Abstract
Objective:
The goal of this study was to describe the quality of naturalistic communication between patients with advanced cancer and their spouse caregivers using observational methods. We also assessed the association between patient and caregiver communication behaviors and psychological and physical health using the actor-partner interdependence model.
Methods:
Data on 81 dyads were gathered as part of a prospective observational study. Patients with advanced cancer and their spouse caregivers completed demographic, physical health, and emotional well-being questionnaires. Cancer and relationship communication captured in “day-in-the-life” audio recordings were coded using Gottman’s Turning System to assess the quality of bids for attention and responses.
Results:
Bids for attention were most often informational (Low Bids) and responses were mostly positive and effortful (Turn Towards); patients and caregivers did not significantly differ in communication behavior. More effortful bids for attention (High Bids) were associated with more positive and effortful responses. Patient communication behaviors were significantly associated with caregiver emotional well-being, whereas caregiver communication behaviors were significantly associated with their own emotional well-being and patient physical health.
Conclusions:
While patients may benefit from caregivers’ more positive and engaged communication at home, the emotional labor of focusing on and engaging the patient may take a toll on caregivers’ own well-being. This work contributes to the understanding of what everyday communication looks like for patients with advanced cancer and their spouse caregivers and how this communication may impact physical and psychological health. Our findings provide a foundation to develop guidelines for psychosocial couple-based interventions.
Keywords: behavior observation, cancer, caregivers, communication, couples, naturalistic study, oncology, quality of life
1 |. BACKGROUND
Cancer is well recognized as a disease that not only impacts patients but also the family members who care for them. This is especially true for advanced cancer patients and their spouse caregivers.1 Spouses often serve as each other’s most important source of support and frequently have interdependent outcomes, such that when one spouse is distressed, the other spouse is more likely to be distressed due to their emotional bond and shared experience.2 Further, advanced cancer can increase the symptom and emotional burden, as well as the amount and complexity of caregiving tasks.3 Thus, advanced cancer patients and their spouse caregivers are at risk of worse psychological and physical health outcomes based on the stress associated with cancer and caregiving.4,5
There is strong evidence that communication is important to facilitate improved individual psychological well-being and physical health outcomes for cancer patients and their spouse caregivers, as well as dyadic relationship-focused outcomes.6 Communication is also a key component in theoretical models exploring dyadic interactions in psycho-oncology.7 For instance, the relationship intimacy model of couple adaptation to cancer suggests that communication behaviors, such as self-disclosure or hostility, can impact individual and dyadic outcomes, mediated by increased or decreased levels of relationship intimacy.8 Similarly, communication behaviors, such as engagement or avoidance, are an important part of models of dyadic coping, which also has been shown to impact caregiver, patient, and dyadic outcomes.9,10 Given this theoretical basis, it is unsurprising that many interventions targeting patient and caregiver dyads include a communication component.11
However, evidence regarding the effectiveness of these communication-based interventions is mixed.12,13 Several factors have thus far limited the identification of an effective dose or timing of key communication behaviors.11 First, interventions focused on improving outcomes for couples coping with cancer have built on couples’ interpersonal communication research, the vast preponderance of which has focused on treating couples’ relationship dysfunction rather than maintaining or promoting relationship function.14 Although some couples coping with cancer have dysfunctional relationships, the majority of older adult couples—the largest demographic of cancer patients and spouse caregivers—are relatively well functioning.15 As such, there is a mismatch between the goal of existing work and the need to support relatively well-functioning couples’ communication in the face of challenges like advanced cancer.
Second, there is little research on affected couples’ interactions in the contexts that make up the majority of their time together, such as everyday interactions in the home. These everyday interactions can serve to maintain, strengthen, or undermine the relationships between partners.16 Until recently,17 methodological and technological challenges made observations of these everyday interactions difficult.18 Instead, the majority of communication research, particularly in the cancer context, has focused on self-reported communication or on analog discussions (eg, conflict discussions in a lab or therapy sessions;19,20 some exceptions are noted21,22). Although informative and with clear logistical advantages, self-report and analog methods may be vulnerable to selection, recall, or presentation bias.
Couples’ communication researchers have advocated for more holistic research in real-world contexts to understand better how well-functioning couples communicate in the face of unique challenges and how best to support these couples.14 Researchers focused on cancer-impacted dyads are in need of observational data to determine how couples interact with each other and what kinds of communication are linked to better outcomes to develop more robust communication interventions.11
The goal of this study was to describe the quality of communication between advanced cancer patients and their spouse caregivers that occurs in the home. Thus, we collected observational data from these dyads in the home, representing a typical “day in the life.” We also assessed the association between communication and psychological and physical health using the actor-partner interdependence model.23
2 |. METHODS
Data were gathered as part of a prospective observational study of couples coping with advanced cancer. A detailed description of study methods can be found elsewhere.18 All procedures were conducted with the approval of the Institutional Review Board.
