Abstract
Introduction
Use of virtual reality (VR) in healthcare has expanded in recent years. The challenges faced by patients with prolonged COVID-19-related hospitalizations – social isolation, disability, neurologic sequelae, adjustment-related anxiety, depression, and stress – may be mitigated by the novel use of VR as one modality of a comprehensive rehabilitation plan. This descriptive study aimed to understand patient satisfaction and perceived benefit of virtual reality on a COVID-19 recovery unit, as well as the logistical and operational feasibility of providing VR content for patients and staff.
Materials and methods
During the COVID-19 surge in New York City in 2020, the COVID-19 Recovery Unit (CRU) of a large academic hospital invited patients and staff to participate in VR sessions with three categories of experience: (1) Guided meditation, (2) Exploration of natural environments, (3) Cognitive stimulation games. Patients and staff were surveyed about satisfaction and perceived benefit.
Results
13 patients and 11 staff were surveyed, with median patient satisfaction scores of 9 out of 10, with ten representing “extremely satisfied,” and median staff satisfaction scores of 10. 13/13 patients answered “yes” to recommending the therapy to others, and 12/13 answered “yes” to perceived enhancement of their treatment. 11/11 staff answered “yes” to recommending the therapy to others, and 11/11 answered “yes” to perceived enhancement of their wellbeing.
Discussion
A VR program implemented on a COVID-19 rehabilitation unit for patients and healthcare providers was rated as highly satisfactory with perceived benefit by survey respondents. Participants commented that the use of VR was useful in coping with isolation and loneliness, and could be implemented within the context of clinical care for COVID-19 patients as part of a comprehensive rehabilitation model. The use of VR was also logistically and operationally feasible on the CRU. Future work to compare benefits of VR to standard neuropsychological rehabilitation is needed.
Keywords: Virtual reality, COVID-19, Inpatient rehabilitation, Mindfulness
1. Introduction
For survivors of COVID-19 respiratory failure and critical illness, the process of recovery remains arduous, with many facing profound end-organ damage, neurocognitive deficits, malnutrition and dysphagia, physical and occupational debility, anxiety, depression, and other sequelae that can require prolonged hospitalizations and ongoing rehabilitation post hospitalization. The prolonged illness and recovery time of COVID-19, coupled with infection prevention measures that make on-site family visits or travel “off unit” difficult or contraindicated, worsens social isolation and loneliness [1], which are known to heighten risk of dementia [2], cognitive decline [3], poor psychiatric outcomes [4], and premature death from every cause [5]. Moreover, the course of COVID-19 illness encapsulates a myriad of symptoms including myalgias, arthralgias, malaise, and weakness; therefore therapeutic modalities that help alleviate these symptoms and help patients cope with changes in functional status are particularly desirable [6]. While patients may benefit from an integrated approach to address COVID-19, this is generally not readily available in the inpatient setting due to inadequate access to integrative health providers and suboptimal resources, particularly during the COVID-19 pandemic.
Mindfulness-based therapies and meditation are increasingly being used as an adjunctive therapy for a variety of clinical reasons, including chronic pain [7,8] emotional regulation, gastrointestinal symptoms, and others. In times of isolation and limited resources, virtual reality (VR) may serve as a vehicle to increase access to these therapies in various health care settings. VR has been studied as a tool for mental health disorders, [9,10] specific motor impairments [11], as well as for enhancing patient motivation and engagement with overall therapeutic goals [12]. Studies have also utilized VR as a tool for acute and chronic pain management due to its properties as a distraction technique, with other studies demonstrating the potential for neuromodulatory effects on pain as well. [[13], [14], [15], [16]] Using VR as a vehicle to teach coping skills and relaxation techniques may also promote independent learning, thereby increasing self-efficacy. Patients may find it to be more engaging than conventional modalities for delivering mindfulness-based interventions, which have been shown to alleviate depression, anxiety, and stress. [[17], [18], [19], [20]]
Emerging research indicates a significant psychiatric burden in recovering COVID-19 patients, [21,22] and novel modalities to mitigate these effects may help reduce this severity. A significant gap in the literature exists regarding use of VR for COVID-19 patients and specifically for COVID-19 patients in the acute rehabilitation setting, both with regards to implementation strategies and acceptability to patients. This study aimed to explore these aspects, though a broad range of work remains to be done.
