Abstract
Purpose:
Timely recognition of critical illness is associated with improved outcomes, but is dependent on accurate triage, which is affected by system factors such as workload and staffing. We sought to first study the effect of delayed recognition on patient outcomes after controlling for system factors and then to identify potential predictors of delayed recognition.
Methods:
We conducted a retrospective cohort study of Emergency Department (ED) patients admitted to the Intensive Care Unit (ICU) directly from the ED or within 48 hours of ED departure. Cohort characteristics were obtained through electronic and standardized chart abstraction. Operational metrics to estimate ED workload and volume using census data were matched to patients’ ED stays. Delayed recognition of critical illness was defined as an absence of an ICU consult in the ED or declination of ICU admission by the ICU team. We employed entropy-balanced multivariate models to examine the association between delayed recognition and development of persistent organ dysfunction and/or death by hospitalization day 28 (POD+D), and multivariable regression modeling to identify factors associated with delayed recognition.
Results:
Increased POD+D was seen for those with delayed recognition (OR 1.82, 95% CI 1.13-2.92). When the delayed recognition was by the ICU team, the patient was 2.61 times more likely to experience POD+D compared to those for whom an ICU consult was requested and were accepted for admission. Lower initial severity of illness score (OR 0.26, 95% CI 0.12-0.53) was predictive of delayed recognition. The odds for delayed recognition decreased when ED workload is higher (OR 0.45, 95% CI 0.23-0.89) compared to times with lower ED workload.
Conclusions:
Increased POD+D is associated with delayed recognition. Patient and system factors such as severity of illness and ED workload influence the odds of delayed recognition of critical illness and need further exploration.
Keywords: emergency department (ED), critically ill, ED boarding, ED crowding, time-to-treatment
Introduction
Timely recognition of critical illness with prompt ICU admission or transfer improves survival, but this decision and process of ICU admission can be influenced by factors such as resource availability at the time of presentation and staff workload.1–3 Delays in ICU admission have been associated with increased risk of mortality.4–7 Patients admitted directly from the ED to the ICU have also been shown to have decreased 30-day mortality compared to patients admitted to the ICU within 24 hours of ward admission.8
The location from which the patient is triaged to the ICU also have a profound impact not only on patient outcomes, but also on resource utilization in the ED and medical wards, as these locations are less likely to be staffed to care for critically ill patients.9–11 Given these limited resources to care for critically ill patients in the ED and wards, poorer outcomes for transferred ICU patients may be attributable in part to resource and staffing constraints in the pre-ICU setting.12,13 These system factors, including ED capacity strain and workload and hospital volume and staffing ratios not matched to an ICU setting can have a negative impact on patients’ morbidity and mortality.14–16 Similarly, ICU workload and capacity strain may also contribute, as excessive patient volume can compromise efficient throughput and the ICU team’s assistance with off-site critically ill patients.17–20 As ICU beds and staff are finite resources, appropriate recognition of critical illness and allocation of these resources through triage is essential.21,22
While delays in ICU transfer have been shown to have a negative impact on outcome,2 the impact of delayed recognition of a patient’s critically ill status, after accounting for system factors affecting resource availability, is not fully described. We seek to assess the effect of delayed recognition on patient outcomes, adjusting for both patient and system factors. We then explore the contribution of patient and system factors on the likelihood for delayed recognition to identify future areas for improvement and intervention. We hypothesize that delayed recognition of critical illness increases the odds of adverse patient outcomes despite controlling for patient and system factors. Our secondary hypothesis is that the odds of delayed recognition increase as ED crowding and workload increase, contributing to the adverse patient outcomes.
Methods
Study Setting and Population
The cohort included patients from a single, academic, urban, 1,134 bed-tertiary care center in New York City with an ED serving an average of 300 visits a day and more than 100,000 visits annually with an average of 300 visits per day. In this 61-bed unit, there is a 5 bed resuscitation bay dedicated the care and monitoring of high acuity patients, those that decompensate while undergoing work up in other parts of the ED, and those designated for and boarding prior to ICU admission. This area is staffed by an ED attending physician. a second year resident, and a 1:3 nursing ratio. The ED team with recommendations and assistance from the ICU team manages the patients in this area until the patient arrives in the ICU. The medical ICU is a 14-bed closed unit, operating at a 91% average occupancy (average census 12.8) with a 1:2 nurse-to-patient ratio. There are also 5 other units (surgical, cardiac, 2 cardiothoracic, and neurosurgical) with 68 additional beds (average census of 57.0) that may serve as overflow units for MICU patients when there is no MICU bed available.
