Abstract
Medical oxygen is the key to survival for COVID-19 patients. To meet the pandemic-driven oxygen demand spike, local hospitals began searching for a suitable medical oxygen delivery system. Among the studies published on the impact of COVID-19 on a range of aspects, including the global economy and the environment, no study has been conducted on the environmental impact of medical oxygen supply to hospitals under epidemic conditions.
In this paper the authors perform a comparative Life Cycle Assessment (LCA) to evaluate the environmental and economic impact of three scenarios (oxygen cylinders, liquid oxygen in tanks and on-site oxygen production) of local oxygen supply to hospitals in Poland. The LCA was performed according to ISO 14040 -14044 standards requirements, using the SimaPro 9.0 software. Results from the analysis showed that the Global Warming Potential (GWP) and Fine Particulate Matter Formation Potential (FPMFP) indicators for the liquid oxygen in tank scenario are the lowest and equal 265 kg CO2 eq and 0.309 kg PM2.5 eq. respectively. The greatest terrestrial acidification reductions (−1.38 kg SO2 eq) can be achieved when applying the on-site oxygen production scenario. Our findings revealed that the oxygen in cylinders scenario has the most harmful impact on the environment. The economic analysis was performed in order to compare the monthly and annual operational costs of analysed scenarios. The results show that hospitals sustain the lowest annual costs when using the on-site oxygen production scenario.
Keywords: COVID-19, Medical oxygen production, Pressure Swing Adsorption (PSA), LCA analysis, Economic analysis
Graphical abstract
1. Introduction
At the beginning of the COVID-19 outbreak, healthcare systems in many countries had to prepare for the challenges associated with this pandemic. They increased hospital capacity, e.g., built new ones (in China) or reorganized old ones into homogeneous infectious disease hospitals (in Poland), or provided more Intensive Care Units (ICUs), and more ventilators. Despite the fact that WHO recommendations for the management of COVID-19 treatment includes oxygen therapy for all severe and critical patients, this was not strongly emphasized at the beginning of the crisis (WHO, 2020a). Less attention has been paid to supplying medical oxygen, which is considered as a standard clinical tool widely available in hospitals (Stein et al., 2020). In many countries, to meet the oxygen-demand spike, governments and hospital managers are searching for the most appropriate solution under pandemic conditions. Thus, one of the aims of this analysis was to help in this decision-making process.
Among the studies published on the impact of COVID-19 on a range of aspects, including the global economy and the environment, no study has been conducted on the environmental impact of medical oxygen supply to hospitals under epidemic conditions (Shakil et al., 2020). The study presented in this paper aims to fill this gap in the literature. The LCA analysis (Table 1) performed to evaluate the environmental impact covers three basic scenarios (oxygen in cylinders, liquid oxygen in tanks, and on-site oxygen production). The selection of the impact categories assessed in this study is representative of the impact that is likely to be caused by an oxygen supply system. Among 18 categories in ReCiPe methodology, three environmental and two human impact categories were chosen. Additionally, to underline the damage to the environment resulting from medical oxygen supply to hospitals, the authors also decided to perform the LCA analysis based on the IMPACT 2002+ characterization. An economic analysis was also conducted to provide an estimation of the economic impact of oxygen distribution in all three cases. Two indicators, monthly and annual costs, were taken into consideration. Due to the prolonged period of the COVID-19 pandemic, the annual cost will be a more relevant expense for hospital managers.
Table 1.
List of the most important abbreviations used in the article.
| LCA | Life Cycle Assessment |
| GHG | Greenhouse Gas |
| ICUs | Intensive Care Units |
| MOP | Medical Oxygen Plant |
| DRDO | Defence Research and Development Organisation |
| PSA | Pressure Swing Adsorption |
| LOX | Liquid Oxygen |
| GWP | Global Warming Potential |
| FPMFP | Fine Particulate Matter Formation Potential |
| TAP | Terrestrial Acidification Potential |
| HCTP | Human Carcinogenic Toxicity Potential |
| HNCTP | Human Non-Carcinogenic Toxicity Potential |
| HHP | Human Health Potential |
| EQP | Ecosystem Quality Potential |
| CCP | Climate Change Potential |
| RP | Resources Potential |
| LCIA | Life Cycle Inventory Assessment |
| KPI | Key Point Indicators |
| DALY | Disability-Adjusted Life Years |
2. Medical oxygen demand versus COVID-19 patients
As the coronavirus (SARS-CoV-2) pandemic spreads, it endangers impoverished countries with fragile healthcare systems and soaring demands for medical oxygen. According to the data provided by the WHO Director-General, around 620,000 m3 of oxygen a day, which is about 88,000 large cylinders, will be required if the number of newly infected people remains at the current level of a million a week. In many countries, demand for medical oxygen is outstripping supply. Moreover, around 80% of the market is dependent on just a few companies such as, Air Liquide, Linde Group (including Praxair), or Nippon Gases (WHO Director-General, 2020).
The severe health crisis is affecting not only developing countries, but also high-income ones, such as France, Italy, Spain and the United States. It has highlighted the crucial importance of access to medical oxygen, e.g., a sudden increase in COVID-19 patients has resulted in a shortage of oxygen in one of the major hospitals in London (Campbell, 2020). In some parts of Italy, consumption of medical oxygen has tripled, forcing rapidly created new methods or improved old methods to ensure a sufficient supply of oxygen (Smith et al., 2020). Low-income countries, such as India or Peru have faced the need to use industrial oxygen for medical applications in cities which did not have a single liquid oxygen factory (Biswas, 2020). Another solution was developed in India by the Defence Research and Development Organisation (DRDO). Medical Oxygen Plant (MOP) technology, which utilizes a Pressure Swing Adsorption (PSA) technique, can be used to generate oxygen directly from ambient air. Such an oxygen-generating plant has been installed on the army site in India and has been successfully operating since 2017 (Siddiqui, 2020).
In South Asia, Latin America, and some parts of Africa, i.e., regions of the world where the epidemic is now spreading rapidly, many hospitals are suffering from shortages of medical oxygen, ventilators, tanks and other equipment, as well as a lack of training to support the correct and optimal use of oxygen therapy (Hinnant et al., 2020; McNeil Jr, 2020; Stein et al., 2020).
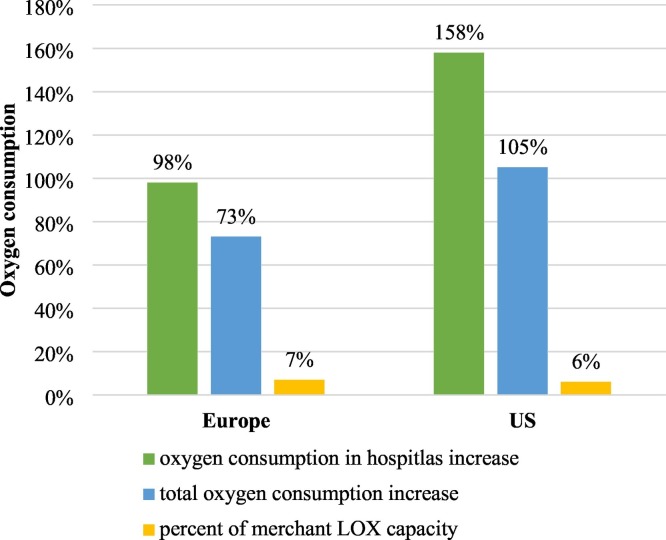
The analysis revealed that the demand for medical oxygen has increased by between three- and five-fold, both in liquid and cylinder form (Scott, 2020). Gasworld's Business Intelligence service also estimated the expected impact of COVID-19 cases on medical oxygen demand (see Fig. 1 ), which should be higher in the US than in Europe. It has been estimated that the oxygen production capacity (represented in Fig. 1 as merchant liquid oxygen (LOX) capacity) should be sufficient to meet the unprecedented increase in demand, especially when other industries are reducing production due to the lockdown (Raquet, 2020).
Fig. 1.
Oxygen consumption increase (Raquet, 2020).
In Poland, by 19 August 2020, over 58,000 cases and approximately 2000 deaths due to COVID-19 had been reported (“Coronavirus: information and recommendations,” 2020). Taking into account the impact of loosening COVID-19 restrictions, Orzechowska and Bednarek estimated that the basic reproductive number in Poland would range between 3.91 and 4.79 (Orzechowska and Bednarek, 2020). In addition, they predicted that by the end of September, the lowest number of new cases would be 263,900. Furthermore, it was calculated that the total number of new cases could exceed one million within the next year.
