Abstract
Somatostatin (SST) is a well-known neuropeptide that is expressed throughout the brain. In the cortex, SST is expressed in a subset of GABAergic neurons and is known as a protein marker of inhibitory interneurons. Recent studies have identified the key functions of SST in modulating cortical circuits in the brain and cognitive function. Furthermore, reduced expression of SST is a hallmark of various neurological disorders, including Alzheimer’s disease and depression. In this review, we summarize the current knowledge on SST expression and function in the brain. In particular, we describe the physiological roles of SST-positive interneurons in the cortex. We further describe the causal relationship between pathophysiological changes in SST function and various neurological disorders, such as Alzheimer’s disease. Finally, we discuss potential treatments and possibility of novel drug developments for neurological disorders based on the current knowledge on the function of SST and SST analogs in the brain derived from experimental and clinical studies.
Subject terms: Molecular neuroscience, Drug development
Neuropeptide: Nerve cell protein may provide treatment options
Developing stable analogues of a key neuronal protein and finding ways to deliver them directly to the brain may provide novel treatments for neurological disorders. The neuropeptide somatostatin (SST) is involved in regulating circuits in the brain cortex and maintaining cognitive function. Reduced SST expression is a recognised feature of brain disorders including Alzheimer’s disease. Seung-Hee Lee and co-workers at the Korea Advanced Institute of Science and Technology, Daejeon, South Korea, reviewed the role of SST and examined its therapeutic potential. SST deficiency appears to cause the significant memory loss found in Alzheimer’s, and there has been some success trialling intravenous injection of SST in patient trials. However, SST is short-lived in the body, limiting its usefulness as a treatment. Stable SST analogues and safe delivery methods could broaden treatment options for multiple brain conditions.
Introduction
In the mammalian cerebral cortex, excitatory and inhibitory neurons (INs) are intermingled and balance network activity to allow processing of cognitive information. INs, which constitute 20–30% of neurons in the cortex, exert local GABAergic inhibition to regulate the firing activity of cortical neurons1 and balance network activity2. The precise morphological, electrophysiological, and neurochemical characteristics of INs have been determined, and distinct types of INs have been identified3. Specifically, INs can be classified into three nonoverlapping subgroups on the basis of neurochemical properties: parvalbumin- (PV+), somatostatin- (SST+), and 5-HT3A receptor-expressing (5HT3AR+) INs4. PV+ and SST+ INs are the two major subgroups of INs in the cortex, comprising ~80% of all GABAergic interneurons. Interestingly, PV+ INs are known to exert perisomatic inhibition, while SST+ INs exert dendritic inhibition. Dendritic computation of synaptic inputs is crucial for integration of thousands of synaptic inputs from other neurons5. Thus, dendritic inhibition by SST+ INs in the cortex is particularly interesting. Previous studies have revealed that SST+ INs receive long-range inputs6, exert local inhibition to balance excitatory synaptic inputs, and modulate cortical processing7. Furthermore, SST+ INs express the neuropeptide SST along with GABA, and these two neurotransmitters can be coreleased upon activation.
In addition to these neurochemical differences, SST+ INs show unique electrophysiological properties compared to other types of neurons. On average, the spike width of SST+ INs is broader than that of PV+ INs but narrower than that of excitatory neurons8. Moreover, while PV+ INs show fast-spiking activity and pyramidal neurons (PNs) show regular-spiking activity, there are heterogeneous populations of SST+ INs that exhibit diverse discharge patterns. They show distinct spiking responses according to the cortical layer in which they reside. The majority of SST+ INs located in the infragranular cortical layers show low-threshold spiking (LTS) because of the long calcium-mediated plateau4. LTS cells show after hyperpolarizations, exhibiting a triphasic waveform composed of early and late peaks. On the other hand, supragranular SST+ INs show regular-spiking activity with frequency adaptation. These cells are referred to as regular-spiking nonpyramidal (RSNP) cells9,10. In addition to the subtypes of SST+ INs mentioned above (LTS and RSNP cells), smaller but diverse subsets of SST+ INs that exhibit nonaccommodating firing patterns analogous to the fast-spiking activity of PV+ INs11, burst irregular spiking, or stuttering responses also exist10,11. The diverse physiological properties of SST+ IN subtypes supposedly indicate their various functions in the cortex.
However, it is still unclear whether all subtypes of SST+ INs play different roles in modulating cortical processing by releasing the neuropeptide SST. The following questions remain: which subtypes of SST+ INs release SST (a subset of or the entire population of SST+ INs) and when is SST released in cortical circuits. Although future studies are needed to answer these questions, we summarized the current knowledge on the specific function of the neuropeptide SST in modulating cortical processing in this review. This knowledge can be linked to the understanding of the physiological role of SST+ INs in the cortex and may be applied to develop drugs that can mimic the function of SST.
Functional roles of SST+ INs in the cortex
SST+ INs are involved in cortical processing in multiple ways. First, SST+ INs modulate excitatory inputs to the sensory cortex during sensory processing. When bottom-up sensory inputs arrive in layer 4 of the sensory cortex via the thalamus, the higher-order cortex gives feedback to distal dendrites of neurons in the superficial layers. Bottom-up (from the thalamus) and top-down (from the higher cortex) inputs to the sensory cortex can be modulated by neighboring SST+ INs, as SST+ INs predominantly innervate the distal dendrites of PNs and exert feedback or feed-forward inhibition of PN activity12. Such inhibition by SST+ INs results in surround suppression of sensory cortical neurons13, top-down modulation of visual processing in the primary visual cortex (VISp) through increased visual gain14, and shaping of auditory processing in the auditory cortex15. In addition, SST+ INs in layer 4 contribute to the disinhibition of PNs by inhibiting PV+ INs that exert perisomatic inhibition of PNs in the sensory cortex16. Therefore, SST+ INs do not simply suppress sensory information but gate the flow of information through PNs. SST+ INs also play a pivotal role in the generation of cortical slow waves17, which is the hallmark of nonrapid eye movement (NREM) sleep. Upon the activation of the SST+ INs, there appears to be an increase in slow-wave activity and NREM sleep duration. This finding suggests the existence of a causal link between the activity of SST+ INs and the generation of slow waves during NREM sleep.
Moreover, SST+ INs are known to be involved in synaptic plasticity. Their activity can be modulated by the repetition of sensory stimuli or by learning. When animals were continuously exposed to a specific stimulus, the neuronal activity of SST+ INs increased, while that of excitatory neurons in layer 2/3 decreased18. Conversely, inhibiting SST+ INs led to an increase in the activity of layer 2/3 PNs, even after habituation to a specific stimulus. Furthermore, SST+ INs play important roles in maintaining temporally the sequential activity of PNs in layer 2/3 of the mouse primary motor cortex during motor training. Activation of SST+ INs disrupted the learning-induced temporal shift in sequential activity of PNs and behavioral improvement19. Therefore, SST+ INs undergo synaptic plasticity during learning and contribute to maintaining the neural activity that represents learned information. Finally, SST+ INs are also known to play an important role in maintaining spatial working memory by selective modulation of nearby PNs20. Optogenetic activation of dmPFC SST+ INs impaired the behavioral performance of mice in memory-guided tasks21.
