Abstract
Background:
Oxygen and continuous positive airway pressure (CPAP) are primary modes of respiratory support for preterm infants. Animal models, however, have demonstrated adverse unintended effects of hyperoxia and CPAP on lung development. We investigate the effects of combined neonatal hyperoxia and CPAP exposure on airway function and morphology in mice.
Methods:
Newborn mice were exposed to hyperoxia (40% O2) 24hrs/day for 7 consecutive days with or without daily (3hrs/day) concomitant CPAP. Two weeks after CPAP and/or hyperoxia treatment ended, lungs were assessed for airway (AW) hyperreactivity and morphology.
Results:
CPAP and hyperoxia exposure alone increased airway reactivity compared to untreated control mice. CPAP-induced airway hyperreactivity was associated with epithelial and smooth muscle proliferation. In contrast, combined CPAP and hyperoxia treatment no longer resulted in increased airway reactivity, which was associated with normalization of smooth muscle and epithelial proliferation to values similar to untreated mice.
Conclusions:
Our data suggests the combination of CPAP and hyperoxia decreases the adverse consequences on airway remodeling of either intervention alone. The complex interaction between mechanical stretch (via CPAP) and hyperoxia exposure on development of immature airways has implications for the pathophysiology of airway disease in former preterm infants receiving non-invasive respiratory support.
BACKGROUND
Despite marked improvement in the mortality of infants born preterm, respiratory morbidity in this population remains excessive. Chronic pulmonary insufficiency of prematurity after preterm birth persists in this population through infancy, childhood, and beyond (1). In extremely low birth weight infants it usually begins with a diagnosis of bronchopulmonary dysplasia [BPD], although optimal diagnostic criteria for BPD remain elusive (2). Over the last decade there has been a marked and successful shift from invasive to non-invasive ventilatory support in neonatal intensive care, however, meta-analysis incorporating four large clinical trials failed to demonstrate significant decrease in BPD in infants exposed to a CPAP versus intubation strategy(3).
Assessment of respiratory function in former preterm infants during childhood is typically focused on history of wheezing disorders and measurement of airway function. Doyle evaluated airflow at 8 years of age in three historical cohorts of extremely preterm infants (4). Between 1997 and 2005 there was a significant increase in days on CPAP accompanied by a non-significant decrease in days of endotracheal intubation (4). There was not an accompanying improvement in airway function over this period; in fact, percent predicted value of FEV1 worsened from 92.0±15.7 to 85.4±14.4, p<0.05 between the 1997 and 2005 cohorts, respectively. The authors speculated that increased duration of supplemental oxygen during CPAP may have been contributory. Although primarily a problem of infants born very preterm, increased airway reactivity is also a problem in moderately preterm or late preterm infants (5–7). It is likely that a significant percent of these infants would also have been exposed to supplemental oxygen delivered via non-invasive positive pressure [CPAP or nasal cannula]. As recently concluded by Been et al, research now needs to focus on understanding underlying mechanisms for the increased risk of asthma in survivors of preterm birth (5).
Over recent years we have begun to explore the physiologic consequences of neonatal CPAP or supplemental O2 exposure on later airway function by developing a survivable mouse pup model. In our prior study, neonatal mice were exposed to intermittent CPAP delivered via facial mask from postnatal days 1–7 followed by two-week recovery. We documented significant small airway hyperreactivity at three weeks employing an in vitro lung slice preparation (8). This raised the question whether CPAP might be a contributor to the subsequent airway hyperreactivity manifest by preterm human infants. Although non-invasive positive airway pressure is often administered to preterm infants in room air, low supplement oxygen usually accompanies CPAP. Reyburn employed our neonatal mouse CPAP model to study the effects of combined CPAP and 50% oxygen over the first week on respiratory system mechanics (9). The combination of CPAP and hyperoxia reversed the elevated baseline respiratory system resistance induced by hyperoxic exposure. This led us to hypothesize in the current study that while CPAP and hyperoxia might individually increase airway reactivity in our model, combined exposure may modify these effects and allow us to begin to explore underlying mechanisms.
METHODS
Time-pregnant mice [C57BL/6J] were purchased from a commercial vendor [Charles River] and were later observed to give birth in our animal facility. Mice were treated with or without CPAP in 21% or 40% O2 for the first week of postnatal life; at three weeks of postnatal age [P21] [i.e., two weeks after CPAP or hyperoxia treatment ended] the lungs were removed in preparation for the measurement of airway reactivity using the precision lung slice preparation. All procedures were carried out in accordance with the National Institutes of Health [NIH] guidelines for care and use of laboratory animals, and were approved by the Animal Care and Use Committee at Case Western Reserve University.
