Abstract
Precision medicine has grown over the past twenty years with the availability of genetic tests and has changed the one-size-fits-all paradigm in medicine. Precision medicine innovations, such as newly available genetic tests, could potentially widen racial and ethnic disparities if access to them is unequal and if interest to use them differs across groups. The objective of this systematic review was to synthesize existing evidence on racial and ethnic differences in knowledge of and attitudes towards genetic testing among adult patients and the general public in the U.S., focusing on research about the use of genetic testing in general, not disease-specific tests. Twelve articles published in 1997-2017 met inclusion and exclusion criteria, with ten including knowledge variables and seven including attitude variables. Studies found consistent patterns of lower awareness of genetic testing in general among non-Whites compared to Whites, lower factual knowledge scores among Blacks and Hispanics/Latinos, and mixed findings of differences in awareness of direct-to-consumer (DTC) genetic testing or the term precision medicine. Blacks, Hispanics/Latinos and non-Whites generally had more concerns about genetic testing than Whites. The findings suggest that patients and the general public need access to culturally-appropriate educational material about the use of genetic testing in precision medicine.
Keywords: precision medicine, genetic testing, pharmacogenomics, health disparities, racial, ethnic, knowledge, awareness, minorities, direct-to-consumer
Introduction
Precision medicine has changed the one-size-fits-all healthcare paradigm for preventing, diagnosing, and treating diseases (Aronson & Rehm, 2015). After decades of efforts to identify genes that caused single-gene diseases, the approval of Herceptin Trastuzumab in 1998 to treat metastatic breast cancer patients with over-expressing human epidermal growth factor receptor 2 (HER2) marked a milestone as the first precision medicine treatment made available to patients outside of clinical trials (Avard & Knoppers, 2009; Genentech, 2017; US Food and Drug Administration, 2017). Subsequent advances in genetics and genomic sequencing have offered patients and the general public the opportunity to access a growing number of options for presymptomatic genetic testing to estimate disease risk and pharmacogenomics testing to tailor drug treatment to the genetic makeup of each individual patient (Caselli et al., 2014; Hammer, 2016; Marson, Bertuzzo, & Ribeiro, 2017; Moonesinghe, Jones, Honoré, Truman, & Graham, 2009). In addition to increasing availability in clinical settings, direct-to-consumer (DTC) genetic tests that have been on the market since 2007 allow consumers to access genetic tests directly from private companies without the involvement of a healthcare provider. DTC tests identify genetic variants to inform users about disease risk, so that consumers can work on prevention strategies (Kolor et al., 2012). There is a growing tendency for healthcare facilities to offer more patients’ affordable blood tests that include a variety of specific genetic tests in the same panel, as opposed to offering individual disease-specific tests that are more expensive (Lynch, Venne, & Berse, 2015).
Over the past 20 years, the term precision medicine has evolved from a variety of related terms, such as personalized medicine, individualized medicine, genomic medicine, pharmacogenetics, and pharmacogenomics. The National Institutes of Health defines precision medicine as “an emerging approach for disease treatment and prevention that takes into account individual variability in genes, environment, and lifestyle for each person” (Peer, 2014; U.S. National Library of Medicine, 2017).
Though precision medicine breakthroughs offer the potential to reduce disease burden and mortality, there is also the potential for them to widen existing racial and ethnic health disparities (Smith et al., 2016). Racial and ethnic health disparities in the U.S. have been linked to unequal healthcare access and social determinants of health (SDH), such as discrimination, residential segregation, low education, poverty and income inequality (Galea, Tracy, Hoggatt, Dimaggio, & Karpati, 2011; Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, 2003; Moy & Freeman, 2014). Consistent with the Diffusion of Innovation Theory (Rogers, 2003), which explains how, why, and at what pace new technologies or ideas are disseminated through a society, new medical innovations tend to be disseminated unevenly, benefiting socially advantaged groups more quickly than disadvantaged groups, such as racial and ethnic minorities. Therefore, given the limited access to healthcare among racial and ethnic minorities, access to newly available genetic tests within the context of precision medicine may be also limited (Fine, Ibrahim, & Thomas, 2005; Moonesinghe et al., 2009). Hispanics/Latinos and African Americans, are less likely to use certain genetic and genomic tests when offered (Armstrong, Micco, Carney, Stopfer, & Putt, 2005; Butrick et al., 2015; Hall et al., 2012; Muller et al., 2018; Susswein et al., 2008). Taken together these factors have the potential to exacerbate existing racial and ethnic health disparities (Levine et al., 2007, 2008, 2010).
Previous reviews have focused on racial and ethnic differences in knowledge and attitudes toward disease-specific genetic testing (Collins, Ryan, & Truby, 2014; Forman & Hall, 2009; Chanita Hughes Halbert, Kessler, & Mitchell, 2005; Hann et al., 2017; Lawrence & Appelbaum, 2011). To date, no systematic review has been conducted on the topic of racial and ethnic differences in knowledge of and attitudes towards genetic testing in general. It is important to understand patterns in people’s general knowledge and attitudes about genetic testing since they would likely influence their willingness to accept either multigene panel testing, disease-specific testing, or DTC testing. This information is crucial to identify strategies to educate patients and the general public to make informed decisions about the use of genetic testing as part of their healthcare, so that all groups can benefit equally from advances in precision medicine. General knowledge and attitudes about genetic testing could also affect the willingness of underrepresented groups to participate in research involving genetic testing or large precision medicine initiatives, such as the national All of Us Research Program (National Institutes of Health, 2018). The objective of this systematic review was to synthesize existing evidence on racial and ethnic differences in knowledge and attitudes about genetic testing in the context of precision medicine among adult patients and the general public in the U.S. This review focused on research about the use of genetic testing in general, not disease-specific tests. Knowledge was considered to include both general awareness and specific factual knowledge. The research questions examined were:
How much do adult patients and the general public know and understand about precision medicine? Are there differences across racial/ethnic groups?
What are the attitudes of adult patients and the general public about the use of precision medicine for clinical care? Are there differences across racial/ethnic groups?
Methods
The protocol for this review was registered in the PROSPERO International Prospective Register of Systematic Reviews, protocol number CRD42017064798 (Canedo, Miller, Myers, & Sanderson, 2017).
Search Strategy
Searches were conducted in PubMed, PsycINFO (Proquest), and CINAHL (EBSCO) databases to identify potentially relevant articles published in peer-reviewed journals. To address negative publication bias, searches for gray literature were conducted in ProQuest Dissertations and Theses Global database, and BMC Proceedings database of scientific meeting presentations. “Gray literature” refers to research reports that are not published in peer-reviewed journals, such as dissertations and scientific conference abstracts (Mahood, Van Eerd, & Irvin, 2014). All searches were conducted for the time period January 1998 to March 2017. The starting year of 1998 was chosen since it was the first year in which a precision medicine treatment was made available to patients (US Food and Drug Administration, 1998). Reference sections of included journal publications and gray literature were also hand searched to identify other potentially relevant articles.
Keywords were combined using Boolean Operators (AND, OR, and NOT) for the searches to include all of the terms used to refer to precision medicine, terms related to knowledge and attitudes, and terms referring to the target adult population. An asterisk was used as a truncation operator, so the search engine would detect any word beginning with the stem of the word before the asterisk. For example, communit* would identify “community” or “communities.” Comprehensive search strings were constructed for each database as follows: [precision medicine, personalized medicine, individualized medicine, genomic medicine, genomic testing, genetic testing, pharmacogenomics, genetic screening] AND [knowledge, understand*, familiar*, awareness, view, attitude, perception*, perceive*, opinion*, belief*, barrier*, facilitator*, benefit*, trust, distrust, mistrust, concern*, fear*, doubt*, skepticism, worry*, worri*] AND [adult*, patient*, communit*, public]. For PubMed, relevant Medical Subject Headings (MeSH) were also included (Precision Medicine OR Pharmacogenetics) AND (Knowledge OR Awareness OR Attitude OR Perception OR Trust OR Fear) AND (Adult OR Patients). See full search strategy in Supplemental Material.
Inclusion and Exclusion Criteria
The inclusion criteria were studies that collected data directly from adult patients or adults in the general public (18 years and older), qualitative or quantitative studies, and studies using observational designs (e.g. surveys, focus groups, interviews). Exclusion criteria were studies that did not include any measures or questions about knowledge or attitudes about precision medicine and related genetic tests; studies that did not report testing racial/ethnic differences in these measures/questions; studies focusing on precision medicine among pediatric patients; studies testing an intervention using an experimental design; and editorials or review articles. Studies using an experimental design were excluded since the objective was to characterize the existing patterns of knowledge and attitudes without the influence of specific interventions.