Functional roles of the neuropeptide SST and its receptors
The neuropeptide SST was first isolated from sheep hypothalamic extracts in 1973 and named SRIH (somatotropin-release inhibiting hormone). There are two types of biologically active SST isoforms that vary in constituent amino acids: SST-14 and SST-28. Generally, SST-14 is more predominant in the central nervous system (CNS), whereas SST-28 is more abundant in peripheral body organs22. SSTs have been found not only in the nervous system but also in various organs, such as the pancreas, gut, and immune cells. When secreted from these organs, SSTs travel throughout the body via the circulatory system. There are a total of five SST receptor (SSTR) subtypes (SSTR1–5), which are expressed in various parts of the body with distinct distribution patterns (Fig. 1). All SSTRs are G-protein-coupled receptors (GPCRs) with seven transmembrane domains and have nanomolar affinity for both SST-14 and SST-28 (ref. 23).
Fig. 1. Overview of the properties of SSTR family members: expression localization, binding affinity for SST and its analogs, and associations with neurological disorders.
Various subtypes of SSTRs are distributed differently across the central nervous system and the peripheral nervous system23. Gray shades indicate the existence of the receptor subtypes in the corresponding area. Red shades indicate receptor subtypes with a strong binding affinity (IC50 < 10 nM). Note that SST shows a high binding affinity for all SSTR subtypes. CST resembles SST and has a similar strong binding affinity for all SSTR subtypes. SST analogs have selective binding properties for certain subtypes of SSTRs and sometimes have higher affinity for SSTRs than SST. Alterations in SSTR expression levels are observed in the neurological disorders discussed in this paper. It is well known that the expression levels of SSTRs are altered in AD patients42, whereas the SSTR expression level in other disorders is less clear.
While SSTR5 has a higher binding affinity for SST-28 than SST-14, other SSTRs show a weaker affinity for SST-28 than SST-14 (ref. 23) (Fig. 1). Binding of SST to SSTRs suppresses the activity of target cells via activation of a G-protein signaling pathway that inhibits exocytosis by reducing the enzymatic activity of adenylate cyclase and the production of cAMPs. One well-known example is the inhibition of the release of pituitary growth hormone (somatotropin) via the activation of SSTRs (SSTR2 and SSTR5) by SST. In addition, induction of insulin secretion (SSTR5), proliferation inhibition (SSTR3), glucagon secretion (SSTR2), and immune responses (SSTR2) can be achieved by the selective binding of SST to particular SSTRs24,25.
Several studies have also contributed to revealing the role of the SST and the SSTRs in cortical processing. It has been shown that in rodents, SSTR blockers can impair perceptual task performance. In mice, administration of an SSTR2 agonist to the main olfactory bulb enhanced olfactory discrimination26. In addition, a recent study showed that SST enhanced visual processing in the VISp27. This study demonstrated that SST reduced excitatory inputs to the PV+ INs and improved visual gain in regular-spiking PNs. Serial block-face scanning electron microscopy (SBEM) data confirmed the presence of microcircuits that can mediate the SST-induced suppression of excitatory synaptic transmission to the proximal dendrites of PV+ INs27. Collectively, SST peptides released from SST+ neurons play a critical role in modulating cortical processing of task-relevant sensory information. In a previous study, researchers further examined the expression of various SSTR subtypes in different cell types in the VISp using single-cell RNA sequencing data shared by the Allen Brain Institute28. They quantified the mRNA level of SSTR expressed in VISp and anterolateral motor cortex (ALM) neurons (Fig. 2). Consistent with a previous report27, SSTR1 was mainly expressed in SST+ INs, suggesting that SSTR1 may function as an autoreceptor that can suppress SST+ INs. Interestingly, SSTR2 was found to be the most abundantly expressed subtype in the cortex. It was shown to be highly expressed in deep layer excitatory neurons and INs originating from the caudal ganglionic eminence29. The same patterns were observed in the VISp and ALM, and these data suggest that the expression patterns of SSTRs are similar across the cortex.
Fig. 2. The expression of five types of SSTRs and SST family genes in excitatory and inhibitory neurons in the VISp and ALM.
a Mean gene expression (RPKM: reads per kilobase of transcript per million mapped reads) of SSTR1–5, CST, and SST in excitatory neurons (left column) and inhibitory neurons (right column) in the VISp. The data are from mouse single-cell RNA sequencing data from the Allen Brain Atlas (total 15,413 cells; version 2018)28. The bars represent the mean ± SEM. Genetic markers of the cortical layers were selected based on previous literature99. Rasgrf2 Ras protein-specific guanine nucleotide releasing factor 2, Calb1 calbindin1, Rorb RAR-related orphan receptor B, Scnn1α sodium channel epithelial 1 subunit alpha, Rbp4 retinol-binding protein 4, Trib2 Tribbles pseudokinase 2, Ctgf connective tissue growth factor, Pvalb parvalbumin, Sst somatostatin, Vip vasoactive intestinal peptide, GAD glutamate decarboxylase. b Same as a, but for the ALM (total 10,068 cells). Cux2 was used as a genetic marker of layer 2/3 excitatory neurons instead of Calb1. Cux2 Cut-like homeobox 2.
Release of SST from the neurons
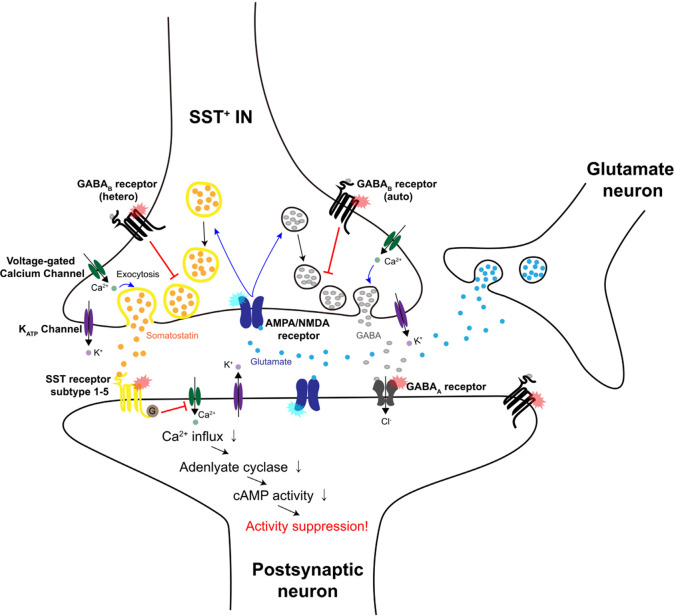
It has been reported that neurons can release SST in a calcium-dependent manner30, even in the absence of exogenous stimuli such as sensory information31. Other studies have shown that membrane depolarization32, glutamate33, or NMDA application34 can stimulate SST release via activation of NMDA and AMPA receptors (Fig. 3). Along with in vitro experiments, several attempts to dissect the mechanism of SST release in vivo have led to the identification of factors that can modulate SST release. Striatal SST+ INs can corelease glutamate and GABA, generating excitation–inhibition sequences in postsynaptic neurons, as the glutamatergic response persists for a shorter period than the inhibitory response35. The corelease of GABA and glutamate from striatal SST+ INs is evoked by glutamate-induced activation of ionotropic AMPA/NMDA receptors that are expressed in axon terminals. Cotransmission of these two neurotransmitters is induced in the striatum but not in the cortex or the hippocampus. Cortical SST+ INs are known to corelease GABA and SST onto postsynaptic neurons upon activation36,37. Interestingly, GABA release from SST+ INs inhibits the release of GABA as well as the spontaneous release of SST31. This autoregulation is induced by GABAB receptors, which are expressed on the axon terminals of SST+ INs38 (Fig. 3). SST+ INs also express SSTR1 in the cortex (Fig. 2), and binding of SST to SSTR1 can modulate the further release of SST or GABA from SST+ INs. Future studies are required to understand the exact molecular mechanisms of the corelease of GABA and SST and how SST release modulates the excitability of postsynaptic neurons in vivo.
