Abstract
THIS ARTICLE PRESENTS THE RESULTS OF A REVIEW of studies of psychology that describe how ordinary human reasoning may lead patients to provide an unreliable history of present illness. Patients make errors because of mistakes in comprehension, recall, evaluation and expression. Comprehension of a question changes depending on ambiguities in the language used and conversational norms. Recall fails through the forgetting of relevant information and through automatic shortcuts to memory. Evaluation can be mistaken because of shifting social comparisons and faulty personal beliefs. Expression is influenced by moods and ignoble failures. We suggest that an awareness of how people report current symptoms and events is an important clinical skill that can be enhanced by knowledge of selected studies in psychology. These insights might help clinicians avoid mistakes when eliciting a patient's history of present illness.
Assessing a patient's current symptoms is an essential clinical skill. Doing so is sometimes the only way to diagnose an illness, assess the effectiveness of treatment or formulate a prognosis.1 Conversely, the failure to take an adequate medical history can lead to mistakes with clinical and economic consequences.2 The skill involved in taking a patient's history is taught in medical school but is seldom reinforced in continuing medical education courses.3,4 Moreover, much advice can come across as clichéd as in admonitions to “be sympathetic” and “take time.”5 In addition, most studies focus only on cases in which the patient is dissatisfied.6,7,8
Consider a middle-aged patient who presents with fatigue. The symptoms started only recently and are not accompanied by any weight loss or pain. In fact, he cannot think of anything else that is wrong and cannot recall any problems. He has wondered whether the fatigue is normal aging, knows of many who are worse off than he is, but says that his son insisted that he see a doctor. Incidentally, he is worried a lot about this son who is unemployed. The patient says nothing else to you. You find nothing on examination. You remain uncertain and decide to see him in a month to determine whether the symptoms have persisted. The patient agrees.
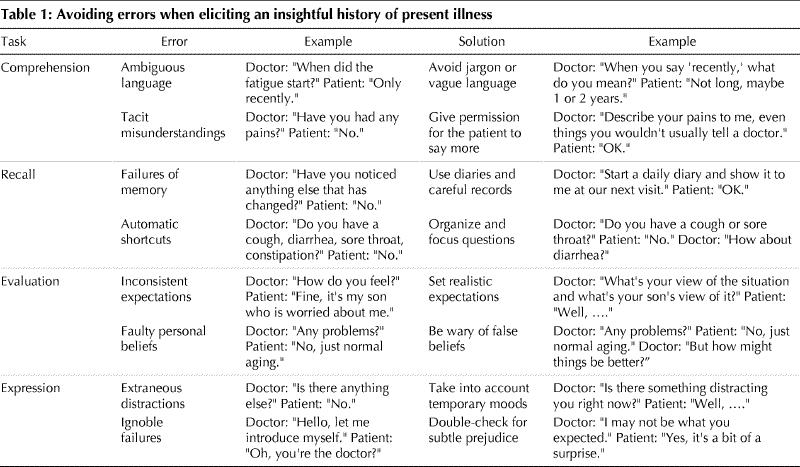
In this article we discuss 8 traps buried in this case history that can lead to a treatment error. In doing so, we review classic findings in psychology on the fallibility of individuals' reporting of current states. These problems can be so well hidden that both the physician and patient might think that nothing has gone wrong. The mistakes are classified as related to comprehension, recall, evaluation or expression (Table 1). Together, these are the 4 basic roots of the problems that can occur when taking a patient's history, despite an apparently complete and satisfactory exchange of information.
Table 1
Comprehension
Ambiguous language
A history cannot be recounted if the patient cannot understand the physician. This is self-evident if the patient is comatose, and is equally true even without an obvious communication barrier. For example, consider the following comedic exchange: Miss Dimple: “Call me a taxi.” Groucho Marx: “OK, you're a taxi.” The principle illustrated by this exchange is that people are prone to answer ambiguous expressions without taking the time to ask for clarification.9 In medicine, the consequences are not funny because the stakes are substantial. Moreover, physicians are prone to use jargon that can intimidate patients, such as “Any loss of libido?”