Study Selection
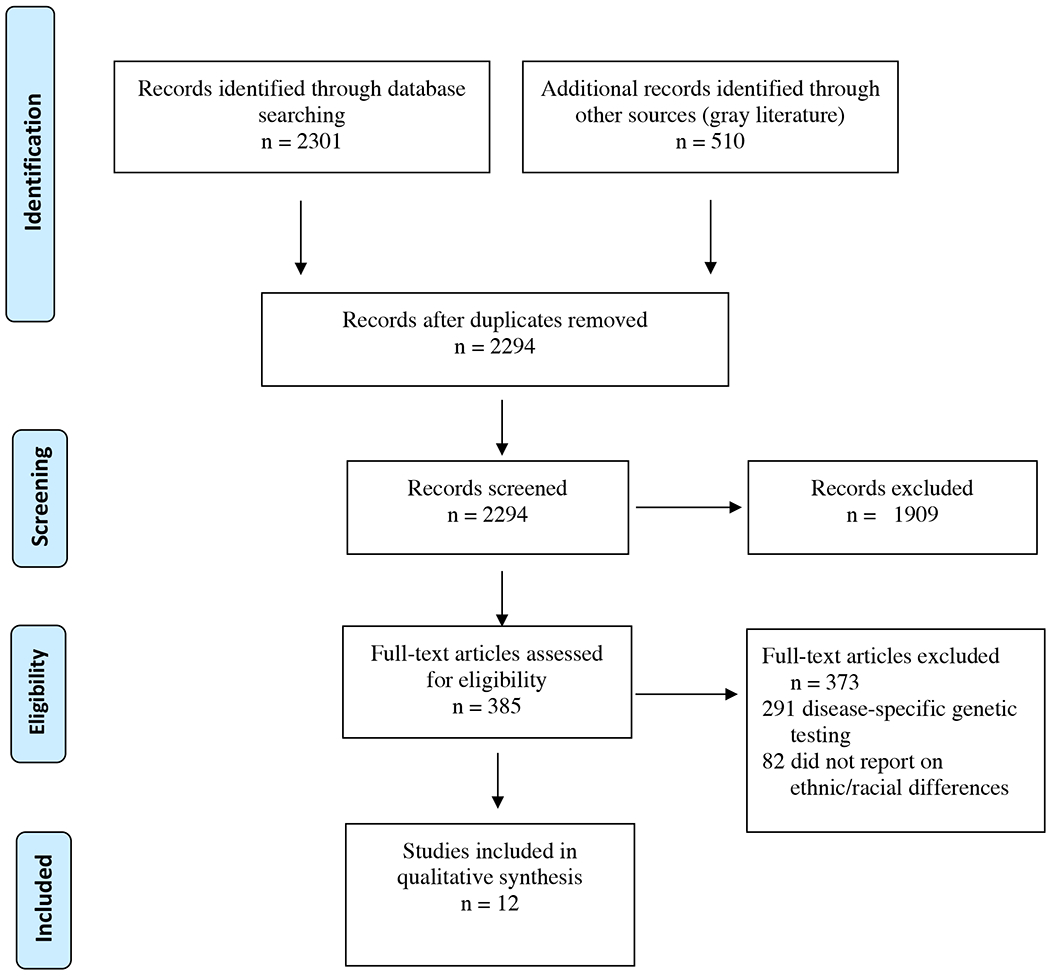
The first author reviewed the titles and abstracts of the articles and gray literature and screened them according to the inclusion and exclusion criteria and eliminated duplicates. Then he reviewed the full text of the articles and gray literature that passed initial screening to identify those that should be excluded based on the exclusion criteria. The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines were followed for reporting the results of the review, including a PRISMA flow diagram of the article selection process (See Figure 1).
Figure 1. PRISMA Flow Diagram.
Data Extraction/Synthesis
Relevant study data were extracted from the final set of articles using a form adapted from the Cochrane systematic review data extraction form and entered into the Research Electronic Data Capture (REDCap) tool developed by Vanderbilt University. REDCap is a secure web based-application designed to support data capture for research studies for building and managing online surveys and databases (Project REDCap, 2017). The first author served as the first reviewer for all articles, then one of the co-authors served as the second reviewer. In all cases, disagreements were resolved with discussion between first and second reviewers.
Key information from the data extraction forms for the final set of studies was summarized in tables. A qualitative synthesis of the studies was developed. A quantitative meta-analysis was not conducted due to the lack of randomized controlled trials in the data extraction, as well as the wide variety of methods and measures used in the included studies (Bearman & Dawson, 2013).
Results
Search engines yielded 2,301 articles in peer-reviewed journals and 272 articles were identified through hand searches of article references. Additionally, representing the gray literature, 238 doctoral dissertations, two meeting reports, and one meeting abstract were identified (Figure 1). After removing duplicates, 2,294 records were screened and 385 reviewed in full text to apply inclusion and exclusion criteria. Among the journal articles, 12 records met all criteria and were selected for the qualitative synthesis. None of the gray literature met the criteria to be included. The data extraction form had 50 items. Across the 12 articles, there was intercoder agreement on 97.7% of the items.
Study Characteristics
All 12 studies were conducted in the U.S. and were published in English (Table 1). Ten articles examined racial and ethnic differences in knowledge about any type of genetic testing (Agurs-Collins et al., 2015; Catz et al., 2005; Diaz, Mainous, Gavin, & Wilson, 2014; Finney Rutten, Gollust, Naveed, & Moser, 2012; Haga, O’Daniel, Tindall, Lipkus, & Agans, 2012; Kolor et al., 2012; Langford, Resnicow, Roberts, & Zikmund-Fisher, 2012; Singer, Antonucci, & Van Hoewyk, 2004; Singer, Couper, Raghunathan, Van Hoewyk, & Antonucci, 2008; Suther & Kiros, 2009), seven examined racial and ethnic differences in attitudes towards genetic testing (Bloss et al., 2010; Catz et al., 2005; Diaz et al., 2014; Singer et al., 2004, 2008; Suther & Kiros, 2009; Zimmerman et al., 2006), and five included both knowledge and attitudes. All but one study (Catz et al., 2005) used a quantitative study design and they all used cross-sectional data. Among the 11 studies using a quantitative design, seven collected primary data (Bloss et al., 2010; Diaz et al., 2014; Haga et al., 2012; Kolor et al., 2012; Singer et al., 2004; Suther & Kiros, 2009; Zimmerman et al., 2006), and four analyzed secondary data sources (Agurs-Collins et al., 2015; Finney Rutten et al., 2012; Langford et al., 2012; Singer et al., 2008). Three of the primary data sources (Haga et al., 2012; Singer et al., 2004; Suther & Kiros, 2009) and all four of the secondary data sources included nationally representative samples (Agurs-Collins et al., 2015; Finney Rutten et al., 2012; Langford et al., 2012; Singer et al., 2008). The other primary data sources were random or convenience samples from one or more specific states. The qualitative study collected focus groups with patients and staff in a local convenience sample. Only three of the 12 studies made reference to a theory or conceptual framework. One study on knowledge used the Social-Cognitive Theory (Agurs-Collins et al., 2015), and two on attitudes applied the Socioecological Model Theory or the Theory of Reasoned Action (Suther & Kiros, 2009; Zimmerman et al., 2006).
Table I.
Characteristics of Reviewed Articles on Racial and Ethnic Differences in Knowledge and Attitudes about Genetic testing
| Knowledge | Attitudes | Primary Quantitative | Secondary Qualitative | Primary Quantitative | Language a | Theory | |
|---|---|---|---|---|---|---|---|
| Agurs-Collins et al. (2015) | X | - | - | X | - | EN | Social Cognitive |
| Bloss et al. (2010) | - | X | X | - | - | EN | - |
| Catz et al. (2005) | X | X | - | - | X | EN, SP, CH | - |
| Diaz et al. (2014) | X | X | X | - | - | EN | - |
| Finney Rutten (2012) | X | - | - | X | - | EN | - |
| Haga et al. (2012) | X | - | X | - | - | EN | - |
| Kolor et al. (2012) | X | - | X | - | - | EN | - |
| Langford et al. (2012) | X | - | - | X | - | EN | - |
| Singer et al. (2004) | X | X | X | - | - | SP | - |
| Singer et al. (2008) | X | X | - | X | - | EN | |
| Suther et al. (2009) | X | X | X | - | - | EN | Socioecological |
| Zimmerman (2006) | - | X | X | - | - | EN | Reasoned Action |
EN=English, SP=Spanish, CH=Chinese
Racial/Ethnic Differences in Knowledge
The ten articles that analyzed racial and ethnic differences in knowledge related to precision medicine or any type of genetic testing are summarized in Table 2, organized by specific topics. Three studies included variables about awareness of genetic testing, measured based on whether or how much respondents had heard of “genetic testing” or “genetic tests.” The two studies using nationally representative survey data found that minorities were less aware of genetic testing compared with Whites. The study analyzing data from the 1990, 1996, and 2004 General Social Survey (GSS) reported that non-Whites were significantly less likely than Whites to have heard “a great deal” about genetic testing versus “nothing” (Beta=−0.632, p < .05) or “not much” versus “nothing” (Beta=−0.763, p < .05) (Singer et al., 2008). In another 2009 national survey, Whites were 74% more likely (OR=1.74, CI=1.22–2.49) to have heard about genetic testing than non-Whites (Haga et al., 2012). On the other hand, a qualitative focus group study in a convenience sample found that White, Black, Latino, and Chinese participants had limited knowledge about genetic testing, with no notable difference in comments across racial/ethnic groups (Catz et al., 2005). Although the smaller qualitative study did not observe differences, the two national studies showed a pattern of lower awareness of genetic testing among Non-Whites.
