Abstract
Purpose
Patient-reported outcome measures (PROMs) have traditionally been used for research purposes, but are now being used to evaluate outcomes from the patient’s perspective and inform ongoing management and quality of care. We used quantitative and qualitative approaches to evaluate the short-version Disabilities of the Arm, Shoulder, and Hand (QuickDASH) and the Patient-Specific Functional Scale (PSFS) with regard to patient preference and measurement of patient goals and their responsiveness after treatment.
Methods
Patients 18 years or older undergoing elective hand surgery received the QuickDASH and PSFS questionnaires before and at 6 weeks after surgery. Two additional questions intended to elicit patients’ preferences regarding the QuickDASH and PSFS were included. Responsiveness was measured by change in pre- to postoperative score. We analyzed patients’ responses to the 2 additional questions to identify themes in PROM preferences. Results from the quantitative and qualitative analyses were combined into a convergent mixed-methods (eg, quantitative and qualitative) analysis.
Results
Thirty-eight patients completed preoperative questionnaires; 25 (66%) completed postoperative questionnaires. Seventeen patients (77%) preferred the PSFS, 3 (14%) had no preference, 2 (9%) preferred the QuickDASH. The average change from pre- to postoperative QuickDASH was −10 (SD, 20), and that of the PSFS was −27 (SD, 26). Ten patients (40%) reported QuickDASH score changes above the minimal clinically importance difference (MCID), 17 patients (68%) reported PSFS score changes above the MCID. Content analysis revealed 4 themes in preference for a PROM: instrument simplicity (ease of instrument understanding and completion), personalized assessment (individualization and relevance), goal directed (having measurable aims or objectives), distinct items (concrete or specific instrument items or functions).
Conclusions
Most patients felt the PSFS better measured their goals because it is a simple, personalized instrument with distinct domains.
Clinical relevance
Whereas standardized PROMs may better compare across populations, physicians, or conditions, employing PROMs that address patient-specific goals may better assess aspects of care most important to patients. A combination of these 2 types of PROMs can be used to assess outcomes and inform quality of care.
Keywords: Hand surgery, patient-centered care, patient-reported outcome measures, shared decision making
AS HEALTH CARE SYSTEMS MOVE toward delivering value-based care, there is growing enthusiasm for the measurement of outcomes from the patient perspective. Patient-reported outcome measures (PROMs) are designed to evaluate aspects of health from the patient’s perspective, in contrast to physician-measured or objective outcomes (eg, range of motion). Although PROMs have traditionally been used to assess outcomes for research, they are increasingly used as part of health care strategy to inform ongoing care, measure outcomes from the patient perspective, and also for reimbursement by insurance carriers.1–3 For example, it is possible that some well-validated PROMs that demonstrate stable psychometric properties may be appropriate to assess patient outcomes for research, but may not be understandable or actionable for use at point of care to inform management decisions to improve quality of care. As such, understanding how patients perceive PROMs and their perspective on which best reflect their own experience and symptoms can improve our understanding of which PROMs may be better for point of care use (eg, those deemed relevant and actionable by the patient and physician).4
Patient-reported outcome measure designs vary by domain and by what is measured. Several validated PROMs are used in the field of hand and upper extremity surgery, and although the majority of standardized PROMs ask about the ability to complete functional tasks, such tasks may not be important to certain patients. For example, a recent qualitative study found that patients define their goals for treatment based on specific functional tasks (eg, yoga, hiking) that may not be queried on a standardized PROM.5 Indeed, just because information from PROMs is “reported by the patient” does not mean it is important or valued by the patient.
Patient-centered outcome measures (PCOMs), a new concept in outcome measurement, are outcome measures that align with the values of the patient and measure the impact of a disease and/or treatment based on what is important to the individual patient.6–8 Patient-centered outcome measures aim to translate an outcome score into an interpretable measure that is important to the patient and actionable. In contrast to the short-version Disabilities of the Arm, Shoulder, and Hand (QuickDASH) (a commonly used hand and upper extremity outcome measurement tool), the Patient-Specific Functional Scale (PSFS), which has been validated for patients with upper extremity musculoskeletal problems,9 allows patients to identify functional goals important to him or her in an open-ended manner. It is currently unknown how each instrument assesses aspects of care that align with the individual patient’s values and preferences while also assessing the patient outcome as a whole (eg, a PROM may measure 1 part of a patient’s outcome as a whole).10 Although the QuickDASH allows for comparison across diagnoses and patients and has been validated in multiple conditions, it may be limited for use at point of care because some questions may not be relevant or important to all patients. Although a relatively new and less-utilized entity, prior research has shown that several tasks frequently listed on the PSFS are not present on the QuickDASH including fastening buttons, nail trimming, and holding a book.5 Eppler et al,11 using a qualitative approach to better understand quality from the patient perspective, also noted that many functional goals described by patients were specific and may be difficult to capture using standardized PROMs.
Although the psychometric properties of the QuickDASH and the PSFS have been studied at length,5,9,12,13 no studies have evaluated which PROM patients feel more appropriately measures their goals in treatment—which prior work has shown can aid in patient communication and involvement in care when used at point of care. As the health care system moves toward an approach that encourages patient-centered and goal-directed care, it is increasingly important to recognize individual patient goals and ensure these goals are reflected in outcome measurement instruments. In this pilot study, we aimed to evaluate patient perspectives of the QuickDASH and PSFS through a mixed-methods (quantitative and qualitative) approach by evaluating which instrument patients prefer and the responsiveness to change of each instrument.