A COVID-19 Recovery Unit (CRU) was created at NewYork-Presbyterian/Weill Cornell in April 2020 to provide comprehensive care to patients recovering from COVID-19 related illness during the pandemic crisis [23]. The 28-bed unit is a novel hybrid medical-rehabilitation floor. Key team members included clinicians from Hospital Medicine, Physical Medicine and Rehabilitation (PM&R), Nursing, Neurology, Psychiatry and Psychology, among others. In this innovation report, we describe the logistical and operational feasibility of implementing VR and report patient and provider satisfaction and perceived benefit of the program.
During the first wave of the COVID-19 pandemic in New York City in the spring of 2020, the impact of the pandemic on both patients and healthcare workers was immediate and extreme, with structural ramifications felt in all aspects of the hospital. The crisis of overwork and isolation for healthcare workers, as well as the collective trauma experienced by patients and providers, has been richly described [24]. For this reason, we offered employees the use of this VR tool, and in this report we also describe satisfaction and perceived benefit among the unit's healthcare workers, as well as among patients.
2. Materials and methods
This VR clinical tool from AppliedVR was implemented at NewYork-Presbyterian/Weill Cornell Medical Center, a large academic medical center in New York City, the initial epicenter of the COVID-19 pandemic in the United States. Patient participants were patients of this 28-bed unit, who were all receiving inpatient acute rehabilitation for sequelae of critical illness following COVID-19 infection. Healthcare workers and staff of the COVID-19 Recovery Unit were also able to participate in the use of the VR tool for their own wellness.
Patients in the COVID-19 Recovery Unit were admitted on the basis of the following inclusion criteria: (1) inpatients with positive COVID-19 PCR test during hospitalization, (2) medical team deems patient medically stable and has ongoing medical and rehabilitative needs, (3) able to tolerate >30+ min PT/OT each daily, (4) PT or OT recommendation for Acute or Subacute rehab at time of discharge, (5) anticipation of remaining in hospital/rehab for ≥1 week, (6) no active suicidal ideation, severe dementia & active delirium, or 1:1 observation required (7) must have non-invasive oxygen needs of 6 L or fewer, or in case of tracheostomy patients have achieved “trach collaring” with anticipated ability to downsize/decannulate. Patients and staff were made aware of the VR intervention through daily multidisciplinary rounds.
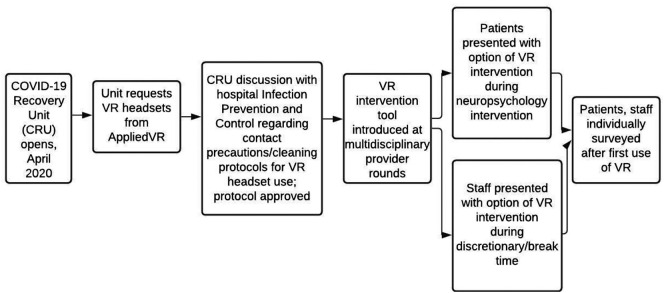
Table 1 describes the patient characteristics via the overarching inclusion criteria for the COVID-19 Recovery Unit at this large urban academic hospital. (See Fig. 1.)
Table 1.
Patient characteristics/inclusion criteria for the COVID-19 recovery unit.
|
|
|
|
|
|
|
Fig. 1.
Flowchart describing implementation of the VR tool within the COVID-19 recovery unit.
2.1. VR tool
The technology used was AppliedVR's SootheVR. The headset, which is commercially available, comes pre-programmed with multiple categories of experience: (1) guided meditation sessions set in highly realistic immersive nature scenes, (2) sessions set in highly realistic natural settings in which patients can passively or actively explore natural and outdoor settings (examples: “swimming” with dolphins, exploring world cities), and (3) cognitive stimulation games (examples: navigating simple mazes, aiming virtual balls towards targets). In appearance, the modules were three-dimensional soothing natural settings (examples: a coastline, underwater, a field in twilight). Patients had the option of exploring these games if they so chose, but were not given tasks to fulfill, in order to maintain their autonomy as a therapeutic aspect of their experience with the neuropsychologist. Patients were offered sessions of up to 30 min (the limit advised by the manufacturer) with a VR headset provided by AppliedVR. Patients typically completed no more than one module per session, thus actual time with VR headset on was generally closer to about 10 min. Fig. 2 depicts sample backgrounds associated with specific modules available within SootheVR.
