Abstract
Objective: For patients with spinal cord injury (SCI) who undergo flap surgery to treat pressure injuries (PIs), the optimal duration of post-operative bedrest to promote healing and successful remobilization to sitting is unknown. At the study center, the minimum duration of post-operative bedrest was changed from 4 to 6 weeks. The purpose of this study is to compare outcomes of patients who underwent flap surgery using bedrest protocols of different duration.
Design: This was a retrospective review of all flap procedures completed at VA Puget Sound Health Care System from 1997 to 2016 to treat PIs in patients with SCI. Surgeries were excluded if they were not a flap (i.e. primary skin closure or graft), involved a non-pelvic region, or were a same-hospitalization revision of a prior surgery. The primary outcome of this investigation was the number of days between surgery and the first time the patient mobilized to sitting out of bed for 2 h with an intact surgical incision.
Methods: 190 patients received a total of 286 flap surgeries from 1994 to 2016. A chart review of each case was completed to determine the planned duration of bedrest (4- vs 6-weeks), first date of successful mobilization out of bed for 2 h, length of stay post-surgery, and occurrence of complications such as dehiscence or need for operative revisions.
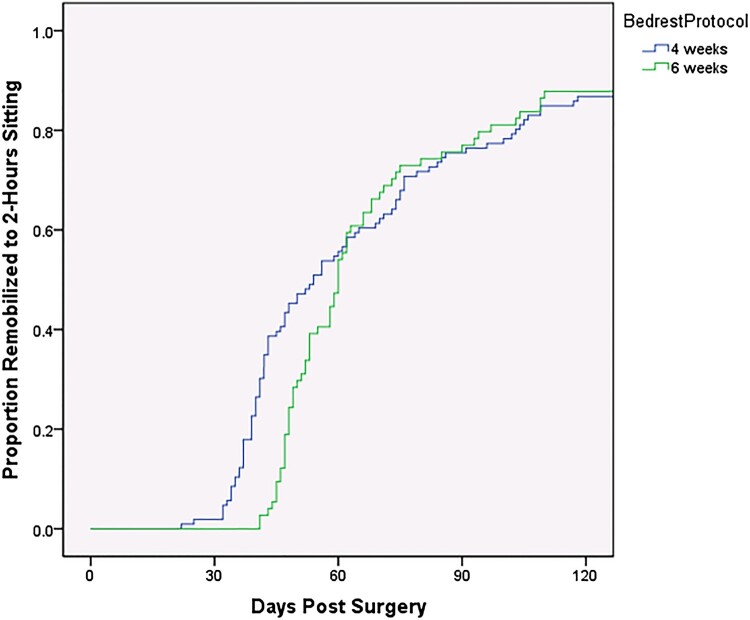
Results: Among 286 primary surgeries, 171 surgeries used the 4-week protocol and 115 used the 6-week protocol. When compared to the 4-week protocol, patients treated with the 6-week protocol were slightly older, more likely to have a diagnosis of diabetes, and less likely to be current smokers. Healing was never achieved after 4 surgeries in the 4-week group and 2 surgeries in the 6-week group. With the analysis restricted to a single surgery per subject who achieved healing (109 treated with 4-week protocol and 75 with 6-week protocol), there was a significant difference in days until 2-h sitting: median 54 days for the 4-week protocol compared to 60 days for the 6-week protocol (p = 0.041). Up to about 60 days post-operatively, the 4-week protocol produced a greater proportion remobilized to sitting, and thereafter the proportion of patients successfully remobilized did not differ between protocols.
Conclusions: The 6-week protocol was not associated with improved remobilization outcomes (reduced rates of dehiscence or surgical revisions), and the 4-week protocol resulted in a significantly shorter time to remobilization to sitting for 2 h as well as a shorter length of stay. We did not identify any subgroup of patients that benefited from the longer protocol.
