Abstract
We present a rare case of a comminuted tibial pilon fracture with entrapment of anterior tibial vessels in fracture site, which was unexpectedly discovered intra-operatively. Following safe extrication of vessels and fracture fixation through minimally invasive approach, the patient recovered uneventfully. Phenomenon of anterior neurovascular entrapment should be kept in mind while dealing with high-energy tibial pilon fractures. Astute clinical examination, judicious use of imaging modality, and strict intra-operative vigilance are key to successful outcome.
Keywords: Tibial pilon, Fracture, Vessels, Entrapment, Management
Introduction
Entrapment of neurovascular structures in fractures is not uncommon, frequently observed in upper limb; sporadic cases have also been reported following tibial shaft fractures [1–3]. However, to the best of our knowledge, there is no such mention of neurovascular entrapment in tibial pilon fractures in literature. The anterior tibial vessels and the deep peroneal nerve are at such risk in cases of tibial pilon fractures due to its location in close proximity to distal tibia [4–6].
We report a case of highly comminuted fracture of the distal tibia (AO/OTA 43-C3) with entrapment of anterior tibial vessels with sparing of deep peroneal nerve, managed with a combination of the conventional technique and minimally invasive approach to preserve the soft-tissue envelope while carefully extracting the incarcerated vessel from the fracture site. The patient was informed that data concerning the case would be submitted for publication, and he gave consent for the same.
Case Report
A 42-year-old-male patient, manual laborer, had sustained injury following fall from tree. He was initially taken to a nearby hospital; relevant radiographs and CT scan of the involved extremity suggested comminuted fracture of tibial pilon (43-C3) with spiral extension of fracture proximally in diaphysis, and concomitant fibular fracture. He was operated upon with external fixator application and open reduction and internal fixation (ORIF) of fibula fracture. Two days after operation, he was referred to our centre for further management. Clinically, there was swelling, no distal sensory-motor deficit; dorsalis pedis artery (DPA) and posterior tibial artery (PTA) pulsations and capillary refill were well appreciated. However, DPA pulsation was feeble which was attributed to swelling. Repeat CT scan could not be obtained due to cost constraints on part of patient. A second-stage surgery was planned 15 days after the first procedure once swelling reduced and clinically wrinkle sign was observed.
Fixation with minimally invasive plate osteosynthesis (MIPO) through anterolateral approach was planned. Upon sufficient exposure of articular fragments, an unusual sight unfolded when the anterior tibial vessels were appeared to be coming out of the medullary canal of tibia. The vessels were traced proximally and were found to be passing precariously between the fragments across the meta-diaphyseal spiral fracture line. A decision for conversion to minimal ORIF was taken; the incision was extended minimally to trace the vessels proximally, and the fragments were distracted using bone hooks and lamina spreader. The vessels were gently guided out of the fracture with a cotton patty, carefully preventing any undue traction and injury. Arterial pulsation was checked immediately and the entire length of exposed vessels was examined to look for any apparent tear or thrombus. Once the health of the vessels was ascertained, the procedure was completed with articular reconstruction and fixation with anterolateral distal tibial LCP using percutaneous technique. The medial malleolar fragment was buttressed with a plate through a separate medial incision. Skin incisions were planned so as to maintain sufficient skin bridge, and soft-tissue dissection and retraction were scrupulously executed (Fig. 1).
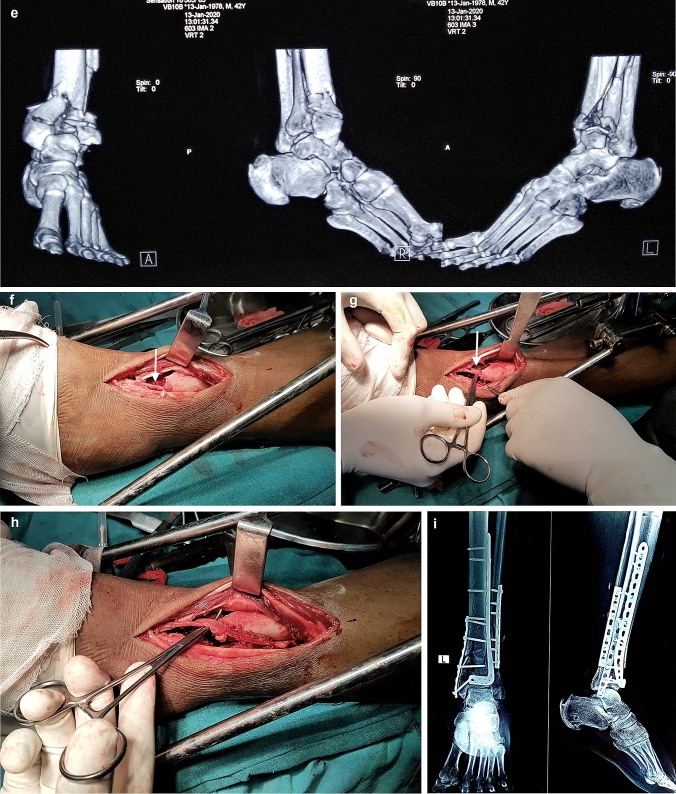
Fig. 1.