During the study period, the ED team initiated all ICU consults, which were initially seen by a Pulmonary and Critical Care Medicine (PCCM) fellow and a PCCM attending physician. All ICU triage decisions were communicated in-person with the bedside ED team with additional treatment recommendations as needed. For patients already admitted to an inpatient team, requests for ICU transfer were initiated by the primary medical team, consisting of medical housestaff and hospitalist attending physicians, with a consult and associated decision for admission given by the ICU team.
The patient cohort includes all adult ED patients (age 18 years and older) who were admitted to the Medical ICU directly from the ED or within 48 hours of ED departure to the inpatient setting, over a 21 month period from October 01, 2013 to June 30, 2015. The cohort was limited to those admitted to the ICU within 48 hours of ED departure to the inpatient setting to minimize confounding by inpatient hospital management or new disease processes.23
Study Design and Measurements
This retrospective cohort study of critically ill ED patients included data queried from electronic health records (EHR) clinical data, operational metrics, and hourly census obtained through the institution’s Data Warehouse. Electronic data capture was validated and further expanded with standardized EHR chart abstraction by trained reviewers. The timing and triage decisions for requests for ICU admission were collected from a structured internal record of Medical ICU consults logged by the fellow physicians at the time of consult request and completion (See Table A1 in Online Appendix for consult log template and data abstraction tool).2
The primary outcome was a composite measure of in-hospital morbidity or mortality: the presence of persistent organ dysfunction or death (POD+D), defined as in-hospital mortality, including discharge to a hospice facility/service, persistent use of vasopressors, the use of new dialysis, or the continued use of invasive mechanical ventilation, by day 28 of hospitalization.24 The primary predictor of interest was delayed recognition of critically ill patients defined as either a) those patients for whom an ICU consult for admission was not requested by the ED team, or b) those patients who were declined for ICU admission by the ICU team.
Covariates of interest included patient characteristics such as age, gender, race/ethnicity, insurance, pre-hospital location (nursing facility/hospital vs. home), severity of illness calculation using the Mortality Probability Model III scores on ICU admission (MPM0-III),25 primary admission critical care diagnosis categories grouped according to the Society for Critical Care Medicine Diagnosis Model,26 any care limitations on admission (no care limitations vs. any care limitations), and ED shift at time of arrival (Night vs. Day). Other key covariates included system factors, specifically ED workload and ED and ICU capacity strain.27 To approximate ED workload experienced during a specific patient visit, ED-specific measures of resource availability and strain were averaged over each patient’s ED stay.27 These included continuous measurements of ED census, the number of critically ill patients, the percentage of active ED patients (those undergoing initial workup and resuscitation, before disposition is determined), and the percentage of higher intensity patients (defined as those requiring eventual inpatient admission) (See Table A2 in Online Appendix). ICU-specific measures included timing of ICU consult (Day vs. Night shift), Medical ICU capacity (presence of bed availability at the time of consult), and census in other ICUs at the time of consult. As both the ED resuscitation bay (location of critically ill ED patients) and the Medical ICU operate at greater than 90% occupancy on average, their capacity was defined as categorical variables (full vs. one or more beds available).
This project was approved by the institutional review board at the study site under expedited review procedure, with a waiver of informed consent.
Statistical Methods
Univariate and bivariate analysis was conducted on continuous and categorical variables. MPM0-III, a continuous variable was log transformed. Comparison between groups using chi-square, Wilcoxon Mann Whitney U, and independent t-tests were completed as appropriate.
The primary analysis examined the association between POD+D and delayed recognition (as defined), using entropy balancing to control for potential confounders. Entropy balancing creates balanced samples in observational studies where the control group can be reweighted to match covariates in the treatment group to reduce noise caused by these variables to less than 1%.28,29 Variables that were significantly different by POD+D in bivariate analysis were included in the entropy balance algorithm. Using the entropy-balanced samples, multivariable logistic regression modeling was then used to determine the effect of delayed recognition on POD+D. We also conducted an a priori stratified analysis of the effect of delayed recognition by the ED vs. the ICU teams on POD+D.
To differentiate between delayed recognition and patient throughput delays, ED patients experiencing prolonged boarding due to limited ICU bed availability after an ED-initiated ICU consult and acceptance for ICU admission, were classified as having no delays in critical illness recognition. Only those who remained in the ED without an ICU consult, those that were denied ICU admission by the ICU team, or those sent to the wards without an ICU consult, that eventually needed an ICU within 48 hours were classified as delayed. All of our models were adjusted for ED length-of-stay (LOS) or time to ICU admission to adjust for the effects of prolonged boarding or delays in transfers. (Other time to consult and pre-ICU boarding characteristics that were tested are detailed in Online Appendix Table A3).
