Abstract
Background:
Pediatric patients are at risk for bleeding after cardiac surgery. Administration of antifibrinolytic agents reduces postoperative blood loss.
Objective:
Evaluation of the efficacy of combined administration of tranexamic acid (TXA) and ethamsylate in the reduction of postoperative blood loss in pediatric cardiac surgery.
Methods:
This prospective randomized study included 126 children submitted for cardiac surgery, and they were allocated into three groups: control group (n = 42); TXA group (n = 42):- received only TXA; and combined ethamsylate TXA group (n = 42):- received a combination of TXA and ethamsylate. The main collected data included sternal closure time, the needs for intraoperative transfusion of blood and its products, the total amount of blood loss, and the amount of the whole blood and its products transfused to the patients in the first 24 postoperative hours.
Results:
Blood loss volume in the first 24 postoperative hours was significantly smaller in combined group than the TXA and control groups and was significantly smaller in the TXA group than the control group. The sternal closure time was significantly shorter in the combined group than the other 2 groups and significantly shorter in TXA than the control group. The amount of whole blood transfused to patients in the combined group during surgery and in the first postoperative 24 h was significantly smaller than the other 2 groups and smaller in TXA group than the control group during surgery.
Conclusion:
Combined administration of ethamsylate and TXA in pediatric cardiac surgery was more effective in reducing postoperative blood loss and whole blood transfusion requirements than the administration of TXA alone.
Keywords: Blood loss, ethamsylate, pediatric cardiac surgery, tranexamic acid
INTRODUCTION
Excessive bleeding and the needs for blood transfusions are common in patients undergoing cardiac surgery requiring cardiopulmonary bypass (CPB),[1] and in some of these patients, there is a need for reoperation because of life-threatening bleeding.[2] Pediatric patients are at risk for bleeding after cardiac surgery because of the small blood volume compared to the CPB prime causing hemodilution, low levels of coagulation factors, hypothermia, and complexity of surgical repair of congenital heart diseases.[3]
Perioperative administration of antifibrinolytic agents (aprotinin, tranexamic acid, and epsilon aminocaproic acid) could help to reduce postoperative blood loss and transfusion of blood components. Aprotinin should be avoided in pediatric cardiac surgery as its use in adult cardiac surgery was associated with an increased risk of renal failure and mortality.[4] Intravenous administration of tranexamic acid (TXA) during cardiac surgery is associated with a significant reduction in postoperative blood loss with minimizing the need for blood transfusion.[5,6,7]
Ethamsylate is a synthetic hemostatic drug that is widely used to reduce blood loss in many surgeries such as obstetric,[8] orthopedic,[9] and urologic[10] surgeries but rarely used in open-heart surgery. Ethamsylate acts on the primary step of hemostasis by restoring of capillary endothelial resistance and activation of platelet adhesiveness, thus minimizing capillary bleeding.[11]
TXA and ethamsylate are readily available, and they are cost-effective drugs. We hypothesized that the use of TXA and ethamsylate combination in pediatric cardiac surgery requiring CPB may be more effective in reducing intra- and postoperative blood loss than the use of TXA alone. The primary outcome measure was the total blood loss in the first 24 postoperative hours. The secondary outcome measures were the sternal closure time, the amount of the blood and its component replacement therapy, postoperative surgical re-exploration, time to extubation, and intensive care unit (ICU) length of stay.
METHODS
This controlled prospective randomized study was carried out in Mansoura University Children Hospital from November 2017 to April 2019 after obtaining an approval from Institutional Review Board (IRB) of Mansoura Faculty of Medicine, Mansoura University given a code number (R/17.09.35) (date 14/11/2017), and a written informed consent was taken from the patient's parents or their legal guardian's. In total, 126 pediatric patients with cyanotic or acyanotic congenital cardiac anomalies of either sex, their age (1–10) years, and scheduled for cardiac surgery requiring CPB were included in this study. Hematological and coagulation studies were done for all patients, and these included complete blood count, partial thromboplastine time, activated clotting time (ACT), international normalization ratio in addition to liver and kidney function tests. Patients with redo cardiac surgery, pre-existing coagulopathy, hepatic or renal dysfunction, and history of allergy to one of the study drugs were excluded from the study.