Pre-operative plain radiograph (a), and axial (b), sagittal (c), coronal (d), and 3D images (e) of CT scan of the involved extremity. Intra-operative photographs (f, g) revealing entrapped anterior tibial vessels emerging from the fracture site (white arrow). Anterolateral incision was extended proximally and entrapped vessels were meticulously extricated (h). Post-operative radiograph (i) depicting satisfactory reconstruction and fixation of fibula fracture, and pilon fracture with restoration of articular congruency
Post-operatively, patient was kept on posterior POP splint. Close regular monitoring was afforded for timely identification of late vascular embarrassment. Patient was kept on subcutaneous low-molecular-weight heparin (LMWH) until hospital discharge, followed by aspirin (150 mg) for 4 weeks. Duplex ultrasonography, before hospital discharge, demonstrated patency of anterior tibial vessels. A repeat duplex ultrasound, after suture removal at 2 weeks post-operatively, elicited satisfactory findings. At the end of 4 months of follow-up, the surgical site healed uneventfully, and radiological sign of callus formation and ongoing union was noted. Patient has no neurovascular deficit and has been allowed to bear weight partially (Fig. 2).
Fig. 2.
Follow-up photographs depicting uneventful healing of surgical wounds (a–c). Patient has no neurovascular deficit
Discussion
High-energy tibial pilon fractures continue to test judgement and skill of orthopaedic traumatologist. Despite evolution of management strategy and surgical tactics, it is fraught with unsatisfactory sequel in many patients [7]. Apart from rendering heightened vigilance for tenuous soft-tissue envelope, phenomena of various soft-tissue entrapments between fracture fragments have caught attention of surgeons lately.
Posteromedial structure entrapments (PMSEs) are recognized eventualities around pilon fractures, particularly in high-energy fractures (43-B/-C). Early recognition of this phenomenon is imperative, since it has implication on subsequent management, selection of appropriate surgical approach, and subsequent follow-up [8–10]. Eastman et al. had found 9.5% incidence of PMSE, with entrapment of posterior neurovascular bundle in 10% of cases [8]; whereas Fokin et al. reported higher frequency of PMSE (19%), albeit they did not notice any posterior neurovascular involvement [9]. Routine CT scan obtained for characterizing fracture geometry is not ideal for delineation of soft-tissue entrapment, which remain undiagnosed by radiologist and orthopaedist alike in as much as 70% of cases [8, 9]. CT scan of our patient at presentation was innocuous; furthermore, we could not get additional CT scan following external fixator application due to cost constraints that is commonplace in this developing country where surgeons are very often confronted with resource constraints and are required to strike a balance to render safe and effective treatment.
Vascular embarrassment following pilon fractures can lead to sinister sequelae if not recognized and intervened early. Wynes et al. identified late vascular insult weeks after injury and surgical treatment in a tibial pilon fracture (43-C2) that subsequently resulted in amputation. They have provided algorithm for timely identification of occult vascular insult with highly specific and sensitive imaging modalities, such as arterial duplex sonography, arteriogram, computed tomography, or magnetic resonance angiography (CTA or MRA) in the presence of high clinical suspicion [11]. LeBus et al. reported computed tomography angiography (CTA) findings on 25 patients with high-energy tibial pilon fractures and showed that more than half of them were associated with arterial abnormality of distal leg, and injury most commonly involved anterior tibial artery (69%). They asserted angiography component can judiciously be added to CT for routine evaluation of high-energy tibial pilon fracture before contemplating surgical reconstruction. Intriguingly, none of the patients with vascular insult in their series have had any wound complications following surgical fixation which was attributed to liberal use of temporizing external fixator, staged treatment, and adoption of minimally invasive approach [12]. To the best of our knowledge, only couple of reports are available in the literature depicting entrapment of anterior tibial vessels and deep peroneal nerve in spiral distal third tibia shaft fractures [2, 3]. Tan et al. attributed non-union of distal third tibia shaft fracture to entrapment of neurovascular structures. They have emphasized limitations of routine non-contrast CT for identifying this distinct possibility and stressed for MRI scan to buttress high suspicion when surgical fixation is contemplated or in the presence of non-healing of fracture at this location, even in the absence of signs or symptoms of neurovascular entrapment [3]. However, routine angiogram and MRA have its own limitations and may not always be pragmatic due to added cost, logistic, and resource. In our present case, sound clinical findings and palpable distal pulses did not raise suspicion of occult proximal vascular embarrassment, which is not unusual due to the presence of rich anastomotic network providing ample distal pulses that mask the clinical evaluation [12]. On intra-operative identification of anterior tibial vessels entrapment, we had to extend the surgical approach proximally to safely extricate the entrapped vessels. Immediate post-operative and follow-up duplex sonography showed patency of vascular trunk. We concur with Wedler et al. for adoption of Doppler sonography for early visualization of vascular anatomy and function—this modality is particularly relevant in a resource constrained orthopaedic facility [1].