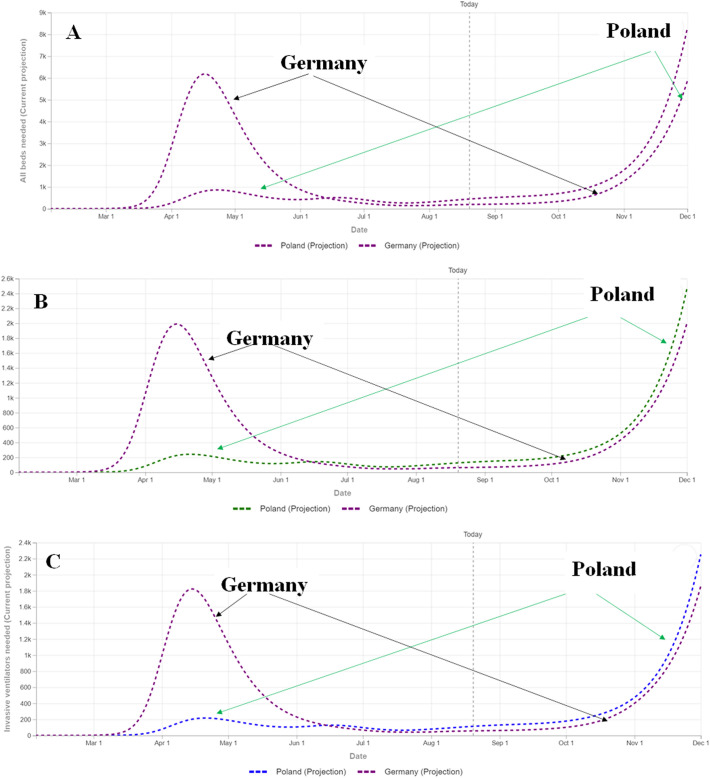
In the face of the pandemic, the availability of ICU beds and ventilators are important factors in preventing the spread of coronavirus (Karagiannidis et al., 2020). The authors of this article compared the number of hospitalized patients, occupied ICU beds, and the number of ventilators “in use” in Poland and Germany (see Fig. 2 ). As can be seen, the trend for all charts is similar. According to data from February to December 2020 (“COVID-19,” 2020) for both countries, the maximum numbers appeared during the lockdown. Poland, compared to its western neighbour, Germany, recorded a slower increasing trend from April to the end of the lockdown, and in the middle of June it exceeded Germany. By the end of the year, the number of hospitalized patients, ICU beds occupied and ventilators in use in Poland may be higher than those recorded for Germany during the first wave of coronavirus SARS-CoV-2 causing COVID-19 illness. It is worth mentioning that Poland, as well as Germany, always had a sufficient number of vacant ICU beds, as stated in their national register (“Coronavirus: information and recommendations,” 2020).
Fig. 2.
Comparison of hospital resources use during COVID-19 pandemic, A) the number of hospitalized patients, B) the number of ICU beds occupied, C) the number of ventilators in use (“COVID-19,” 2020).
3. Oxygen production
Medical oxygen accounts for approximately 15% of overall oxygen production (Raquet, 2020). In both industrial and medical applications, oxygen is separated from the air using cryogenic distillation or Pressure Swing Adsorption (PSA). The purity level of the oxygen produced is approximately 99 + % and 90 ± 5%, respectively. Medical grade oxygen for patients should be at least 82% (Ackley, 2019; WHO, 2020a).
Oxygen delivery for COVID-19 treatment healthcare facilities is a complex process involving a variety of technologies. In order to choose the most appropriate solution, it is important to consider many factors, such as the amount of oxygen needed at the healthcare facility (this may vary between different levels of the healthcare system, e.g., home, community care, county hospital, specialist hospital), overall cost, access to infrastructure and accessories, electricity and/or trained personnel, etc. (Smith et al., 2020). According to technical specifications and guidance for oxygen therapy devices from WHO and UNICEF, there are multiple sources and storage facilities available for supplying medical oxygen in healthcare facilities including cylinders, tanks, concentrators, and on-site PSA plants (WHO, 2020a).
3.1. Oxygen cylinders
Pressurized gas cylinders are widely regarded as the most common form of oxygen storage used in hospitals. The oxygen produced in a manufacturing plant, either via cryogenic distillation or a process known as PSA, is stored as compressed gas in a cylinder. Consequently, transportation to and from the manufacturing facility is required. Oxygen delivery to a patient via cylinders may be accomplished in one of two ways. A stand-alone storage vessel can be connected directly to a patient or installed in a piping system, or the patient can be connected to a manifold system of a group of cylinders. The cylinders, when filled, require neither a power source nor costly maintenance. However, periodic maintenance is required and is usually provided by gas suppliers during refilling. It should be noted that this cost is included in the cylinder rental and delivery charges. The use of oxygen cylinders may present the risk of a fall or rupture, caused by frequent transport between manufacturing facilities, warehouses, healthcare facility stores and ultimately to a patient's bed. In times of COVID-19 lockdown and soaring demand for medical oxygen in cylinders, there may be a greater risk of disruption as they require continuous refilling. Although only 15–20% of cylinders in use are certified for medical use, it is a difficult logistical issue to manage this number of cylinders, especially as oxygen demand becomes increasingly fragmented. Therefore, cylinders are most useful where the central refilling and transportation infrastructure is reliable and affordable (Smith et al., 2020; WHO, 2020a; WHO, 2019).
3.2. Liquid oxygen in bulk storage tanks
This solution requires a pipeline system connected to large bulk oxygen tanks and a vaporizer which converts the liquid oxygen into a gaseous state. The oxygen is supplied by self-vaporization, which means that a power supply is not required. The manufacturing process takes place in a cryogenic facility located outside the hospital and the liquid oxygen is periodically supplied by truck from the gas supplier to the healthcare facility's storage tank. The use of liquid oxygen tanks may be related to the risk of damage. Thus, maintenance of liquid oxygen tanks requires a great deal of technical knowledge, adequate ventilation, well-maintained piping and auxiliary equipment, as well as trained personnel. From a financial point of view, bearing in mind the cost of maintenance and rental, administrators of a hospital may decide to buy only one huge tank to supply the oxygen demand. This can be an attractive option if there are liquid oxygen facilities nearby and the liquid oxygen supplier takes care of the supply logistics. As in the case of cylinders, liquid oxygen supplies rely on uninterrupted transport from the facility to the hospital. This may be disrupted by a pandemic outbreak or geographical location (Smith et al., 2020; WHO, 2020a; WHO, 2019).
3.3. Oxygen concentrators
Oxygen concentrators obtain air from the environment and concentrate the oxygen, usually via the PSA technique. They require a constant supply of electricity and routine maintenance. When power supplies are inadequate or susceptible to voltage fluctuations, power stabilizers or an uninterruptible power supply may be needed. Once installed, they are not dependent on periodic re-supplies. These devices produce up to 95.5% concentrated oxygen and they can be used at any level of health facility to provide oxygen therapy (WHO, 2020b). However, the level of oxygen flow that they deliver (usually between 5 and 10 l·min−1) may be insufficient for critical COVID-19 patients requiring 30 l·min−1 (WHO, 2020a; WHO Director-General, 2020). In general, there are two types of commercial concentrators. The first one is stationary and is designed for hospitals or home use and is not easy to transport (weighing approximately 27 kg). The second one is a portable oxygen concentrator, which is smaller and lighter. It can be easily transported by an individual patient and even used when traveling by plane (Ackley, 2019).
3.4. On-site oxygen (PSA) plant
The oxygen from ambient air can be concentrated through PSA or Vacuum Swing Adsorption (VSA) techniques (the same technology as oxygen concentrators, but on a larger scale). For a PSA plant, the oxygen output typically ranges from 2 to 200 Nm3·hr−1 and varies depending on the estimated oxygen demand (WHO, 2015). Such an on-site PSA installation may be connected with an oxygen compressor in order to fill the oxygen cylinders for distribution within the same healthcare facility and other smaller healthcare facilities, or it may be piped directly from the oxygen tank to the wards. An on-site PSA plant requires a reliable source of electricity, greater capital investment and comes with considerable maintenance requirements. To prevent malfunctions, it is important to establish a strict maintenance schedule. If repairs are required, they should be performed as part of a contract by the manufacturer or the distributor's personnel. Moreover, specialist training is required for hospital personnel to operate and maintain all the necessary equipment and supplies. All medical PSA oxygen generator plants operate 24 h a day, seven days a week while they produce medical-grade oxygen. With the medical oxygen demand exploding due to the COVID-19 pandemic, the benefits of oxygen PSA facilities have proved to be more obvious than ever (Smith et al., 2020; WHO, 2020a; WHO, 2019). Once the hospital is equipped with the oxygen PSA installation, it becomes its own oxygen supplier, oxygen is produced on-site, on demand, from ambient air. Moreover, this solution avoids the countless transport journeys to bring medical oxygen to the hospital. Consequently, this reduces the negative impact on the environment by reducing air pollution.
4. Material and methods
4.1. Life cycle assessment
The authors used the gate-to-gate LCA approach to consider raw material acquisition, transport, infrastructure, operational material, and energy needed for the oxygen production. The gate-to-gate methodology was applied since the aim was not to compare the production technologies and their overall impact. Rather, the goal was to compare the economic and environmental impact of medical oxygen supply to hospitals during the COVID-19 pandemic. In order to perform the analysis, the authors used SimaPro 9.0 software. Therefore, the authors chose the gate-to-gate methodology, which made it possible to take into account the entire problem. The issue of medical oxygen availability in relation to its supply and demand, and the economic aspect. This analysis was intended to help the directors of medical facilities as well as managers, to facilitate the selection of the most favourable oxygen supply method for a given moment during the COVID-19 pandemic.