Patients were randomly allocated into three groups using computer-generated random numbering, each of them included 42 patients:-
Control group (n = 42): - patients did not received any hemostatic drugs.
Tranexamic acid group (n = 42): - each patient received TXA loading dose of 6.4 mg/kg at the induction of anesthesia followed by a continuous infusion at a rate of 3 mg/kg/h for 24 h. This dose regimen of TXA was described by Grassin-Delyle et al.[12] in children with age older than 12 months and up to 12 years to maintain the therapeutic serum concentration of TXA at (20–30) μg/ml.
Combined (ethamsylate and TXA) group (n = 42):- each patient received a combination of TXA the same dose regimen as in the control group and intravenous ethamsylate 12.5 mg/kg every 6 h[13] starting at the induction of anesthesia and for 24 h postoperatively.
The surgical team and anesthetic management were the same for all patients. All patients received intramuscular ketamine 3 mg/kg, midazolam 0.15 mg/kg, and atropine sulfate 0.015 mg/kg, as premedication 30 min before induction of anesthesia. Pulse oximetry and five leads electrocardiography were attached to the patient. Anesthesia was induced with ketamine 2 mg/kg, fentanyl 5 ug/kg, and rocuronium 0.9 mg/kg and maintained with isoflurane 1% with oxygen in air, fentanyl (2–3) ug/kg/h, and rocuronium 0.5 mg/kg/h. An arterial catheter was inserted after complete aseptic condition either in the femoral or radial artery, and a central venous catheter was inserted into the right internal jugular vein guided by ultrasound with strict aseptic precautions.
All operations were done through the standard median sternotomy. Heparin 400 IU/kg was administered through the central venous catheter prior to cannulation to keep activated clotting time greater than 480 s. CPB was conducted after aorto-bicaval cannulation at normothermia (temperature 35°C or more) using a membrane oxygenator. Circuits of CPB were primed with (20–30) ml/kg, with the smallest priming volume 400 ml, Ringer's lactate, 25% albumin, sodium bicarbonate, mannitol, and packed red blood cells (packed RBCs) were added to the pump prime. Blood cardioplegia in a dose of (20–30) ml/kg was administered over (3–5) min after clamping aorta to preserve the myocardium, and half of this dose was given every 30 min until removal of aortic cross-clamp. The pump flow was maintained at (100–150) ml/kg/min to keep the mean arterial pressure at (40–70) mmHg. Hemofiltration was performed during CPB to maintain hematocrit of (25–30)' and (30–35)' just before weaning from CPB. After weaning off CPB protamine, sulphate was administered in a dose of 1 mg for each 100 IU heparin slowly over 10 min, if ACT was higher than the preoperative value by more than 20%, another dose of protamine was given.
After weaning from CPB, the following blood products were transfused and their volumes were recorded in ml/kg, packed RBCs if hemoglobin was less than 10 gm/dl or less than 25% of the preoperative value, platelet concentrate if platelets count was less than 100.000/uL, and fresh frozen plasma if there was excessive oozing from the wound or the site of chest tubes insertion. All patients were transferred to ICU while they were intubated and mechanically ventilated and managed by a separate ICU team.
Data collection
The following data were recorded in the operative theater: - sternal closure time (is the time from giving full dose protamine till closure of the sternum), needs for transfusion of blood and its products (whole blood, packed RBCs, fresh frozen plasma, and platelets concentrate), total dose of heparin, total dose of protamine, aortic cross-clamp time, CPB time, and total duration of surgery.
The postoperative data collected in ICU included the total amount of blood loss drained through mediastinal and pleural drainage tubes during the first 24 postoperative hours, the rate of blood loss every 6 h in the first postoperative 24 h (first 6 h, 6–12 h, 12–18 h, and 18–24 h), and the amount of the whole blood and its products (RBCs, platelets, and fresh frozen plasma) transfused to the patients during the first 24 postoperative hours. Extubation time, ICU length of stay, number of patients explored because of excessive bleeding or the clinical suspicion of cardiac tamponade, seizures, and any evidence of thromboembolic complications (stroke or paresis) were also recorded while the patient was still in the hospital. Hematocrit value, platelets count, and serum creatinine were measured after the first postoperative 24 h in ICU.