Table II.
Racial and Ethnic Differences in Knowledge about Genetic Testing
| Source | Article Title | Year/Data a | Study Sample (Public/Patients) | Knowledge Variable(s) | Knowledge Findings (Reference group listed last) b |
|---|---|---|---|---|---|
| Awareness of Genetic Tests | |||||
| Singer et al. 2008 | Trends in U.S. Attitudes toward Genetic Testing, 1990-2004 | 1990, 1996, 2004 GSS, Nationally representative sample | General public 1990: N=917 1996: N=969 2004: N=2,812 U.S. | “How much would you say you have heard or read about genetic testing?” | Great deal vs nothing: NW vs W: Beta= −0.632 (p<.05) Not much vs nothing: NW vs W: Beta=−0.763 (p<.05) |
| Haga et al. 2012 | Survey of U.S. Public Attitudes Towards Pharmacogenetic Testing | 2009 survey, Nationally representative sample | General public N=1,139 U.S. | Have heard about genetic tests (question not provided) | W vs NW: OR=1.74 (CI= 1.22-2.49) |
| Catz et al. 2005 | Attitudes about Genetics in Underserved, Culturally Diverse Populations | 2003 Focus groups, Convenience sample | Patients and healthcare workers N=55 New York | “Medical tests to find out if of having some kinds of diseases are called genetic tests. These tests do not tell you if you have a disease. These tests can tell you your chances (or risks) of getting a disease. What have you heard, seen or read about genetic testing?” | W, B, H, and C all had low awareness of genetic testing (no difference observed) |
| Awareness of Direct-to-Consumer (DTC) Genetic Tests | |||||
| Langford et al. 2012 | Racial and Ethnic Differences in Direct to-Consumer Genetic Tests Awareness in HINTS 2007: Sociodemographic and Numeracy Correlates | 2007 HINTS, Nationally representative sample | General public N=6,754 U.S. | “Genetic tests that analyze your DNA, diet, and lifestyle for potential health risks are currently being marketed by companies directly to consumers. Have you heard or read about these genetic tests?” | B vs W: OR=0.79 (CI=0.65-0.97) H vs W: NSc |
| Finney Rutten 2012 | Increasing Public Awareness of Direct-to-Consumer Genetic Tests: Health Care Access, Internet Use, and Population Density Correlates | 2008, 2011 HINTS, Nationally representative sample representative sample | General public 2008: N=7,674 2011: N=3,959 U.S. | “Genetic tests that analyze your DNA, diet, and lifestyle for potential health risks are currently being marketed by companies directly to consumers. Have you heard or read about these genetic tests?” | B vs W: OR=0.79 (CI=0.62-1.00) H vs W: NS |
| Agurs-Collins et al. 2015 | Public Awareness of Direct-to-Consumer Genetic Tests: Findings from the 2013 U.S. Health Information National Trends Survey | 2013 HINTS, Nationally representative sample | General public N=3,185 U.S. | “Genetic tests that analyze your DNA, diet, and lifestyle for potential health risks are currently being marketed by companies directly to consumers. Have you heard or read about these genetic tests?” | B vs W: NS A vs W: NS AI vs W: NS NH vs W: NS H vs W: NS |
| Kolor et al. 2012 | Public awareness and Use of Direct-to-Consumer Personal Genomic Tests from Four State Population-Based Surveys, and Implications for Clinical and Public Health Practice | 2008 HealthStyles Survey, Nationally representative sample; and 2009 BRFSS in four states, representative samples | General public U.S.: N=5,399 Connecticut: N=6,019 Michigan: N=5,883 Oregon: N=1,931 Utah: N=2,606 | “Several companies [insert names] are advertising genetic tests that examine a person’s entire genetic makeup for health risks. You can order these tests directly, without the involvement of a healthcare provider [by swabbing the inside of your cheek and sending that sample to the company]. Have you heard or read [anything] about these tests?” | B vs W: U.S.: OR=0.7 (CI=0.6-0.9) Connecticut: NS Michigan: OR=0.6 (CI=0.4-0.9) Oregon: NAd Utah: NA H vs W: U.S.: OR=0.8 (CI=0.6-0.9) Connecticut: NS Michigan: NS Oregon: NA Utah: OR=0.5 (CI=0.2-1.0) |
| Awareness of Personalized Medicine | |||||
| Diaz et al. 2014 | Racial Differences in Attitudes toward Personalized Medicine | 2012 survey, Convenience sample | General public and patients N=190 South Carolina |
“Have you heard of personalized medicine?” | B vs W: NS |
| Knowledge about Genetic Tests | |||||
| Singer et al. 2004 | Racial and Ethnic Variations in Knowledge and Attitudes about Genetic Testing | 2000 survey, Nationally representative sample plus B and H samples | General public N=1,763 U.S. |
Index of seven items,e range 0 to 7 items correct: “As far as you know, is each of the following statements about the use of genetic testing true or false, or are you not sure?” |
B vs W: Mean 3.18 vs 3.39 (p<.05) H vs W: Mean 2.70 vs 3.39 (p<.01) |
| Suther et al. 2009 | Barriers to the Use of Genetic Testing: A Study of Racial and Ethnic Disparities | 2000 survey, Nationally representative sample | General public N=1,724 U.S. |
Index of seven items,e range 0 to 6 items correct: “As far as you know, is each of the following statements about the use of genetic testing true, false, or are you not sure?” |
B vs W: OR=0.72 (CI=0.57-0.93) H vs W: OR=0.48 (CI=0.37-0.62) |
HINTS= Health Information National Trends Survey, BRFSS=Behavioral Risk Factor Surveillance System, GSS= General Social Survey
W= White, NW= Non-White, B= Black/African American, H=Hispanic/Latino, C =Chinese, A =Asian, AI= American Indian/Alaska Native, NH= Native Hawaiian/Pacific Islander
NS= No significant
NA= Not available due to small sample sizes
Knowledge index items (correct answer in parentheses):
a. Genetic testing can be used in adults to find out if they have a greater than average chance of developing certain kinds of cancer. (True)
b. Genetic testing can be used in adults to find out if they have a greater than average chance of developing depression. (False)
c. Genetic testing can be used in adults to predict whether a person will have a heart attack. (False)
d. Genetic testing can be used during pregnancy to find out whether the baby will develop sickle cell disease or cystic fibrosis. (True)
e. Gene therapy is currently being used to correct many of the defects found through genetic testing. (False)
f. Sickle cell anemia is a genetic blood disease that affects mainly African-Americans. As far as you know, is there a cure for sickle cell anemia? (No)
g. Cystic fibrosis is a genetic disease that may lead to serious problems with breathing and digestion. As far as you know, is there a cure for cystic fibrosis? (No)
Four articles included measures on awareness of DTC genetic testing. Two studies examined 2007 Health Information National Trends Survey (HINTS) data found Blacks were 21% (OR=0.79, CI=0.65-0.97) less likely to have heard about DTC genetic tests than their White counterparts, while Hispanics/Latinos’ awareness did not significantly differ from Whites (Langford et al., 2012). A subsequent analysis of data from 2008 and 2011 HINTS also found the same result for Blacks (OR=0.79, CI=0.62-1.00) and no significant difference between Hispanics/Latinos and Whites (Finney Rutten et al., 2012). Nationally representative data from the 2008 HealthStyles Survey showed that Blacks were 30% less likely (OR=0.7, CI=0.6-0.9) and Hispanics/Latinos were 20% less likely (OR=0.8, CI=0.6-0.9) to be aware of DTC than Whites. The same study examined Behavioral Risk Factor Surveillance System (BRFSS) data from Connecticut, Michigan, Oregon, and Utah and found lower awareness among Blacks in Michigan (OR=0.6, CI=0.4-0.9) and among Hispanics/Latinos in Utah (OR=0.5, CI=0.2-1.0) compared with Whites, although they had insufficient data to make some of the racial/ethnic comparisons (Kolor et al., 2012). The most recent analysis of national HINTS data from 2013 found that no significant differences in awareness of DTC genetic testing among Blacks, Asians, American Indian/Alaska Natives, Native Hawaiian/Pacific Islanders, and Hispanic/Latinos compared to Whites (Agurs-Collins et al., 2015). Therefore, three out of four national surveys found lower awareness of DTC genetic testing among Blacks versus Whites, while only one out of four found lower awareness among Hispanics/Latinos versus Whites, with the most recent one showing no racial/ethnic differences.