Fig. 3. Schematic illustration of SST release in the presynaptic terminal of an SST+ IN.
In SST-expressing neurons, SST and GABA are known to be colocalized and coreleased. SST (yellow dots) and GABA (gray dots)-containing vesicles are first delivered to the presynaptic terminal and released in a calcium-dependent manner through exocytosis. It has been reported that more time and higher calcium levels are needed to release SST from SST+ neurons with higher activity than GABA, as SST is usually delivered in dense-core vesicles (yellow circles). Furthermore, glutamate (blue dots) released from nearby glutamatergic neurons can evoke the release of SST and GABA by activating AMPA/NMDA receptors on axon terminals. Released GABA can inhibit GABA release and SST release through activation of GABAB autoreceptors and heteroreceptors, respectively. Released SST can bind to SSTR subtypes 1–5 expressed on postsynaptic neurons and then inhibit calcium influx. This eventually leads to the reduced excitability of postsynaptic neurons through a downstream signaling pathway.
Decrease in SST expression in various neurological disorders
It has been reported that neurodegenerative and neuropsychiatric disorders such as Alzheimer’s disease (AD), Parkinson’s disease (PD), Huntington’s disease (HD), major depressive disorder (MDD), bipolar disorder, and schizophrenia (SCZ) are linked to a decrease in the expression of SST (Fig. 4). Here, we summarize these findings and describe the relationship between SST expression in the brain and neurological disorders.
Fig. 4. Decrease in SST expression in the brain in the context of various neurological disorders.
In the normal human brain (left), SST is highly expressed throughout the brain and in the cerebrospinal fluid. The most abundant SST isoform in the brain is SST-14, which contains 14 amino acids with a disulfide bond between cysteine residues. In the context of various neurological disorders (right), alterations in SST expression in a specific region or throughout the brain are observed. A decrease in SST expression might lead to a shrinkage of the brain and an imbalance in neural networks and function. The following disorders showing such pathologies are discussed in the text: Alzheimer’s disease, Parkinson’s disease, Huntington’s disease, major depressive disorder, and schizophrenia. Three approaches can be used to deliver functional neuropeptide SST to the brain for the treatment of these disorders: chemical modification to enhance BBB penetration, nanoformulations, and gene therapy techniques.
Alzheimer’s disease
It has been repeatedly reported that SST expression is reduced in AD patients and mouse models, both in the brain and the cerebrospinal fluid (CSF)39. In AD patients, total SST expression levels and the number of neurons expressing SST in the frontal cortex and hippocampus were decreased to less than 30% of those in control subjects39. In the hippocampus, the loss of SST+ neurons and the reduction in SST mRNA expression occurred earlier than the alteration in the expression of other GABAergic, glutamatergic, and cholinergic markers or the number of principal neurons40. Although the number of cortical and hippocampal SST+ INs was markedly reduced in AD41, the changes in the expression of different SSTR subtypes were not consistent42. In the AD cortex, the expression of SSTR4 and SSTR5 was significantly reduced, SSTR2 immunoreactivity showed a modest decrease, and SSTR1 seemed unaffected. Conversely, the expression of SSTR3 was increased in the frontal cortices of AD patients42. Therefore, the reduction in SST expression in the AD brain is more consistent than that in SSTR expression. It has been shown that an increase in the level of Aβ peptide is linearly correlated with SST deficiency43, indicating that a decrease in the expression of SST is likely involved in amyloid accumulation in the context of AD pathogenesis. We will further discuss this phenomenon below (“Disruption in SST function causes AD pathogenesis”).
Parkinson’s disease
PD is caused by the loss of dopaminergic neurons in the substantia nigra pars compacta and the locus coeruleus, leading to dopamine depletion that causes the gradual onset and progression of motor and nonmotor symptoms44. The molecular pathological mechanisms that underlie PD are the accumulation of α-synuclein (αSyn) and the formation of Lewy bodies45. In PD, accumulation of αSyn occurs throughout the brain, including both cortical and subcortical areas as well as the central and peripheral (autonomic) nervous systems46. Interestingly, changes in SST expression and SSTRs in cortical regions (the frontal and entorhinal cortices and hippocampus) and the CSF have been demonstrated in PD47. A decrease in SST levels in these cortical areas can be the putative cause of cognitive impairments. One recent paper showed a decrease in the number of SST+ INs and SST mRNA levels in PARK2-specific iPSCs derived from PD patients48. A PARK2 mutation in SST+ INs may cause a decrease in SST transcripts and mitochondrial dysfunction, which might cause an excitatory/inhibitory (E/I) imbalance culminating in the motor and nonmotor symptoms observed in PD49.
Huntington’s disease
HD is a genetic disorder that is caused by the expansion of CAG trinucleotide repeats in exon 1 of the huntingtin (HTT) gene on chromosome 4 over a certain threshold (>39 repeats). The translation of this mutated gene results in the production of mutant HTT protein (mHTT), which has toxic effects and causes pathological changes in neurons, such as synaptic dysfunction and axonal transport impairment50. HD’s characteristic neuropathological feature is atrophy of the striatum, cerebral cortex, hippocampus, thalamus, hypothalamus, and cerebellum51. Massive degeneration and loss of spiny projection neurons in the striatum are observed, which might disrupt the relay of information from the cortex and the thalamus to the output structures of the basal ganglia52. A reduced number of PV+, SST+, and cholinergic INs in addition to spiny neurons, a reduction in dendritic arborization, and altered physiology are observed in HD mice53,54. In particular, SSTR1 and SSTR5 double knockout mice were found to exhibit neurochemical changes that mimic those observed in HD55. In addition, postmortem analysis of HD patients showed a reduction in the number of SST+ neurons in the nucleus tuberalis lateralis of the hypothalamus56.
Major depressive disorder
MDD is accompanied by persistent changes in various cognitive functions, such as attention, short-term and working memory57, and cognitive control58. In MDD, SST levels are decreased in the CSF, and the level of SST expression is restored to the normal level when patients recover from MDD59. Low levels of SST expression in the CSF were correlated with elevated levels of urinary cortisol in MDD patients, who also exhibited hypothalamic–pituitary–adrenal (HPA) dysfunction60. However, it is unclear whether a decrease in SST expression causes MDD pathophysiology. A tendency for SST expression to be downregulated in the CSF and brain areas such as the ACC61 and amygdala62 was observed in human postmortem studies. Interestingly, females showed higher vulnerability to MDD development and a greater reduction in SST expression in the cortex and amygdala than males63,64. Future studies are required to understand the molecular function of SST in MDD pathology.