Fig. 2.
Sample backgrounds of VR modules offered.
Upper left: “Tibetan singing bowl,” Upper right: “Swim with dolphins,” Bottom left: “Bear blast borealis,” Bottom right: “Breathing life.”
This VR tool was offered in the inpatient CRU: in the context of guided use with neuropsychologist staff, or with independent use following an introduction to VR. Following the patient's first use of the VR tool, they were then offered a survey. The subsequent experiences that patients had with the VR tool were not re-surveyed. There were typically three headsets available which could be shared among patients in the context of their group activities, or in the context of individual use.
Infection control measures included use of PPE, disinfection of each headset between use, and separate headsets for COVID-19 recovery patients and staff. For safety, patients were monitored the entire time by unit neuropsychologists, and patient use of the VR headset was guided by proprietary manufacturer recommendations. The neuropsychologists helped patients reflect and debrief on their emotional experiences.
Patients who wished to use the VR headset were free to choose which module(s) they wished to experience among the VR tool's offerings. This was done to provide patients with a sense of autonomy and agency which was frequently diminished during their prolonged hospitalization. Unfortunately, this limited comparative analysis of the different VR content that was used.
One headset was reserved for the use of clinicians and staff of the CRU to allow firsthand experience of the therapy received by patients. Staff had the option of either experiencing VR mindfulness therapy in a guided format led by a dedicated neuropsychologist, or of self-directing their VR experience during break times at their own discretion. For self-directed experiences, staff were not given specific instructions regarding the duration of a VR experience, although the program was advertised with a banner including the phrase “Have ten minutes?” in an effort to be mindful of the staff's limited break time and competing needs for other forms of self-care (eating meals, etc).
AppliedVR currently provides software only in English, limiting full participation to patients with English proficiency (although non-English speakers could still participate in the experiential relaxation models, which are non-verbal). Patients needed to demonstrate enough head and neck strength to wear the headsets comfortably, and sufficiently oriented mental status to be trained in VR navigation and communication of needs during the sessions. The headsets were contraindicated for patients with a history of seizures. Per the manufacturer's recommendations, patients were advised not to use the headsets for intervals longer than 30 min at a time, as this could lead to excessive eye strain.
The aim of this clinical innovation was to understand patient satisfaction and perceived benefit of virtual reality on a COVID-19 recovery unit, as well as the logistical and operational feasibility of providing VR content for patients and staff on this unit.
2.2. Survey tool
The survey tool designed to understand satisfaction and perceived benefit of VR to patients and staff was a simple 4-item survey. Table 2 provides survey questions for patients and staff.
Table 2.
Survey questions administered to patients and staff.
| Patient survey items |
| “How satisfied were you with the virtual reality tool in managing your pain or anxiety?” (1–10, 1 = “not at all satisfied,” 10 = “extremely satisfied”) |
| “Would you recommend the virtual reality tool to other patients?” (yes/no/maybe) |
| “Do you feel like virtual reality added to, or enhanced, your treatment?” (yes/no) |
| “Is there anything else you would like to share about the virtual reality tool?” (free text) |
| Staff survey items |
| “How satisfied were you with the virtual reality tool in managing stress?” (1–10, 1 = “not at all satisfied,” 10 = “extremely satisfied”) |
| “Would you recommend the virtual reality tool to other staff for wellness/stress management?” (yes/no/maybe) |
| “Do you feel like virtual reality added to, or enhanced, your wellbeing at work?” (yes/no) |
| “Is there anything else you would like to share about the virtual reality tool?” (free text) |
As this was a clinical innovation, the Weill Cornell Medicine Institutional Review Board determined that IRB approval was not required for this project.
3. Results
Responses among patients to the VR experience were markedly positive, with patients reporting a median satisfaction of 9, mean of 8.42 (range: 5–10) on a scale of 1–10. Staff had an even more positive response, reporting a median satisfaction of 10, mean of 9.45 (range: 8–10). All patients except for one, and all staff, reported that VR enhanced treatment and well-being, respectively. All recommended VR for further use. All patients and staff who chose to experience the VR tool were willing to subsequently complete surveys (100%).
Table 3 lists the responses to questions and rating scales employed in assessing patient and staff satisfaction and feedback.
Table 3.