Keywords: Spinal cord injury, SCI, Flap surgery, Flap protocol, Pressure injury, Decubitus ulcer
Introduction & background
There are an estimated 291,000 persons with traumatic spinal cord injury (SCI) in the U.S., with about of 17,730 new SCI cases each year.1,2 It is generally accepted that persons with SCI and related disorders are at the highest risk of developing pressure injuries (PIs). In the SCI population, the general lifetime incidence of developing a PI is estimated to be anywhere from 25 to 66%.3 A systematic meta-analysis of therapeutic interventions for PI after SCI found that the annual incidence of PI is 20–31%.4
The lack of volitional motor activity, absence of protective sensation, neurovascular impairment, lack of access to pressure-relieving equipment, and other medical comorbidities (i.e. diabetes, malnutrition, anemia, tobacco dependence) may place SCI individuals at high risk for development of PIs. Once a severe PI develops, surgical treatment may be necessary, requiring hospitalization and a greater utilization of medical services.
There have been efforts in the SCI literature to examine PI recurrences and complications following surgical reconstruction, as well as to analyze and determine best practice for post-flap surgical protocols to optimize outcomes and return to functional activities. In 1999, Goodman et al. reviewed 48 SCI Veterans who had surgical treatment of PIs and examined complication rates and related risk factors.5 In that study, the average time until the patient began a sitting program was 6.1 weeks, with patients spending an average of 11.2 weeks in the hospital setting. In another 1996 study at the University of Washington, Isik et al. in 1996 looked at 2- vs. 3-week protocols following PI surgery. There was no difference in the total hospital length of stay (LOS) between the two groups.6
In our literature review, recurrence (3–33%) and complication (6–53%) rates, post-operative protocol durations (3–6 weeks of complete bedrest), and surgical flap techniques (musculocutaneous, fasciocutaneous, and perforator approaches) have varied widely.7
At the VA Puget Sound Health Care System (VAPSHCS), SCI patients receiving flap surgery for PIs were previously treated with a post-flap bedrest protocol that lasted 4 weeks, comprised of 3 weeks of complete bedrest followed by 1 week of stretching (described in detail in “Materials & Methods” section below) but were transitioned in November 2006 to a 6-week protocol (5 weeks of bedrest followed by 1 week of stretching). The purpose of this study was to compare outcomes in patients from the 4-week protocol to those in the current 6-week protocol. We hypothesized that patients in the 6-week protocol group would have better outcomes compared to the 4-week protocol group. Hypothesized outcomes included a faster time to 2-h sitting due to less PI recurrence and flap failure rates, and/or that the 6-week protocol would be advantageous for certain patients who were slower to heal or considered high-risk.
Materials & methods
The study database included all surgical procedures performed at VAPSHCS by plastic surgery to treat PIs between 1994 and 2016. We excluded hospitalizations prior to 1997, the year when nursing staff began documenting in the electronic medical record (EMR). We also excluded all surgeries performed on patients who did not have SCI, all non-flap surgeries (such as primary closures and skin grafts), same-hospitalization surgical revisions, flap surgeries performed to treat PIs in non-pelvic region locations, and any surgery that did not have enough data on remobilization outcome. For this study, a surgical revision was defined as failure to heal from the initial surgery (the first surgery during the patient’s hospitalization), which then required a subsequent surgery for definitive closure during the same hospitalization.
A comprehensive chart review of the EMR was completed to determine the planned duration of bedrest (4 vs. 6 weeks), the number of days between surgery and successful remobilization × 2 h of sitting, and the rate of complications such as dehiscence or operative revisions. Low-frequency complications, including large hematomas (2), flap congestion (1) and severe epidermolysis (1) were combined with dehiscence events to reduce the number of post-operative complication categories for the analyses.
Subject demographics, ulcer location, select medical comorbidities, and flap surgeries prior to the study period were determined from chart review. Since definitions for neurological classifications changed and were not consistently applied over the study years, the neurological level as recorded in a locally maintained registry was used. Most patients did not have an American Spinal Injury Association Impairment Scale grade recorded in the registry, so this was omitted from analyses. In contrast, only 3% of patients had an unspecified neurological level.