Neonatal CPAP and Hyperoxia Exposure:
Following the day of birth [P0] a dam and her litter were randomly assigned to receive either room air [21% O2] or hyperoxia [40% O2] exposure for seven consecutive days. This level of hyperoxia was chosen based on our prior study demonstrating effects of various levels of O2 on lung morphology and airway reactivity (10, 11). In addition, within a given litter, both male and female pups were then randomly assigned to receive either CPAP [6 cm H2O] or no CPAP starting the following day [P1] for the first seven postnatal days. The pups and the dam were maintained in a temperature controlled room during a 12:12 hour, light:dark cycle, and provided food and water ad lib. Each day the mice were removed from the dam and fitted with a custom made mask to fit snuggly around the head for administering CPAP (8, 9). CPAP was administered to unanesthetized mice, while placed on a temperature controlled heat pad [Gaymar T/pump, NY] for temperature support. The mask was designed with an entry port to deliver a flow of humidified gas, which passed through to an exit port to a downstream manometer and an adjustable leak; the leak allowed fine-tuning of the level of CPAP while maintaining flow through the mask. CPAP was maintained at 6 cm H2O by adjusting the downstream leak or the upstream flow into the mask. CPAP lasted just two hours for the first day to minimize time spent away from the nursing dam, but was increased to three hours/session for the following six consecutive days [7 days total]. Control mice were also removed from the dam, fitted with the same masks, placed on the same heat pad, received the same airflow via the same tubing, but did not receive CPAP. These control animals breathed the same humidified gas source, but the tubing from the mask was disconnected from the circuit to prevent any risk of backpressure that may arise by virtue of resistance potentially imposed by the excurrent tubing. After each bout of CPAP the mask was removed and the pups were returned to the mother to resume normal rearing. At the end of the seven days of CPAP the mice were allowed an additional two weeks of uninterrupted maternal care. These groups comprised room air exposed control [no CPAP] and room air CPAP-treated animals. Two other groups were treated the same way as the room air treated animals described above, with the exception that they received 40% O2 for the first postnatal week. Hyperoxia exposure was achieved by placing the dam and her pups in a 38 L Plexiglas chamber with a continuous flow of 40% O2 [4 L/min] for first seven postnatal days. Hyperoxia was achieved by mixing air and 100% oxygen at appropriate amounts to achieve the desired level of oxygen, which was monitored daily [MiniOX I; MSA Medical]. Hyperoxia exposed mice that were designated to receive CPAP were removed from the hyperoxia chamber and immediately placed on a mask that also delivered 40% oxygen while the mice were on the mask to receive CPAP as described above. After the seventh day of exposure, the pups and nursing dam were removed from hyperoxia and allowed to develop normally for an additional 14 days in room air. Airway reactivity [and tissue collection, see below] was assessed at P21 [i.e., 2 wks after treatment] using the in vitro living lung slice preparation, as described previously (8, 10).
Measurement of Airway Reactivity (AWR):
At P21 mice were sacrificed via anesthetic overdose [intraperitoneal injection of a ketamine/xylazine mix (100 mg/kg/10mg/kg, respectively)] to prepare the lungs for in vitro measurement of airway reactivity to methacholine. After death was confirmed the mouse was placed supine for cannulation of the trachea using a syringe loaded with agarose. The cannula [PE tubing, diameter: 0.5 mm (P8) or 0.58 mm (P21)] was inserted through a small ventral incision through the neck and into the anterior most part of the trachea. The cannula was advanced approximately 3 mm and held securely in place with suture. Liquefied agarose [40° C] was gently injected to inflate the lungs [0.8 ml] and the mouse placed in the refrigerator for 30 minutes to allow the agarose to cool and gel. The entire lung was then removed, placed on a vibratome, sliced into 300 μm sections, and immersed in DMEM + Pen/Strep solution for overnight incubation [5% CO2; 37° C]. The following day the lung slices were then rinsed in HBSS and mounted in an in vitro recording chamber for live imaging of airway (AW) responses to increasing doses of methacholine.
