panel) and 4C score (bottom panel) in patients with normal (n = 57, empty bars) or abnormal (n = 37, full bars) DLCO (% of predicted). One-way ANOVA: * = p < 0.05, ** = p < 0.01
Also Charlson Comorbidity Index significantly correlated with predicted DLCO in a direct way when absolute values were considered, while survival at 10 years was inversely correlated with DLCO (Table 6). Similarly, those patients with altered DLCO had significantly different Charlson Comorbidity Indices (Fig. 1). A similar result was obtained for 4C mortality score and predicted DLCO (Table 6, Fig. 1). No association with predicted DLCO/VA and risk score was observed.
A multivariate Cox regression analysis was also performed considering the outcome in terms of predicted DLCO (normal/altered: any alteration) and all the previously mentioned risk scores as prognostic factors; only the Brixia radiologic score evaluated at follow up remained in the model and were found to be significantly and independently associated with the occurrence of death (P = 0.027).
Discussion
COVID-19 has been associated with a very high mortality rate being interstitial pneumonia with respiratory failure the main cause of death [1, 6]. Among COVID-19 patients, about 25% present a severe complication of infection including acute respiratory distress syndrome (ARDS), with a rapid worsening of clinical conditions leading to the need of mechanical or invasive ventilation to support respiratory functions in intensive care units [25]. Although the direct cytopathic effect of the virus and viral invasion seems to be critical for a worsening of the clinical course, there is evidence that other factors may be implicated in the prognosis of the acute respiratory distress syndrome, including age and comorbidity [1, 7].
Some reports have suggested that a number of patients may have short-medium-term consequences of the disease, in terms of development of ILD/pulmonary fibrosis [4, 5]. However, the precise prevalence of potentially long-lasting lung consequences of the disease is uncertain.
In a retrospective study of 57 COVID-19 patients [3], abnormalities were detected in the pulmonary function tests in 43 (75.4%) of the patients, and 30 (52.6%) patients had DLCO values less than 80% of predicted values. Thirty-one patients (54.3%) had abnormal CT findings. However, the follow up period was restricted to the early convalescence phase (30 days after discharge from the hospital), therefore these findings may be regarded as short-term clinical sequelae of the disease.
Similarly, a study has enrolled 60 COVID-19 patients assessed 12 weeks after symptoms onset [2]. At least one pulmonary function variable was abnormal in 58% of patients and 88% had abnormal imaging on chest CT. An abnormal DLCO was present in 52% of patients. There was a strong association between days on oxygen supplementation during the acute phase of COVID-19 and both DLCO (% predicted) and total CT score [2]. A persistence of some symptoms, including dyspnea (20% of patients) was observed [2]. The persistence of symptoms and radiologic abnormalities was confirmed in a study enrolling 55 patients; SARS-CoV-2 infection related symptoms were detected after 3 months in 35 of them and different degrees of radiological abnormalities were detected in 39 patients [26]. However, a crucial point is represented by the medium/long term reversibility of lung alterations. A larger study investigated 384 COVID-19 patients followed for a median of 54 days post discharge: 53% reported persistent breathlessness, 34% cough and 69% fatigue while 14.6% had depression; 38% of chest radiographs remained abnormal with 9% deteriorating [16]. Wong et al. found ground-glass opacity with reticulation and irregular interlobular septal thickening in 64 out of 70 (91.4%) patients on CT examination within 48 days after discharge. In that study, follow-up at 3 and 6 months showed the findings were largely unchanged [27, 28].
A severe psychological impact of COVID-19 was also documented, with 46.6% showing alterations at the Impact of Event Scale-Revised [17] while in another study 52.4% showed persistent symptoms of anxiety and depression [18].
While in some reports it was suggested that the lung damage due to COVID-19 could be, in great part, reversible [29], there are obviously still no long-term studies in this regard.
