Abstract
Purpose: To test the effectiveness (Participant A) and tolerability (Participant B) of urinary stone comminution in the first-in-human trial of a new technology, burst-wave lithotripsy (BWL).
Materials and Methods: An investigational BWL and ultrasonic propulsion system was used to target a 7-mm kidney stone in the operating room before ureteroscopy (Participant A). The same system was used to target a 7.5 mm ureterovesical junction stone in clinic without anesthesia (Participant B).
Results: For Participant A, a ureteroscope inserted after 9 minutes of BWL observed fragmentation of the stone to <2 mm fragments. Participant B tolerated the procedure without pain from BWL, required no anesthesia, and passed the stone on day 15.
Conclusions: The first-in-human tests of BWL pulses were successful in that a renal stone was comminuted in <10 minutes, and BWL was also tolerated by an awake subject for a distal ureteral stone.
Clinical Trial NCT03873259 and NCT02028559.
Keywords: lithotripsy, urolithiasis, calculi, shock wave lithotripsy, burst wave lithotripsy, ultrasound, physics
Introduction
Our vision for the noninvasive surgical management of stones is an office-based, handheld ultrasound (US) device to target, break, dislodge, and expel stones and stone fragments from the upper urinary tract. Burst-wave lithotripsy (BWL) is a novel ultrasonic technology developed at the University of Washington (UW) within an NIH Program Project Grant to perform consistent and effective lithotripsy of stones (Fig. 1) while minimizing the side effects of pain and tissue damage.1–4 Ultrasonic propulsion from the same probe and system may then be used to noninvasively reposition the fragments to facilitate their clearance.5 If successful, the clinical application of BWL may open up an entirely new paradigm for noninvasive kidney stone treatment at point-of-care and without the need for anesthesia. In this study we present the first-in-human tests of this new technology: first, comminution is tested, and second, tolerance by an awake subject is tested.
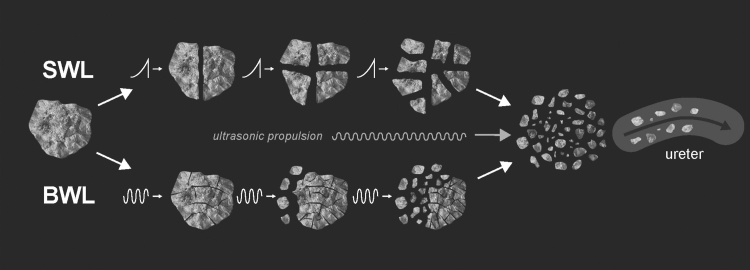
FIG. 1.
Graphical illustration of the concepts of how SWL and BWL are believed to fragment stones which may then be repositioned to the ureter by ultrasonic propulsion.5 Traditional SWL (upper image sequence) fragments stones noninvasively through sequential shock waves that create localized stress, leading to a primary fracture point within the stone. Typically, stones treated with SWL break from larger fragments into proportionally smaller fragments with repeated shockwaves, analogous to a “fragmenting” strategy in laser lithotripsy.7,8 In contrast, BWL comminution of stones (lower image sequence) occurs through small pieces shedding off a single large stone, more analogous to a “dusting” strategy in laser lithotripsy.4,9 This action is achieved using focused sinusoidal bursts of US waves that repetitively stress multiple regions within the stone. BWL's lower pressure amplitude avoids cavitation clouds that can shield the stone from US energy and possibly cause tissue injury.4,10 Clinically, BWL is advantageous because a higher rate can be used compared with SWL (10–100 Hz vs 1–2 Hz) again because of lower amplitudes, which allows energy to be delivered more quickly.2,10,11 (Image courtesy of Kim Reading of Applied Physics Laboratory.) BWL, burst-wave lithotripsy; SWL, shockwave lithotripsy.