For live imaging of individual AWs the slices were covered with a thin, lightweight sheet of mesh and a coverslip, which were held in place with silicone grease. The recording chamber containing the slice was mounted on a microscope [DMLFS, Leica Microsystems, Wetzler, Germany] and perfused [7 ml/min] continuously with HBSS at room temperature using a perfusion pump [MPII, Harvard Apparatus, Holliston, MA]. The microscope mounted with a camera [Rolera Fast, QImaging, Canada] was used to identify individual AWs under 5X magnification. After an initial three minute period of baseline, the chamber was perfused with increasing doses of methacholine and changes in AW lumen area were recorded continuously. The extent of AW constriction in response to increasing doses of methacholine [0.25, 0.5, 1, 2, 4, and 8 μM] was determined at the end of a two minute period of exposure to each dose. Image analysis software [ImageJ] was used to determine the luminal area [in pixels] at each dose of methacholine to determine the extent of AW constriction. The greater the decrease in luminal area, the more reactive the AWs.
Individual AWs were chosen at random and the response to methacholine was performed on one AW/lung section, although we typically collected 2–3 sections per animal. Thus, treatment groups consisted typically of 2–3 AWs/animal spread across 2–3 litters. Measurements of contractility were assessed only on airways less than 0.05 mm2 in lumen area since we showed previously that CPAP effects on airway reactivity were size-dependent (8).
Airway morphology:
Lungs from the four groups were inflation-fixed [25 cm H2O] for 10 minutes with 4% paraformaldehyde, embedded in paraffin, and sectioned at 5 μm. One set was stained with hematoxylin and eosin, and airways identified under light microscopy (Nikon Ti2; 20X Plan Fluor lens; QImaging 12 bit camera). Images were captured and analyzed with Nikon Elements software. Airway epithelial thickness was measured and averaged over 6 points per airway. For consistency, 3 airways of comparable size per lung were selected. Another set of sections was de-paraffinated and immunolabeled with rabbit anti-alpha smooth muscle myosin antibody [1:5,000; Sigma] and Cy3 anti-rabbit antibody. Images were captured on the Nikon microscope with a Photonics high sensitivity camera. The fluorescently tagged area in the mesenchymal layer was measured and normalized to the diameter of the airway.
PCNA Immunohistochemistry:
Lungs from the four groups were inflation-fixed [25 cm H2O] for 10 minutes with 4% paraformaldehyde. The 5 μm paraffin embedded tissue was treated with 3% H2O2 after antigen retrieval. Lung sections were incubated 24 hours at 4° C with rabbit anti-PCNA antibody [1:10,000; Abcam, Cambridge, MA]. The secondary antibody was biotinylated goat anti-rabbit [1:1,000 Jackson ImmunoResearch West Grove, PA, USA], followed by ABC reagent incubation and visualization by diaminobenzidine [Vectastain, Vector Laboratories, Burlingame, CA, USA]. Finally, lung sections were dehydrated and mounted with permount. Primary antibody was omitted for negative controls. All images were obtained using a Rolera XR CCD camera [Q-Imaging, Canada] mounted on a Leica DMLB microscope [Leica Microsystems, Germany]. Images were analyzed using ImageJ 1.47t software [NIH, Bethesda, USA]. Numbers of labeled PCNA were counted in 4–5-five airways at 20X magnification from 5–6 animals/group.
Data Analysis:
Statistical comparison of responses to methacholine between control and CPAP/hyperoxia treated groups was made using a two-way, repeated measures ANOVA. Comparison of airway morphology parameters between groups was made using two-way ANOVA. Differences were considered significant at p <0.05. All values for AW lumen area are expressed as mean ± SEM of all airways and [where relevant] presented as a fraction of initial baseline value, although individual data points are also shown. Sample sizes were based on prior power analysis using Sigmstat/Sigmaplot software based using input values based on our prior studies.