4.1.1. Goal and scope
The LCA has been prepared according to the principles of ISO 14040:2006 (“ISO - ISO 14040:2006 - Environmental management — Life cycle assessment — Principles and framework,” 2006) and ISO 14044:2006 (“ISO - ISO 14044:2006 - Environmental management — Life cycle assessment — Requirements and guidelines,” 2006). The goals of the performed LCA were as follows:
-
–
to provide an estimation of the environmental impact associated with oxygen distribution using three different scenarios,
-
–
to provide an estimation of the economic impact associated with oxygen distribution using three different scenarios,
-
–
to compare the scenarios under analysis with systems providing the same services, i.e., oxygen transportation from a gas supplier or oxygen production on site.
4.1.2. Impact assessment categories and relevant metrics
The selection of the impact categories assessed in this study is representative of the impact to be likely to be caused by an oxygen supply system, based on the ReCiPe characterization factors for mid-point potential impacts. To underline the damage to the environment resulting from medical oxygen supply to hospitals, the authors decided to perform the LCA analysis based on the IMPACT 2002+ characterization. Ozone Depletion Potential (ODP) has been omitted from the selected impact categories as this is not considered to be a significant issue since the introduction of the Montreal Protocol in 1987 which has drastically reduced both the consumption and emission of ozone depleting substances (UNEP, 2007).
Among 18 midpoint categories in ReCiPe methodology (Stavropoulos et al., 2016) the following environmental impact categories and Key Point Indicators (KPIs) are evaluated in the LCA:
-
I.Environmental impact categories:
-
a)Global Warming Potential (GWP),
-
b)Fine Particulate Matter Formation Potential (FPMFP),
-
c)Terrestrial Acidification Potential (TAP).
-
a)
-
II.Human impact categories:
-
a)Human Carcinogenic Toxicity Potential (HCTP),
-
b)Human Non-Carcinogenic Toxicity Potential (HNCTP).
-
a)
Among 14 available midpoint categories available in IMPACT 2002+ methodology (Jolliet et al., 2003) the authors have decided that in order to assess the damage, the following categories will also be analysed:
-
a)
Human Health Potential (HHP),
-
b)
Ecosystem Quality Potential (EQP),
-
c)
Climate Change Potential (CCP),
-
d)
Resources Potential (RP).
In order to calculate the uncertainty range of the result on the basis of the given uncertainty information, the SimaPro software used in this study enables a Monte Carlo analysis to be carried out (“Behind the Scenes at Monte Carlo Simulations - SimaPro,” 2015). The Monte Carlo method is a sampling-based method. All uncertainty data in the inventory is accounted for in SimaPro using different distributions. The result desired is then calculated by randomly drawing from the specified uncertainty distributions of the input variables. This calculation is repeated a given number of times to estimate the result's probability distribution. This distribution is typically used to inform decision-makers about certain characteristics, such as the mean value, the standard deviation or coefficient of variation and enable a better, clearer, and more conscious decision making (Heijungs, 2020). The authors decided to use the probability graph in this study.
4.1.3. Functional unit
The functional unit is a key element of LCA analysis which has to be clearly defined as it provides a reference to which the inputs and outputs can be related. The functional unit in this study is 64,800 m3 of oxygen distributed to a hospital per month of hospital functioning during COVID-19 lockdown. The authors of this article assumed that the number of patients was 100, of which 75 were severe and 25 were in a critical condition. The number of patients was set at 100 because, in the authors' opinion, this number would enable readers to easily and quickly convert the presented results into the number of patients. Data on the amount of oxygen required per 100 patients were adapted from the WHO report (WHO, 2020a). It was also presumed that the average oxygen flow rate for 100 patients was equal to 90 m3/h. The amount of medical oxygen needed was calculated based on the information obtained from one of the Polish hospitals, which indicated that:
-
–
patients on ventilators take about 12–15 breaths per minute, sucking 500–700 ml of the mixture (95% O2 and 5% ambient air) for inspiration,
-
–
patients undergoing oxygen therapy also take 12–15 breaths per minute, but in their case about 3–9 l of medical oxygen are consumed.
4.2. Scenario 1: oxygen cylinders
The first analysed scenario includes oxygen transportation in the 40 l cylinders from the local supplier. The distance was estimated to be 84.4 km. The authors assumed that the oxygen would be transported in a 16-ton truck with EURO 6 and 80% load factor (data according to the gas supplier). The oxygen cylinders would be stocked within the hospital territory. Next, the cylinders would be connected to the manifold of the central pipeline distribution system to transport the oxygen to the patients. In the LCA procedure, the authors did not consider the process of medical oxygen production, but assumed the transport of the “final product” from the gas supplier located in Poland.
4.3. Scenario 2: liquid oxygen in tank
The second scenario assumed that there was a liquid oxygen tank near to the hospital. The authors assumed that the oxygen would be transported by means of a truck with a tank. According to the gas supplier the maximum mass of liquid oxygen that could be transported in this scenario is 23,000 kg of medical oxygen. The estimate of the weight of the oxygen was based on Polish transport regulations, which state that the weight of the tanker with its load may not exceed 40,000 kg.
Based on the information gathered from hospitals, it was assumed that the oxygen tank would have a capacity of 10,000 l, and 9500 l of liquid oxygen would be the volume of liquid oxygen consumed. Additionally, it was presumed that the distance of oxygen transportation would be the same as in the first scenario (oxygen in cylinders). The authors took into account that after the transportation of the oxygen to the hospital territory, it would be pumped into the tank and then delivered to the patients through the central pipeline distribution system. Also, in this scenario, the authors did not consider the process of medical oxygen production for the LCA, but assumed the transport of the “final product” from the gas supplier located in Poland.
4.4. Scenario 3: on-site oxygen production
In the third scenario, the oxygen is produced via a PSA system and is directly transported to the hospital. It was assumed that the PSA plant would be connected to the manifold of the central pipeline distribution system, which distributes oxygen directly to the patients. For medical oxygen production it was assumed that low voltage electricity would be used. The authors estimated the electricity consumption at 1.10 kW·Nm−3 of the product (“OXYGEN GENERATORS - Oreco,” 2003; OXYMAT, 2018).
It was presumed that the PSA installation would consist of an air compressor with an air dryer and pre-filters with automatic drains, filter assembly, an oxygen generator unit, an oxygen analyser for medical application, and an oxygen tank (WHO, 2020b). For the purposes of this study, it was also assumed that the adsorbent in the oxygenation unit would not be replaced by a new one during the time considered. The mass of the adsorbent contributed to one of the largest shares of the mass of the entire PSA unit. The authors presumed that the average mass of the adsorbent would be equal to 2 tons. Later, on the basis of data obtained from the manufacturer of the PSA plant, the amount of adsorbent was confirmed.
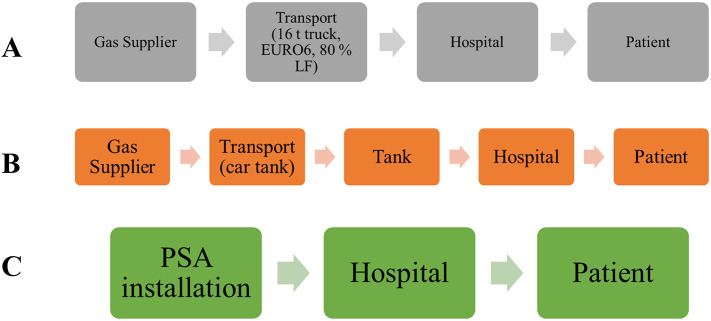
The schematic overview of the analysed scenarios is presented in Fig. 3 .
Fig. 3.
Schematic overview of the oxygen supply considered in the analysed scenarios A) Scenario I- oxygen in cylinders, B) Scenario II- liquid oxygen in tank, C) Scenario III- on-site production of oxygen.
4.5. Life cycle inventory
The required inventory data were acquired from a process simulation. Data regarding the distance of oxygen transportation, the vehicle used, and the fuel needed were obtained from the local hospital and the gas supplier in Poland. In Table 2 - the authors present the input and output data used for the calculation of the environmental impact. The inputs and outputs were introduced into SimaPro 9.0 software, which enabled the environmental impact of applying these scenarios in the oxygen supply system to be determined.
Table 2.