More subtle misunderstandings can arise because the wording of a question may shape the nature of the response. In one experiment, for example, college students were interviewed after watching a film of a traffic collision.10 Those asked “How fast were the cars going when they smashed into each other?” gave higher estimates than those asked “How fast were the cars going when they hit each other?” Indeed, those asked the “smashed” question were more likely to report having seen broken glass than those asked the “hit” question, even though no glass was shown (32% v. 14%, p = 0.03). In medicine, slight changes in the wording of even simple questions might also shape patients' replies.
Language problems often occur with extremely common expressions. For example, the inquiry “Do you feel better?” is ambiguous because the word “better” can mean either “improved” or “normalized.” Hence, a patient can impose an interpretation that may not be what the speaker intended. This problem could be avoided by starting with an open question such as “How are you today?” Other examples of ambiguous language to avoid in medicine include “a right-sided stroke,” “do you drink much?” and “started recently.” Only a sharp-witted patient will ask for clarification, even though each of these expressions has more than one interpretation. Most patients just say nothing rather than disclose their uncertainty.
Tacit misunderstandings
Complicating things further are the tacit norms that govern everyday conversation.11 For example, consider a study that asked students to rate their happiness and their satisfaction with life.12 When each of the 2 questions appeared in a different survey, the mean ratings were similar (80% v. 82%, p = 0.68). Presumably, respondents interpreted the 2 questions as having the same meaning. In contrast, the mean ratings diverged when both questions appeared next to each other on the same survey (82% v. 74%, p < 0.05). In this format, respondents presumably thought that the 2 questions had different interpretations. Together, these results illustrate how tacit norms can shape people's responses.
All cultures have norms that exert significant control even when people hardly sense their existence. Sportscasters commenting on tennis players, for example, never noticed that they were much more likely to refer to women than to men by using only a first name (53% v. 8%, p < 0.05).13 A lack of shared norms, of course, invites misunderstandings. For example, for an adolescent, the distinction “a wicked skier” is a triumph not a failing.14 Clinicians need to be aware that different cultures are reticent to different degrees and vary in what they feel is appropriate for an ill person to say.
A special problem with societal norms relates to innuendo. Consider an emergency physician who asks, “How long ago did your chest pain start?” This question is legitimate and may have important implications for thrombolytic therapy. However, the patient may mistakenly infer that the question signals disapproval rather than diligence. A responsible patient does not want to seek care with undue haste or delay; unfortunately, the physician's question smacks of reproach as if to insinuate that the patient sought care at the wrong time. Insinuation is not what the physician intended but can occur when a person in authority asks a question. One way to lessen this problem is for the physician to explain the reason for asking the question.
Recall
Failures of memory
Without memory there is no history, as shown by dialogue with a patient with end-stage Alzheimer's disease. Even a question such as “Is your hearing better or worse?” assumes that the patient can remember. However, even healthy people's memories are fallible. For example, students were interviewed in 1973 and again in 1982 about marijuana legalization. The first finding was that individuals' attitudes changed substantially between 1973 and 1982. The second finding was that individuals did not appreciate how much their attitudes had changed. As a consequence, each person's memory of their attitudes in 1973 was closer to their attitudes in 1982 than to those that they had reported in 1973.
The fallibility of memory is one of the most rigorously demonstrated findings in psychology. As one study colourfully stated,15 “It is all too common for caterpillars to become butterflies and then to maintain that in their youth they had been little butterflies.” Additional difficulties arise because the decay never stops. In one study, people could remember 100% of their classmates' names on the day of graduation from high school, 75% of names after 7 years and only 57% of names after a further 7 years.16 Evidently, being able to remember an item for a few years is no guarantee that it will be retained for a few more. Technical details fade faster than personal feelings, so that patients may be unable to recall a doctor's instructions soon after returning home.
An appreciation of the fallibility of memory might encourage physicians to consider protective strategies. First, some patients, such as those with unexplained allergic reactions or chronic fatigue, should be asked to keep a symptom diary. Second, nonintrusive recording devices can sometimes be worthwhile, such as automatic electronic registers for patients with diabetes who self-monitor their blood sugars. Third, some patients might benefit from being told in advance what questions will probably be asked at the next visit. Fourth, physicians may wish to write down for the patient some of the key points that they have discussed. Inaccurate recall is exacerbated when patients are confident of their memory and have no way to check for mistakes.