Only one study asked a question about awareness of the term “personalized medicine.” This survey of a convenience sample in South Carolina found no significant difference between Whites and Blacks on this variable (Diaz et al., 2014). Finally, two surveys in nationally representative samples assessed factual knowledge about “genetic testing” by asking a series of true/false or yes/no questions and counting the number of correct answers to create a knowledge index. One study compared the difference in mean knowledge index scores and found a lower average score for Blacks (3.18 vs 3.39, p<.05) and for Hispanics/Latinos. (2.70 vs 3.39, p<.01) versus Whites (Singer et al., 2004). The other study treated the knowledge index as an ordinal variable using variable using an ordinal logistic regression, and identified the same pattern of lower knowledge about genetic testing among Blacks (OR=0.72, CI=0.57-0.93) and Hispanics/Latinos (OR=0.48, CI=0.37-0.62) compared to Whites (Suther & Kiros, 2009). Thus, the two national surveys were consistent in reporting lower knowledge among Blacks and Hispanics/Latinos compared with Whites, but they did not test comparisons between Blacks and Hispanics/Latinos.
Racial/Ethnic Differences in Attitudes
Table 3 summarizes the seven quantitative studies and one qualitative study focused on racial and ethnic differences in attitudes related to precision medicine or any type of genetic testing. Two studies assessed expectations about genetic testing, which were measured by asking if the respondents thought that “genetic testing” would do more good than harm or more harm than good. In analysis of three years of nationally-representative GSS data (1990, 1996, and 2000), non-White respondents were less likely than Whites to think that genetic testing did more good than harm, when compared to the category “don’t know” (Beta=−0.512, p < .05). At the same time, non-Whites were also less likely than Whites to think that genetic testing did more harm than good, when compared to “don’t know” (Beta=−0.238, p < .05) (Singer et al., 2008). The other study used a nationally representative sample combined with random samples of Black and Hispanic adults. The percentage of respondents who expected that genetic testing would do more harm than good was 18.2% for Blacks, 15.3% for Hispanics/Latinos, and 12.4% for Whites. The difference was significant between Latinos and Whites (p<.05) but not significant between Blacks and Whites (Singer et al., 2004). Although the comparison categories were different in the two studies, they both found that perceived harm was more common about Blacks and Hispanics/Latinos than Whites.
Table III.
Racial and Ethnic Differences in Attitudes about Genetic Testing
| Source | Study Title | Year/Dataa | Study Sample (Public/Patients) | Attitude Variable(s) | Attitude Findings (Reference group listed last) |
|---|---|---|---|---|---|
| Expectations about Genetic Testing | |||||
| Singer et al. 2008 | Trends in U.S. Attitudes toward Genetic Testing, 1990-2004 | 1990, 1996, 2004 GSS, Nationally representative samples | General public 1990: N=917 1996: N=969 2004: N=2,812 U.S. | “Some people say that genetic testing is a wonderful advance. Others think it may cause trouble. Based on what you know, do you think genetic testing will do more good than harm, or more harm than good?” | Good vs Don’ know NW vs W: Beta= − 0.512 (p<.05) Harm vs Don’t know NW vs W: Beta= − 0.238 (p<.05) |
| Singer et al. 2004 | Racial and Ethnic Variations in Knowledge and Attitudes about Genetic Testing | 2000 survey, Nationally representative sample plus B and H samples | General public N=1,763 U.S. | “Some people say genetic testing is a wonderful medical advance. Others think it may cause trouble. What about you—do you think genetic testing will do more good than harm, or more harm than good?” | More harm than good: B vs W: 18.2% vs 12.4% (NS)b L vs W: 15.3% vs 12.4% (p<.05) |
| Concerns about Genetic Testing | |||||
| Singer eat al. 2004 | Racial and Ethnic Variations in Knowledge and Attitudes about Genetic Testing | 2000 survey, Nationally representative sample plus B and H samples | General public N=1,763 U.S. |
Index of eight itemsc range 0 to 16: “For each of the following statements, please tell me if you strongly agree, somewhat agree, somewhat disagree, or strongly disagree.” |
B vs W: 6.34 vs 4.96 (p<.01) L vs W: 5.89 vs 4.96 (p<.01) |
| Suther et al. 2009 | Barriers to the Use of Genetic Testing: A Study of Racial and Ethnic Disparities | 2000 survey, Nationally representative sample | General public N=1,724 U.S. | Index of eight items,c range 1 to 3: “For each of the following statements, please tell me if you strongly agree, somewhat agree, somewhat disagree, or strongly disagree.” |
B vs W: OR=1.66 (CI=1.28-2.15) L vs W: OR=1.58 (CI=1.21-.2.07) |
| Zimmerman 2006 | Racial Differences in Beliefs about Genetic Screening among Patients at Inner-City Neighborhood Health Centers | 2004 survey, Random and convenience samples | Patients N=314 Pennsylvania | Indicate level of agreement: a. “Genetic testing will lead to racial discrimination” b. “Genetic testing will lead to discrimination against handicapped” |
a. B vs W: OR=3.02 (CI=1.51-6.05) b. B vs W: 64% vs 47% (p<.01) |
| Bloss et al. 2010 | Consumer Perceptions of Direct-to-Consumer Personalized Genomic Risk Assessments | 2008 survey, Convenience sample | General public and patients N=3,640 California |
“Do Doyou have concerns about participating in this initiative? Concerns related to… ” a. “learning about my disease risk from my DNA testing” b. “not knowing how I will feel about my results” c. “the quality and reliability of the testing lab and the results” d. “potential privacy issues about my data” |
a. NW vs W: 15.6% vs 12.5% (p<.05) b. NW vs W: 16.9% vs 16.0% (NS) c. NW vs W: 21.1% vs 15.4% (p<.001) d. NW vs W: 35.7% vs 36.1% (NS) |
| Diaz et al. 2014 | Racial Differences in Attitudes toward Personalized Medicine | 2012 survey, Convenience sample | General public and patients N=190 South Carolina | How worried about the following: a. Using genes without consent b. Genetic information being shared without consent c. Discrimination based on genes d. Not being able to receive personalized medicine due to costs e. People being kept alive longer than they should be (questions not provided) |
a. B vs W: 57.3% vs 20.6% (p<.001) b. B vs W: 65.0% vs 35.6% (p<.001) c. B vs W: 62.4% vs 34.3% (p<.001) d. B vs W: 75.0% vs 48.0% (p<.001) e. B vs W: 27.6% vs 20.8% (NS) |
| Other Attitudes about Genetic Testing | |||||
| Zimmerman 2006 | Racial Differences in Beliefs about Genetic Screening among Patients at Inner-City Neighborhood Health Centers | 2004 survey, Random and convenience samples | Patients N=314 Pennsylvania | Indicate level of agreement: a. “Genetic testing to check risk of getting a disease is a good idea” b. “Employers should be able to see the results of genetic testing before hiring workers” |
a. B vs W: NS b. B vs W: NS |
| Bloss et al. 2010 | Consumer Perceptions of Direct-to-Consumer Personalized Genomic Risk Assessments |
2008 survey, Convenience sample | General public and patients N=3,640 California |
“Would you want to know your genetic risk for a disease you couldnť do anything to prevent?” | W vs NW: OR=1.43 (CI=1.13-1.81) |
| Catz et al. 2005 | Attitudes about Genetics in Underserved, Culturally Diverse Populations | 2003 Focus groups, Convenience sample | Patients and healthcare workers N=55 New York | Feelings about genetic testing (question not provided) |
H and C had most positive feelings about genetic testing B had most negative feelings towards genetic testing |
GSS= General Social Survey
NS= No significant
Concern index items:
1. Genetic testing during pregnancy is a good thing because it allows people to choose to have the children they really want.
2. Genetic testing will lead to discrimination against people [who are not perfect].
3. Anonymous genetic testing, where no record is kept of the person’s name, should be available to people who want it.
4. Genetic testing will mostly benefit people who already have a lot of advantages. (If the respondent does not understand “advantages,” just say, “people who already have a lot”.)