RESULTS:
Airway reactivity to in vitro methacholine:
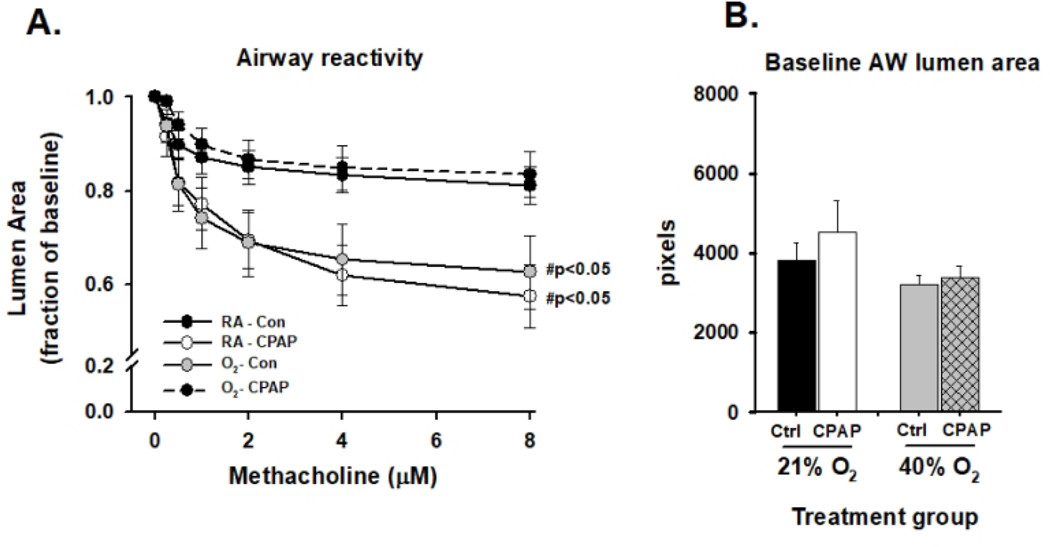
Seven days of neonatal CPAP (RA-CPAP) increased AW constriction to bath-applied methacholine at P21 days compared to untreated control mice (RA-Con; Fig. 1A). Similarly, seven days of neonatal hyperoxia exposure alone (O2-Con) also caused a long-term increase in airway reactivity compared to RA-Con, which was similar in magnitude to RA-CPAP treated mice. In contrast, however, when CPAP was administered simultaneously with hyperoxia (O2-CPAP) for the first postnatal week, airway reactivity was significantly reduced compared with either CPAP or hyperoxia treatment alone (Fig. 1A). In fact, airway reactivity in O2-CPAP treated mice was not different from untreated (RA-Con) mice. There was no difference in baseline airway size between treatment groups (Fig. 1B)
Figure 1:
Airway (AW) responses to methacholine challenge in the in vitro living lung slice preparation from 21 day old male (A) mice pre-treated with 7 days of neonatal (P1-7) CPAP (RA-CPAP), hyperoxia (O2-Con), or combined hyperoxia with CPAP (O2-CPAP). Values are expressed as fraction of baseline lumen size; smaller lumen size at increasing concentration to methacholine signifies increased AW reactivity. Untreated control animals represent animals raised in room air without CPAP treatment (RA-Con). Baseline starting AW lumen area (in image pixels) is also provided to demonstrate studies were performed on airways of equal size between groups (B).#indicates slope of the response for a given treatment group is significantly different from RA-Con. (N=7–10 airways from 4–5 mice/group).
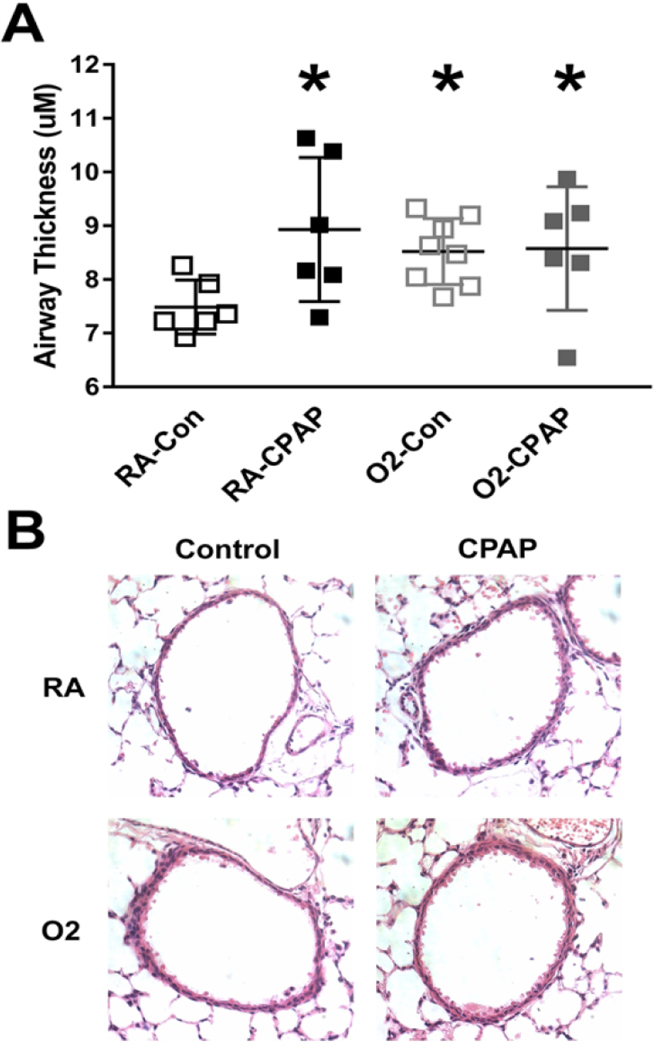
Airway epithelial thickness:
Seven days of neonatal CPAP (RA-CPAP) increased airway epithelial thickness at P21 days compared to RA-Con mice (Fig. 2A), demonstrating a long-term effect on epithelial morphology. Similarly, hyperoxia exposure also increased epithelial thickness compared to O2-Con. Combined hyperoxia and CPAP treatment (O2-CPAP) also caused an increase in airway epithelial thickness and was similar in magnitude to either CPAP or hyperoxia alone (Fig. 2A). Representative images of airways from all four treatment groups are also provided (Fig. 2B).