For our secondary exploratory analysis, we sought to determine predictors of delayed recognition using multivariable logistic regression modeling. Census variables were divided into quartiles to test the role of increasing workload. Goodness of fit and optimal models were determined using the Akaike information criterion (AIC) and R2. All hypotheses were evaluated using 2 tailed tests with a significant p-value of less than 0.05. All analyses were conducted using Stata 14.1 (StataCorp LP, College Station, TX).
Results
Baseline Characteristics
During the study period, 672 ED patients were admitted to the ICU within 48 hours of presentation, of which 143 (21.3%) experienced delayed recognition of critical illness (see Figure A1 in Online Appendix). Analysis of the baseline cohort characteristics, described in Table 1, showed significant differences between groups, as those in the delayed recognition group had lower MPM0-III scores, presented during ED night shift, and experienced longer ED and hospital LOS. Those that had delayed recognition of critical illness had lower MPM0-III scores, presented more often during ED night shift, and had higher ED and hospital LOS. The ED resuscitation bay was at capacity more often for those without delayed recognition, while there was no difference in medical ICU bed availability. (See Online Appendix Table A2). Time from ED arrival to ICU consult, as well as time from ICU consult to ICU admission was also longer in those with delayed recognition (See Online Appendix Table A3).
Table 1.
Baseline Patient-Level Characteristics for Study Cohort of Emergency Department (ED) Patients Who Were Admitted to the Intensive Care Unit (ICU) Directly From the ED or Within 48 Hours of ED Departure.
| Baseline characteristic | Patients without delayed recognition of critical illness, N = 529 | Patients with delayed recognition of critical illness, N = 143 | ||
|---|---|---|---|---|
| Patient Characteristics | ||||
| Age, median, IQR | 62 | 52 to 71 | 64 | 52 to 77 |
| Female gender, N % | 264 | 49.9 | 75 | 52.5 |
| Race | ||||
| Caucasian | 135 | 25.5 | 35 | 24.5 |
| African American | 147 | 27.8 | 46 | 32.2 |
| Hispanic/Latino | 182 | 34.4 | 42 | 29.4 |
| Other/unknown | 65 | 12.3 | 20 | 14.0 |
| Critical illness diagnosis category | ||||
| Respiratory failure | 192 | 36.3 | 48 | 33.6 |
| Septic shock | 68 | 12.9 | 18 | 12.6 |
| sGastrointestinal bleed | 62 | 11.7 | 8 | 5.6 |
| Cardiovascular illness | 49 | 9.3 | 7 | 4.9 |
| Other | 104 | 19.7 | 30 | 21.0 |
| Unknown/none | 54 | 10.2 | 32 | 22.4 |
| Severity of illness score (Log10MPM0-III score), median, IQRa | −0.82 | −1.16 to −0.55 | −0.93 | −1.24 to −0.64 |
| Charlson Comorbidity Score, median, IQR | 3 | 1 to 5 | 3 | 1 to 5 |
| Code status at time of consult, N % | ||||
| No care limitations (full code) | 403 | 97.1 | 64 | 94.1 |
| Care limitation (Do not resuscitate/intubate) | 12 | 2.9 | 4 | 5.9 |
| Night vs day shift presentation, N %a | 239 | 45.18 | 89 | 62.24 |
| Hospital course characteristics | ||||
| ED LOS, hours, median, IQRa | 8.2 | 5.6 to 12.0 | 11.9 | 7.7 to 21.3 |
| Hospital LOS, days, median, IQRa | 8.3 | 4.3 to 16.0 | 10.0 | 6.3 to 17.9 |
| ICU LOS, days, median, IQR | 3.0 | 1.7 to 6.2 | 2.9 | 1.5 to 7.3 |
| Mortality at 28 days, N % | 101 | 19.1 | 35 | 24.8 |
| Location of death, N % | ||||
| ICU | 82 | 81.2 | 26 | 70.3 |
| Ward | 15 | 14.9 | 5 | 14.2 |
| Hospice | 4 | 4.0 | 4 | 11.4 |
Baseline differences statistically significant, p < 0.05.
Abbreviations: ED, emergency department; BMI, body-mass index; LOS, length of stay; ICU, intensive care unit; N, Number; IQR, interquartile range; Log10 MPM0-III, logarithm of mortality probability model on admission.