Another interesting result of our study is the observation that the Radiologic Brixia score [12], both evaluated at hospital admission and at follow up was a predictor of impairment of lung function at follow up, in particular in terms of DLCO (% of predicted). Also, the Charlson Comorbidity Index, both as absolute values and as estimation of survival at 10 years as well as the 4C Mortality Score were predictors of residual short/term impairment of lung function. However, according to a multivariate Cox regression analysis, only Brixia radiologic score at follow up is an independent predictor of pulmonary outcome. We could not use in our study the QCOVID score [30] since we did not evaluate body mass index in our hospital records.
However, these scores have substantial limitations [31, 32] and care must also be taken when interpreting the predictions generated by these models since they are poorly reported, at high risk of bias, and their performance probably optimistic [29, 30]. It should be acknowledged that correlations between risk scores and DLCO observed in our study, although statistically significant, were not particularly close, and this may be ascribed to the inherent limitations of any risk score in this context.
Another caveat is related to the fact that decreased DLCO may not always reflect pulmonary fibrosis. Pulmonary fibrosis implies an irreversible structural change of the lung which does not seem to occur even after acute respiratory distress syndrome (ARDS) of other origin as suggested by the long term continuous improvement of different lung function parameters, including DLCO, after 5 years after discharge from intensive care units because of ARDS [33].
Conclusions
In conclusion, our study demonstrated that SARS-CoV-2-related pneumonia is associated to relevant short-term clinical consequences, both in terms of persistence of symptoms and in terms of impairment of DLCO (indicator of a possible development of pulmonary fibrosis); some severity indices of the disease may predict short-term clinical outcome. Therefore, discharge may not be the end of treatment, since attentions should be paid to short-medium term sequelae of COVID-19 [34]. Further studies are however needed to ascertain whether such manifestations may persist long-term or even indefinitely [35].
Declarations
Funding
Open access funding provided by Università degli Studi di Brescia within the CRUI-CARE Agreement.
Conflict of interest
All authors declare no conflict of interests.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Availability of data and material/code availability
Not applicable.
Authors' contributions
Not applicable.
Contributor Information
Daniele Turini, Email: danieleturini79@gmail.com.
Damiano Rizzoni, Email: damiano.rizzoni@unibs.it.
References
- 1.Boari GEM, Chiarini G, Bonetti S, Malerba P, Bianco G, Faustini C, Braglia-Orlandini F, Turini D, Guarinoni V, Saottini M, Viola S, Ferrari-Toninelli G, Pasini G, Mascadri C, Bonzi B, Desenzani P, Tusi C, Zanotti E, Nardin M, Rizzoni D. Prognostic factors and predictors of outcome in patients with COVID-19 and related pneumonia: a retrospective cohort study. Biosci Rep. 2020;40(12):BSR20203455. doi: 10.1042/BSR20203455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shah AS, Wong AW, Hague CJ, Murphy DT, Johnston JC, Ryerson CJ, Carlsten C. A prospective study of 12-week respiratory outcomes in COVID-19-related hospitalisations. Thorax. 2020:thoraxjnl-2020-216308. [DOI] [PubMed]