Figure 2:
Immunohistochemical analysis (H&E staining) of airway thickness in P21 day old mice following neonatal (P1-7) CPAP with or without prior concomitant hyperoxia exposure. Treatment groups include untreated mice (no CPAP raised in room air, RA-Con; Open black squares), CPAP exposure alone (RA-CPAP, solid squares), hyperoxia exposure alone (O2-Con, open grey squares) and combined CPAP with hyperoxia (O2-CPAP, solid grey squares). Values are mean ± SEM; individual squares represent values for individual animals.* indicates sig different from RA-Con group). Representative images are also shown (B). (N=6–8 airways from 3–4 mice/group).
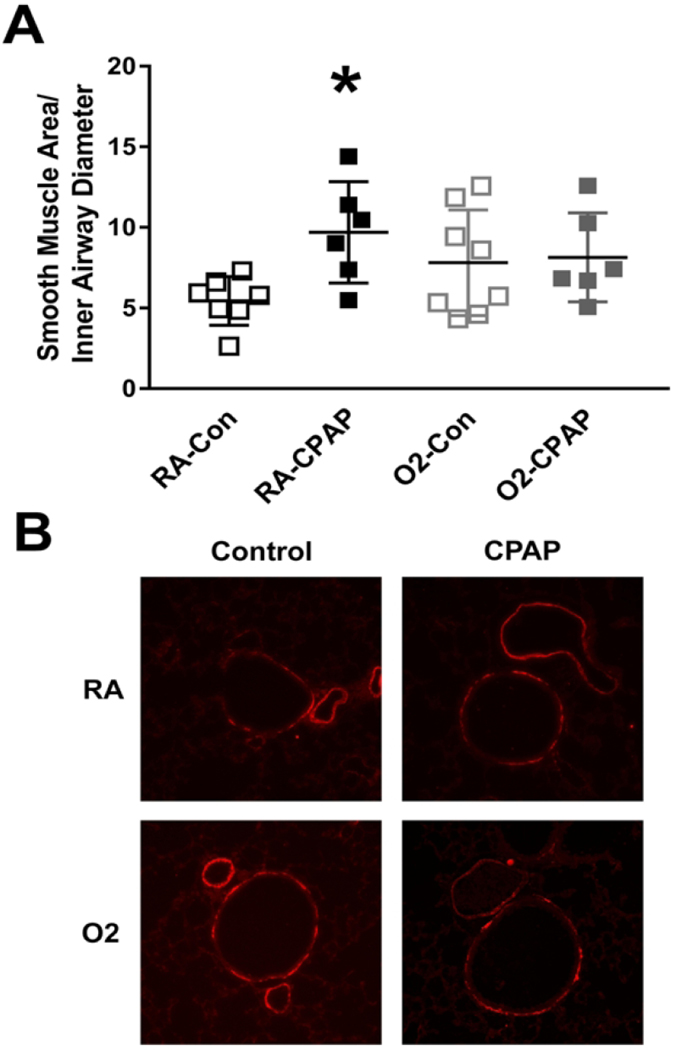
Airway smooth muscle (ASM) area:
Neonatal CPAP (RA-CPAP) increased smooth muscle area at P21 days compared to RA-Con mice (Fig. 3A), demonstrating a long-term effect on airway smooth muscle morphology. Hyperoxia exposure tended to increase smooth muscle area, although this was not statistically significantly different from RA-Con mice. Interestingly, in contrast to the RA-CPAP group, smooth muscle area was no longer increased in the combined O2-CPAP treatment group (Fig. 3A). Representative images of airways from all four treatment groups are also provided (Fig. 3B).
Figure 3:
Immunohistochemical analysis of airway α-smooth muscle actin staining in P21 day old mice following neonatal (P1-7) CPAP with or without prior concomitant hyperoxia exposure. Treatment groups include untreated mice (no CPAP raised in room air, RA-Con; Open black squares), CPAP exposure alone (RA-CPAP, solid squares), hyperoxia exposure alone (O2-Con, open grey squares) and combined CPAP with hyperoxia (O2-CPAP, solid grey squares). Values are mean ± SEM; individual squares represent values for individual animals. * indicates sig different from RA-Con group). Representative images are also shown (B). (N=6–8 airways from 3–4 mice/group).