Materials and Methods
Both studies utilized an investigational BWL ultrasonic lithotripter and propulsion system called Propulse 1, which consists of an SC-60 therapy transducer (Sonic Concepts, Bothell, WA; Fig. 2a) driven by a high-voltage amplifier (ENI AP400B; Electronic Navigation Systems) controlled by a function generator (Agilent 33250, Santa Clara, CA) and integrated with an imaging probe (P4-2; ATL/Philips, Bothell, WA) controlled by a research US imaging platform (VDAS-1; Verasonics, Inc., Redmond, WA).1,6 These combined probes allow for simultaneous visualization and comminution or propulsion of kidney stones. Coupling to the skin was accomplished through a water-filled, handheld scanhead using coupling gel. The treatment zone was determined by the focal beam and fixed focus (Fig. 2b). The burst length was 51 μs delivered at a frequency of 390 kHz. Ultrasonic propulsion was also applied for up to 3 seconds at a time and 2.4 MPa maximum pressure. Our studies were approved by the United States Food and Drug Administration and the Western Institutional Review Board (IRB) (Case A) and the UW IRB (Case B) after a progression through a series of preclinical2,3,14–18 and clinical trials5,14,19 of both technologies.
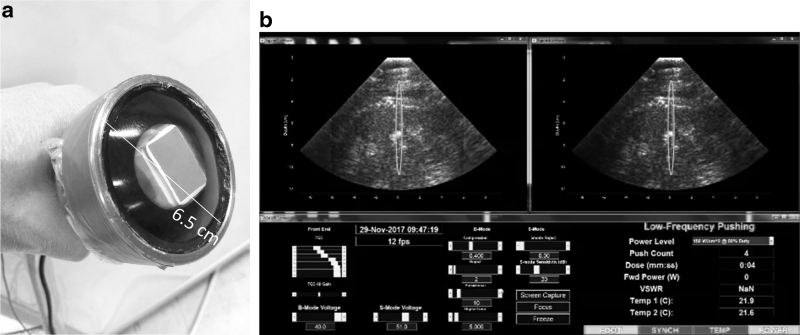
FIG. 2.
(a) Custom handheld BWL and ultrasonic propulsion probe with a water-circulating coupling head. The therapy probe (black/silver, peripheral) is a single element annulus that supports coaxial alignment of a P4-2 imaging probe (red, central). The overall probe diameter (SC-60) is 6.5 cm. (b) User interface demonstrating real-time imaging. The upper right panel displays the B-mode image. The red oval represents the treatment focus, where a stone must be aligned for treatment to be effective. The upper left panel displays the customized “S-mode” image,12,13 utilizing color-flow Doppler to make the stone stand out in green. The bottom panel includes the system settings and system feedback parameters for monitoring operation. Pulses are triggered with a footswitch.
Participant A was consented and enrolled in clinical trial NCT03873259 and was the first ever to undergo BWL. Although the ultimate goal was an office-based system, Participant A, per protocol, was treated with BWL while anesthetized, and before inserting the guidewire to be used for subsequent ureteroscopy. The stone (Fig. 3) was treated for a total of 9 minutes of BWL treatment exposure, including 8.5 minutes at 7 MPa peak negative pressure and 10 Hz repetition rate, and 30 seconds at 6 MPa and 17 Hz. The 30-second exposure tested feasibility of this second setting. The operator triggered the BWL pulses during the phases of the breathing cycle where the stone was within the target area on the US image. After 9 minutes of treatment, ureteroscopy was performed. The linear dimensions of residual stones were determined by analysis of the ureteroscope video by three blinded reviewers measuring fragment size with the 273-μm laser fiber for scale in a custom MATLAB program (Stonesizer ver 1.0). Participant A received a renal US examination as clinical follow-up to the ureteroscopy procedure.