METHODS
Patient selection
After obtaining institutional review board approval, we recruited patients undergoing elective hand and upper extremity surgery in the preoperative holding area on the day of their surgery. Patients of 1 hand and upper extremity–trained surgeon (R.N.K.) were enrolled by a research assistant via consecutive sampling between March 2018 and May 2018. Inclusion criteria were age equal to or greater than 18, elective surgery, and English literacy. We excluded those having surgery for trauma and patients that would be immobilized for greater than 4 weeks after surgery. We chose immobilization time of less than 4 weeks to ensure patients had an opportunity to realize a functional improvement by their 6-week follow-up visit. As an initial pilot investigation, we aimed to enroll at least 35 patients. Accounting for 20% loss to follow-up, we intended to have at least 25 patients with completed questionnaires, based on prior work achieving saturation in qualitative analysis.14–17
Data collection
After consent, patients were given the QuickDASH and the PSFS questionnaires prior to undergoing surgery. The QuickDASH is an 11-item questionnaire that was adapted from the 30-item DASH as a region-specific measure of disability and symptoms in patients with upper extremity disorders.18,19 The QuickDASH asks patients questions about their ability to conduct 6 specific, predetermined tasks, their limitations in work and social activities, and their level of pain, tingling, and interferences with sleep. The QuickDASH is scored from 0 to 100, 0 indicating no disability and 100 indicating extreme disability. The PSFS asks patients to identify between 3 and 5 activities with which they have difficulty because of their hand or upper extremity condition and rate them on a scale from 1 (unable to perform activity) to 10 (able to perform activity at same level as before injury or problem). The scores for each activity are averaged to produce a score from 1 to 10 (1 indicating extreme disability and 10 indicating no disability). Patients were subsequently given the same questionnaires at their second follow-up visit, at least 6 weeks from the date of their surgery. The PSFS was given prior to the QuickDASH to prevent bias (so that the standardized items provided on the QuickDASH did not affect the open-ended items patients provided on the PSFS). After completion of the questionnaires, they were asked 2 follow-up questions: (1) Which questionnaire (the QuickDASH or the PSFS) better addressed your goals during this clinical experience? and (2) Please explain why you chose that questionnaire.
Quantitative data analysis
Patient demographics were recorded, including the procedure performed. The PSFS score was standardized (so that a higher score represented greater disability)20 and normalized to match the QuickDASH (so that each score was out of 100)21–23 for analysis. Pre- and postsurgical QuickDASH and PSFS scores were calculated. Descriptive statistics (mean and SD) of the change in score for each questionnaire were recorded. The frequency and percent of questionnaire preference was recorded. Change in score was used as a proxy for responsiveness. We calculated the frequency and percent of patient changes above the minimal clinical importance difference (MCID) for each questionnaire based on prior work (eg, proportions of patients that reach the MCID threshold). Because MCID refers to the smallest difference between scores that a patient can detect to be beneficial or harmful, we used MCID thresholds for responsiveness of the instrument. An MCID of 14 and 25 were used for the QuickDASH and the PSFS, respectively, based upon previous literature.9,24–31
Qualitative data analysis
We analyzed the patients’ answers to the open-ended questions regarding why they chose a specific questionnaire using qualitative content analysis.32–34 The authors followed the consolidated criteria for reporting qualitative research (COREQ) (Appendix A; available on the Journal’s Web site at www.jhandsurg.org),35 a 32-item checklist to ensure study rigor and aid in interpretation. Two members of the research team (R.N.K., L.M.S.) independently analyzed the open-ended responses to identify themes. Three phases of coding were conducted: open coding, selective coding, and development of themes for answers to the question, “Please explain why you chose that questionnaire”. During open coding, the 2 coders reviewed patient responses, took notes on these responses, and identified concepts of interest that they labeled with subcodes. Reviewers met after coding 5 responses to create an agreed-upon codebook and then completed open coding of all responses. The codebook was applied to all of the patient responses, new codes were included until there were no further new codes identified (saturation), and the final codebook was reapplied to all transcripts. Discrepancies in coding were resolved by discussion to consensus.
Convergent data analysis
Results from the quantitative and qualitative analyses were integrated and arrayed side-by-side with a convergent mixed-methods analysis in accordance with prior investigations.36–38 The integration involved merging the results from the quantitative and qualitative data so that a comparison could be made and a more complete understanding could emerge than what was provided by the quantitative or the qualitative results alone.
RESULTS
Thirty-eight patients completed the preoperative questionnaires (no patients declined to participate). Twenty-five patients (66%) completed the postoperative questionnaires. Patient demographics, procedure type, and number of procedures are noted in Table 1.
TABLE 1.