Automatic shortcuts
A predictable memory failure occurs when a person is asked a question that requires laborious work for a perfect answer. Try to remember, for example, whether more people died last year in fires or by drowning. People generally guess that fires are a more common cause of death, yet statistics show the opposite.17 The misconception arises because people make such a calculation by judging the ease with which examples come to mind — and fires are highly reported. People tend to use fallible memory shortcuts rather than rigorous mental counting when facing a complex mental task. For example, the question “How many cigarettes do you smoke daily?” is likely to produce an underestimate. A better question might be “How long does it take you to finish a pack?”
Properly organized questions tend to generate more insightful responses. In one experiment, students were asked to recall 3 white foods: most could not. In contrast, other students were asked to recall 3 white dairy foods: almost all succeeded. Evidently, people sometimes have more information buried inside them than gets released when asked an awkward question. Inquiries can be made less burdensome if they are logically organized. Clinicians need to recognize how easy it is to ask a sloppy question and how doing so inhibits a careful reply. Disorganized lines of questioning may explain, for example, why unskilled interviewers are poor at taking a patient's psychiatric history.18
Evaluation
Inconsistent expectations
People normally supress most feelings and focus only where their perceptions conflict with their expectations; for example, healthy people do not notice their breathing. Conversely, teenagers who develop diabetes are often quite unhappy about the need for injections and other violations of their expectations. With time, many seem to adapt, despite showing no objective improvement in their disease.19 This adaptation is often facilitated by contact with other patients, who provide not just practical tips but also a new set of social comparisons. Changing personal expectations imply that there is no simple connection between patients' subjective severity of symptoms and their objective severity of disease.20
Social comparisons and other personal standards, however, produce errors because of their inconsistent application. For example,21 researchers evaluated Olympic athletes and found that, on a 10-point scale, gold medalists showed the most signs of happiness. Surprisingly, bronze medalists showed more signs of happiness than silver medalists (7.1 v. 4.8, p < 0.001). The most likely reason for this paradox was that bronze medalists could easily imagine themselves winning nothing, whereas silver medalists could easily imagine themselves winning gold. Because downward comparisons are comforting and upward comparisons are dreary, such social comparisons may lead those who are worse off objectively to feel better off subjectively. In oncology, many patients express more anguish when diagnosed with cancer than when at the final stages.
Social comparisons flourish when patients evaluate their health. The inconsistencies are perhaps the fundamental explanation for the paradox of health; namely, that the collective health of the nation has improved in past decades but population surveys report declining levels of subjective well-being.22 Such a paradox, of course, is not unique to medicine but is a basic feature of human psychology. For example, 90% of American adults claim, contrary to the laws of probability, that they are less likely to develop a drug addiction than their peers.23 One way for physicians to reduce patients' misconceptions is to provide a wider perspective, for example, by describing the diversity of those treated for drug addiction.
Faulty personal beliefs
Counterfactual thinking, that is, the ability to imagine a state that is contrary to fact, can also provide a standard for evaluation. A patient, for example, can always engage in the imaginative exercise of thinking “There but for the grace of God go I.” In one study of people whose property was destroyed in a large fire, the common finding was that older people and younger people each thought that they were better off than those in the other age group.24 Evidently, people sometimes minimize their deficiencies by imaginative comparisons. Doing so serves several functions such as creating a positive mood and minimizing the stigma of being a victim.25
Patients' symptoms can also be influenced by their beliefs about the causes of their symptoms. In one experiment, university students volunteered for a study that required electric shocks.26 At the start, half were given a placebo that was deceptively described as causing sweating, irregular breathing and anxiety. The theory was that those receiving the placebo would attribute their symptoms to the pill rather than to the shocks and would, thereby, tolerate more pain. The findings confirmed this hypothesis, with those given the placebo tolerating more shocks than those given nothing (26 v. 16, p = 0.004). Analogous issues may arise in patients who are convinced that symptoms improve at the moment when they first start taking antibiotics.