Association of Delayed Recognition and POD+D
In an unadjusted analysis, those patients with delayed recognition had a high percentage of pressor and mechanical ventilation use at 28 days. (See Table A5). Using the entropy-balanced samples (Online Appendix Table A4), a multivariate logistic regression model adjusted for patient factors showed that delayed recognition of critical illness (OR 1.82, 95% CI 1.13-2.92) was associated with a 82% increase in odds of POD+D (Table 2). This increase in likelihood of POD+D remained prominent in the delayed group for all levels of severity of illness (Figure 1). In the stratified analysis looking at delays in critical illness recognition by the ED or by the ICU, we found a trend toward an increase in odds for POD+D when the ED team did not request an ICU consult, (see Table A6). When ICU team denied ICU admission when consulted by the ED, the patient was 2.61 times more likely to experience POD+D compared to those directly accepted after ICU consult (see Table A7). Patient factors affecting POD+D included Charlson Comorbidity Score (OR 1.26, 95% CI 1.15-1.38), having septic shock (OR 0.39, 95% CI 0.18–0.86), GI bleeding (OR 0.23, 95% CI 0.09-0.56), or other critical illness diagnosis (OR 0.69, 95% CI 0.17-0.56) compared to respiratory failure, being from a facility compared to being from home (OR 3.54, 95% CI 1.691-6.55), severity of illness definite by the Log10MPM0-III score (OR 2.48, 95% CI 1.89-3.26), and hospital length of stay (OR 1.03, 95% CI 1.01-1.05).
Table 2.
Association Between Delayed Recognition# of Critical Illness and Persistent Organ Dysfunction + Death (POD+D); N = 672.
| Covariates | OR | 95% CI | |
|---|---|---|---|
| Delayed Recognition of Critical Illness** | 1.82 | 1.13 | 2.92 |
| Age** | 0.98 | 0.97 | 1.00 |
| Female Gender | 1.37 | 0.88 | 2.14 |
| Race | |||
| Caucasian | Reference | ||
| African American | 1.59 | 0.85 | 2.96 |
| Hispanic/Latino | 0.79 | 0.43 | 1.44 |
| Other/Unknown | 0.64 | 0.30 | 1.40 |
| Payor | |||
| Medicare or Private Payor | Reference | ||
| Medicaid | 0.78 | 0.45 | 1.35 |
| Self-Pay/Other | 0.89 | 0.29 | 2.75 |
| Charlson Comorbidity Score*** | 1.26 | 1.15 | 1.38 |
| Critical Illness Diagnosis Category | |||
| Respiratory failure | Reference | ||
| Septic shock** | 0.39 | 0.18 | 0.86 |
| Gastrointestinal bleed*** | 0.23 | 0.09 | 0.56 |
| Cardiovascular illness | 0.43 | 0.19 | 1.02 |
| Other*** | 0.30 | 0.17 | 0.56 |
| Unknown/none | 0.69 | 0.36 | 1.33 |
| Origin from nursing home or facility vs. home*** | 3.54 | 1.91 | 6.55 |
| Severity of Illness Score (Log10MPM0-III score)*** | 2.48 | 1.89 | 3.26 |
| Hospital Length of Stay*** | 1.03 | 1.01 | 1.05 |
| ED Length of Stay | 1.00 | 0.98 | 1.03 |
Statistically significant,
p < 0.01,
p < 0.05.
Results from an entropy balanced multivariate logistic regression model.
Delayed recognition is defined as those patients for whom an ICU consult for admission was not requested by the ED team or who were declined for ICU admission by the ICU team while still in the ED.