Demographics, procedure type, and number of procedures*
| Characteristic | Count, n (%) |
|---|---|
| Total | 25 |
| Mean Age, y (SD) | 54.8 (18.9) |
| Sex, n (%) | |
| Male | 10 (40) |
| Female | 15 (60) |
| Annual household income, n (%) | |
| <$49,000 | 1 (7.7) |
| $50,000–$99,999 | 4 (30.8) |
| $100,000–$149,999 | 0 (0) |
| $150,000–$199,999 | 3 (23.1) |
| $200,000–$249,999 | 2 (15.4) |
| >$250,000 | 3 (23.1) |
| Race/ethnicity, n (%) | |
| White/Caucasian | 17 (73.9) |
| Black or African American | 1 (4.3) |
| American Indian or Alaska Native | 0 (0) |
| Asian | 1 (4.3) |
| Hispanic | 3 (13.0) |
| Native Hawaiian or other Pacific Islander | 0 (0) |
| Other | 1 (4.3) |
| Employment status, n (%) | |
| Full-time | 7 (41.2) |
| Part-time | 1 (5.9) |
| Retired | 6 (35.3) |
| No work outside the home | 0 (0) |
| Disabled | 1 (5.9) |
| Unemployed | 1 (5.9) |
| Student | 1 (5.9) |
| Highest level of education, n (%) | |
| Elementary school | 0 (0) |
| High school | 2 (12.5) |
| 2-Year college | 3 (18.8) |
| 4-Year college | 5 (31.3) |
| Postcollege/graduate | 6 (37.5) |
| Relationship status, n (%) | |
| Married | 14 (82.4) |
| Domestic partnership | 0 (0) |
| Single, never married | 1 (5.9) |
| Single, divorced or separated | 1 (5.9) |
| Single, widowed | 1 (5.9) |
| Primary insurance type, n (%) | |
| Medicaid/Medi-Cal | 1 (5.6) |
| Medicare | 8 (44.4) |
| Military | 0 (0) |
| Privately insured | 9 (50) |
| San Mateo County Health Insurance | 0 (0) |
| Uninsured | 0 (0) |
| Procedure, n (%) | |
| Carpal tunnel release | 9 (36) |
| Trigger finger release | 7 (28) |
| DeQuervain release | 2 (8) |
| Other | 7 (28) |
| Number of procedures, n (%) | |
| 1 | 23 (92) |
| 2 | 2 (8) |
| 3 or more | 0 (0) |
Some patients did not fully complete the demographics questionnaire; therefore, not all raw numbers add up to 25.
Quantitative results
When asked which PROM they preferred, 17 patients (77%) preferred the PSFS, 3 patients (14%) had no preference, and 2 patients (9%) preferred the QuickDASH. The average change in score from pre- to postoperative QuickDASH was −10 (SD, 20) and that of the PSFS was −27 (SD, 26) (Table 2).
TABLE 2.
PROM Scores
| Measurement Instrument | Preoperative Score Mean (SD) | Postoperative Score Mean (SD) | Mean Change in Score (SD) |
|---|---|---|---|
| QuickDASH | 43.8 (23.8) | 33.5 (19.7) | −10.26 (20.4)* |
| PSFS | 67.4 (17.7) | 40.2 (20.3) | −27.24 (26.2)* |
Indicates significant difference (P < .05).
Ten patients (40%) reported a change in QuickDASH above the MCID, 17 (68%) reported a change in PSFS above the MCID. Among 15 patients who did not demonstrate QuickDASH score changes above the MCID, 9 (60%) demonstrated changes greater than the MCID of their PSFS score. Among 6 patients who did not demonstrate changes greater than the MCID on their PSFS questionnaire, 1 demonstrated a change in the QuickDASH greater than the MCID. Table 3 demonstrates scenarios in which the MCID of the QuickDASH and PSFS vary by calculation method and patient population.
TABLE 3.
Results Displayed as Number and Percentage of Patients Above MCID for the QuickDASH and PSFS, Respectively
| QuickDASH MCID | |||||
|---|---|---|---|---|---|
| 6.830 | 829 | 1128 | 1424 | ||
| PSFS MCID | 2031 | 15 (60) | 20 (80) | 14 (56) | 20 (80) | 13 (52) | 20 (80) | 10 (40) | 20 (80) |
| 2531 | 15 (60) | 17 (68) | 14 (56) | 17 (68) | 13 (52) | 17 (68) | 10 (40) | 17 (68) | |
| 299 | 15 (60) | 11 (44) | 14 (56) | 11 (44) | 13 (52) | 11 (44) | 10 (40) | 11 (44) | |
| 3031 | 15 (60) | 11 (44) | 14 (56) | 11 (44) | 13 (52) | 11 (44) | 10 (40) | 11 (44) | |
Qualitative results
Representative responses as to why patients preferred a specific instrument are listed in Figure 1. Analysis of the open-ended responses revealed 4 themes: (1) instrument simplicity, defined as the ease of understanding and completion of the instrument; (2) personalized assessment, defined as the individualization and relevance of an instrument to a specific patient; (3) goal-directed, defined as having a measurable aim or objective that a patient wishes to achieve; and (4) distinct items, defined as concrete or specific tasks or functions that are recognizably different from other tasks or functions.