5. Information from genetic tests is likely to be misused.
6. Genetic testing is the first step to getting rid of people the government considers undesirable.
7. Scientists are creating unrealistic hopes how soon cures will be found for genetic diseases.
8. Research on genes is taking away money that should be used for other health problems.
Five studies reported on racial and ethnic differences in concerns about various aspects of genetic testing or personalized medicine. Two studies in 2000 that used the same eight-item genetic testing concern index with similar findings in separate nationally-representative samples in 2000. One of them tested the difference in mean concern index scores and found a higher average score for Blacks versus Whites (6.34 vs 4.96, p<.01) and for Hispanics/Latinos versus Whites (5.89 vs 4.96, p<.01) (Singer et al., 2004). The other study, which treated the concern index as an ordinal variable and used ordinal logistic regression, found the same pattern with greater concerns about genetic testing among Blacks (OR=1.66, CI=1.28-2.15) and Latinos (OR=1.58, CI=1.21.2.07) compared with Whites (Suther & Kiros, 2009). Three studies surveying local convenience samples examined differences in specific concerns. One using a sample from inner-city neighborhood health centers in Pennsylvania in 2004 found that Blacks were three times more likely than Whites (OR=3.02, CI=1.51-6.05) to believe that genetic testing would lead to racial discrimination, and also more likely to believe it would lead to discrimination against handicapped persons (Zimmerman et al., 2006). Another surveying participants who agreed to take a DTC genetic test in California in 2008 found no significant difference in the overall concern about genetic testing between Non-Whites and Whites (Bloss et al., 2010). Blacks were more worried than Whites about genetic information being used without their consent (57.3% vs 20.6%), about genetic information being shared without consent (65.0% vs 35.6%), about discrimination based on genetic information (62.4% vs 34.3%), and about not being able to afford the cost of receiving precision medicine (75.0% vs 48.0%). The concern about people being kept alive longer than they should be was not significantly different for both racial groups (Diaz et al., 2014). Overall, across studies, concerns about genetic testing were more common among non-Whites, Blacks, and Hispanics/Latinos compared to Whites.
Three studies examined a variety of other types of variables related to attitudes about genetic testing. The study mentioned above that surveyed patients in Pennsylvanian inner-city neighborhood health centers detected no significant difference between Blacks and Whites when asked if it was a good idea to get genetic testing to learn about disease risk, or if employers should have access to genetic testing of prospective employees (Zimmerman et al., 2006). The California survey of DTC genetic testing participants reported that Whites were 43% percent more likely (OR=1.43, CI=1.13-1.81) to desire to know their genetic risk for nonpreventable disease compared with non-Whites (Bloss et al., 2010). A qualitative study among diverse patients and healthcare workers in New York identified a pattern of Hispanics/Latinos and Chinese participants having the most positive feelings about genetic testing and Blacks having the most negative feelings about genetic testing (Catz et al., 2005).
Discussion
This systematic review summarized 12 relevant studies identified across nearly 20 years of research in the U.S. that examined racial and ethnic differences in knowledge and attitudes about genetic testing within the broad context of precision medicine. While some studies have examined a variety of disease-specific genetic tests, a paucity of research has focused on racial and ethnic differences in knowledge and attitudes towards general, non-disease-specific genetic testing in precision medicine. Although we used a broad range of search terms related to precision medicine, almost all of the eligible studies focused narrowly on “genetic testing” or the use of genetic tests to predict disease risk, with none referencing pharmacogenomic applications of genetic tests to guide medication prescribing decisions.
Several patterns were identified for knowledge about genetic testing in precision medicine across these 12 studies. First, awareness of “genetic testing” in general was consistently lower among non-Whites compared to Whites (Haga et al., 2012; Singer et al., 2008). This finding was similar to several existing studies that found that Black and Hispanic women had lower awareness of genetic testing for cancer risk (Kuhl et al., 2005; Peters, Rose, & Armstrong, 2004; Ricker et al., 2006; Thompson, Valdimarsdottir, Jandorf, & Redd, 2003). A previous systematic review also found that African American women had lower knowledge about breast cancer genetic testing compared with White women (Chanita Hughes Halbert et al., 2005). However, awareness does not necessarily mean people understand what genetic tests are or how they are used. In a knowledge assessment about genetic testing, on average, people answered less than half the questions correctly, and the number of correct answers was lower for Blacks and Hispanics/Latinos compared to Whites (Singer et al., 2004). These findings were consistent with a disease-specific review that found that racial and ethnic minority groups had lower knowledge and awareness about of genetic testing for cancer susceptibility compared with Whites (Hann et al., 2017).
Second, findings were mixed regarding racial and ethnic differences in awareness of DTC testing. Among four national studies, three out of four found lower awareness of DTC genetic tests among Blacks (Finney Rutten et al., 2012; Kolor et al., 2012; Langford et al., 2012), and only one out of four found lower awareness among Hispanics/Latinos compared with Whites. Only one of these national studies considered other ethnic groups but found no differences in awareness of DTC tests. Examination of four state-level representative surveys also showed inconsistent results of differences in awareness of DTC tests among Blacks and Hispanics/Latinos compared to Whites. Third, only one study measured awareness of “personalized medicine” and found no significant difference between Blacks and Whites. However, these results were based on a state-level convenience sample, and more evidence is needed. Finally, two studies using nationally representative surveys samples measured factual knowledge about genetic testing and consistently found that Blacks and Hispanics/Latinos had lower knowledge than Whites (Singer et al., 2004; Suther & Kiros, 2009).
Some patterns were also identified regarding attitudes toward genetic testing in general. First, two studies using nationally-representative samples reported inconsistent results about differences in expectations about whether “genetic testing” will do more harm than good (Singer et al., 2004, 2008). Secondly, five studies showed that Blacks, Hispanics/Latinos, and non-Whites generally had more concerns about genetic testing than Whites, both in nationally representative and convenience samples (Bloss et al., 2010; Diaz et al., 2014; Singer et al., 2004; Suther & Kiros, 2009; Zimmerman et al., 2006). Third, two studies using convenience samples in different states compared interest in return of information from genetic tests that predict disease, but only one showed a racial difference, with lower interest among non-Whites (Bloss et al., 2010; Zimmerman et al., 2006). Finally, one small qualitative study reported that Hispanics/Latinos and Chinese had the most positive feelings and Blacks had the most negative feelings about genetic testing in general (Catz et al., 2005). These findings on general attitudes are in contrast to a previous systematic review, which found that African American women had positive attitudes towards genetic testing specifically for breast cancer (Chanita Hughes Halbert et al., 2005).
The lower levels of knowledge about genetic testing among Blacks and Hispanics/Latinos may be related to the greater number of concerns regarding genetic testing among these two groups compared to Whites (Singer et al., 2004; Suther & Kiros, 2009). Blacks were more worried than Whites about genetic tests leading to racial and disability discrimination, using or sharing genetic information without consent, and lack of access to genetic tests due to cost (Diaz et al., 2014; Zimmerman et al., 2006). A similar concern about confidentiality of results was found among Blacks when asked specifically about genetic testing for psychiatric disorders (Murphy & Thompson, 2009). Research on attitudes about genetic testing for cancer, including breast and ovarian cancer, have also found that minorities had more concerns than Whites about social and insurance discrimination (Peters et al., 2004; Thompson et al., 2003). To prevent discrimination and potential abuse of genetic data, the U.S. Congress enacted the Genetic Information Nondiscrimination Act (GINA) of 2008 (Feldman, 2012). However, there is low awareness of these protections among the general public (Prince & Roche, 2014).
The higher level of concerns about genetic testing among Blacks may be related to larger problems of distrust of medicine and biomedical research in this population due to past abuses, such as “The United States Public Health Service Study of Untreated Syphilis in the Negro,” more commonly known as the Tuskegee Study (Laws, 2018). However, interestingly, no significant racial variations were found in concern about potential privacy issues about their genetic information (Bloss et al., 2010).
Technological advances in genetic and genomic sequencing have offered physicians more opportunities to employ precision medicine by making preemptive medical-care decisions based on patients’ individual genetic makeup (Bielinski et al., 2014). The leading force for changing the traditional one-size-fits-all paradigm in medicine is the innovative use of genetic tests for personalized diagnoses and targeted disease treatments. Overall, around 80% of adults in the U.S. say they have heard of genetics tests (Haga et al., 2012). Awareness and perceived benefits of genetic testing have improved over time as more and more genetic tests have become available to patients and legislative changes such as GINA have emerged (Singer et al., 2008). A growing number of Americans have also heard of DTC genetics tests, increasing from 29% in 2008 to 36% in 2013 (Agurs-Collins et al., 2015; Finney Rutten et al., 2012).
However, consistent with Diffusion of Innovation Theory (Rogers, 2003), this systematic review suggested that awareness and understanding of genetic testing has been disseminated unevenly. Uneven dissemination means that socially advantaged groups will benefit more quickly from precision medicine than disadvantaged groups, especially given the context of unequal access to healthcare in the U.S. (Levine et al., 2007, 2008, 2010). While the reason for this dissemination trend is not completely understood, many physicians have low knowledge about genetic testing, and racial and ethnic minority patients are less likely to receive a physician offer or referral for genetic testing (Forman & Hall, 2009; Hamilton et al., 2017; Kolb, Wallace, Hill, & Royce, 2006).