Survey responses by patient participants and staff participants.
| Patient self-report |
Staff self-report |
||||
|---|---|---|---|---|---|
| Satisfaction (1−10) | Recommend? (Y/N/Maybe) | Enhanced treatment? (Y/N) | Satisfaction (1–10) | Recommend? (Y/N/Maybe) | Enhanced well-being? (Y/N) |
| 9 | Y | Y | 8 | Y | Y |
| 10 | Y | N | 9 | Y | Y |
| 10 | Y | Y | 10 | Y | Y |
| 10 | Y | Y | 9 | Y | Y |
| 10 | Y | Y | 10 | Y | y |
| 6.5 | Y | Y | 10 | Y | Y |
| 10 | Y | Y | 10 | Y | Y |
| 8 | Y | Y | 10 | Y | Y |
| 9 | Y | Y | 9 | Y | Y |
| 8 | Y | Y | 10 | Y | Y |
| 5 | Y | Y | 9 | Y | Y |
| 7 | Y | Y | Mean: 9.45 Median: 10 | 11/11 “Y” | 11/11 “Y” |
| 7 | Y | Y | |||
| Mean: 8.42 Median: 9 | 13/13 “Y” | 12/13 “Y” | |||
Themes that emerged from patients' free text responses to VR use included ideas of “travel” and “escape,” whereby the experience allowed patients to imagine themselves outside the confines of the hospital. Staff also emphasized the tool's utility as a way of enhancing coping and self-care. Staff noted that conditions in the hospital, even after the peak pandemic surge in our region, remained high-stress and fast-paced, with ongoing challenges particular to the COVID-19 era.
Finally, qualitative observations from neuropsychology staff who assisted patients indicated that patients were highly engaged and immersed in the experience, and frequently and spontaneously commented about the excitement of using the VR headset. Neuropsychologists noted that patients who initially expressed skepticism about the technology developed interest and enthusiasm over time, often after discussing with peers during group sessions and opportunities for socialization. These direct clinical observations were made by staff and are considered hypothesis-generating. The only surveyed encounter was each patient's first encounter with the VR intervention, rather than subsequent re-encounters. There were no side effects or adverse events noted by patients or clinicians.
Table 4 gives examples of free responses offered by patients and staff in response to their VR experiences.
Table 4.
Patient and staff comments on free-response section of survey.
| Patient feedback | Staff feedback |
|---|---|
| “I was curious. I traveled away from my present problems and illness.” | “Excellent escape and immersive experience, providing access to things that don't feel as accessible in this present climate.” |
| “I enjoyed it and would do it again.” | “6 min to shut your mind off and go to a different place. Super relaxing!” |
| “The more you explain, the better for patients; [I could see this being used] as an escape from unpleasant medical procedures.” | “It allows you to escape from the real world. Although it was only a couple of minutes, I really enjoyed it.” |
| “It will help others feel connected with what they see on the VR.” | “Great coping. Brings a certain zen to a hectic day at work.” |
| “Made me feel more relaxed. I felt like I was in London. It was nice to see people.” | “The opportunity to pause and care for myself is a welcomed and necessary intervention.” |
| “Make my brain feel sharper. I feel like this helps me feel more alert.” | “Amazing escape to reset and recharge. Would be nice to have the full experience of a relaxation room, ex. dimmed lights, aromatherapy.” |
4. Discussion
In this exploratory phase and preliminary clinical innovation of the novel use of virtual reality (VR) as part of an integrative care delivery model on a COVID-19 recovery unit (CRU), feedback was considered hypothesis-generating rather than evaluating efficacy. Two themes emerged from feedback by patients and staff members in the CRU: the use of VR could be implemented within the context of clinical care for COVID-19 patients, and that both patients and staff members reported overall positive satisfaction and perceived benefit with VR as part of a comprehensive rehabilitation model.
VR in the healthcare setting has expanded in recent years, serving as an educational tool, a distraction measure for pain, and as an additional modality to deliver evidence-based interventions such as mindfulness in neurorehabilitation and psychotherapy. In the present study, there was a strongly positive response to the introduction of this innovation in a hybrid medicine-rehabilitation inpatient unit. The complexity of the COVID-19 illness and associated isolation during this pandemic poses many obstacles. Many patients on this unit experienced a hospital length of stay exceeding three months – and in accordance with the New York State Department of Health guidelines, visitors were almost entirely restricted from the hospital between late March and late June of 2020. Isolation, confinement, and lack of variety in patients' environment and lifestyle were among the major psychosocial challenges of the pandemic. For some involved in the present study, VR served as an escape, while others felt this was a coping tool. VR served as an additional modality for delivery of experiences that would be otherwise difficult to obtain.