FIGURE 1:
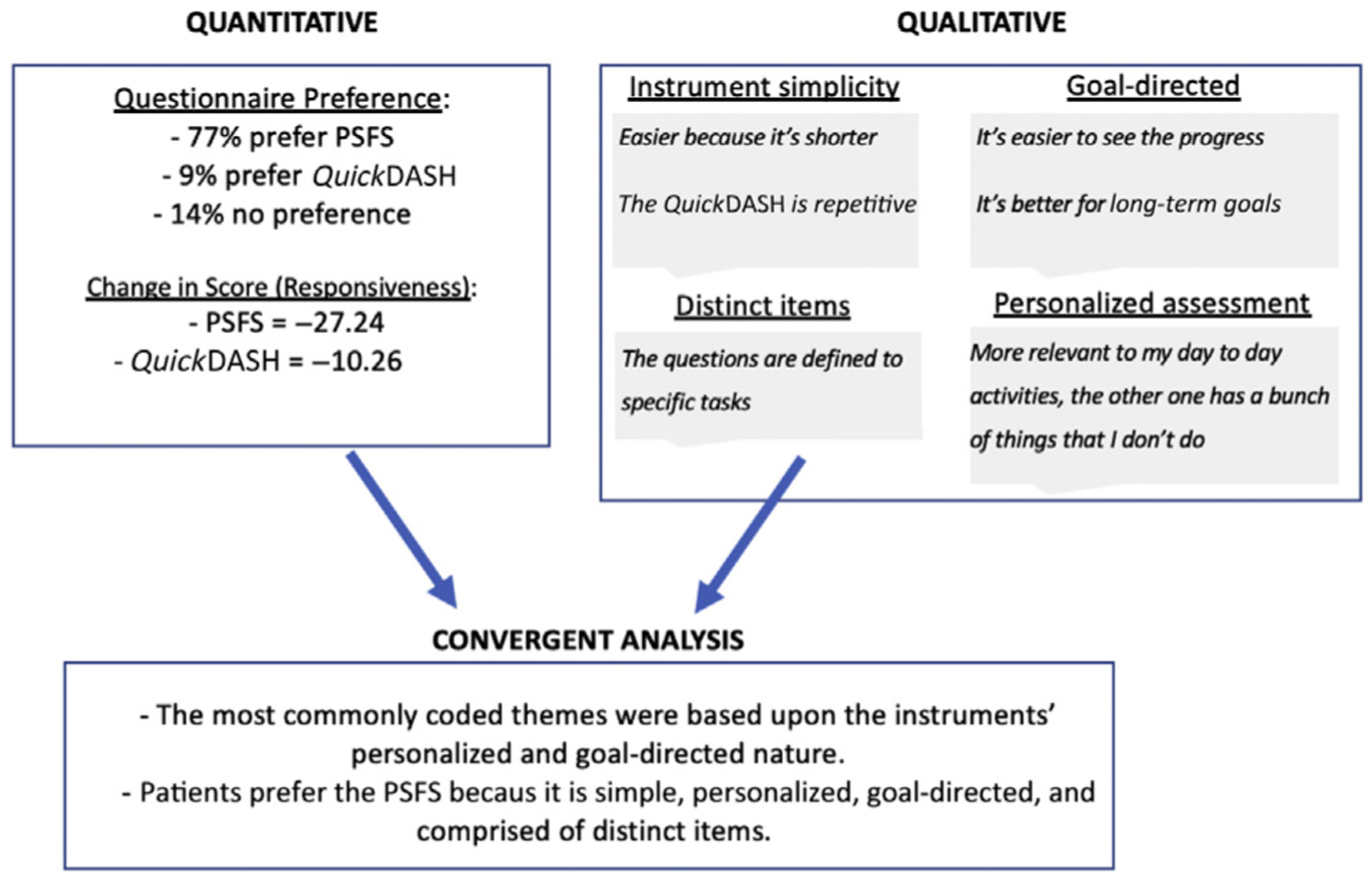
Illustration of the convergent mixed-methods analysis allowing integration of quantitative and qualitative data.
DISCUSSION
Patient-reported outcome measures are transitioning from being used solely for research purposes toward informing care decisions to improve quality of care. As such, we sought to understand the patient perspective on 2 PROMs that measure different constructs (eg, functional goals vs upper extremity disability) to assess whether one construct and instrument was preferred by patients. Our quantitative results suggest that patients believe the PSFS addresses their goals for hand surgery more frequently than the QuickDASH. Based on responses to open-ended questions, we also identified why patients believe the PSFS better addresses their goals and potentially why it can be more useful as a PROM for use and communication at point of care: it is a simple, personalized, and goal-directed instrument with distinct domains. Whereas traditional PROMs such as the DASH/QuickDASH can be important for assessing outcomes as a whole (eg, disability of the arm), their results may not be understandable and actionable for individual patients. As such, using instruments like the PSFS that allow patients to track their own progress toward their functional goals may be more actionable in improving quality of care and may be able to be used in conjunction with those that assist in comparisons across physicians or conditions or in clinical research efforts.