The 4-week post-flap protocol used prior to November 2006 specified a minimum of 3 weeks of bedrest in an air-fluidized bed (Clinitron C-2 or Rite Hite). After 3 weeks, if the surgical incision was intact, the patient was transferred to a standard protective mattress surface. SCI PTs then evaluated the patient for tightness of the soft tissues near the surgical site. Tissue mobilization and progressive stretching was provided if needed until the patient could achieve at least 90 degrees of hip flexion, which typically required approximately 7 days. Once attained, the patient began remobilization to wheelchair sitting, first for 15 min followed by skin inspection for non-blanching erythema, blistering, or dehiscence. Sitting time was gradually advanced per the VAPSHCS SCI post-flap remobilization protocol (see Table 1).
Table 1. 4-week vs. 6-week protocol.
| Protocol | Bedrest on air-fluidized surface | Pre-mobilization: transition to non-air fluidized surface, scar mobilization, stretching to attain him range of motion | Progressive sitting up to 2 h (minimum days) ** | Minimum total days for post-flap remobilization |
|---|---|---|---|---|
| 4-week | 21 days | 7 days* | 10 days | 38 days* |
| 6-week | 35 days | 7 days | 10 days | 52 days |
* Although the 4-week protocol did not specify a minimum number of days for pre-mobilization, typically this phase took 7 days and was shorter only if there was no tension on the surgical incision with hip flexion for sitting, i.e. some trochanteric ulcer surgeries. Thus, for those small number of patients the minimum time for the 4-week protocol would be 31–38 days.
** Progressive sitting schedule: began with 15 min of sitting × 3 sessions; sitting time advanced by 15-min intervals until 1-h duration, then advanced by 30-min intervals. Mobilizations sessions were performed up to 2 times per day. The shortest time to achieve 2-h of sitting with this protocol was 10 days.
Beginning in November 2006, the period of strict bedrest was increased to 6 weeks (5 weeks on an air-fluidized surface, followed by 1 week on a standard protective mattress surface). During the final week of bedrest, SCI PTs performed similar evaluation and treatment with a progression schedule identical to what was used for the 4-week protocol (see Table 1). Each phase of the protocol could be paused or modified if the patient developed a dehiscence or did not meet criteria to advance. On occasion, providers shortened phases of the protocols, typically at the request of a patient.
The primary outcome was number of days between surgery and the first day of sitting for 2 h with an intact surgical incision. This outcome was chosen because we hypothesized that patients who were remobilized too early would develop wound dehiscence or minor blistering on the surgical incision soon after beginning the progressive sitting protocol. Also, this is typically the point at which the progressive sitting protocol was turned over from SCI PTs to inpatient SCI nursing staff. Of these surgeries, only a single patient who remobilized to sitting during hospitalization lacked enough documentation to determine the date of first sitting 2 h, and this patient was excluded from all analyses. For those patients who required surgical revision, our study used the interval of time from the initial surgery to time of sitting at 2 h following revision surgery or surgeries.
We initially intended to limit the analysis to patients who had completely healed and mobilized to sitting for 2 h prior to discharge. However, a larger than expected number of patients were discharged from the hospital prior to healing and remobilization in the earlier years studied. This occurred in approximately 9% of hospitalizations when using the 4-week protocol, vs. only 2% of hospitalizations when using the 6-week protocol. Therefore, we reviewed post-discharge medical records to estimate the date at which discharged patients had completely healed and remobilized to sitting, and this date was used to determine the primary outcome of days between surgery and remobilization to 2 h of sitting. We restricted the primary outcome analysis to one flap surgery per patient by randomly selecting one surgery for those patients who had multiple separate flap surgeries during the study period. The magnitude of the difference in primary outcome between the two protocols was only altered by one day when all surgeries were included, so for secondary outcomes we included all surgeries in those analyses.