Abbreviations: OR = Odds ratio; 95% CI = 95% Confidence Interval; Log10 MPM0-III = Logarithm of Mortality Probability Model on Admission.
Figure 1.
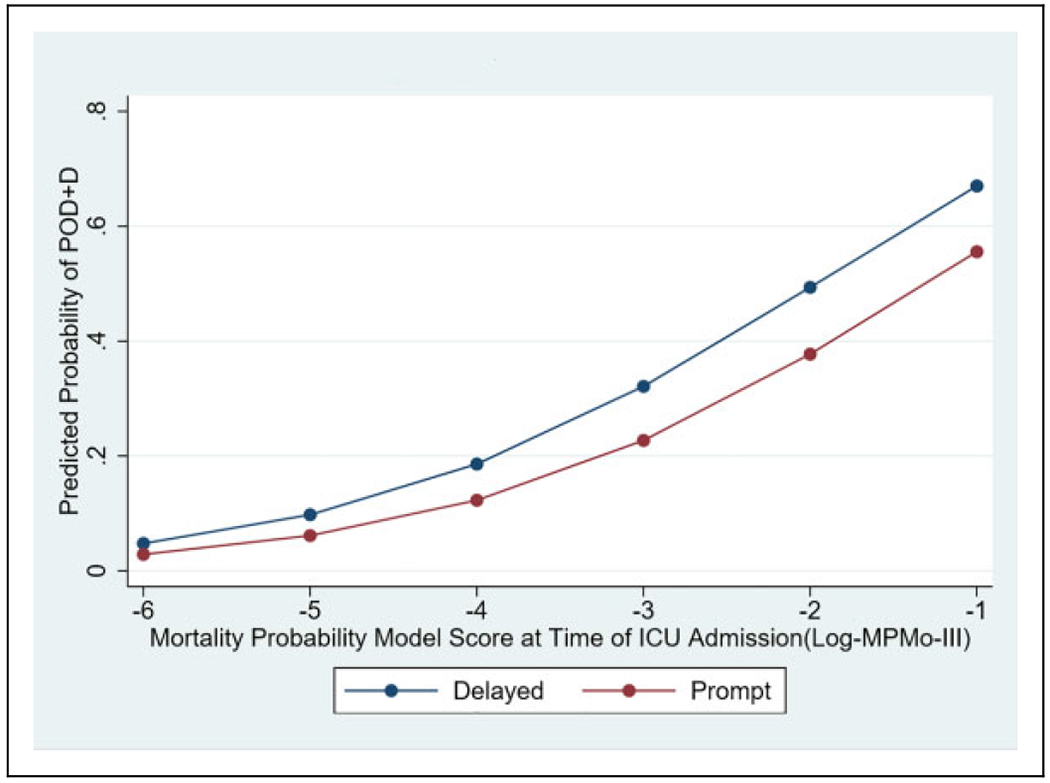
Predicted probability of Persistent Organ Dysfunction + Death (POD+D) by Logarithm of Mortality Probability Model on Admission (Log10MPM0-III) stratified by patients with delayed recognition of critical illness or prompt recognition of critical illness. In this cohort of critically ill ED patients admitted to the ICU within 48 hours of presentation, delayed recognition of critical illness is associated with an increase in the probability of dying or having significant morbidity during the hospitalization.
Predictors of Delayed Recognition
Age (OR 1.03, 95% CI 1.01-1.05) and time from ED arrival to first ICU consult (OR 1.14, 95% CI 1.11-1.17) were predictive of delayed recognition of critical illness. Having a lower severity of illness score at presentation (log10MPM0-III) (OR 0.26, 95% CI 0.12-0.53) was also predictive of delayed recognition (please note predictor variable was log transformed). We chose to log transform MPM0-III (which was not normally distributed) vs. segmenting since it is clinically more appropriate as a continuous variable; too much information was lost with categorizing based on distribution as they were clinically meaningless cutoffs. The odds for delayed recognition were decreased during heavier ED workload periods (represented by the volume of high intensity ED patients) (OR 0.45, 95% CI 0.23-0.89) compared to times with lighter ED workload (Table 3).
Table 3.
Predictors of Delayed Recognition of Critical Illness: Results From the Multivariate Logistic Regression Model.
| Predictors | OR | 95% CI | |
|---|---|---|---|
| Age*** | 1.03 | 1.01 | 1.05 |
| Female Sex (Reference: Male) | 1.26 | 0.80 | 2.00 |
| Race | |||
| Caucasian | Reference | ||
| African American | 1.66 | 0.89 | 3.12 |
| Hispanic/Latino | 1.14 | 0.61 | 2.15 |
| Other/Unknown | 1.46 | 0.67 | 3.18 |
| Payor | |||
| Medicare or Private Payor | Reference | ||
| Medicaid | 1.20 | 0.67 | 2.16 |
| Self-pay/Other | 0.50 | 0.12 | 2.01 |
| Charlson Comorbidity Score | 1.06 | 0.96 | 1.16 |
| Critical Illness Diagnosis Category | |||
| Respiratory failure | Reference | ||
| Septic shock | 0.78 | 0.40 | 1.53 |
| Gastrointestinal bleed | 0.72 | 0.30 | 1.71 |
| Cardiovascular illness | 0.46 | 0.17 | 1.22 |
| Other | 0.43 | 0.14 | 1.28 |
| Unknown/none | 0.72 | 0.34 | 1.52 |
| Origin from nursing home or facility vs. home | 1.15 | 0.48 | 2.78 |
| Severity of Illness Score (Log10MPM0-III score)*** | 0.26 | 0.12 | 0.53 |
| ED Arrival to First ICU Consult (Hours)*** | 1.14 | 1.11 | 1.17 |
| Volume of high intensity ED patients (requiring eventual admission) | |||
| First quartile | Reference | ||
| Second quartile | 0.85 | 0.45 | 1.60 |
| Third quartile | 1.17 | 0.64 | 2.14 |
| Fourth quartile** | 0.45 | 0.23 | 0.89 |
Statistically significant,
p < 0.01
p < 0.05.
Abbreviations: OR = Odds ratio; 95% CI = 95% Confidence Interval; ICU = Intensive Care Unit; Log10 MPM0-III = Logarithm of Mortality Probability Model on Admission; ESI = Emergency Severity Index.