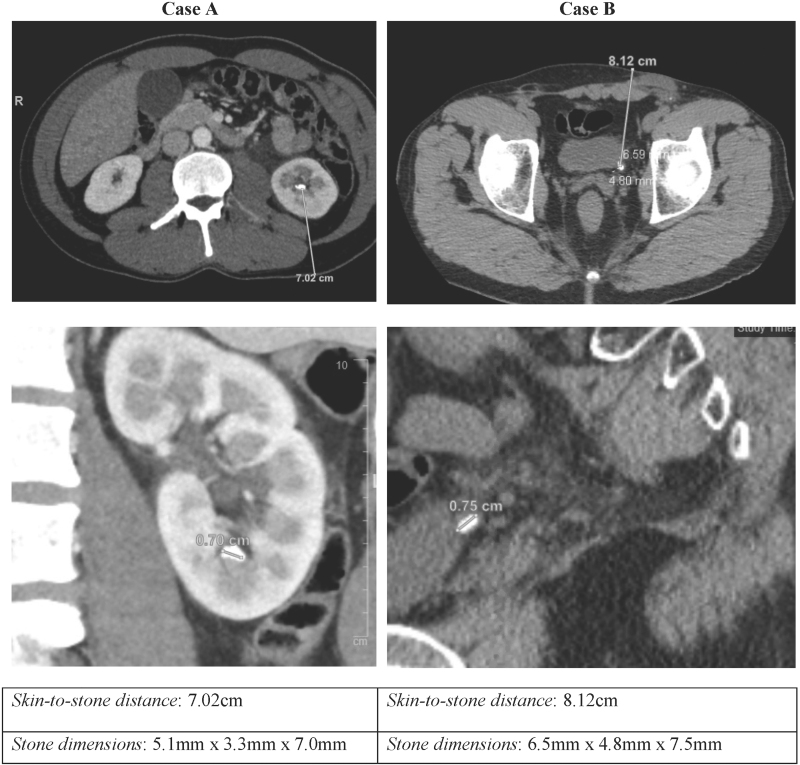
FIG. 3.
CT images of the targeted stones and SSD. Axial images of each subject shown in the top row. Coronal view of Participant A (lower left) and sagittal view of Participant B (lower right). SSD, skin-to-stone distances.
On the same day, Participant B was recruited in the Emergency Department with a ureteral stone. Five days later in clinic, Participant B was consented and enrolled in trial NCT02028559 and became the first awake participant to undergo BWL. He was asked to lie on the table supine in his street clothes with his shirt raised. The BWL probe was placed on his abdomen. Our goal was to use BWL bursts in 30-second exposures in conjunction with ultrasonic propulsion to dislodge and reposition the obstructing ureteral stone. Per this protocol, the peak negative pressure was limited to 6 not 7 MPa. The goal in this study was to assess tolerance of the treatment in an awake participant with a symptomatic stone, and to facilitate stone passage. A pain score of 0 to 10 based on a visual analog score was queried before treatment, after each of the first three bursts, and after completion. Pain score was also obtained after any burst that was felt, or anytime there were a change in pain level. Both participants received a weekly follow-up phone call for 3 weeks and received an US examination after 6 weeks. In this study, participants were recruited from the Emergency Department where subsequent US is often used to confirm if a ureteral stone has passed and hydronephrosis has resolved.
Results
Participant A
Immediately after 9 minutes of BWL, the ureteroscope was inserted and visually confirmed fragmentation of the 7 mm stone (Fig. 4). Within the lower pole, there were numerous small fragments of stone. There was a negligible amount of blood in the calix and a small amount of reddening of the urothelial lining of the nearby infundibulum. All fragments were measured to be smaller than 2 mm. Deviation in size measurements between three blinded reviewers was 11% for the largest fragment (1.85 ± 0.2 mm) and 3% for the third largest fragment (1.3 ± 0.03 mm).
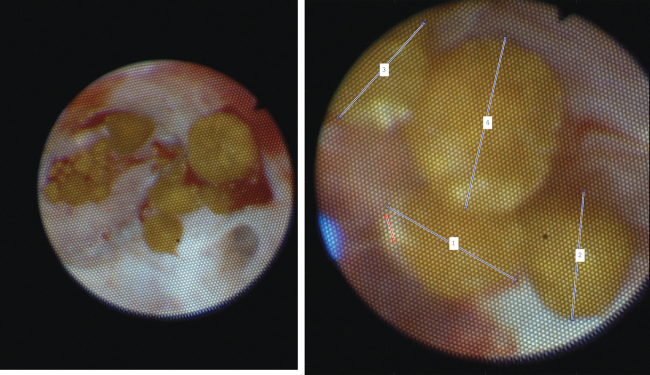
FIG. 4.
Participant A—Initial view of the fragments the 7-mm stone after 9 minutes of BWL (left) and the sizes measured on video using the laser fiber as scale (right). The four largest fragments in the image are (1.9, 1.6, 1.4, and 1.4 mm). Minimal bleeding, clotting, and discoloration of the tissue can be observed.
