PURPOSE
In 2016, there were 1,308,061 cases of cancer being treated in Indonesia, with 2.2 trillion rupiahs spent, amounting to $486,960,633 in US dollars (purchasing power parity 2016). The high burden of cancers in Indonesia requires a valid data collection to inform future cancer-related policies. The purpose of this study is to report cancer epidemiological data from 2008 to 2012 based on Hospital-Based Cancer Registry (HBCR) data from Cipto Mangunkusumo Hospital, Indonesia.
METHODS
This was a descriptive study with cross-sectional design. Data were collected from Cipto Mangunkusumo Hospital HBCR 2008-2012. Demographical, diagnostic, stages of cancer, and histopathological types of cancer data were extracted.
RESULTS
After screening, 18,216 cases were included. A total of 12,438 patients were older than 39 years of age (68.3%), with a female-to-male ratio of 9:5. Most patients have cancers at advanced stages (stages III and IV, 10.2%). The most common sites of cancer were cervix uteri (2,878 cases, 15.8%), breast (2,459 cases, 13.5%), hematopoietic and reticuloendothelial systems (1,422 cases, 7.8%), nasopharynx (1,338 cases, 7.4%), and lymph nodes (1,104 cases, 6.1%).
CONCLUSION
From this HBCR, cancer incidence in female was almost twice the incidence in male, largely because of the burden of cervical and breast cancers. The cervix uteri as one of the top five cancer sites based on this HBCR, 2008-2012, are still approximately consistent with Global Cancer Incidence, Mortality and Prevalence 2018, which portrayed that Indonesia has been severely afflicted by cervical cancer cases more than any other Association of Southeast Asian Nations countries. The HBCR could serve as a robust database of epidemiological data for cancer cases in Indonesia.
INTRODUCTION
Cancer is one of the primary causes of death in both developing and developed countries. Based on data from the global cancer statistics (Global Cancer Incidence, Mortality and Prevalence [GLOBOCAN]), a prediction tool estimating cancer incidence and mortality worldwide by the International Agency for Research on Cancer, there has been an increasing trend in cancer incidence and death. There was an estimate of 18.1 million new cancer cases worldwide in 2018, from previously 14.1 million in 2012. Furthermore, cancer was responsible for an estimated 9.6 million deaths in 2018, from previously 8.2 million in 2012.1-3 Although the increase is happening globally, the types of cancer are different between developing and developed countries, among various measures of demography. Overall highest cancer incidences based on the organ are lung (11.58%), followed by breast (11.55%) and colorectum (10.23%), with highest mortality in lung (18.43%), liver and biliary duct (9.91%), and stomach (8.19%).2 For Indonesia, GLOBOCAN estimates were derived by incorporating weighted averages from Malaysia (2008-2010) and Brunei Darussalam (2010-2012) applied to 2018 population for incidence, with all-site estimates from neighboring countries partitioned using national frequency data from national cancer registry at Dharmais National Cancer Center, and by using the South-Eastern Asia model for mortality, which extrapolated mortality from the national incidence, using incidence-mortality ratios derived from cancer registries in China (90 registries), Japan (nine registries), and Korea.4,5
CONTEXT
Key Objective
What are the top five cancer sites in an Indonesian hospital-based cancer registry (HBCR)?
Knowledge Generated
This first 5-year HBCR study from Indonesia’s national referral hospital, Cipto Mangunkusumo Hospital, has revealed that the top five cancer sites were cervix uteri (16 percent), breast (14%), hematopoietic and reticuloendothelial systems (8%), nasopharynx (7%), and lymph nodes (6%). Cancer incidence in female was almost twice the incidence in male, largely because of the cervical and breast cancers.
Relevance
In the era of big data, Indonesia spearheaded a robust HBCR-Population-Based Cancer Registry framework since 2016 to inform health policies and improve cancer outcomes. The cervix uteri as one of the most common cancer sites in this HBCR are still approximately consistent with the Global Cancer Incidence, Mortality and Prevalence 2018 data, which have ranked Indonesia first among Association of Southeast Asian Nations countries in the total number of cervical cancer cases. The fourth most populous country in the world is seeing a significant uptrend of cancer burden within the past decade.
More than half of the cancer incidence (56.8%) and death (64.9%) occurred in developing countries, with a prediction for the level to be higher in the future. In 2018, GLOBOCAN approximated 291 from 100,000 Indonesians suffered from cancers.3 In 2013, according to the Basic Health Research (Riskesdas), cancer prevalence in Indonesia was 1.4 in 1,000 population.6 In 2016, Social Insurance Administration Organization reported that from 1,308,061 cancer cases treated, a total of 2.2 trillion rupiahs was spent, amounting to $486,960,633 in US dollars (purchasing power parity 2016).7,8 The high burden of cancer in Indonesia requires a valid data collection, which can help to decide future regulation regarding cancer.
As the world’s fourth most populous country with more than 260 million population, it will do justice to improve Indonesian cancer epidemiological data to contribute to the GLOBOCAN model. For this reason, in 2008, we have established a Hospital-Based Cancer Registry (HBCR) for Cipto Mangunkusumo Hospital, the highest national referral hospital in Indonesia’s National Health Insurance (Jaminan Kesehatan Nasional [JKN]) scheme, to collect and provide real data on cancer. The JKN was initiated in 2014 by President Joko Widodo. Within 5 years, it has become the world’s largest single-payer national health insurance. Indonesia has a total of 9,993 community health centers (puskesmas) in 2018 and 2,813 hospitals in 2017 to cover an area of 1.9 million km2.9 Dharmais National Cancer Center was built in Jakarta in 1993. Patients with cancer in Indonesia are eventually referred to both Dharmais National Cancer Center and Cipto Mangunkusumo Hospital, which are public hospitals, apart from a few patients treated at private facilities or going abroad. Meanwhile, most lung cancers are referred to Persahabatan National Respiratory Center in Jakarta, which is also a public hospital.