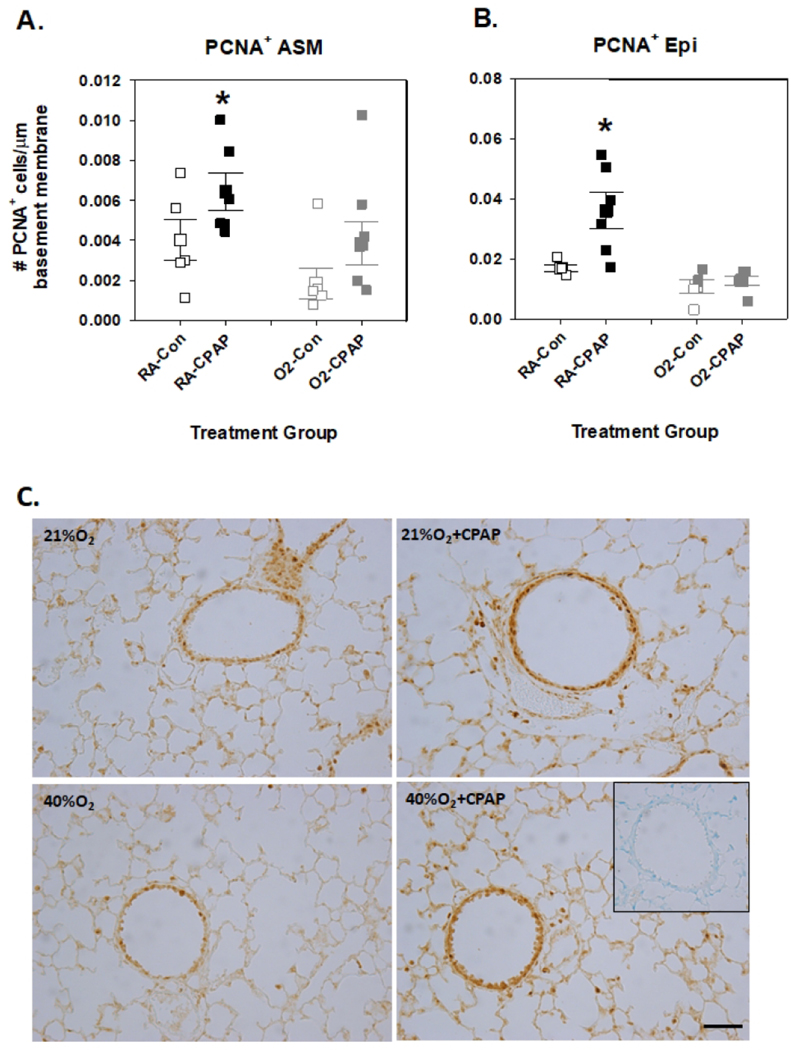
PCNA+ Airway smooth muscle and epithelial cells
As a nuclear marker for identifying cells in a proliferative state, we quantified the number of ASM and epithelial cells stained positively with PCNA. CPAP alone increased the number of both ASM (Fig. 4A) and epithelial cell (Fig. 4B) PCNA+ cells compared to RA-Con mice, whereas hyperoxia alone had no effect. Combined CPAP and O2 exposure prevented the CPAP-induced increase in PCNA+ cells. Representative images are provided in Fig. 4C.
Figure 4:
Analysis of PCNA+ immunoreactivity for airway smooth muscle (A) and epithelium (B) in P21 day old mice following neonatal (P1-7) CPAP with or without prior concomitant hyperoxia exposure. Treatment groups include untreated mice (no CPAP raised in room air, RA-Con; Open black squares), CPAP exposure alone (RA-CPAP, solid squares), hyperoxia exposure alone (O2-Con, open grey squares) and combined CPAP with hyperoxia (O2-CPAP, solid grey squares). Values are mean ± SEM; individual squares represent values for individual animals. * indicates sig different from RA-Con group). Representative images are also shown (C). (N=5–6 airways from 3–4 mice/group).
