Supplemental Digital Content is Available in the Text.
Participation and adherence rates of cardiac rehabilitation (CR) remain low. This study investigated reasons for nonattendance and noncompletion. Our results show that reasons were mostly motivational or perceptive based indicating possible misconceptions or inferior knowledge regarding CR. To increase uptake and completion of CR, adequate motivation, information, and more personalized solutions are needed.
Keywords: cardiac rehabilitation, compliance, participation, secondary prevention
Abstract
Purpose:
Despite strong recommendations and beneficial health effects of cardiac rehabilitation (CR), participation rates remain low. Little data are available on reasons beyond quantitative factors in the underutilization of CR. The aim of this study was to identify personal reasons for nonattenders and noncompletions of CR among Dutch and German patients with cardiovascular diseases (CVD) eligible for CR.
Methods:
Between December 2017 and January 2019, a total of 4265 questionnaires were distributed among eligible patients for CR in the bordering area of the eastern Netherlands and western Germany. Patients were eligible if they had an indication for CR according to national guidelines. Questionnaires were used to assess reasons of nonattendance and noncompletion of CR, when applicable.
Results:
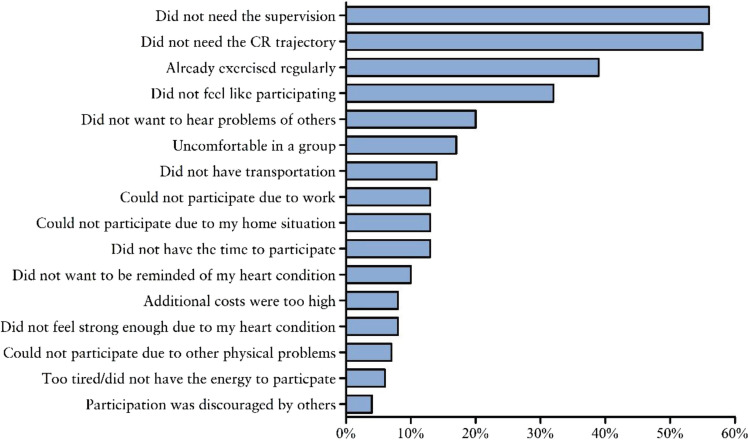
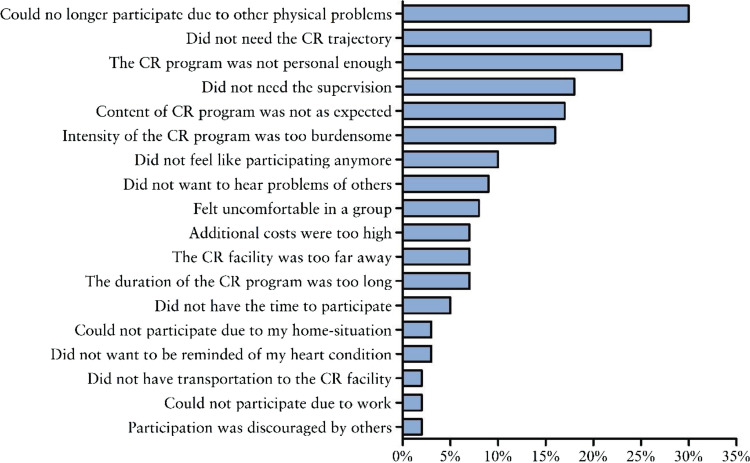
A total of 1829 patients with CVD completed the questionnaire. Of these, 1278 indicated that they received referral to CR. Despite referral, 192 patients decided not to participate in CR and 88 patients with CVD withdrew from the CR program. The three most reported reasons for nonattendance were as follows: (1) did not need the supervision (56%, n = 108), (2) did not need the CR trajectory (55%, n = 105), and (3) already exercised regularly (39%, n = 74). The most reported reasons for noncompletion were as follows: (1) could no longer participate because of other physical problems (30%, n = 26), (2) did not need the CR trajectory (26%, n = 23), and (3) the CR program was not personal enough (23%, n = 20).
Conclusions:
Most patients had motivational or perceptive reasons for nonattendance or noncompletion to CR. These possible misconceptions as well as perceived shortcomings of traditional CR underline the need for adequate motivation, information, and more personalized solutions (eg, eHealth, home-based CR) to increase the uptake and completion of CR.