Results
Between 1997 and 2016, 190 SCI patients underwent 286 non-revision flap surgeries to treat pelvic region PIs. At the time of each patient’s first surgery during the review period, mean age was 57.5 (SD 11.3) years, and injury duration was 18.7 (SD 12.9) years. SCI was due to traumatic etiology for 84.3% of patients. The neurological level was paraplegia for 58.4%, tetraplegia for 36.8%, and unspecified for 4.9%. At the time of the first surgery of the study period, 63.2% of patients had never had prior flap surgery, 15.1% had 1 prior flap surgery, 11.9% had 2 prior flap surgeries, and the remaining 9.6% had 3 or more prior flap surgeries. During the years reviewed for this study, 51.4% of patients received a single flap surgery, 28.6% received two, 15.7% received three, and 4.3% received four or more flap surgeries. A total of 34 primary surgeries required surgical revision during the same hospitalization, including some primary surgeries that received multiple same-hospitalization revisions. For surgeries requiring revision, the time until remobilization was calculated from the date of the first surgery until remobilization after any subsequent revision surgeries.
Table 2 shows characteristics of the 286 surgeries treated with the 4-week vs. 6-week protocol. Of these surgeries, 171 used the 4-week protocol and 115 used the 6-week protocol. Compared to the 4-week protocol, surgeries using the 6-week protocol included patients with slightly greater age (3.5 years older), less frequent use of tobacco in the month prior to surgery (17.4% vs. 50.3%), and higher prevalence of diabetes (32.2% vs. 14.0%). Assessed characteristics were otherwise similar between the 2 patient groups, as shown in Table 2.
Table 2. Protocol used for 286 flap surgeries.
| Factor | 4-week protocol (n = 171) | 6-week protocol (n = 115) | P value (and test used) |
|---|---|---|---|
| Age | 55.8 +/– 11.3 | 59.3 +/– 11.4 | 0.01 (T-test) |
| Injury duration | 19.3 +/– 12.2 | 20.6 +/– 14.1 | 0.44 (T-test) |
| Injury level Tetraplegia Paraplegia | 67 (39.6%) 102 (60.4%) | 43 (37.4%) 58 (50.4%) 5 (4.3%) 1 (0.9%) 8 (7.0%) 43 (40.2%) 64 (59.8%%) | p = 1.0 (Fisher’s exact test) |
| Etiology Traumatic Non-traumatic | 147 (86.0%) 24 (14.0%) | 101 (87.8%) 14 (12.2%) | p = 0.72 (Fisher’s exact test) |
| BMI | 24.5 +/– 5.5 | 25.4 +/– 5.3 | 0.18 (T-test) |
| Smoking | 86 (50.3%) | 20 (17.4%) | <0.001 (Fisher’s Exact Test) |
| Diabetes | 24 (14.0%) | 37 (32.2%) | <0.001 (Fisher’s Exact Test) |
| Albumin <3.5 | 73/160 (45.6%) | 45/111 (40.5%) | 0.39 (Fisher’s exact test) |
| Ulcer location Ischium Sacrum Trochanter Other pelvic | 90 (52.6%) 49 (28.7%) 27 (15.8%) 5 (2.9%) | 63 (54.8%) 31 (27.0%) 15 (13.0%) 6 (5.2%) | 0.70 (Chi-Square test) |
| Multiple surgeries on same day | 14 (8.1%) | 12 (10.4%) | 0.54 (Fisher’s Exact Test) |
| Multiple surgeries in same hospitalization (*excludes revision surgeries) | 20 (11.7%) | 12 (10.4) | 0.85 (Fisher’s Exact Test) |
| Surgery performed to treat ulcer recurrence | 32 (18.7%) | 20 (17.4) | 0.88 (Fisher’s Exact Test) |
Table 3 shows the outcomes for the 4-week and 6-week protocols. For these outcomes, surgeries that did not result in eventual complete healing and remobilization (4/171 with 4-week protocol and 2/115 with 6-week protocol) are excluded from the outcomes for days until achieving remobilization and days until discharge. When the analysis was restricted to only one randomly selected surgery per patient who eventually healed, the median days between surgery and remobilization to 2 h sitting was 6 days longer for the 6-week protocol (54 vs. 60 days; p = 0.041). If multiple separate flap surgeries per patient were included in the analysis, across all surgeries there was a similar difference in medians of 5 days (54 vs. 59 days; p = 0.019), favoring the 4-week protocol.