2.1 |. Recruitment
Research staff screened patient appointment lists in thoracic and gastrointestinal (GI) clinics for eligible patient-participants. Aside from prostate and breast cancer, for which may gender may be a confounding factor, lung and colorectal cancer are the most common types of cancer diagnosed in the United States and are responsible for the most deaths.24 As such, the thoracic and GI clinics at our institution have relatively high censuses of patients with advanced disease. Inclusion criteria for patients included a diagnosis of stages III or IV non-small cell lung, pancreatic, esophageal, gastric, gallbladder, colorectal, hepatocellular, or bile duct cancer; a Karnofsky Performance Status score of 70+; a prognosis of more than 6 months; and undergoing active treatment. Patients had to have a cohabiting spouse (or long-term romantic partner) who identified as providing some care and also agreed to participate. Spouses were not required to be heterosexual. Both patient and caregiver were required to be over 18 years of age and English-speaking/writing.
On the day of their scheduled appointment, patients and caregivers were approached in clinic and study procedures were described. Staff verified eligibility and invited participation. Research sessions were scheduled for eligible and interested couples, either to take place in their homes or the clinic (with participants taking research materials home for later use).
2.2 |. Procedure
At the research session, both the patient and caregiver provided written informed consent and were asked to independently complete questionnaires assessing demographic information as well as physical and psychological health. Most questionnaires were completed in the home immediately prior to recording, but some participants were sent home with study materials for remote participation, and thus some baseline questionnaires may have been completed up to several days before or after.18
Each participant rated their overall health on a one-item measure ranging from excellent (5) to poor (1). Anxiety and depression were captured using the 14-item Hospital Anxiety and Depression Scale (HADS).25 The HADS contains a seven-item anxiety subscale and a seven-item depression subscale. Each item is scored from 0 to 3, and a summed score is calculated for each subscale with higher scores indicating more anxiety/depression. The four-item Perceived Stress Scale (PSS)26 was used to capture baseline stress levels. Each item is scored on a scale from 0 to 3, and a summed score is calculated with higher scores indicating more perceived stress.
Each participant was provided a digital audio recorder and lavaliere microphone, and couples were asked to simultaneously record on a pre-selected day when the patient and caregiver expected to be home together. Both patient and caregiver were asked to carry a small recorder with them to record the full breadth of communication within the day and to provide a backup for the couple if one recorder failed. The recorders often were carried in a pocket, but belt bags were also provided to participants. Recordings typically began in the morning and ended in the evening before bed. Staff was available to answer participant questions throughout the day. Equipment was returned either in clinic at the next appointment or by mail.
2.3 |. Coding and processing
Recent work suggests that the topic of discussion may influence how couples communicate.27 As such, we selected cancer and the relationship talk for targeted analysis. These topics were also key topics in previous research focused on the impact of communication on patient and caregiver outcomes.8,28
Trained coders used Noldus Observer to identify conversation related to the relationship (eg, any talk about what one’s spouse/family meant to him/her, how the couple was getting along, or emotions toward the spouse—both affection or complaints) and/or cancer (eg, any information exchange or positive or negative emotional expression regarding medication, symptoms, insurance, appointments, etc.). Data on the frequency of these topical domains are presented elsewhere.29
The unit of analysis was, speaker turn, defined as when an individual has the floor within a conversational exchange. Within each speaker turn, coders used an adapted version of the Turning System, developed by Driver & Gottman to capture ways couples interact in everyday life and to identify bids for attention and responses.30 In this system, any attempt to interact was coded as a bid for attention. Low Bids for attention included comments or questions related to information exchange. High Bids included comments or questions related to thoughts, feelings, or attempts at humor. Responses to an initial bid were coded as either Turn Toward, Turn Away, or Turn Against. Turn Toward included attentive, enthusiastic, or playful responses. Turn Away included passive or inactive responses, such as ignoring the bid, responding nonverbally (ie, not captured by audio), or low-energy comments (eg, “uh-huh”). Turn Against codes were used to capture contempt or belligerence. Descriptions and examples are included in Table 1. If a conversation continued after one turn (eg, patient bids, spouse responds, patient speaks again), further turns were coded using the same code categories (ie, whoever made the initial bid retains bidding codes, and whoever responded to the initial bid retains responding codes) until the end of the segment of topic-relevant communication. Either patient or spouse could receive bidding or responder codes.
TABLE 1.