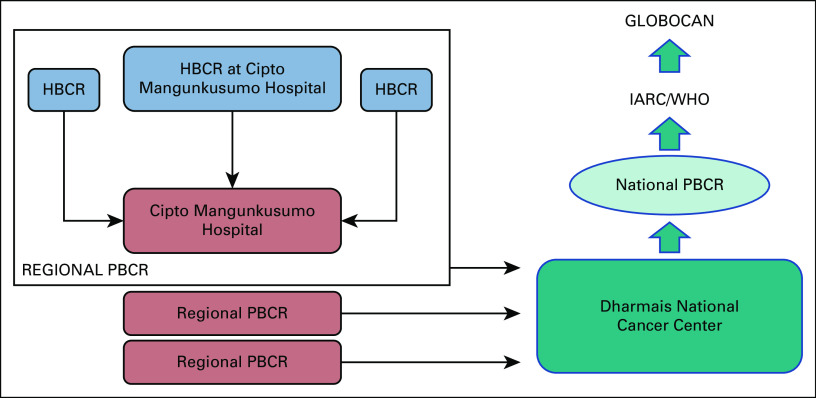
The HBCR has also served as a fundamental framework to spearhead Indonesia’s effort in cancer big data in Indonesia. We undertook the initiation of the Population-Based Cancer Registry (PBCR) shortly after its hospital counterpart, in the hope that both databases can be potential game changers in the future GLOBOCAN prediction model and more robust estimates of Indonesia’s cancer incidence and mortality. Medical records in Indonesian hospitals are not integrated. As a result, Cipto Mangunkusumo Hospital was appointed as the regional cancer registry hospital for Jakarta by the Ministry of Health since 2016 to collect HBCRs from hospitals in Jakarta, including this HBCR, and data from private facilities without established HBCRs. Regional data from all provinces are then reported to Dharmais National Cancer Center, which is the appointed national cancer burden control center by the Ministry of Health to establish the national PBCR since 2016 (Fig. 1). This study aims to report 5-year cancer epidemiological data, 2008-2012, from Cipto Mangunkusumo Hospital’s cancer registry.
FIG 1.
HBCR-PBCR Framework in Indonesia. In 2016, the Ministry of Health appointed Cipto Mangunkusumo Hospital as one of the regional cancer registry hospitals and Dharmais National Cancer Center as the national cancer burden control center. The vertical relationship between HBCR and PBCR shows that individual HBCRs are collected in a bottom-up fashion by the regional cancer registry hospitals, which form the regional PBCRs and submit them to the national cancer registry hospital. GLOBOCAN, Global Cancer Incidence, Mortality and Prevalence; HBCR, hospital-based cancer registry; PBCR, population-based cancer registry.
METHODS
This study was a descriptive study using cross-sectional design, based on data from the HBCR of Indonesia’s National Referral Hospital, Cipto Mangunkusumo Hospital, from 2008 to 2012. Data collection was performed since the re-establishment of Cancer Registry, under the Oncology Center of Cipto Mangunkusumo Hospital in 2015. Subjects were taken by total sampling method. The inclusion criteria were patients suspected or diagnosed with cancer proven by histopathology or other investigations, that is, cytology, clinical examinations only, clinical investigation using ultrasound, unknown from referral cases, death certificate only, and surgery or autopsy. There were no exclusion criteria in this study. Deaths were confirmed solely from the medical records at Cipto Mangunkusumo Hospital.
Data Collection
Collecting data for HBCR involves several steps, from raw data collection, data abstraction and coding, first verification, data input, second verification, data quality stratification, data analysis, and reporting. Lists of patients were collected from all departments in the hospital, medical records, and hospital information system. The lists were filtered for duplication and hand-searched for the respective medical record, followed by data abstraction and coding. During abstraction, the summary of patients was coded into SRIKANDI form (a specific cancer registry form in the hospital). Then, the data were verified by an officer (by intervariable matching through the SRIKANDI form) and inserted into the cancer registry software (Canreg 5) to undergo second verification. For the 2008-2012 HBCR, the steps done for data filtering are separation of patients with cancer from the main hospital registry, elimination of duplicates, and filtering based on years. Capture-recapture method was used to finalize the data.
Data Analysis
Based on the data acquired, demographical, diagnostic, staging, and histopathological data were extracted. Univariate data analysis was conducted by using Microsoft Excel and SPSS 16.0.
Ethical Clearance
This study has been reviewed and accepted by The Research Ethical Committee of Faculty of Medicine, Universitas Indonesia, in accordance with the Declaration of Helsinki.
RESULTS
To our knowledge, this was the first established HBCR report in Indonesia conducted at the National Referral Hospital of Indonesia, Cipto Mangunkusumo Hospital. During the initial screening, 37,790 cases were collected, followed by another screening using capture-recapture method, which yielded 18,216 final cases. Of those cancer cases, 3,842 (21.09%) cases were from 2008, 3,483 (19.12%) cases were from 2009, 3,788 (20.80%) cases were from 2010, 3,447 (18.92%) cases were from 2011, and 3,656 (20.07%) cases were from 2012.