Table 3. Outcomes by Protocol Duration (n = 286 surgeries; for surgeries that required revisions, the days from initial surgery until healed post-revision is used for duration. Patients who never achieved remobilization are excluded from some analyses – see text).
| 4-week | 6-week | Difference (6 vs. 4 week) | p | |
|---|---|---|---|---|
| Days from surgery to 2 h sitting – each subject included only once (random) | 54 median (IQR = 54)(n = 109) | 60 median (IQR = 37)(n = 75) | +6d | 0.041 (Mann–Whitney U test) |
| Days from surgery to 2 h sitting – subject included more than once | 54 median (IQR = 46)(n = 167) | 59 median (IQR = 28)(n = 113) | +5 d | 0.019 (Mann–Whitney U test) |
| Days from surgery to discharge – | 70 median (IQR = 60)(n = 167) | 78 median (IQR = 44)(n = 113) | +8 d | 0.019 (Mann–Whitney U Test). |
| Dehiscence rate | 88/171 (51.5%) | 66/115 (57.4%) | +5.9% | 0.34 (Fisher’s Exact Test) |
| Revision surgery performed during hospitalization | 24/171 (14.0%) | 10/115 (8.7%) | –5.3% | 0.20 (Fisher’s Exact Test) |
| Rate of recurrence during first year post-surgery (excluding deceased, lost to follow-up, or never healed) | 46/157 (29.3%) | 22/111 (19.8%) | –9.5% | 0.089 (Fisher’s Exact Test) |
In Figure 1, we demonstrate that prior to about 60-days post-surgery, a larger proportion of patients treated with the 4-week protocol were successfully remobilized, whereas after 60 days the rate of successful remobilization was similar for the two protocols.
Figure 1.
Survival curves showing proportion of population healed and sitting 2 h over the first 4 months post-surgery. Each subject included once.
When length of stay between surgery and discharge was considered (Table 3), median days until discharge was 8 days shorter with the 4-week protocol. There were no significant differences in rates of dehiscence or revision surgery between 4- and 6-week protocols. There was a trend (p = 0.089) favoring a lower 1-year recurrence rate when using the 6-week protocol, with no significant difference in the number of days until recurrence within the first year. Regarding 1-year recurrence rates, a very small proportion had an inadequate follow-up: healed but deceased within 1 year (n = 8); never healed within 1 year of surgery (n = 6); or lost to follow-up (n = 4).
Injury duration, paraplegia vs. tetraplegia, BMI, diabetes, and prior PI at the site did not show a signification association with number of days remobilized to sitting for 2 h. A low preoperative albumin was associated with increased days until sitting 2 h (median 52.5 days [IQR = 33] with albumin >=3.5, vs. 64.5 days [IQR = 54] with albumin <3.5; p = 0.005, Mann–Whitney U Test). However, there was no evidence that those with low albumin benefited from the 6-week bedrest protocol, as days until remobilization for 2 h did not differ significantly for those patients between the 4-week and 6-week protocols (median 64.5 vs. 63.5 days; p = 0.51).
Discussion
Our findings demonstrate that for patients with SCI undergoing flap surgery for PIs, the median days between surgery and remobilization to 2 h sitting was at least 5 days faster for the 4-week protocol compared to the 6-week protocol.