Turning system codes, examples, and descriptive data
| Code | Description | Example | Patient M (SD) | Patient Median (Range) | Caregiver M (SD) | Caregiver Median (Range) |
|---|---|---|---|---|---|---|
| Low Bid | Information exchange. | “I’m going to take my pill before lunch with Kate.” “Did you make that appointment?” |
95.49 (73.95) | 86.5 (2–372) | 92.95 (84.57) | 62 (2.5–419) |
| High Bid | Comment or question pertaining to opinions, thoughts, or feelings. Also includes humor. | “I’m sad that you look so tired.” “Do you feel up to having a date night?” “The CIA is watching us hold hands” (joke) |
13.88 (17.66) | 8 (0–83) | 10.04 (10.02) | 6 (0–53) |
| Turn Toward | Welcomes the bid. Makes an effort to continue the conversation, including asking relevant questions. Also includes humor. | “I was thinking the same thing.” “No, I totally disagree! Tell me why you think that.” “Add it to my tab!” (joke) |
78.10 (73.43) | 56.5 (1–330) | 77.94 (64.04) | 64.5 (1–275) |
| Turn Away | It is clear that the bid has been received, but minimal effort is taken to reply. These statements do not add anything meaningful to the conversations. | “Hmmm” “Yeah” Non-verbal |
11.06 (11.28) | 7 (0–59) | 14.12 (17.06) | 9 (0–97) |
| Turn Against | Contempt, belligerence, criticism, or defensiveness. | “At least I’m not lazy like you.” “Stop bugging me!” |
0.46 (1.21) | 0 (0–7) | 0.67 (1.86) | 0 (0–10) |
A random sample of 10% of recordings was scored by two coders to calculate interrater agreement. Percent agreement between coders was excellent, ranging from 84 to 99%. Frequency of codes from separate patient and caregiver recordings were averaged together to further improve reliability. In six couples, only one member of the dyad submitted a recording (three patients, three caregivers). In these cases, only the data from one individual’s recording was used. There were no significant differences between these couples and the larger sample.
3 |. ANALYSIS
Descriptive analyses were conducted on demographic variables and Turning System communication codes. Multivariate analysis was used to assess potential demographic predictors of communication, including age, sex, education, and financial situation. Paired-samples t tests were used to compare patient and caregiver communication variables.
Two Actor-Partner Interdependence Models were used to assess associations among communication and emotional and physical health variables for patients and caregivers. First, a model was tested to determine how patient and caregiver bids for attention predicted their own or their partner’s responses using the total frequency of each communication behavior in a between-couple analysis. Second, structural equation modeling was used to test how patient and caregiver Turning System communication (both bids and responses) predicted their own and their partner’s emotional well-being and physical health. Emotional well-being was modeled as a latent variable consisting of self-reported anxiety (HADS anxiety subscale), depression (HADS depression subscale), and self-reported stress (PSS). Physical health was an observed variable: the one-item self-report measure. This two-model approach was used to approximate a mediation model, which was not feasible to run given our small sample size and the large number of parameters.
4 |. RESULTS
4.1 |. Descriptive Analysis
Demographic characteristics for the 81 participating patient-caregiver dyads are presented in Table 2. Patients were mostly men and averaged 67.01 years of age. Caregivers were mostly women and averaged 64.95 years of age. Both patients and caregivers were mostly White and relatively well educated, and most reported that their financial situation was “comfortable.” Patients and caregivers reported being married an average of 35.60 years and had relatively high levels of relationship satisfaction. As reported elsewhere,29 the median length of recording was 9.78 hours (range = 1.35–16.0 hours). The mean amount of cancer and relationship talk (ie, communication coded using the Turning System) was 4.50 minutes per recording but varied widely (range = 0–41 minutes). Of this, more talk on average was devoted to cancer (M = 3.85 minutes) than the relationship (M = 0.60 minutes), but the majority of overall talk throughout the day was about daily tasks or chit-chat. Both caregivers and patients had similar amounts of talk (t = 0.35, df = 80, P = .73). Participants reported that being recorded did not significantly impact their behavior and that the recorded day was somewhat to very typical.29
TABLE 2.
Demographic characteristics of participants**
| Patient (N = 81) |
Caregiver (N = 81) |
|
|---|---|---|
| Characteristics | M (SD) | M (SD) |
| Age | 67.01 (8.97) | 64.95 (9.29) |
| Years married | 35.60 (15.10) | |
| Relationship satisfaction (range 4–24) | 20.69 (2.97) | 19.91 (3.94) |
| n (%) | n (%) | |
| Sex | ||
| Female | 23 (28.4) | 58 (71.6) |
| Male | 58 (71.6) | 23 (28.4) |
| Race | ||
| American Indian/Alaska Native | 1 (1.2) | 1 (1.2) |
| Black/African American | 4 (4.9) | 3 (3.7) |
| White/Caucasian | 75 (92.6) | 74 (91.4) |
| Other | 0 | 1 (1.2) |
| Ethnicity | ||
| Hispanic or Latinx | 3 (3.7) | 3 (3.7) |
| Highest level of schooling | ||
| 7–11 Years | 3 (3.7) | 2 (2.5) |
| High school graduate or equivalent | 12 (14.8) | 14 (17.3) |
| Some college or vocational school | 26 (31.1) | 29 (35.8) |
| College graduate | 15 (18.5) | 12 (14.8) |
| Some graduate or professional school | 6 (7.4) | 5 (6.2) |
| Graduate or professional degree | 18 (22.2) | 18 (22.2) |
| Currently employed | ||
| No | 63 (77.8) | 49 (60.5) |
| Part-time | 2 (2.5) | 11 (13.6) |
| Full-time | 14 (17.3) | 17 (21.0) |
| Missing/No response | 2 (2.4) | 4 (3.9) |
| Financial situation | ||
| Not very good | 9 (11.1) | 8 (9.8) |
| Comfortable | 46 (56.8) | 52 (64.2) |
| More than adequate | 23 (28.4) | 19 (23.5) |
| Missing/No response | 3 (3.7) | 2 (2.4) |
| HADS anxiety (range 0–21) | 5.03 (3.46) | 7.49 (4.29) |
| HADS depression (range 0–21) | 4.66 (3.07) | 4.70 (3.72) |
| Perceived stress (range 0–12) | 4.43 (2.97) | 5.66 (2.95) |
| Self-reported health (range 1–5) | 2.86 (0.96) | 2.26 (0.74) |
1 dyad missing on all demographics.
