Abstract
Type 1 diabetes (T1DM) is a chronic disease characterized by hyperglycemia due to a deficiency in endogenous insulin production, resulting from pancreatic beta cell death. Persistent hyperglycemia leads to enhanced oxidative stress and liver injury. Several studies have evaluated the anti-diabetic and protective effects of probiotic strains in animal models. In the present study, we investigated, through histopathological and biochemical analyses, the effects of eight weeks of administration of Saccharomyces boulardii (S. boulardii) yeast on the liver of streptozotocin (STZ) induced diabetic C57BL/6 mice. Our results demonstrated that S. boulardii attenuates hepatocytes hydropic degeneration and hepatic vessels congestion in STZ-induced diabetic mice. The treatment attenuated the oxidative stress in diabetic mice leading to a reduction of carbonylated protein concentration and increased activity of antioxidant enzymes superoxide dismutase and glutathione peroxidase, compared to untreated diabetic animals. The results also show the beneficial influence of S. boulardii in regulating the hepatic concentration of renin angiotensin system (RAS) peptides. Therefore, our results demonstrated that S. boulardii administration to STZ-induced diabetic mice reduces oxidative stress and normalizes the concentration of RAS peptides, supporting the hypothesis that this yeast may have a role as a potential adjunctive therapy to attenuate diabetes-induced liver injury.
Subject terms: Diabetes complications, Type 1 diabetes
Introduction
Type 1 diabetes (T1DM) is a chronic autoimmune disease characterized by hyperglycemia caused by a deficiency in endogenous insulin production as a consequence of pancreatic beta cell death1–3. Persistent hyperglycemia increases the formation of reactive oxygen species (ROS), which can occur during glucose oxidation, nonenzymatic glycation of proteins, and oxidative degradation of glycated proteins4,5.
The antioxidant enzyme superoxide dismutase (SOD) is responsible for degrading these oxygen-free radicals to hydrogen peroxide, which then can be converted to water by glutathione peroxidase (GPx) or to water and oxygen by catalase (CAT)6. In diabetic individuals, the formation of ROS combined with a decrease in the antioxidant defense leads to an increase in oxidative stress, which in turn can cause oxidation of proteins and lipids, excessive activation of pro-inflammatory pathways and DNA damage. In the liver, these cell injuries are associated with hepatocyte necrosis and apoptosis7–9.
Renin angiotensin system (RAS) is a key regulator of vascular resistance, sodium and water homeostasis, and has been strongly implicated in the pathophysiology of diabetic complications, including pancreatic beta cell dysfunction, renal and cardiovascular disease10. Whereas the circulating RAS is usually normal or suppressed in T1DM, hyperglycemia activates local RAS, increasing renin activity and the synthesis of the main RAS peptide, angiotensin II (Ang II) in renal11, cardiac12 and pancreatic cells13, which in turn stimulates ROS generation. In the liver, Ang II can be secreted by activated hepatic stellate cells after liver damage, and plays a critical role during liver disease pathogenesis, amplifying oxidative stress14,15. Also, the local RAS might affect tissue angiogenesis, proliferation, cell growth, apoptosis, tissue inflammation and fibrosis, stimulating insulin resistance, de novo lipogenesis and mitochondrial dysfunction, especially during injury15.
On the other hand, it is well known that the maintenance of intestinal microbiota influences metabolic health and inflammatory processes16, and during metabolic imbalance, probiotics also regulate oxidative stress17. Saccharomyces boulardii (S. boulardii) is a non-pathogenic yeast that was first isolated from the lychee fruit in Indochina and used to treat diarrhea in the early 1950s18. Recent studies have shown a beneficial effect of this probiotic in the context of metabolic disorders, and inflammatory conditions originated from intestinal infections or liver damage19–21.
Our research group has already demonstrated that administration of S. boulardii in streptozotocin (STZ) induced diabetic mice improves the cardiac inflammatory profile and attenuates autonomic cardiovascular dysfunction, modulating several pathophysiological mechanisms22. Additionally, our group demonstrated the beneficial effects of S. boulardii on gut microbiota composition and its capacity to improve hepatic inflammatory and metabolic profile in the experimental model of T1DM23. In the present study, we investigated the effect of S. boulardii administration on the liver injury of STZ-induced diabetic mice as well as its role in the modulation of hepatic RAS peptides and oxidative stress markers.
Methods
Animals
C57BL/6 male mice (15–20 g, 5 weeks old) were purchased from CEDEME (Federal University of São Paulo—UNIFESP, Brazil). Mice were maintained in the animal facility of the Department of Science and Technology (ICT/UNIFESP—São José dos Campos, Brazil). Animals had free access to commercial diet and water and were kept at a room temperature of 22 ± 2 °C under a 12-h light–dark cycle. Mice were randomly allocated into four groups: Control (C), Control + Probiotic (CP), Diabetes (D), and Diabetes + Probiotic (DP) (n = 6–9/group). All animal studies were approved by the Institutional Ethics Committee on Use of Animal (CEUA-UNIFESP/Protocol #2898091216) and were conducted in accordance with guidelines established by the National Council of Control of Animal Experimentation (CONCEA)23. The present study was performed in compliance with the principles of the ARRIVE (Animal Research: Reporting of In Vivo Experiments) guidelines24.
Experimental design
Mice (six-week-old) from D and DP groups received a single intraperitoneal injection of STZ (150 mg/kg, Sigma Chemical Co., St. Louis, MO, USA) dissolved in 0.01 M citrate buffer at pH 4.522,23. C and CP groups injection consisted of an equivalent volume of citrate buffer. After the administration of STZ, the animals were given a 5% glucose solution to prevent hypoglycemia, for 24 h. Single STZ high dose exerts direct toxicity on beta cells, which results in necrosis within 48–72 h and permanent hyperglycemia25,26.
Four days after the STZ injection, blood samples were collected through the tail vein, and blood glucose level was determined (Accu-Check Advantage Blood Glucose Monitor—Roche Diagnostic Corporation, Indianapolis, IN). Mice with blood glucose ≥ 250 mg/dl after fasting for four hours were considered diabetic. During eight weeks, mice from CP and DP groups received a daily dose (0.5 × 108 colony-forming units, CFU) of S. boulardii, THT 500,101 strain (THT: Probiotics and Starters Cultures, Belgium) dissolved in 0.3 ml of sterile water, by oral gavage22,23. The control groups received the same volume of sterile water. After eight weeks of treatment, animals were euthanized by decapitation.
The liver was rapidly excised, precisely dissected, and weighed. Caudate lobe was stored at − 80 °C for further analyses, and the median lobe was fixed in 10% buffered formalin for histological analyses. Trunk blood was collected in ice-chilled heparinized tubes and blood was centrifuged at 10,000×g for 10 min at 4 °C. Serum was separated, aliquoted and stored at − 80 °C for further analyses.
Histological measurements
Hepatocytes area
For morphometric analysis of Hematoxylin & Eosin stained sections (400 × magnification), the hepatocyte perimeters of three random regions of the tissue were determined freehand by one blinded reader, and 500 to 1100 hepatocytes per group were measured. We carefully selected the tissue sections, avoiding cells around hepatic veins or in the edges of the slices, since they might present distortions. To avoid any uncertainty measurement, we included a high number of cells in the analysis and also used the three sections from each slide. Digital photomicrographs were captured using the software Pannoramic Viewer (3DHISTECH Ltd.) and the number of hepatocytes per area from four random sections of each sample was computed.
Collagen content
Six hundred images of stained sections with Picrosirius Red were captured by Olympus Bx43 microscope connected to a digital camera Q-Color 3 Olympus. The images were digitalized at 2048 × 1536 pixels, 24 bit/pixel of resolution with a global magnification of 100 × by cellSens Standard Olympus. The quantitative evaluation of the area occupied by collagen deposition over the total area of liver tissue was performed using the image analysis software CellProfiler 3.1.527, according to a pipeline adapted from Sant’anna, Sant’anna, and Parolini28.