The graphical display of healing as survival curves demonstrates that at around 60 days both the 4-week and 6-week protocols had about one-third of patients who had still not yet remobilized. These patients had delay in successful remobilization, typically due to surgical incision dehiscence which in some cases required revision surgery. The data did not show any significant differences in other outcomes between 4-week and 6-week protocols, including dehiscence rates, frequency of same-hospitalization revision surgeries, and 1-year recurrence rates, so there is not likely an added benefit of the additional 2 weeks of bedrest. There was a trend towards lower 1-year recurrence in the 6-week protocol with a rate that was one-third lower than the 4-week protocol, but this was not statistically significant. The length of stay from surgery to discharge was also decreased by 8 days in the 4-week protocol when looking at patients who healed before leaving the hospital. The only notable differences in our populations were that the 6-week protocol patients were slightly older, and had higher prevalence of diabetes, which we postulate may be related to greater vigilance in screening and detecting diabetes, or a change in diagnostic criteria, and not a true change in prevalence of this magnitude. The lower prevalence of tobacco use during the 6-week protocol likely reflects changes in preoperative requirements, as patients are now required to be tobacco-free for 30 days prior to flap surgery.
With this information, we also wanted to determine if there were any specific subgroups that could benefit from a longer bedrest protocol. However, injury duration, paraplegia vs. tetraplegia, BMI, diabetes, low albumin, and prior PI at the same site were not significantly associated with reduced time to successful remobilization when the longer bedrest protocol was used.
This study compared different lengths of bedrest protocols after flap surgeries in patients with SCI. Other studies have used different lengths of bedrest, and the ideal length of time has remained unclear. However, our study has shown that 4 weeks is sufficient in most cases compared to a longer period of 6 weeks. It may be useful to further compare other lengths of immobilization (i.e. 3 or 5 weeks) to 4 weeks to determine an ideal length of bedrest before mobilization.
There were several limitations to this study. First, this was not a randomized-controlled trial, where we assigned patients to a 4- or 6-week protocol group controlling for all other variables. Second, many treatment variables in the treatment of PIs pre- or post-flap surgery have changed over time (i.e. treatment of osteomyelitis with antibiotics, stretching and range of motion programs, seating prescription, and bed/mattress surface availability). Another limitation of this study was that for many patients, the completeness of SCI was not known. It may be helpful to review the ASIA International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) to determine completeness of injury, as that could help describe the individual’s ability to mobilize and pressure-relieve, depending on their level of available volitional motor activity and protective sensation. Also, a limitation was that for patients discharged prior to healing, we reviewed post-discharge medical records to estimate the date at which discharged patients had completely healed. Outpatient notes were less frequently written than inpatient notes resulting in less precision on exact healing dates. Lastly, our patient population, which included only Veterans, who are primarily older males, may limit the generalizability of our findings.
Despite the above limitations of our study, we aimed to identify an optimal post-flap protocol duration for SCI individuals undergoing flap surgery. The importance of having a successful post-flap protocol cannot be underestimated. Previous research has shown that SCI individuals with PIs are substantially more dissatisfied with their ability to participate in their primary activities that they value or spend most of their time doing when compared to SCI individuals without PIs. With SCI, PIs adversely affected participation in 19 of 26 daily and community activities compared to having SCI without PI.8 These findings show that having a PI has a significant impact in activity participation and therefore quality of life.
Finally, a study by Kierney et al. highlighted the importance of the multidisciplinary team approach in caring for post-flap patients and opined that this collaboration led to an overall low recurrence rate and high percentage of patients who manifested long-term maintenance of skin integrity.9 Our study included several treatment variables in the treatment of PIs with flap surgery and involved multiple members of the interdisciplinary rehabilitation and surgical team. Many disciplines are involved in the treatment of PIs and the collaborative approach to care is tantamount to the successful return of the SCI patient to function.
Conclusion
Our study aimed at developing a best practice for rehabilitation management and remobilization of individuals with SCI after definitive surgical management of neurogenic PIs. Based on our study’s findings, there is no clear benefit of the 6-week remobilization protocol over the 4-week remobilization protocol for most patients.