Summary of life cycle inventory of 64,800 m3 of medical oxygen distributed to a hospital per month.
| Inventory | Unit | Applied scenario | |
|---|---|---|---|
| Inputs | |||
| Feed air | 1,044,000 | Nm3/month | Scenario 3- on-site oxygen production |
| Electricity | 1100 | W/Nm3 | Scenario 3- on-site oxygen production |
| Diesel, truck | 35 | L/100 km | Scenario 1- oxygen in cylinders, Scenario 2- liquid oxygen in tank |
| Distance | 84.4 | km | Scenario 1- oxygen in cylinders, Scenario 2- liquid oxygen in tank |
| PSA facility | 1 | unit | Scenario 3- on-site oxygen production |
| Tank | 1 | unit | Scenario 2- liquid oxygen in tank |
| Cylinders | 338 | unit/day | Scenario 1- oxygen in cylinders |
| Output | |||
| Medical oxygen | 64,800 | Nm3/month | Scenario 1, Scenario 2, Scenario 3 |
5. Results
5.1. Characterization
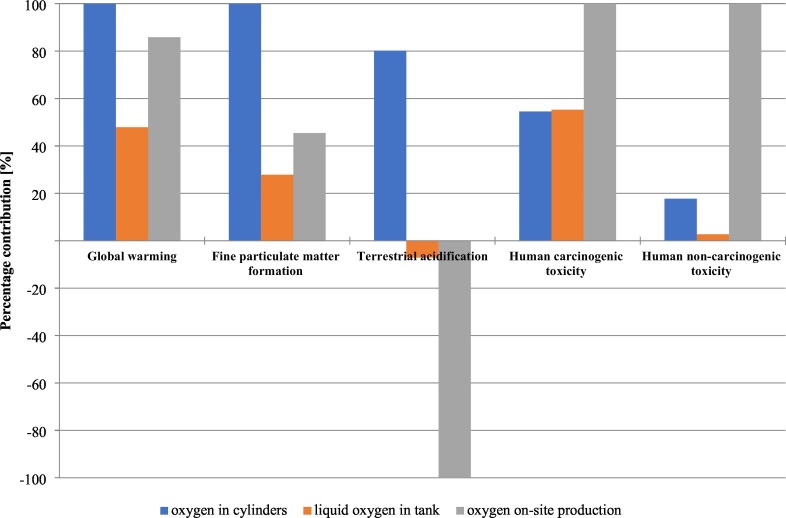
A selection of environmental impacts resulting from the 64,800 m3 of oxygen supply is given in Fig. 4 . Analysis was performed with the application of ReCiPe Midpoint Hierarchist methodology. The authors decided to choose these indicators, since, in their opinion, these indicators present the impact of the scenarios on the environment in the best way. The chosen indicators are:
-
a)
Global Warming Potential (GWP), which enables the CO2 emissions to be monitored, is calculated with the following formula:
| (1) |
where:
AGWPz, TH - the amount of radiative forcing integrated over time (for the Hierarchist option, it is a 100-year time horizon) caused by the emission of 1 kg of GHG,
AGWPCO2, TH - the amount of radiative forcing integrated over that same time horizon caused by the release of 1 kg of CO2.
-
b)
Fine Particulate Matter Formation Potential (FPMFP), which enables the PM2.5 emission to be monitored, is calculated with the following formula:
| (2) |
where:
iFx, i – the intake fraction of fine particulate matter due to emissions in region i per precursor x,
iFPM2.5, world – the emission-weighted world average of the intake fraction of fine particulate matter of PM2.5.
-
c)
Terrestrial Acidification Potential (TAP), which enables the SO2 emissions to be monitored, is calculated with the following formula:
| (4) |
where:
iFx, i – the fate fraction of acidification due to emissions in grid i per precursor x,
iFPM2.5, world – the emission-weighted world average of the fake fraction of acidification of SO2.
-
d)
Human Carcinogenic Toxicity Potential (HCTP), which enables the emission of carcinogens such as PAHS to be monitored. However, the unit which is given to this category is 1,4-DCB eq (eq states stands for equivalent).
-
e)
Human Non-Carcinogenic Toxicity Potential (HNCTP), which enables the emission of harmful elements such as Hg, As, and Cu to be monitored. The unit which is given for this indicator is the same as for HCTP, i.e., 1,4-DCB eq.
Fig. 4.
Comparison of the environmental impact of the analysed scenarios.
The human toxicological characterization factors at midpoint level for carcinogenic or non-carcinogenic effects of substances x to emission compartment i for cultural perspective c, through the ReCiPe method are calculated with the same formula as follow:
| (3) |
where:
iFi, x, r, g, cand iFDCB, ua, r, g, c – the human population intake fraction of substance x or chemical 1,4-dichlorobenzene (1,4-DCB) emitted to urban air, at geographical scale g via intake route r emitted to compartment i for cultural perspective c,
EFx, r, c/nc, c – the carcinogenic or non-carcinogenic effect factor of substance x or chemical 1,4-DCB for intake route r related to cultural perspective c.
A detailed description of the equations presented can be found in De Schryver et al. (2009), Goedkoop et al. (2013), Huijbregts et al., 2017a, Huijbregts et al., 2017b.
In order to compare of the obtained results with future publications, the authors presented results (Fig. 4 and Fig. 5 ) as percentage values. The X axis shows the percentage contribution, while the Y axis shows the results obtained for the analysed scenarios.
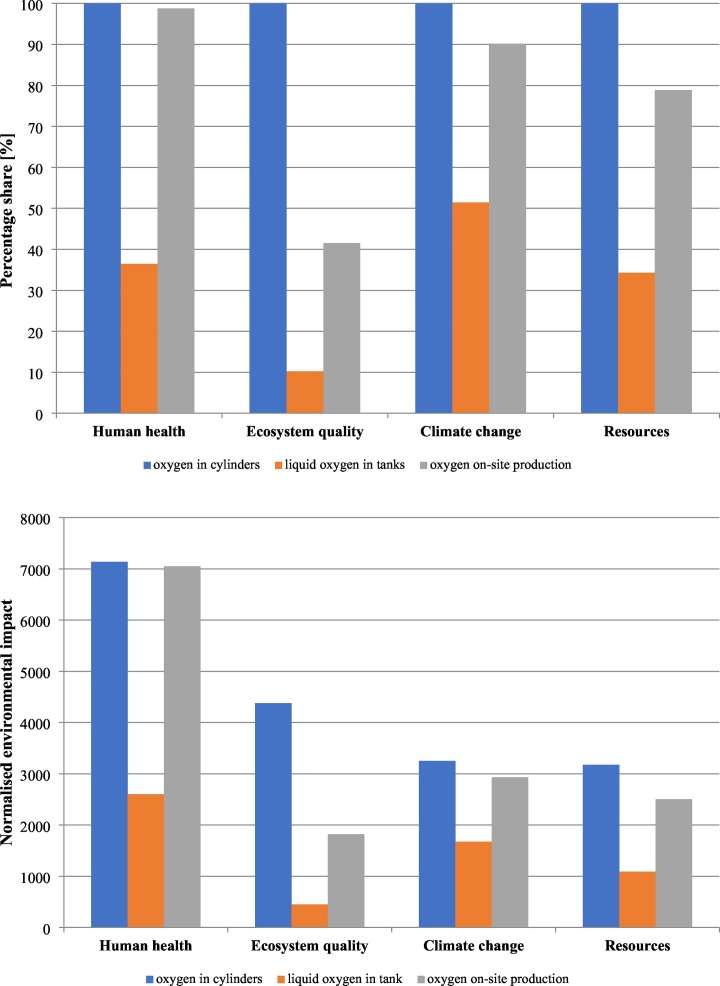
Fig. 5.
A) Damage assessment of analysed scenarios, B) normalized environmental impact of damage assessment of analysed scenarios.
In the LCA methodology, when carrying out the analysis, it should be remembered that when the obtained result is a negative value, it means that it has a positive impact on the environment. Such a situation is presented in Fig. 4, which means that Scenario 2 (liquid oxygen in tank) and Scenario 3 (on-site oxygen production) have a positive impact on the environment, as implementing the analysed scenario would lead to lowering the emission of monitored components included as this indicator. However, a greater positive effect was obtained for the oxygen on-site production scenario when analysing results for TAP.
The highest GWP was observed for the oxygen in the cylinders scenario, next was oxygen on-site production, while the lowest GWP was observed for the liquid oxygen in tank scenario. It is worth mentioning that both the oxygen in cylinders scenario and the liquid oxygen in tank scenario do not include the process of oxygen production. Despite this, the oxygen in cylinders scenario has the greatest impact on GWP. The biggest impact of the oxygen in cylinders scenario was also estimated for FPMFP and TAP. The oxygen on-site scenario had the greatest impact on both HCTP and HNCTP. The values were the highest among all analysed scenarios, however the authors believe that if the production of oxygen in the oxygen in cylinders scenario and the liquid oxygen in tank scenario was considered (this phase has to be omitted as the assumptions related to the gate-to-gate methodology does not include the medical oxygen production phase at the suppliers), then the obtained results would be very different, i.e., the results for oxygen on-site production would have a lower impact than the other scenarios. Comparing the results obtained in the HNCTP for the oxygen in cylinders scenario and the liquid oxygen in tank scenario, a higher impact was calculated for the oxygen in cylinders scenario. While the calculated values in HCTP for those scenarios were comparable, a slightly higher impact was calculated for the liquid oxygen in tank scenario.