Cardiovascular diseases (CVD) affect >85 million people across Europe.1 The development of medical technology and treatment of patients with CVD have resulted in increased survival in recent decades.2 Hence, secondary prevention is important to reduce the burden of CVD and to optimize disability-free survival.3
Cardiac rehabilitation (CR) is an evidence-based strategy to change high-risk behavior, such as physical inactivity, unhealthy diet, tobacco consumption, and being overweight or obese.4 Contemporary CR programs are multifaceted and include group-based exercise training, lifestyle modification therapy, and individual counseling when indicated (eg, consulting a psychologist or dietician). Previous studies found significant reductions in all-cause mortality, CVD mortality, unplanned hospitalization, and reinfarctions among CVD patients participating in CR.5–7 Hence, CR participation is a class I recommendation in current guidelines of European and American cardiovascular societies.8–10
Despite these strong recommendations and beneficial effects, CR participation rates remain low. The European Cardiac Rehabilitation Inventory Survey revealed that <50% of eligible CVD patients are participating in CR in Europe, with considerable variance between countries.11,12 In addition, recent studies have shown that patient adherence to CR differs considerably between countries with a dropout rate ranging from 12-56%.13,14
A number of quantitative factors are known to influence nonattendance or noncompletion of CR such as sociodemographic factors, diagnosis, treatment, infrastructure-related factors, and low referral rates.15–17 However, there is little research that investigates the role of personal reasons and perception in the underutilization of CR. To date, only a small number of studies among few CR patients investigated the individual-reported reasons for nonattendance and/or noncompletion. These studies showed that patients often believe that they can solve their problems themselves, did not find the motivation to participate, or had other personal (family related) duties.18–21 These studies are limited, however, by small sample sizes, heterogenous data collection techniques, and methodologies, and it remains unknown whether the reported reasons are universal and applicable to all CVD patients. To improve attendance and completion of CR, a better overall understanding of the reasons for nonattendance and noncompletion is needed.
This study aimed to identify personal reasons for nonattendance and noncompletion in a large group of CVD patients eligible for CR. For this purpose, a multicenter two-country quantitative approach using questionnaires was chosen.
METHODS
STUDY DESIGN/RECRUITMENT
Questionnaires were distributed to cardiac patients eligible to enroll in CR in the bordering area of the eastern Netherlands and western Germany. Dutch patients were enrolled by one urban and two community hospitals and through an ongoing large-population based study.22 In Germany, cardiac patients were enrolled in the North Rhine-Westphalia area by a large health insurance company (AOK Rheinland/Hamburg), which covers approximately one-third of the total German population.23
PARTICIPANTS
Patients in the Netherlands were eligible if they had an indication for CR according to the Dutch guidelines.24 For this study, both absolute and relative indications were included. Absolute indications included acute coronary syndrome, stable angina pectoris, percutaneous coronary intervention, and coronary artery bypass grafting. Relative indications included heart failure, congenital heart disease, cardiac transplants, implantable cardioverter defibrillator or pacemaker implants, arrhythmia, valve surgery, and other cardiothoracic surgery. In Germany, patients were eligible if they were diagnosed with an ischemic heart disease (code: I20-I25) according to the International Classification of Diseases, Tenth Revision (ICD-10, Version: 2016). Dutch patients were recruited by their treating cardiologist, whereas German patients were approached directly by the health insurance company based on ICD code.
CR PROGRAM
Cardiac rehabilitation protocols in Germany and the Netherlands had slight variations in setting/organization. In the Netherlands, CR was solely outpatient and consisted of several group-based therapies within policlinics for several hr/wk for 6-12 wk while patients stayed in their home environment.25 German CR programs can be inpatient or outpatient, depending on their preference and recommendation. Inpatient CR programs consist of a 3-wk course in which patients follow daily sessions such as exercise and lifestyle.26 Outpatient CR programs last 6-12 wk and consist of group-based therapies within policlinics while patients stayed in their home environment. Although the content of the CR programs had slight variation between locations in both countries, all programs consisted of four main goals: physical, psychological, social, and changing high-risk behavior.