Hepatic vascular congestion
To determine the degree of vascular congestion, hepatic vessels from Hematoxylin & Eosin stained sections (200 × magnification) were counted and classified as (1) no congestion, (2) slight congestion (less than half of the vessels full of blood cells), (3) moderate congestion (about half of the hepatic vessels presenting signs of congestion) and severe congestion (more than half of the vessels filled up with blood cells). The results were presented as a percentage of the total number of analyzed blood vessels.
Determination of serum ALT and AST levels
The alanine aminotransferase (ALT) and aspartate aminotransferase (AST) activities were determined to investigate liver damage using commercially available kits (Labtest Diagnostica S/A, Lagoa Santa, MG, Brazil) according to the manufacturer’s instructions.
Preparation of liver homogenate
On the day of extraction, a frozen liver fragment was homogenized for 30 to 45 s, in a cooled 2 ml microcentrifuge tube, with stainless steel beads in it. For this, ice-cold phosphate buffer 30 mM and potassium chloride pH 7.4, containing sucrose (240 mM), NaCl (300 mM), and the following protease inhibitors: potassium EDTA (25 mM), o-phenanthroline (0.44 mM), pepstatin A (0.12 mM), 4-chloromercuribenzoic acid (1 mM), phenylmethanesulfonyl fluoride (PMSF) 100 mM and protease inhibitor cocktail (1 tablet/10 ml extraction solution, cOmplete Mini Protease Inhibitor, Roche, USA), were added to the microcentrifuge tube in a proportion 10 ml per gram of tissue and used for homogenate preparation. Samples were centrifuged at 4000 rpm for 10 min and the supernatant was stored at 80 ºC for biochemical analyses.
Protein oxidation
Protein oxidation was determined through a reaction of protein carbonyl groups with 2,4-dinitrofenylhydrazyne to form 2,4-dinitrophenylhydrazone, which can be measured spectrophotometrically at 360 nm29. The reaction medium consisted of guanidine 6 M in hydrochloric acid 2.5 M at pH 2.5, 2,4 dinitrophenylhydrazine in hydrochloric acid 2.5 M, trichloroacetic acid (TCA) 20%, TCA 10% and ethanol-ethyl acetate 1:1 (v/v).
Chemiluminescence induced by tert-butyl hydroperoxide (tBOOH)
The chemiluminescence was measured by a beta counter (TriCrab 2800TR, PerkinElmer) in a darkroom. The reaction medium consisted of a phosphate-buffer solution 20 mmol/l (with potassium chloride 140 mmol/l, pH 7.4) and tert-butyl hydroperoxide 400 mmol/l30.
Antioxidant enzyme activity
The SOD activity was evaluated by the inhibition of the reaction between peroxide anion and pyrogallol. The determination of CAT activity was by monitoring the decrease in hydrogen peroxide (H2O2) absorbance at 240 nm31. GPx activity was determined by adding glutathione reductase, glutathione and, later on, nicotinamide adenine dinucleotide phosphate (NADPH) and monitoring the alteration of absorbance at 340 nm32.
Angiotensin quantification
The samples were prepared for solid-phase extraction with the addition of the Sar1-Leu8 Ang II internal standard and thus extracted on Sep-PakC18 3 cc columns (Waters, USA). Extraction control was done using a tenfold concentration with the peptides of interest: angiotensin I (Ang I), Ang II, angiotensin 1–7 (Ang 1–7), angiotensin 1–5 (Ang 1–5), angiotensin 1–9 (Ang 1–9), angiotensin III (Ang III) and angiotensin 3–7 (Ang 3–7) (Sigma, USA). The peptides were separated on a Luna C18 reverse-phase column (100 × 2.0 mm, 3 μm, Phenomenex, USA) using a linear gradient of mobile phase A (H2O, ammonium acetate and formic acid) and mobile phase B (methanol, ammonium acetate, and formic acid) in Agilent 1260 HPLC (Agilent, USA), and subsequently injected into the Mass Spectrometer coupled to HPLC, AB Sciex 5500 QTRAP (Sciex, USA). The peptides' detection was performed with the multiple monitoring reaction (MRM) according to their mass/load (m/z) and retention. Calculations were performed from a calibration curve (with matrix) in the range of 0.5 fmol to 200 fmol per injection. Quantification of the samples was determined by calculating the peak area displayed for the mass of the target ions in the spectrometer, referenced to the known amount of standard peptides acquired under the same conditions over the same time. The results were analyzed using Multiquant 3.0.3 software (Sciex, USA). The results were expressed as fmol/mg.
Statistical analysis
For this study, the sample size was calculated based on the total of proposed experimental groups (4), the standard deviation of blood glucose (58 mg/dl), and the difference in blood glucose measurement between the control and the STZ-induced diabetic group (241 mg/dl); α = 0.05 and 95% statistical power were considered33. Statistical analysis was performed using GraphPad Prism. The Kolmogorov–Smirnov algorithm was used to determine whether each variable had a normal distribution. Parametric results were evaluated with Two-way ANOVA followed by Tukey test for multiple comparisons of means, expressed as mean ± standard error of the mean, and nonparametric results were evaluated with Kruskal–Wallis, followed by Dunn’s multiple comparisons test, expressed as median ± IQR (interquartile range). Differences were considered statistically significant when p ≤ 0.05.
Results
Blood glucose and body weight
Before treatment, diabetic mice presented significantly lower body weight compared with C and CP groups (C = 19.30 ± 0.51 g, CP = 19.07 ± 0.56 g vs. D = 13.90 ± 0.38 g, DP = 15.80 ± 0.37 g). The difference remained until the end of the eight-week protocol, and probiotic did not affect this parameter (C = 22.16 ± 0.58 g, CP = 22.31 ± 0.50 g vs. D = 14.54 ± 0.91 g, DP = 16.90 ± 0.46 g).
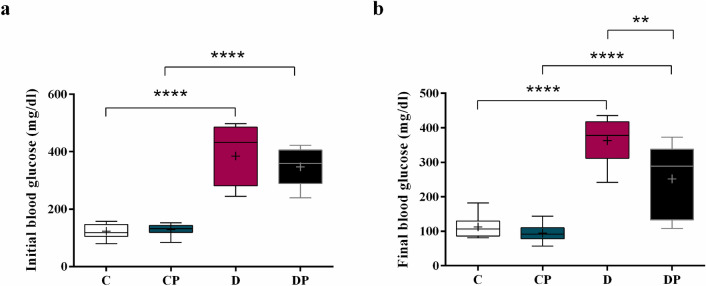
After diabetes induction, mice with blood glucose levels higher than 250 mg/dl were considered diabetic (Fig. 1a). The diabetic group that received a daily dose of S. boulardii presented a 30% reduction of blood glucose compared to the untreated group (DP = 251.9 ± 36.40 mg/dl vs. D = 362.9 ± 21.26 mg/dl), showing the beneficial effect of the probiotic on glucose homeostasis (Fig. 1b).
Figure 1.
Fasting blood glucose in mg/dl (a) at the beginning and (b) at the end of the protocol (week 8). Control (C), control + probiotic (CP), diabetic (D) and diabetic + probiotic (DP) groups (n = 6–9/group). Data are from C57BL/6 STZ-induced diabetic mice, + /− Saccharomyces boulardii (0.5 × 108 colony-forming units, THT 500,101 strain, Probiotics and Starters Cultures, Belgium) for 8 weeks. A horizontal line inside the box indicates the median value of the samples within each group, and the upper and lower edges of the box indicate the quartiles. The significance was determined by Two-way ANOVA followed by Tukey test for multiple comparisons of means (GraphPad Prism 6). + indicates mean value. **p ≤ 0.01, ****p ≤ 0.0001.