Importantly, we are not advocating for the sole use of the PSFS to evaluate outcomes, but instead, that outcomes assessment may be enhanced with the combined use of instruments to assess multiple facets of a patient’s outcome. The PSFS (and other non-standardized PROMs) do have limitations, some of which are mitigated by the concurrent use of a standardized PROM. Given that the PSFS asks patients to identify activities that they have difficulty performing, it may miss important patient symptoms like pain and numbness that are related to only certain activities. Additionally, the PSFS is less well studied with regard to its psychometric properties (eg, MCID, validity) and the populations/conditions in which it has been studied (compared with legacy instruments like the QuickDASH). Also, important to note is that evaluating change over time and comparisons between patients for each instrument differs—the QuickDASH outcome is a score based upon patients answering the same questions, whereas the PSFS outcome is a score based upon patient-selected and, therefore, varying goals. In addition, individualized and patient-specific PROMs are a relatively new entity and the barriers to their use, integration into clinical practice, and advantages/disadvantages war-rant further study.39–41
In a value-based delivery model in which physicians are reimbursed based upon outcomes and cost of care, understanding how outcomes are defined is critical. Quality of care can be measured from various perspectives. The importance of the patient perspective has led to the use of PROMs to assess quality in hand and orthopedic surgery. For example, the Centers for Medicare and Medicaid services is collecting data on quality measures using PROMs (Hip disability and Osteoarthritis Outcome Score [HOOS] and Knee Injury and Osteoarthritis Outcome Score [KOOS]) for total joint arthroplasty through Patient-Reported Outcome Performance Measures (PRO-PMs).1 Private payers have also begun implementing similar payment models.2,3 Our results suggest that this area requires further analyses prior to implementation of PRO-PMs by payers.
To our knowledge, no studies have sought to evaluate which outcome measures patients feel better addresses their goals in undergoing hand surgery. Prior studies have evaluated and established the psychometric properties of the PSFS for various hand and upper extremity conditions.9,12,13,42 McMillan and Binhammer12 evaluated the responsiveness of the DASH, Michigan Hand Outcomes Questionnaire (MHQ), and PSFS for various hand and wrist conditions and found the MHQ to be the most responsive at 6 months after surgery for those with carpal tunnel syndrome and the PSFS to be the most responsive for finger contracture. It is important to note that psychometric properties of various PROMs vary by patient population and condition studied.43,44 In addition, responsiveness assumes that constructs being measured are of equal weight to each individual patient. For example, when outcomes are measured based upon domains insignificant or irrelevant to the patient, a measure may be highly responsive and yet not important to the patient.
Our results should be viewed within their limitations. We used MCID thresholds as a proxy for minimum levels of responsiveness. The MCID varies by patient population and calculation method and should be interpreted with caution.43–45 The authors chose an MCID of 25 and 14 for the PSFS9,25–27 and QuickDASH,24–31,46 respectively; based upon prior literature however, the pathologies and patients from which these numbers were derived are different from those in this study. In addition, there is variation in the exact calculation method (eg, anchor-, distribution-, Delphi-based methods) used in the literature, each having their own advantages and disadvantages. Table 3 demonstrates scenarios in which MCIDs of the QuickDASH and PSFS vary by calculation method and patient population. Indeed, the variation in MCIDs in the published literature for various PROMs may, in part, reflect the variation in importance patients place on the items of the PROM. Our inclusion criteria and 66% follow-up rate represents a study limitation as well. We aimed to avoid e-mail or phone follow-up to avoid introducing bias into the results. In addition, we do not believe that those patients lost to follow-up represent a cohort different enough in their instrument preferences or surgical goals to affect our results. Given the different numerical outcomes scales of the QuickDASH and PSFS, direct comparison of the 2 is difficult. We attempted to align the 2 scales to achieve the best comparison with regard to responsiveness for the purpose of this investigation, in line with prior investigation.20–23
Limitations of the mixed-methods approach should be noted as well. Investigator bias and the researchers’ preconceived notions may affect the results for the qualitative analysis. We aimed to minimize such biases by including 2 reviewers (L.M.S. and R.N.K.). In addition, the patient transcripts were gathered in a standardized manner, which minimizes bias related to data collection and data interpretation, but lacks the depth that could be achieved by an interview. Other limitations include the small sample size, lack of a priori sample size estimate, and the heterogeneous population evaluated, which limit the external validity of the study. The goal of this study was not to validate the responsiveness of either instrument for a specific condition but, instead, to assess the quantitative responsiveness of an instrument in conjunction with the qualitative rationale for delivering care that is based on individual patients’ values and preferences. In addition, we did not measure the time needed to complete each instrument and the potential effect of response burden. It is possible that having patients derive their own goals and limitations requires more thought and effort; however, this is not reflected in the qualitative feedback received. In addition, we recognize that asking patients which instrument better addressed their goals in treatment may bias the results toward the PSFS (because it asks patients to identify their own goals); however, as the health care system moves toward an approach that encourages patient-centered and goal-directed care, we believe the recognition and alignment of patient goals with outcome measurement instruments becomes increasingly important. Prior work has shown the PSFS to display a floor effect (high number of patients recording minimum scores),42 which reduces the responsiveness of the instrument; however, no patient in this study recorded lower than a score of 28 on the preoperative PSFS. Lastly, the results of qualitative research are not necessarily meant to be generalizable, nor did we evaluate the PSFS from a population perspective, nor across various contexts (eg, language, region). Instead, the goal was to study a process and generate hypotheses about the mechanism.