Descriptive data for Turning System communication behaviors are presented in Table 1. Both patients and caregivers had many more Low Bids than High Bids. The most common response was Turn Toward, followed by Turn Away. There were very few Turn Against responses, as might be expected from a sample of relatively well-functioning couples.
Demographic factors did not significantly predict Turning System variables (ps > .08). Patients had marginally significantly fewer High Bids than caregivers (P = .05), but patients and caregivers did not significantly differ in other Turning System variables.
4.2 |. Predictive analysis
Two Actor-Partner Interdependence Models23 were used to assess how one individual’s communication behaviors predicted their own emotional well-being and physical health (actor effects) and the emotional well-being and physical health of their spouse (partner effects). In these models, we dropped the Turn Against communication behavior due to low frequency.
In the first model, shown in Figure 1, we assessed how bids for attention were associated with responses. For both patients and caregivers, High Bids for attention were significantly positively associated with their partner’s Turn Toward response (patient bid/caregiver response B = 0.51, SE = 0.11, P < .01; caregiver bid/patient response B = 0.66, SE = 0.21, P < .01). Caregiver High Bids were also significantly positively associated with their own Turn Toward behavior (B = 0.72, SE = 0.22, P < .01) and negatively associated with their own Turn Away behavior (B = −0.42, SE = 0.19, P = .03). Both patient and caregiver Low Bids were significantly positively associated with both Turn Toward and Turn Away behavior in their partners (patient bid/caregiver Turn Toward B = 0.74, SE = 0.04, P < .01; patient bid/caregiver Turn Away B = 0.18, SE = 0.03, P < .01; caregiver bid/patient Turn Toward B = 0.76, SE = 0.03, P < .01; caregiver bid/patient Turn Away B = 0.12, SE = 0.01, P < .01). There were no significant actor effects for either patient High Bids or Low Bids or caregiver Low Bids.
FIGURE 1.
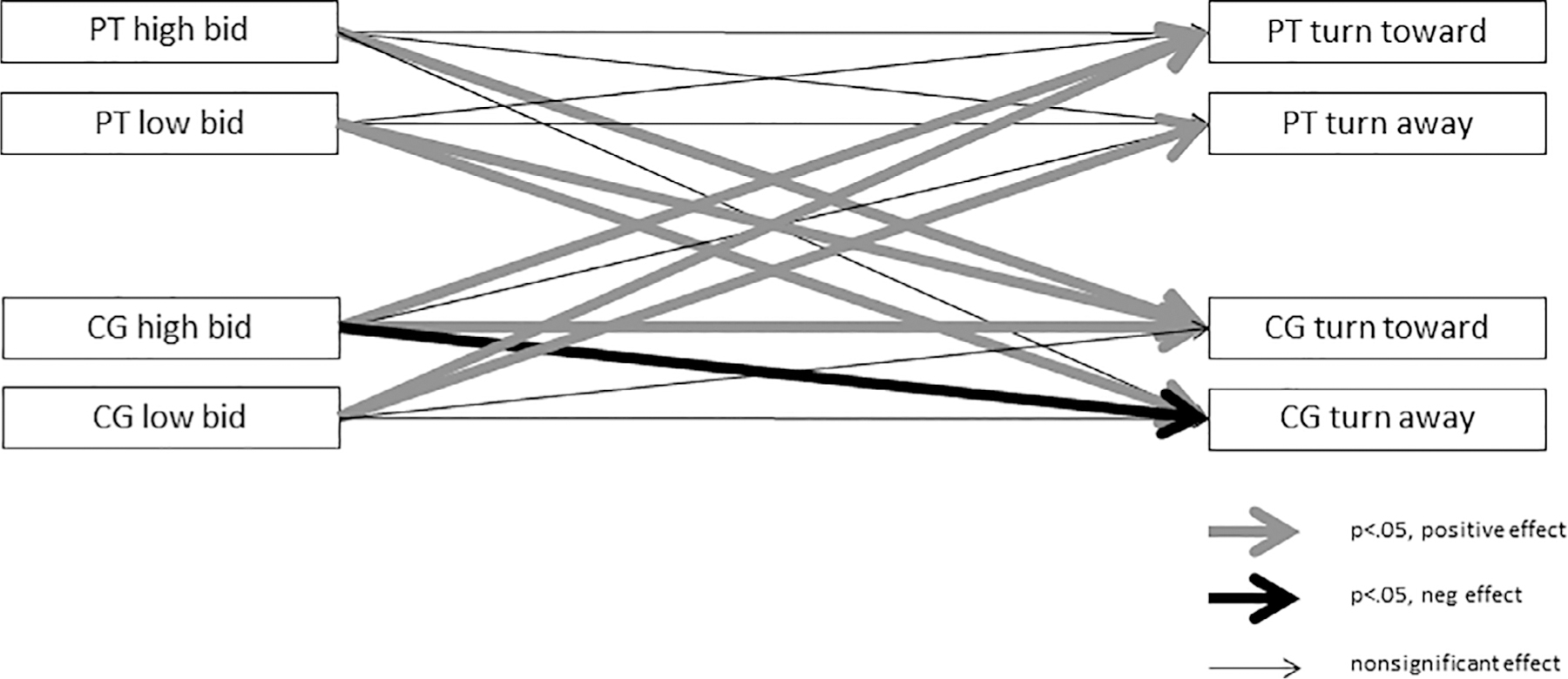
Actor-partner interdependence model of patient and caregiver bids for attention and responses. CG, caregiver; PT, patient
The second model, shown in Figure 2, assessed how communication behaviors predicted one’s own (actor effects) and one’s partner’s (partner effects) emotional well-being and physical health. There were no significant relationships between High Bids for attention and emotional well-being or physical health. Patient Low Bids were significantly positively associated with caregiver emotional well-being (B = 0.13, SE = 0.06, P = .04), whereas caregiver Low Bids were significantly negatively associated