Whites are also disproportionately represented as study participants in genetic research compared to Non-Whites (Oh, White, Gignoux, & Burchard, 2016). In a qualitative study, African Americans perceived individual, family, and community benefits of participating in genetic research for cancer; however, they also reported reasons for being hesitant to participate, including distrust of researchers and concerns about exploitation and mishandling of genetic information (McDonald et al., 2014). In a national survey of African Americans, distrust in research was the only significant barrier or facilitator to participating in a hypothetical genetic study for cancer after controlling for education, employment, and healthcare access (Chanita Hughes Halbert, McDonald, Vadaparampil, Rice, & Jefferson, 2016; McDonald et al., 2012)(Halbert, McDonald, Vadaparampil, Rice, & Jefferson, 2016; McDonald et al., 2014, 2012). While the studies in this review did not focus on research participation, one study found that Blacks had more concerns about genes being used without consent and genetic information being shared without consent. Lower participation of racial and ethnic minority groups in genetic studies will delay group-specific precision medicine developments. Lower participation combined with barriers to minority patients being offered and accepting genetic testing as part of their healthcare could potentially widen health disparities affecting racial and ethnic minority populations in the U.S. (C.H. Halbert & Harrison, 2018).
Study Limitations
A limitation of this systematic review was not comparing differences in knowledge and attitudes based on other socioeconomic factors that contribute to disparities, such as income or educational attainment. However, very few studies have tested differences based on those variables. Future systematic reviews should examine whether other demographics are associated with knowledge and attitudes toward genetic testing in general. Another limitation was that only one author applied the selection criteria to the abstracts and full-text articles. Strengths of this systematic review included the comprehensive search strategy including a range of terms related to genetic testing and precision medicine, and use of a data extraction form adapted from Cochrane. Furthermore, the data extraction form was implemented using the web-based REDCap tool, which provided online access to reviewers of the extracted data and facilitate resolution of any discrepancies in an efficient way.
Practice Implications
Some research not included in this review has examined racial and ethnic differences in knowledge and attitudes toward genetic tests for the diagnosis or treatment of specific diseases, such as breast cancer, colorectal cancer, ovarian cancer, cardiovascular disease, sickle cell disease, etc. (Durfy, Bowen, McTiernan, Sporleder, & Burke, 1999; Long, Thomas, Grubs, Gettig, & Krishnamurti, 2011). However, comprehensive panels that offer multiple genetics tests at the same time, both from DTC companies and in healthcare settings are becoming more common (Lynch et al., 2015). For example, pre-emptive pharmacogenomic tests are recommended to be performed in asymptomatic persons and are increasingly being included as routine medical tests and incorporated into electronic health records for future clinical decisions (Bielinski et al., 2014). Thus, general perspectives of patients towards genetic testing are important to understand because they will influence patients’ willingness to accept both disease-specific tests and multigene panels, which patients will be more likely to be offered in the future.
The findings of this systematic review contribute to the literature a synthesis of information about racial and ethnic differences in knowledge and attitudes toward various types of genetic testing. The findings of lower levels of knowledge among racial and ethnic minorities suggest the need for targeted educational efforts directed toward minority patients in clinical settings and in the general public. Some educational efforts could focus on disseminating information among racial and ethnic minorities about the protections under GINA against genetic discrimination, as well as educating physicians on how to be compliant with this act (Feldman, 2012). Physicians and genetic counselors should be trained in cultural competency to provide education and recommendations regarding genetic testing and precision medicine to racially- and ethnically-diverse patients in a sensitive and effective way that addresses both group differences and individual needs and preferences. Previous studies that have developed and tested culturally-targeted genetic counseling for African American women have shown promising results (C. H Halbert, Kessler, Stopfer, Domchek, & Wileyto, 2006; C. H. Halbert, Kessler, Troxel, Stopfer, & Domchek, 2010; Pal et al., 2005).
Lower awareness and understanding and greater concerns about genetic testing among racial and ethnic minority groups could also affect their willingness to participate in the national All of Us study or other research studies involving genetic testing. Such studies may consider including targeted outreach efforts to improve knowledge and attitudes about genetic testing as part of recruitment efforts.
Research Recommendations
This systematic review highlighted several gaps in the current literature on racial and ethnic differences in knowledge and attitudes about genetic testing in general. First, the studies did not have a large enough sample to be able to make subgroup comparisons for many racial and ethnic groups. Only nine studies made direct comparisons with Blacks, five made comparisons with Hispanics/Latinos, two with Chinese, and one each with Native American and Native Hawaiian. No other specific racial and ethnic groups were analyzed. Second, the studies reviewed did not take into consideration diversity within each group, such as Hispanics/Latinos from different countries or Blacks of different socioeconomic levels. Third, attitudes about genetic testing are measured inconsistently, with a variety of potential concerns included in different surveys, which makes it difficult to compare findings across studies. None of the studies asked specifically about knowledge or attitudes about pharmacogenomics testing.
Data synthesized in this systematic review suggest the need for more research to examine systematically the trends and disparities in knowledge and attitudes towards genetic testing among different population subgroups to determine whether these disparities are narrowing or widening over time. Future research could focus on factors that contribute to the unequal distribution of knowledge about various types of genetic testing in racial and ethnic minority populations. The findings also point to the need for further research on the development and implementation of culturally-appropriate interventions to improve knowledge and attitudes about precision medicine among racial and ethnic minorities (Chanita Hughes Halbert et al., 2012; Hann et al., 2017). Furthermore, clinical studies testing precision medicine approaches should include minority populations and collect cultural and socioeconomic data from patients, along with genetic, genomic, and epigenetic information in their clinical assessments (Avilés-Santa et al., 2017).
Conclusion
While the unequal distribution and adoption of innovations in healthcare persists, health disparities will continue to negatively impact positive health outcomes for minority populations in the U.S. Many racial and ethnic minorities express concern and distrust toward genetic testing. In order for precision medicine to contribute to reducing health disparities rather than widening them, all patients would need equal access to these innovations and culturally-appropriate educational material would be needed for the education of patients and the general public from diverse backgrounds with accurate information.
Acknowledgments:
This research was supported by the Vanderbilt Institute for Clinical and Translational Research (VICTR), grant number UL1-TR000445 and Meharry Clinical and Translational Research Center (MeTRC), grant number U54MD007593. The authors would like to thank Rachel Lane Walden of the Vanderbilt University, Annette and Irwin Eskind Biomedical Library for her assistance with the literature search strategy.
Dr. Melanie Myers served as Action Editor on the manuscript review process and publication decision.
Footnotes
Conflict of Interest:
Juan R. Canedo, Stephania T. Miller, Hector Myers, Maureen Sanderson declare that they have no conflict of interest.
Human Studies and Informed Consent:
No human studies were carried out by the authors for this article.
Animal Studies:
No animal studies were carried out by the authors of this article.