Discussion
In contrast to previous studies which address delays in transfers to the ICU or boarding time,4,6,8,30 our study focused on the contribution of delayed recognition of critical illness on morbidity and mortality while adjusting for delays in transfer and boarding time. Our findings show that despite controlling for clinical presentation and ED course, there is a continued association between delayed recognition of critical illness and morbidity and mortality. While our model does not account for many factors that can affect a clinician’s ability to recognize the critically ill patient, our results support that this problem cannot be solved by just addressing boarding times or transfer delays alone.
We also found that patients declined for ICU admission after the first ICU consult had a significantly higher likelihood of POD+D. While we saw a similar trend toward increased odds of POD+D when the ED failed to request a consult, this was not statistically significant. Delving deeper into the reasons for delayed recognition of critical illness by the ED or ICU, including reasoning for initial and later consults, might present a clearer understanding of the effects of delayed recognition of critical illness on patient outcomes. Of the 65 patients in the subset had delayed recognition by the ICU, 32 patients were accepted from the ED after second consult, and 33 from the floor. The number of subjects within each category is too small to make any meaningful conclusions; however, a more granular analysis of why the ICU denied the patient admission might also provide more insight into whether these are true delays in critical illness recognition by the ICU affecting patient outcomes versus decisions made by the ICU team based on the patient’s likelihood to benefit from critical care.31 Several aspects, including patient, system, and provider factors, affect initial triage decision making and warrant further exploration and research.32–34 While this data is not available within our current dataset and is a limitation of this study, it presents an avenue for future research, where more granular aspects of factors influencing triage decisions, such as the number of waiting patients, available beds, functional status, reasoning behind initial rejection followed by acceptance of patient are considered.
Not surprisingly, a lower severity of illness by log10MPM0-III was also predictive of delayed recognition, and was different between those with and without delayed recognition. One reason for this might be that these patients have a more indolent presentation and may not overtly declare themselves immediately as requiring ICU admission (e.g., through hemodynamic instability, worsening of other objective parameters, or need for critical care interventions). We had also hypothesized that the delayed recognition of critical illness could be attributed to increased workload; however, our findings supported the converse, where increasing workload led to more ED-based ICU consults. As factors such as particular staffing ratios in the ED and pre-ICU monitoring of critically ill patients vary and have an effect on delayed recognition, it was important to control for them when determining their contribution toward delayed recognition within our cohort. There may be a workload threshold to prompt ICU consults sooner to help off-load the cognitive load on the staff. The effect of workload on delayed recognition of critical illness, which is an important consideration when staffing EDs and ICUs during high demand or periods of surge, or when assessing patients during off-peak hours with limited staff warrants more exploration.
A major strength of our study was our precise capture of care delivery at the ED-ICU interface, specifically details of the timing of ICU consultation for admission, the associated triage decision, and granular census variables with operational determinations of acuity based on disposition selection, timing, and location within the ED. These variables allowed us to more accurately adjust our analysis for system-related factors, improving our understanding of the impact of operational factors on care delivery and associated downstream patient outcomes. In contrast to the limitations of many retrospective studies, our process timestamp data helped to differentiate delays in critical illness recognition from delays attributable to low inpatient bed availability, the latter of which has been shown to worsen their outcomes.2 Our models were adjusted for ED LOS and time to ICU admission, and while this does not account for all delays in care delivery, it attenuates some of the effect of prolonged boarding after ICU acceptance. Additionally, our use of a composite endpoint that measures both morbidity and mortality as an outcome also strengthens our study as the true impact of delayed recognition of critical illness might be underestimated when the primary outcome is limited strictly to mortality. While the generalizability of our findings are somewhat limited by institutional-specific triage and ICU admission policies, our approach and inclusion of these processes and system factors in our modeling is informative to understanding pre-ICU critical care delivery. Finally, our findings are strengthened by the use of entropy balancing to account for confounding in this retrospective observational cohort.
Limitations of our study are common to retrospective studies that require electronic capture of data which include limited capture of the frequency and nature of MD- and nurse-patient contact in the ED, events within the hospital course, or timing of re-consult to the ICU which presumably could contribute to POD+D. However, our electronic data collection allowed for more robust and accurate measurement of surrogate markers of ED workload to better estimate ED provider cognitive load. The data also does not contain the exact reason for delay of ICU consult and admission, but models delayed recognition based on available predictors. To capture as many patients as possible for whom their decompensation could be attributable to their ED presentation, we limited our cohort to those transferred to the ED within 48 hours, understanding that outcomes may vary based on timeframes of delays in recognition of critical illness. Our sample size was insufficient to perform robust comparisons between smaller timeframes (e.g., 6, 12, 18, and 24 hours). Our cohort is also limited to a single center serving a large, urban, and diverse catchment area but without major burn, trauma, or pediatric cases; therefore, the generalizability of the data to other disparate systems might be limited. However, most ED patients requiring an ICU level of care were triaged by the medical ICU team with suggestions for surgical or cardiovascular interventions and consultations.