The interplay between symptoms and beliefs can occur in almost any clinical setting because patients often think of causes for their symptoms that are unduly benign or malignant. These imaginings can be substantially affected by a physician, and physicians should use such power carefully. For example, vertigo caused by viral labyrinthitis is distressing not just because of the dizziness but also because it creates worries about a possible brain tumour. The savvy clinician, therefore, should be aware that many symptoms can be lessened by giving the patient a clear diagnosis, addressing some underlying misconception and not prescribing medication.27
Expression
Extraneous distractions
Speech can be destroyed by an acute stroke, and can be distorted by a multitude of much more subtle forces. In one experiment,28 participants were asked to rate their health while being interviewed in 1 of 2 rooms. The pleasant room was a friendly office in good condition. The unpleasant room was a dirty laboratory with too much heat, flickering light, distracting noise and a bad smell. Mean ratings were about 15% higher on an 11-point scale in the pleasant room than in the unpleasant room (9.4 v. 8.1, p < 0.05). Similar discrepancies have also been found with sunny weather and other extraneous factors.29,30,31
Temporary mood states seem to influence subjective reporting in 2 different ways. On the one hand, moods may increase the accessibility of emotionally congruent information in the memory; that is, when one is happy, it is easy to remember other sources of happiness, whereas when sad it is easy to remember other sources of sadness. On the other hand, moods can also be misinterpreted as valid indicators of a person's well-being with insufficient recognition of their evanescent nature. Regardless of explanation, patients may base their summaries of their state of health on momentary feelings, and 2 physicians might obtain divergent histories from the same person.
Peoples' moods are influenced by their surroundings. It is not surprising, therefore, that patients in a crowded emergency department often feel poorly when waiting for a bed and often feel better after being admitted to a private room. Failure to appreciate these extraneous factors, however, might lead a clinician to overestimate the severity of disease in the emergency department, exaggerate the effectiveness of the initial treatments and underestimate the progressive nature of an underlying disorder. In some cases, moreover, both the patient and the physician have a vested interest in keeping things positive and want to believe that the medical treatment is effective.
Ignoble failures
Eliciting a patient's history is also a human interaction vulnerable to ignoble failures. Consider, for example, discrimination. Studies show that women tend to pay more than men when buying the same automobile.32 In one study, the dealer's profit margin was about US$92 higher for women than for men (US$656 v. US$564, respectively). The deals were particularly poor for black women, who tended to pay about US$411 more than white men (US$975 v. US$564, p = 0.006). The surprising finding, however, was that black women obtained their best deals from white male dealers, not black or female dealers. These results suggest that the worst aspects of human nature sometimes have counterintuitive features.
Most of the disgraceful characteristics of both patients and physicians are not the subject of public debate, rigorous research or scientific advances. Instead, most people hope that such failings in physicians are either eliminated by medical school admission requirements or extinguished during professional training. Furthermore, most people hope that exemplary behaviour by clinicians can mollify any such tendencies in patients. We hold a less optimistic perspective. There are no easy solutions because ignoble failings can be more complicated or more subtle than is generally recognized.
A better scientific understanding of ignoble failures is hampered by at least 2 realities in medicine. First, such projects are rarely funded given that industry sources of support for medical research have other priorities.33 Second, readers can usually find flaws in the final study that allow the conclusions to be called into doubt. For black women, the reported shortfalls in cardiac care will probably take longer to sort out than the surcharges in automobile deals.34,35,36,37,38,39 Minimizing ignoble failures, therefore, is yet another priority that requires clinical judgement and not just scientific literature. Turning a blind eye solves nothing.
Conclusion
This article reviews observations from psychology that are relevant when taking a patient's history of present illness. The 4 main areas of interest are comprehension, recall, evaluation and expression, even though the issues interact at several levels. The overall theme is that communication may be problematic even if all parties seem satisfied. The patient case in the Introduction describes a situation containing 8 specific traps (Table 1). These pitfalls may explain why one of us (D.A.R.) missed the diagnosis of acromegaly and why such patients generally have a 5-year delay in diagnosis, resulting in permanent disfigurement.40
Articles to date in this series .
Redelmeier DA, Ferris LE, Tu JV, Hux JE, Schull MJ. Problems for clinical judgement: introducing cognitive psychology as one more basic science. CMAJ 2001;164(3):358-60.