Histological analyses
Hepatocyte area and collagen content
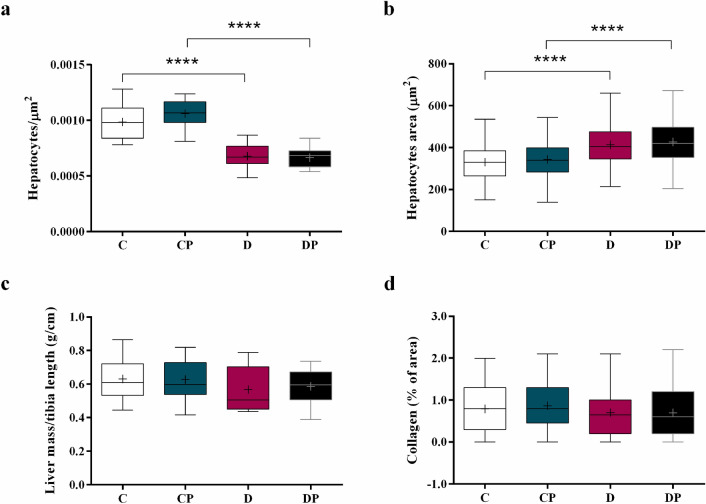
The number of hepatic cells per µm2 in D and DP groups decreased (Fig. 2a) (D = 0.0007 hepatocytes/µm2, DP = 0.0007 hepatocytes/µm2 vs. C = 0.0010 hepatocytes/µm2, CP = 0.0011 hepatocytes/µm2), and the hepatocytes area increased (Fig. 2b) (D = 404.7 ± 130.2 µm2, DP = 419.4 ± 143.4 µm2 vs. C = 329.6 ± 120.0 µm2, CP = 339.8 ± 115.5 µm2 ) compared with C and CP groups. However, the liver mass (Fig. 2c) was not affected by diabetes or probiotic. The collagen content data (analyzed from the histological images of hepatic tissue with 100 × magnitude) did not significantly change (Fig. 2d).
Figure 2.
(a) Number of hepatocytes per µm2 (b) hepatocytes area in µm2, (c) liver mass corrected by tibia length (g/cm), (d) collagen content (%) analyzed using CellProfiler 3.1.5 in control (C), control + probiotic (CP), diabetic (D) and diabetic + probiotic (DP) groups (n = 6–9/group). Data are from C57BL/6 STZ-induced diabetic mice, + /− Saccharomyces boulardii (0.5 × 108 colony-forming units, THT 500,101 strain, Probiotics and Starters Cultures, Belgium) for 8 weeks. A horizontal line inside the box indicates the median value of the samples within each group, and the upper and lower edges of the box indicate the quartiles. For (b,d) significance was determined by Kruskal–Wallis followed by Dunn’s test, and for (a,c) significance was determined by Two-way ANOVA followed by Tukey test for multiple comparisons of means (GraphPad Prism 6). + indicates mean value. **** p ≤ 0.0001.
Hepatic vascular congestion
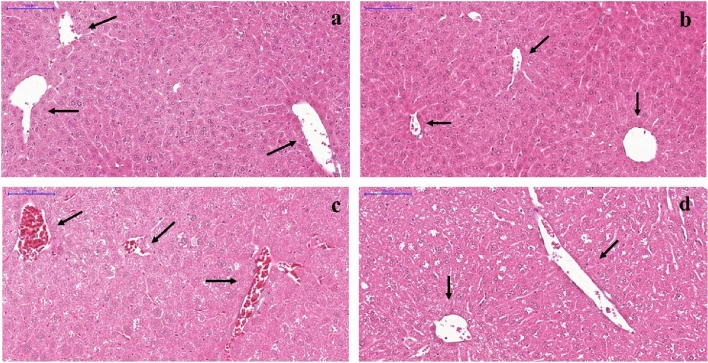
Regarding the degree of hepatic congestion, C, CP, and DP groups (Fig. 3 a, b, and d, respectively) presented mostly slight congestion. On the other hand, most of the hepatic vessels from non-treated diabetic mice exhibited severe congestion (Fig. 3c). Figure 4 presents the percentage of vessels classified as presenting no congestion, slight, moderate, or severe congestion in the histological analyses of the hepatic tissue, of each group.
Figure 3.
Representative photomicrographs of Hematoxylin & Eosin stained liver from C57BL/6 STZ-induced diabetic mice, + /− Saccharomyces boulardii (0.5 × 108 colony-forming units, THT 500,101 strain, Probiotics and Starters Cultures, Belgium) for 8 weeks. Control (a) and control + probiotic (b) show normal hepatocytes organization and hepatic vessels (→) with no sign of congestion. Hepatic vessels ( →) from the diabetic group (c) showed severe congestion while diabetic mice + probiotic (d) showed slight vessel congestion similar to control. Scale bar: 100 μm; 200 × magnification.
Figure 4.
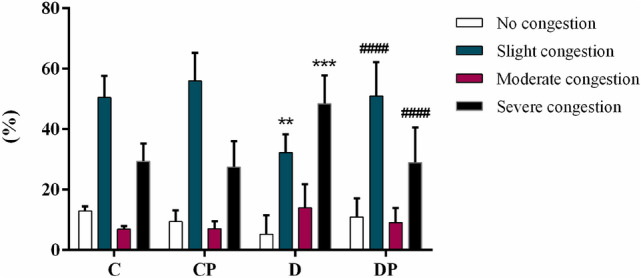
Level of congestion in hepatic vessels (%) from control (C), control + probiotic (CP), diabetic (D) and diabetic + probiotic (DP) groups (n = 6–9/group). Data are from C57BL/6 STZ-induced diabetic mice, + /− Saccharomyces boulardii (0.5 × 108 colony-forming units, THT 500101 strain, Probiotics and Starters Cultures, Belgium) for 8 weeks. Two-way ANOVA followed by Tukey test for multiple comparisons of means (GraphPad Prism 6). **p ≤ 0.01, ***p ≤ 0.001 versus C in the same degree of injury; and ####p ≤ 0.0001 versus D in the same degree of injury.
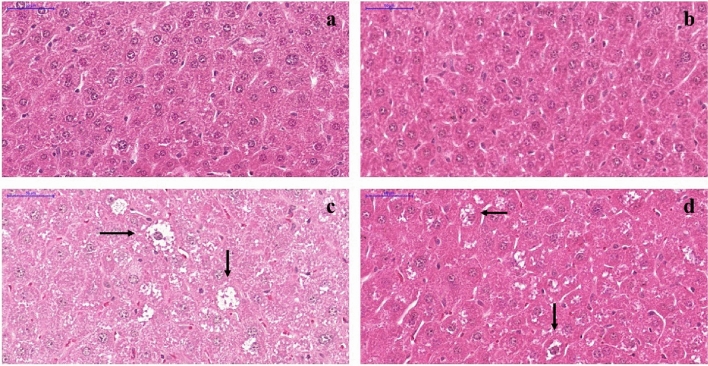
Hydropic degeneration
Signs of severe hydropic degeneration were found in hepatic tissue from D group (Fig. 5c). In mice from DP group, however, S. boulardii attenuated the injury as shown in Fig. 5d. In mice from C and CP groups the hepatocytes show normal organization (Fig. 5a,b).
Figure 5.
Histological sections of liver stained with Hematoxylin & Eosin from C57BL/6 STZ-induced diabetic mice, + /- Saccharomyces boulardii (0.5 × 108 colony-forming units, THT 500,101 strain, Probiotics and Starters Cultures, Belgium) for 8 weeks. Control (a) and Control treated with S. boulardii (b) show normal hepatocytes organization. The diabetic group (c) showed hepatocytes with signs of hydropic degeneration which consists in enlarged cells and clear cytoplasm due to the presence of small clear vacuoles with indistinct shape and limits (→), and in diabetic group treated with S. boulardii (d) it is attenuated.