We found that on the provider and program development end, we were able to rapidly implement this VR program on an acute COVID-19 recovery unit. We worked closely with the unit staff and with our hospital's infection prevention and control department. Despite enhanced precautions to prevent infection transmission and ensure patient and provider safety, we found that the VR intervention successfully aligned with Infection Control and general hospital policies regarding COVID-19.
4.1. Limitations
Drawbacks to the evaluation methodology used include response bias or observer–expectancy effect, particularly given that due to staffing constraints during the pandemic, written survey responses were collected by the neuropsychologist staff who administered the VR intervention. Independent researchers and data-collectors without clinical roles were generally restricted from the unit during this time due to Infection Prevention and Control policies. Given patients' overall level of muscle weakness, neuropathy, and other sequelae of COVID-19 critical illness, patients were often unable to fill out feedback forms privately, and instead dictated their responses to unit staff members. Since patients' treatment plans were formulated in this unit in an interdisciplinary, multilateral fashion with multiple providers involved, this concern for bias is somewhat tempered by no sole treatment provider on the unit having an exclusive role in patient care. Next steps in gathering future feedback of this kind could be through trained research assistants who have no further contact with the patient care team, or using voice-activated dictation to collect feedback. In addition to not being able to report feedback independently, independent use of the headset may be difficult in those regaining muscle function and dexterity. There has already been an evolution in the hardware options available over the years, and as technology continues to evolve, ease of use of the headsets will be an important factor to continue assessing.
In this clinical innovation, patients had their choice of which modules to use during their VR experience, and supervising clinicians did not have a method of ascertaining with certainty which modules a patient chose to use. Because of this limitation, we chose not to separate survey data by module-type. Future studies may be able to disaggregate the results of each type of module (relaxation, free exploration, cognitive stimulation) by surveying module types separately and measuring effect separately. On the other hand, this limitation in clinicians' ability to dictate the patient's VR experience may be one aspect of its appeal from the standpoint of patient autonomy.
A further limitation to our implementation design is that we did not perform formal thematic analysis of the patient and staff free-text comments. Given the clinical reality that this was a rapidly implemented program within the first wave of the COVID-19 pandemic in New York, we opted to choose a simpler implementation-focused methodology that would permit us to proceed as rapidly as possible. Future efforts in elucidating the impact of VR-based interventions on acute rehabilitation and/or hospitalized patients would benefit from more formal thematic analysis of participants' unstructured comments.
For both patient and staff participants, small sample size, lack of systematic protocol (including frequency and duration of VR use), and site-designed survey lacking established reliability or validity are all limitations. With regard to healthcare staff use of the VR intervention, additional limitations include staff time pressure posing practical restrictions on their utilization of the VR tool. Moreover, staff used the VR tool in an admittedly different context than patients, via self-directed experience, rather than within a therapeutic session. Future studies on this subject would ideally allot protected additional time (not standard “break time”) for staff to utilize the intervention in the presence of supervising researchers.
5. Conclusions
We found that a VR program implemented on a COVID-19 rehabilitation unit for patients and healthcare providers was rated as highly satisfactory with perceived benefit for enhancing patient treatment and healthcare staff well-being. The acceptance of VR use on the CRU not only made patients more interested in ongoing use, but it has also triggered staff interest in expansion of VR use in the inpatient setting. Next steps could include conducting a prospective study to determine whether exposure to the VR content is associated with improved outcomes, such as mood, anxiety, sleep, pain, and feelings of isolation. COVID-19 has demonstrated the need for creativity and alternative modalities for delivery of healthcare. In addition, next steps would seek to separately measure the comparative effects of different kinds of modules within the VR system, and also measure whether frequency of use impacts patient satisfaction.
Our initial findings that this was a readily implementable, clinically feasible, and patient-accepted therapeutic modality add to the existing literature that VR may be an important complement to more traditional forms of integrative health in the inpatient setting [[11], [12], [13], [14], [15], [16]]. VR may serve as an accessible and immersive way to bring beneficial clinical interventions to hospitalized patients, particularly during the current ongoing presence of COVID-19 throughout the United States and beyond.