Schizophrenia
SCZ is a neuropsychiatric disorder characterized by positive (e.g., hallucinations and delusions), negative (e.g., blunted affect, apathy, and social avoidance), and cognitive (e.g., deficits in attention and executive function) symptoms. The most common cause of positive symptoms in SCZ is excessive subcortical dopamine release, considering that D2 receptor antagonists reduce positive symptoms and thus are used as antipsychotics65. Although no observable primary pathology has been identified in the dopamine system in SCZ patients, it has been postulated that upstream areas of the dopamine system are impaired in SCZ, such as the ventral hippocampus66. Indeed, hyperactivity of the ventral hippocampus has been observed in SCZ patients, and it has been suggested that this might be the result of a loss of INs, such as PV+ and SST+ INs67. Reduced expression of SST in SCZ patients was observed not only in the CSF68 but also in the hippocampus, thalamic reticular nucleus, and cortical areas67,69. Additionally, in a postmortem study of SCZ patients, neurochemical changes accompanied a reduction in SST levels in the lateral amygdala69. As shown in an SCZ mouse model with a mutation in the region corresponding to human chromosome 16p11.2 (16p11.2 duplication mice)70, disruption of hippocampal–orbitofrontal and hippocampal–amygdala functional connectivity in the SCZ correlates with a reduction in SST expression.
Disruption of SST function in AD pathogenesis
Considering that AD patients exhibit low SST expression in the cortex and hippocampus39, a causal link between SST function and AD pathogenesis has been postulated. The main symptom of AD is gradual but severe memory loss. Numerous studies have reported that memory loss in AD patients may have been derived from deficits in SST function. Electroconvulsive shock-induced amnesia in rodents performing an active avoidance task was reversed after intracerebroventricular injections of SST71. In AD patients, SST infusion into the brain and systemic SST administration improved cognitive defects. Craft et al.72 further showed that catheter-mediated intravenous (IV) administration of octreotide, which is an analog of SST and is known to activate SSTR2, SSTR3, and SSTR5, improved memory loss.
Interestingly, SST enhanced the enzyme activity of neprilysin, which promotes Aβ degradation and is downregulated with aging and in the early stage of AD progression73. In a study using amyloid precursor protein (APP) transgenic mice74, a well-known AD mouse model, amyloid plaque formation and embryonic lethality in mutant mice were fully reversed by overexpression of neprilysin. Furthermore, delivery of neprilysin to the presynaptic site using a recombinant adeno-associated viral vector blocked Aβ deposition in the hippocampi of APP-transgenic mice and neprilysin-deficient mice75. SST enhanced neprilysin expression in cultured murine neurons but decreased Aβ42 expression via binding to its receptors76. Similarly, blocking the function of SSTR by administering BIM23056 (an SSTR5 antagonist) or pertussis toxin (a GPCR blocker that inhibits adenylyl cyclases) reduced these effects. Moreover, in SST knockout (KO) mice, there was a 50% decrease in neprilysin activity and an increase in Aβ42 accumulation76. These findings demonstrate the correlation between the expression levels of SST, neprilysin, and Aβ42, which are important pathological hallmarks for diagnosing AD. However, in some of the AD mouse models, such as APPswe/PS1dE9 mice, the SST level was increased or remained constant despite the disruption in cognitive brain function and the occurrence of amyloid deposition77. Future studies are required to identify the direct causal relationships between SST and AD pathology.
Hyperphosphorylation of tau proteins is another key factor in AD pathogenesis. Tau proteins regulate the assembly and organization of microtubules. Phosphorylation of the tau protein weakens its affinity for microtubules and subsequently induces the depolymerization of microtubules78. Furthermore, there is increasing evidence that an increase in Aβ fibrils results in tau phosphorylation in cultured hippocampal and cortical neurons79. In AD pathogenesis, the phosphorylation, polymerization, and deposition of the tau protein are facilitated in affected brain areas80. Interestingly, SST treatment decreased the phosphorylation of tau at Ser262, a site that is known to be affected in the AD brain81. The phosphorylation of the tau protein at Ser262 via activation of SSTR2 and SSTR4 was observed in the cortex not in other brain areas.
SST analogs developed for therapeutic applications
SST exerts potent inhibitory effects on a wide range of endocrine and exocrine systems in the body. It is well known to inhibit the secretion of growth hormone to suppress body growth. Nevertheless, its ability to be readily degraded in its natural form, along with its short half-life (1–3 min), hinder its application as a drug for various diseases. Several SST analogs (SSAs) that show enhanced stability in the body have been developed. They share a similar structure and function with SST but show distinct receptor-binding properties (Fig. 1). One well-known natural analog of SST is cortistatin (CST), which has been identified as a natural neuropeptide expressed in the cortex that bears the same amino acid sequence in the receptor-binding site as SST. CST can bind to all subtypes of SSTRs with nanomolar affinity and has a functionally similar role as SST in that it also suppresses neural activity82. Due to the difference in tissue expression patterns and the detailed molecular structures, CST and SST exhibit different functions. For example, CST, but not SST, can enhance slow-wave activity82 and is able to consolidate short- and long-term memories83. These differences may be due to differences in molecular partners activated by CST and SST. Despite the different roles of CST, cortical injection of CST was shown to induce the same enhancement of perceptual behaviors in mice as SST27. Future studies are required to compare and understand the roles of SST and CST in the cortex in vivo.
In addition to CST, five synthetic SSAs have been further developed for the treatment of disorders: SMS 201–995 (octreotide), BIM 23014 (lanreotide), RC-160 (vapreotide), MK 678 (seglitide), and SOM 230 (pasireotide). Three of these SSAs (octreotide, lanreotide, and pasireotide) were approved by the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) for the clinical treatment of disorders characterized by excessive release of growth hormone. Octreotide acetate and lanreotide are first-generation SSAs, and have a longer half-life (2–600 h) than SST84,85. Octreotide is an octapeptide that evokes similar effects as SST but exerts more variable, prolonged, and selective inhibitory effects on target tissues. Octreotide and lanreotide specifically show strong binding affinity for SSTR2 and SSTR5. On the other hand, pasireotide is a second-generation SSA that is also known as Signifor. The first version of this orphan drug, Signifor® (Novartis, Geneva), has a 9.6- to 12.6-h half-life. The improved version, Signifor® LAR (Novartis, Geneva), has a much longer half-life (375–443 h)86. This analog has a higher binding affinity for SSTR1, SSTR3, and SSTR5 than octreotide but a similar affinity for SSTR2 (ref. 86) (Fig. 1).
Some SSAs have a receptor-activating motif (Phe–Trp–Lys–Thr) as well as another motif that can strongly suppress hormonal secretion. These modifications are useful for treating hyperhormonal diseases, including neuroendocrine tumors and acromegaly87,88. For example, pasireotide is used to treat acromegaly patients who do not respond to first-generation SSAs89. SSAs are also applied to treat various diseases, such as pituitary adenomas and gastroenteropancreatic neuroendocrine tumors. For example, SSAs, as inhibitors of adrenocorticotropic hormone secretion, can be used to treat Cushing’s disease, a form of pituitary adenoma89.