Conclusion
Delayed recognition is associated with increased patient morbidity and mortality. Patient and system factors such as severity of illness and ED workload influence the odds of delayed recognition of critical illness and need further exploration.
Supplementary Material
Acknowledgments
We would also like to acknowledge Ioannis Konstantinidis, MD, and Marie Lauzon, MS, for their contribution to our work.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported in part through the Mount Sinai Data Warehouse (MSDW) resources and staff expertise provided by Scientific Computing at the Icahn School of Medicine at Mount Sinai.
Declaration of Conflicting Interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article. NNG has received study support from the NIH National Heart, Lung, and Blood Institute (Award: DHHS-1T32 HL129974-PI: Richardson). KSM has received study support from the NIH National Heart, Lung, and Blood Institute (Award: 1K23HL130648-PI: Mathews). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute and the National Institutes of Health. [NNG] reports no additional conflict of interest other than the above funding sources, and contributed to this work through data analysis, and manuscript preparation. [MSD] reports no conflict of interest, and contributed to this work through conceptual design and data collection. [CVT] reports no conflict of interest, and contributed to this work through data analysis. [LDR] reports no conflict of interest, and contributed to this work through conceptual design. [KSM] reports no additional conflict of interest other than the above funding sources, and contributed to this work through conceptual design, data collection, analysis, and manuscript preparation.
Footnotes
Preliminary results from the work described in this manuscript was presented at the May 2017 American Thoracic Society Annual Meeting, Washington D.C.
Supplemental Material
Supplemental material for this article is available online.
References
- 1.Gopalan PD, Pershad S. Decision-making in ICU—a systematic review of factors considered important by ICU clinician decision makers with regard to ICU triage decisions. J Crit Care. 2019;50: 99–110. [DOI] [PubMed] [Google Scholar]
- 2.Mathews KS, Durst MS, Vargas-Torres C, Olson AD, Mazumdar M, Richardson LD. Effect of emergency department and ICU occupancy on admission decisions and outcomes for critically ill patients. Crit Care Med. 2018;46(5):720–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Greenland CNL, Termorshuizen F, Rietdijk WJR, et al. Emergency department to ICU time is associated with hospital mortality: a registry analysis of 14,788 patients from six university hospitals in The Netherlands. Crit Care Med. 2019;47(11): 1564–1571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cardoso LT, Grion CM, Matsuo T, et al. Impact of delayed admission to intensive care units on mortality of critically ill patients: a cohort study. Crit Care. 2011;15(1):R28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chalfin DB, Trzeciak S, Likourezos A, Baumann BM, Dellinger RP; Delay-ED study group. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007;35(6):1477–1483. [DOI] [PubMed] [Google Scholar]
- 6.Churpek MM, Wendlandt B, Zadravecz FJ, Adhikari R, Winslow C, Edelson DP. Association between intensive care unit transfer delay and hospital mortality: a multicenter investigation. J Hosp Med. 2016;11(11):757–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Young MP, Gooder VJ, McBride K, James B, Fisher ES. Inpatient transfers to the intensive care unit: delays are associated with increased mortality and morbidity. J Gen Intern Med. 2003; 18(2):77–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parkhe M, Myles PS, Leach DS, Maclean AV. Outcome of emergency department patients with delayed admission to an intensive care unit. Emerg Med (Fremantle). 2002;14(1):50–57. [DOI] [PubMed] [Google Scholar]
- 9.Edbrooke DL, Minelli C, Mills GH, et al. Implications of ICU triage decisions on patient mortality: a cost-effectiveness analysis. Crit Care. 2011;15(1):R56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Robert R, Coudroy R, Ragot S, et al. Influence of ICU-bed availability on ICU admission decisions. Ann Intensive Care. 2015; 5(1):55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stelfox HT, Hemmelgarn BR, Bagshaw SM, et al. Intensive care unit bed availability and outcomes for hospitalized patients with sudden clinical deterioration. Arch Intern Med. 2012;172(6): 467–474. [DOI] [PubMed] [Google Scholar]