with their own emotional well-being (B = −0.12, SE = 0.05, P = .01) and patient physical health (B = −.02, SE = 0.01, P = .04). Caregiver Turn Toward behavior was significantly negatively associated with their own emotional well-being (B = −0.14, SE = 0.07, P = .04), whereas patient Turn Away behavior was significantly positively associated with caregiver well-being (B = 0.25, SE = 0.10, P = .02). There were no significant effects for caregiver Turn Away behavior or patient Turn Toward behavior.
FIGURE 2.
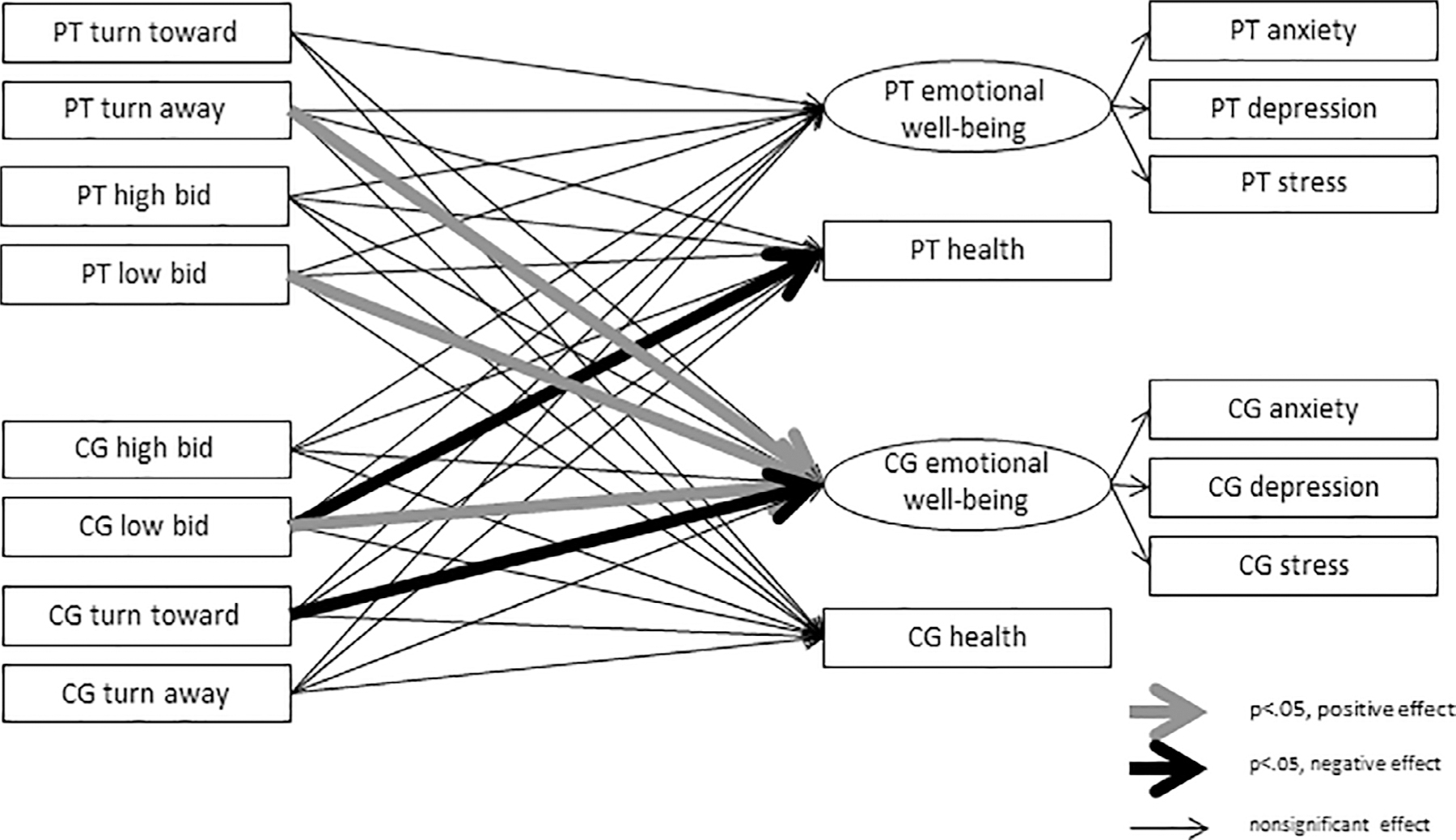
Actor-partner interdependence model of patient and caregiver communication behaviors, emotional well-being, and health. CG, caregiver; PT, patient
5 |. DISCUSSION
This study is one of the first to describe how advanced cancer patients and their spouse caregivers communicate about cancer and their relationships in everyday life. These two domains of communication have been shown to be important predictors for well-being outcomes in previous research using self-report data,8,31 yet there has been little naturalistic observational work to validate these findings. This research is needed to develop more robust communication interventions to support advanced cancer patients and their spouse caregivers.11
As might be expected, both patients and caregivers had higher numbers of Low Bids for attention than High Bids for attention. As in other research assessing naturalistic communication in families, couples spend the majority of their time exchanging information and dealing with planning day-to-day tasks, rather than discussing their thoughts and feelings.16 Additionally, it is unsurprising that the majority of responses in our relatively high-functioning sample were Turn Toward and very few Turn Against behaviors were present. Also, the significant difference in High Bids between patient and caregiver may be due to the impact of cancer; patients may have lower levels of energy to put into effortful bids for attention.
Our predictive model suggests that, as expected, High Bids for attention were associated with the more effortful and positive Turn Toward response from partners, whereas Low Bids are associated with both Turn Toward and Turn Away responses from partners. For caregivers only, their High Bids were associated with more Turn Toward, and fewer Turn Away responses of their own, suggesting a more generally positive communication style. However, our second model suggests that this caregiver effort and positivity may have a cost to their own emotional well-being. This finding is in direct contrast to previous research (in healthy samples) that suggests that Turn Toward behaviors, such as encouraging discussion and engaging in humor, would be linked to one’s own improved well-being.32,33