Recently, the development of SSA drugs has focused on chemical formulations for oral delivery. The SSAs approved thus far must be administered by injected subcutaneous or intramuscular injection, which are accompanied by discomfort and pain, leading some patients to delay or skip treatments. Two important issues that must be taken into account when designing oral formulations of SSAs are their stability in the presence of gastrointestinal (GI) peptidases and their ability to pass through the intestine to reach the blood vessels. Since most existing SSAs are stable in the presence of GI enzymes, the key issue is their poor ability to pass through the epithelium (<0.3%) of the small intestine90. As several attempts to enhance the ability of orally administered drugs to pass through the intestine have been made91, future application of these techniques may be useful for developing SSA drugs for oral delivery.
Development of SST-related drugs for the treatment of brain disorders in the future
Although SSAs have been used for hormone regulation in the body, there are still no SSA drugs that are approved for the treatment of brain disorders. The first hurdle for the application of SSAs for the treatment of brain disorders is the poor ability of SSAs to enter the brain. The use of iodinated Tyr-SST administered via carotid artery injection92 and octapeptide analogs of SST administered via IV injection93 is hindered by the limited ability of these drugs to penetrate the brain. Indeed, the greatest challenge to the development of drugs for neurological disorders is the difficulty in delivering drugs across the blood–brain barrier (BBB) and the blood–CSF barrier to the brain94. Although the BBB is a tight barrier that prevents large substances from entering the brain, some viruses can easily penetrate the BBB by the biological mechanisms of receptor binding and tranport95. Thus, many researchers have used such mechanisms to develop drug delivery systems. The chemical motifs of drugs are modified to allow them to bind the surface receptors of endothelial cells and be transported into the brain96 (Fig. 4).
For the delivery of therapeutic drugs across the BBB, nanotechnology-based engineering approaches that introduce desired functions to packaged drugs using the unique physicochemical properties of biocompatible and biodegradable nanomaterials have also been considered97. Nanocarriers such as micelles, liposomes, polymeric nanoparticles, solid lipid nanoparticles, nanoemulsions, and dendrimers are currently being developed94. Several studies have investigated the systemic delivery of neuroprotective peptides loaded in nanoparticles and showed improved brain functions in rodent models98. Similarly, encapsulation of SSAs may be useful for developing SSA drugs that can improve brain functions. Since many neurological disorders linked to SST function are associated with a reduction in SST expression, direct delivery of SSAs as well as gene therapy techniques can be used to express genetically encoded SSAs in the brain more permanently (Fig. 4). Future studies are required to design gene delivery methods that can target specific neuronal and nonneuronal cells for long-term expression of SSAs in the brain.
Concluding remarks
In this paper, we summarized the pivotal functions of SST and its receptors in the brain, especially in cortical processing. We also described their relationships with various neurological disorders, including AD. We further discussed and suggested possible strategies for developing SSAs that can be used to treat neurological disorders. Regardless of the numerous attempts that have been made to deliver peptide drugs to the CNS, several barriers, such as chemical stability, receptor sensitivity, and BBB permeability, remain major challenges to developing more efficient SSA drugs. In future studies, chemical modification, encapsulation in biocompatible and biodegradable materials or nanovesicles, and delivery of SSA genes may be used to overcome these barriers and stably deliver SST-related drugs to the brain.
Acknowledgements
This work was supported by grants to S.-H.L. from the National Research Foundation of Korea funded by the Ministry of Science and ICT (2017R1A2B3008270, 2017M3C7A1030798, and 2018R1A4A1025616) and the KAIST (Global Singularity Program for 2020) and a grant to Y.-H.S. from the National Research Foundation of Korea funded by the Ministry of Science and ICT (2020R1I1A1A0107412511).
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: You-Hyang Song, Jiwon Yoon
References
- 1.Isaacson JS, Scanziani M. How inhibition shapes cortical activity. Neuron. 2011;72:231–243. doi: 10.1016/j.neuron.2011.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Okun M, Lampl I. Instantaneous correlation of excitation and inhibition during ongoing and sensory-evoked activities. Nat. Neurosci. 2008;11:535–537. doi: 10.1038/nn.2105. [DOI] [PubMed] [Google Scholar]
- 3.Petilla Interneuron Nomenclature G, et al. Petilla terminology: nomenclature of features of GABAergic interneurons of the cerebral cortex. Nat. Rev. Neurosci. 2008;9:557–568. doi: 10.1038/nrn2402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fishell G, Rudy B. Mechanisms of inhibition within the telencephalon: “where the wild things are”. Annu Rev. Neurosci. 2011;34:535–567. doi: 10.1146/annurev-neuro-061010-113717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.London M, Hausser M. Dendritic computation. Annu. Rev. Neurosci. 2005;28:503–532. doi: 10.1146/annurev.neuro.28.061604.135703. [DOI] [PubMed] [Google Scholar]
- 6.Wall NR, et al. Brain-wide maps of synaptic input to cortical interneurons. J. Neurosci. 2016;36:4000–4009. doi: 10.1523/JNEUROSCI.3967-15.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kvitsiani D, et al. Distinct behavioural and network correlates of two interneuron types in prefrontal cortex. Nature. 2013;498:363–366. doi: 10.1038/nature12176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ji XY, et al. Thalamocortical innervation pattern in mouse auditory and visual cortex: laminar and cell-type specificity. Cereb. Cortex. 2016;26:2612–2625. doi: 10.1093/cercor/bhv099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Riedemann, T. Diversity and function of somatostatin-expressing interneurons in the cerebral cortex. Int. J. Mol. Sci.10.3390/ijms20122952 (2019). [DOI] [PMC free article] [PubMed]
