INTRODUCTION
Although the COVID-19 pandemic quickly emerged in several countries, the first cases did not appear in Brazil until March 2020, when several clusters appeared in heavily populated areas, such as São Paulo and Rio de Janeiro. Based on international recommendations and examples, Brazil responded with a plan focused on social distancing and health-care prioritization.1
CONTEXT
Key Objective
Would changes in the public health system caused by the COVID-19 pandemic have an impact on cancer care?
Knowledge Generated
During the March to May period, we saw a decrease of biopsies (29%), colonoscopies (57%), mammograms (55%), and oncologic surgeries (9%).
Analyzed data also showed a reduction of 21% in the number of hospitalizations. By contrast, there was an increase of 14% in the in-hospital mortality rate.
Relevance
These results can be used as a source of information to guide public health system plans to improve cancer care in Brazil in the post-pandemic period.
In addition to the immense increase in patients infected with SARS-CoV-2 and a high number of related deaths, an inevitable reality was the mortality from other diseases, such as cancer. Notably, the COVID-19 pandemic has threatened patients with cancer in several ways.2 Because of their associated immunocompromised status, malignancies have been reported to increase the risk of COVID-19, and these diseases represent an independent risk factor for more serious harmful effects.3 Moreover, the use of systemic treatment, such as chemotherapy and targeted therapy, and the need for visits to hospitals and health-care facilities might place patients with cancer and their relatives at higher risk of infection.4
Notably, the heterogeneous Brazilian health-care system has been substantially affected by COVID-19. Hence, as observed in other countries, the pandemic might result in delayed diagnosis and suboptimal care for people with cancer. The complexity of cancer had already imposed significant challenges on the health-care systems struggling with restricted resources. However, the additional burden of the pandemic has caused cancellation or delay in screening tests and consultations with specialists. Nonetheless, to prioritize resources to preserve capacity for patients with COVID-19 in a scenario of historical constraints, elective cancer treatments have been postponed, increasing the already prolonged wait times, and the hospitalization of patients with cancer has been avoided.5-7
Brazil is an epicenter of the COVID-19 pandemic. Although the impact of the pandemic on oncology care is noticeable, no comparisons with historical trends have been reported. Understanding the effects of COVID-19 on patients with cancer and oncological care in Brazil could help predict the pandemic’s influence on life-threatening conditions worldwide. Hence, this study examined the changes in the number of cancer-related procedures and hospitalizations and the mortality rate during the COVID-19 pandemic.
METHODS
This observational study of time series data analyzed the procedures and hospitalizations associated with conditions related to neoplasms as recorded by Brazil’s National Health System (Sistema Único de Saúde [SUS]). The study periods were March through May each year between 2016 and 2020. SUS is a universal and completely integrated public health system that includes the entire Brazilian population.
Data were collected from the SUS Hospital and Ambulatory Information Systems using the DATASUS (Departamento de Informática do Sistema Único de Saúde) platform—a public database that does not record personal identification—per article I of resolution 510/2016 of the National Ethics Commission in Research.
Furthermore, to assess the number of procedures related to neoplasms, the codes of the Management System of the Table of Procedures, Drugs and Orthotics, Prostheses and Materials of SUS were used. In addition, the hospital and ambulatory production of each procedure were added and categorized as follows: (1) diagnostic procedures: biopsy, colonoscopy, and mammography; (2) therapeutic procedures: bone marrow transplant, chemotherapy, hormone therapy, and surgery.
This categorization might help differentiate the short-term and long-term effects of the pandemic on therapeutic and diagnostic procedures. Moreover, it is worth mentioning that radiotherapy was not included in this study because there was a change related to its registration in the system in 2019.
Concerning hospitalizations related to neoplasms, only records matching chapter II of the List of Morbidity of the Tenth Review of the International Statistical Classification of Diseases and Related Health Problems were selected. In addition, these analyses comprised the mortality rates associated with these hospitalizations.
Statistical Analysis
A descriptive analysis of the procedures was performed for diagnostic and therapeutic categories according to the procedure type and region (North, Northeast, Southeast, South, and Midwest). Regarding hospitalizations and deaths, variables such as sex, age (0-19, 20-59, and ≥ 60 years), ethnicity (White, Black, Brown, Indigenous, Asian, and no information), and extent of urgency (elective or urgent) were considered.
Nevertheless, to grasp the actual impact of the pandemic on cancer care, assessing the variation in the registered numbers between 2019 and 2020 is not sufficient because a hypothetical fluctuation might occur, owing to trends already established during the previous years. Therefore, a linear regression was performed using data from 2016 to 2019 to detect the trend and estimate the expected value in 2020. The estimation was then tested against the registered value in 2020. Hence, if the values were statistically different, the difference recorded in 2020 was not attributable to the trend or chance.