DISCUSSION:
While the etiology of the chronic lung injury to which preterm infants are predisposed remains multifactorial, supplemental oxygen and intermittent positive pressure delivered via an endotracheal tube are widely implicated (12). It has been difficult to limit hyperoxic exposure to the immature respiratory system, however, non-invasive ventilatory techniques, including CPAP, are now widely employed as an alternative to endotracheal intubation (3, 4). This has motivated our research group to explore the effects of supplemental oxygen and the addition of mask CPAP on subsequent airway function in a neonatal mouse model. Our prior in vivo studies demonstrated that hyperoxia-induced increase in baseline respiratory system resistance (11) was no longer apparent after combined exposure to 50% oxygen and CPAP (9). Therefore, we sought to employ the in vitro lung slice preparation to characterize airway reactivity after individual and combined hyperoxia and CPAP exposures and begin to explore underlying mechanisms.
Numerous investigators have studied the role of hyperoxic exposure in eliciting lung injury in neonatal rodent models, although the focus on airway function after milder degrees of hyperoxia has been somewhat limited (13, 14). We have previously used the in vitro living lung slice preparation to document an increase in methacholine-induced airway contraction after a 7-day exposure to 40% supplemental oxygen followed by a two week normoxic recovery (10). This was accompanied by a decrease in radial alveolar counts and an increase in expression of airway α-smooth muscle actin after hyperoxic exposure (10) although increase in smooth muscle area did not reach significance in the current study.
We have used our novel model of neonatal CPAP administered daily to neonatal mice over the first week of life. CPAP clearly increased airway contractility in the lung slices after two weeks of normoxic recovery. We have previously shown that CPAP administered under normoxic conditions did not affect baseline respiratory system resistance [Rrs] in mouse pups (9). While baseline Rrs cannot be measured in the slice preparation, the currently observed increase in lung slice contractility was consistent with our prior data (8). In the current study, the accompanying increase in airway smooth muscle area is consistent with this physiologic effect of CPAP.
Our data clearly demonstrate that the marked airway hyperreactivity induced individually by mild [40%] hyperoxia and CPAP is eliminated when CPAP is applied in the presence of hyperoxia. These findings suggest that CPAP and hyperoxia increase ASM contractility via different mechanisms, or their combined effects would be synergistic. Hyperoxic exposure has been clearly shown to induce proinflammatory mechanisms in the neonatal lung (15), which in turn, is a likely contributor to the parenchymal lung injury induced by hyperoxia. Our prior data have demonstrated a decrease in lung macrophage infiltration after hyperoxia when there is concurrent CPAP exposure (9), which could contribute to our current observations. We speculate that CPAP-induced stretch and resultant ASM and epithelial proliferation may somehow contribute to normalization of the apparent adverse effects imposed by either treatment alone. Our current data are consistent with recent evidence demonstrating intermittent CPAP limits severe hyperoxia-induced lung damage in a rabbit model of BPD (16), although the effects of CPAP alone were not studied. They observed a decrease in respiratory system resistance when CPAP was superimposed on hyperoxia which is consistent with our prior study (9). Gie et al., [2020] also observed a significant attenuation of hyperoxic-induced changes in epithelial morphology when CPAP was combined with superimposed hyperoxia. They speculated that the benefits of CPAP resulted from as yet unknown mechanisms that mediate the biological transduction of physical stretch. Although alterations in alveolarization may impact airway function (17), Gie et al., [2020] could not attribute the benefit of CPAP superimposed on hyperoxia on alteration in alveolar structure.
CONCLUSIONS:
Our findings may have potential translational significance for the respiratory morbidity exhibited by former preterm infants (4, 5). There has been a marked increase in the use of various forms of non-invasive ventilation for preterm infants, although the ability of those devices to deliver CPAP is not readily quantifiable (18, 19). Many of these modes of CPAP delivery, including nasal cannulae, are administered for prolonged periods of time to support lung volume and upper airway patency at a time when supplemental oxygen is minimal or has been discontinued. It is possible that such prolonged CPAP delivery to an immature, but relatively normal lung, may be an antecedent to later airway hyperreactivity and COPD. This may be aggravated by sustained administration of high levels of CPAP. We recognize that data obtained in neonatal rodents may not translate to preterm human infants. Nonetheless, our findings support our hypothesis that combined CPAP and mild hyperoxic exposure attenuate the individual adverse effects of either CPAP or hyperoxia exposure alone.
Impact:
CPAP and mild hyperoxia exposure alone increase airway reactivity in the neonatal mouse model
In contrast, combined CPAP and hyperoxia no longer induce airway hyperreactivity
Combined CPAP and hyperoxia normalize smooth muscle and epithelial proliferation to control values
Interaction between CPAP-induced stretch and mild hyperoxia exposure on immature airways has important implications for airway pathophysiology in former preterm infants
Acknowledgements:
We would like to acknowledge the commitment from Morgan Hazard for assistance with CPAP exposure.