Statistical analysis
A sample size of 38 patients for each group was sufficient to detect 9 ml/kg reduction in blood loss the first postoperative 24 h as obtained from a previous study,[14] with the standard deviation of 14, a power of 80%, and a significance level of 5%. The number of patients in each group was increased to 42 patients to allow for 10% drop out rate.
IBM's Statistical Package for the Social Sciences statistics (SPSS) for Windows (version 25, 2017) was used for statistical analysis of the collected data. Shapiro-Wilk test was used to check the normality of the data distribution in continuous variables. Continuous variables were expressed as mean ± SD, whereas categorical ones were expressed as number and percentage. One-way Anova and Kruskal-Wallis tests were used to compare normally and abnormally distributed continuous variables with no follow-up readings, respectively. Repeated measures ANOVA model with Bonferroni post hoc test and 95% confidence interval to compare the follow-uP values of continuous data. Fisher exact test was used for inter-group comparison of nominal and ordinal data using the crosstabs function. Comparison of follow-up and basal values (intra-group) was conducted using Wilcoxon signed ranks test and McNemar test for ordinal and nominal data, respectively. All tests were conducted with 95% confidence interval. Charts were generated using SPSS' chart builder. P (probability) value <0.05 was considered statistically significant.
RESULTS
A total 126 patients were enrolled in this prospective study and were randomly classified into three groups: control group (n = 42); TXA group (n = 42); and combined ethamsylate TXA group (n = 42).
There were no statistically significant differences in patient's characteristics in the studied groups [Table 1].
Table 1.
Patients characteristics and the type of congenital heart disease of the studied groups
| Variables | Control G n=42 | Tranexamic G n=42 | Combined G n=42 | P |
|---|---|---|---|---|
| Age (months) | 33.7±30.1 | 33.8±24.1 | 37±27.1 | 0.951 |
| Sex | ||||
| Male (n & %) | 24 (57.2%) | 22 (52.4%) | 19 (45.2%) | 0.872 |
| Female (n & %) | 18 (42.8%) | 20 (47.6%) | 23 (54.8%) | 0.812 |
| Weight (Kg) | 16.8±6.8 | 18.5±7.2 | 17.4±7.5 | 0.861 |
| Height (cm) | 93.2±18.8 | 90.9±17 | 92.4±18.7 | 0.961 |
| Body surface area (m2) | 0.61±0.18 | 0.59±0.17 | 0.6±0.16 | 0.961 |
| Congenital heart disease | ||||
| Non-cyanotic patients (n & %) | 23 (54.8%) | 25 (59.5%) | 24 (57.2%) | 0.922 |
| Cyanotic patients (n & %) | 19 (45.2%) | 17 (40.5%) | 18 (42.8%) | 0.862 |
Data are expressed as mean±standard deviation (SD), number (n), and percentage (%). 1P was generated using one-way ANOVA. 2P was generated Cramer’s V Chi-square test
The total amount of blood loss in the first 24 postoperative hours in the combined ethamsylate TXA group was significantly smaller than the TXA and control groups [Figure 1]. The total amount of blood loss in the first 24 postoperative hours in the TXA group was significantly smaller than the control group [Figure 1].
Figure 1.