Demographic Profile
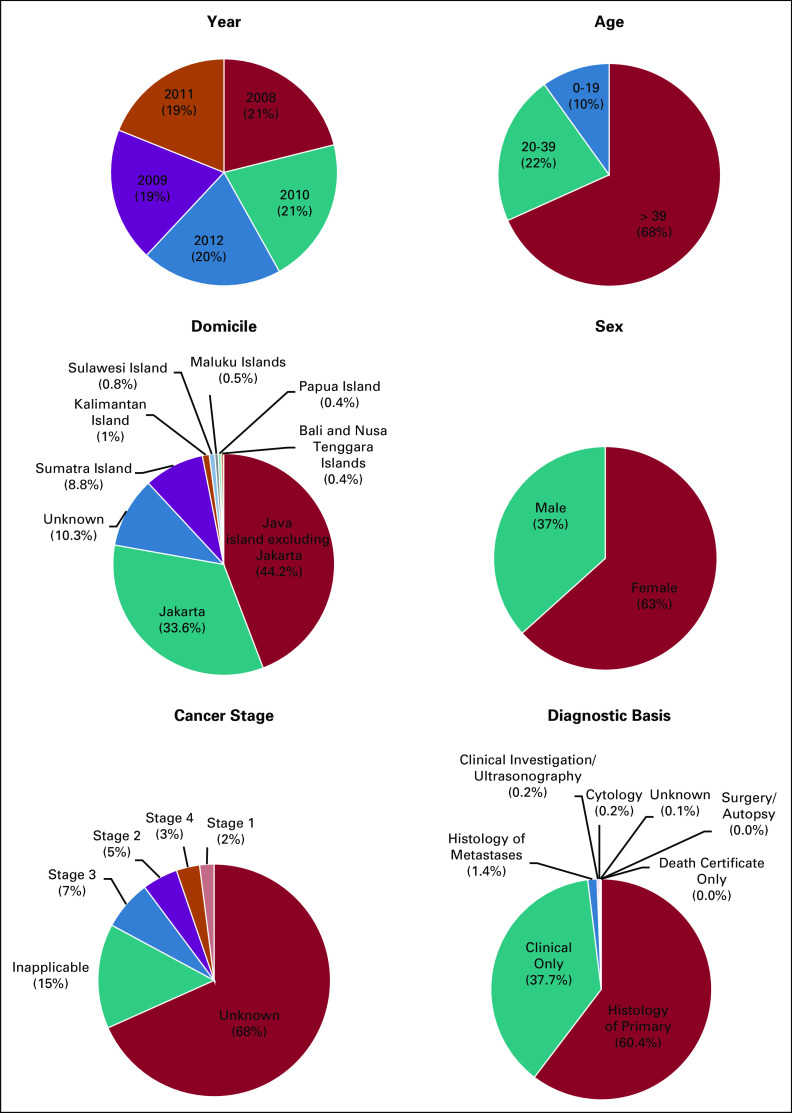
Table 1 and Figure 2 show the study characteristics of patients involved in the study. The characteristics are admission year, age, domicile, sex, cancer stage, tumor location, and diagnostic basis.
TABLE 1.
Tumor Locations of the Patients With Cancer
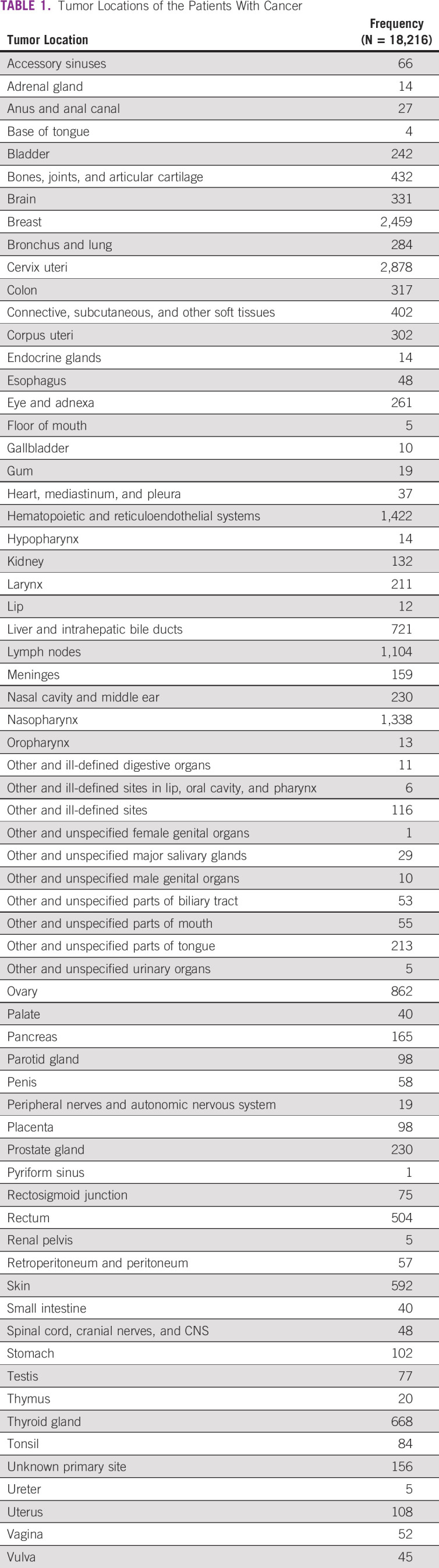
FIG 2.
Study characteristics of the 2008-2012 HBCR patients at Cipto Mangunkusumo Hospital, Indonesia. The demographic profile of the HBCR patients are grouped based on admission