One possibility is that caregivers are investing this effort in helping the patient explore their thoughts and feelings, but are not engaging in these behaviors to explore their own thoughts and feelings with their partners. Avoiding conversations and limiting self-disclosure to protect ones’ partner, known as “protective buffering,” has been linked to worse individual and relationship outcomes.34,35 Caregivers are often in the unique position of sharing the patients’ stress, but feeling unable or unwilling to share the stress of caregiving with their partners.36 To protect the relationship, yet benefit from exploring thoughts and feelings, other research suggests that emotional disclosure about cancer-related stress may be less beneficial between patient and spouse caregiver;20,37 rather, disclosing to someone other than the spouse may be a better coping strategy.
Our finding that patient Low Bids were significantly positively associated with caregiver emotional well-being, whereas caregiver Low Bids were significantly negatively associated with patient physical health may have broader implications. For example, when patients share more information about their cancer, this may indicate increased dyadic coping, which has been shown in other research to be beneficial to emotional well-being.10 In contrast, when caregivers are engaged in information provision, this may indicate that due to the patients’ declining health, they have taken ownership of the stressor rather than sharing the stressor with the patients.38 This may be a natural function of the increasing roles and responsibilities of caregivers of patients with advanced stage disease.
5.1 |. Limitations
Although our study is one of the few to capture continuous naturalistic recordings, advanced cancer patients and spouse caregivers discuss cancer and their relationships relatively infrequently, and there is high variability in the total amount of talk. A larger sample of more diverse couples and/or a longer assessment period may provide a more robust view of communication and how it predicts patient and caregiver outcomes. Our study is also limited in its cross-sectional nature and our discussion should be interpreted in light of this limitation. Further, psychological well-being and physical health likely have reciprocal relationships with communication; how couples communicate may have health and well-being outcomes as proposed in our discussion, but health and well-being may also influence how couples communicate. Additional research is needed to fully explore causal models and determine how to enhance existing couples’ communication strategies and ultimately improve couples’ psychological well-being and physical health.