According to the calculations, it seemed that by applying the on-site oxygen production, the number of medical oxygen deliveries would automatically reduce the number of trucks (fuelled with diesel) used for transport. For a 64,800 m3 supply of medical oxygen, we need 338 units of 40 l cylinders per day, which means we need four 16-ton trucks to transport 338 cylinders per day. This means that in order to deliver sufficient oxygen per 100 patients, we would need 120 trucks per month, which is equal to a total of approximately 7050 l of diesel. Thus, instead of a negative environmental impact caused by the use of 16-ton trucks, implementing a PSA plant would positively affect the environment.
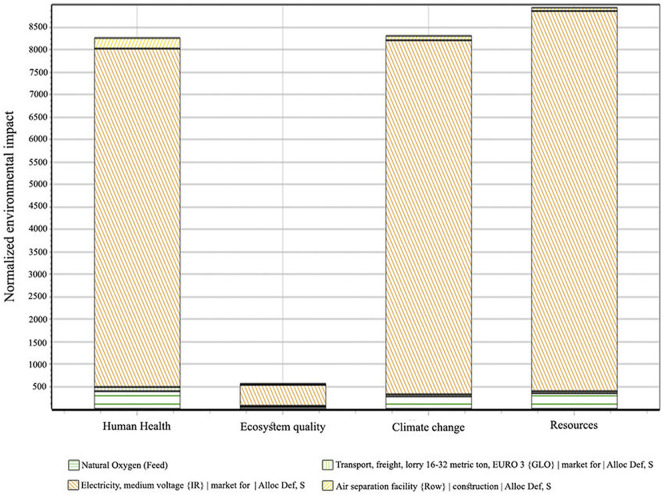
5.2. Damage assessment
In order to compare the damage assessment of the analysed scenarios, IMPACT 2002 + methodology was applied. Fig. 5 A presents the damage assessment results of analysed scenarios, while Fig. 5 B shows the normalized values of impact categories. The authors compared impact categories such as: Human Health Potential (HHP), Ecosystem Quality Potential (EQP), Climate Change Potential (CCP) and Resources Potential (RP).
The authors chose IMPACT 2002 + damage assessment (Jolliet et al., 2003) methodology in order to determine the impact of implementing the analysed scenarios. The chosen indicators are:
-
a)
HHP presents the results with the unit DALY (Disability-Adjusted Life Years). This indicator takes into account the years lost due to premature death and expresses the reduced quality of life due to illness in years as well as resulting from implementing the analysed scenario.
-
b)
EQP presents the results with the unit PDF·m2·yr, (PDF refers to Potentially Disappeared Fraction of species). This indicator accounts for a fraction of species richness that may be potentially lost due to an environmental mechanism.
-
c)
CCP presents the results with the unit kg CO2 eq. This indicator is based on the total gaseous emissions released in Europe per year multiplied with the global warming potentials for a 500-year horizon.
-
d)
and RP presents the results with the unit MJ primary. This indicator is calculated including the total non-renewable energy consumption, including nuclear energy consumption.
The highest values for all analysed impact categories were obtained for the oxygen in cylinders scenario, while the lowest values were for the liquid oxygen in tank scenario. The impact of oxygen on-site scenario production was the second dominant in all analysed categories. However, the authors believe that if the production of oxygen in the oxygen in cylinders scenario and the liquid oxygen in tank scenario was considered, then the obtained results would be completely different. The results for oxygen on-site production would have a lower impact than the other scenarios.
5.3. Monte Carlo uncertainty results
In this part of the study, the results of Monte Carlo uncertainty analysis are presented. A Monte Carlo simulation enables the uncertainty to be calculated. All uncertainty distributions that are defined in the flows, parameters and characterization factors are considered for the simulation.
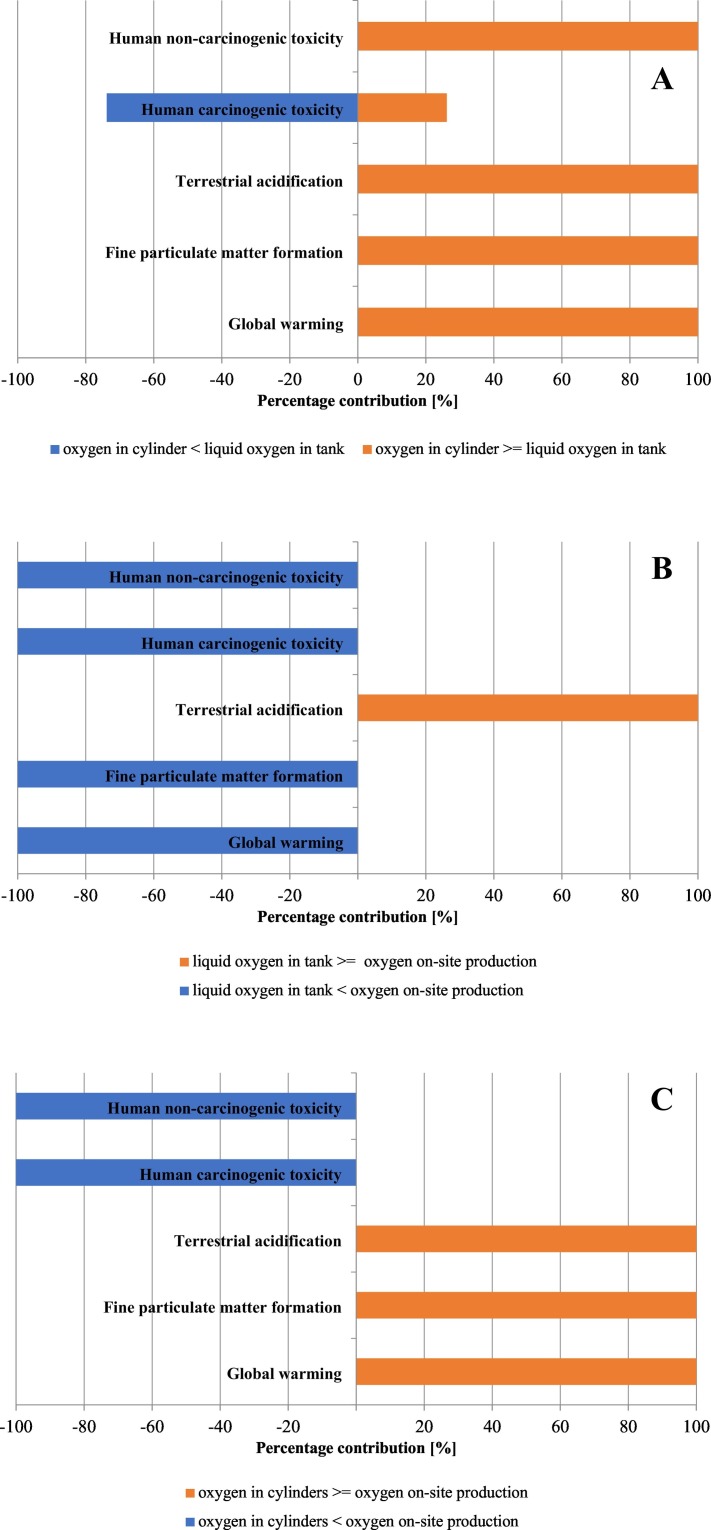
The simulation results are presented in the form of a table. The SimaPro counts the number of comparison runs in which product A is larger than (or equal to) product B. Fig. 6 A shows the Monte Carlo simulation results of characterized LCIA comparison between 64,800 m3 of oxygen in cylinders and 64,800 m3 of liquid oxygen in tank. The chart shows that the authors have 100% certainty that for the oxygen in cylinders scenario in HNCTP, TAP, FPMFP and GWP, results are better than for liquid oxygen in tanks. Only the value obtained for HCTP shows that the oxygen in cylinders scenario has approximately 25% better results.
Fig. 6.
Monte Carlo uncertainty analysis A) of oxygen in cylinders scenario and liquid oxygen in tank scenario, B) of liquid oxygen in tank scenario and oxygen on-site production scenario, C) of oxygen in cylinders scenario and oxygen on-site production scenario.
Fig. 6B shows the Monte Carlo simulation results of characterized LCIA comparison between 64,800 m3 of liquid oxygen in tank and 64,800 m3 of oxygen on-site production. The chart shows that only for TAP calculated for liquid oxygen in tank are the values better than those obtained for the oxygen on-site production scenario. For the other analysed impact categories (HNCTP, HCTP, FPMFP and GWP) the Monte Carlo simulation results show that the liquid oxygen in tank scenario produced better results.
Fig. 6C shows the Monte Carlo simulation results of characterized LCIA comparison between 64,800 m3 of oxygen in cylinders and 64,800 m3 of oxygen on-site production. The chart shows that in TAP, FPMFP and GWP calculated for oxygen in cylinders; this scenario outperforms the oxygen on-site production scenario. For the other analysed impact categories (HNCTP, HCTP) the oxygen in cylinders scenario outperforms the oxygen on-site production scenario.