CRediT authorship contribution statement
Laura Kolbe: Conceptualization, Writing - original draft, Writing - review & editing. Abhishek Jaywant: Conceptualization, Writing - review & editing, Data curation. Alka Gupta: Conceptualization, Writing - review & editing. W. Michael Vanderlind: Writing - review & editing, Data curation. Gina Jabbour: Conceptualization, Writing - review & editing
Declaration of Competing Interest
Dr. Kolbe, Dr. Jaywant, Dr. Gupta, Dr. Vanderlind, and Dr. Jabbour have nothing to disclose.
Acknowledgments
We thank our colleagues in hospital medicine, physiatry, nursing, physical therapy, occupational therapy, speech language pathology, and social work for creating a strong core team to face the challenges of COVID-19 recovery in the CRU. In particular, the work of physiatry director, Dr. Leroy Lindsay, and Patient Care Director, Michele Dziedzic, was instrumental for creating a workflow that could support and encourage VR and other mindfulness modalities. We thank our consultant colleagues, particularly in neurology and psychiatry, for helping us improve the mental and physical well-being of each patient. We are deeply grateful to AppliedVR for allowing us to use their VR content and providing training and technical support throughout the project. We also thank Karen Wen for administrative support with the study.
Data availability
No data was used for the research described in the article.
References
- 1.Eghtesadi M. Breaking social isolation amidst covid-19: a viewpoint on improving access to technology in long-term care facilities. J Am Geriatr Soc. 2020 May;68(5):949–950. doi: 10.1111/jgs.16478. 32277470 Epub 2020 Apr 24. PMC7262151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sutin A.R., Stephan Y., Luchetti M., Terracciano A. Loneliness and risk of dementia. J Gerontol B Psychol Sci Soc Sci. 2018 Oct 26 doi: 10.1093/geronb/gby112. 30365023 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lara E., Caballero F.F., Rico-Uribe L.A., Olaya B., Haro J.M., Ayuso-Mateos J.L., et al. Are loneliness and social isolation associated with cognitive decline? Int J Geriatr Psychiatry. 2019 Nov;34(11):1613–1622. doi: 10.1002/gps.5174. 31304639 Epub 2019 Jul 25. [DOI] [PubMed] [Google Scholar]
- 4.Wang J., Mann F., Lloyd-Evans B., Ma R., Johnson S. Associations between loneliness and perceived social support and outcomes of mental health problems: a systematic review. BMC Psychiatry. 2018;18(1):156. doi: 10.1186/s12888-018-1736-5. Published 2018 May 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alcaraz K.I., Eddens K.S., Blase J.L., Diver W.R., Patel A.V., Teras L.R., et al. Social isolation and mortality in US Black and White men and women. Am J Epidemiol. 2019 Jan 1;188(1):102–109. doi: 10.1093/aje/kwy231. 30325407 PMC6321805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Widyadharma I.P.E., Sari N.N.S.P., Pradnyaswari K.E., et al. Pain as clinical manifestations of COVID-19 infection and its management in the pandemic era: a literature review. Egypt J Neurol Psychiatry Neurosurg. 2020;56:121. doi: 10.1186/s41983-020-00258-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reiner K., Tibi L., Lipsitz J.D. Do mindfulness-based interventions reduce pain intensity? A critical review of the literature. Pain Med. 2013 Feb;14(2):230–242. doi: 10.1111/pme.12006. Epub 2012 Dec 13. Review. PubMed PMID: 23240921. [DOI] [PubMed] [Google Scholar]
- 8.Zeidan F., Vago D.R. Mindfulness meditation-based pain relief: a mechanistic account. Ann N Y Acad Sci. 2016 Jun;1373(1):114–127. doi: 10.1111/nyas.13153. 27398643 Review. PMC4941786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mitrousia V, Giotakos O. Virtual reality therapy in anxiety disorders. Psychiatriki. 2016 Oct-Dec;27(4):276–286. 10.22365/jpsych.2016.274.276. Review. PubMed PMID: 28114091. [DOI] [PubMed]