References
- Agurs-Collins T, Ferrer R, Ottenbacher A, Waters EA, O’Connell ME, & Hamilton JG (2015). Public Awareness of Direct-to-Consumer Genetic Tests: Findings from the 2013 U.S. Health Information National Trends Survey. Journal of Cancer Education: The Official Journal of the American Association for Cancer Education, 30(4), 799–807. 10.1007/s13187-014-0784-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong K, Micco E, Carney A, Stopfer J, & Putt M (2005). Racial differences in the use of BRCA1/2 testing among women with a family history of breast or ovarian cancer. JAMA, 293(14), 1729–1736. 10.1001/jama.293.14.1729 [DOI] [PubMed] [Google Scholar]
- Aronson SJ, & Rehm HL (2015). Building the foundation for genomics in precision medicine. Nature, 526(7573), 336–342. 10.1038/nature15816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avard D, & Knoppers BM (2009). Genomic medicine: considerations for health professionals and the public. Genome Medicine, 1(2), 25. 10.1186/gm25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avilés-Santa ML, Heintzman J, Lindberg NM, Guerrero-Preston R, Ramos K, Abraído-Lanza AL,… Vázquez MA (2017). Personalized medicine and Hispanic health: improving health outcomes and reducing health disparities — a National Heart, Lung, and Blood Institute workshop report. BMC Proceedings, 11(11), 11. 10.1186/s12919-017-0079-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bearman M, & Dawson P (2013). Qualitative synthesis and systematic review in health professions education. Medical Education, 47(3), 252–260. 10.1111/medu.12092 [DOI] [PubMed] [Google Scholar]
- Bielinski SJ, Olson JE, Pathak J, Weinshilboum RM, Wang L, Lyke KJ,… Kullo IJ (2014). Preemptive genotyping for personalized medicine: design of the right drug, right dose, right time-using genomic data to individualize treatment protocol. Mayo Clinic Proceedings, 89(1), 25–33. 10.1016/j.mayocp.2013.10.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloss CS, Ornowski L, Silver E, Cargill M, Vanier V, Schork NJ, & Topol EJ (2010). Consumer perceptions of direct-to-consumer personalized genomic risk assessments. Genetics in Medicine: Official Journal of the American College of Medical Genetics, 12(9), 556–566. 10.1097/GIM.0b013e3181eb51c6 [DOI] [PubMed] [Google Scholar]
- Butrick M, Kelly S, Peshkin BN, Luta G, Nusbaum R, Hooker GW,… Schwartz MD (2015). Disparities in uptake of BRCA1/2 genetic testing in a randomized trial of telephone counseling. Genetics in Medicine: Official Journal of the American College of Medical Genetics, 17(6), 467–475. 10.1038/gim.2014.125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canedo JR, Miller ST, Myers HF, & Sanderson M (2017). Racial and ethnic differences in knowledge and attitudes about precision medicine in the US: Systematic Review. PROSPERO. Retrieved from http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42017064798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caselli RJ, Langbaum J, Marchant GE, Lindor RA, Hunt KS, Henslin BR,… Robert JS (2014). Public perceptions of presymptomatic testing for Alzheimer disease. Mayo Clinic Proceedings, 89(10), 1389–1396. 10.1016/j.mayocp.2014.05.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catz DS, Green NS, Tobin JN, Lloyd-Puryear MA, Kyler P, Umemoto A,… Wolman F (2005). Attitudes about genetics in underserved, culturally diverse populations. Community Genetics, 8(3), 161–172. 10.1159/000086759 [DOI] [PubMed] [Google Scholar]
- Collins J, Ryan L, & Truby H (2014). A systematic review of the factors associated with interest in predictive genetic testing for obesity, type II diabetes and heart disease. Journal of Human Nutrition and Dietetics: The Official Journal of the British Dietetic Association, 27(5), 479–488. 10.1111/jhn.12179 [DOI] [PubMed] [Google Scholar]
- Diaz VA, Mainous AG, Gavin JK, & Wilson D (2014). Racial differences in attitudes toward personalized medicine. Public Health Genomics, 17(1), 1–6. 10.1159/000354785 [DOI] [PubMed] [Google Scholar]
- Durfy SJ, Bowen DJ, McTiernan A, Sporleder J, & Burke W (1999). Attitudes and interest in genetic testing for breast and ovarian cancer susceptibility in diverse groups of women in western Washington. Cancer Epidemiology, Biomarkers & Prevention: A Publication of the American Association for Cancer Research, Cosponsored by the American Society of Preventive Oncology, 8(4 Pt 2), 369–375. [PubMed] [Google Scholar]
- Feldman EA (2012). The Genetic Information Nondiscrimination Act (GINA): public policy and medical practice in the age of personalized medicine. Journal of General Internal Medicine, 27(6), 743–746. 10.1007/s11606-012-1988-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fine MJ, Ibrahim SA, & Thomas SB (2005). The role of race and genetics in health disparities research. American Journal of Public Health, 95(12), 2125–2128. 10.2105/AJPH.2005.076588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finney Rutten LJ, Gollust SE, Naveed S, & Moser RP (2012). Increasing Public Awareness of Direct-to-Consumer Genetic Tests: Health Care Access, Internet Use, and Population Density Correlates. Journal of Cancer Epidemiology, 2012, 309109. 10.1155/2012/309109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forman AD, & Hall MJ (2009). Influence of race/ethnicity on genetic counseling and testing for hereditary breast and ovarian cancer. The Breast Journal, 15 Suppl 1, S56–62. 10.1111/j.1524-4741.2009.00798.x [DOI] [PubMed] [Google Scholar]
- Galea S, Tracy M, Hoggatt KJ, Dimaggio C, & Karpati A (2011). Estimated deaths attributable to social factors in the United States. American Journal of Public Health, 101(8), 1456–1465. 10.2105/AJPH.2010.300086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genentech. (2017). Genentech: Herceptin® (trastuzumab) Development Timeline. Retrieved May 5, 2017, from https://www.gene.com/media/product-information/herceptin-development-timeline [Google Scholar]
- Haga SB, O’Daniel JM, Tindall GM, Lipkus IR, & Agans R (2012). Survey of US public attitudes toward pharmacogenetic testing. The Pharmacogenomics Journal, 12(3), 197–204. 10.1038/tpj.2011.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halbert CH, Kessler L, Stopfer JE, Domchek S, & Wileyto EP (2006). Low rates of acceptance of BRCA1 and BRCA2 test results among African American women at increased risk for hereditary breast-ovarian cancer. Genetics in Medicine: Official Journal of the American College of Medical Genetics, 8(9), 576–582. https://doi.org/10.109701.gim.0000237719.37908.54 [DOI] [PubMed] [Google Scholar]
- Halbert CH, Kessler L, Troxel AB, Stopfer JE, & Domchek S (2010). Effect of genetic counseling and testing for BRCA1 and BRCA2 mutations in African American women: a randomized trial. Public Health Genomics, 13(7–8), 440–448. 10.1159/000293990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halbert CH, & Harrison BW (2018). Genetic counseling among minority populations in the era of precision medicine. American Journal of Medical Genetics. Part C, Seminars in Medical Genetics, 178(1), 68–74. 10.1002/ajmg.c.31604 [DOI] [PubMed] [Google Scholar]
- Halbert Chanita Hughes, Kessler L, Collier A, Weathers B, Stopfer J, Domchek S, & McDonald JA (2012). Low rates of African American participation in genetic counseling and testing for BRCA1/2 mutations: racial disparities or just a difference? Journal of Genetic Counseling, 21(5), 676–683. 10.1007/s10897-012-9485-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halbert Chanita Hughes, Kessler LJ, & Mitchell E (2005). Genetic testing for inherited breast cancer risk in African Americans. Cancer Investigation, 23(4), 285–295. [DOI] [PubMed] [Google Scholar]
- Halbert Chanita Hughes, McDonald J, Vadaparampil S, Rice L, & Jefferson M (2016). Conducting Precision Medicine Research with African Americans. PloS One, 11(7), e0154850. 10.1371/journal.pone.0154850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall MJ, Manne SL, Myers RE, Keenan EM, Balshem AM, & Weinberg DS (2012). Predictors of patient uptake of colorectal cancer gene environment risk assessment. Genome Medicine, 4(11), 92. 10.1186/gm393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton JG, Abdiwahab E, Edwards HM, Fang M-L, Jdayani A, & Breslau ES (2017). Primary care providers’ cancer genetic testing-related knowledge, attitudes, and communication behaviors: A systematic review and research agenda. Journal of General Internal Medicine, 32(3), 315–324. 10.1007/s11606-016-3943-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammer MJ (2016). Precision Medicine and the Changing Landscape of Research Ethics. Oncology Nursing Forum, 43(2), 149–150. 10.1188/16.ONF.149-150 [DOI] [PubMed] [Google Scholar]
- Hann KEJ, Freeman M, Fraser L, Waller J, Sanderson SC, Rahman B,… PROMISE study team. (2017). Awareness, knowledge, perceptions, and attitudes towards genetic testing for cancer risk among ethnic minority groups: a systematic review. BMC Public Health, 17(1), 503. 10.1186/s12889-017-4375-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. (2003). Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. (Smedley BD, Stith AY, & Nelson AR, Eds.). Washington (DC): National Academies Press (US). Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK220358/ [PubMed] [Google Scholar]
- Kolb B, Wallace AM, Hill D, & Royce M (2006). Disparities in cancer care among racial and ethnic minorities. Oncology (Williston Park, N.Y.), 20(10), 1256–1261; discussion 1261, 1265, 1268–1270. [PubMed] [Google Scholar]