Despite these limitations, we reason that a patient-specific PROM and standardized PROM may be used in a complementary manner or based upon the question at hand (eg, employing patient-specific PROMs to evaluate individual patient outcomes, employing standardized PROMs to evaluate populations of patients, and using both PROMs to evaluate quality of care delivered and support value-based reimbursement models).
ACKNOWLEDGMENTS
This work was supported by a National Institutes of Health K23AR073307-01 award (R.N.K.). The content of this work is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
The authors have complied with the ethical standards as detailed in Instructions to the Author set forth by the Journal of Hand Surgery.
APPENDIX A. COREQ PSFS
| Topic | Guide Questions/Description | Reported on (Page No.) and Comments |
|---|---|---|
| Domain 1: Research Team and Reflexivity | ||
| Personal characteristics | ||
| Interviewer/facilitator | Which author/s conducted the interview or focus group? | S.L.E. and L.M.S. distributed questionnaires |
| Credentials | What were the researcher’s credentials? eg, PhD, MD | L.M.S. — MD and S.L.E. — MPH (Title page) |
| Occupation | What was their occupation at the time of the study? | Resident and social sciences research professional |
| Sex | Was the researcher male or female? | Female |
| Experience and training | What experience or training did the researcher have? | Both facilitators have prior quantitative and qualitative research experience, S.L.E. has an MPH |
| Relationship with participants | ||
| Relationship established | Was a relationship established prior to study commencement? | No prior relationship was established |
| Participant knowledge of the interviewer | What did the participants know about the researcher? eg, personal goals, reasons for doing the research | The purpose of the research and research process were discussed during the consent process |
| Interviewer characteristics | What characteristics were reported about the interviewer/facilitator? eg, bias, assumptions, reasons and interests in the research topic? | No specific characteristics, biases, assumptions were reported |
| Domain 2: Study Design | ||
| Theoretical framework | ||
| Methodological orientation and theory | What methodological question was stated to underpin the study? eg, grounded theory, discourse analysis, ethnography, phenomenology, content analysis | Content analysis (page 7) |
| Participant selection | ||
| Sampling | How were participants selected? eg, purposive, convenience, consecutive, snowball | Convenience sample of those meeting inclusion criteria |
| Method of approach | How were participants approached? eg, face-to-face, telephone, mail, e-mail | Participants were approached in person (page 5) |
| Sample size | How many participants were in the study? | 38 patients were initially included (page 8) |
| Nonparticipation | How many people refused to participate or dropped out? Reasons? | 25 patients completed postoperative surveys. 13 patients did not come to their postoperative appointment (page 8) |
| Setting | ||
| Setting of data collection | Where were the data collected? eg, home, clinic, workplace | Baseline data were collected in the preoperative holding area. Follow-up data were collected in the clinic |
| Presence of nonparticipants | Was anyone else present besides the participants and researchers? | Occasionally patients’ family members were present in the preoperative holding area or in the clinic room during survey completion |
| Description of sample | What are the important characteristics of the sample? eg, demographic data, date | Patient demographics are listed in Table 1 |
| Data collection | ||
| Interview guide | Were questions, prompts, guides provided by the authors? Was it pilot-tested? | Question prompts were provided by the authors. The question prompts were not pilot-tested |
| Repeat interviews | Were repeat interviews carried out? If yes, how many? | No repeat interviews were carried out |
| Audio/visual recording | Did the research use audio or visual recording to collect the data? | No audio or visual recording was used |
| Field notes | Were field notes made during and/or after the interview or focus group? | No field notes were made, analyzed data were based upon patient responses |
| Duration | What was the duration of the interviews and focus groups? | Survey completion took about 5–10 minutes; however, this was not timed |
| Data saturation | Was data saturation discussed? | Data saturation was discussed during the analysis period (page 5) |
| Transcripts returned | Were transcripts returned to participants for comment and/or correction? | Researchers did not use transcripts. Surveys were not returned to patients |
| Domain 3: Analysis and Findings | ||
| Data analysis | ||
| Number of data coders | How many data coders coded the data? | Two researchers coded the data (L.M.S. and R.N.K.) (page 7) |
| Description of the coding tree | Did authors provide a description of the coding tree? | A codebook was developed but was not provided (page 7) |
| Derivation of themes | Were themes identified in advance or derived from data? | Themes were identified from the data not in advance |
| Software | What software, if applicable, was used to manage the data? | Web-based and HIPAA (Health Insurance Portability and Accountability Act)–compliant RedCap (Research Electronic Data Capture) was used to store data. Microsoft Excel was used to organize and code data |
| Participant checking | Did participants provide feedback on the findings? | Participants did not provide feedback |
| Reporting | ||
| Quotations presented | Were participant quotations presented to illustrate the themes/findings? Was each quotation identified? eg, participant number | Participant quotations were presented to illustrate themes, findings. Fig. 1. These quotations were kept anonymous |
| Data and findings consistent | Was there consistency between data presented and the findings? | Yes, there was consistency between presented data and our findings |
| Clarity of major themes | Were major themes clearly presented in the findings? | Major themes are clearly presented—Fig. 1 (page 8) |
| Clarity of minor themes | Is there a description of diverse cases or discussion of minor themes? | The researchers did not analyze minor themes |
REFERENCES
- 1.Centers for Medicare & Medicaid Services, U.S. Department of Health and Human Services. Medicare program; comprehensive care for joint replacement payment model for acute care hospitals furnishing lower extremity joint replacement services. 2015. Available at: https://www.federalregister.gov/documents/2015/11/24/2015-29438/medicare-program-comprehensive-care-for-joint-replacement-payment-model-for-acute-care-hospitals. Accessed April 5, 2018.