year, age, domicile, sex, cancer stage, tumor location, and diagnostic basis. See Table 1 for the grouping based on the tumor location. HBCR, hospital-based cancer registry.
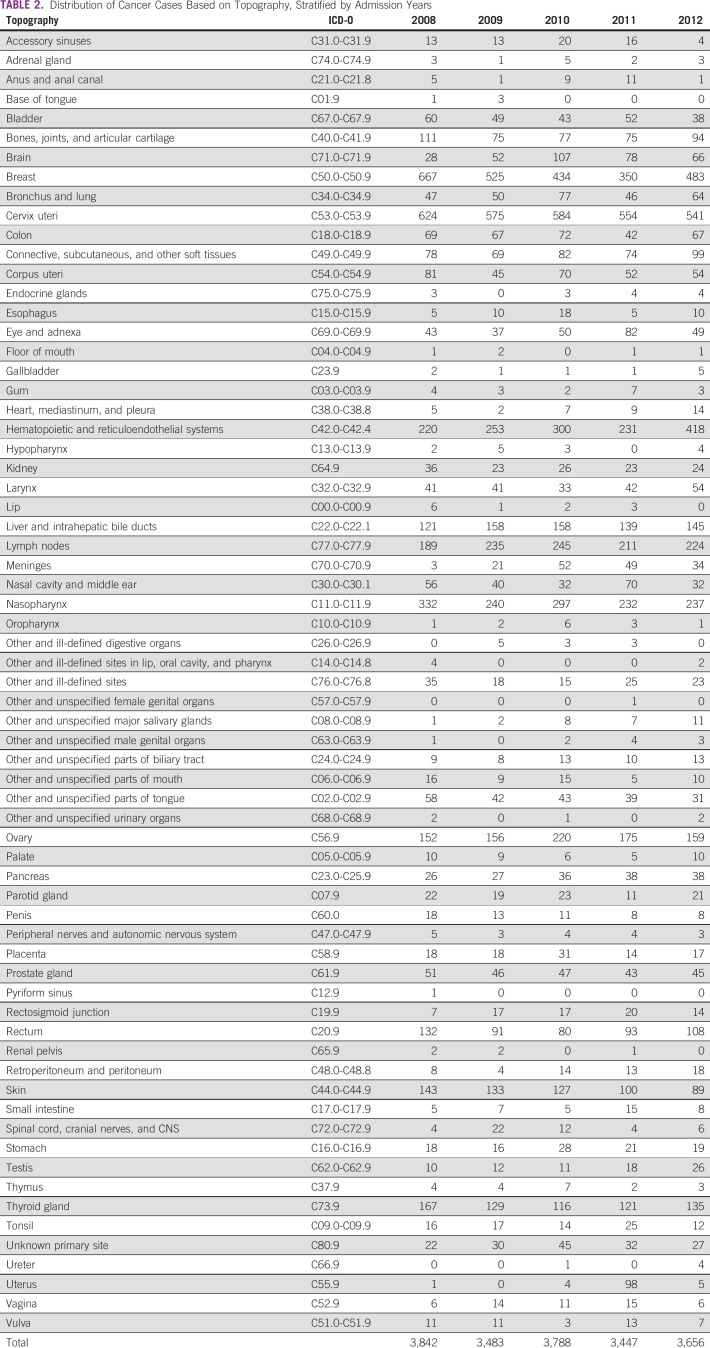
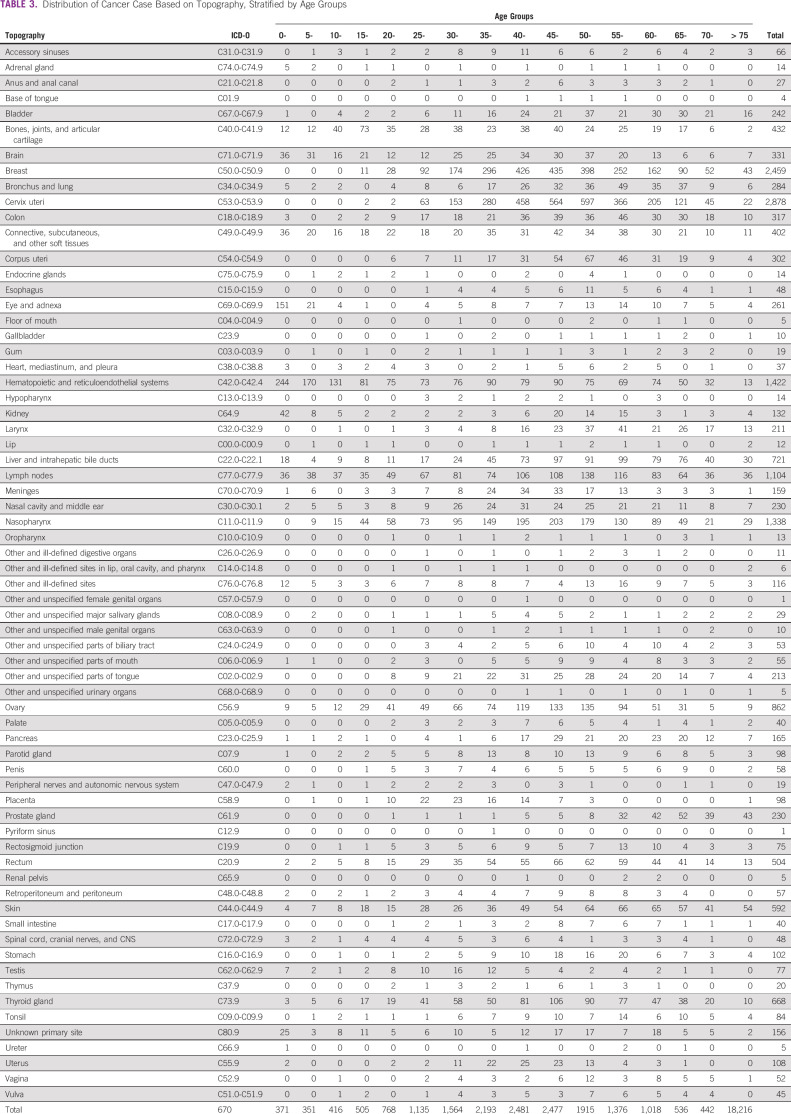
Distribution of cancer cases based on topography is shown in Tables 2 and 3. Table 2 stratifies the data by admission years, whereas Table 3 stratifies the data by age groups.
TABLE 2.
Distribution of Cancer Cases Based on Topography, Stratified by Admission Years
TABLE 3.