- 10.Riedemann T, Straub T, Sutor B. Two types of somatostatin-expressing GABAergic interneurons in the superficial layers of the mouse cingulate cortex. PLoS ONE. 2018;13:e0200567. doi: 10.1371/journal.pone.0200567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang Y, et al. Anatomical, physiological and molecular properties of Martinotti cells in the somatosensory cortex of the juvenile rat. J. Physiol. 2004;561:65–90. doi: 10.1113/jphysiol.2004.073353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Silberberg G, Markram H. Disynaptic inhibition between neocortical pyramidal cells mediated by Martinotti cells. Neuron. 2007;53:735–746. doi: 10.1016/j.neuron.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 13.Adesnik H, Bruns W, Taniguchi H, Huang ZJ, Scanziani M. A neural circuit for spatial summation in visual cortex. Nature. 2012;490:226–231. doi: 10.1038/nature11526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang S, et al. Selective attention. Long-range and local circuits for top-down modulation of visual cortex processing. Science. 2014;345:660–665. doi: 10.1126/science.1254126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li LY, et al. Differential receptive field properties of parvalbumin and somatostatin inhibitory neurons in mouse auditory cortex. Cereb. Cortex. 2015;25:1782–1791. doi: 10.1093/cercor/bht417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xu H, Jeong HY, Tremblay R, Rudy B. Neocortical somatostatin-expressing GABAergic interneurons disinhibit the thalamorecipient layer 4. Neuron. 2013;77:155–167. doi: 10.1016/j.neuron.2012.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Funk CM, et al. Role of somatostatin-positive cortical interneurons in the generation of sleep slow waves. J. Neurosci. 2017;37:9132–9148. doi: 10.1523/JNEUROSCI.1303-17.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kato HK, Gillet SN, Isaacson JS. Flexible sensory representations in auditory cortex driven by behavioral relevance. Neuron. 2015;88:1027–1039. doi: 10.1016/j.neuron.2015.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adler A, Zhao R, Shin ME, Yasuda R, Gan WB. Somatostatin-expressing interneurons enable and maintain learning-dependent sequential activation of pyramidal neurons. Neuron. 2019;102:202–216 e207. doi: 10.1016/j.neuron.2019.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim D, et al. Distinct roles of parvalbumin- and somatostatin-expressing interneurons in working memory. Neuron. 2016;92:902–915. doi: 10.1016/j.neuron.2016.09.023. [DOI] [PubMed] [Google Scholar]
- 21.Kamigaki T, Dan Y. Delay activity of specific prefrontal interneuron subtypes modulates memory-guided behavior. Nat. Neurosci. 2017;20:854–863. doi: 10.1038/nn.4554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Francis BH, Baskin DG, Saunders DR, Ensinck JW. Distribution of somatostatin-14 and somatostatin-28 gastrointestinal-pancreatic cells of rats and humans. Gastroenterology. 1990;99:1283–1291. doi: 10.1016/0016-5085(90)91151-u. [DOI] [PubMed] [Google Scholar]
- 23.Abdel-Rahman O, Lamarca A, Valle JW, Hubner RA. Somatostatin receptor expression in hepatocellular carcinoma: prognostic and therapeutic considerations. Endocr. Relat. Cancer. 2014;21:R485–R493. doi: 10.1530/ERC-14-0389. [DOI] [PubMed] [Google Scholar]
- 24.Patel YC. Somatostatin and its receptor family. Front. Neuroendocrinol. 1999;20:157–198. doi: 10.1006/frne.1999.0183. [DOI] [PubMed] [Google Scholar]
- 25.Weiss RE, Reddi AH, Nimni ME. Somatostatin can locally inhibit proliferation and differentiation of cartilage and bone precursor cells. Calcif. Tissue Int. 1981;33:425–430. doi: 10.1007/BF02409466. [DOI] [PubMed] [Google Scholar]
- 26.Lepousez G, Mouret A, Loudes C, Epelbaum J, Viollet C. Somatostatin contributes to in vivo gamma oscillation modulation and odor discrimination in the olfactory bulb. J. Neurosci. 2010;30:870–875. doi: 10.1523/JNEUROSCI.4958-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Song YH, et al. Somatostatin enhances visual processing and perception by suppressing excitatory inputs to parvalbumin-positive interneurons in V1. Sci. Adv. 2020;6:eaaz0517. doi: 10.1126/sciadv.aaz0517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tasic B, et al. Shared and distinct transcriptomic cell types across neocortical areas. Nature. 2018;563:72–78. doi: 10.1038/s41586-018-0654-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Miyoshi G, et al. Genetic fate mapping reveals that the caudal ganglionic eminence produces a large and diverse population of superficial cortical interneurons. J. Neurosci. 2010;30:1582–1594. doi: 10.1523/JNEUROSCI.4515-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tapia-Arancibia L, Pares-Herbute N, Astier H. Calcium dependence of somatostatin (SRIF) release and cyclic AMP levels in cultured diencephalic neurons. Neuroendocrinology. 1989;49:555–560. doi: 10.1159/000125167. [DOI] [PubMed] [Google Scholar]
- 31.Gamse R, et al. Release of immunoreactive somatostatin from hypothalamic cells in culture: inhibition by gamma-aminobutyric acid. Proc. Natl Acad. Sci. USA. 1980;77:5552–5556. doi: 10.1073/pnas.77.9.5552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tapia-Arancibia L, Astier H. Actions of excitatory amino acids on somatostatin release from cortical neurons in primary cultures. J. Neurochem. 1989;53:1134–1141. doi: 10.1111/j.1471-4159.1989.tb07406.x. [DOI] [PubMed] [Google Scholar]
- 33.Fontana G, De Bernardi R, Ferro F, Gemignani A, Raiteri M. Characterization of the glutamate receptors mediating release of somatostatin from cultured hippocampal neurons. J. Neurochem. 1996;66:161–168. doi: 10.1046/j.1471-4159.1996.66010161.x. [DOI] [PubMed] [Google Scholar]
- 34.Rage F, Rougeot C, Tapia-Arancibia L. GABAA and NMDA receptor activation controls somatostatin messenger RNA expression in primary cultures of hypothalamic neurons. Neuroendocrinology. 1994;60:470–476. doi: 10.1159/000126783. [DOI] [PubMed] [Google Scholar]
- 35.Cattaneo, S. et al. Somatostatin-expressing interneurons co-release GABA and glutamate onto different postsynaptic targets in the striatum. Preprint at https://www.biorxiv.org/content/10.1101/566984v1 (2019).
- 36.Liguz-Lecznar M, Urban-Ciecko J, Kossut M. Somatostatin and somatostatin-containing neurons in shaping neuronal activity and plasticity. Front. Neural Circuits. 2016;10:48. doi: 10.3389/fncir.2016.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baraban SC, Tallent MK. Interneuron diversity series: interneuronal neuropeptides–endogenous regulators of neuronal excitability. Trends Neurosci. 2004;27:135–142. doi: 10.1016/j.tins.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 38.Bonanno G, Carita F, Cavazzani P, Munari C, Raiteri M. Selective block of rat and human neocortex GABA(B) receptors regulating somatostatin release by a GABA(B) antagonist endowed with cognition enhancing activity. Neuropharmacology. 1999;38:1789–1795. doi: 10.1016/s0028-3908(99)00084-2. [DOI] [PubMed] [Google Scholar]
