Abstract
Background and Purpose:
Multiple continuity indexes are available, however, their properties are not understood sufficiently for examining the influence of nurse staffing pattern on patient outcomes. We examined continuity measures to understand their properties and potential limitations for measuring nursing care continuity.
Methods:
We examined the behavior of continuity indexes as applied to clinical practice data that were collected with the Hands-on Automated Nursing Documentation System and data from computer simulation.
Results:
Different continuity measures exhibited very different statistical characteristics. Most importantly, many continuity measures contain a length-of-stay dependent term that is uncorrelated with continuity.
Conclusion:
Findings provide a deep understanding of the conceptual foundations and properties of various continuity measures that will help researchers select proper measures and interpret analysis outcomes in their research.
Keywords: continuity index, care continuity, acute care hospital setting, length of stay, Hands-on Automated Nursing Documentation System, HANDS
Introduction
Continuity is an understudied variable in nurse staffing in hospitals. There are multiple continuity indexes in the literature; however, their properties are not well understood. Continuity indexes, if adapted appropriately in nursing research, may provide important insight about the impact of staffing patterns on patient outcomes, leading to improvement in practice-based nurse staffing policies. The purpose of this article is to examine continuity measures to reveal their properties and potential limitations for measuring nursing care continuity.
Background
Using a variety of measures for quantifying care continuity, multiple investigators have studied the effects of care continuity on patient outcomes. A systematic review of articles assessing continuity in physician-patient relationship revealed 32 different indexes used in 44 studies (Jee & Cabana, 2006). The authors classified these indexes into those that calculated continuity primarily based on duration of provider relationship, density of visits, dispersion of providers, sequence of providers, or subjective perception of patients. More recently, van Walraven et al. examined 18 studies of association between continuity and patient outcomes and found 10 different continuity indexes employed (Jee & Cabana, 2006; van Walraven, Oake, Jennings, & Forster, 2010). Despite the variety in indexes used, important relationships have emerged.
Systematic reviews on the relationship between continuity and care quality show that increased continuity has significant association with decreased health utilization, increased patient satisfaction, and more preventive services (Jee & Cabana, 2006; van Walraven et al., 2010). Findings reported in these reviews and elsewhere offered tantalizing clues on the potential positive impact of care continuity (Bostrom, Tisnado, Zimmerman, & Lazar, 1994; Russell, Rosati, Rosenfeld, & Marren, 2011), although other studies did not find a positive association between continuity and improved patient outcomes (Siow, Wypij, Berry, Hickey, & Curley, 2013; Stifter et al., 2015).
To address this knowledge gap for the published continuity indexes, we started by examining their definitions and mathematical properties. Our analysis provided insight on rationale behind definitions of various continuity measures and will enable researchers to have better conceptual understanding of each measure. Our analysis also revealed that these continuity indexes can be grouped into categories with indexes in each category exhibiting very similar behaviors. With this insight, we identified representative continuity indexes for further study. Utilizing actual nursing care data collected in clinical practice as well as computer simulation, we then investigated the behavior of these indexes. The insight on the behavior of these indexes will enable researchers to make informed decisions about how to operationalize their concept of continuity given their research question and how to interpret their study findings.
Methods
We consider the measure of nurse continuity, broadly defined as the intensity and consistency of a patient’s exposure to the nurses caring for a patient during a continuous stay on a hospital unit. Although the scenarios we describe and terminologies we use in the following sections came from nursing, the fundamental properties revealed in this study are broadly applicable to other caregiver-patient relationships.
We will refer to a patient’s continuous stay on a hospital unit as a patient episode, which typically consists of many nursing shifts, during each of which one nurse is assigned to the care of the patient. Suppose a patient stays on a unit staffed by M unique nurses for a period of time. During the stay, K (out of M available) unique nurses provide care to the patient, with nurse i (i=1, …, K) being in charge of the care during ni of the total N nursing shifts that occur over that period of time.
We first reviewed the continuity measures we found in the literature and grouped them into five categories based on the similarity of their mathematical definitions. We demonstrated that indexes within each category are variations of each other and share the same conceptual model in measuring continuity. We then applied the definitions of continuity indexes to clinical practice data collected using HANDS (Hands on Automated Nursing Documentation System) (Keenan et al., 2002).