- 2.Massachusetts Medical Society. Patient-reported outcome measures: current state and MMS principles. 2019. Available at: http://www.massmed.org/proms/. Accessed May 4, 2019.
- 3.Blue Shield of California. Knee arthroplasty for adults. 2016. Available at: https://www.blueshieldca.com/bsca/bsc/public/common/PortalComponents/provider/StreamDocumentServlet?fileName=PRV_KneeArthroplasty_Adult.pdf. Accessed May 4, 2019.
- 4.Kamal RN, Lindsay SE, Eppler SL. Patients should define value in health care: a conceptual framework. J Hand Surg Am. 2018;43(11): 1030–1034. [DOI] [PubMed] [Google Scholar]
- 5.Wright HH, O’Brien V, Valdes K, et al. Relationship of the patient-specific functional scale to commonly used clinical measures in hand osteoarthritis. J Hand Ther. 2017;30(4):538–545. [DOI] [PubMed] [Google Scholar]
- 6.Morel T, Cano SJ. Measuring what matters to rare disease patients—reflections on the work by the IRDiRC taskforce on patient-centered outcome measures. Orphanet J Rare Dis. 2017;12(1):171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.International Rare Diseases Research Consortium. Patient-centered outcome measures. Available at: http://www.irdirc.org/activities/task-forces/patient-centered-outcome-measures/. Accessed May 4, 2019.
- 8.Øvretveit J, Zubkoff L, Nelson EC, Frampton S, Knudsen JL, Zimlichman E. Using patient-reported outcome measurement to improve patient care. Int J Qual Health Care. 2017;29(6):874–879. [DOI] [PubMed] [Google Scholar]
- 9.Hefford C, Abbott JH, Arnold R, Baxter GD. The patient-specific functional scale: validity, reliability, and responsiveness in patients with upper extremity musculoskeletal problems. J Orthop Sports Phys Ther. 2012;42(2):56–65. [DOI] [PubMed] [Google Scholar]
- 10.Stratford P, Gill C, Westaway M, Binkley J. Assessing disability and change on individual patients: a care report of a patient specific measure. Physiother Can. 1995;47(4):258–263. [Google Scholar]
- 11.Eppler SL, Kakar S, Sheikholeslami N, Sun B, Pennell H, Kamal RN. Defining quality in hand surgery from the patient’s perspective: a qualitative analysis. J Hand Surg Am. 2019;44(4):311–320.e4. [DOI] [PubMed] [Google Scholar]
- 12.McMillan CR, Binhammer PA. Which outcome measure is the best? Evaluating responsiveness of the Disabilities of the Arm, Shoulder, and Hand Questionnaire, the Michigan Hand Questionnaire and the Patient-Specific Functional Scale following hand and wrist surgery. Hand (N Y). 2009;4(3):311–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Novak CB, Williams MM, Conaty K. Evaluation of the Patient-Specific Functional Scale in hand fractures and dislocations. Hand (N Y). 2015;10(1):85–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saunders B, Sim J, Kingstone T, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893–1907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mason M. Sample size and saturation in PhD studies using qualitative interviews. Forum Qual Soc Res. 2010;11(3):Article 8. Available from: http://www.qualitative-research.net/index.php/fqs/article/view/1428/3028. Accessed April 25, 2019. [Google Scholar]
- 16.Ayton DR, Barker AL, Peeters GMEE, et al. Exploring patient-reported outcomes following percutaneous coronary intervention: a qualitative study. Health Expect. 2018;21(2):457–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Elliott IS, Sonshine DB, Akhavan S, et al. What factors influence the production of orthopaedic research in East Africa? A qualitative analysis of interviews. Clin Orthop Relat Res. 2015;473(6): 2120–2130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med. 1996;29(6):602–608. [DOI] [PubMed] [Google Scholar]
- 19.Beaton DE, Wright JG, Katz JN. Upper Extremity Collaborative Group. Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg Am. 2005;87(5):1038–1046. [DOI] [PubMed] [Google Scholar]
- 20.Patel S, Hee SW, Mistry D, et al. Chapter 5: Crosswalking between disability questionnaire scores. In: Patel S, Hee SW, Mistry D, et al. , eds. Identifying Back Pain Subgroups: Developing and Applying Approaches Using Individual Patient Data Collected Within Clinical Trials. Southampton, UK: NIHR Journals Library; 2016. [PubMed] [Google Scholar]
- 21.Evans JP, Porter I, Gangannagaripalli JB, et al. Assessing patient-centred outcomes in lateral elbow tendinopathy: a systematic review and standardised comparison of English language clinical rating systems. Sports Med Open. 2019;5(1):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Impellizzeri FM, Mannion AF, Leunig M, Bizzini M, Naal FD. Comparison of the reliability, responsiveness, and construct validity of 4 different questionnaires for evaluating outcomes after total knee arthroplasty. J Arthroplasty. 2011;26(6):861–869. [DOI] [PubMed] [Google Scholar]