Such statistical analyses were applied using the number of procedures and hospitalizations during March through May 2020 (the months in which the effects of the pandemic were the most severe in Brazil). In addition, analyses were performed for each procedure individually and the total number of diagnostic and therapeutic procedures. Similar analyses were performed for hospitalizations, deaths, and mortality rates among age groups, regions, and ethnicities.
Because the linear regression presents a Gaussian error, Student’s t-test was performed to compare the projected values with those recorded in 2020. The null hypothesis was rejected at P < .05. Microsoft Excel and Scilab 6.1.0 were used to perform statistical analysis and create tabs and graphs.
RESULTS
Overall, 10,031,625 procedures (5,836,393 diagnostic and 4,195,232 therapeutic), 994,828 hospitalizations, and 84,460 deaths were surveyed.
Hereafter, the presentation of the results focuses on the percentage variation between the projected and registered value in 2020, indicating the magnitude of this fluctuation and the statistical significance of the discrepancy. Detailed data concerning the analyses stratified based on age, ethnicity, and region are presented in the Data Supplement.
Diagnostic Procedures
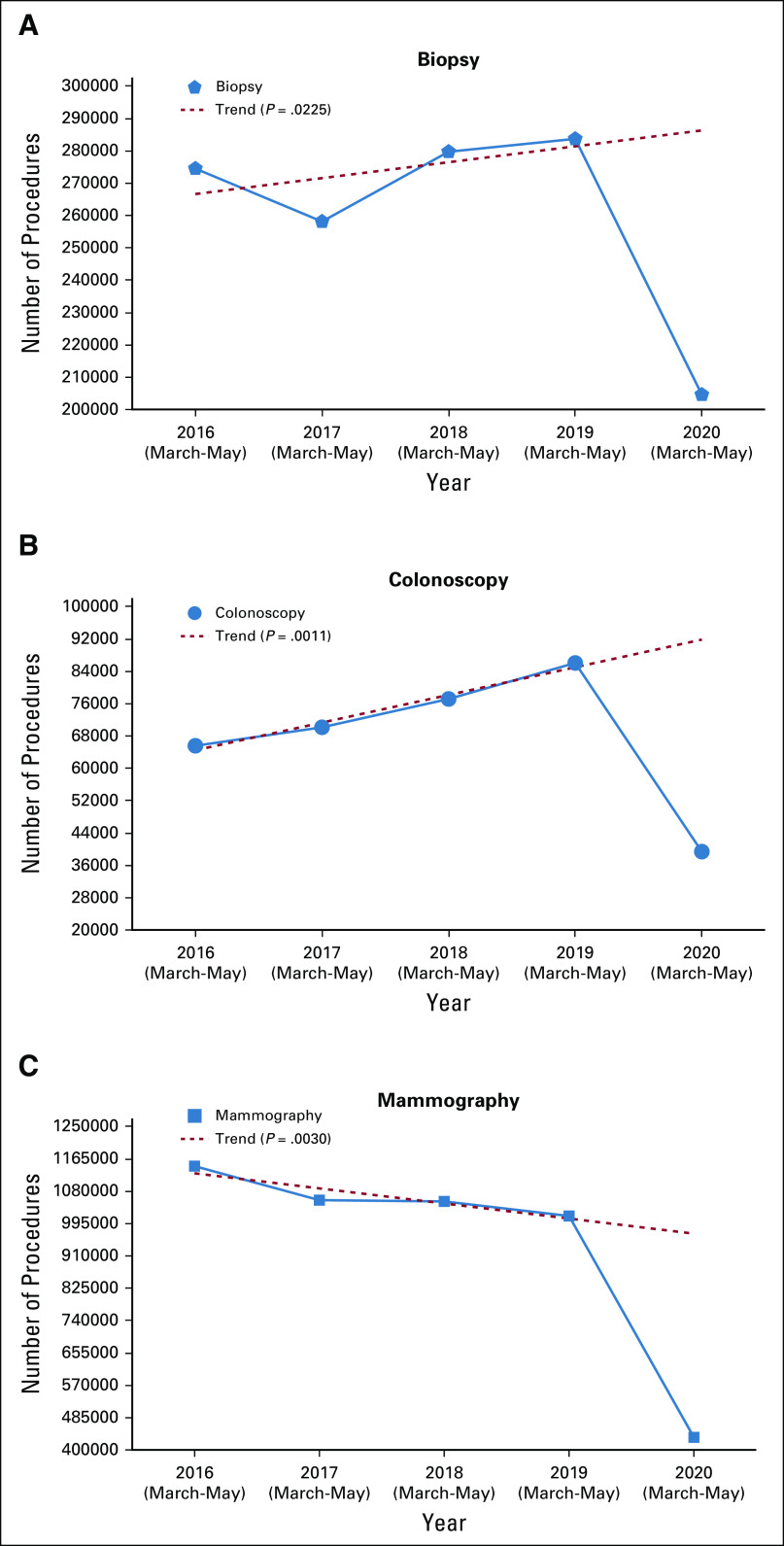
The number of registered diagnostic procedures performed in 2020 was 50% lower than the estimated value (P = .0041). For specific procedures, the registered numbers of biopsies, colonoscopies, and mammograms were reduced by 29% (P = .0225), 57% (P = .0011), and 55% (P = .0030), respectively, compared with the expected values (Fig 1).