Further analysis and research may help delineate variables contributing to these differences, and to help identify characteristics of high-risk patients whom should undergo the 6-week post-flap protocol. Pursuing this knowledge will help ensure optimal outcomes, guide best practice, decrease PI recurrence, lessen hospital length of stay, and improve medical costs and resource utilization.
Given these findings, returning to a 4-week protocol for most patients seems prudent as an additional 2 weeks of bedrest and hospitalization has significant added financial costs and may have implications on patients’ mood, quality of life, and likelihood of hospital-associated complications, such as infections, delirium, or deep vein thromboses.
Disclaimer statements
Contributors None.
Funding None.
Conflict of interest Authors have no conflict of interest to declare.
References
- 1.National Spinal Cord Injury Statistical Center . Facts and Figures at a Glance. Birmingham, AL: University of Alabama at Birmingham; 2019. Data Source: Jain NB, Ayers GD, Peterson EN, et al. Traumatic spinal cord injury in the United States, 1993-2012. JAMA. 2015;313(22):2236-43. [DOI] [PMC free article] [PubMed]
- 2.National Spinal Cord Injury Statistical Center . Facts and Figures at a Glance. Birmingham, AL: University of Alabama at Birmingham; 2019. Data Source: Lasfargues JE, Custis D, Morrone F, Carswell J, Nguyen T. A model for estimating spinal cord injury prevalence in the United States. Paraplegia. 1995;33(2):62-68. [DOI] [PubMed]
- 3.Kruger EA, Pires M, Ngann Y, Sterling M, Rubayi S.. Comprehensive management of pressure ulcers in spinal cord injury: current concepts and future trends. J Spinal Cord Med. 2013 Nov;36(6):572–585. doi: 10.1179/2045772313Y.0000000093. Epub 2013 May 21. PMID:24090179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Regan MA, Teasell RW, Wolfe DL, Keast D, Mortenson WB, Aubut JA; Spinal cord injury rehabilitation evidence research team. A systematic review of therapeutic interventions for pressure ulcers after spinal cord injury. Arch Phys Med Rehabil. 2009 Feb;90(2):213–31. PMID:19236976 doi: 10.1016/j.apmr.2008.08.212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goodman CM, Cohen V, Armenta A, Thornby J, Netscher DT.. Evaluation of results and treatment variables for pressure ulcers in 48 veteran spinal cord-injured patients. Ann Plast Surg. 1999 Jun;42(6):665–72. PMID: 10382806. doi: 10.1097/00000637-199906000-00015 [DOI] [PubMed] [Google Scholar]
- 6.Isik FF, Engrav LH, Rand RP, Kierney P, Cardenas DD.. Reducing the period of immobilization following pressure Sore surgery: a prospective, randomized trial. Plast Reconstr Surg. 1997 Aug;100(2):350–4. PMID:9252601. [DOI] [PubMed] [Google Scholar]
- 7.Sameen M, Au M, Wood T, Farrokhyar F, Mahoney J.. A systematic review of complications and recurrences in flaps for pressure sores. Plast Reconstr Surg 2012 Jul;130(1);67e–77e. PMID:22743956. doi: 10.1097/PRS.0b013e318254b19f [DOI] [PubMed] [Google Scholar]
- 8.Jordan SW, De la Garza M, Lewis, Jr VL.. Two-stage treatment of ischial pressure ulcers in spinal cord injury patients: technique and outcomes over 8 years. J Plast Reconstr Aesthet Surg. 2017 Jul;70(7):959–66. Epub 2017 Jan 23. PMID: 28285012. doi: 10.1016/j.bjps.2017.01.004 [DOI] [PubMed] [Google Scholar]
- 9.Kierney PC, Engrav LH, Isik FF, Esselman PC, Cardenas DD, Rand RP.. Results of 268 pressure sores in 158 patients managed jointly by plastic surgery and rehabilitation medicine. Plast Reconstr Surg. 1998 Sep;102(3):765–72. PMID:9727442. doi: 10.1097/00006534-199809010-00022 [DOI] [PubMed] [Google Scholar]