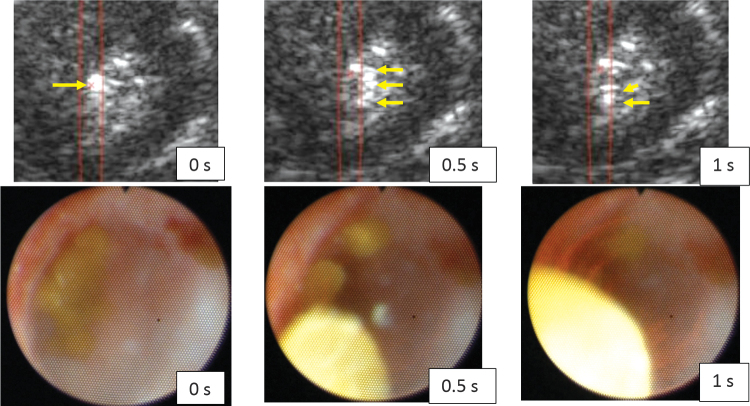
Fragmentation of the stone was elucidated by application of ultrasonic propulsion with real-time US imaging. In Figure 5, the fragments seen in Figure 4 were repositioned with a single ultrasonic propulsion pulse. These fragments were visualized moving out of the calix with both US and ureteroscopy.
FIG. 5.
Ultrasonic propulsion of the stone fragments after BWL, visualized with the US Propulse 1 system (top) and by ureteroscopy (lower). The times (0, 0.5, and 1 second) show frames just before, in the middle of, and at the end of the 1-second ultrasonic propulsion pulse, which is traveling down in the US frames and out of the page in the ureteroscope frames. The red x and red lines in the US frames indicate the focus and focal region on the Propulse 1 display, and yellow arrows were added in postprocessing to show the one collection of fragments at 0 second spreading and moving downward in the frames at 0.5 and 1 second. This motion and US imaging revealed to the operator that the stone was no longer intact stone but was instead many fragments as has been observed in vitro.1 One ultrasonic propulsion pulse was observed to move the fragments out of the calix, and in ultimate clinical use, many pulses may move the stones out of the collecting system to facilitate clearance. (Supplementary Videos S1 and S2) are included.
The stones were then further fragmented by laser to <1 mm, and a ureteral stent was placed. At the completion of the procedure, there was no noticeable bruising or petechiae on the skin overlying the treated flank. The patient awoke with minimal pain and was discharged with standard postureteroscopy medications consisting of nonsteroidal anti-inflammatories, tamsulosin, and oral narcotic pain medications if needed.
Participant B
Participant B reported a pain score of 2 of 10 with intermittent left flank pain before the procedure. The 7.5 mm ureterovesical junction (UVJ) stone was identified with the research device. About 9 minutes of BWL (6 MPa and 17 Hz) and one to three ultrasonic propulsion pulses about every 2 minutes were applied for a total of 10 minutes of exposure. The participant reported no feeling with the BWL bursts, a slight sensation “of the stone moving” with some of the propulsion bursts, and no pain afterward. No change in hydronephrosis was observed, and no displacement of the stone along the ureter was observed. No discoloration was seen on his skin. He reported complete resolution of his flank pain, rated at 0 of 10 after the procedure.
Postprocedure follow-up
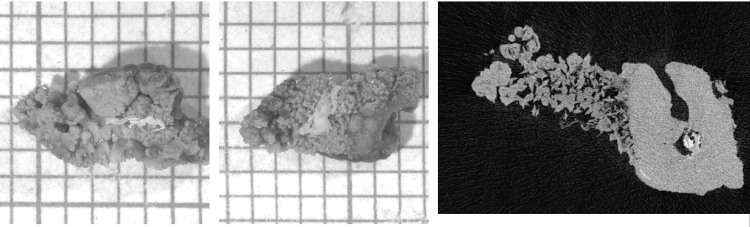
In the 3-week follow-up, neither patient reported any adverse events or narcotic medication use. Participant A had hematuria and urgency following the procedure that included ureteroscopy and stent, which was managed with tamsulosin and ibuprofen that resolved after stent removal. Participant B reported blood in the first urination after treatment but none thereafter. After the first week, he reported resolution of urinary urgency that was present before therapy. After 15 days he passed the stone (Fig. 6). Specifically, both participants denied nausea, fever, constipation, diarrhea, voiding problems, urinary tract infection, skin changes, and abnormal pain or discomfort. Follow-up imaging with a renal US examination at 6 weeks showed no stones or hydronephrosis in either participant.
FIG. 6.