QUESTIONNAIRE AND DATA COLLECTION
Between December 2017 and January 2019, questionnaires were sent out to eligible patients. Patients received either a personal invitation by e-mail to fill in a web-based questionnaire regarding CR or a paper version of the questionnaire. Alongside the questionnaire, there was an (digital) invitation letter in which the rationale, purpose, and procedure of the study were explained. Because of the study setup, no information of nonresponders could be collected. Paper version was manually entered into the online-secured database. The content of the survey was developed in close collaboration with cardiac patients, members of the CVD patient organization, researchers, and health care professionals. Using focus groups, the personal experience for nonattendance and noncompletion was collected by the researcher from patients, health care professionals, and members of the CVD patient organization. Hereafter, the most important reasons were summarized and coded into the questions used in the questionnaire. The survey involved questions ranging from binary (yes/no), four-point Likert scales, prescribed selection, and open-ended questions. The first part of the questionnaire collected information on personal characteristics such as age, sex, nationality, involved hospital, living situation, level of education, and employment status. The second part contained questions on details of their cardiac disease and the received information on CR. The third part was either focused on reported factors for nonattendance or noncompletion dependent on participation and attendance. Patients who did not participate in CR or dropped out during CR received a list of predetermined reasons and were asked to indicate to what extent each reason was applicable to their situation on a four-point Likert scale varying from strongly agree to strongly disagree.
DATA ANALYSIS
To identify reported personal reasons for nonattendance and noncompletion, we defined the following groups: (1) patients who received referral and started CR (attendees) and (2) patients who received referral but chose not to participate (nonattenders). Hereafter, the attendees group was divided into the follow subgroups: (3) patients who started CR but withdrew during the program (noncompleters), and (4) patients who completed the CR program (completers). Demographic characteristics were determined for attendees, nonattenders, completers, and noncompleters. Categorization of educational status was classified in high, middle, and low, based on the highest completed education (according to school system used in the Netherlands and Germany). Characteristics were checked for normal distribution by the Shapiro-Wilk normality test and visual inspection and reported as mean ± SD or median (IQR) and as counts (%) for categorical variables. Differences in characteristics between attendees and nonattenders and between completers and noncompleters were determined by an independent t test for continuous variables and χ2 test for categorical variables. Reasons for nonattendance and noncompletion were reported as descriptive statistics. All of the reasons were mentioned at least once. The two open-ended questions regarding an additional reason for nonattendance/noncompletion and additional information were collected and analyzed separately by two researchers. These questions were coded as reasons if they overlapped with any previous questions regarding reasons for nonattendance or noncompletion of the CR program and included in the total count if the reasons were not selected previously by the participant. Exploratory stratified analyses were performed to investigate possible differences in reported reasons between the two countries. However, due to differences in recruitment and response rates, no direct statistical comparison could be made between Dutch and German respondents. Data processing and statistical analyses were performed using SPSS Version 24 (IBM Corp).
RESULTS
A total of 4265 questionnaires were sent: 2000 in Germany and 2265 in the Netherlands (see Supplemental Digital Content 1, available at: http://links.lww.com/JCRP/A255). The overall response rate was 43%, resulting in a total of 1829 completed questionnaires. The majority of the returned questionnaires originated from the Netherlands (74%). Of all respondents, 1278 patients (70%) indicated to have received referral for CR. A total of 192 patients (15%) decided not to participate in CR despite referral. Of the 1086 attendees, 88 patients (8%) did not complete the CR program.
CHARACTERISTICS FOR NONATTENDANCE
The Table presents an overview of nonattenders and attendees characteristics. Mean age was 66 ± 11 yr in both groups. The majority of the nonattendance group was male (64%) and contained 10% more females compared with the attendees group (P = .005). On average, nonattenders had a lower education level than attendees (46 vs 38%) while the majority of patients in both groups were retired (53 vs 52%) and living with a significant other (82 vs 75%). Almost one-third of the nonattenders (29%) suffered from myocardial infarction, compared with 46% of the attendees (P < .001).