FIG 1.
Analysis of the trend of the number of diagnostic procedures in oncology between March and May each year from 2016 to 2020: (a) biopsy, (b) colonoscopy, and (c) mammography.
The analysis data stratified based on the region revealed a more profound decrease in the number of diagnostic procedures in the Northeast region. The total number of procedures was reduced by 55%, and the numbers of biopsies, colonoscopies, and mammograms were reduced by 42% (P = .0141), 71% (P = .0029), and 58% (P = .0217), respectively (Data Supplement).
Therapeutic Procedures
Overall, the number of therapeutic procedures was 7% lower than expected (P = .0398), in line with the 9% reduction in oncological surgeries (P = .0316).
The number of bone marrow transplants performed in 2020 matched the predicted value. Likewise, the use of chemotherapy did not significantly deviate from the expectation. Contrarily, a discrepancy was observed between the estimated and registered use of hormonal therapy (P = .0440). Although its use remained stable in 2020 compared with that a year ago, a strong ascending trend was noted. In addition, the number of surgical procedures deviated from the expectation, with the number of procedures declining in 2020, in contrast to the rising trend in the preceding years (Fig 2).
FIG 2.
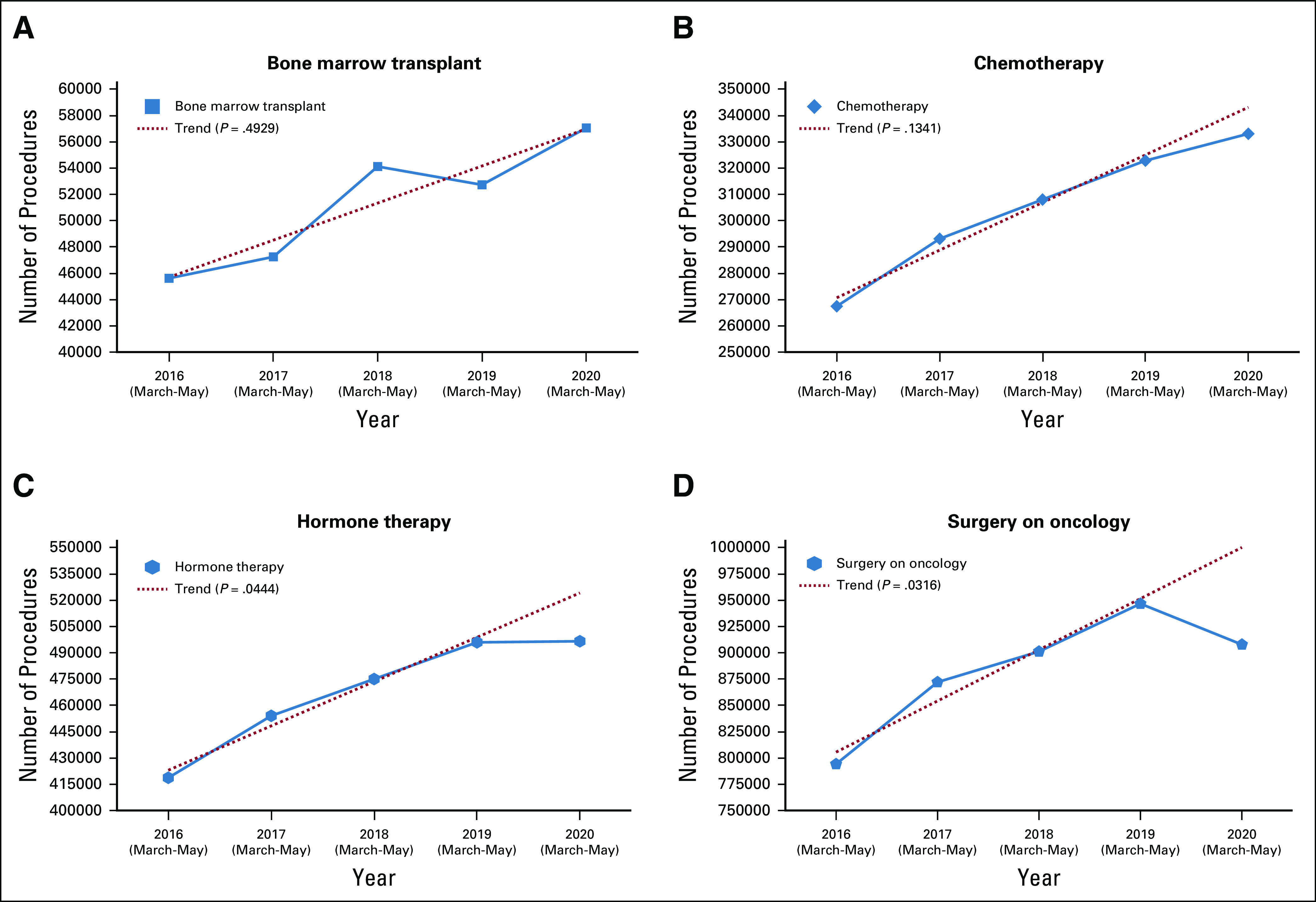
Analysis of the trend of the number of therapeutic procedures in oncology between March and May each year from 2016 to 2020: (a) bone marrow transplant, (b) chemotherapy, (c) hormone therapy, and (d) surgery.
Regarding the analysis based on region, the most significant decline in therapeutic procedures occurred in North Brazil (26%, P = .0250). These data are presented in detail in the Data Supplement.
Hospitalizations and Mortality Rate
The number of hospitalizations increased in previous years, whereas the mortality rate declined. However, opposite trends were observed in 2020. The number of hospitalizations for neoplasms decreased by 21% in 2020 compared with the estimated value (P = .0014), whereas the mortality rate of hospitalized patients with cancer rose by 14% (P = .0152, Fig 3).
FIG 3.
Comparative analysis of the trends of the number of hospitalizations and the mortality rate during March through May each year from 2016 to 2020.