5.2 |. Clinical Implications
This research suggests that there may be a need to provide spouse caregivers of advanced cancer patients’ opportunities to share their concerns and engage in emotional disclosure outside of their relationships. While patients are benefiting from caregivers’ more positive and engaged communication at home, the emotional labor of focusing on and engaging the patients may affect caregivers’ own well-being. Many cancer centers offer caregiver support groups, yet there are often logistical barriers for caregivers to attend.39 New health care models that increase accessibility to these groups or that encourage caregivers to identify supportive others within their own social networks may provide the support they need to support the patients better while maintaining their own well-being.
5.3 |. Conclusion
Little previous research has captured the quality of everyday communication between advanced cancer couples through naturalistic observational methods. More observational research must be done to assess couples’ organic communication about cancer to better understand how these conversations naturally occur in context prior to developing intervention guidelines.14 Our work provides a foundation identifying what kind of communication exists in these couples and what communication behaviors are associated with better psychological well-being and physical health. This work can be used to develop future guidelines for psychosocial couple-based interventions.
ACKNOWLEDGEMENTS
Research reported in this publication was supported by the American Cancer Society (ACS MRSG 13-234-01-PCSM; PI Reblin) and the National Cancer Institute (5T32CA090314-16; MPI Brandon/Vadaparampil). The authors would like to thank the participants who make this research possible.
Funding information
American Cancer Society, Grant/Award Number: MRSG 13-234-01-PCSM; National Cancer Institute, Grant/Award Number: 5T32CA090314-16
Footnotes
CONFLICT OF INTEREST
The authors declare no conflicts of interest with respect to the research, authorship, and/or publication of this article.
ETHICS STATEMENT
The research activities reported in this manuscript were conducted in accordance with a protocol approved by Chesapeake Institutional Review Board (MCC 18495).
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1.Hagedoorn M, Sanderman R, Bolks HN, Tuinstra J, Coyne JC. Distress in couples coping with cancer: a meta-analysis and critical review of role and gender effects. Psychol Bull 2008;134(1):1–30. [DOI] [PubMed] [Google Scholar]
- 2.Jacobs JM, Shaffer KM, Nipp RD, et al. Distress is interdependent in patients and caregivers with newly diagnosed incurable cancers. Ann Behav Med 2017. [DOI] [PMC free article] [PubMed]
- 3.National Academies of Sciences E, and Medicine. Families Caring for an Aging America Washington, DC: The National Academies Press; 2016. 10.17226/23606. [DOI] [PubMed] [Google Scholar]
- 4.Williams AL, McCorkle R. Cancer family caregivers during the palliative, hospice, and bereavement phases: a review of the descriptive psychosocial literature. Palliat Support Care 2011;9(3):315–325. [DOI] [PubMed] [Google Scholar]
- 5.Northouse LL, Katapodi MC, Schafenacker AM, Weiss D. The impact of caregiving on the psychological well-being of family caregivers and cancer patients. Semin Oncol Nurs 2012;28(4):236–245. [DOI] [PubMed] [Google Scholar]
- 6.Li Q, Loke AY. A literature review on the mutual impact of the spousal caregiver-cancer patients dyads: ‘communication’, ‘reciprocal influence’, and ‘caregiver-patient congruence’. Eur J Oncol Nurs 2014;18 (1):58–65. [DOI] [PubMed] [Google Scholar]
- 7.Donovan EE, LeBlanc Farris K. Interpersonal communication and coping with cancer: a multidisciplinary theoretical review of the literature. Commun Theory 2018;29(2):236–256. [Google Scholar]
- 8.Manne S, Badr H, Zaider T, Nelson C, Kissane D. Cancer-related communication, relationship intimacy, and psychological distress among couples coping with localized prostate cancer. J Cancer Surviv 2010;4 (1):74–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Falconier MK, Kuhn R. Dyadic coping in couples: a conceptual integration and a review of the empirical literature. Front Psychol 2019; 10(571). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Traa MJ, De Vries J, Bodenmann G, Den Oudsten BL. Dyadic coping and relationship functioning in couples coping with cancer: a systematic review. Br J Health Psychol 2015;20(1):85–114. [DOI] [PubMed] [Google Scholar]
- 11.Badr H New frontiers in couple-based interventions in cancer care: refining the prescription for spousal communication. Acta Oncol 2017;56(2):139–145. [DOI] [PubMed] [Google Scholar]
- 12.Li Q, Loke AY. A systematic review of spousal couple-based intervention studies for couples coping with cancer: direction for the development of interventions. Psychooncology 2014;23(7):731–739. [DOI] [PubMed] [Google Scholar]
- 13.Walczak A, Butow PN, Bu S, Clayton JM. A systematic review of evidence for end-of-life communication interventions: who do they target, how are they structured and do they work? Patient Educ Couns 2016;99(1):3–16. [DOI] [PubMed] [Google Scholar]
- 14.Bradbury TN, Lavner JA. How can we improve preventive and educational interventions for intimate relationships? Behav Ther 2012;43 (1):113–122. [DOI] [PubMed] [Google Scholar]
- 15.Luong G, Charles ST, Fingerman KL. Better with age: social relationships across adulthood. J Soc Pers Relat 2011;28(1):9–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Campos B, Graesch AP, Repetti R, Bradbury T, Ochs E. Opportunity for interaction? A naturalistic observation study of dual-earner families after work and school. J Fam Psychol 2009;23(6):798–807. [DOI] [PubMed] [Google Scholar]
- 17.Mangelsdorf SN, Conroy R, Mehl MR, Alisic E. Clinicians’ Perspectives on Innovative Naturalistic Observations of Families in Therapy 2019.