Table. Characteristics of Attendees Versus Nonattenders and Completers Versus Noncompletersa.
| Attendees (n = 1086) | Nonattenders (n = 192) | P Value | Completers (n = 998) | Noncompleters (n = 88) | P Value | |
|---|---|---|---|---|---|---|
| Characteristics | ||||||
| Age, yr | 66 ± 11 | 66 ± 10 | .37 | 65 ± 11 | 68 ± 9 | .008 |
| Male | 797 (74) | 121 (64) | .005 | 732 (74) | 65 (74) | .96 |
| Education | .06 | .018 | ||||
| High/academic | 371 (34) | 51 (27) | 340 (34) | 31 (35) | ||
| Intermediate | 279 (26) | 47 (25) | 266 (27) | 13 (15) | ||
| Low | 412 (38) | 88 (46) | 368 (37) | 44 (50) | ||
| Missing | 24 (2) | 6 (3) | 24 (2) | 0 (0) | ||
| Occupation | .012 | .09 | ||||
| Housewife | 58 (5) | 22 (12) | 54 (5) | 4 (5) | ||
| Working | 332 (31) | 50 (26) | 315 (32) | 17 (19) | ||
| Retired | 576 (53) | 99 (52) | 520 (52) | 56 (64) | ||
| Other | 118 (11) | 20 (10) | 107 (11) | 11 (13) | ||
| Missing | 2 (0) | 1 (1) | 2 (0) | 0 (0) | ||
| Living situation | .10 | .21 | ||||
| Alone | 175 (16) | 42 (22) | 157 (16) | 18 (20) | ||
| Together | 888 (82) | 145 (75) | 818 (82) | 70 (80) | ||
| Other | 20 (2) | 5 (3) | 20 (2) | 0 (0) | ||
| Missing | 3 (0) | 0 (0) | 3 (0) | 0 (0) | ||
| Heart disease | <.001 | .86 | ||||
| Myocardial infarction | 497 (46) | 56 (29) | 455 (46) | 42 (48) | ||
| Angina pectoris | 189 (18) | 43 (22) | 173 (17) | 16 (18) | ||
| Other | 388 (36) | 92 (48) | 359 (36) | 29 (33) | ||
| Missing | 12 (1) | 1 (1) | 11 (1) | 1 (1) | ||
| Cardiac rehabilitation | ||||||
| Distance to center, km | 19 ± 32 | 25 ± 47 | .10 | 18 ± 31 | 22 ± 41 | .41 |
aData presented as mean ± SD or n (%).
REASONS FOR NONATTENDANCE
Figure 1 provides an overview of the patient-reported reasons for nonattendance. More than half of the respondents replied with the reason “Did not need the supervision” (56%, n = 108) and/or “Did not need the CR trajectory” (55%, n =105). Another 61 patients (32%) replied “Did not feel like participating,” despite referral. The group aspect of the CR program was a recurring theme with approximately 20% of the respondents reporting one or both of the following reasons: (1) “Did not want to hear problems of others” (n = 39) and (2) “Uncomfortable in a group” (n = 32). Practical reasons such as “Did not have transportation” (14%, n = 26), “Did not have the time to participate” (13%, n = 24), and “Could not participate due to work” (13%, n = 24) were less reported reasons for nonattendance. In addition, we performed exploratory stratified analysis of subcategories but did not find any significant differences in the reasons for nonattendance for sex, education level, or age.
Figure 1.
Reasons (multiple answers were possible) for nonattendance of CR despite receiving a referral from treating physician and/or nurse. Data are presented per reason as (%) of total number of nonparticipants (n = 192). Abbreviation: CR, cardiac rehabilitation. This figure is available in color online (www.jcrpjournal.com).
CHARACTERISTICS AND REASONS FOR NONCOMPLETION
The Table summarizes the characteristics of completers and noncompleters. In total, 998 CVD patients completed the CR program and 88 patients initiated CR but did not complete the program. Noncompleters were on average 3 yr older than completers (P = .008) and 74% of both groups were male. Of all noncompleters, 50% had low education level compared with 37% of the completers (P = .018). Occupation, living situation, and heart-disease diagnosis were similar between groups (see Supplemental Digital Content 2, available at: http://links.lww.com/JCRP/A256, and Supplemental Digital Content 3, available at: http://links.lww.com/JCRP/A257).