Distribution of Cancer Case Based on Topography, Stratified by Age Groups
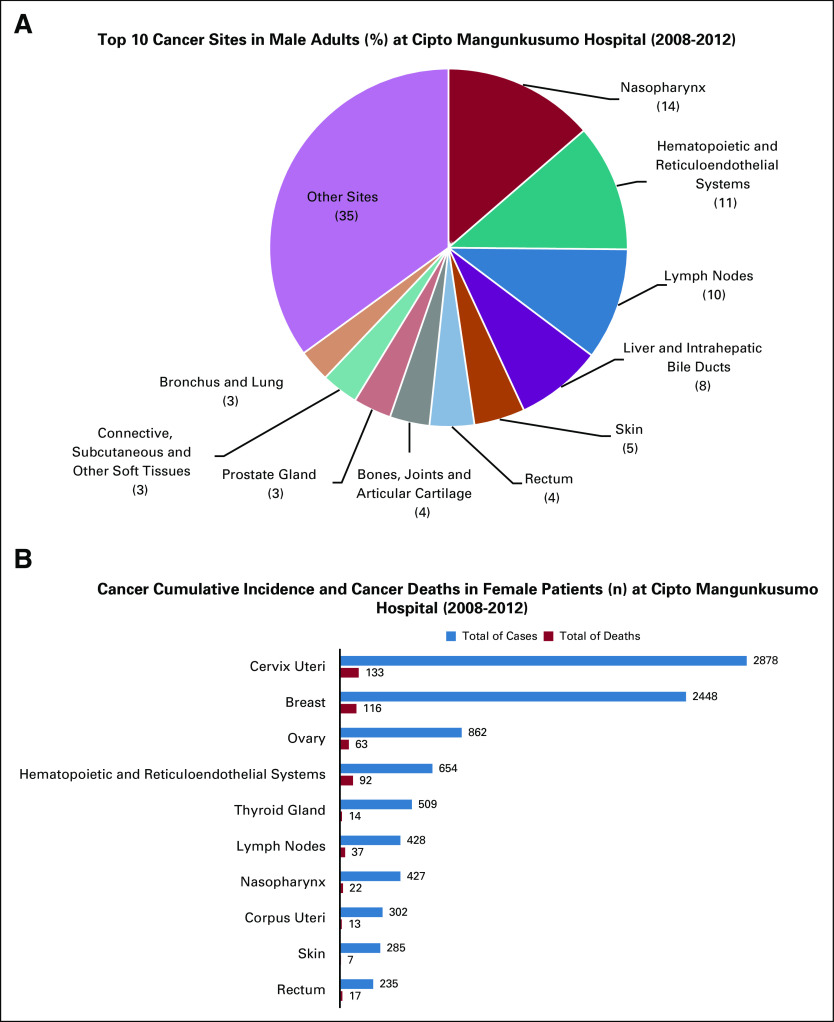
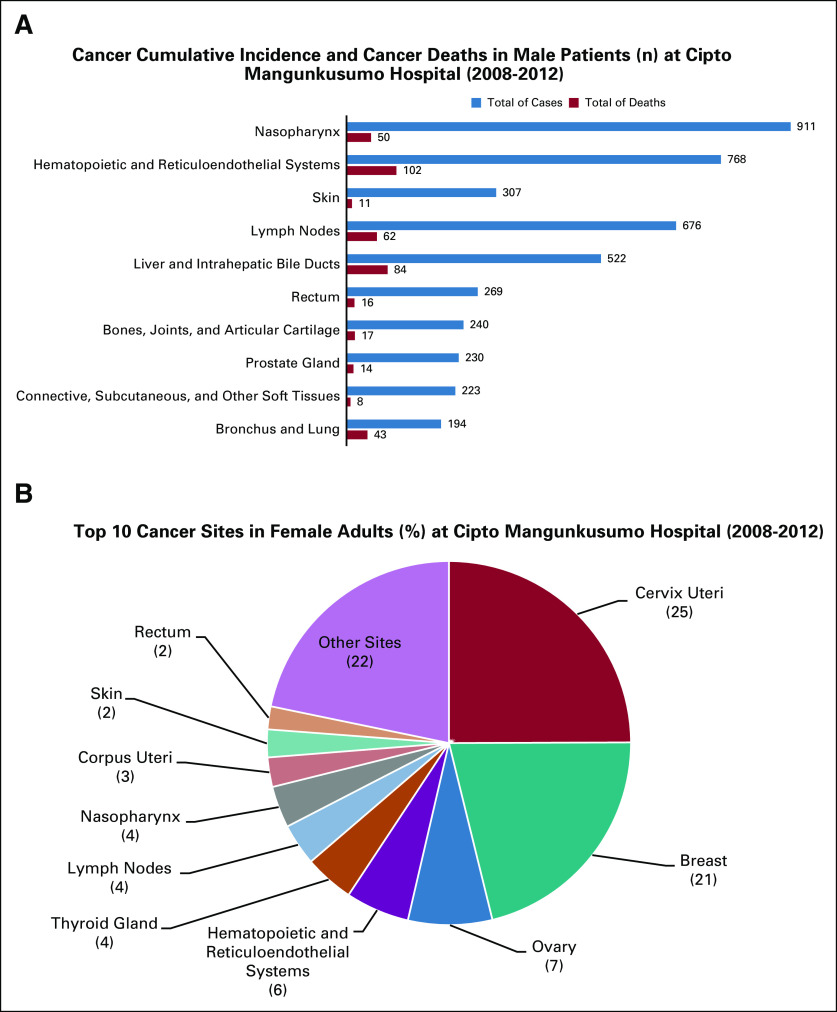
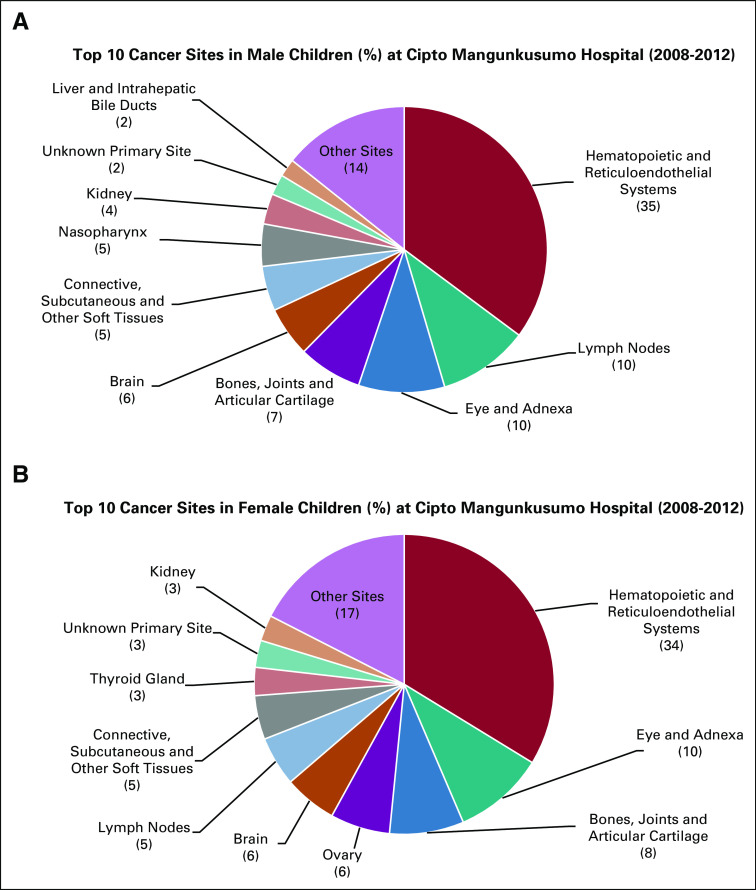
The 10 highest cancer cases for male and female are shown in Figure 3, accompanied by the number of cancer deaths in Figure 4. After stratifying by sex, nasopharyngeal cancer was placed the highest occurring cancer among male patients with 911 cases (13.6%), whereas cervical cancer was the highest among female patients with 2,878 cases (24.9%). Hematopoietic and reticuloendothelial system cancer was responsible for the highest number of deaths in male patients (102 deaths, 25.1%), whereas cervical cancer was responsible for the highest number of deaths in female patients (133 deaths, 25.9%). Meanwhile, the ten highest cancer cases in children (0-19 years of age) are shown in Figure 5. Hematopoietic and reticuloendothelial system cancer was the highest among male children, with 347 cases (35.2%), and also for female children, with 278 cases (33.8%).