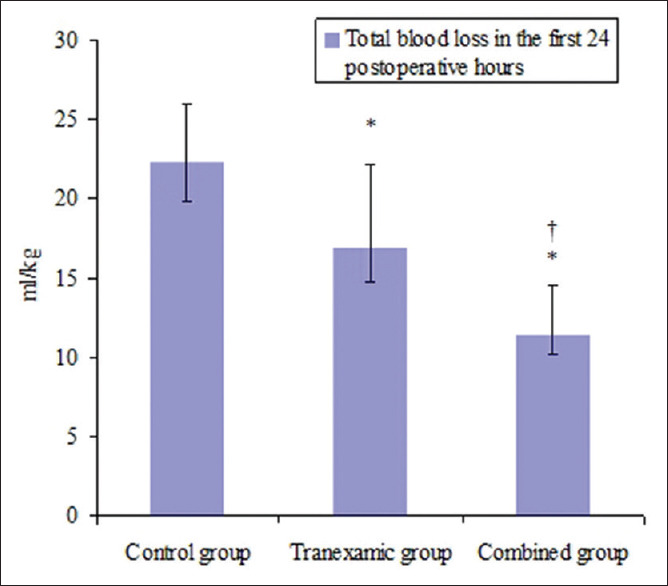
Total blood loss during the first postoperative 24 h. Data are expressed as mean ± standard deviation. P value was generated using repeated measure ANOVA. *P < 0.05 is significant when compared with the control group. †P < 0.05 is significant when compared with the tranexamic group
Figure 2 shows the rate of blood loss during the first 24 postoperative hours. The volume of blood loss was significantly smaller in the combined ethamsylate TXA group than TXA group after 6 h and at 6 to 12 h after surgery and than the control group after 6 hours, at 6 to 12 h and at 12 to 18 h after surgery. The amount of blood loss in the TXA group was significantly smaller than the control group after 6 h and at 6 to 12 h after surgery.
Figure 2.
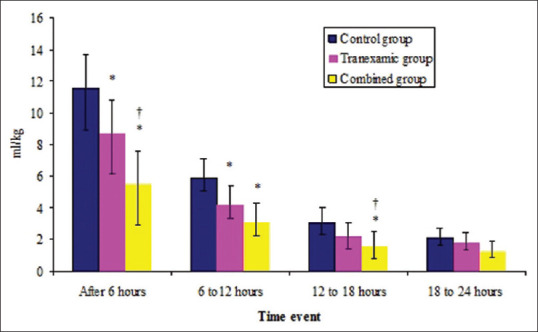
Blood loss during the first postoperative 24 h. Data are expressed as mean ± standard deviation. P value was generated using repeated measure ANOVA. *P < 0.05 is significant when compared with the control group. †P < 0.05 is significant when compared with the tranexamic group
The intraoperative variables (operative time, CPB time, aortic clamp time, total dose of heparin, and total dose of protamine) were comparable in the studied groups [Table 2]. The sternal closure time was significantly shorter in the combined ethamsylate TXA group than the other 2 groups [Table 2], and significantly shorter in TXA than the control group [Table 2].
Table 2.
Intraoperative variables
| Variables | Control G n=42 | Tranexamic G n=42 | Combined G n=42 | P |
|---|---|---|---|---|
| Operative time (hours) | 4.6±0.95 | 5±1.23 | 4.6±1.12 | 0.54 |
| CPB time (minutes) | 75.6±27.5 | 84.8±35.5 | 81.2±25.7 | 0.79 |
| Clamp time (minutes) | 52.2±17.9 | 58±26.7 | 56.5±20 | 0.83 |
| Total dose of heparin (IU/kg) | 497.8±55.5 | 502±54.4 | 497±40.3 | 0.97 |
| Total dose of protamine (mg/kg) | 4.9±0.59 | 5±0.57 | 4.9±0.4 | 0.88 |
| Sternal closure time (min) | 50±9.8 | 46.6±6.3* | 39.7±7.6*,† | 0.021 |
Data are expressed as mean±standard deviation (SD). CPB: cardiopulmonary bypass, P was generated using one-way ANOVA. *P<0.05 is significant when compared with the control group. †P<0.05 is significant when compared with the tranexamic group
The volume of whole blood transfused to patients in the combined ethamsylate TXA group during surgery and in the first postoperative 24 h was significantly smaller than the other 2 groups [Table 3]. The volume of whole blood transfused to patients in the TXA group during surgery was significantly smaller than the control group [Table 3]. There were no significant differences between the studied groups as regard to (packed RBCs, fresh frozen plasma, and platelets concentrate) transfused to the patients during surgery and in the first postoperative 24 h [Table 3].