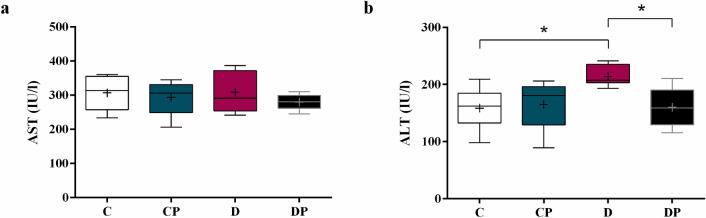
Circulating ALT and AST levels
Serum concentration of AST did not significantly change in response to diabetes of probiotic (Fig. 6a). On the other hand, ALT did increase in D group and S. boulardii reduced the concentration to the control level (Fig. 6b) (D = 213.7 ± 6.728 IU/l vs. C = 158.4 ± 11.56 IU/l, DP = 159.8 ± 13.83 IU/l).
Figure 6.
Aminotransferases (a) AST and (b) ALT in IU/l. Control (C), control + probiotic (CP), diabetic (D) and diabetic + probiotic (DP) groups (n = 6–9/group). Data are from C57BL/6 STZ-induced diabetic mice, + /− Saccharomyces boulardii (0.5 × 108 colony-forming units, THT 500,101 strain, Probiotics and Starters Cultures, Belgium) for 8 weeks. A horizontal line inside the box indicates the median value of the samples within each group, and the upper and lower edges of the box indicate the quartiles. Two-way ANOVA followed by Tukey test for multiple comparisons of means (GraphPad Prism 6). + indicates mean value. *p ≤ 0.05.
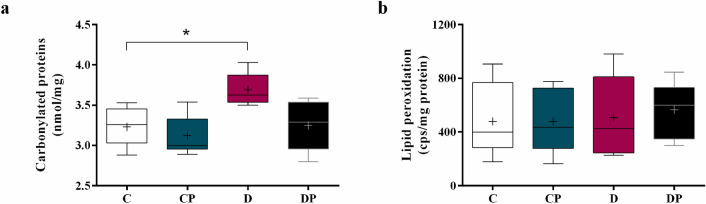
Carbonylated proteins and lipid peroxidation
The measurement of carbonylated proteins showed significantly higher levels of protein damage in D compared to C group (Fig. 7a) (D = 3.62 ± 0.33 nmol/mg vs. C = 3.26 ± 0.42 nmol/mg), and probiotic attenuated this alteration in DP group (DP = 3.29 ± 0.58 nmol/mg). No significant alterations regarding lipid peroxidation were observed among the experimental groups (Fig. 7b).
Figure 7.
Carbonylated proteins (nmol/mg) and lipid peroxidation (cps/mg protein) in hepatic tissue of control (C), control + probiotic (CP), diabetic (D) and diabetic + probiotic (DP) groups (n = 6–9/group). Data are from C57BL/6 STZ-induced diabetic mice, + /- Saccharomyces boulardii (0.5 × 108 colony-forming units, THT 500,101 strain, Probiotics and Starters Cultures, Belgium) for 8 weeks. A horizontal line inside the box indicates the median value of the samples within each group, and the upper and lower edges of the box indicate the quartiles. For (a) the significance was determined by Kruskal–Wallis followed by Dunn’s test and for (b) the significance was determined by Two-way ANOVA followed by Tukey test for multiple comparisons of means (GraphPad Prism 6). + indicates mean value. *p ≤ 0.05.
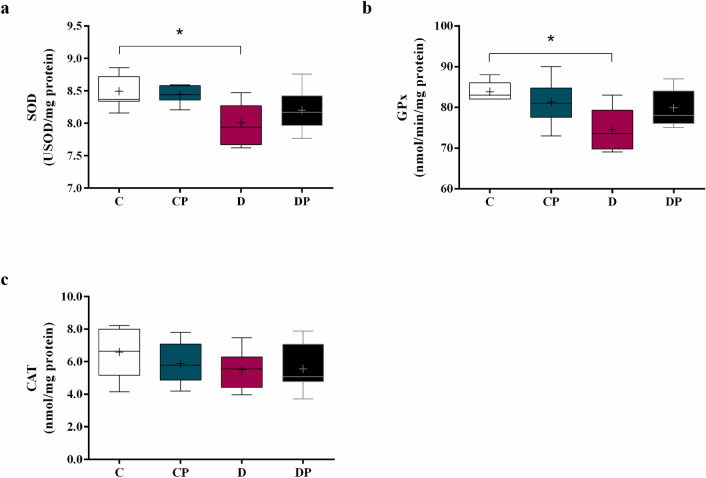
Antioxidant enzyme activity
SOD activity decreased in D group compared to C (D = 8.00 ± 0.12 USOD/mg vs. C = 8.49 ± 0.10 USOD/mg). After treatment, SOD activity showed a trend to recover (DP = 8.20 ± 0.14 USOD/mg), as shown in Fig. 8a. GPx presents the same pattern as SOD (C = 83.00 ± 4.00 nmol/min/mg, D = 73.50 ± 9.50 nmol/min/mg, DP = 78.00 ± 8.00 nmol/min/mg) (Fig. 8b). CAT activity was not influenced by diabetes or probiotic, as shown in Fig. 8c.
Figure 8.
Activity of (a) superoxide dismutase (SOD), (b) glutathione peroxidase (GPx) and (c) catalase (CAT) in hepatic tissue of control (C), control + probiotic (CP), diabetic (D) and diabetic + probiotic (DP) groups (n = 6–9/group). Data are from C57BL/6 STZ-induced diabetic mice, + /- Saccharomyces boulardii (0.5 × 108 colony-forming units, THT 500,101 strain, Probiotics and Starters Cultures, Belgium) for 8 weeks. A horizontal line inside the box indicates the median value of the samples within each group, and the upper and lower edges of the box indicate the quartiles. For (a) significance was determined by Two-way ANOVA followed by Tukey’s test. For (b, c) results were evaluated with Kruskal–Wallis, followed by Dunn’s test. + indicates mean value (GraphPad Prism 6). * p ≤ 0.05.
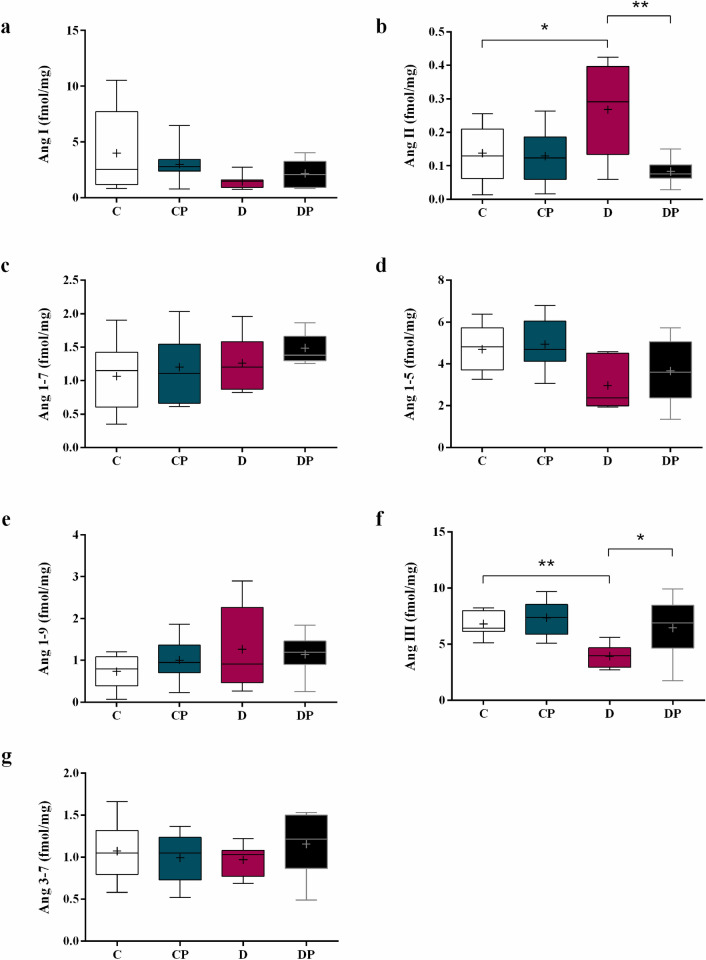
Renin angiotensin system components
Liver Ang I, Ang 1–7, Ang 1–5, Ang 1–9, and Ang 3–7 concentrations were not affected by diabetes or treatment (Fig. 9a,c–e,g). On the other hand, liver Ang II increased in D compared to C group. In DP group, Ang II concentration returned to control level (Fig. 9b) (D = 0.27 ± 0.05 fmol/mg vs. C = 0.14 ± 0.02 fmol/mg and DP = 0.08 ± 0.01 fmol/mg). Ang III concentration decreased in D group and the values return to the control level in DP group (Fig. 9f) (D = 3.93 ± 0.35 fmol/mg vs. C = 6.81. ± 0.34 fmol/mg, and DP = 6.45 ± 0.92 fmol/mg).