FIG 3.
Top 10 cancer sites in male and female adults (%) at Cipto Mangunkusumo Hospital, Indonesia (2008-2012). (A) In male adults, top 10 cancer sites were nasopharynx, hematopoietic and reticuloendothelial systems, lymph nodes, liver and intrahepatic bile ducts, skin, rectum, bones, joints and articular cartilage, prostate gland, connective, subcutaneous and other soft tissues, and bronchus and lung. (B) In female adults, top 10 cancer sites were cervix uteri, breast, ovary, hematopoietic and reticuloendothelial systems, thyroid gland, lymph nodes, nasopharynx, corpus uteri, skin, and rectum.
FIG 4.
Cancer cumulative incidence and cancer deaths stratified by sex (n) at Cipto Mangunkusumo Hospital, Indonesia (2008-2012). (A) In male patients, nasopharynx was the most common cancer site, but the highest proportion of deaths was due to the cancers of bronchus and lung. (B) In female patients, cervix uteri were the most common cancer site, but the highest proportion of deaths was due to the cancers of hematopoietic and reticuloendothelial systems.
FIG 5.
Top 10 cancer sites in male and female children (%) at Cipto Mangunkusumo Hospital, Indonesia (2008-2012). (A) In male children, top 10 cancer sites were hematopoietic and reticuloendothelial systems, lymph nodes, eye and adnexa, bones, joints and articular cartilage, brain, connective, subcutaneous and other soft tissues, nasopharynx, kidney, unknown primary site, and liver and intrahepatic bile ducts. (B) In female children, top 10 cancer sites were hematopoietic and reticuloendothelial systems, eye and adnexa, bones, joints and articular cartilage, ovary, brain, lymph nodes, connective, subcutaneous and other soft tissues, thyroid gland, unknown primary site, and kidney.
DISCUSSION
In this 5-year HBCR, no differences are observed among annual numbers of cancer cases from 2008 until 2012. Most patients are older than 39 years of age (12,438 cases, 68.3%), whereas 3,971 (21.8%) patients are in the age group of 20-39 years and 1,807 patients (9.9%) are in the age group of 0-19 years. For domicile, 56.1% of the patients came from outside Jakarta, whereas 33.6% came from Jakarta. The rest (10.3%) have unknown domicile. From outside Jakarta, 15.6% came from Sumatra Island, 78.8% came from Java Island excluding Jakarta, 1.8% came from Kalimantan Island (Borneo), 1.4% came from Sulawesi Island (Celebes), 0.7% came from Bali and Nusa Tenggara (Lesser Sunda) Islands, 0.9% came from Maluku Islands (the Moluccas), and 0.8% came from Papua Island. This signifies the health disparity among the islands in the archipelago, in terms of health access, facilities, and capacity. A majority of patients outside Jakarta still came from Java, which is the most populous island in Indonesia with the best access to health resources, including the national referral hospitals. The data were heavily skewed to Java Island, including Jakarta. The stretched disparity in life expectancy between Java and the other islands in Indonesia inherently marks the probability of seeing higher cancer cases in Java.
The hospital had more female patients, which are 1.73 times more common than male patients or a ratio of 9:5. Of 18,216 patients, 11,538 patients (63.3%) were female, whereas 6,678 patients (36.7%) were male. There were 2,652 patients whose cancers (eg, cancers of the meninges, brain, or blood) were inapplicable to staging (14.6%) and 12,443 patients with unknown (staging data not found) staging (68.3%), whereas the rest are mostly at stage III (1,263 cases, 6.9%). A big proportion of unknown staging was mainly due to the low-coverage insurances during pre-JKN era (prior to 2014), leading to cancers directly treated without staging workups.
The most common site of cancer is cervix (2,878 cases, 15.80%), followed by breast (2,459 cases, 13.50%), hematopoietic and reticuloendothelial systems (1,422 cases, 7.81%), nasopharynx (1,338 cases, 7.35%), and lymph nodes (1,104 cases, 6.06%). The most used basis for diagnosis is histology of primary (60.35%), followed by clinical only (37.69%), histology of metastases (1.34%), and others such as cytology, death certificate, and surgery or autopsy.
This HBCR is one of the three main cancer centers in Indonesia. To achieve the goal of portraying cancer burden in the archipelago, one must keep in mind of this limitation. A comprehensive analysis spanning the three main HBCRs of Cipto Mangunkusumo, Dharmais, and Persahabatan is instrumental, before analyzing the regional and national PBCR data, some of which have been reported in previous studies.10-14 Furthermore, a complete follow-up of death data was not achieved in the early days of the HBCR because of resource constraint and, therefore, should be addressed in the future by directly contacting patients or the local population and civil registration offices to capture death data beyond medical records.
For both sexes, cervical cancer was the most common cancer (15.80%), with an increase in the age group of 30-34 years (153 cases), peaking in age group of 50-54 years (597 cases). Breast cancer was the second most common cancer, increasing in incidence with age and peaking in 45-49 years (435 cases). Cancer of hematopoietic and reticuloendothelial systems has a different incidence distribution based on age, with the most common age group being 0-4 years (244 cases), and then kept decreasing until the age group of 10-14 years (131 cases). Older than 15 years of age, the differences in incidence among age groups were not large. For nasopharyngeal carcinoma, age corresponds linearly with the increasing incidence, peaking in the age group of 45-49 years (203 cases). Lymphoma was the fifth most common cancer, and the incidence is significantly higher in the age group of 40-59 years, peaking in the age group of 50-54 years (138 cases). Compared with the data from 2008, in Association of Southeast Asian Nations (ASEAN) countries, the top five sites of cancer were lung, breast, liver, colorectal, and mouth, whereas the top five sites of cancer death in ASEAN nations were lung, liver, colorectal, breast, and stomach.15 According to data from Malaysian National Cancer Registry, between 2007 and 2011, the top 10 cancer sites were breast, colorectal, trachea, bronchus and lung, lymphoma, nasopharynx, leukemia, cervix, liver, ovary, and stomach.16 In this HBCR, breast is similarly one of the top five cancer sites as in ASEAN’s and Malaysia’s top five sites, but cervix uteri ranked the highest in the HBCR’s top five sites where it was not found in ASEAN’s and Malaysia’s top five sites. This finding is still approximately consistent with the latest GLOBOCAN data of 2018,3 which reported that Indonesia had the highest cervical cancer cases among ASEAN countries. This showed that cervical cancer has played a major role in shaping women’s health in Indonesia since at least a decade ago.