HANDS is an electronic care planning system that nurses use to describe the care provided to a patient on each shift within an episode. The system automatically links information about the nurse in charge of a patient on each shift to the care plan data documented. Applying multiple continuity indexes to HANDS data allowed us to compare and contrast the behavior of different continuity measures when applied to real data, which fully reflected the complexity of clinical practice.(Keenan et al., 2012)
The behavior of continuity indexes applied to data collected during clinical practice were inevitably affected by numerous factors, including conditions of all patients on the unit, specialty and experience of all nurses available during a shift, dynamics of individual patient-nurse dyads, and many others. To eliminate any potential confounding and isolate the causes of some of the behaviors we observed when applying the continuity indexes to practice data, we also conducted computer simulation to further examine the properties of the continuity indexes. We simulated a virtual unit of 70 unique RNs with 8-hour shifts. We generated patient episodes with random lengths of stay (number of shifts). For each shift, the assignment of a nurse to a patient in each 8-hour shift was random and independent of episode length. The assignment is weighted, with nurses that had cared for the same patient in the previous 24 hours given a weight coefficient of greater than or equal to one, while other nurses are given a weight of one. A nurse assigned a weight of say 3 is three times as likely to be assigned as one assigned a unit weight. A larger weight for continuing nurses therefore means that nurses are more likely to be assigned to the same patients on consecutive days, leading to a higher nurse continuity.
Results
Categories of Continuity Care Measures
Based on the mathematical properties of the continuity measures, we grouped them into five categories (Table 1). The first category includes Modified Continuity of Care Index (MCCI), which measures the fraction of visits made by a returning provider (a nurse that had prior exposure to this patient during the current hospital stay). The operational definition is the proportion of total time with nurses who care for a patient on 2 or more shifts during an episode of care. Other measures in this category, including Continuity of Care Index (CCI), Known Provider continuity index (K index) (Ejlertsson & Berg, 1984), Modified Continuity Index (MCI), Modified Modified Continuity Index (MMCI), and Consistency Index, can be seen as minor variations of MCCI.
Table 1.
Summary of Continuity Indexes.
| Measure | Interpretation | Variations |
|---|---|---|
| Modified Continuity of Care Index (MCCI) | Fraction of visits (shifts) by a returning provider (RN) | Continuity of Care Index (CCI); Known Provider continuity index (K index) (Ejlertsson & Berg, 1984); Modified Continuity Index (MCI); Modified Modified Continuity Index (MMCI); Consistency |
| Usual Provider of Care index (UPC) (Breslau & Reeb, 1975) | Fraction of visits (shifts) by the usual provider (primary RN) | UPC measured in time (instead of visits); Fundamental Continuity of Care Index (FCCI) |
| Herfindahl-Hirschman (HH) Index | Dispersion (difference) of visit (shift) distribution among M providers (RNs) | Standardized Index of Concentration (CON); FRAC; Continuity of Care index (COC) (Bice & Boxerman, 1977) |
| GINI index (Shortell, 1976) | Dispersion (absolute difference) of visit (shift) distribution among M providers (RNs) | |
| Sequential Continuity of Care index (SECON) (Steinwachs, 1979) | Fraction of visits (shifts) that a patient sees a provider (RN) from previous visit (day) | Generalized sequential continuity |
Instead of taking into account all providers involved, the second category, represented by the Usual Provider of Care (UPC) index (Breslau & Reeb, 1975), evaluates the portion of care provided by the usual provider. This index can be operationalized in one of two ways as the proportion of shifts or proportion of time spent by the primary or main nurse (i.e., the nurse that spent the most time caring for the patient during a hospital stay) caring for a patient during an episode of care. The two variants cof the UPC indexes (portion of visits and portion of time) can be multiplied together to generate the Fundamental Continuity of Care Index (FCCI) (Citro, Ghosh, & Churgin, 1997).
The third category of continuity indexes try to measure the dispersion, in terms of average square difference, of the number of visits made by each provider. The more a patient’s visits are concentrated among just a small portion of providers, the higher the variance (dispersion). For this category of indexes, COC is operationalized as the degree to which care provided to a patient is concentrated among a fraction of nurses who worked on the unit during the episode. The representative of this category is the Herfindahl-Hirschman (HH) Index and its variations include Standardized Index of Concentration (CON), Rae Index of Fragmentation (FRAC) (Roos, 1980), and Continuity of Care index (COC) (Bice & Boxerman, 1977). These variations are simple transformations of HH to achieve a normalized range (CON, COC) or desired directionality.
The fourth category also tries to measure the dispersion of shifts among nurse providers but using the absolute difference metric (i.e., the absolute value of the difference). The related index, Gini Index (Shortell, 1976), is often used to assess income inequality in economics and is used in the healthcare setting to measure the inequality in the share of care provided by different providers. More inequality implies a concentration of patient care in a smaller portion of providers and hence better continuity. One would expect this index to be highly correlated with those in the third category.
The last category, sequential continuity index (SECON), assesses the continuity in a chronological order and is operationalized by measuring the fraction of time a patient is visited by a provider that saw the patient in the recent past and therefore is providing continuity of care (Steinwachs, 1979). For example, for nursing care, we can define a 24-hour window, seeing a patient within the last 24 hours counts as seeing the patient recently. The time window for the definition of the recent visit can be flexible, resulting in many possible variations for SECON.