Figure 9.
Liver concentration of (a) Ang I, (b) Ang II, (c) Ang (1–7), (d) Ang (1–5) (e) Ang (1–9), (f) Ang III and (g) Ang (3–7) in control (C), control + probiotic (CP), diabetic (D) and diabetic + probiotic (DP) groups (n = 6–9/group). Data are from C57BL/6 STZ-induced diabetic mice, + /- Saccharomyces boulardii (0.5 × 108 colony-forming units, THT 500101 strain, Probiotics and Starters Cultures, Belgium) for 8 weeks. A horizontal line inside the box indicates the median value of the samples within each group, and the upper and lower edges of the box indicate the quartiles. The significance was determined by Two-way ANOVA followed by Tukey’s test for multiple comparisons of means (GraphPad Prism 6). + indicates mean value. *p ≤ 0.05, **p ≤ 0.01.
Discussion
Some studies have already evaluated the anti-diabetic effects of probiotic strains in animal models16,34–37, as well as the close association between the gut microbiota and the development of liver injury19,21,23,38–40. Gut microbiota modulation may induce beneficial adaptations, including the reduction of oxidative stress and inflammation, attenuation of fibrosis, and decrease of apoptosis and necrosis38. Our research group has already demonstrated the benefits of S. boulardii in cardiac function, liver metabolism, and inflammatory profile of diabetic STZ-induced mice. In the present study, we have shown the beneficial effects of S. boulardii on liver oxidative stress and local renin angiotensin system, attenuating liver damage on the model of T1DM mice.
Persistent hyperglycemia stimulates the production of reactive oxygen species and decreases the antioxidant defense, increasing liver oxidative stress and also the complications of T1DM4,41. In the present study, we demonstrated that diabetes was associated with a decrease of liver antioxidant enzymes SOD and GPx, with no effect on CAT activity, consistent with previous findings42–45. We also observed an increased concentration of carbonylated proteins in the diabetic group compared to the control, probably due to an overload on metabolic pathways of reactive carbonyl species detoxification8.
On the other hand, diabetic mice treated with S. boulardii exhibited a decreased concentration of carbonylated proteins and also a trend to increase the SOD and GPx activities. In this case, the attenuation of hepatic oxidative stress was associated with the improvement of blood glucose control, reducing the formation of free radicals in response to S. boulardii. Although the induction of experimental T1DM by STZ causes intense destruction of pancreatic beta cells, drastically reducing the levels of insulin secreted by the pancreas, a previous study has shown that 10—14% of the cells are preserved even when high doses of the substance are used (up to 200 mg/kg)25. Thus, in the present study, the reduction of blood glucose and hepatic oxidative stress may be related to the effect of S. boulardii on reminiscent beta cell, improving insulin production as previously demonstrated by our group23. Moreover, probiotics modulate the redox state by increased antioxidant defenses and modulation of gut microbiota after liver injury21,23,39,46, and in fact, it has already been shown that S. boulardii presents strong antioxidant activity and reducing power47,48.
The activation of hepatic stellate cells, which produce excessively type 1 collagen, is the main factor contributing to liver fibrosis and can be caused by the generation of free radicals and by malondialdehyde, which is a product of lipid peroxidation49. Our results show that after eight weeks of treatment there was still no significant increase in the lipid peroxidation, neither stimulation for exacerbated collagen production by hepatic stellate cells in diabetic animals. However, we also demonstrated that the liver of diabetic mice presented vessel congestion compared to control mice, suggesting the presence of fibrotic tissue impairing blood flow. Along with the attenuation of oxidative stress in the treated group, the severe congestion of vessels was reversed after S. boulardii administration.
It has been described that the liver presents a local RAS50 and that the major effector peptide of the system, Ang II, can be secreted by activated hepatic stellate cells and plays an important role in amplifying oxidative stress in the organ14,15. Investigating these local RAS components, our analysis shows that Ang II is increased in diabetic mice and S. boulardii reduced the hepatic concentration of this peptide to the control level. On the other hand, the concentration of Ang III was decreased in the diabetic mice compared to the control group, probably as a result of the loss of aminopeptidase A activity. In the present study, the hepatic concentration of Ang II was found lower than the concentration of other RAS peptides, including Ang III. Similar results have already been described in the literature, showing that Ang I and Ang III concentration were higher than Ang II in the plasma of wild type mice51. However, it is worth mentioning that the liver of rats with chronic injury are hyper-responsive to Ang II52, suggesting that Ang II exerts important effects despite its low concentration in this tissue.
Ang II actions can be mediated by the Ang II receptors (AT1R and AT2R). Ang II/AT1R is the classical RAS, while Ang II/AT2R and Ang (1–7)/MasR are the alternative RAS, and counterbalance the effects of the classical axis. Although we did not evaluate the expression of AT1 and AT2 receptors in the present study, based on our results and those described in the literature, we believe that the activation of the classical RAS (Ang II/AT1R) is at least in part responsible for the liver damage described in the diabetic group, and also that S. boulardii exerts some modulation on this pathway. It is well known that both of the Ang II receptors (AT1R and AT2R) are expressed in the liver; however, the AT1R is reported to be far more abundant and responsible for most of the Ang II-mediated effects53. Furthermore, Bosnyak showed that all endogenous angiotensin peptide fragments show a higher affinity for AT2R than Ang II, and they suggest the metabolites act mainly through AT2R while Ang II acts through AT1R54. Besides, a large number of studies have shown that the activation of the ACE/Ang II/AT1R pathway is associated with various pathological responses including diabetic injury55, and as mentioned before, Ang II interaction with AT1R enhances oxidative stress56. Gopal et al. showed that Ang II infusion in the liver caused hepatic damage triggering hepatocyte degeneration, hepatic cell apoptosis, sinusoidal dilatation and fluid accumulation57. Accordingly, our results show increased oxidative stress in diabetic mice concomitant with increased levels of Ang II and liver damage. On the other hand, S. boulardii reduced the Ang II concentration back to the control level, and also attenuated organ damage in diabetic treated groups, suggesting an important role of this peptide on the development of diabetic liver injury.