- 39.Davies P, Katzman R, Terry RD. Reduced somatostatin-like immunoreactivity in cerebral cortex from cases of Alzheimer disease and Alzheimer senile dementa. Nature. 1980;288:279–280. doi: 10.1038/288279a0. [DOI] [PubMed] [Google Scholar]
- 40.Ramos B, et al. Early neuropathology of somatostatin/NPY GABAergic cells in the hippocampus of a PS1 x APP transgenic model of Alzheimer’s disease. Neurobiol. Aging. 2006;27:1658–1672. doi: 10.1016/j.neurobiolaging.2005.09.022. [DOI] [PubMed] [Google Scholar]
- 41.Terry RD, Katzman R. Senile dementia of the Alzheimer type. Ann. Neurol. 1983;14:497–506. doi: 10.1002/ana.410140502. [DOI] [PubMed] [Google Scholar]
- 42.Kumar U. Expression of somatostatin receptor subtypes (SSTR1-5) in Alzheimer’s disease brain: an immunohistochemical analysis. Neuroscience. 2005;134:525–538. doi: 10.1016/j.neuroscience.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 43.Ramos B, et al. Early neuropathology of somatostatin/NPY GABAergic cells in the hippocampus of a PS1xAPP transgenic model of Alzheimer’s disease. Neurobiol. Aging. 2006;27:1658–1672. doi: 10.1016/j.neurobiolaging.2005.09.022. [DOI] [PubMed] [Google Scholar]
- 44.Fearnley JM, Lees AJ. Ageing and Parkinson’s disease: substantia nigra regional selectivity. Brain. 1991;114(Pt 5):2283–2301. doi: 10.1093/brain/114.5.2283. [DOI] [PubMed] [Google Scholar]
- 45.Wakabayashi K, et al. The Lewy body in Parkinson’s disease and related neurodegenerative disorders. Mol. Neurobiol. 2013;47:495–508. doi: 10.1007/s12035-012-8280-y. [DOI] [PubMed] [Google Scholar]
- 46.Braak H, Braak E. Pathoanatomy of Parkinson’s disease. J. Neurol. 2000;247:II3–II10. doi: 10.1007/PL00007758. [DOI] [PubMed] [Google Scholar]
- 47.Epelbaum J, et al. Somatostatin and dementia in Parkinson’s disease. Brain Res. 1983;278:376–379. doi: 10.1016/0006-8993(83)90277-9. [DOI] [PubMed] [Google Scholar]
- 48.Iwasawa C, et al. Reduced expression of somatostatin in GABAergic interneurons derived from induced pluripotent stem cells of patients with parkin mutations. Mol. Brain. 2019;12:5. doi: 10.1186/s13041-019-0426-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.McGregor MM, Nelson AB. Circuit mechanisms of Parkinson’s disease. Neuron. 2019;101:1042–1056. doi: 10.1016/j.neuron.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 50.Bates GP, et al. Huntington disease. Nat. Rev. Dis. Prim. 2015;1:15005. doi: 10.1038/nrdp.2015.5. [DOI] [PubMed] [Google Scholar]
- 51.Waldvogel HJ, Kim EH, Tippett LJ, Vonsattel JP, Faull RL. The neuropathology of Huntington’s disease. Curr. Top. Behav. Neurosci. 2015;22:33–80. doi: 10.1007/7854_2014_354. [DOI] [PubMed] [Google Scholar]
- 52.Bolam JP, Hanley JJ, Booth PA, Bevan MD. Synaptic organisation of the basal ganglia. J. Anat. 2000;196(Pt 4):527–542. doi: 10.1046/j.1469-7580.2000.19640527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Holley SM, Galvan L, Kamdjou T, Cepeda C, Levine MS. Striatal GABAergic interneuron dysfunction in the Q175 mouse model of Huntington’s disease. Eur. J. Neurosci. 2019;49:79–93. doi: 10.1111/ejn.14283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Holley, S. M. et al. Enhanced GABAergic inputs contribute to functional alterations of cholinergic interneurons in the R6/2 mouse model of Huntington’s disease. eNeuro10.1523/ENEURO.0008-14.2015 (2015). [DOI] [PMC free article] [PubMed]
- 55.Rajput PS, et al. Somatostatin receptor 1 and 5 double knockout mice mimic neurochemical changes of Huntington’s disease transgenic mice. PLoS ONE. 2011;6:e24467. doi: 10.1371/journal.pone.0024467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kremer HP, Roos RA, Dingjan G, Marani E, Bots GT. Atrophy of the hypothalamic lateral tuberal nucleus in Huntington’s disease. J. Neuropathol. Exp. Neurol. 1990;49:371–382. doi: 10.1097/00005072-199007000-00002. [DOI] [PubMed] [Google Scholar]
- 57.Murrough JW, Iacoviello B, Neumeister A, Charney DS, Iosifescu DV. Cognitive dysfunction in depression: neurocircuitry and new therapeutic strategies. Neurobiol. Learn Mem. 2011;96:553–563. doi: 10.1016/j.nlm.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 58.Disner SG, Beevers CG, Haigh EA, Beck AT. Neural mechanisms of the cognitive model of depression. Nat. Rev. Neurosci. 2011;12:467–477. doi: 10.1038/nrn3027. [DOI] [PubMed] [Google Scholar]
- 59.Rubinow DR, Gold PW, Post RM, Ballenger JC. CSF somatostatin in affective illness and normal volunteers. Prog. Neuropsychopharmacol. Biol. Psychiatry. 1985;9:393–400. doi: 10.1016/0278-5846(85)90192-7. [DOI] [PubMed] [Google Scholar]
- 60.Holsboer F. The corticosteroid receptor hypothesis of depression. Neuropsychopharmacology. 2000;23:477–501. doi: 10.1016/S0893-133X(00)00159-7. [DOI] [PubMed] [Google Scholar]
- 61.Seney ML, Tripp A, McCune S, Lewis DA, Sibille E. Laminar and cellular analyses of reduced somatostatin gene expression in the subgenual anterior cingulate cortex in major depression. Neurobiol. Dis. 2015;73:213–219. doi: 10.1016/j.nbd.2014.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Guilloux JP, et al. Molecular evidence for BDNF- and GABA-related dysfunctions in the amygdala of female subjects with major depression. Mol. Psychiatry. 2012;17:1130–1142. doi: 10.1038/mp.2011.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tripp A, Kota RS, Lewis DA, Sibille E. Reduced somatostatin in subgenual anterior cingulate cortex in major depression. Neurobiol. Dis. 2011;42:116–124. doi: 10.1016/j.nbd.2011.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Seney ML, et al. The role of genetic sex in affect regulation and expression of GABA-related genes across species. Front. Psychiatry. 2013;4:104. doi: 10.3389/fpsyt.2013.00104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Leucht S, et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet. 2013;382:951–962. doi: 10.1016/S0140-6736(13)60733-3. [DOI] [PubMed] [Google Scholar]
- 66.Lodge DJ, Grace AA. Hippocampal dysregulation of dopamine system function and the pathophysiology of schizophrenia. Trends Pharm. Sci. 2011;32:507–513. doi: 10.1016/j.tips.2011.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Konradi C, et al. Hippocampal interneurons are abnormal in schizophrenia. Schizophr. Res. 2011;131:165–173. doi: 10.1016/j.schres.2011.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Reinikainen KJ, Koponen H, Jolkkonen J, Riekkinen PJ. Decreased somatostatin-like immunoreactivity in the cerebrospinal fluid of chronic schizophrenic patients with cognitive impairment. Psychiatry Res. 1990;33:307–312. doi: 10.1016/0165-1781(90)90047-9. [DOI] [PubMed] [Google Scholar]