Comparing the above five categories, we observe that they either try to measure (1) the portion of visits with some continuity of care providers (first, second, and fifth categories) or (2) the concentration of visits among available providers (third and fourth categories). An examination of the relationship of the measures in different categories would be informative for future research.
Correlations between Indexes
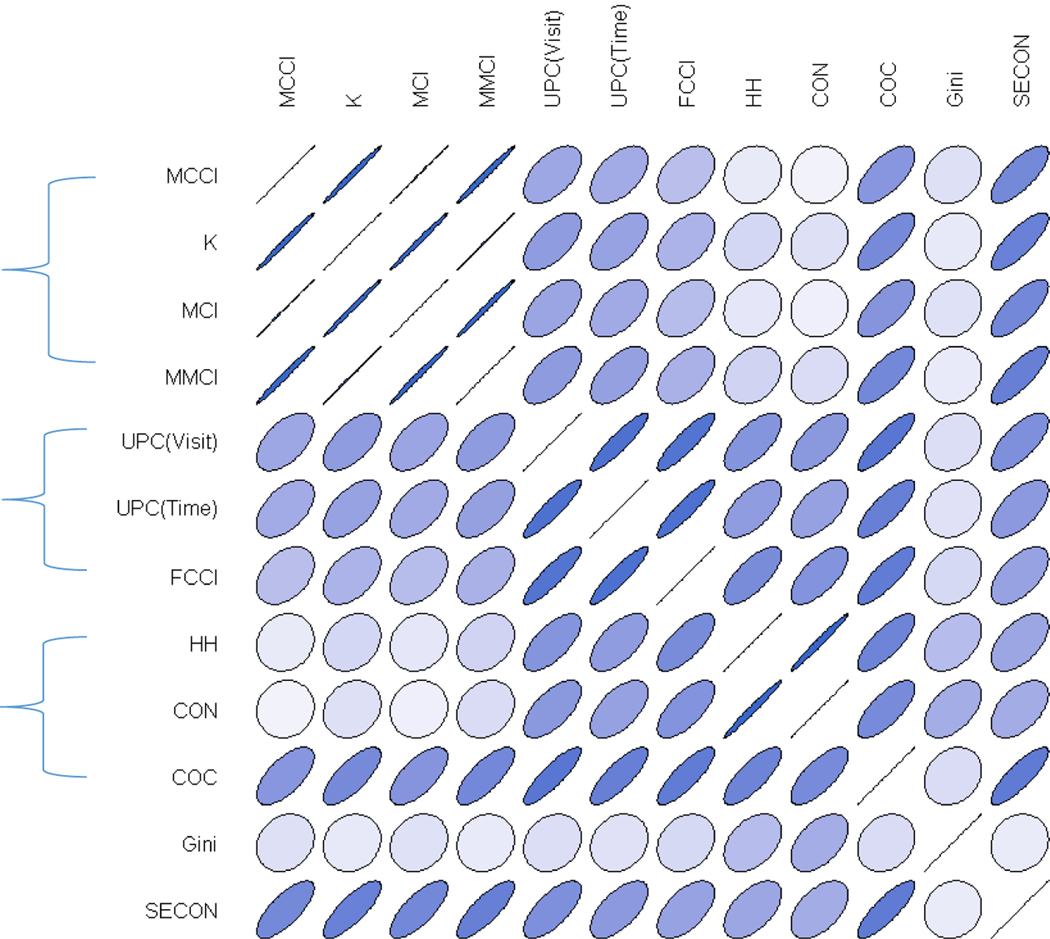
Applying the definitions of continuity indexes to nursing care data in HANDS, we obtained the continuity measures for patient care episodes documented over a two-year period in four Midwestern hospitals. We focused on episodes with a length of stay (LoS) of 48 hours or longer, since the concept of continuity is not very meaningful for shorter episodes. Figure 1 shows the magnitudes of correlations between various continuity measures. We have excluded continuity measures with perfect correlation to the representative measures of their respective categories, including CCI, consistency, and FRAC. Narrower ellipse and darker color signify a higher correlation while lighter color and a rounder shape indicate a correlation closer to 0. We observe from Figure 1 that continuity indexes belonging to the same category in general were much more highly correlated with each other than with other indexes. The only exception is COC, whose correlations with many indexes in other categories were higher than its correlations with the other indexes in its category. The COC was derived from the HH index by a linear transformation to normalize its range to be 0 to 1 for any value of N (number of visits), while the range of HH is 1/N to 1 for a given value of N. This seemingly minor transformation reduces the correlation between COC and HH to 0.78. For longer episodes (N≥20 visits), the effect of transformation was minor and the correlation between the two indexes was high (r=0.95). Given the clustering of indexes we observed in these analyses, in the following analyses we focused only on five representative indexes: MCCI, UPC (Visit), HH, Gini, and SECON, as well as the COC, which was somewhat dissimilar with other indexes in its category.
Figure 1.