In this HBCR, cancer cases in male are most commonly found in nasopharynx, followed by hematopoietic and reticuloendothelial systems, lymph nodes, liver and intrahepatic bile ducts, and skin. There are 911 cases (13.6%) of nasopharyngeal carcinoma in male, with the incidence peaking in the age group of 45-49 years, and most patients came with stage III. The number of cancer deaths in male patients because of nasopharyngeal cancer was 50. In cancer of hematopoietic and reticuloendothelial systems, there are 768 cases (11.50%), with most incidence occurring in babies of age 0-4 years. Although cancer of hematopoietic and reticuloendothelial systems was the second most common cancer in male, its mortality was the highest in male with 102 cases. Lymphoma cases in male occurred in 676 patients (10.12%), with most patients in the age group of 50-54 years, and the number of cancer deaths was 62. Cancer of liver and intrahepatic bile ducts occurred in 522 patients (7.82%) with mortality in 84 cases, whereas skin cancer incidence in male was 307 cases (4.60%) with mortality in 11 cases. Meanwhile, according to the GLOBOCAN 2008, the top five sites of cancer in male in ASEAN countries were lung, liver, colorectal, mouth, and stomach, with almost the same rank for cancer death.15 Compared with Malaysian National Cancer Registry between 2007 and 2011, in male, the top 10 cancer sites were colorectal, trachea, bronchus and lung, nasopharynx, lymphoma, prostate, liver, leukemia, stomach, bladder, and other skin.16 Data from this HBCR were closely similar to Malaysia’s data, but almost completely in contrast to ASEAN’s data. However, this HBCR recorded more nasopharyngeal cancer because a separate hospital is dedicated to treat lung cancer (Persahabatan National Respiratory Center) and their data are not incorporated with this HBCR. This is one of the limitations of interpreting data from this HBCR.
In female, the most common cancer sites were cervix, followed by breast, ovary, hematopoietic and reticuloendothelial systems, and thyroid gland. Cervical cancer in female was found in 2,878 cases (24.94%), with a high incidence in the age group of 25-74 years and peaking in the age group of 50-54 years. Cervical cancer was also the highest in female cancer mortality (133 deaths, 26.76%). Breast cancer was the second most common cancer in female, with an incidence of 2,447 cases (21.21%). Breast cancer was more common in females of age > 20 years, peaking in the age group of 45-49 years. Breast cancer accounts for 116 deaths (23.34%) of a total of 497 deaths in female cancer cases. Most patients with breast cancer came with stage IIIB or IV. The third most common cancer found in female was ovarian cancer, with an incidence of 862 cases (7.47%). The incidence is increasing with age, peaking in the age group of 50-54 years. Most patients came with stage III to IVB, and the highest incidence was in stage IIIC. Mortality cases were found in 63 cases among patients with ovarian cancer. The fourth and fifth most common cancers in female were cancer of hematopoietic and reticuloendothelial systems with 654 cases (5.67%) and cancer of thyroid gland with 509 cases (4.41%). Cancer of hematopoietic and reticuloendothelial systems has the third highest cancer deaths in female, at 92 cases, whereas cancer deaths in cancer of thyroid gland occurred in 14 cases. Compared with the cancer incidence in ASEAN countries in 2008, the top five cancer sites in female were breast, cervix, colorectal, lung, and liver, with almost the same rank for cancer deaths.15 Meanwhile, in Malaysia, according to Malaysian National Cancer Registry between 2007 and 2011, in female, the top 10 cancer sites were breast, colorectal, cervix, ovary, trachea, bronchus and lung, lymphoma, corpus uteri, leukemia, thyroid, and stomach.16 The data of this HBCR were consistent with ASEAN’s and Malaysia’s data in that breast, cervix, and ovary placed among the top five cancer sites, but, in this HBCR, cervix is the most common site followed by breast, as opposed to ASEAN’s and Malaysia’s data, which were breast followed by cervix. This might be due to improved case detection for cervical cancer compared with breast cancer. However, Indonesia’s data followed suit with breast replacing cervix as the most common site of cancer in GLOBOCAN 2018.3 Yet, Indonesia still has the highest cervical cancer incidence in ASEAN according to the latest data, albeit being placed the second most common site.3 This might imply that Indonesia’s preventive efforts against cervical cancer, such as pap smear, visual inspection using acetoacetic acid, and vaccination, are still lacking compared with other ASEAN countries.
The differences between the patterns of adult and childhood cancers are consistent with expectations. In male children, the top five cancer sites were hematopoietic and reticuloendothelial systems (35.44%), lymph nodes (10.29%), eye and adnexa (9.78%), bones, joints and articular cartilage (7.23%), and brain (5.70%). In female children, the top five cancer sites were hematopoietic and reticuloendothelial systems (33.70%), eye and adnexa (9.82%), bones, joints, and articular cartilage (8.00%), ovary (6.67%), and brain (5.82%).
In conclusion, of the 18,216 cases recorded in this HBCR, ten most common sites of cancer were cervix uteri, breast, hematopoietic and reticuloendothelial, nasopharynx, lymph node, ovary, liver and intrahepatic bile ducts, thyroid gland, skin, and rectal. No differences were observed among annual numbers of cases from 2008 to 2012. Female patients were twice more common than male patients, because of the huge burden of cervical and breast cancers. Patients with cancer that can be staged, mostly came with an advanced stage cancer (3 and 4). The cervix uteri as one of the top five cancer sites based on this HBCR are still approximately consistent with GLOBOCAN 2018, which portrayed that Indonesia has been severely afflicted by cervical cancer more than any other ASEAN countries. The HBCR could serve as a robust database of epidemiological data for cancers in Indonesia.