Funding: Funded by the National Heart, Lung and Blood Institute (Bethesda, MD) Grants R01HL138402, R01HL056470 and the Department of Pediatrics, Rainbow Babies and Children’s Hospital, Cleveland, Ohio. This study was also funded in part by generous financial contributions from William and Lois Briggs.
Footnotes
DECLARATIONS:
Ethics approval: All procedures were carried out in accordance with the National Institute of Health (NIH) guidelines for care and use of laboratory animals and were approved by the Animal Care and Use Committee at Case Western Reserve University.
Consent for publication: Not applicable.
Competing interests: Not applicable.
Availability of Data and Materials: The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Disclosure: The authors have no conflicts of interest to declare.
Patient Consent: not required.
Category: Basic Science
REFERENCES
- 1.Steinhorn R, et al. 2017Chronic Pulmonary Insufficiency of Prematurity: Developing Optimal Endpoints for Drug Development. J Pediatr 191:15–21.e11. [DOI] [PubMed] [Google Scholar]
- 2.Poindexter BB, et al. 2015Comparisons and Limitations of Current Definitions of Bronchopulmonary Dysplasia for the Prematurity and Respiratory Outcomes Program. Ann Am Thorac Soc 12:1822–1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schmölzer GM, et al. 2013Non-invasive versus invasive respiratory support in preterm infants at birth: systematic review and meta-analysis. Bmj 347:f5980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Doyle LW, et al. 2017Ventilation in Extremely Preterm Infants and Respiratory Function at 8 Years. N Engl J Med 377:329–337. [DOI] [PubMed] [Google Scholar]
- 5.Been JV, et al. 2014Preterm birth and childhood wheezing disorders: a systematic review and meta-analysis. PLoS Med 11:e1001596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harju M, et al. 2014The burden of childhood asthma and late preterm and early term births. J Pediatr 164:295–299.e291. [DOI] [PubMed] [Google Scholar]
- 7.Colin AA, McEvoy C, Castile RG 2010Respiratory morbidity and lung function in preterm infants of 32 to 36 weeks’ gestational age. Pediatrics 126:115–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mayer CA, Martin RJ, MacFarlane PM 2015Increased airway reactivity in a neonatal mouse model of continuous positive airway pressure. Pediatr Res 78:145–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reyburn B, et al. 2016The Effect of Continuous Positive Airway Pressure in a Mouse Model of Hyperoxic Neonatal Lung Injury. Neonatology 109:6–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Onugha H, et al. 2015Airway Hyperreactivity Is Delayed after Mild Neonatal Hyperoxic Exposure. Neonatology 108:65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang H, et al. 2014Severity of neonatal hyperoxia determines structural and functional changes in developing mouse airway. Am J Physiol Lung Cell Mol Physiol 307:L295–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Higgins RD, et al. 2018Bronchopulmonary Dysplasia: Executive Summary of a Workshop. J Pediatr 197:300–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Belik J, Jankov RP, Pan J, Tanswell AK 2003Chronic O2 exposure enhances vascular and airway smooth muscle contraction in the newborn but not adult rat. J Appl Physiol (1985) 94:2303–2312. [DOI] [PubMed] [Google Scholar]
- 14.Denis D, et al. 2001Prolonged moderate hyperoxia induces hyperresponsiveness and airway inflammation in newborn rats. Pediatr Res 50:515–519. [DOI] [PubMed] [Google Scholar]
- 15.O’Reilly MA, Marr SH, Yee M, McGrath-Morrow SA, Lawrence BP 2008Neonatal hyperoxia enhances the inflammatory response in adult mice infected with influenza A virus. Am J Respir Crit Care Med 177:1103–1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gie AG, et al. 2020Intermittent CPAP limits hyperoxia-induced lung damage in a rabbit model of bronchopulmonary dysplasia. Am J Physiol Lung Cell Mol Physiol 318:L976–l987. [DOI] [PubMed] [Google Scholar]
- 17.O’Reilly M, Harding R, Sozo F 2014Altered small airways in aged mice following neonatal exposure to hyperoxic gas. Neonatology 105:39–45. [DOI] [PubMed] [Google Scholar]
- 18.Claure N, Bancalari E 2015Non-invasive ventilation in premature infants. Arch Dis Child Fetal Neonatal Ed 100:F2–3. [DOI] [PubMed] [Google Scholar]
- 19.McEvoy CT, et al. 2014Bronchopulmonary dysplasia: NHLBI Workshop on the Primary Prevention of Chronic Lung Diseases. Ann Am Thorac Soc 11 Suppl 3:S146–153. [DOI] [PMC free article] [PubMed] [Google Scholar]