Correlations between Continuity Measures. MCCI, Modified Continuity of Care index; UPC, Usual Provider of Care index; HH, Herfindahl-Hirschman index; COC, Continuity of Care index; SECON, Sequential continuity index. Narrower ellipse and darker color signify a higher correlation while lighter color and a rounder shape indicate a correlation closer to 0.
The descriptive statistics for the six indexes (applied to clinical practice data in HANDS) are listed in Table 2, where we have listed the statistics for short episodes (fewer than 10 shifts) and the remaining episodes that were relatively long separately. We observed that although all indexes by definition are between 0 and 1, they had very different ranges. Gini index were almost always greater than 0.5, while HH and COC rarely exceeded 0.5. The only index with a range of [0, 1] was SECON. More importantly, different indexes would lead to different conclusions regarding the relative level of continuity of short versus long episodes. Compared with short episodes, long episodes had substantially larger mean MCCI (0.8 SD larger), but substantially smaller HH (1.2 SD smaller) and Gini index (0.7 SD smaller). The differences for the other three indexes were not substantial (around 0.3 SD for UPC and COC and close to 0 for SECON).
Table 2.
Properties of the Representative Indexes of Continuity
| Short Episodes (N<10 shifts) | Long Episodes (N≥10 shifts) | |||||
|---|---|---|---|---|---|---|
| Index | Mean±SD | Median [IQR] | Range | Mean±SD | Median [IQR] | Range |
| MCCI | 0.23±0.15 | 0.22 [0.14, 0.33] | 0.00–0.67 | 0.36±0.14 | 0.36 [0.27, 0.45] | 0.00–0.79 |
| UPC | 0.18±0.11 | 0.17 [0.13, 0.25] | 0.00–0.67 | 0.15±0.06 | 0.15 [0.10, 0.20] | 0.00–0.44 |
| HH | 0.24±0.07 | 0.22 [0.18, 0.28] | 0.11–0.63 | 0.14±0.05 | 0.13 [0.10, 0.16] | 0.03–0.38 |
| COC | 0.09±0.07 | 0.08 [0.05, 0.13] | 0.00–0.50 | 0.07±0.04 | 0.07 [0.04, 0.09] | 0.00–0.31 |
| Gini | 0.95±0.04 | 0.96 [0.94, 0.97] | 0.67–0.99 | 0.91±0.06 | 0.93 [0.89, 0.95] | 0.48–0.99 |
| SECON | 0.34±0.26 | 0.33 [0.17, 0.50] | 0.00–1.00 | 0.34±0.16 | 0.33 [0.23, 0.44] | 0.00–1.00 |
Note. SD, Standard Deviation; MCCI, Modified Continuity of Care index; UPC, Usual Provider of Care index; HH, Herfindahl-Hirschman index; COC, Continuity of Care index; SECON, Sequential continuity index.
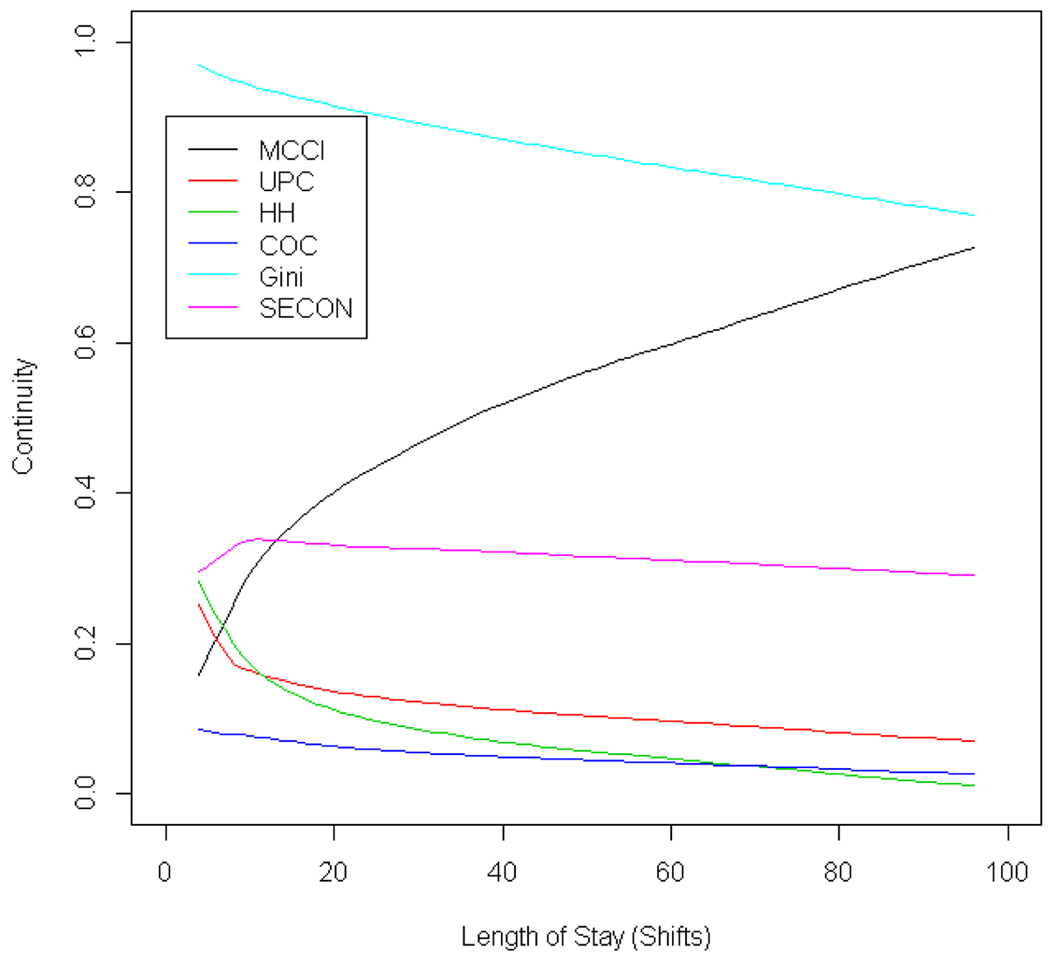
Figure 2 shows the dependence of different continuity indexes on the LoS. The average MCCI grew by over 0.5 and about 3.6 SD as LoS increases. On the other hand, the average of HH and Gini indexes decreased by about 3.4 SD and 3.8 SD, respectively, as LoS increases. Earlier, we did not see in Table 2 substantial difference in the average continuity as measured by UPC, COC, and SECON when grouping patient episodes as below 10 shifts versus 10 shifts or longer. The closer look afforded by Figure 2, however, shows that there seemed to be dependence over LoS. Average UPC decreased by 0.2 and 2 SD as LoS increases; average COC decreased by 0.06 and 1 SD as LoS increases. Average SECON demonstrated a small increase as LoS starts to increase and then a small decrease as LoS continues to increase, but the gap between the maximum and the minimum was only 0.2 SD.