Additionally, the authors present the uncertainty parameters calculated for analysed scenarios. The characteristic uncertainty parameters i.e., mean, median, standard deviation (SD), and coefficient of variation (CV), were computed to visualize and describe the LCA results and to compare simulation outputs for different scenarios and use that information for decision support. Based on the coefficient of variation, defined as the ratio of the standard deviation of a probability distribution to its mean, in Table 3 . it is observed that uncertainty in scenario 1 is much higher when compared to scenario 2, as indicated by the CV and the standard derivation for all of the indicators. Moreover, by comparing the median to the mean for all indicators, the differences between them are not significant, which indicated that the datasets are evenly distributed. The values presented in Table 3 are given for the 1 Nm3 of medical oxygen.
Table 3.
Characteristic uncertainty parameters obtained for analysed Scenarios (per 1 Nm3).
| Scenario | Mean | Median | SD | CV[%] |
|---|---|---|---|---|
| Scenario 1 | ||||
| GWP [kg CO2] | 555 | 555 | 13.7 | 2.47 |
| TAP [kg SO2] | 1.11 | 1.11 | 0.027 | 2.47 |
| FPMFP [kg PM2.5] | 1.11 | 1.11 | 0.027 | 2.47 |
| HCTP [kg 1,4-DCB] | 42.8 | 42.7 | 1.05 | 2.47 |
| HNCTP [kg 1,4-DCB] | 535 | 535 | 13.2 | 2.47 |
| Scenario 2 | ||||
| GWP [kg CO2] | 265 | 265 | 0.0035 | 0.001 |
| TAP [kg SO2] | −0.098 | −0.098 | 1.59E-5 | −0.0162 |
| FPMFP [kg PM2.5] | 0.31 | 0.31 | 1.01E-5 | 0.0033 |
| HCTP [kg 1,4-DCB] | 43.3 | 43.3 | 0.00012 | 0.00027 |
| HNCTP [kg 1,4-DCB] | 81.7 | 81.7 | 0.0030 | 0.0037 |
| Scenario 3 | ||||
| GWP [kg CO2] | 476 | 474 | 8.81 | 1.85 |
| TAP [kg SO2] | −1.38 | −1.38 | 0.0184 | −1.33 |
| FPMFP [kg PM2.5] | 0.504 | 0.502 | 0.018 | 3.55 |
| HCTP [kg 1,4-DCB] | 78.3 | 78.2 | 0.77 | 0.99 |
| HNCTP [kg 1,4-DCB] | 3.01E3 | 3.01E3 | 17.1 | 0.57 |
6. Economic analysis
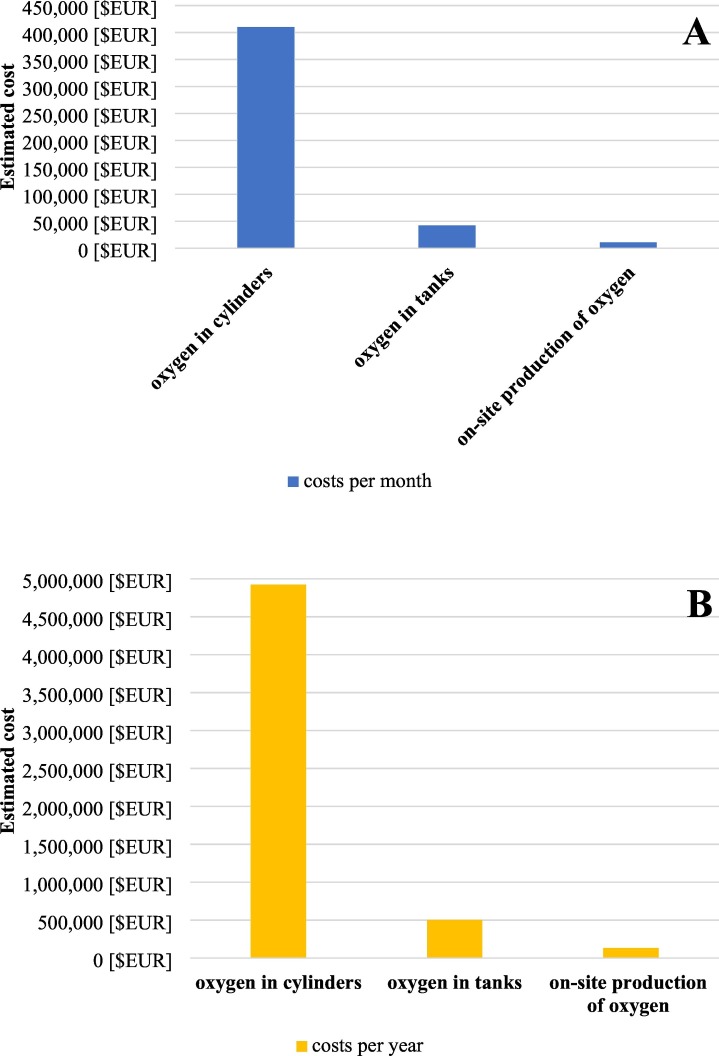
The second part of the study was to compare the operational costs of analysed scenarios. The authors estimated the costs, which are shown in Fig. 7 A and Fig. 7 B on the basis of the data available on the website of the gas supplier (Linde Healthcare, 2020) and PSA manufacturers. To confirm prices for medical oxygen, both liquid and gaseous, as well as the costs of transport and leasing of the cylinders, we conducted a survey among Polish hospitals which reorganized themselves into homogeneous infectious disease hospitals during the first wave of the COVID-19 pandemic. As neither of the surveyed hospitals has used a PSA plant, the price of such an installation has been established with the manufacturer so that it meets all the assumptions made in the article. All prices presented in Table 4 exclude VAT.
Fig. 7.
Comparison of the estimated A) monthly costs of the analysed scenarios, B) annual costs of the analysed scenarios.
Table 4.
Input data using in the economic analysis.
| Value | Unit | Applied scenario | |
|---|---|---|---|
| Oxygen purchase price | |||
| PSA installation | 140,000 | € | Scenario 3- on-site oxygen production |
| Liquid oxygen installation | 85,043.30 | € | Scenario 2- liquid oxygen in tank |
| Liquid oxygen and delivery | 0.49 | €/kg | Scenario 2- liquid oxygen in tank |
| Oxygen in 40 l cylinders and delivery | 39.80 | €/piece | Scenario 1- oxygen in cylinders |
| Cylinder lease | 0.47 | €/day | Scenario 1- oxygen in cylinders |
| Electricity | |||
| Consumption | 1.10 | kWh/Nm3 | Scenario 3- on-site oxygen production |
| Price | 0.14 | €/kWh | Scenario 3- on-site oxygen production |
When calculating the oxygen in cylinders scenario, the cost of transporting oxygen (including the cost of producing oxygen) and the cost of leasing the cylinders were considered. According to the information from the hospitals surveyed and on the website of the gas supplier these prices are 39.80 €/piece (as mentioned in paragraph 4.2, the authors assumed that all cylinders hold 40 l, i.e., 6.4 cubic meters of oxygen) and 0.47 €/day for the leasing of one single cylinder, respectively (Linde Healthcare, 2020). It was assumed that only 500 cylinders are leased at any given time and the gas supplier bears all costs connected with cylinder maintenance and repairs by a lease agreement.
For the purpose of the liquid oxygen in tank calculation, the estimated amount of oxygen necessary for functioning was based on WHO guidelines (WHO, 2020a, WHO, 2020b). This was multiplied by the cost of transporting oxygen (including the cost of production and replenishment of the tank). According to the website of the gas supplier this price equals 0.45 €/kg for 1 kg of liquid oxygen. It was assumed that regardless of the delivery distance, the price is fixed (Linde Healthcare, 2020). As the tank was owned by the hospital, the costs also included the liquid oxygen installation purchase costs which included costs of tank, vaporizer, transport, and installation charges. The maintenance of the equipment is by an annual maintenance contract, with the cost of spares being borne by the hospital. These were assumed to be 5% of the monthly cost of supplying liquid oxygen.
The costs calculated for the oxygen on-site production scenario included the purchase cost of the PSA plant and the cost of the electricity needed to produce medical oxygen. Based on the manufacturer's evaluation and information provided, it was assumed that the cost of installing PSA included installation fees and equipment maintenance costs, as well as the cost of spare parts were borne by the manufacturer in the first year of the operation under an annual service and warranty contract. The cost of electricity was calculated for the average cost of 1 kWh for the hospitals in Poland. In addition, the authors would like to point out that the cost of purchasing the installation was included in two scenarios, in the estimation of monthly and annual costs.
Moreover, employee remunerations were not taken into account for any of the scenarios, as there was neither an increase nor a decrease in the number of the employees (hospitals have already recruited employees and their remunerations were already included into hospital's expenses) regardless of the scenario adopted. For scenario 2-liquid oxygen in tank and scenario 3-on-site oxygen production, we assumed a 10% depreciation rate per year assuming that the effective life span of the installation is 10 years. Depreciation was calculated by the straight-line method (Mivechian and Pakizeh, 2013; Somu, 2009).