- 3.Huang Y, Tan C, Wu J, Chen M, Wang Z, Luo L, Zhou X, Liu X, Huang X, Yuan S, Chen C, Gao F, Huang J, Shan H, Liu J. Impact of coronavirus disease 2019 on pulmonary function in early convalescence phase. Respir Res. 2020;21(1):163. doi: 10.1186/s12931-020-01429-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Picchi G, Mari A, Ricciardi A, Carucci AC, Sinatti G, Cosimini B, Di Norcia M, Iapadre N, Balsano C, Grimaldi A. Three cases of COVID-19 pneumonia in female patients in Italy who had pulmonary fibrosis on follow-up lung computed tomography imaging. Am J Case Rep. 2020;21:e926921. doi: 10.12659/AJCR.926921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Deng L, Khan A, Zhou W, Dai Y, Eftekhar M, Chen R, Cheng G. Follow-up study of clinical and chest CT scans in confirmed COVID-19 patients. Radiol Infect Dis. 2020;7:106–113. doi: 10.1016/j.jrid.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. China Medical Treatment Expert Group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Iaccarino G, Grassi G, Borghi C, Ferri C, Salvetti M, Volpe M, SARS-RAS Investigators Age and multimorbidity predict death among COVID-19 patients: results of the SARS-RAS study of the Italian Society of Hypertension. Hypertension. 2020;76:366–372. doi: 10.1161/HYPERTENSIONAHA.120.15324. [DOI] [PubMed] [Google Scholar]
- 8.Iaccarino G, Grassi G, Borghi C, Carugo S, Fallo F, Ferri C, Giannattasio C, Grassi D, Letizia C, Mancusi C, Minuz P, Perlini S, Pucci G, Rizzoni D, Salvetti M, Sarzani R, Sechi L, Veglio F, Volpe M, Muiesan ML, SARS-RAS Investigators Gender differences in predictors of intensive care units admission among COVID-19 patients: the results of the SARS-RAS study of the Italian Society of Hypertension. PLoS One. 2020;15(10):e0237297. doi: 10.1371/journal.pone.0237297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mancusi C, Grassi G, Borghi C, Carugo S, Fallo F, Ferri C, Giannattasio C, Grassi D, Letizia C, Minuz P, Muiesan ML, Perlini S, Pucci G, Rizzoni D, Salvetti M, Sarzani R, Sechi L, Veglio F, Volpe M, Iaccarino G, SARS-RAS Investigators. Determinants of healing among patients with COVID-2019: the results of the SARS-RAS study of the Italian Society of Hypertension. J Hypertens. 2020 (Online ahead of print).
- 10.Badawi A, Ryoo SG. Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): a systematic review and meta-analysis. Int J Infect Dis. 2016;49:129–133. doi: 10.1016/j.ijid.2016.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Inciardi RM, Adamo M, Lupi L, Cani DS, Di Pasquale M, Tomasoni D, Italia L, Zaccone G, Tedino C, Fabbricatore D, Curnis A, Faggiano P, Gorga E, Lombardi CM, Milesi G, Vizzardi E, Volpini M, Nodari S, Specchia C, Maroldi R, Bezzi M, Metra M. Characteristics and outcomes of patients hospitalized for COVID-19 and cardiac disease in Northern Italy. Eur Heart J. 2020;41:1821–1829. doi: 10.1093/eurheartj/ehaa388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Borghesi A, Maroldi R. COVID-19 outbreak in Italy: experimental chest X-ray scoring system for quantifying and monitoring disease progression. Radiol Med. 2020:1–5. [DOI] [PMC free article] [PubMed]
- 13.Borghesi A, Zigliani A, Golemi S, Carapella N, Maculotti P, Farina D, Maroldi R. Chest X-ray severity index as a predictor of in-hospital mortality in coronavirus disease 2019: A study of 302 patients from Italy. Int J Infect Dis. 2020;96:291–293. doi: 10.1016/j.ijid.2020.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maroldi R, Rondi P, Agazzi GM, Ravanelli M, Borghesi A, Farina D. Which role for chest x-ray score in predicting the outcome in COVID-19 pneumonia? Eur Radiol. 2020:1–7. (Online ahead of print). [DOI] [PMC free article] [PubMed]