Figure 2.
Continuity versus Length of Stay. MCCI, Modified Continuity of Care index; UPC, Usual Provider of Care index; HH, Herfindahl-Hirschman index; COC, Continuity of Care index; SECON, Sequential continuity index.
The association between various continuity indexes and LoS was confirmed when we examined the correlations between them (Table 3). HH, MCCI and Gini showed moderate correlations with LoS; UPC and COC showed weak but clinically meaningful correlation with LoS; only SECON showed negligible correlation with LoS. MCCI showed positive correlation with LoS, while UPC, COC, HH, and Gini were negatively correlated with LoS. Given this, one would expect a negative correlation between MCCI and these other four indexes, but MCCI was positively correlated with UPC, COC, and HH (p<.001 for all) and only negatively correlated with Gini index. This finding indicates that many continuity measures likely contain at least two factors, one that is related to LoS and one that is not. While we conjectured that the other factor measures the continuity, we could not exclude the possible contributions of numerous other factors existent in clinical practice. In addition, LoS and continuity likely have significant association in clinical practice, making it even more difficult if not impossible if continuity measures contain LoS-dependent bias terms from clinical data.
Table 3.
Correlations with LoS and MCCI obtained from HANDS data
| Correlation with LoS | Correlation with MCCI | |||
|---|---|---|---|---|
| Correlation | p Value | Correlation | p Value | |
| MCCI | 0.465 | .000 | 1 | .000 |
| UPC | −0.175 | .000 | 0.551 | .000 |
| HH | −0.620 | .000 | 0.130 | .000 |
| COC | −0.191 | .000 | 0.662 | .000 |
| Gini | −0.453 | .000 | −0.185 | .000 |
| SECON | −0.020 | .024 | 0.749 | .000 |
Note. LOS, length of stay; MCCI, Modified Continuity of Care index; UPC, Usual Provider of Care index; HH, Herfindahl-Hirschman index; COC, Continuity of Care index; SECON, Sequential continuity index.
To eliminate the influences of potential confounders, we examined the correlation between continuity indexes and LoS using computer simulation. From Table 4, we observe that MCCI showed substantial positive correlation with LoS; UPC, HH, COC, and Gini showed substantial negative correlation with LoS; SECON showed negligible correlation with LoS. These findings are consistent with the correlations obtained from clinical practice data. We also examined the correlation between continuity indexes and the continuity weights used in our simulation. We see that all indexes were positively correlated with the weight an assignment policy gave to past history with a patient, confirming our intuition that these continuity indexes measure continuity. The correlation between the weight coefficient and the LoS was negligible (r=0.016, p=.472), indicating that with the exception of SECON, continuity indexes consist of two uncorrelated components, one reflecting the weight assigned to continuity in nurse assignment and one correlated with the LoS.
Table 4.