Based on the histomorphological investigation, we also demonstrated that the number of hepatocytes is decreased in the liver of diabetic mice when compared to the non-diabetic groups, although the liver mass is not reduced. Moreover, we observed that hepatic cells are enlarged in D groups and that the probiotic does not have an influence on any of these parameters. Based on these data, we concluded that as long as hyperglycemia and the consequent increased oxidative stress lead to hepatic cells apoptosis and necrosis, hypertrophy in the diabetic group is occurring as a compensatory mechanism for organ mass loss. Besides that, as the angiotensin generated peptide fragments are also associated with cell growth, cell proliferation, and apoptosis14,58, the increased level of Ang II in the liver as well as the prolonged stimulation of the system, are contributing to the abnormal cell growth59,60.
Consistent with our finds, studies showed that STZ-induced diabetic rodents presented congestion in portal vessels and sinusoids and hydropic degeneration of hepatocytes in the analysis made between two and eight weeks after the induction61, 62. The hydropic degeneration, also evidenced in the present study, is caused by the retention of electrolytes and water by cells as a result of an imbalance in their transport across membranes. This imbalance, in turn, can result from injuries to the plasma membrane caused by oxidative stress. The retention of sodium, the decrease in the amount of potassium, and the consequent increase of intracellular osmotic pressure lead to water influx, and cells acquire a vacuolar aspect63. Together with the decrease in oxidative stress markers, hydropic degeneration was attenuated after the administration of S. boulardii. Although hydropic degeneration could contribute to cell enlargement in the context of diabetes, it does not seem to be the main factor, since the administration of S. boulardii attenuates this maladaptation with no significant effect on liver mass. We hypothesize that S. boulardii attenuates hydropic degeneration induced by diabetes, but not the mechanisms responsible for cell hypertrophy. Our results are consistent with others showing that to survive oxidative stress, hepatic cells may inhibit proliferation, and the recovery of liver mass preferentially occurs by hypertrophic mechanisms, allowing immediate responses to maintain homeostasis64–66. It is important to mention that although we did not observe hepatic steatosis in this study, Albuquerque et al. demonstrated that the content of triglycerides is increased in STZ-induced diabetic mice and that the treatment with S. boulardii restored it.
At last, we can affirm that the non-diabetic mice receiving probiotic S. boulardii did not present a considerable difference when compared to control in any of the evaluated parameters, which proves that the probiotic administration does not have any effect on oxidative stress, RAS or cause damage to the liver of healthy animals. Our results show that neither AST nor ALT levels were negatively affected by S. boulardii administration. On the other hand, increased ALT activity was observed in D group, and S. boulardii reduced it, showing that the hepatocellular injury induced by diabetes was attenuated by the probiotic. Aminotransferases AST and ALT are both found in high concentrations in hepatic cells, and they leak into the circulation when the hepatocytes are damaged67,68. AST can also be found in the heart muscle, skeletal muscle, kidney, neuronal cell bodies, pancreas and blood cells, while ALT is primarily in the liver69,70. Therefore, an increase in ALT is a more specific indicator of liver injury. Moreover, as the intracellular ALT is found only in the cell cytoplasm, while most of AST content is found in the cell mitochondria, increased AST is related to severe hepatic injury since it shows not only cytoplasmic enzymes leaked into the circulation but the mitochondrial enzymes as well70,71.
Limitations of the present study include the lack of expression analysis of the angiotensin receptors (AT1R and AT2R) in the liver. The precise pathways activated by Ang II and Ang III in the context of diabetes and S. boulardii treatment remain to be elucidated, but the results from the present study do imply that the imbalance of RAS peptides could well have a role in the development of diabetic-liver injury. Besides, our results demonstrated that S. boulardii administration normalizes the concentration of RAS peptides while liver damage was also attenuated, showing that the changes in RAS peptides levels are at least in part responsible for this beneficial effect. Further studies will be needed to elucidate which pathway is predominantly activated by Ang II and Ang III, to understand the exact function of those peptides in the liver of diabetic animals.
Thus, in summary, this study provided histomorphological and biochemical analyses on the liver after S. boulardii administration on T1DM mice. Our results demonstrated that S. boulardii administration in STZ-induced diabetic mice reduces oxidative stress, normalizes the level of RAS components, and attenuates diabetes-induced liver injury, supporting the hypothesis that this yeast may have a role in the treatment of diabetes as a potential adjunctive therapy to reduce hepatic and metabolic complications of the disease.
Author contributions
T.C., I.A., A.B., and M.S. participated and conceived the research design. L.B., I.A., A.B., R.A., F.F., L.S., D.D., and R.Y. performed experiments and data analyses. T.C., I.A., K.A., D.C., C.T. and L.B. interpreted and discussed the data. L.B. wrote the manuscript. T.C., C.T., D.C. and K.A. refined the final draft and revised the manuscript. All authors read and approved the final version of the manuscript.
Funding
This work was supported by the Fundação de Amparo à Pesquisa do Estado de São Paulo, FAPESP [grant number 2016/24059-2]; and by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brasil (CAPES)—Finance Code 001.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Eisenbarth GS. Type I diabetes mellitus. A chronic autoimmune disease. N. Engl. J. Med. 1986;314:1360–1368. doi: 10.1056/NEJM198605223142106. [DOI] [PubMed] [Google Scholar]
- 2.Atkinson MA, Eisenbarth GS, Michels AW. Type 1 diabetes. Lancet (London, England) 2014;383:69–82. doi: 10.1016/S0140-6736(13)60591-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Katsarou A, et al. Type 1 diabetes mellitus. Nat. Rev. Dis. Prim. 2017;3:17016. doi: 10.1038/nrdp.2017.16. [DOI] [PubMed] [Google Scholar]
- 4.Maritim AC, Sanders RA, Watkins JB. Diabetes, oxidative stress, and antioxidants: A review. J. Biochem. Mol. Toxicol. 2003;17:24–38. doi: 10.1002/jbt.10058. [DOI] [PubMed] [Google Scholar]
- 5.Halliwell B. Antioxidants in human health and disease. Annu. Rev. Nutr. 1996;16:33–50. doi: 10.1146/annurev.nu.16.070196.000341. [DOI] [PubMed] [Google Scholar]
- 6.Korshunov SS, Skulachev VP, Starkov AA. High protonic potential actuates a mechanism of production of reactive oxygen species in mitochondria. FEBS Lett. 1997;416:15–18. doi: 10.1016/S0014-5793(97)01159-9. [DOI] [PubMed] [Google Scholar]
- 7.Gutteridge JMC, Halliwell B. Antioxidants: Molecules, medicines, and myths. Biochem. Biophys. Res. Commun. 2010;393:561–564. doi: 10.1016/j.bbrc.2010.02.071. [DOI] [PubMed] [Google Scholar]