Proximity of anterior neurovascular structure to distal tibia, which are located at a mean of 3 mm from anterior tibial cortex, makes it vulnerable to injury in tibial pilon fractures and also during minimally invasive plating [4–6]. No such evidence is available in the literature hitherto of anterior vascular entrapment in tibial pilon fractures. It is possible that fracture displacement that occur during injury could create potential space for intrusion of soft-tissue structures as they course through the distal leg and ankle [8]. However, selective involvement of anterior tibial vessels without deep peroneal nerve was intriguing; we speculate that fracture spike could have entrapped more laterally located vessels. It is further speculated that entrapment could have happened following ligamentotaxis during external fixator application.
Our present case purportedly represents first such report of anterior tibial vessels entrapment in high-energy tibial pilon fracture. Our meticulous soft-tissue handling and minimally invasive fixation strategy have resulted in uneventful wound healing. We believe that high index of suspicion is imperative for comminuted tibial pilon fractures; careful clinical examination coupled with liberal use of imaging modality, such as arterial duplex sonography or CTA, should be instituted for timely identification of vascular embarrassment before planning definitive surgical treatment. While performing MIPO for comminuted tibial pilon fractures, this entity should be kept in mind, and if need arises, exposure can be converted to minimal ORIF to expose the fracture site is in its entirety for better delineation without devitalizing soft tissues.
Acknowledgements
None.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interests.
Ethical standard statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed consent
The patient was informed that data concerning the case would be submitted for publication, and he gave consent for the same.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wedler V, Labler L, Köhler C, Guggenheim M, Künzi W, Trentz O. Iatrogenic neurovascular entrapment injuries caused by reduction and intramedullary fixation of fractures of the lower limb. European Journal of Trauma. 2006;32:381–386. doi: 10.1007/s00068-006-6127-9. [DOI] [Google Scholar]
- 2.Miki, R.A., Lawrence, J.P., Gillon, T.J., Lawrence, B.D., & Zell, R.A. (2008). Anterior tibial artery and deep peroneal nerve entrapment in spiral distal third tibia fracture. Orthopedics. 10.3928/01477447-2008-1201-13. [DOI] [PubMed]
- 3.Tan ET, Tan TJ, Poon KB. Entrapment of the deep peroneal nerve and anterior tibial vessels by a spiral tibial fracture causing partial non-union: a case report. Skeletal Radiology. 2016;45(4):551–554. doi: 10.1007/s00256-015-2259-5. [DOI] [PubMed] [Google Scholar]
- 4.Wolinsky P, Lee M. The distal approach for anterolateral plate fixation of the tibia: an anatomic study. Journal of Orthopaedic Trauma. 2008;22(6):404–407. doi: 10.1097/BOT.0b013e31817614b2. [DOI] [PubMed] [Google Scholar]
- 5.Ali AA, Gregory JJ, Ockenden M, Hill SO, Makwana NK. Anatomic description of the distal tibia: implications for internal fixation. The Journal of Foot and Ankle Surgery. 2012;51(3):296–298. doi: 10.1053/j.jfas.2011.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Lidder S, Masterson S, Grechenig C, Clement H, Gänsslen A, Grechenig S. The risk of neurovascular injury in minimally invasive plate osteosynthesis (MIPO) when using a distal tibia anterolateral plate: a cadaver study. Acta Chirurgiae Orthopaedicae et Traumatologiae Cechoslovaca. 2014;81(5):313–316. [PubMed] [Google Scholar]
- 7.Zelle BA, Dang KH, Ornell SS. High-energy tibial pilon fractures: an instructional review. International Orthopaedics. 2019;43(8):1939–1950. doi: 10.1007/s00264-019-04344-8. [DOI] [PubMed] [Google Scholar]
- 8.Eastman JG, Firoozabadi R, Benirschke SK, Barei DP, Dunbar RP. Entrapped posteromedial structures in pilon fractures. Journal of Orthopaedic Trauma. 2014;28(9):528–533. doi: 10.1097/BOT.0000000000000046. [DOI] [PubMed] [Google Scholar]
- 9.Fokin A, Jr, Huntley SR, Summers SH, et al. Computed tomography assessment of peroneal tendon displacement and posteromedial structure entrapment in pilon fractures. Journal of Orthopaedic Trauma. 2016;30(11):627–633. doi: 10.1097/BOT.0000000000000658. [DOI] [PubMed] [Google Scholar]
- 10.Henry PDG, McKee MD. Irreducible tibial pilon fracture secondary to posterior tibial tendon entrapment: a case report. JBJS Case Connector. 2012;2(4):e69. doi: 10.2106/JBJS.CC.L.00030. [DOI] [PubMed] [Google Scholar]
- 11.Wynes J, Kirksey L. Assessing vascular status and risk of latent ischemia with ankle fracture: a case report and algorithm for treatment. The Journal of Foot and Ankle Surgery. 2014;53(3):353–355. doi: 10.1053/j.jfas.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 12.LeBus GF, Collinge C. Vascular abnormalities as assessed with CT angiography in high-energy tibial plafond fractures. Journal of Orthopaedic Trauma. 2008;22(1):16–22. doi: 10.1097/BOT.0b013e31815cf6e9. [DOI] [PubMed] [Google Scholar]