Correlations obtained from Computer Simulation
| Correlation with LoS | Correlation with Continuity Weight | |||
|---|---|---|---|---|
| Correlation | p Value | Correlation | p Value | |
| MCCI | 0.440 | .000 | 0.700 | .000 |
| UPC | −0.489 | .000 | 0.574 | .000 |
| HH | −0.702 | .000 | 0.454 | .000 |
| COC | −0.548 | .000 | 0.590 | .000 |
| Gini | −0.583 | .000 | 0.614 | .000 |
| SECON | −0.015 | .504 | 0.796 | .000 |
Note. LoS, Length of Stay; MCCI, Modified Continuity of Care index; UPC, Usual Provider of Care index; HH, Herfindahl-Hirschman index; COC, Continuity of Care index; SECON, Sequential continuity index.
Discussion
Continuity is an understudied variable in nurse staffing in hospitals. If adapted appropriately, continuity indices may be important measures for examining the influence of nurse staffing on patient outcomes. This work provides insight on the properties of continuity measures that will inform the selection and utilization of continuity measures in research on effects of nurse staffing on patient outcomes. In addition, our findings can be applied to the study of continuity of care from other healthcare providers.
Our analysis of the mathematical definitions of various continuity indexes revealed that they either try to assess the portion of visits with continuity of care providers or try to measure the concentration of visits among providers. Among the former, one category of indexes including MCCI and its variations measure the portion of visits with providers that have seen the patient before; one category focuses on the role of the primary provider and examines the portion of visits by this primary provider; SECON and its variations measure the portion of providers that have seen the patient in the recent past. Indexes that measure the concentration include HH, COC, and others that use the square difference to assess the dispersion of visits among providers, as well as the Gini index that uses the absolute difference to assess the dispersion.
Examination of the correlations between continuity indexes showed that with the exception of COC, continuity indexes within a category are highly correlated with each other. As a consequence, we focused on the five representative indexes, MCCI, UPC (Visit), HH, Gini, and SECON, as well as COC, which exhibits some dissimilarity with other indexes in its category, in our analysis using clinical data as well as simulation to evaluate the properties of continuity indexes. Descriptive statistics of these six indexes when applied to clinical data collected in HANDS showed that they had very different means, standard deviations, and ranges, suggesting that we need to be careful about what values for an index indicate a high continuity or a low continuity. More importantly, we discovered substantial correlations between continuity indexes and the LoS in both directions (positive and negative). In practice, a patient condition might dictate nurse assignment. For example, expert nurses are often assigned to the most complex patients. If there are only a few expert nurses on a unit, then a complex patient will most likely see a high continuity in care. More complex patients likely will have longer LoS (Moy, Coffey, Moore, Barrett, & Hall, 2016). On the other hand, the higher quality of care they receive from continuous care of expert nurses might contribute to a reduction of LoS. Therefore, patient condition is a confounder in the association between continuity indexes and LoS. Similar, numerous other factors could influence the behavior of continuity indexes computed from data obtained through complex clinical practice. Computer simulation allowed us to eliminate these confounders and examine the intrinsic association between various continuity indexes and LoS due purely to their mathematical definitions, excluding effects of any potential confounders.
Our computer simulation showed that with the exception of SECON, which had negligible correlation with the LoS, all continuity indexes contain two components, one reflecting the continuity of the nurse assignment and one related to the LoS. The presence of the LoS component, even though it is independent from nurse assignment in our simulation, in many continuity indexes has major implications in analysis involving continuity. Although LoS is but one possible patient outcome, it likely is associated with many other patient outcomes as well as patient characteristics. Therefore, this LoS component will confound the analysis of the effects of care continuity on patient outcomes.
Among all continuity indexes examined, SECON was the only one with little correlation with LoS and yet showed high correlation with continuity weight used by the nurse assignment policy described in the methods section. Furthermore, the definition of SECON also allows it to be evaluated for each individual visit, a property shared by MCCI, UPC, and their variants, but not dispersion based indexes. This would be very useful if a study aims to uncover the effect of continuity on the outcome of each individual visit. SECON index can also be easily generalized, for example, to give partial continuity score to providers, whose exposures to the patient are from more distant past, to give credit to repeated exposures to a patient, or to account for proximity exposures through handoff from a provider with multiple recent exposures. Regardless of which continuity measure a researcher adopts or devises, our findings showed that a careful analysis of its property is needed to avoid misinterpretation of analytical outcomes. In particular, if a continuity measure is substantially correlated with LoS, this correlation should always be accounted for when determining the association between continuity and LoS or other patient outcomes that might be correlated with LoS.