Figure 2 provides an overview of the patient-reported reasons for not completing the CR program. Nearly one-third of the respondents withdrew from the CR because they “Could no longer participate because of other physical problems” (30%, n = 26), such as orthopedic injuries or worsening of their heart diseases. The most reported reasons for nonattenders “Did not need the CR trajectory” and “Did not need the supervision” were recurrent reasons in noncompleters as well. Content-related reasons such as “The CR program was not personal enough” (n = 20), “Content of CR program was not as expected” (n = 15), and “Intensity of the CR program was too burdensome” (n = 14) were reported by approximately 15-20% of respondents. The results of the stratified analyses performed between the two countries have been added as a supplemental (see Supplemental Digital Content 4, available at: http://links.lww.com/JCRP/A258, and Supplemental Digital Content 5, available at: http://links.lww.com/JCRP/A259).
Figure 2.
Reasons (multiple answers were possible) for noncompletion after starting the CR program. Data are presented per reason as (%) of total number of noncompleters (n = 88). Abbreviation: CR, cardiac rehabilitation. This figure is available in color online (www.jcrpjournal.com).
DISCUSSION
This study investigated reasons for nonattendance and noncompletion of CR in a multicenter multicountry setting. We collected a total of 1829 questionnaires of which 192 respondents did not attend CR despite receiving advice (nonattenders) and 88 participants withdrew from the CR program after starting (noncompleters). The most reported reasons for nonattendance were not feeling the need for CR, feeling that they did not need the supervision, or they already exercised enough. Discontinuing the CR program because of physical reasons was mentioned the most among noncompleters. Furthermore, a high percentage of noncompleters reported that the program was not personal enough and, similar to nonattendance, they did not need the program or supervision. These data suggest that the majority of the patients have a motivational or perception reason for nonattendance. Reasons for noncompletion, however, are more practical or CR-program related. Findings from this study are valuable to develop novel strategies to increase CR uptake among cardiac patients.
We found that patients who were male, more highly educated, working, and living closer to a CR center were more likely to participate to CR. In addition, we found a higher participation rate among patients diagnosed with myocardial infarction than among nonattenders. These sociodemographic findings are in line with a recent meta-analysis that concluded that patient characteristics such as age, sex, employment status, socioeconomic status, comorbidities, and civil status influence the attendance and completion of CR,19 and confirm the inclusion of a representative sample of cardiac patients.
REASONS FOR NONATTENDANCE
The most reported reasons for nonattendance found in this study were intrapersonal and related to the perception of the CR program itself. Intrapersonal reasons and perception of the CR program might suggest that regardless of sociodemographic characteristics, a group of patients exist who have their own individual reasons for nonattendance. Despite referral, patients decided not to participate and reported not needing the supervision or the CR program as a whole. The findings of reasoning about participation in CR support a previous study that observed a small group of interviewees who perceived themselves to be not suitable for the CR program.27 Not feeling the need for CR and not needing supervision might indicate that these patients are not motivated, are not aware of the beneficial effects of CR, or they feel that they are already living an active lifestyle and they can solve their problems themselves. The high percentage of patients reporting these two reasons is worrying, as CR is not only an exercise program, it is also meant to introduce a healthy lifestyle, improve the ability to deal with CVD, and provide psychological help. Motivational or perception reasons to refrain from CR could indicate a misconception and/or inferior knowledge about the complete CR program, which plays an important role in the decision-making process of participation and adherence. Misconceptions about the value of CR are clinically problematic, given the decreasing length of hospital stay following cardiovascular events, such as myocardial infarction. The short hospital stay allows patients less time to fully understand the severity of their disease and the importance of the CR program.28 To improve adherence and emphasize the importance of the CR program among all patients, a well-founded information protocol and encouragement from health care professionals are vital.
REASONS FOR NONCOMPLETION
Similar to nonattendance, intrapersonal reasons for withdrawing from the CR program were mentioned by the noncompleters. However, the main reason for not completing the CR program was because of other physical reasons and was reported by one-third of respondents. Among other physical reasons, both heart-related diseases, such as needing an additional revascularization procedure, and non–heart-related physical problems, such as orthopedic injuries, were mentioned. Furthermore, context-related reasons such as the group aspect, transportation, and the lack of personal guidance played a big role in withdrawing from the CR program. In addition, patients reporting “The CR program was not personal enough” indicated that the exercises and guidance offered by the CR center were too general and did not fit their needs and/or preferred type of exercise. These findings suggest that in order to improve CR adherence, health care professionals should explore the center-specific or local reasons given for not completing in CR, so that alterative personalized solutions can be offered to a broader range of patients and circumstances.