Participant B—Two photographs of the passed stone on millimeter graph paper and a μCT slice of the stone with dimensions of μCT of 7.4 mm × 3.4 mm × 3.1 mm and the determined volume was 21.96 mm3. IR analysis identified the stone as calcium oxalate monohydrate, and the μCT analysis20 reported COM/COD/apatite 57%/37%/6% by volume. μCT, micro-CT.
Discussion
We present the findings of the initial application of a new lithotripsy technology, BWL, to comminute a renal stone before ureteroscopy and treat a distal ureteral stone in an awake subject without anesthesia. The US imaging of the research device gave real-time feedback on the treatment of the stone that helped guide treatment duration. The incorporated ultrasonic propulsion could also be used to reposition fragments to facilitate clearance.
Participant A demonstrated excellent comminution of the stone with only 9 minutes of treatment. Participant B was awake and without any anesthesia while a distal ureteral stone was targeted. The therapy did not cause additional pain and was well tolerated. He reported preexisting discomfort from the obstructing UVJ stone but felt no added sensation from the BWL dislodging treatment. In addition to not necessitating operating room resources, an awake patient might improve the treatment by controlled breathing or easily changing position. However, we did not obtain visual confirmation of the stone fracturing (the US image was unchanged throughout the treatment), and it is unclear if the dislodging BWL pulses facilitated or potentially delayed stone passage as the stone did not pass until 15 days after treatment. Comparing the dimensions of the passed stone with preoperative CT dimensions, it is possible that the treatment decreased the stone width. However, the primary intent was to test tolerability for future stone breaking efforts.
This study was limited to 10 minutes of treatment to be mindful of time used in the operating room or clinic, but the goal is <30 minutes of treatment. The current probe is optimized for stones up to 7 mm, but our group is working to expand the focal zone with a goal of treating stones over 10 mm.1,21 Likewise, our current probe produces BWL exposures at a skin-to-stone depth (SSD) of 5 to 7 cm, which with pushing on the skin with the US probe is comparable with a 10-cm SSD on CT,5 and to treat a larger range of body shapes either a section of probes with different focal depths or on probe array with varying focal depth will be needed. There was no difficulty imaging and targeting the stones in these participants, but generally image quality for targeting is degraded by larger SSD.
Further study of BWL in humans is currently underway and other studies have been submitted for approval since BWL may have many potential benefits. For example, it would be interesting to know if BWL could offer unique benefits to vulnerable groups such as pregnant women, children, or individuals with spinal cord injury, or to patients with <7 mm stones or fragments that might otherwise be observed. In addition to the two trials mentioned here, there is a third trial sponsored by Sonomotion, Inc., which licensed the BWL technology from UW. Together, these trials aim to build evidence supporting the use of BWL as a front-line noninvasive treatment for urolithiasis without some limitations of traditional shockwave lithotripsy. Successful treatment of upper tract urinary stones without anesthesia avoids significant risk, delay, and inconvenience to patients. This modality may also allow for immediate treatment of kidney and ureteral stones at presentation in an emergency department or a urology clinic, which would be significantly less costly than the operating room and may shift the clinical decision-making about treating asymptomatic stones.
Conclusions
BWL was used for the first time in humans to noninvasively target and treat a kidney and ureteral stone. In these initial two participants, BWL appeared safe and effective in breaking the renal stone and was tolerated without pain in an awake participant who later passed the targeted UVJ stone. Additional studies of this novel technology are underway to fully evaluate safety, effectiveness, and tolerability.
Supplementary Material
Abbreviations Used
- μCT
micro-CT
- BWL
burst-wave lithotripsy
- CT
computed tomography
- SSD
skin-to-stone depth
- SWL
shockwave lithotripsy
- US
ultrasound
- UVJ
ureterovesical junction
- UW
University of Washington
Author Disclosure Statement
A.D.M., B.W.C., B.D., M.R.B., and M.D.S. have consulting agreements with and equity in SonoMotion, Inc., which has licensed this technology from the University of Washington.
Funding Information
BWL and ultrasonic propulsion development and testing is funded by NIH National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) grants P01 DK043881 and K01 DK104854, NASA has funded the study of facilitating passage of UVJ stones. Resources through the VA Puget Sound Health Care System, Seattle, WA were used. The authors thank their colleagues on these grants and those in their departments who have made this study possible.