- 8.Baynes JW, Thorpe SR. Role of oxidative stress in diabetic complications: A new perspective on an old paradigm. Diabetes. 1999;48:1–9. doi: 10.2337/diabetes.48.1.1. [DOI] [PubMed] [Google Scholar]
- 9.Sánchez-Valle V, Chávez-Tapia NC, Uribe M, Méndez-Sánchez N. Role of oxidative stress and molecular changes in liver fibrosis: A review. Curr. Med. Chem. 2012;19:4850–4860. doi: 10.2174/092986712803341520. [DOI] [PubMed] [Google Scholar]
- 10.Evangelista FS. Complications of type 1 diabetes mellitus are associated with renin angiotensin system: The role of physical exercise as therapeutic tool. Pancreat. Disord. Ther. 2014;04:1–7. doi: 10.4172/2165-7092.1000133. [DOI] [Google Scholar]
- 11.Vidotti DB, et al. High glucose concentration stimulates intracellular renin activity and angiotensin II generation in rat mesangial cells. Am. J. Physiol. 2004;286:1039–1045. doi: 10.1152/ajprenal.00371.2003. [DOI] [PubMed] [Google Scholar]
- 12.Singh VP, Le B, Khode R, Baker KM, Kumar R. Intracellular angiotensin II production in diabetic rats is correlated with cardiomyocyte apoptosis, oxidative stress, and cardiac fibrosis. Diabetes. 2008;57:3297–3306. doi: 10.2337/db08-0805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ko SH, et al. High glucose increases extracellular matrix production in pancreatic stellate cells by activating the renin-angiotensin system. J. Cell. Biochem. 2006;98:343–355. doi: 10.1002/jcb.20797. [DOI] [PubMed] [Google Scholar]
- 14.Taskin E, Guven C. Local renin-angiotensin system at liver and crosstalk with hepatic diseases. Renin-Angiotensin Syst. 2017;I:215–239. [Google Scholar]
- 15.Bataller R, et al. Activated human hepatic stellate cells express the renin-angiotensin system and synthesize angiotensin II. Gastroenterology. 2003;125:117–125. doi: 10.1016/S0016-5085(03)00695-4. [DOI] [PubMed] [Google Scholar]
- 16.Stenman LK, Burcelin R, Lahtinen S. Establishing a causal link between gut microbes, body weight gain and glucose metabolism in humans: Towards treatment with probiotics. Benef. Microbes. 2016;7:11–22. doi: 10.3920/BM2015.0069. [DOI] [PubMed] [Google Scholar]
- 17.Gomes AC, Bueno AA, de Souza RGM, Mota JF. Gut microbiota, probiotics and diabetes. Nutr. J. 2014;13:60. doi: 10.1186/1475-2891-13-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McFarland LV, Bernasconi P. Saccharomyces boulardii: A review of an innovative biotherapeutic agent. Microb. Ecol. Health Dis. 1993;6:157–171. [Google Scholar]
- 19.Duman DG, et al. Saccharomyces boulardii ameliorates clarithromycin- and methotrexate-induced intestinal and hepatic injury in rats. Br. J. Nutr. 2013;110:493–499. doi: 10.1017/S000711451200517X. [DOI] [PubMed] [Google Scholar]
- 20.Szajewska H, Kołodziej M. Systematic review with meta-analysis: Saccharomyces boulardii in the prevention of antibiotic-associated diarrhoea. Aliment. Pharmacol. Ther. 2015;42:793–801. doi: 10.1111/apt.13344. [DOI] [PubMed] [Google Scholar]
- 21.Everard A, Matamoros S, Geurts L, Delzenne NM, Cani PD. Saccharomyces boulardii administration changes gut microbiota and reduces hepatic steatosis, low-grade inflammation, and fat mass in obese and type 2 diabetic db/db mice. MBio. 2014;5:e01011–e1014. doi: 10.1128/mBio.01011-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brandão ABP, et al. Saccharomyces Boulardii attenuates autonomic cardiovascular dysfunction and modulates inflammatory cytokines in diabetic mice. Diabetes. 2018 doi: 10.2337/db18-2365-PUB. [DOI] [Google Scholar]
- 23.Albuquerque RCMF, et al. Saccharomyces boulardii Tht 500101 changes gut microbiota and ameliorates hyperglycaemia, dyslipidaemia, and liver inflammation in streptozotocin-diabetic mice. Benef. Microbes. 2019;10:901–912. doi: 10.3920/BM2019.0056. [DOI] [PubMed] [Google Scholar]
- 24.Percie du Sert N, et al. Reporting animal research: Explanation and elaboration for the ARRIVE guidelines 2.0. PLOS Biol. 2020;18:e3000411. doi: 10.1371/journal.pbio.3000411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hayashi K, Kojima R, Ito M. Strain differences in the diabetogenic activity of streptozotocin in mice. Biol. Pharm. Bull. 2006;29:1110–1119. doi: 10.1248/bpb.29.1110. [DOI] [PubMed] [Google Scholar]
- 26.Deeds MC, et al. Single dose streptozotocin-induced diabetes: Considerations for study design in islet transplantation models. Lab. Anim. 2011;45:131–140. doi: 10.1258/la.2010.010090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lamprecht MR, Sabatini DM, Carpenter AE. Cell Profiler: Free, versatile software for automated biological image analysis. Biotechniques. 2007;42:71–75. doi: 10.2144/000112257. [DOI] [PubMed] [Google Scholar]
- 28.Sant’Anna LB, Sant’Anna N, Parolini O. Application of computer assisted image analysis for identifying and quantifying liver fibrosis in a experimental model. J. Comput. Interdiscip. Sci. 2011;2:139–148. [Google Scholar]
- 29.Reznick AZ, Packer L. Oxidative damage to proteins: spectrophotometric method for carbonyl assay. Methods Enzymol. 1994;233:357–363. doi: 10.1016/S0076-6879(94)33041-7. [DOI] [PubMed] [Google Scholar]
- 30.Gonzalez Flecha B, Llesuy S, Boveris A. Hydroperoxide-initiated chemiluminescence: an assay for oxidative stress in biopsies of heart, liver, and muscle. Free Radic. Biol. Med. 1991;10:93–100. doi: 10.1016/0891-5849(91)90002-K. [DOI] [PubMed] [Google Scholar]
- 31.Boveris A, Chance B. The mitochondrial generation of hydrogen peroxide General properties and effect of hyperbaric oxygen. Biochem. J. 1973;134:707–716. doi: 10.1042/bj1340707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Flohé L, Günzler WA. Assays of glutathione peroxidase. Methods Enzymol. 1984;105:114–121. doi: 10.1016/S0076-6879(84)05015-1. [DOI] [PubMed] [Google Scholar]
- 33.Han X, et al. Knockout of the TauT gene predisposes C57BL/6 mice to streptozotocin-induced diabetic nephropathy. PLoS ONE. 2015;10:1–13. doi: 10.1371/journal.pone.0117718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Le TKC, et al. Bifidobacterium species lower serum glucose, increase expressions of insulin signaling proteins, and improve adipokine profile in diabetic mice. Biomed. Res. 2015;36:63–70. doi: 10.2220/biomedres.36.63. [DOI] [PubMed] [Google Scholar]
- 35.Memarrast F, et al. Comparative evaluation of probiotics effects on plasma glucose, lipid, and insulin levels in streptozotocin-induced diabetic rats. Diabetes. Metab. Res. Rev. 2017;33:e2912. doi: 10.1002/dmrr.2912. [DOI] [PubMed] [Google Scholar]
- 36.Razmpoosh E, Javadi M, Ejtahed H-S, Mirmiran P. Probiotics as beneficial agents in the management of diabetes mellitus: A systematic review. Diabetes. Metab. Res. Rev. 2016;32:143–168. doi: 10.1002/dmrr.2665. [DOI] [PubMed] [Google Scholar]
- 37.Al-Salami H, et al. Probiotic treatment reduces blood glucose levels and increases systemic absorption of gliclazide in diabetic rats. Eur. J. Drug Metab. Pharmacokinet. 2008;33:101–106. doi: 10.1007/BF03191026. [DOI] [PubMed] [Google Scholar]
- 38.Meng X, Li S, Li Y, Gan RY, Li HB. Gut microbiota’s relationship with liver disease and role in hepatoprotection by dietary natural products and probiotics. Nutrients. 2018;10:1457. doi: 10.3390/nu10101457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yu L, et al. Saccharomyces boulardii administration changes gut microbiota and attenuates D-galactosamine-induced liver injury. Sci. Rep. 2017;7:1359. doi: 10.1038/s41598-017-01271-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Li M, Zhu L, Xie A, Yuan J. Oral administration of Saccharomyces boulardii ameliorates carbon tetrachloride-induced liver fibrosis in rats via reducing intestinal permeability and modulating gut microbial composition. Inflammation. 2014;38:170–179. doi: 10.1007/s10753-014-0019-7. [DOI] [PubMed] [Google Scholar]