ALTERNATIVE SOLUTIONS
Solutions such as eHealth and home-based programs might be an alternative for traditional center–based CR, especially since there is a growing amount of evidence showing that home-based programs can be as effective as traditional CR.29 Home-based solutions can be used for different subgroups of patients by offering a personalized intervention. In nonattenders who consider themselves too fit and active to participate in a regular CR program, more emphasis and guidance on the different aspects of CR could provide more personalized programs that help optimizing the control of their CVD. In addition, if the center-based exercise program is found not for them (due to personal preference) and patients prefer exercising on their own while still in contact with a health care professional, telemonitoring could provide a solution. Otherwise, for patients who are not motivated, limited by other external barriers, not feeling comfortable in a group, not wanting to hear problems of others, or feel that the current CR program is not for them, home-based programs can be a solution by offering a flexible and personalized program, increasing the likeliness of attending and adherence to CR.30 Hence, future studies on the topic of alternative forms of CR should try to include patients with motivational or perception reasons for nonattendance or noncompletion to a regular CR program with bottom-up approach. By collaborating with the patients reporting individual reasons for nonattendance and noncompletion, future alternative solutions will be more tailored and personalized for the needs of end users.
STRENGTHS AND LIMITATIONS
This study had several strengths. We were able to distribute a large number of questionnaires in a multicenter, two-country setting and had a good response rate (see Supplemental Digital Content 6, available at: http://links.lww.com/JCRP/A260, and Supplemental Digital Content 7, available at: http://links.lww.com/JCRP/A261). A potential limitation of this study is that some form of selection bias may have occurred. Referral rate (70%) and CR uptake (85%) were higher compared with findings from previous studies.11 This is probably explained by the distribution of questionnaires among patients who already started the CR program by one of the hospitals that only addressed patients already referred to the CR program. In addition, recall bias may have occurred since patients had to recall whether or not CR was proposed to them and their reasons to not attend or complete the program. It was not possible to assess the characteristics of nonresponders, which may have led to an underestimation of nonattenders and noncompleters as these groups are more likely to ignore the questionnaire than highly motivated patients attending CR. In addition, we found a lower response rate in Germany than in the Netherlands, which can be explained in part by two factors: (1) German patients were approached by their health insurance company instead of treating physician, which may have affected the urge to participate in the study, and (2) the majority of German patients received a paper questionnaire, whereas an online questionnaire was most common in the Netherlands. Unfortunately, these differences in response rate made it impossible to derive well-founded conclusions from the comparisons of reported reasons between countries. Although no comparison between countries could be made, results from previous research indicate that despite differences in region and health care systems, barriers to CR enrollment and program completion seem to be universal between countries. Considering these results, we decided to combine the data from both countries despite the difference in response rate, as there is a large overlap in respondent characteristics, content of Dutch and German CR programs, and the mentioned reasons for nonattendance and noncompletion. Although no direct comparison was made, the country-specific data indicate that the top four reasons for nonattendance and noncompletion were similar between the countries, supporting the evidence for reasons being universal between countries. Notwithstanding these limitations, quantitative factors that are known to be associated with nonattendance and noncompletion were similar in our study compared with previous work,19 highlighting the validity of our cohort.
CONCLUSION
The majority of the patients have a motivational or perception reason, which might indicate a misconception and/or inferior knowledge about CR. This finding provides great potential in improving a more personalized approach in CR programs as the reported reasons are often modifiable, especially when health care professionals are aware of this information. These results underline the need for a personalized approach that includes adequate motivation, information, and alternative solutions (eg, eHealth, home-based or a more flexible program) to increase uptake and completion of CR.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank all the participants for their participation. Furthermore, they thank all participating health care professionals and the AOK Rheinland/Hamburg for helping in the inclusion process. This project is funded by an Interreg grant (“Zorg Verbindt” #203072). The work of T.M.H.E is supported by the Netherlands Heart Foundation (Senior E-Dekker grant no. 2017T051).