- Kolor K, Duquette D, Zlot A, Foland J, Anderson B, Giles R,… Khoury MJ (2012). Public awareness and use of direct-to-consumer personal genomic tests from four state population-based surveys, and implications for clinical and public health practice. Genetics in Medicine: Official Journal of the American College of Medical Genetics, 14(10), 860–867. 10.1038/gim.2012.67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhl CK, Schrading S, Leutner CC, Morakkabati-Spitz N, Wardelmann E, Fimmers R,… Schild HH (2005). Mammography, breast ultrasound, and magnetic resonance imaging for surveillance of women at high familial risk for breast cancer. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology, 23(33), 8469–8476. 10.1200/JCO.2004.00.4960 [DOI] [PubMed] [Google Scholar]
- Langford AT, Resnicow K, Roberts JS, & Zikmund-Fisher BJ (2012). Racial and ethnic differences in direct-to-consumer genetic tests awareness in HINTS 2007: sociodemographic and numeracy correlates. Journal of Genetic Counseling, 21(3), 440–447. 10.1007/s10897-011-9478-2 [DOI] [PubMed] [Google Scholar]
- Lawrence RE, & Appelbaum PS (2011). Genetic testing in psychiatry: a review of attitudes and beliefs. Psychiatry, 74(4), 315–331. 10.1521/psyc.2011.74.4315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laws T (2018). Tuskegee as Sacred Rhetoric: Focal Point for the Emergent Field of African American Religion and Health. Journal of Religion and Health, 57(1), 408–419. 10.1007/s10943-017-0505-y [DOI] [PubMed] [Google Scholar]
- Levine RS, Briggs NC, Kilbourne BS, King WD, Fry-Johnson Y, Baltrus PT,… Rust GS (2007). Black-White mortality from HIV in the United States before and after introduction of highly active antiretroviral therapy in 1996. American Journal of Public Health, 97(10), 1884–1892. 10.2105/AJPH.2005.081489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine RS, Kilbourne BE, Baltrus PA, Williams-Brown S, Caplan L, Briggs NC,… Rust GE (2008). Black-white disparities in elderly breast cancer mortality before and after implementation of Medicare benefits for screening mammography. Journal of Health Care for the Poor and Underserved, 19(1), 103–134. 10.1353/hpu.2008.0019 [DOI] [PubMed] [Google Scholar]
- Levine RS, Rust GS, Pisu M, Agboto V, Baltrus PA, Briggs NC,… Hennekens CH (2010). Increased Black-White disparities in mortality after the introduction of lifesaving innovations: a possible consequence of US federal laws. American Journal of Public Health, 100(11), 2176–2184. 10.2105/AJPH.2009.170795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long KA, Thomas SB, Grubs RE, Gettig EA, & Krishnamurti L (2011). Attitude and beliefs of African-Americans toward genetics, genetic testing, and sickle cell disease education and awareness. Journal of Genetic Counseling, 20(6), 572–592. 10.1007/s10897-011-9388-3 [DOI] [PubMed] [Google Scholar]
- Lynch JA, Venne V, & Berse B (2015). Genetic tests to identify risk for breast cancer. Seminars in Oncology Nursing, 31(2), 100–107. 10.1016/j.soncn.2015.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahood Q, Van Eerd D, & Irvin E (2014). Searching for grey literature for systematic reviews: challenges and benefits. Research Synthesis Methods, 5(3), 221–234. 10.1002/jrsm.1106 [DOI] [PubMed] [Google Scholar]
- Marson FAL, Bertuzzo CS, & Ribeiro JD (2017). Personalized or Precision Medicine? The Example of Cystic Fibrosis. Frontiers in Pharmacology, 8. 10.3389/fphar.2017.00390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald JA, Vadaparampil S, Bowen D, Magwood G, Obeid JS, Jefferson M,… Hughes Halbert C (2014). Intentions to donate to a biobank in a national sample of African Americans. Public Health Genomics, 17(3), 173–182. 10.1159/000360472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald JA, Weathers B, Barg FK, Troxel AB, Shea JA, Bowen D,… Halbert CH (2012). Donation Intentions for Cancer Genetics Research Among African Americans. Genetic Testing and Molecular Biomarkers, 16(4), 252–258. 10.1089/gtmb.2011.0119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moonesinghe R, Jones W, Honoré PA, Truman BI, & Graham G (2009). Genomic medicine and racial/ethnic health disparities: promises, perils, and the challenges for health care and public health policy. Ethnicity & Disease, 19(4), 473–478. [PubMed] [Google Scholar]
- Moy E, & Freeman W (2014). Federal investments to eliminate racial/ethnic health-care disparities. Public Health Reports (Washington, D.C.: 1974), 129 Suppl 2, 62–70. 10.1177/00333549141291S212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller C, Lee SM, Barge W, Siddique SM, Berera S, Wideroff G,… Kupfer SS (2018). Low Referral Rate for Genetic Testing in Racially and Ethnically Diverse Patients Despite Universal Colorectal Cancer Screening. Clinical Gastroenterology and Hepatology: The Official Clinical Practice Journal of the American Gastroenterological Association, 16(12), 1911–1918.e2. 10.1016/j.cgh.2018.08.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy E, & Thompson A (2009). An exploration of attitudes among black Americans towards psychiatric genetic research. Psychiatry, 72(2), 177–194. 10.1521/psyc.2009.72.2.177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institutes of Health. (2018). About the All of Us Research Program. Retrieved September 22, 2018, from https://allofus.nih.gov/about/about-an-us-research-program [Google Scholar]
- Oh SS, White MJ, Gignoux CR, & Burchard EG (2016). Making Precision Medicine Socially Precise. Take a Deep Breath. American Journal of Respiratory and Critical Care Medicine, 193(4), 348–350. 10.1164/rccm.201510-2045ED [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pal T, Permuth-Wey J, Betts JA, Krischer JP, Fiorica J, Arango H,… Sutphen R (2005). BRCA1 and BRCA2 mutations account for a large proportion of ovarian carcinoma cases. Cancer, 104(12), 2807–2816. 10.1002/cncr.21536 [DOI] [PubMed] [Google Scholar]
- Peer D (2014). Precision medicine--delivering the goods? Cancer Letters, 352(1), 2–3. 10.1016/j.canlet.2014.04.011 [DOI] [PubMed] [Google Scholar]
- Peters N, Rose A, & Armstrong K (2004). The association between race and attitudes about predictive genetic testing. Cancer Epidemiology, Biomarkers & Prevention: A Publication of the American Association for Cancer Research, Cosponsored by the American Society of Preventive Oncology, 13(3), 361–365. [PubMed] [Google Scholar]
- Prince AER, & Roche MI (2014). Genetic information, non-discrimination, and privacy protections in genetic counseling practice. Journal of Genetic Counseling, 23(6), 891–902. 10.1007/s10897-014-9743-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Project REDCap. (2017). Software — REDCap. Retrieved September 13, 2017, from https://projectredcap.org/software/ [Google Scholar]
- Ricker C, Lagos V, Feldman N, Hiyama S, Fuentes S, Kumar V,… Weitzel J (2006). If we build it … will they come?--establishing a cancer genetics services clinic for an underserved predominantly Latina cohort. Journal of Genetic Counseling, 15(6), 505–514. 10.1007/s10897-006-9052-5 [DOI] [PubMed] [Google Scholar]
- Rogers EM (2003). Diffusion of innovations. New York: Free Press. [Google Scholar]
- Singer E, Antonucci T, & Van Hoewyk J (2004). Racial and ethnic variations in knowledge and attitudes about genetic testing. Genetic Testing, 8(1), 31–43. 10.1089/109065704323016012 [DOI] [PubMed] [Google Scholar]
- Singer E, Couper MP, Raghunathan TE, Van Hoewyk J, & Antonucci TC (2008). Trends in U.S. Attitudes Toward Genetic Testing, 1990-2004. Public Opinion Quarterly, 72(3), 446–458. 10.1093/poq/nfn033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith CE, Fullerton SM, Dookeran KA, Hampel H, Tin A, Maruthur NM,… Ordovas JM (2016). Using Genetic Technologies To Reduce, Rather Than Widen, Health Disparities. Health Affairs (Project Hope), 35(8), 1367–1373. 10.1377/hlthaff.2015.1476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Susswein LR, Skrzynia C, Lange LA, Booker JK, Graham ML, & Evans JP (2008). Increased uptake of BRCA1/2 genetic testing among African American women with a recent diagnosis of breast cancer. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology, 26(1), 32–36. 10.1200/JCO.2007.10.6377 [DOI] [PubMed] [Google Scholar]
- Suther S, & Kiros G-E (2009). Barriers to the use of genetic testing: a study of racial and ethnic disparities. Genetics in Medicine: Official Journal of the American College of Medical Genetics, 11(9), 655–662. 10.1097/GIM.0b013e3181ab22aa [DOI] [PubMed] [Google Scholar]
- Thompson HS, Valdimarsdottir HB, Jandorf L, & Redd W (2003). Perceived disadvantages and concerns about abuses of genetic testing for cancer risk: differences across African American, Latina and Caucasian women. Patient Education and Counseling, 51(3), 217–227. [DOI] [PubMed] [Google Scholar]
- US Food and Drug Administration. (1998). Trastuzumab, Genentech Herceptin approval letter. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/appletter/1998/trasgen092598L.pdf [Google Scholar]
- US Food and Drug Administration. (2017). US FDA Approval for Trastuzumab [cgvArticle]. Retrieved September 18, 2017, from https://www.cancer.gov/about-cancer/treatment/drugs/fda-trastuzumab [Google Scholar]
- U.S. National Library of Medicine. (2017). What is precision medicine? Retrieved September 19, 2017, from https://ghr.nlm.nih.gov/primer/precisionmedicine/definition [Google Scholar]
- Zimmerman RK, Tabbarah M, Nowalk MP, Raymund M, Jewell IK, Wilson SA, & Ricci EM (2006). Racial differences in beliefs about genetic screening among patients at inner-city neighborhood health centers. Journal of the National Medical Association, 98(3), 370–377. [PMC free article] [PubMed] [Google Scholar]