- 23.Giesinger K, Hamilton DF, Jost B, Holzner B, Giesinger JM. Comparative responsiveness of outcome measures for total knee arthroplasty. Osteoarthr Cartil. 2014;22(2):184–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sorensen AA, Howard D, Tan WH, Ketchersid J, Calfee RP. Minimal clinically important differences of 3 patient-rated outcomes instruments. J Hand Surg Am. 2013;38(4):641–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chatman AB, Hyams SP, Neel JM, et al. The Patient-Specific Functional Scale: measurement properties in patients with knee dysfunction. Phys Ther. 1997;77(8):820–829. [DOI] [PubMed] [Google Scholar]
- 26.Cleland JA, Fritz JM, Whitman JM, Palmer JA. The reliability and construct validity of the Neck Disability Index and patient specific functional scale in patients with cervical radiculopathy. Spine (Phila Pa 1976). 2006;31(5):598–602. [DOI] [PubMed] [Google Scholar]
- 27.Maughan EF, Lewis JS. Outcome measures in chronic low back pain. Eur Spine J. 2010;19(9):1484–1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Polson K, Reid D, McNair PJ, Larmer P. Responsiveness, minimal importance difference and minimal detectable change scores of the shortened disability arm shoulder hand (QuickDASH) questionnaire. Man Ther. 2010;15(4):404–407. [DOI] [PubMed] [Google Scholar]
- 29.Mintken PE, Glynn P, Cleland JA. Psychometric properties of the shortened disabilities of the Arm, Shoulder, and Hand Questionnaire (QuickDASH) and Numeric Pain Rating Scale in patients with shoulder pain. J Shoulder Elbow Surg. 2009;18(6):920–926. [DOI] [PubMed] [Google Scholar]
- 30.Kazmers NH, Qiu Y, Yoo M, Stephens AR, Tyser AR, Zhang Y. The Minimal Clinically Important Difference of the PROMIS and QuickDASH Instruments in a nonshoulder hand and upper extremity patient population. J Hand Surg Am. 2020;45(5):399–407.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Horn KK, Jennings S, Richardson G, Vliet DV, Hefford C, Abbott JH. The patient-specific functional scale: psychometrics, clinimetrics, and application as a clinical outcome measure. J Orthop Sports Phys Ther. 2012;42(1):30–42. [DOI] [PubMed] [Google Scholar]
- 32.Bengtsson M. How to plan and perform a qualitative study using content analysis. Nursing Plus Open. 2016;2:8–14. [Google Scholar]
- 33.López A, Detz A, Ratanawongsa N, Sarkar U. What patients say about their doctors online: a qualitative content analysis. J Gen Intern Med. 2012;27(6):685–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jenssen BP, Klein JD, Salazar LF, Daluga NA, DiClemente RJ. Exposure to tobacco on the internet: content analysis of adolescents’ internet use. Pediatrics. 2009;124(2):e180–e186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. [DOI] [PubMed] [Google Scholar]
- 36.Loft MI, Esbensen BA, Kirk K, et al. Nursing staffs self-perceived outcome from a rehabilitation 24/7 educational programme—a mixed-methods study in stroke care. BMC Nurs. 2018;17:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Creswell JW. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. 4th ed. Thousand Oaks, CA: SAGE Publications; 2014. [Google Scholar]
- 38.Creswell JW. A Concise Introduction to Mixed Methods Research. 1st ed. Thousand Oaks, CA: SAGE Publications; 2015. [Google Scholar]
- 39.Snyder CF, Aaronson NK. Use of patient-reported outcomes in clinical practice. Lancet. 2009;374(9687):369–370. [DOI] [PubMed] [Google Scholar]
- 40.Greenhalgh J. The applications of PROs in clinical practice: what are they, do they work, and why? Qual Life Res. 2009;18(1): 115–123. [DOI] [PubMed] [Google Scholar]
- 41.Feldman-Stewart D, Brundage MD. A conceptual framework for patient-provider communication: a tool in the PRO research tool box. Qual Life Res. 2009;18(1):109–114. [DOI] [PubMed] [Google Scholar]
- 42.Rosengren J, Brodin N. Validity and reliability of the Swedish version of the Patient Specific Functional Scale in patients treated surgically for carpometacarpal joint osteoarthritis. J Hand Ther. 2013;26(1):53–60. [DOI] [PubMed] [Google Scholar]
- 43.McKenna SP. Measuring patient-reported outcomes: moving beyond misplaced common sense to hard science. BMC Med. 2011;9:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cooper SR, Gonthier C, Barch DM, Braver TS. The role of psychometrics in individual differences research in cognition: a case study of the AX-CPT. Front Psychol. 2017;8:1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wright A, Hannon J, Hegedus EJ, Kavchak AE. Clinimetrics corner: a closer look at the minimal clinically important difference (MCID). J Man Manip Ther. 2012;20(3):160–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Franchignoni F, Vercelli S, Giordano A, Sartorio F, Bravini E, Ferriero G. Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (QuickDASH). J Orthop Sports Phys Ther. 2014;44(1):30–39. [DOI] [PubMed] [Google Scholar]