Regarding ethnicity, the largest increases in the number of hospitalizations relative to expectations were recorded for Indigenous (43%, P = .0020) and Asian patients (36%, P = .0405). Regional analysis revealed that the North (35%, P = .0006) and Northeast regions (26%, P = .0026) had the largest decrease in hospitalizations. In addition, the largest increase in mortality was observed in the Northeast region (22%, P = .0237). Regarding age-based analysis, a large reduction in hospitalizations was observed among patients 20-59 years of age (24%, P = .0025), and the mortality rate was 23% higher than expected (P = .0133). The detailed results of hospitalizations for neoplasms based on ethnicity, region, and age are presented in the Data Supplement.
DISCUSSION
As a population-based retrospective analysis, this study could not confirm the cause-effect relationship between the SARS-CoV-2 outbreak and the number of cancer-related procedures. However, it is well known that cancer care has been affected directly and indirectly by the COVID-19 pandemic. Compared with the general population, the COVID-19–specific mortality rate is higher among patients with cancer, exceeding 20% in some series.8,9 Indirectly, the overload on the health system has caused several changes in the daily practice in cancer treatment centers. Worldwide protocols were modified to reduce the frequency of visits or degree of immunosuppression to maintain oncology services during the pandemic.10
In this study, the most apparent effect was observed on diagnostic procedures, the numbers of which were significantly reduced. Because resources had to be redirected to support the care of infected patients to avoid a complete health system collapse, nonurgent procedures were postponed. Screening programs were dramatically affected, including those for cervix, breast, and prostate cancers. In addition, elective diagnostic procedures, such as upper endoscopies and colonoscopies, were delayed because of the risk of aerosol generation or the prolonged fecal shedding of the virus. Hence, without diagnostic examinations, the number of early-stage diagnoses is expected to be reduced.11 This situation is an additional concern because more patients will consequently be diagnosed with more advanced disease.
Regarding therapeutic procedures, no decrease was noted in the use of chemotherapy and bone marrow transplantation at the time of this analysis, probably because those treatments are being applied in previously diagnosed patients. The decrease in the number of treatment procedures would perhaps occur later. Typically, surgery is an earlier procedure in patients with cancer, and we have already observed a large decrease in its use.