Table 3.
Intra- and postoperative whole blood and blood products replacement therapy
| Variables | Control G n=42 | Tranexamic G n=42 | Combined G n=42 | P |
|---|---|---|---|---|
| Whole blood (ml/kg) | ||||
| Intraoperative | 22.9±2.7 | 18.3±3.2* | 15.6±2.9*,† | 0.004 |
| Postoperative | 15.9±3.9 | 14±3.3 | 9.6±1.6*,† | 0.003 |
| Packed RBCs (ml/kg) | ||||
| Intraoperative | 10.8±3.4 | 9.3±4.6 | 8.6±3.1 | 0.62 |
| Postoperative | 8.8±3.8 | 10.2±2.5 | 8.7.7±3.8 | 0.781 |
| Fresh frozen plasma (ml/kg) | ||||
| Intraoperative | 10.5±3.3 | 10.2±3.2 | 10.3±3.9 | 0.96 |
| Postoperative | 8.9±2.7 | 8.5±2.3 | 6.8±2.5 | 0.158 |
| Platelets concentrate (ml/kg) | ||||
| Intraoperative | 6.3±1.5 | 5.5±2.1 | 4.2±1.4 | 0.39 |
| Postoperative | 5.5±2.1 | 6.4±1.4 | 7.1±1.1 | 0.813 |
Data are expressed as mean±standard deviation (SD). RBCs: packed red blood cells. P was generated using one-way ANOVA. *P<0.05 is significant when compared with the control group. †P<0.05 is significant when compared with the tranexamic group
Time to extubation and ICU length of stay were comparable in the three studied groups [Table 4]. There were no significant differences between the three studied groups as regard the value of (hematocrit, platelets count, and serum creatinine) measured 24 h after surgery and the number of patients re-explored because of bleeding [Table 4]. There were no patients developed clinical seizures or thromboembolic complications (stroke or paresis) in the three studied groups [Table 4].
Table 4.
Intensive care unit postoperative variables, the value of hematocrit (%), S. creatinine (mg/dL), and platelets count/uL measured 24 h after surgery and postoperative complications (seizures and thrombo embolic complications)
| Variables | Control G n=42 | Tranexamic G n=42 | Combined G n=42 | P |
|---|---|---|---|---|
| Extubation time (h) | 18.2±7.5 | 14.8±7.7 | 13.3±6.6 | 0.3451 |
| ICU stay (h) | 53.7±14.4 | 50.6±15.7 | 51.7±10.8 | 0.8311 |
| Hematocrit (%) | 41.8±4.9 | 40.9±5.5 | 41.4±6.3 | 0.9381 |
| S. creatinine mg/dL | 0.46±0.1 | 0.48±0.12 | 0.51±0.08 | 0.4561 |
| Platelets count/uL | 259.8±79.9 | 231.8±63.1 | 241.2±90.1 | 0.7181 |
| Re exploration (n & %) | 1 (2.5) % | 0 (0) % | 1 (2.5) % | 0.8932 |
| Siezures (n & %) | 0 (0) % | 0 (0) % | 0 (0) % | ns |
| Thrombo embolism (n & %) | 0 (0) % | 0 (0) % | 0 (0) % | ns |
Data are expressed as mean±standard deviation (SD), number (n), and percentage (%). ICU: intensive care unit, ns: non significant. 1P was generated using one-way ANOVA. 2P was generated Cramer’s V Chi-square test
DISCUSSION
The main results of the current study showed that the combined use of ethamsylate and TXA in pediatric cardiac surgery was more effective in reducing sternal closure time, the postoperative blood loss, and whole blood transfusion requirements during surgery and in ICU than the use of TXA alone. The superiority of combined use of ethamsylate and TXA over TXA alone in reduction postoperative loss was not reflected in decrease in intra- and postoperative blood products requirements (packed RBCs, fresh frozen plasma, and platelets concentrate). The use of TXA alone significantly reduced intraoperative whole blood transfusion requirements, sternal closure time, and postoperative blood loss than the group.