- 15.Knight SR, Ho A, Pius R, Buchan I, Carson G, Drake TM, Dunning J, Fairfield CJ, Gamble C, Green CA, Gupta R, Halpin S, Hardwick HE, Holden KA, Horby PW, Jackson C, Mclean KA, Merson L, Nguyen-Van-Tam JS, Norman L, Noursadeghi M, Olliaro PL, Pritchard MG, Russell CD, Shaw CA, Sheikh A, Solomon T, Sudlow C, Swann OV, Turtle LC, Openshaw PJ, Baillie JK, Semple MG, Docherty AB, Harrison EM, ISARIC4C investigators Risk stratification of patients admitted to hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: development and validation of the 4C Mortality Score. BMJ. 2020;370:3339. doi: 10.1136/bmj.m3339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mandal S, Barnett J, Brill SE, Brown JS, Denneny EK, Hare SS, Heightman M, Hillman TE, Jacob J, Jarvis HC, Lipman MCI, Naidu SB, Nair A, Porter JC, Tomlinson GS, Hurst JR, ARC Study Group. ‘Long-COVID’: a cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19. Thorax. 2020:thoraxjnl-2020-215818. [DOI] [PMC free article] [PubMed]
- 17.Chieffo DPR, Delle Donne V, Massaroni V, Mastrilli L, Belella D, Monti L, Silveri MC, Cauda R. Psychopathological profile in COVID-19 patients including healthcare workers: the implications. Eur Rev Med Pharmacol Sci. 2020;24(22):11964–11970. doi: 10.26355/eurrev_202011_23858. [DOI] [PubMed] [Google Scholar]
- 18.Tomasoni D, Bai F, Castoldi R, Barbanotti D, Falcinella C, Mulè G, Mondatore D, Tavelli A, Vegni E, Marchetti G, d’Arminio Monforte A. Anxiety and depression symptoms after virological clearance of COVID-19: A cross-sectional study in Milan, Italy. J Med Virol. 2020. 10.1002/jmv.26459(Online ahead of print). [DOI] [PMC free article] [PubMed]
- 19.Sanders JM, Monogue ML, Jodlowski TZ, Cutrell JB. Pharmacologic treatments for coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;323:1824–1836. doi: 10.1001/jama.2019.20153. [DOI] [PubMed] [Google Scholar]
- 20.De Rossi N, Scarpazza C, Filippini C, Cordioli C, Rasia S, Mancinelli CR, Rizzoni D, Romanelli G, Cossi S, Vettoretto N, Bove S, Manfredini S, Beindorf EA, Mosca C, Scipione V, Flamminio G, Albini EA, Giansiracusa P, Capra R, Montichiari COVID-19 Study Group Early use of low dose tocilizumab in patients with COVID-19: A retrospective cohort study with a complete follow-up. EClinicalMedicine. 2020;11:08. doi: 10.1016/j.eclinm.2020.100459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Toniati P, Piva S, Cattalini M, Garrafa E, Regola F, Castelli F, Franceschini F, Airò P, Bazzani C, Beindorf EA, Berlendis M, Bezzi M, Bossini N, Castellano M, Cattaneo S, Cavazzana I, Contessi GB, Crippa M, Delbarba A, De Peri E, Faletti A, Filippini M, Filippini M, Frassi M, Gaggiotti M, Gorla R, Lanspa M, Lorenzotti S, Marino R, Maroldi R, Metra M, Matteelli A, Modina D, Moioli G, Montani G, Muiesan ML, Odolini S, Peli E, Pesenti S, Pezzoli MC, Pirola I, Pozzi A, Proto A, Rasulo FA, Renisi G, Ricci C, Rizzoni D, Romanelli G, Rossi M, Salvetti M, Scolari F, Signorini L, Taglietti M, Tomasoni G, Tomasoni LR, Turla F, Valsecchi A, Zani D, Zuccalà F, Zunica F, Focà E, Andreoli L, Latronico N. Tocilizumab for the treatment of severe COVID-19 pneumonia with hyperinflammatory syndrome and acute respiratory failure: a single center study of 100 patients in Brescia, Italy. Autoimmun Rev. 2020;19:102568. doi: 10.1016/j.autrev.2020.102568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 23.Low ET, Medford ARL, Millar AB, Tulloh RMR. Lung function in pulmonary hypertension. Respir Med. 2015;109:1244–1249. doi: 10.1016/j.rmed.2015.05.022. [DOI] [PubMed] [Google Scholar]