All costs are given in euros and have been estimated based on the average monthly exchange rate for the month of July 2020. Table 5 shows the monthly cost of each scenario.
Table 5.
The monthly cost of each scenario.
| Scenario 1- oxygen in cylinders | Scenario 2- liquid oxygen in tank | Scenario 3- on-site oxygen production | |
|---|---|---|---|
| Fixed assets (€): | |||
| Cost of the installation | – | 85,043.30 | 140,000.00 |
| Operating costs (€/month): | |||
| Cost of oxygen (including delivery charge) |
403,260.28 | 39,350.25 | – |
| Leasing of 500 cylinders | 7,077.58 | – | – |
| Spares and maintenance charges | – | 1,967.51 | – |
| Electricity consumption | – | – | 9,881.60 |
| Economics (€/month): | |||
| Fixed assets | – | 708.69 | 1,166.67 |
| Operating costs | 410,337.86 | 41,317.76 | 9,881.60 |
| Total: | 410,337.86 | 42,026.46 | 11,048.26 |
Table 5 and Fig. 7 A show the monthly costs of the compared scenarios for 64,800 m3 of oxygen supply to the hospital. The highest costs were calculated for the oxygen in cylinders scenario. When comparing the liquid oxygen in tank and oxygen on-site production scenarios, the calculated costs were lower for the on-site production scenario. Fig. 7 B shows the annual costs of compared scenarios for 64,800 m3/month of oxygen supply to the hospital. The highest costs were calculated for the oxygen in cylinders scenario (nearly 5,000,000 €). The costs calculated for liquid oxygen in tank scenario were accounted for only around 10% of the oxygen in cylinders scenario. While the costs estimated for oxygen on-site production scenarios were almost at a minimal level, when compared to the previously mentioned scenarios. The estimated cost for the oxygen on-site production scenario was approximately 133,000 €.
7. Discussion
7.1. Environmental impact
This paragraph is devoted to comparing the environmental impact of the analysed hospital oxygen supply scenarios. According to the data presented in this paper, the authors concluded that the highest environmental impact relates to the oxygen in cylinders scenario, which contributed the most to GWP, FPMFP and TAP (see Fig. 4). From the environmental point of view, without taking into consideration the process of oxygen production, the best solution for oxygen production would be the liquid oxygen in tank scenario. However, the authors believe that if one takes into consideration the oxygen production, then the lowest environmental impact would be calculated for the on-site oxygen production scenario.
The authors wanted to compare the results with other papers, but only one study has been published in this area of interest (Shourkaei et al., 2018). Shourkaei et al. analysed the environmental impact of cryogenic oxygen production using SimaPro software. According to this study the highest environmental impact connected with cryogenic oxygen production relates to air separation facility construction, which contributed to approximately 90% of the selected impact categories. Shourkaei et al. calculated the normalized environmental potential impact of cryogenic oxygen production, which is presented in Fig. 8 . According to Shourkaei et al. the normalized values of the Human Health impact was estimated at 8250 mPt, Ecosystems Quality was estimated at 600 mPt, Climate Change was estimated at 8350 mPt, and Resources was estimated at 9000 mPt for 8.1 tons of cryogenic oxygen production.
Fig. 8.
Normalized diagram of cryogenic oxygen production with IMPACT 2002+ according to Shourkaei et al., 2018
The normalized values of damage assessment calculated in this study (shown in Fig. 5 B) were estimated at: 7050 mPt for Human Health, 1817 mPt for Ecosystem Quality, 2932 mPt for Climate Change and 2501 mPt for Resources. The results obtained by Shourkaei et al. were significantly higher for two out of four aspects examined for the much lower amount of oxygen produced. This situation is puzzling, considering that in our study we calculated the effect for 64,000 m3 of oxygen, while Shourkaei et al. studied the effect of producing 8.1 tons of oxygen. The results obtained by Shourkaei et al. should be multiplied by approximately 9025 to show the damage assessment calculated in this study. This would result in enormous numbers, therefore the authors have not undertaken a comparison of these two studies.
7.2. Economic analysis
This paragraph is devoted to the comparison of the calculations made during the economic analysis. In the on-site oxygen production scenario for electricity costs, the authors used the cost stated on the electricity supplier's website as the hospital electricity supply rate. Regarding the costs included in the cylinder oxygen scenario, the cost of transporting oxygen (including the cost of producing oxygen) and the cost of leasing the cylinder were considered. The authors collected all the necessary information from the gas supplier to analyse the cost of the oxygen in cylinders and the liquid oxygen in tank scenarios, as well as the estimated cost of the PSA installation from the manufacturer for the cost analysis of the on-site oxygen production scenario. Therefore, the authors can guarantee with 100% certainty that the calculated costs are actual and not estimated. All costs are given in euros and have been estimated based on the average monthly exchange rate for the month of July 2020.
When comparing the calculated costs, the authors noted that the greatest financial burden was related to the oxygen in cylinders scenario, which would cost approximately 400,000 € per month. On the other hand, using the other two scenarios, hospitals would be able to cut their oxygen supply costs by more than half, as evidenced by the economic data on a monthly basis for both the liquid oxygen in tank and on-site oxygen production scenarios. Monthly on-site oxygen production costs were 67% lower than in the oxygen in cylinders scenario. While for the liquid oxygen in tank scenario, the estimated monthly costs were 89% lower than in the oxygen in cylinders scenario.
If, on the other hand, the increased demand for oxygen lasted longer, the savings resulting from installing the PSA unit at the hospital (on-site oxygen production scenario) would be as much as 96% compared to the oxygen in cylinders scenario on an annual basis. Applying the liquid oxygen in tank scenario would allow for annual savings of 53% compared to the oxygen in cylinders scenario.
Nevertheless, while writing this article, the authors did not find a single publication that would allow a comparison of the calculated costs. Therefore, a number of measures were taken to limit possible errors and ensure the highest possible reliability of the published results.
8. Conclusions
This work presents the results of the Life Cycle Assessment analysis of the three basic scenarios of medical oxygen supply to hospitals in Poland in accordance with the ISO standards. This LCA shows the environmental impact per 64,800 m3/month of oxygen produced by the three analysed scenarios. This article was prepared with the intention of helping hospital directors and managers to make decisions about medical oxygen supply in COVID-19 pandemic conditions.
-
A.
The lowest environmental impact was observed for the liquid oxygen in tank scenario.
-
B.
The highest environmental impact results were observed for the oxygen in cylinders scenario.
-
C.
A positive effect for TAP was observed for both the liquid oxygen in tank scenario and on-site oxygen production. However, the greater TAP effect was calculated for the on-site oxygen production scenario.
-
D.
The biggest impact on human health, via carcinogenic and non-carcinogenic toxicity was calculated for on-site oxygen production. Nevertheless, the authors believe that when the oxygen production is taken into consideration in the calculations for the oxygen in cylinders and the liquid oxygen in tank scenarios, the values indicate a significant benefit of on-site oxygen production.
Another part of this study was economic analysis of the three scenarios.
-
A.
When comparing the calculated costs (see Fig. 7), the authors noted that the greatest financial burden was related to the cylinder oxygen scenario, which was billed at approximately 400,000 € per month.
-
B.
By using the liquid oxygen tank scenario, hospitals can reduce costs by 89.76% per month.
-
C.
However, the greatest reduction in monthly costs can be achieved by using the on-site oxygen production scenario, where hospitals can reduce oxygen costs by 97.31%.
-
D.
The same relationships was observed when the increased demand for oxygen lasted longer, the savings resulting from installing the PSA unit at the hospital would be as much as 97.31% compared to the oxygen in cylinders scenario on an annual basis. Applying the liquid oxygen in tank scenario would allow for annual savings of 89.76% compared to the oxygen in cylinders scenario.
-
E.
Moreover, the scenario 3 avoids the countless truck journeys bringing medical oxygen to the hospital, consequently reducing the negative impact on the environment and air pollution. This results from the fact that all medical PSA oxygen generator plants operate 24 h a day, seven days a week while they produce medical-grade oxygen.
The on-site oxygen production scenario would enable hospitals to save a significant amount of money. In the anticipated situation, i.e., another wave of COVID-19 cases, the analysed solutions would improve the situation of hospitals in terms of independence from gas suppliers. This would mean that the hospital is no longer concerned about oxygen deficiency as it has constant access to it. The on-site oxygen production scenario allows a healthcare facility to become its own oxygen supplier. The oxygen is produced on site and on demand from the ambient air from the moment that the hospital is equipped with the oxygen PSA plant. Despite the high initial cost of installing the plant, the authors found more benefits of this solution.
This study is the first of its kind. The analysis may constitute the basis for further studies in other parts of the world, depending on the degree of economic development, geographical and urban conditions, and other local conditions (electricity, fuel, working time). A similar analysis, which will complement the data presented in this paper, could be carried out for other countries or regions of residence.