There are few studies concerning the combined administration of ethamsylate and TXA to reduce postoperative blood loss. Hussain SH et al.[15] compared the effect of oral versus intravenous combination of ethamsylate and TXA on postoperative blood loss in adult patients submitted for mitral valve replacement. They found that both routes were effective in reducing blood loss through mediastinal and pleural drainage tubes to about (300–600) ml in the first postoperative 24 h, whereas the average blood loss reported by Bilecen S et al.[16] in patients not receiving any hemostatic drug was (400–1090) ml in the first postoperative 24 h.
Abdel Fatah et al. found that the combined use of intravenous ethamsylate and TXA significantly reduced postoperative blood loss in patients with a high risk of postoperative bleeding after lower segment cesarean section.[17]
Cobo-Nuñez MY et al. studied the effects of ethamsylate on the anticoagulant activity of heparin in both vivo and vitro.[18] They found that ethamsylate significantly reduced the elevated active prothrombin time and the increase in bleeding time induced by heparin. Cobo-Nuñez MY et al. concluded that ethamsylate administration interferes with the anti-coagulant activity of heparin in both vivo and vitro and this explains the significant reduction in sternal closure time, postoperative blood loss, and perioperative whole blood requirements in ethamsylate group when compared to TXA and the control groups.
In the current study, the use of TXA alone significantly reduced sternal closure time, intraoperative whole blood requirements, and blood loss in the first postoperative 24 h when compared to the control group. Zhang Y et al.[19] in their retrospective study that included 2,026 pediatric patients submitted for total correction of Tetralogy of Fallot, atrial, or ventricular septal defects reported that the administration of TXA was safe in pediatric cardiac surgery and was associated with a significant reduction of postoperative blood loss but not transfusion requirements when compared to the control group.
Giordano R et al. in their retrospective study that included both cyanotic and acyanotic pediatric patients submitted for open-heart surgery found a significant reduction in postoperative blood loss and packed RBCs requirements in the group of patients receiving TXA when compared to the control group.[20]
Shimizu K et al. in their randomized prospective study that included 160 pediatric patients (81 cyanotic and 79 acyanotic) undergoing cardiac surgery requiring CPB found that TXA administration was associated with a significant reduction in the amount of first 24 postoperative hours blood loss but not blood transfusion requirements when compared with the control group.[21]
In their retrospective study, Sampathkumar et al. reported that the use of high dose of TXA in small cyanotic children less than 10 kg is safe and effective in reducing blood loss and blood transfusion requirements after cardiac surgery.[6]
Chauhan et al. compared the effect of TXA and epsilon aminocaproic acid on the reduction of blood loss in the first postoperative 24 h and whole blood and its products requirements in children with congenital cyanotic heart disease undergoing cardiac surgery requiring CPB. They found that both TXA and aminocaproic acid had significantly shorter sternal closure time, lesser blood loss, and lesser whole blood and its products requirements.[14]
In the current study, no patients developed clinical seizures in the three studied groups, as we used the smallest dose of TXA described by Grassin-Delyle et al.[12] to maintain its serum therapeutic concentration. A retrospective study conducted by Couture P et al.[22] showed that the risk of seizures associated with TXA use in cardiac surgery was dose-dependent with increased risk at higher doses and decreased the risk at lower doses.
The results of the current study demonstrated that the combined intravenous administration of both TXA and ethamsylate in pediatric cardiac surgery was more effective in reducing postoperative blood loss and whole blood transfusion requirements than the use of TXA alone. Both drugs act by different mechanisms on hemostasis. Ethamsylate acts first, reducing capillary bleeding by promoting platelets adhesiveness and restoring capillary endothelial resistance.[11] Ethamsylate administration interferes with the anticoagulant activity of heparin;[18] therefore, it could counteract the residual effects of heparin after weaning from CPB. TXA is an antifibrinolytic drug that can prevent the breakdown of fibrin clot by binding to plasminogen.[23] Ethamsylate and TXA are complementary to each other during hemostasis, and the combined intravenous administration of both drugs could result in a synergistic effect on reduction of intra- and postoperative blood loss. The use of this combination could help to avoid high doses of TXA and its adverse effects.