Footnotes
The authors declare no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jcrpjournal.com).
Contributor Information
Thijs Vonk, Email: thijs.vonk@radboudumc.nl.
Malou A. H. Nuijten, Email: malou.nuijten@radboudumc.nl.
Martijn F. H. Maessen, Email: martijn.maessen@vgz.nl.
Esther P. Meindersma, Email: esther.meindersma@radboudumc.nl.
Hetty J. J. Koornstra-Wortel, Email: h.koornstra@pantein.nl.
Marc M. Waskowsky, Email: m.waskowsky@isala.nl.
Johan A. Snoek, Email: j.a.snoek@isala.nl.
Thijs M. H. Eijsvogels, Email: thijs.eijsvogels@radboudumc.nl.
Maria. T. E. Hopman, Email: maria.hopman@radboudumc.nl.
REFERENCES
- 1.Wilkins E WL, Wickramasinghe K, Bhatnagar P, et al. European Cardiovascular Disease Statistics 2017. Brussels, Belgium: European Heart Network; 2017. [Google Scholar]
- 2.Ford ES, Ajani UA, Croft JB, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980-2000. N Engl J Med. 2007;356(23):2388–2398. [DOI] [PubMed] [Google Scholar]
- 3.Writing Group M, Mozaffarian D, Benjamin EJ, et al. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation. 2016;133(4):e38–e360. [DOI] [PubMed] [Google Scholar]
- 4.Piepoli MF, Corra U, Adamopoulos S, et al. Secondary prevention in the clinical management of patients with cardiovascular diseases. Core components, standards and outcome measures for referral and delivery: a policy statement from the cardiac rehabilitation section of the European Association for Cardiovascular Prevention & Rehabilitation. Endorsed by the Committee for Practice Guidelines of the European Society of Cardiology. Eur J Prev Cardiol. 2014;21(6):664–681. [DOI] [PubMed] [Google Scholar]
- 5.Heran BS, Chen JM, Ebrahim S, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2011(7):CD001800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lawler PR, Filion KB, Eisenberg MJ. Efficacy of exercise-based cardiac rehabilitation post-myocardial infarction: a systematic review and meta-analysis of randomized controlled trials. Am Heart J. 2011;162(4):571–584. e572. [DOI] [PubMed] [Google Scholar]
- 7.Anderson L, Oldridge N, Thompson DR, et al. Exercise-based cardiac rehabilitation for coronary heart disease: cochrane systematic review and meta-analysis. J Am Coll Cardiol. 2016;67(1):1–12. [DOI] [PubMed] [Google Scholar]
- 8.Piepoli MF, Hoes AW, Agewall S, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016;37(29):2315–2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2012;126(25):e354–e471. [DOI] [PubMed] [Google Scholar]
- 10.Smith SC, Jr, Benjamin EJ, Bonow RO, et al. AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and other Atherosclerotic Vascular Disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011;124(22):2458–2473. [DOI] [PubMed] [Google Scholar]
- 11.Bjarnason-Wehrens B, McGee H, Zwisler AD, et al. Cardiac rehabilitation in Europe: results from the European Cardiac Rehabilitation Inventory Survey. Eur J Cardiovasc Prev Rehabil. 2010;17(4):410–418. [DOI] [PubMed] [Google Scholar]
- 12.van Engen-Verheul M, de Vries H, Kemps H, Kraaijenhagen R, de Keizer N, Peek N. Cardiac rehabilitation uptake and its determinants in the Netherlands. Eur J Prev Cardiol. 2013;20(2):349–356. [DOI] [PubMed] [Google Scholar]
- 13.Turk-Adawi KI, Grace SL. Narrative review comparing the benefits of and participation in cardiac rehabilitation in high-, middle- and low-income countries. Heart Lung Circ. 2015;24(5):510–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oosenbrug E, Marinho RP, Zhang J, et al. Sex differences in cardiac rehabilitation adherence: a meta-analysis. Can J Cardiol. 2016;32(11):1316–1324. [DOI] [PubMed] [Google Scholar]