- 69.Hoftman GD, et al. Altered cortical expression of GABA-related genes in schizophrenia: illness progression vs developmental disturbance. Schizophr. Bull. 2015;41:180–191. doi: 10.1093/schbul/sbt178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bristow GC, et al. 16p11 duplication disrupts hippocampal-orbitofrontal-amygdala connectivity, revealing a neural circuit endophenotype for schizophrenia. Cell Rep. 2020;31:107536. doi: 10.1016/j.celrep.2020.107536. [DOI] [PubMed] [Google Scholar]
- 71.Vécsei L, Bollók I, Telegdy G. Intracerebroventricular somatostatin attenuates electroconvulsive shock-induced amnesia in rats. Peptides. 1983;4:293–295. doi: 10.1016/0196-9781(83)90135-3. [DOI] [PubMed] [Google Scholar]
- 72.Craft S, et al. Enhancement of memory in Alzheimer disease with insulin and somatostatin, but not glucose. Arch. Gen. Psychiatry. 1999;56:1135–1140. doi: 10.1001/archpsyc.56.12.1135. [DOI] [PubMed] [Google Scholar]
- 73.Iwata N, Takaki Y, Fukami S, Tsubuki S, Saido TC. Region-specific reduction of a beta-degrading endopeptidase, neprilysin, in mouse hippocampus upon aging. J. Neurosci. Res. 2002;70:493–500. doi: 10.1002/jnr.10390. [DOI] [PubMed] [Google Scholar]
- 74.Leissring MA, et al. Enhanced proteolysis of beta-amyloid in APP transgenic mice prevents plaque formation, secondary pathology, and premature death. Neuron. 2003;40:1087–1093. doi: 10.1016/s0896-6273(03)00787-6. [DOI] [PubMed] [Google Scholar]
- 75.Iwata N, et al. Presynaptic localization of neprilysin contributes to efficient clearance of amyloid-beta peptide in mouse brain. J. Neurosci. 2004;24:991–998. doi: 10.1523/JNEUROSCI.4792-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Saito T, et al. Somatostatin regulates brain amyloid beta peptide Abeta42 through modulation of proteolytic degradation. Nat. Med. 2005;11:434–439. doi: 10.1038/nm1206. [DOI] [PubMed] [Google Scholar]
- 77.Savonenko A, et al. Episodic-like memory deficits in the APPswe/PS1dE9 mouse model of Alzheimer’s disease: relationships to beta-amyloid deposition and neurotransmitter abnormalities. Neurobiol. Dis. 2005;18:602–617. doi: 10.1016/j.nbd.2004.10.022. [DOI] [PubMed] [Google Scholar]
- 78.Drechsel DN, Hyman AA, Cobb MH, Kirschner MW. Modulation of the dynamic instability of tubulin assembly by the microtubule-associated protein tau. Mol. Biol. Cell. 1992;3:1141–1154. doi: 10.1091/mbc.3.10.1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Busciglio J, Lorenzo A, Yeh J, Yankner BA. β-Amyloid fibrils induce tau phosphorylation and loss of microtubule binding. Neuron. 1995;14:879–888. doi: 10.1016/0896-6273(95)90232-5. [DOI] [PubMed] [Google Scholar]
- 80.Hanger DP, Anderton BH, Noble W. Tau phosphorylation: the therapeutic challenge for neurodegenerative disease. Trends Mol. Med. 2009;15:112–119. doi: 10.1016/j.molmed.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 81.Wang JZ, Grundke-Iqbal I, Iqbal K. Kinases and phosphatases and tau sites involved in Alzheimer neurofibrillary degeneration. Eur. J. Neurosci. 2007;25:59–68. doi: 10.1111/j.1460-9568.2006.05226.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.de Lecea L. Cortistatin—functions in the central nervous system. Mol. Cell Endocrinol. 2008;286:88–95. doi: 10.1016/j.mce.2007.12.014. [DOI] [PubMed] [Google Scholar]
- 83.Sanchez-Alavez M, et al. Cortistatin modulates memory processes in rats. Brain Res. 2000;858:78–83. doi: 10.1016/s0006-8993(99)02336-7. [DOI] [PubMed] [Google Scholar]
- 84.Yang LP, Keating GM. Octreotide long-acting release (LAR): a review of its use in the management of acromegaly. Drugs. 2010;70:1745–1769. doi: 10.2165/11204510-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 85.Hu M, Tomlinson B. Pharmacokinetic evaluation of lanreotide. Expert Opin. Drug Metab. Toxicol. 2010;6:1301–1312. doi: 10.1517/17425255.2010.513700. [DOI] [PubMed] [Google Scholar]
- 86.Bruns C, Lewis I, Briner U, Meno-Tetang G, Weckbecker G. SOM230: a novel somatostatin peptidomimetic with broad somatotropin release inhibiting factor (SRIF) receptor binding and a unique antisecretory profile. Eur. J. Endocrinol. 2002;146:707–716. doi: 10.1530/eje.0.1460707. [DOI] [PubMed] [Google Scholar]
- 87.Chalabi M, et al. Somatostatin analogs: does pharmacology impact antitumor efficacy? Trends Endocrinol. Metab. 2014;25:115–127. doi: 10.1016/j.tem.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 88.Melmed S. New therapeutic agents for acromegaly. Nat. Rev. Endocrinol. 2016;12:90–98. doi: 10.1038/nrendo.2015.196. [DOI] [PubMed] [Google Scholar]
- 89.Wildemberg LE, Gadelha MR. Pasireotide for the treatment of acromegaly. Expert Opin. Pharmacother. 2016;17:579–588. doi: 10.1517/14656566.2016.1146688. [DOI] [PubMed] [Google Scholar]
- 90.Drewe J, Fricker G, Vonderscher J, Beglinger C. Enteral absorption of octreotide: absorption enhancement by polyoxyethylene-24-cholesterol ether. Br. J. Pharm. 1993;108:298–303. doi: 10.1111/j.1476-5381.1993.tb12799.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Fricker G, et al. Phospholipids and lipid-based formulations in oral drug delivery. Pharm. Res. 2010;27:1469–1486. doi: 10.1007/s11095-010-0130-x. [DOI] [PubMed] [Google Scholar]
- 92.Banks WA, Kastin AJ. Peptides and the blood-brain barrier: lipophilicity as a predictor of permeability. Brain Res. Bull. 1985;15:287–292. doi: 10.1016/0361-9230(85)90153-4. [DOI] [PubMed] [Google Scholar]
- 93.Banks WA, et al. Permeability of the murine blood-brain barrier to some octapeptide analogs of somatostatin. Proc. Natl Acad. Sci. USA. 1990;87:6762–6766. doi: 10.1073/pnas.87.17.6762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wong HL, Wu XY, Bendayan R. Nanotechnological advances for the delivery of CNS therapeutics. Adv. Drug Deliv. Rev. 2012;64:686–700. doi: 10.1016/j.addr.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 95.Spindler KR, Hsu T-H. Viral disruption of the blood–brain barrier. Trends Microbiol. 2012;20:282–290. doi: 10.1016/j.tim.2012.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Alexander A, et al. Recent expansions of novel strategies towards the drug targeting into the brain. Int. J. Nanomed. 2019;14:5895. doi: 10.2147/IJN.S210876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kaur IP, Bhandari R, Bhandari S, Kakkar V. Potential of solid lipid nanoparticles in brain targeting. J. Control Release. 2008;127:97–109. doi: 10.1016/j.jconrel.2007.12.018. [DOI] [PubMed] [Google Scholar]
- 98.Pahuja R, et al. Trans-blood brain barrier delivery of dopamine-loaded nanoparticles reverses functional deficits in parkinsonian rats. ACS Nano. 2015;9:4850–4871. doi: 10.1021/nn506408v. [DOI] [PubMed] [Google Scholar]
- 99.Zeng H, et al. Large-scale cellular-resolution gene profiling in human neocortex reveals species-specific molecular signatures. Cell. 2012;149:483–496. doi: 10.1016/j.cell.2012.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]