CONCLUSION
The combined administration of TXA and ethamsylate in pediatric cardiac surgery was more effective in reducing postoperative blood loss and whole blood transfusion requirements in the first postoperative 24 h than the administration of TXA alone.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Robich MP, Koch CG, Johnston DR, Schiltz N, Chandran Pillai A, Hussain ST, et al. Trends in blood utilization in United States cardiac surgical patients. Transfusion. 2015;55:805–14. doi: 10.1111/trf.12903. [DOI] [PubMed] [Google Scholar]
- 2.Biancari F, Mikkola R, Heikkinen J, Lahtinen J, Airaksinen KE, Juvonen T. Estimating the risk of complications related to re-exploration for bleeding after adult cardiac surgery: A systematic review and meta-analysis. Eur J Cardiothorac Surg. 2012;41:50–5. doi: 10.1016/j.ejcts.2011.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cholette JM, Faraoni D, Goobie SM, Ferraris V, Hassan N. Patient blood management in pediatric cardiac surgery: A review. Anesth Analg. 2018;127:1002–16. doi: 10.1213/ANE.0000000000002504. [DOI] [PubMed] [Google Scholar]
- 4.Faraoni D, Rahe C, Cybulski KA. Use of antifibrinolytics in pediatric cardiac surgery: Where are we now? Paediatr Anaesth. 2019;29:435–4. doi: 10.1111/pan.13533. [DOI] [PubMed] [Google Scholar]
- 5.Myles PS, Smith JA, Forbes A, Silbert B, Jayarajah M, Painter T, et al. Tranexamic acid in patients undergoing coronary-artery surgery. N Engl J Med. 2017;376:136–48. doi: 10.1056/NEJMoa1606424. [DOI] [PubMed] [Google Scholar]
- 6.Sampathkumar SV, Raju V, Balakrishnan S, Moorthy SM, Arul A, Muthuswamy KS, et al. Efficacy of high dose tranexamic acid in decreasing bleeding after cardiac surgery for cyanotic congenital heart disease in children less than ten kilo body weight. World J Cardiovascular Surg. 2018;8:93–102. [Google Scholar]
- 7.Du Y, Xu J, Wang G, Shi J, Yang L, Shi S, et al. Comparison of two tranexamic acid dose regimens in patients undergoing cardiac valve surgery. J Cardiothorac Vasc Anesth. 2014;28:1233–7. doi: 10.1053/j.jvca.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 8.Suryakumari B, Parveen S. A comparative study of tranexamic acid versus ethamsylate used prophylactically in lower segment caesarean section- A prospective randomised double-blinded study. J Evid Based Med Health. 2017;4:4435–8. [Google Scholar]
- 9.Ramos-Sánchez TA, Ramos-Morales T, Morales-Avalos R, Blázquez-Saldaña J, Peña-Martínez VM, Vílchez-Cavazos F. Use of ethamsylate to reduce postoperative bleeding and transfusion index in total hip arthroplasty.A randomized clinical trial. Cir Cir. 2018;86:270–6. doi: 10.24875/CIRU.M18000043. [DOI] [PubMed] [Google Scholar]
- 10.Negrete OR, Molina M, Gutierrez-Aceves J. Preoperative administration of ethamesylate: Reduces blood loss associated with percutaneous nephrolithotomy.A prospective randomized study? J Urol. 2009;181:625. [Google Scholar]
- 11.Garay RP, Chiavaroli C, Hannaert P. Therapeutic efficacy and mechanism of action of ethamsylate, a long-standing hemostatic agent. Am J Ther. 2006;13:236–47. doi: 10.1097/01.mjt.0000158336.62740.54. [DOI] [PubMed] [Google Scholar]