- 15.Bennett KK, Smith AJ, Harry KM, et al. Multilevel factors predicting cardiac rehabilitation attendance and adherence in underserved patients at a safety-net hospital. J Cardiopulm Rehabil Prev. 2019;39(2):97–104. [DOI] [PubMed] [Google Scholar]
- 16.Ruano-Ravina A, Pena-Gil C, Abu-Assi E, et al. Participation and adherence to cardiac rehabilitation programs. A systematic review. Int J Cardiol. 2016;223:436–443. [DOI] [PubMed] [Google Scholar]
- 17.Zhang L, Sobolev M, Pina IL, Prince DZ, Taub CC. Predictors of cardiac rehabilitation initiation and adherence in a multiracial urban population. J Cardiopulm Rehabil Prev. 2017;37(1):30–38. [DOI] [PubMed] [Google Scholar]
- 18.De Vos C, Li X, Van Vlaenderen I, et al. Participating or not in a cardiac rehabilitation programme: factors influencing a patient's decision. Eur J Prev Cardiol. 2013;20(2):341–348. [DOI] [PubMed] [Google Scholar]
- 19.Neubeck L, Freedman SB, Clark AM, Briffa T, Bauman A, Redfern J. Participating in cardiac rehabilitation: a systematic review and meta-synthesis of qualitative data. Eur J Prev Cardiol. 2012;19(3):494–503. [DOI] [PubMed] [Google Scholar]
- 20.McKee G, Biddle M, O' Donnell S, Mooney M, O' Brien F, Moser DK. Cardiac rehabilitation after myocardial infarction: what influences patients' intentions to attend? Eur J Cardiovasc Nurs. 2014;13(4):329–337. [DOI] [PubMed] [Google Scholar]
- 21.Fletcher SM, McBurney H. Strategic moments: identifying opportunities to engage clients in attending cardiac rehabilitation and maintaining lifestyle changes. J Cardiopulm Rehabil Prev. 2016;36(5):346–351. [DOI] [PubMed] [Google Scholar]
- 22.Maessen MFH, Verbeek ALM, Bakker EA, Thompson PD, Hopman MTE, Eijsvogels TMH. Lifelong exercise patterns and cardiovascular health. Mayo Clinic Proc. 2016;91(6):745–754. [DOI] [PubMed] [Google Scholar]
- 23.AOK-Die Gesundheitskasse. The AOK: one of the leading health insurance companies. https://en.zuwanderer.aok.de/home/staying-healthy-in-germany/health-care-for-you-in-germany/the-aok-one-of-the-leading-health-insurance-companies/. Published July 9, 2019. Accessed September 7, 2019.
- 24.Revalidatiecommissie NVVC/NHS en projectgroep PAAHR. Multidisciplinaire Richtlijn Hartrevalidatie. Utrecht, the Netherlands: Nederlandse Vereniging voor Cardiolgie; 2011. [Google Scholar]
- 25.PAAHR RNNep. Multidisciplinaire Richtlijn Hartrevalidatie. Utrecht, the Netherlands: Nederlandse Vereniging voor Cardiologie; 2011. [Google Scholar]
- 26.Hahmann HW. Kardiologische rehabilitation. Herz. 2012;37(1):22–29. [DOI] [PubMed] [Google Scholar]
- 27.Herber OR, Smith K, White M, Jones MC. “Just not for me”—contributing factors to nonattendance/noncompletion at phase III cardiac rehabilitation in acute coronary syndrome patients: a qualitative enquiry. J Clin Nurs. 2017;26(21-22):3529–3542. [DOI] [PubMed] [Google Scholar]
- 28.Swaminathan RV, Rao SV, McCoy LA, et al. Hospital length of stay and clinical outcomes in older STEMI patients after primary PCI: a report from the National Cardiovascular Data Registry. J Am Coll Cardiol. 2015;65(12):1161–1171. [DOI] [PubMed] [Google Scholar]
- 29.Anderson L, Sharp GA, Norton RJ, et al. Home-based versus centre-based cardiac rehabilitation. Cochrane Database Syst Rev. 2017;6(6):Cd007130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thomas RJ, Beatty AL, Beckie TM, et al. Home-based cardiac rehabilitation: a scientific statement from the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. J Cardiopulm Rehab Prev. 2019;39(4):208–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.