A limitation of the series of analyses we undertook is inherent in the nature of the phenomenon we studied. The continuity measures reviewed and analyzed in this study focus on the continuity of patient-care provider interactions. Continuity of care, however, is a very complex concept consisting of multiple facets, including seamless care coordination across multiple disciplines, unencumbered information sharing between team members, learning of a patient’s unique characteristics over time, and trust building between patient/family and care providers. Fully capturing the complexity of continuity of care thus requires the development of novel instruments that are tailored to address the research questions with greater precision. Although we focused on LoS as a potential confounder, factors such as the condition of the patient, experience and specialties of the nurses or providers, and relationship between the patient and provider all need to be considered when investigating the relationship between continuity and patient outcomes.
In conclusion, our systematic analysis of the mathematical properties of continuity of care measure provided insights to inform experimental application of measures to a robust nursing care dataset and revealed that caution is needed when interpreting the meaning of values across measures and including LoS in the analysis. Simulation analyses confirmed these insights. Overall, the complexity of continuity of care should be carefully considered as studies are designed and results interpreted until novel instruments are available.
Acknowledgments
Funding:
This study was in part funded by grant numbers 1R36HS023072, R01HS015054, and R01NR012949 from the Agency for Healthcare Research and Quality (AHRQ) and the National Institute of Nursing Research (NINR), respectively. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the AHRQ and NINR. The final peer-reviewed manuscript is subject to the National Institutes of Health Public Access Policy.
Appendix. Continuity Measures
0. Definitions
M = total number of potentially available providers (nurses on a unit)
K = total number of providers (nurses) that provide care during a patient episode
N = total number of provider visits (nursing shifts) during a patient episode
ni = number of visits by the ith provider (shifts by ith nurse), i = 1, 2, …, M
1. Modified Continuity of Care Index (MCCI)
1.1. Definition:
1.2. Interpretation:
The fraction of visits (shifts) to a patient by a returning provider (RN).
1.3. Variations
Continuity of Care Index (CCI):
-
Known Provider Continuity (K) Index (Ejlertsson & Berg, 1984): .
It was obtained by dividing MCCI with a normalization constant so that the maximum value is equal to 1.
Modified Continuity Index (MCI):
Modified Modified Continuity Index (MMCI): . It was modified from MCI by dividing MCI with a normalization constant so that the maximum possible value is equal to 1.
Consistency:
2. Usual Provider of Care (UPC)
2.1. Definition (Breslau & Reeb, 1975):
2.2. Interpretation:
The fraction of visits (shifts) associated with the provider (nurse) seen most frequently during the patient episode.
2.3. Variations:
UPCtime: Fraction of time patient spends with the primary care provider.
Fundamental Continuity of Care Index (FCCI):
3. Herfindahl-Hirschman (HH) Index
3.1. Definition:
3.2. Interpretation:
HH measures the dispersion of visits among M available providers, as can be seen in the following:
3.3. Variations
Standardized Index of Concentration (CON): The linear transformation is applied so that the range of CON is 0, attained when visits were equally distributed among M providers, and 1, attained when only one provider visits.
FRAC (Roos 1980):
Continuity of Care (COC; Bice & Boxerman, 1977): Here the linear transformation is to make sure that the range is 0 to 1, with 0 attained when N (N≤M) providers visit, one visit for each provider.
4. Gini Index
4.1. Definition:
Order the providers in a non-decreasing order of number of visits, that is, n1≤n2≤…≤nM. The Gini index is defined as
4.2. Interpretation:
The Gini index was from the field of economics where it is often used to assess the income inequality by measuring area between the 45 degree line (of equality) and the Lorenz curve (of income distribution). It is shown to be equal to the relative mean absolute difference:
From this definition, we can see that it is similar to HH index in that it is also measuring the dispersion of visits among providers but instead of using square difference as HH, it uses absolute difference.
5. Sequential Continuity Index (SECON)
5.1. Definition (Steinwachs, 1979):
, where c(n)=1 if the same provider provides care for visits n and n-1; c(n)=0 otherwise.
5.2. Interpretation:
fraction of visits a patient sees the same provider as the previous visit.
5.3. Variations:
SECON for nursing care: where t(n) is the time (hours) after admission when shift n starts; and c(n)=1 if shift RN last sees the patient less than one day ago and c(n)=0 otherwise.
Generalized sequential continuity: c(n) can be generalized to be any monotonic non-increasing function of the time between last time shift RN for the n-th shift sees the patient and the start time of the n-th shift.
Footnotes
Conflict of Interest:
All but one of the authors have no financial or any other kind of personal conflicts with this manuscript. The HANDS software that was used in this study is now owned and distributed by HealthTeam IQ, LLC. Dr. Gail Keenan is currently the President and CEO of this company and has a current conflict of interest statement of explanation and management plan in place with the University of Florida.
Contributor Information
Yingwei Yao, Department of Biobehavioral Nursing Science, College of Nursing, University of Florida.
Hyochol Ahn, Department of Family, Community and Health System Science, College of Nursing, University of Florida, Gainesville, Florida.