- 10.Botella C., Fernández-Álvarez J., Guillén V., García-Palacios A., Baños R. Recent progress in virtual reality exposure therapy for phobias: a systematic review. Curr Psychiatry Rep. 2017 Jul;19(7):42. doi: 10.1007/s11920-017-0788-4. 28540594 Review. PubMed PMID. [DOI] [PubMed] [Google Scholar]
- 11.O’Neil O., Fernandez M.M., Herzog J., Beorchia M., Gower V., Gramatica F., et al. Virtual reality for neurorehabilitation: insights from 3 European clinics. PM R. 2018 Sep;10(9 Suppl 2):S198–S206. doi: 10.1016/j.pmrj.2018.08.375. 30121365 Epub 2018 Aug 16. Review. [DOI] [PubMed] [Google Scholar]
- 12.Kefaliakos A., Pliakos I., Kiekkas P., Charalampidou M., Diomidous M. virtual reality in the rehabilitation of patients with neurological disorders. Stud Health Technol Inform. 2016;226:45–47. 27350462 Review. [PubMed] [Google Scholar]
- 13.Zeidan F., Vago D.R. Mindfulness meditation-based pain relief: a mechanistic account. Ann N Y Acad Sci. 2016 Jun;1373(1):114–127. doi: 10.1111/nyas.13153. 27398643 Review. PMC4941786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zeidan F, Grant JA, Brown CA, McHaffie JG, Coghill RC. Mindfulness meditation-related pain relief: evidence for unique brain mechanisms in the regulation of pain. Neurosci Lett 2012 Jun 29;520(2):165–73. 10.1016/j.neulet.2012.03.082. Epub 2012 Apr 6. Review. PubMed PMID: 22487846; PubMed Central PMCID: PMC3580050. [DOI] [PMC free article] [PubMed]
- 15.Gupta A., Scott K., Dukewich M. Innovative technology using virtual reality in the treatment of pain: does it reduce pain via distraction, or is there more to it? Pain Med. 2018 Jan 1;19(1):151–159. doi: 10.1093/pm/pnx109. 29025113 Review. PubMed PMID. [DOI] [PubMed] [Google Scholar]
- 16.Pourmand A., Davis S., Marchak A., Whiteside T., Sikka N. Virtual reality as a clinical tool for pain management. Curr Pain Headache Rep. 2018 Jun 15;22(8):53. doi: 10.1007/s11916-018-0708-2. 29904806 Review. PubMed PMID. [DOI] [PubMed] [Google Scholar]
- 17.Lamothe M., Rondeau É., Malboeuf-Hurtubise C., Duval M., Sultan S. Outcomes of MBSR or MBSR-based interventions in health care providers: a systematic review with a focus on empathy and emotional competencies. Complement Ther Med. 2016;24:19–28. doi: 10.1016/j.ctim.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 18.Serpa J.G., Taylor S.L., Tillisch K. Mindfulness-based stress reduction (MBSR) reduces anxiety, depression, and suicidal ideation in veterans. Med Care. 2014;52(12):S19–S24. doi: 10.1097/MLR.0000000000000202. [DOI] [PubMed] [Google Scholar]
- 19.Goldin P.R., Gross J.J. Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion. 2010;10(1):83. doi: 10.1037/a0018441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lao S.A., Kissane D., Meadows G. Cognitive effects of MBSR/MBCT: a systematic review of neuropsychological outcomes. Conscious Cogn. 2016;45:109–123. doi: 10.1016/j.concog.2016.08.017. [DOI] [PubMed] [Google Scholar]
- 21.Rogers J.P., Chesney E., Oliver D., Pollak T.A., McGuire P., Fusar-Poli P., et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020 Jul;7(7):611–627. doi: 10.1016/S2215-0366(20)30203-0. Epub 2020 May 18. PubMed PMID: 32437679; PubMed Central PMCID: PMC7234781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Taquet M., Luciano S., Geddes J.R., Harrison P.J. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2020;8(2):130–140. doi: 10.1016/S2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gupta R., Gupta A., Ghosh A.K., Stein J., Lindsay L., Beckley A., et al. A paradigm for the pandemic: a COVID-19 recovery unit. NEJM Catalyst. 2020 May 29 doi: 10.1056/CAT.20.0238. [DOI] [Google Scholar]
- 24.Resnick K.S., Fins J.J. Professionalism and resilience after COVID-19. Acad Psychiatry. 2021 March 2 doi: 10.1007/s40596-021-01416-z. 33649940 On-line ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data was used for the research described in the article.