- 12.Grassin-Delyle S, Couturier R, Abe E, Alvarez JC, Devillier P, Urien S. A practical tranexamic acid dosing scheme based on population pharmacokinetics in children undergoing cardiac surgery. Anesthesiology. 2013;118:853–62. doi: 10.1097/ALN.0b013e318283c83a. [DOI] [PubMed] [Google Scholar]
- 13.Schulte J, Osborne J, Benson JW, Cooke R, Drayton M, Murphy J, et al. Developmental outcome of the use of etamsylate for prevention of periventricular haemorrhage in a randomized controlled trial. Arch Dis Child Fetal Neonatal Ed. 2005;90:F31–5. doi: 10.1136/adc.2003.035790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chauhan S, Das SN, Bisoi A, Kale S, Kiran U. Comparison of epsilon aminocaproic acid and tranexamic acid in pediatric cardiac surgery. J Cardiothorac Vasc Anesth. 2004;18:141–3. doi: 10.1053/j.jvca.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 15.Hussain BS, Gaddam M, Srinivas G. Combination of oral versus intravenous formulation of tranexamic acid and ethamsylate in controlling postoperative bleeding of cardiac surgeries done under CPB. IRPMS. 2016;2:21–7. [Google Scholar]
- 16.Bilecen S, de Groot JA, Kalkman CJ, Spanjersberg AJ, Brandon Bravo Bruinsma GJ, Moons KG, et al. Effect of fibrinogen concentrate on intraoperative blood loss among patients with intraoperative bleeding during high-risk cardiac surgery a randomized clinical trial. JAMA. 2017;317:738–47. doi: 10.1001/jama.2016.21037. [DOI] [PubMed] [Google Scholar]
- 17.Abdel Fatah AT, El-Mohandes MI, Madany YA. Tranexamic acid and ethamsylate for reducing blood loss in patient undergoing LSCS at high risk for postpartum hemorrhage. Egypt J Hospital Med. 2018;73:6452–6. [Google Scholar]
- 18.Cobo-Nuñez MY, El Assar M, Cuevas P, Sánchez-Ferrer A, Martínez-González J, Rodríguez-Mañas L, et al. Haemostatic agent etamsylate in vitro and in vivo antagonizes anti-coagulant activity of heparin. Eur J Pharmacol. 2018;827:167–72. doi: 10.1016/j.ejphar.2018.03.028. [DOI] [PubMed] [Google Scholar]
- 19.Zhang Y, Zhang X, Shi J, Yuan S, Wang Y, Ran J, et al. Efficacy and safety of tranexamic acid in pediatric patients undergoing cardiac surgery: A single-center experience. Front Pediatrs. 2019;7:181. doi: 10.3389/fped.2019.00181. doi. org/10.3389/fped. 2019.00181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Giordano R, Palma G, Poli V, Palumbo S, Russolillo V, Cioffi S, et al. Tranexamic acid therapy in pediatric cardiac surgery: A single-center study. Ann Thorac Surg. 2012;94:1302–6. doi: 10.1016/j.athoracsur.2012.04.078. [DOI] [PubMed] [Google Scholar]
- 21.Shimizu K, Toda Y, Iwasaki T, Takeuchi M, Morimatsu H, Egi M, et al. Effect of tranexamic acid on blood loss in pediatric cardiac surgery: A randomized trial. J Anesth. 2011;25:823–30. doi: 10.1007/s00540-011-1235-z. [DOI] [PubMed] [Google Scholar]
- 22.Couture P, Lebon JS, Laliberté É, Desjardins G, Chamberland MÈ, Ayoub C, et al. Low-dose versus high-dose tranexamic acid reduces the risk of non ischemic seizures after cardiac surgery with cardiopulmonary bypass. J Cardiothorac Vasc Anesth. 2017;31:1611–7. doi: 10.1053/j.jvca.2017.04.026. [DOI] [PubMed] [Google Scholar]
- 23.McCormack PL. Tranexamic acid: A review of its use in the treatment of hyperfibrinolysis. Drugs. 2012;72:585–617. doi: 10.2165/11209070-000000000-00000. [DOI] [PubMed] [Google Scholar]