Janet Stifter, Center for Care Innovation and Transformation, the American Organization of Nurse Executives (AONE), Chicago, Illinois.
Diana J. Wilkie, Prairieview Trust – Earl and Margo Powers Endowed Professor, and Director, Academic Center of Excellence in Palliative Care Research and Education, Department of Biobehavioral Nursing Science, College of Nursing, University of Florida.
Gail Keenan, Teaching and Research in Clinical Nursing Excellence, Department of Family, Community and Health System Science, College of Nursing, University of Florida, Gainesville, Florida.
Annabel Davis Jenks Endowed, Teaching and Research in Clinical Nursing Excellence, Department of Family, Community and Health System Science, College of Nursing, University of Florida, Gainesville, Florida.
References
- Bice TW, & Boxerman SB (1977). A quantitative measure of continuity of care. Medical Care, 15(4), 347–349. [DOI] [PubMed] [Google Scholar]
- Bostrom J, Tisnado J, Zimmerman J, & Lazar N. (1994). The impact of continuity of nursing care personnel on patient satisfaction. Journal of Nursing Administration, 24(10), 64–68. [DOI] [PubMed] [Google Scholar]
- Breslau N, & Reeb KG (1975). Continuity of care in a university-based practice. Journal of Medical Education, 50(10), 965–969. [DOI] [PubMed] [Google Scholar]
- Citro R, Ghosh S, & Churgin PG (1997). Modeling and evaluation of continuity of care in a staff model HMO. MD Computing: Computers in Medical Practice, 15(5), 298–306 [PubMed] [Google Scholar]
- Ejlertsson G, & Berg S. (1984). Continuity-of-care measures. An analytic and empirical comparison. Medical Care, 22(3), 231–239. [DOI] [PubMed] [Google Scholar]
- Jee SH, & Cabana MD (2006). Indices for continuity of care: a systematic review of the literature. Medical Care Research and Review, 63(2), 158–188. doi: 10.1177/1077558705285294 [DOI] [PubMed] [Google Scholar]
- Keenan G, Stocker J, Geo-Thomas A, Soparkar N, Barkauskas V, & Lee J. (2002). The HANDS project: Studying and refining the automated collection of a cross-setting clinical data set. Computers Informatics Nursing, 20(3), 89–100. [DOI] [PubMed] [Google Scholar]
- Keenan GM, Yakel E, Yao Y, Xu D, Szalacha L, Tschannen D, . . . Wilkie DJ (2012). Maintaining a consistent big picture: meaningful use of a Web-based POC EHR system. International Journal of Nursing Knowledge, 23(3), 119–133. doi: 10.1111/j.2047-3095.2012.01215.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moy E, Coffey RM, Moore BJ, Barrett ML, & Hall KK (2016). Length of stay in EDs: variation across classifications of clinical condition and patient discharge disposition. American Journal of Emergency Medicine, 34(1), 83–87. doi: 10.1016/j.ajem.2015.09.031 [DOI] [PubMed] [Google Scholar]
- Roos LL, Roos NP, Gilbert P, & Nicol JP (1980). Continuity of care: does it contribute to quality of care? Medical Care, 18(2), 174–184. [DOI] [PubMed] [Google Scholar]
- Russell D, Rosati RJ, Rosenfeld P, & Marren JM (2011). Continuity in home health care: is consistency in nursing personnel associated with better patient outcomes? Journal of Healthcare Quality, 33(6), 33–39. doi: 10.1111/j.1945-1474.2011.00131.x [DOI] [PubMed] [Google Scholar]
- Shortell SM (1976). Continuity of medical care: conceptualization and measurement. Medical Care, 14(5), 377–391. [DOI] [PubMed] [Google Scholar]
- Siow E, Wypij D, Berry P, Hickey P, & Curley MA (2013). The effect of continuity in nursing care on patient outcomes in the pediatric intensive care unit. Journal of Nursing Administration, 43(7–8), 394–402. doi: 10.1097/NNA.0b013e31829d61e5 [DOI] [PubMed] [Google Scholar]
- Steinwachs DM (1979). Measuring provider continuity in ambulatory care: an assessment of alternative approaches. Medical Care, 17(6), 551–565. [DOI] [PubMed] [Google Scholar]
- Stifter J, Yao Y, Lodhi MK, Lopez KD, Khokhar A, Wilkie DJ, & Keenan GM (2015). Nurse Continuity and Hospital-Acquired Pressure Ulcers: A Comparative Analysis Using an Electronic Health Record “Big Data” Set. Nursing Research, 64(5), 361–371. doi: 10.1097/NNR.0000000000000112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Walraven C, Oake N, Jennings A, & Forster AJ (2010). The association between continuity of care and outcomes: a systematic and critical review. Journal of Evaluation in Clinical Practice, 16(5), 947–956. doi: 10.1111/j.1365-2753.2009.01235.x [DOI] [PubMed] [Google Scholar]