AUTHOR CONTRIBUTIONS
Conception and design: Soehartati Gondhowiardjo, Gregorius B. Prajogi, Angela Giselvania, Marlinda Adham, Agus R.A.H. Hamid, Gatot Purwoto, Alvita Dewi Siswoyo, Nadia A. Mulansari, Nurul Ratna, Ceva W. Pitoyo, Sonar Soni Panigoro, Rizky K. Wardhani
Financial support: Soehartati Gondhowiardjo, Endang Widyastuti
Administrative support: Soehartati Gondhowiardjo, Salik Hawariy, Steven Octavianus, Angela Giselvania, Gatot Purwoto, Sonar Soni Panigoro, Rizky K. Wardhani, Tresia F.U. Tambunan
Provision of study materials or patients: Soehartati Gondhowiardjo, Fahmi Radityamurti, Andre Prawira Putra, Sri M. Sekarutami, Angela Giselvania, Agus R.A.H. Hamid, Tiara Aninditha, Gatot Purwoto, Alvita Dewi Siswoyo, Wulyo Rajabto, Nurul Ratna, Ceva W. Pitoyo, Erwin D. Yulian, Rossalyn S. Andrisa
Collection and assembly of data: Soehartati Gondhowiardjo, Nadia Christina, Ngakan P.D. Ganapati, Fahmi Radityamurti, Steven Octavianus, Andre Prawira Putra, Sri M. Sekarutami, Angela Giselvania, Agus R.A.H. Hamid, Yogi Prabowo, Tiara Aninditha, Gatot Purwoto, Renindra A. Aman, Trifona P. Siregar, Alvita Dewi Siswoyo, Diah R. Handjari, Djumhana Atmakusuma, Wulyo Rajabto, Nadia A. Mulansari, Ceva W. Pitoyo, Diani Kartini, Erwin D. Yulian, Rossalyn S. Andrisa, Wifanto S. Jeo, Tresia F.U. Tambunan, Feranindhya Agianda, Priyambodho
Data analysis and interpretation: Soehartati Gondhowiardjo, Salik Hawariy, Vito F. Jayalie, Andre Prawira Putra, Sri M. Sekarutami, Marlinda Adham, Endang Widyastuti, Yogi Prabowo, Gatot Purwoto, Lisnawati, Ceva W. Pitoyo
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/go/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Rizky K. Wardhani
Employment: Ciptomangunkusumo Hospital
No other potential conflicts of interest were reported.
REFERENCES
- 1.American Cancer Society : Global Cancer Facts & Figures (ed 3). Atlanta, GA, American Cancer Society, 2015. [Google Scholar]
- 2.International Agency for Research on Cancer : Latest World Cancer Statistics Global Cancer Burden Rises to 14.1 Million New Cases in 2012: Marked Increase in Breast Cancers Must Be Addressed, 2013 Update. Lyon/Geneva, France/Switzerland, IARC, 2013. https://www.iarc.fr/wp-content/uploads/2018/07/pr223_E.pdf/ [Google Scholar]
- 3.Bray F, Ferlay J, Soerjomataram I, et al. : Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide of 36 cancers in 185 countries. CA Cancer J Clin 68:394-424, 2018 [DOI] [PubMed] [Google Scholar]
- 4.Ferlay J, Colombet M, Soerjomataram I, et al. : Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer 144:1941-1953, 2019 [DOI] [PubMed] [Google Scholar]
- 5.Bray F, Colombet M, Ferlay J, et al. : Cancer Incidence in Five Continents (Vol. XI). Lyon, France, International Agency for Research on Cancer, 2017. http://ci5.iarc.fr [Google Scholar]
- 6.Health Research and Development Agency : Basic Health Research 2013. Jakarta, Indonesia, Ministry of Health Republic of Indonesia, 2013 [Google Scholar]
- 7.Tempo : 2016, BPJS is Responsible for the Treatment of 1.3 Million Cases of Cancer. https://nasional.tempo.co/read/841873/2016-bpjs-tanggung-perawatan-13-juta-kasus-kanker [Google Scholar]
- 8.OECD : Purchasing Power Parities (PPP). https://data.oecd.org/conversion/purchasing-power-parities-ppp.htm#indicator-chart [Google Scholar]
- 9.Ministry of Health Republic of Indonesia : Center of Data and Information. Jakarta, Indonesia, Ministry of Health Republic of Indonesia, 2019, p c2014 [Google Scholar]
- 10.Gondhowiardjo S, Silalahi M, Manuain DA, et al. : Cancer profile in Central Jakarta: A 5-year descriptive study. Radioter Onkol Indonesia 9:34-42, 2018 [Google Scholar]
- 11.Gondhowiardjo S, Handoyo D, Auzan M, et al. : Cancer profile in West Jakarta: A 5-year descriptive study. Radioter Onkol Indonesia 9:43-47, 2018 [Google Scholar]
- 12.Gondhowiardjo S, Bramantyo DF, Octavianus S, et al. : Cancer profile in North Jakarta and Kepulauan Seribu: A 5-year descriptive study. Radioter Onkol Indones 9:48-53, 2018 [Google Scholar]
- 13.Gondhowiardjo S, Hanum FJ, Hanifah R, et al. : Cancer profile in East Jakarta: A 5-year descriptive study. Radioter Onkol Indones 9(2):54-60, 2018 [Google Scholar]
- 14.Gondhowiardjo S, Raharjo FB, Hudiya E, et al. : Cancer profile in South Jakarta: A 5-year descriptive study. Radioter Onkol Indones 9:61-68, 2018 [Google Scholar]
- 15.Kimman M, Norman R, Jan S, et al. : The burden of cancer in member countries of the Association of Southeast Asian Nations (ASEAN). Asian Pac J Cancer Prev 13:411-420, 2012 [DOI] [PubMed] [Google Scholar]
- 16.Manan AA, Ibrahim Tamin NS, Abdullah NH, et al. : Malaysian National Cancer Registry Report 2007-2011. Putrajaya, Malaysia, National Cancer Institute, Ministry of Health, 2016 [Google Scholar]