- 41.Baynes JW. Role of oxidative stress in development of complications in diabetes. Diabetes. 1991;40:405–412. doi: 10.2337/diab.40.4.405. [DOI] [PubMed] [Google Scholar]
- 42.Shukla K, Dikshit P, Tyagi MK, Shukla R, Gambhir JK. Ameliorative effect of Withania coagulans on dyslipidemia and oxidative stress in nicotinamide–streptozotocin induced diabetes mellitus. Food Chem. Toxicol. 2012;50:3595–3599. doi: 10.1016/j.fct.2012.07.026. [DOI] [PubMed] [Google Scholar]
- 43.Sheweita SA, Mashaly S, Newairy AA, Abdou HM, Eweda SM. Changes in oxidative stress and antioxidant enzyme activities in streptozotocin-induced diabetes mellitus in rats: Role of Alhagi maurorum extracts. Oxid. Med. Cell. Longev. 2016;2016:1–8. doi: 10.1155/2016/5264064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lucchesi AN, de Freitas NT, Cassettari LL, Marques SFG, Spadella CT. Diabetes mellitus triggers oxidative stress in the liver of alloxan-treated rats: a mechanism for diabetic chronic liver disease. Acta Cir. Bras. 2013;28:502–508. doi: 10.1590/S0102-86502013000700005. [DOI] [PubMed] [Google Scholar]
- 45.Bukan N, et al. Lipid peroxidation and scavenging enzyme levels in the liver of streptozotocin-induced diabetic rats. Indian J. Biochem. Biophys. 2003;40:447–450. [PubMed] [Google Scholar]
- 46.Wang Y, et al. Antioxidant properties of probiotic bacteria. Nutrients. 2017;9:521. doi: 10.3390/nu9050521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fakruddin M, Hossain MN, Ahmed MM. Antimicrobial and antioxidant activities of Saccharomyces cerevisiae IFST062013, a potential probiotic. BMC Complement. Altern. Med. 2017;17:1–11. doi: 10.1186/s12906-017-1591-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Datta S, Timson DJ, Annapure US. Antioxidant properties and global metabolite screening of the probiotic yeast Saccharomyces cerevisiae var. boulardii. J. Sci. Food Agric. 2017;97:3039–3049. doi: 10.1002/jsfa.8147. [DOI] [PubMed] [Google Scholar]
- 49.Lee KS, Buck M, Houglum K, Chojkier M. Activation of hepatic stellate cells by TGF alpha and collagen type I is mediated by oxidative stress through c-myb expression. J. Clin. Invest. 1995;96:2461–2468. doi: 10.1172/JCI118304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Leung PS, Chappell MC. A local pancreatic renin-angiotensin system: Endocrine and exocrine roles. Int. J. Biochem. Cell Biol. 2003;35:838–846. doi: 10.1016/S1357-2725(02)00179-6. [DOI] [PubMed] [Google Scholar]
- 51.Wysocki J, Ye M, Batlle D. Plasma and kidney angiotensin peptides: importance of the aminopeptidase A/angiotensin III axis. Am. J. Hypertens. 2015;28:1418–1426. doi: 10.1093/ajh/hpv054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Herath CB, et al. Upregulation of hepatic angiotensin-converting enzyme 2 (ACE2) and angiotensin-(1–7) levels in experimental biliary fibrosis. J. Hepatol. 2007;47:387–395. doi: 10.1016/j.jhep.2007.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lubel JS, Herath CB, Burrell LM, Angus PW. Liver disease and the renin-angiotensin system: Recent discoveries and clinical implications. J. Gastroenterol. Hepatol. 2008;23:1327–1338. doi: 10.1111/j.1440-1746.2008.05461.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bosnyak S, et al. Relative affinity of angiotensin peptides and novel ligands at AT1 and AT2 receptors. Clin. Sci. (Lond) 2011;121:297–303. doi: 10.1042/CS20110036. [DOI] [PubMed] [Google Scholar]
- 55.Cruz-Diaz N, Wilson BA, Chappell MC. Peptidases and the renin-angiotensin system: The Alternative angiotensin-(1–7) cascade. Enzyme Inhibit. Activ. 2017 doi: 10.5772/65949. [DOI] [Google Scholar]
- 56.Souza-Mello V. Hepatic structural enhancement and insulin resistance amelioration due to AT1 receptor blockade. World J. Hepatol. 2017 doi: 10.4254/wjh.v9.i2.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gopal K, et al. Attrition of hepatic damage inflicted by angiotensin II with α-tocopherol and β-carotene in experimental apolipoprotein e knock-out mice. Sci. Rep. 2015;5:1–15. doi: 10.1038/srep18300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Padia SH, et al. Conversion of renal angiotensin II to angiotensin III is critical for AT2 receptor-mediated natriuresis in rats. Hypertension. 2008;51:460–465. doi: 10.1161/HYPERTENSIONAHA.107.103242. [DOI] [PubMed] [Google Scholar]
- 59.Natarajan A, Villar VAM, Jose PA. Nephrology and Fluid/electrolyte Physiology (Third Edition) Amsterdam: Elsevier Inc; 2019. Renal Modulation: The Renin-Angiotensin System; pp. 165–188. [Google Scholar]
- 60.Warner FJ, Lubel JS, McCaughan GW, Angus PW. Liver fibrosis: a balance of ACEs? Clin. Sci. 2007;113:109–118. doi: 10.1042/CS20070026. [DOI] [PubMed] [Google Scholar]
- 61.Salih ND, Muslih RK, Hamoodi SR. Histological liver changes in streptozotocin induced diabetic mice. Int. Med. J. Malaysia. 2009;8:1–4. [Google Scholar]
- 62.Guven A, et al. Effects of melatonin on streptozotocin-induced diabetic liver injury in rats. Acta Histochem. 2006;108:85–93. doi: 10.1016/j.acthis.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 63.Nayak NC, et al. The nature and significance of liver cell vacuolation following hepatocellular injury: An analysis based on observations on rats rendered tolerant to hepatotoxic damage. Virchows Arch. 1996;428:353–365. doi: 10.1007/BF00202202. [DOI] [PubMed] [Google Scholar]
- 64.Haga S, et al. Compensatory recovery of liver mass by Akt-mediated hepatocellular hypertrophy in liver-specific STAT3-deficient mice. J. Hepatol. 2005;43:799–807. doi: 10.1016/j.jhep.2005.03.027. [DOI] [PubMed] [Google Scholar]
- 65.Nagy P, et al. Reconstitution of liver mass via cellular hypertrophy in the rat. Hepatology. 2000;33:339–345. doi: 10.1053/jhep.2001.21326. [DOI] [PubMed] [Google Scholar]
- 66.Miyaoka Y, et al. Hypertrophy and unconventional cell division of hepatocytes underlie liver regeneration. Curr. Biol. 2012;22:1166–1175. doi: 10.1016/j.cub.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 67.Kew MC. Serum aminotransferase concentration as evidence of hepatocellular damage. Lancet. 2000;355:591–592. doi: 10.1016/S0140-6736(99)00219-6. [DOI] [PubMed] [Google Scholar]
- 68.Schmidt E, Schmidt FW. Enzyme diagnosis of liver disease. Clin. Biochem. 1993;26:241–251. doi: 10.1016/0009-9120(93)90123-N. [DOI] [PubMed] [Google Scholar]
- 69.Lindblom P, et al. Isoforms of alanine aminotransferases in human tissues and serum: Differential tissue expression using novel antibodies. Arch. Biochem. Biophys. 2007;466:66–77. doi: 10.1016/j.abb.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 70.Ozer J, Ratner M, Shaw M, Bailey W, Schomaker S. The current state of serum biomarkers of hepatotoxicity. Toxicology. 2008;245:194–205. doi: 10.1016/j.tox.2007.11.021. [DOI] [PubMed] [Google Scholar]
- 71.Rej R. Aspartate aminotransferase activity and isoenzyme proportions in human liver tissues. Clin. Chem. 1978;24:1971–1979. doi: 10.1093/clinchem/24.11.1971. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.