Prevalence of myalgia, arthralgia and fatigue is high in coronavirus disease 2019 (COVID-19) patients [1], [2] and current literature outlines the possibility of viral [3] or reactive [4], [5], [6] arthritis in individuals exposed to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). However, in our experience, the spectrum of post-COVID-19 manifestations potentially referable to the heterogeneous family of spondyloarthritides may be even broader and also include predominant entheseal involvement. We would like to share the case of a 55-year-old man presenting to our rheumatology clinic in November 2020 with a 2-weeks history of left knee pain and range of motion limitation along with right elbow and bilateral heel tenderness. The patient denied previous inflammatory back pain, enthesitis, peripheral arthritis, dactylitis, psoriasis or uveitis.
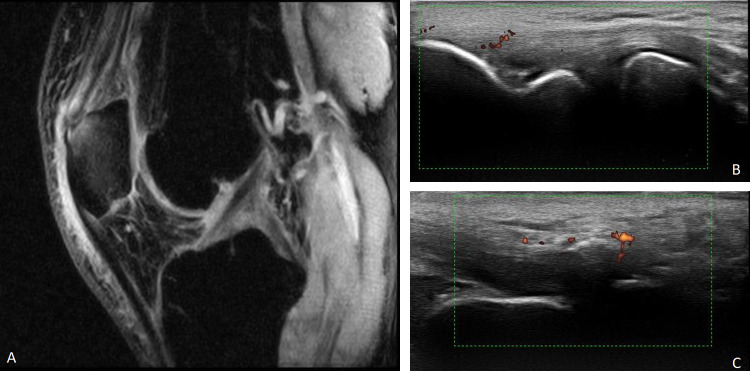
Clinical examination revealed bilateral mild tenderness on palpation of the Achilles tendon calcaneal insertion, in the left greater trochanter area and over the lateral and medial epicondyles of right elbow. Assessment of the knee elicited pain by resisted flexion and revealed tenderness in the left prepatellar and suprapatellar region. The Spondyloarthritis Research Consortium of Canada (SPARCC) index [7] was 9 over a total of 16. Complete blood count, liver and kidney function, uric acid levels and acute phase reactants were within normal limits. Anti-cyclic citrullinated peptide antibodies, rheumatoid factor and antinuclear antibodies were negative. Human leukocyte antigen (HLA) B*27 was present. Recent symptoms suggestive of a preceding infection were denied but the patient recalled mild complaints of headache, myalgia, dry cough and low-grade fever in September 2020. At that time, self-treatment with over-the-counter drugs led to rapid resolution of symptoms and no test to ascertain SARS-CoV-2 exposure was obtained. Therefore, a SARS-CoV-2 IgG/IgM rapid test was included in the laboratory workup, turning out a positive result for IgG with negative IgM. As recommended by the protocol of our Institution, a reverse transcription polymerase chain reaction from nasopharyngeal swab was then performed, testing negative. A quantitative anti-SARS-CoV-2 S1 and S2 subunits IgG test was obtained, showing an antibody level of 68.7 AU/ml (negative <12 AU/ml). The findings were consistent with past SARS-CoV-2 infection. Magnetic resonance imaging (MRI) of the left knee showed quadriceps tendon and patellar tendon enthesitis, bone marrow perientheseal edema and prepatellar bursitis (Fig. 1A). Ultrasound of right elbow and Achilles tendon calcaneal insertions confirmed the presence of enthesitis in the examined sites (Fig. 1B and C) according to the Outcome Measures in Rheumatology (OMERACT) definition of enthesitis in spondyloarthritis [8]. There was no evidence of synovitis or significant joint effusion.
Fig. 1.
A. Sagittal T2 fat-saturated weighted MRI sequence showing hyperintense thickened distal quadriceps tendon, with calcific enthesopathy and adjacent patellar bone marrow edema. Soft tissue peri-entheseal edema and prepatellar bursitis were also noted. B. Longitudinal ultrasound of the right lateral epicondyle showing a moderately thickened and hypoechoic common extensor tendon with presence of calcification and hypervascularity at the insertion site with grade 1 power Doppler signal. C. Longitudinal ultrasound of the right Achilles tendon enthesis showing a moderately thickened and hypoechoic tendon with presence of enthesophyte and hypervascularity at the insertion site with grade 1 power Doppler signal.
Therapy with non-steroidal anti-inflammatory drugs was initiated and symptoms improved. At time of writing this report, the patient is in rheumatological follow-up. Besides the emerging evidence of viral and reactive arthritis in COVID-19 patients, our case highlights the possibility of a different inflammatory involvement within the spectrum of spondyloarthritides. Although we acknowledge that the lack of definitive temporal correlation is a limitation, to the best of our knowledge this is the first described patient presenting with onset of distinct polyenthesitis after exposure to SARS-CoV-2.
Funding
None.
Disclosure of interest
The authors declare that they have no competing interest.
References
- 1.Ciaffi J., Meliconi R., Ruscitti P., et al. Rheumatic manifestations of COVID-19: a systematic review and meta-analysis. BMC Rheumatol. 2020;4:65. doi: 10.1186/s41927-020-00165-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Costantino F., Bahier L., Tarancón L.C., et al. COVID-19 in French patients with chronic inflammatory rheumatic diseases: clinical features, risk factors and treatment adherence. Joint Bone Spine. 2020;88:105095. doi: 10.1016/j.jbspin.2020.105095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parisi S., Borrelli R., Bianchi S., et al. Viral arthritis and COVID-19. Lancet Rheumatol. 2020;2:e655–e657. doi: 10.1016/S2665-9913(20)30348-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Stefano L., Rossi S., Montecucco C., et al. Transient monoarthritis and psoriatic skin lesions following COVID-19. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-218520. [DOI] [PubMed] [Google Scholar]
- 5.Ono K., Kishimoto M., Shimasaki T., et al. Reactive arthritis after COVID-19 infection. RMD Open. 2020;6:e001350. doi: 10.1136/rmdopen-2020-001350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wendling D., Verhoeven F., Chouk M., et al. Can SARS-CoV-2 trigger reactive arthritis? Joint Bone Spine. 2020;88:105086. doi: 10.1016/j.jbspin.2020.105086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mease P. Enthesitis in psoriatic arthritis (Part 3): clinical assessment and management. Rheumatology (Oxford) 2020;59:i21–i28. doi: 10.1093/rheumatology/keaa042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Balint P.V., Terslev L., Aegerter P., et al. Reliability of a consensus-based ultrasound definition and scoring for enthesitis in spondyloarthritis and psoriatic arthritis: an OMERACT US initiative. Ann Rheum Dis. 2018;77:1730–1735. doi: 10.1136/annrheumdis-2018-213609. [DOI] [PubMed] [Google Scholar]