- 24.Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, Coates A, van der Grinten CPM, Gustafsson P, Hankinson J, Jensen R, Johnson DC, MacIntyre N, McKay R, Miller MR, Navajas D, Pedersen OF, Wanger J. Interpretative strategies for lung function tests. Eur Respir J. 2005;26:948–968. doi: 10.1183/09031936.05.00035205. [DOI] [PubMed] [Google Scholar]
- 25.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhao YM, Shang YM, Song WB, et al. Follow-up study of the pulmonary function and related physiological characteristics of COVID-19 survivors three months after recovery. EClinicalMedicine. 2020;25:100463. doi: 10.1016/j.eclinm.2020.100463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wong KT, Antonio GE, Hui DSC, Ho C, Chan P, Ng W, Shing K, Wu A, Lee N, Yap F, Joynt GM, Sung JJY, Ahuja AT. Severe acute respiratory syndrome: thin-section computed tomography features, temporal changes, and clinicoradiologic correlation during the convalescent period. J Comput Assist Tomogr. 2004;28:790–795. doi: 10.1097/00004728-200411000-00010. [DOI] [PubMed] [Google Scholar]
- 28.Ojo AS, Balogun SA, Williams OT, Ojo OS. Pulmonary fibrosis in COVID-19 survivors: predictive factors and risk reduction strategies. Pulm Med. 2020;2020:6175964. doi: 10.1155/2020/6175964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu C, Ye L, Xia R, et al. Chest computed tomography and clinical follow-up of discharged patients with COVID-19 in Wenzhou City, Zhejiang, China. Ann Am Thorac Soc. 2020;17:1231–1237. doi: 10.1513/AnnalsATS.202004-324OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Clift AK, Coupland CAC, Keogh RH, Diaz-Ordaz K, Williamson E, Harrison EM, Hayward A, Hemingway H, Horby P, Mehta N, Benger J, Khunti K, Spiegelhalter D, Sheikh A, Valabhji J, Lyons RA, Robson J, Semple MG, Kee F, Johnson P, Jebb S, Williams T, Hippisley-Cox J. Living risk prediction algorithm (QCOVID) for risk of hospital admission and mortality from coronavirus 19 in adults: national derivation and validation cohort study. BMJ. 2020;20(371):m3731. doi: 10.1136/bmj.m3731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sperrin M, McMillan B. Prediction models for covid-19 outcomes. BMJ. 2020;20(371):m3777. doi: 10.1136/bmj.m3777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wynants L, Van Calster B, Collins GS, Riley RD, Heinze G, Schuit E, Bonten MMJ, Damen JAA, Debray TPA, De Vos M, Dhiman P, Haller MC, Harhay MO, Henckaerts L, Kreuzberger N, Lohman A, Luijken K, Ma J, Andaur CL, Reitsma JB, Sergeant JC, Shi C, Skoetz N, Smits LJM, Snell KIE, Sperrin M, Spijker R, Steyerberg EW, Takada T, van Kuijk SMJ, van Royen FS, Wallisch C, Hooft L, Moons KGM, van Smeden M. Prediction models for diagnosis and prognosis of covid-19 infection: systematic review and critical appraisal. BMJ. 2020;369:m1328. doi: 10.1136/bmj.m1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Herridge MS, Tansey CM, Matté A, Tomlinson G, Diaz-Granados N, Cooper A, Guest CB, Mazer CD, Mehta S, Stewart TE, Kudlow P, Cook D, Slutsky AS, Cheung AMP, Canadian Critical Care Trials Group Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364:1293–1304. doi: 10.1056/NEJMoa1011802. [DOI] [PubMed] [Google Scholar]
- 34.Zhang C, Wu Z, Li JW, Tan K, Yang W, Zhao H, Wang GQ. Discharge may not be the end of treatment: Pay attention to pulmonary fibrosis caused by severe COVID-19. J Med Virol. 2020 (Epub ahead of print). [DOI] [PubMed]
- 35.Rai DK, Sharma P, Kumar R. Post covid 19 pulmonary fibrosis—is it reversible? Indian J Tuberc. 2020. 10.1016/j.ijtb.2020.11.003(Epub ahead of print). [DOI] [PMC free article] [PubMed]