- 18.Reblin M, Heyman RE, Ellington L, Baucom BRW, Georgiou PG, Vadaparampil ST. Everyday couples’ communication research: overcoming methodological barriers with technology. Patient Educ Couns 2018;101:551–556. [DOI] [PubMed] [Google Scholar]
- 19.Zaider TI, Kissane DW, Schofield E, Li Y, Masterson M. Cancer-related communication during sessions of family therapy at the end of life. Psychooncology 2020;29(2):373–380. [DOI] [PubMed] [Google Scholar]
- 20.Bakhshaie J, Bonnen M, Asper J, Sandulache V, Badr H. Emotional disclosure and cognitive processing in couples coping with head and neck cancer. J Behav Med 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Robbins ML, López AM, Weihs KL, Mehl MR. Cancer conversations in context: naturalistic observation of couples coping with breast cancer. J Fam Psychol 2014;28(3):380–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Demiray B, Mischler M, Martin M. Reminiscence in everyday conversations: a naturalistic observation study of older adults. J Gerontol Ser B 2017;74(5):745–755. [DOI] [PubMed] [Google Scholar]
- 23.Kenny DA, Ledermann T. Detecting, measuring, and testing dyadic patterns in the actor-partner interdependence model. J Fam Psychol 2010;24(3):359–366. [DOI] [PubMed] [Google Scholar]
- 24.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin 2019;69(1):7–34. [DOI] [PubMed] [Google Scholar]
- 25.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67(6):361–370. [DOI] [PubMed] [Google Scholar]
- 26.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav 1983;24(4):385–396. [PubMed] [Google Scholar]
- 27.Williamson HC, Hanna MA, Lavner JA, Bradbury TN, Karney BR. Discussion topic and observed behavior in couples’ problem-solving conversations: do problem severity and topic choice matter? J Fam Psychol 2013;27(2):330–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Manne SL, Siegel S, Kashy D, Heckman CJ. Cancer-specific relationship awareness, relationship communication, and intimacy among couples coping with early-stage breast cancer. J Soc Pers Relat 2014; 31(3):314–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reblin M, Sutton SK, Vadaparampil ST, Heyman RE, Ellington L. Behind closed doors: how advanced cancer couples communicate at home. J Psychosoc Oncol 2019;37(2):228–241. 10.1080/07347332.2018.1508535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Driver JLGJM. Daily marital interactions and positive affect during marital conflict among newlywed couples. Fam Process 2004;43(3): 301–314. [DOI] [PubMed] [Google Scholar]
- 31.Manne SL, Ostroff JS, Norton TR, Fox K, Goldstein L, Grana G. Cancer-related relationship communication in couples coping with early stage breast cancer. Psychooncology 2006;15(3):234–247. [DOI] [PubMed] [Google Scholar]
- 32.Horn AB, Samson AC, Debrot A, Perrez M. Positive humor in couples as interpersonal emotion regulation: a dyadic study in everyday life on the mediating role of psychological intimacy. J Soc Pers Relat 2019;36(8):2376–2396. [Google Scholar]
- 33.Robbins ML, Wright RC, María López A, Weihs K. Interpersonal positive reframing in the daily lives of couples coping with breast cancer. J Psychosoc Oncol 2019;37(2):160–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Perndorfer C, Soriano EC, Siegel SD, Laurenceau J-P. Everyday protective buffering predicts intimacy and fear of cancer recurrence in couples coping with early-stage breast cancer. Psychooncology 2019; 28(2):317–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Langer SL, Brown JD, Syrjala KL. Intra- and inter-personal consequences of protective buffering among cancer patients and caregivers. Cancer 2009;115(18 Suppl):4311–4325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tranberg M, Andersson M, Nilbert M, Rasmussen BH. Co-afflicted but invisible: a qualitative study of perceptions among informal caregivers in cancer care. J Health Psychol 0(0):1359105319890407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bultz BD, Speca M, Brasher PM, Geggie PHS, Page SA. A randomized controlled trial of a brief psychoeducational support group for partners of early stage breast cancer patients. Psychooncology 2000;9(4):303–313. [DOI] [PubMed] [Google Scholar]
- 38.Reblin M, Clayton MF, Xu J, et al. Caregiver, patient, and nurse visit communication patterns in cancer home hospice. Psychooncology 2017;26(12):2285–2293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mallya S, Daniels M, Kanter C, et al. A qualitative analysis of the benefits and barriers of support groups for patients with brain tumours and their caregivers. Support Care Cancer 2019. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