Supplementary Material
References
- 1. Ramesh S, Chen TT, Maxwell AD, et al. Urinary stone comminution testing with a clinical burst wave lithotripsy (BWL) system. J Endourol 2020. 10.1089/end.2019.0873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Maxwell AD, Wang YN, Kreider W, et al. Evaluation of renal stone comminution and injury by burst wave lithotripsy in a pig model. J Endourol 2019;33:787–792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. May PC, Kreider W, Maxwell AD, et al. Detection and evaluation of renal injury in burst wave lithotripsy using ultrasound and magnetic resonance imaging. J Endourol 2017;31:786–792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Maxwell AD, Cunitz BW, Kreider W, et al. Fragmentation of renal calculi in vitro by focused ultrasound bursts. J Urol 2015;193:338–344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Harper JD, Cunitz BW, Dunmire B, et al. First-in-human clinical trial of ultrasonic propulsion of kidney stones. J Urol 2016;195 (4, Part 1):956–964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Janssen KM, Brand TC, Cunitz BW, et al. Safety and effectiveness of a longer focal beam and burst duration in ultrasonic propulsion for repositioning urinary stones and fragments. J Endourol 2017;31:793–799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zhu S, Cocks FH, Preminger GM, et al. The role of stress waves and cavitation in stone comminution in shock wave lithotripsy. Ultrasound Med Biol 2002;28:661–671 [DOI] [PubMed] [Google Scholar]
- 8. Sapozhnikov OA, Maxwell AD, MacConaghy B, et al. A mechanistic analysis of stone fracture in lithotripsy. J Acoust Soc Am 2007;112:1190–1202 [DOI] [PubMed] [Google Scholar]
- 9. Maxwell AD, MacConaghy B, Bailey MR, et al. An investigation of elastic waves causing stone fracture in burst wave lithotripsy. J Acoust Soc Am 2020; 147:1607–1622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Maeda K, Colonius T, Maxwell AD, et al. Modeling and numerical simulation of the bubble cloud dynamics in an ultrasound field for burst wave lithotripsy. Proc Meet Acoust 2018;35:020006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. McAteer JA. Williams, JC, Jr., Bailey MR, et al. Strategies for improved shock wave lithotripsy. Minerva Urol Neffrol 2005;57:271–287 [PubMed] [Google Scholar]
- 12. Cunitz BW, Dunmire B, Sorensen MD, et al. Quantification of renal stone contrast with ultrasound in human subjects. J Endourol 2017;31:1123–1130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cunitz B, Dunmire B, Paun M, et al. Improved detection of kidney stones using an optimized Doppler imaging sequence. IEEE Int Ultrason Symp 2014;2014:452–455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bailey MR, Wang YN, Kreider W, et al. Update on clinical trials results of kidney stone repositioning and preclinical results of stone breaking with one ultrasound system. Proc Meet Acoust 2018;35:020004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Harper JD, Sorensen MD, Cunitz, BW, et al. , Focused ultrasound to expel calculi from the kidney: Safety and efficacy of a clinical prototype device. J Urol 2013;190:1090–1095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Connors BA, Evan AP, Blomgren PM, et al. Comparison of tissue injury from a novel technique of focused ultrasonic propulsion of kidney stones versus extracorporeal shock wave lithotripsy. J Urol 2014;191:235–241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wang Y-N, Simon JC, Cunitz BW, et al. Determination of the thresholds for renal tissue injury caused by focused ultrasound: a prospective focused on renal calculi expulsion. Ther Ultrasound 2014;2:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Harper JD, Dunmire B, Wang YN, et al. Preclinical safety and effectiveness studies of ultrasonic propulsion of kidney stones. Urology 2014;84:484–489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dai JC, Harper JD, Chang HC, et al. Quantitative assessment of effectiveness of ultrasonic propulsion of kidney stones. J Endourol 2019;33:850–857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Williams, JC.Jr., McAteer JA, Evan AP, et al. Micro-computed tomography for analysis of urinary calculi. Urol Res 2010;38:477–484 [DOI] [PubMed] [Google Scholar]
- 21. Randad A, Ghanem MA, Bailey MR, et al. Design, fabrication, and characterization of broad beam transducers for fragmenting large renal calculi with burst wave lithotripsy. J Acoust Soc Am 2020;148:44–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.