Brazil is a country with continental dimensions and a heterogeneous distribution concerning the development index. North and Northeast Brazil are regions with fewer economic resources, and these regions had larger decreases in the number of diagnostic procedures and higher in-hospital mortality rates. Because of its dimensions, Brazil had a nonuniform peak of the incidence of infection, with different regions going through different stages of the pandemic. The North region was one of the first regions to have a peak incidence of COVID-19 and experienced a collapse of the health system. Hence, this fact can explain the significant reduction in the number of treatment procedures in this region.
Notably, the mortality rate increased in 2020 compared with the projected value. Therefore, we can infer that the hospitalized patients had worsened clinical conditions, most likely because of reduced access to and availability of diagnostic services and because a large number of patients avoided health-care services over fears of contracting the SARS-CoV-2 infection, thereby worsening their oncologic disease. Furthermore, the analyzed data revealed a greater reduction in hospitalization rates among young adults, indicating that the hospitalized population during the pandemic was older than the historical controls, probably resulting in a higher mortality rate.
In an elegant population-based modeling study, a group from the United Kingdom forecast an increase in avoidable cancer deaths for four major tumor types—breast, colorectal, lung, and esophageal—because of diagnostic delays attributable to COVID-19. The researchers projected an additional 3,291-3,621 deaths, including an increase of up to 16.6% in colorectal cancer mortality.12 However, it is too soon to measure the actual impact of COVID-19 on the survival of patients with cancer.
In conclusion, to the best of our knowledge, this is the most extensive study regarding cancer care during the COVID-19 pandemic in Brazil. We observed that the pandemic has dramatically affected the public health system, including a decrease in the number of diagnostic procedures and the availability of hospital beds and a significant increase in the in-hospital mortality rate.
AUTHOR CONTRIBUTIONS
Conception and design: Gabriela A. Fonseca, Paulo G. Normando, Luiz Victor M. Loureiro, Rodrigo E. F. Rodrigues, Marcelo D. T. Melo, Iuri Amorim de Santana
Administrative support: Marcelo D. T. Melo
Collection and assembly of data: Gabriela A. Fonseca, Paulo G. Normando, Rodrigo E. F. Rodrigues, Victor A. OliveiraIuri, Amorim de Santana
Data analysis and interpretation: Gabriela A. Fonseca, Paulo G. Normando, Rodrigo E. F. Rodrigues, Marcelo D. T. Melo
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS’ DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO’s conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/go/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Iuri Amorim de Santana
Speakers' Bureau: Boehringer Ingelheim
Travel, Accommodations, Expenses: MSD Oncology
No other potential conflicts of interest were reported.
REFERENCES
- 1.Sternberg C, Andrade TL, Nova APGAV, et al. : Oncology practice during COVID-19 pandemic: A fast response is the best response. Revista da Associação Médica Brasileira 66:338-344, 2020 [DOI] [PubMed] [Google Scholar]
- 2.de Joode K, Dumoulin DW, Engelen V, et al. : Impact of the coronavirus disease 2019 pandemic on cancer treatment: The patients’ perspective. Eur J Cancer 136:132-139, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kuderer NM, Choueiri TK, Shah DP, et al. : Clinical impact of COVID-19 on patients with cancer (CCC19): A cohort study. Lancet 395:1907-1918, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhou F, Yu T, Du R, et al. : Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 395:1054-1062, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sharpless NE: COVID-19 and cancer. Science 368:1290, 2020 [DOI] [PubMed] [Google Scholar]
- 6.van de Haar J, Hoes LR, Coles CE, et al. : Caring for patients with cancer in the COVID-19 era. Nat Med 26:665-671, 2020 [DOI] [PubMed] [Google Scholar]
- 7.Sud A, Torr B, Jones ME, et al. : Effect of delays in the 2-week-wait cancer referral pathway during the COVID-19 pandemic on cancer survival in the UK: A modelling study. Lancet Oncol 21:P1035-P1044, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miyashita H, Mikami T, Chopra N, et al. : Do patients with cancer have a poorer prognosis of COVID-19? An experience in New York City. Ann Oncol 31:1088-1089, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mehta V, Goel S, Kabarriti R, et al. : Case fatality rate of cancer patients with COVID-19 in a New York hospital system. Cancer Discov 10:935-941, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pramesh CS, Badwe RA: Cancer Management in India during Covid-19. N Engl J Med 382:e61, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dinmohamed AG, Visser O, Verhoeven RHA, et al. : Fewer cancer diagnoses during the COVID-19 epidemic in the Netherlands. Lancet Oncol 21:750-751, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maringe C, Spicer J, Morris M, et al. : The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: A national, population-based, modelling study. Lancet Oncol 21:1023-1034, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]