The authors of this article are aware that the economic and LCA analysis is not the only aspect on which hospital directors and managers make decisions about medical oxygen supply. Moreover, the scenarios presented here are not the only ones available. It is also possible to apply scenarios in which the use of individual sources are mixed, e.g., combining oxygen supply in cylinders with the production of medical oxygen in the PSA installation or liquid oxygen supply to the tank and oxygen production in the PSA installation. This provides an opportunity for further research.
CRediT authorship contribution statement
Mieczysław Bałys: Conceptualization, Software, Project administration, Writing – review & editing. Ewelina Brodawka: Data curation, Writing – original draft, Validation. Anna Korzeniewska: Data curation, Writing – original draft, Validation. Jakub Szczurowski: Methodology, Software, Writing – review & editing, Validation. Katarzyna Zarębska: Conceptualization, Methodology, Supervision, Project administration, Funding acquisition.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors gratefully acknowledge financial support from the “Initiative of Excellence – Research University - IDUB, Activity no. 4” programme of AGH University of Science and Technology in Krakow, Poland.
Editor: Deyi Hou
References
- Ackley M.W. Springer US; 2019. Medical Oxygen Concentrators: A Review of Progress in Air Separation Technology, Adsorption. [DOI] [Google Scholar]
- Behind the Scenes at Monte Carlo Simulations - SimaPro [WWW Document], 2015. URL https://simapro.com/2015/behind-the-scenes-at-monte-carlo-simulations/ (accessed 12.7.20).
- Biswas S. BBC News; 2020. The Struggle to Keep India’s Covid-19 Patients Breathing. [Google Scholar]
- Campbell D. Guard; 2020. Coronavirus: London Hospital Almost Runs out of Oxygen for Covid-19 Patients. [Google Scholar]
- Coronavirus: information and recommendations [WWW Document], 2020. Counc. Minist. Repub. Pol. URL https://www.gov.pl/web/coronavirus (accessed 8.20.20).
- COVID-19 [WWW Document], 2020. Inst. Heal. Metrics Eval. URL http://covid19.healthdata.org/poland?view=total-deaths&tab=trend (accessed 8.20.20).
- De Schryver A.M., Brakkee K.W., Goedkoop M.J., Huijbregts M.A.J. Characterization factors for global warming in life cycle assessment based on damages to humans and ecosystems. Environ. Sci. Technol. 2009;43:1689–1695. doi: 10.1021/es800456m. [DOI] [PubMed] [Google Scholar]
- Goedkoop M., Heijungs R., Huijbregts M., Schryver A. De, Struijs J., van Zelm R. First edition (version 1.08). Report I: Characterisation. 2013. ReCiPe 2008: a life cycle impact assessment method which comprises harmonised category indicators at the midpoint and the endpoint level. [Google Scholar]
- Heijungs R. On the number of Monte Carlo runs in comparative probabilistic LCA. Int. J. Life Cycle Assess. 2020;25:394–402. doi: 10.1007/s11367-019-01698-4. [DOI] [Google Scholar]
- Hinnant L., Petesch C., Diallo B. Glob. News; 2020. Coronavirus: Short Supply of Medical Oxygen Worldwide Leaves Many Gasping for Air. [Google Scholar]
- Huijbregts M.A.J., Steinmann Z.J.N., Elshout P.M.F., Stam G., Verones F., Vieira M., Zijp M., Hollander A., van Zelm R. ReCiPe2016: a harmonised life cycle impact assessment method at midpoint and endpoint level. Int. J. Life Cycle Assess. 2017;22:138–147. doi: 10.1007/s11367-016-1246-y. [DOI] [Google Scholar]
- Huijbregts M.A.J., Steinmann Z.J.N., Elshout P.M.F., Stam G., Verones F., Vieira M.D.M., Hollander A., Zijp M., van Zelm R. Report I: Characterization, RIVM Report 2016-0104. 2017. ReCiPe 2016 v1.1: a harmonized life cycle impact assessment method at midpoint and endpoint level. [Google Scholar]
- ISO - ISO 14040:2006 - Environmental management — Life cycle assessment — Principles and framework [WWW Document], 2006. URL https://www.iso.org/standard/37456.html (accessed 8.17.20).
- ISO - ISO 14044:2006 - Environmental management — Life cycle assessment — Requirements and guidelines [WWW Document], 2006. URL https://www.iso.org/standard/38498.html (accessed 12.7.20).
- Jolliet O., Margni M., Charles R., Humbert S., Payet J., Rebitzer G., Rosenbaum R. IMPACT 2002+: a new life cycle impact assessment methodology. Int. J. Life Cycle Assess. 2003;8:324–330. doi: 10.5479/si.00963801.32-1531.411. [DOI] [Google Scholar]
- Karagiannidis, C., Mostert, C., Hentschker, C., Voshaar, T., Malzahn, J., Schillinger, G., Klauber, J., Janssens, U., Marx, G., Weber-Carstens, S., Kluge, S., Pfeifer, M., Grabenhenrich, L., Welte, T., Busse, R., 2020. Case characteristics, resource use, and outcomes of 10 021 patients with COVID-19 admitted to 920 German hospitals: an observational study. Lancet Respir. Med. 2600, 1–10. doi: 10.1016/S2213-2600(20)30316-7. [DOI] [PMC free article] [PubMed]
- Linde Healthcare, 2020.
- McNeil, D.G. Jr., 2020. A Simple Way to Save Lives as Covid-19 Hits Poorer Nations. New York Times.
- Mivechian A., Pakizeh M. Hydrogen recovery from Tehran refinery off-gas using pressure swing adsorption, gas absorption and membrane separation technologies: simulation and economic evaluation. Korean J. Chem. Eng. 2013;30:937–948. doi: 10.1007/s11814-012-0221-y. [DOI] [Google Scholar]
- Orzechowska M., Bednarek A.K. Forecasting COVID-19 pandemic in Poland accor ding to gover nment r egulations and people behavior. Frontiers (Boulder) 2020 doi: 10.1101/2020.05.26.20112458. [DOI] [Google Scholar]
- OXYGEN GENERATORS - Oreco [WWW Document], 2003. URL https://www.oreco.com/products/oxygen-generators/?gclid=EAIaIQobChMInL6vguXx6gIVkqkYCh2EhQlbEAAYBCAAEgL4HPD_BwE (accessed 12.8.20).
- OXYMAT, 2018. Oxygen & Nitrogen On-site Solutions.
- Raquet J. Gasworld; 2020. Covid-19 Versus Oxygen Supply. [Google Scholar]
- Scott, A., 2020. Medical oxygen demand soars. C&EN Glob. Enterp. 98, 11–11. doi: 10.1021/cen-09815-buscon3. [DOI]
- Shakil M.H., Munim Z.H., Tasnia M., Sarowar S. COVID-19 and the environment: a critical review and research agenda. Sci. Total Environ. 2020;745 doi: 10.1016/j.scitotenv.2020.141022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shourkaei A.M., Rashidi A., Karimi-Sabet J. Life cycle assessment of oxygen-18 production using cryogenic oxygen distillation. Chinese J. Chem. Eng. 2018;26:1960–1966. doi: 10.1016/j.cjche.2017.12.008. [DOI] [Google Scholar]
- Siddiqui H. Fight against Coronavirus: critical LCA technology offered to the hospitals by DRDO. Financ. Express. 2020 [Google Scholar]
- Smith L., Baker T., Demombynes G., Yadav P., Center for Global Development, https www cgdev org COVID-19 and oxygen: selecting supply options in LMICs that balance immediate needs with long-term cost-effectiveness. Cent. Glob. 2020;Dev:1–8. [Google Scholar]
- Somu G. Application of modern management techniques in healthcare. Internet J. Healthc. Adm. 2009;7:1–8. [Google Scholar]
- Stavropoulos P., Giannoulis C., Papacharalampopoulos A., Foteinopoulos P., Chryssolouris G. Life cycle analysis: comparison between different methods and optimization challenges. Procedia CIRP. 2016;41:626–631. doi: 10.1016/j.procir.2015.12.048. [DOI] [Google Scholar]
- Stein F., Perry M., Banda G., Woolhouse M., Mutapi F. Oxygen provision to fight COVID-19 in sub-Saharan Africa. BMJ Glob. Heal. 2020;5:1–4. doi: 10.1136/bmjgh-2020-002786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNEP, 2007. UN Environment Programme 2007 Annual Report.
- WHO . WHO Medical Device Technical Series; 2015. Technical Specifications for Oxygen Concentrators. [Google Scholar]
- WHO, 2020a. Oxygen Sources and Distribution for COVID-19 Treatment Centres.
- WHO, 2020b. Technical Specifications for Pressure Swing Adsorption (PSA) Oxygen Plants.
- WHO Director-General, 2020. WHO Director-General's Opening Remarks at the Media Briefing on COVID-19.
- WHO, UNICEF, 2019. WHO-UNICEF Technical Specifications and Guidance for Oxygen Therapy Devices Medical Device Technical Series.