- 12.McQuillan P, Pilkington S, Allan A, et al. Confidential inquiry into quality of care before admission to intensive care. BMJ. 1998; 316(7148):1853–1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eriksson CO, Stoner RC, Eden KB, Newgard CD, Guise JM. The association between hospital capacity strain and inpatient outcomes in highly developed countries: a systematic review. J Gen Intern Med. 2017;32(6):686–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Perimal-Lewis L, Hakendorf PH, Thompson CH. Characteristics favouring a delayed disposition decision in the emergency department. Intern Med J. 2015;45(2):155–159. [DOI] [PubMed] [Google Scholar]
- 15.Perimal-Lewis L, Ben-Tovim DI, Li JY, Hakendorf PH, Thompson CH. Emergency department lengths of stay: characteristics favouring a delay to the admission decision as distinct from a delay while awaiting an inpatient bed. Intern Med J. 2014; 44(4):384–389. [DOI] [PubMed] [Google Scholar]
- 16.Boarding of admitted and intensive care patients in the emergency department. Ann Emerg Med. 2017;70(6):940–941. [DOI] [PubMed] [Google Scholar]
- 17.Tarnow-Mordi WO, Hau C, Warden A, Shearer AJ. Hospital mortality in relation to staff workload: a 4-year study in an adult intensive-care unit. Lancet. 2000;356(9225):185–189. [DOI] [PubMed] [Google Scholar]
- 18.Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K. Nurse-staffing levels and the quality of care in hospitals. N Engl J Med. 2002;346(22):1715–1722. [DOI] [PubMed] [Google Scholar]
- 19.Lapichino G, Gattinoni L, Radrizzani D, et al. Volume of activity and occupancy rate in intensive care units. Association with mortality. Intensive Care Med. 2004;30(2):290–297. [DOI] [PubMed] [Google Scholar]
- 20.Dimick JB, Pronovost PJ, Heitmiller RF, Lipsett PA. Intensive care unit physician staffing is associated with decreased length of stay, hospital cost, and complications after esophageal resection. Crit Care Med. 2001;29(4):753–758. [DOI] [PubMed] [Google Scholar]
- 21.Wagner J, Gabler NB, Ratcliffe SJ, Brown SE, Strom BL, Halpern SD. Outcomes among patients discharged from busy intensive care units. Ann Intern Med. 2013;159(7):447–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mery E, Kahn JM. Does space make waste? The influence of ICU bed capacity on admission decisions. Crit Care. 2013;17(3):315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kennedy M, Joyce N, Howell MD, Lawrence Mottley J, Shapiro NI. Identifying infected emergency department patients admitted to the hospital ward at risk of clinical deterioration and intensive care unit transfer. Acad Emerg Med. 2010;17(10): 1080–1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Heyland DK, Muscedere J, Drover J, Jiang X, Day AGCanadian Critical Care Trials Group. Persistent organ dysfunction plus death: a novel, composite outcome measure for critical care trials. Crit Care. 2011;15(2):R98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Higgins TL, Teres D, Copes WS, Nathanson BH, Stark M, Kramer AA. Assessing contemporary intensive care unit outcome: an updated mortality probability admission model (MPM0-III). Crit Care Med. 2007;35(3):827–835. [DOI] [PubMed] [Google Scholar]
- 26.Nates JL, Nunnally M, Kleinpell R, et al. ICU admission, discharge, and triage guidelines: a framework to enhance clinical operations, development of institutional policies, and further research. Crit Care Med. 2016;44(8):1553–1602. [DOI] [PubMed] [Google Scholar]
- 27.Owyang CG, Kim JL, Loo G, Ranginwala S, Mathews KS. The effect of emergency department crowding on lung-protective ventilation utilization for critically ill patients. J Crit Care. 2019;52: 40–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhao Q, Percival D. Entropy balancing is doubly robust. J Causal Inference. 2016;5:23. [Google Scholar]
- 29.Hainmueller J, Xu Y.ebalance: a Stata package for entropy balancing. J Stat Softw. 2013;54(7):1–18. [Google Scholar]
- 30.Al-Qahtani S, Alsultan A, Haddad S, et al. The association of duration of boarding in the emergency room and the outcome of patients admitted to the intensive care unit. BMC Emerg Med. 2017;17(1):34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Valley TS, Admon AJ, Zahuranec DB, Garland A, Fagerlin A, Iwashyna TJ. Estimating ICU benefit: a randomized study of physicians. Crit Care Med. 2019;47(1):62–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goel NN, Rodriguez S, Vidal K, et al. Triage decision-making by ICU and emergency medicine physicians: a mixed methods analysis. C95. Enhancing Patient-Centered Care in Critical Care: A5574-A5574. American Journal of Respiratory and Critical Care Medicine, 2019;199:A5574. [Google Scholar]
- 33.Flaatten H, Van Heerden V, Jung C, et al. The good, the bad and the ugly: pandemic priority decisions and triage. J Med Ethics. 2020;0:1–3. doi: 10.1136/medethics-2020-106489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rathi NK, Haque SA, Morales F, et al. Variability in triage practices for critically ill cancer patients: a randomized controlled trial. J Crit Care. 2019;53:18–24. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