Footnotes
This article has been peer reviewed.
Competing interests: None declared.
Reprint requests to: Dr. Donald A. Redelmeier, Sunnybrook & Women's College Health Sciences Centre, Rm. G151, 2075 Bayview Ave., Toronto ON M4N 3M5; fax 416 480-6048; dar@ices.on.ca
References
- 1.Sapira JD. The art and science of bedside diagnosis. Baltimore (MD): Urban & Schwarzenberg; 1990. p. 33.
- 2.Rubsamen DS. Medical malpractice. Sci Am 1976;235:18-23. [DOI] [PubMed]
- 3.Novack DH, Volk G, Drossman DA, Lipkin M. Medical interviewing and interpersonal skills teaching in US medical schools: progress, problems, and promise. JAMA 1993;269:2101-5. [PubMed]
- 4.Brown JB, Boles M, Mullooly JP, Levinson W. Effect of clinician communication skills training on patient satisfaction: a randomized controlled trial. Ann Intern Med 1999;131:822-9. [DOI] [PubMed]
- 5.DeGowin EL, DeGowin RL. Bedside diagnostic examination. 4th ed. New York: Macmillan Publishing; 1981. p. 15-6.
- 6.Boon H, Stewart M. Patient-physician communication assessment instruments: 1986 to 1996 in review. Patient Educ Couns 1998;35:161-76. [DOI] [PubMed]
- 7.Williams S, Weinman J, Dale J. Doctor-patient communication and patient satisfaction: a review. Fam Pract 1998;15:480-92. [DOI] [PubMed]
- 8.Ong LM, de Haes JC, Hoos AM, Lammes FB. Doctor-patient communication: a review of the literature. Soc Sci Med 1995;40:903-18. [DOI] [PubMed]
- 9.Fischhoff B, Bostrom A, Quadrel MJ. Risk perception and communication. Annu Rev Public Health 1993;14:183-203. [DOI] [PubMed]
- 10.Loftus EF, Palmer JC. Reconstruction of automobile destruction: an example of the interaction between language and memory. J Verbal Learn Verbal Behav 1974;13:585-9.
- 11.Grice HP. Logic and conversation. In: Cole P, Morgan JL, editors. Syntax and semantics. 3: Speech acts. New York: Academic Press; 1975. p. 41-58.
- 12.Strack F, Schwarz N, Wänke M. Semantic and pragmatic aspects of context effects in social and psychological research. Social Cognition 1991;9:111-25.
- 13.Myers DG. Social psychology. 5th ed. New York: McGraw Hill; 1996. p. 203-4.
- 14.Barnsley J, Williams AP, Cockerill R, Tanner J. Physician characteristics and the physician-patient relationship. Impact of sex, year of graduation, and specialty. Can Fam Physician 1999;45:935-42. [PMC free article] [PubMed]
- 15.Vallant GE. Adaptation to life. Boston: Little Brown; 1997.
- 16.Bradburn NM, Rips LJ, Shevell SK. Answering autobiographical questions: the impact of memory and inference on surveys. Science 1987;236:157-61. [DOI] [PubMed]
- 17.US Census Bureau. Statistical abstract of the United States 1996: the national data book. 116th ed. Washington: US Census Bureau; 1997. p. 101.
- 18.Helzer JE, Robins LN, McEvoy LT, Spitznagel EL, Stoltzman RK, Farmer A, et al. A comparison of clinical and diagnostic interview schedule diagnoses. Physician reexamination of lay-interviewed cases in the general population. Arch Gen Psychiatry 1985;42:657-66. [DOI] [PubMed]
- 19.Grey M, Boland EA, Davidson M, Yu C, Tamborlane WV. Coping skills training for youths with diabetes on intensive therapy. Appl Nurs Res 1999;12:3-12. [DOI] [PubMed]
- 20.Redelmeier DA, Goldstein RS, Min ST, Hyland RH. Spirometry and dyspnea in patients with COPD: when small differences mean little. Chest 1996;109:1163-8. [DOI] [PubMed]
- 21.Medvec VH, Madey SF, Gilovich T. When less is more: counterfactual thinking and satisfaction among Olympic medalists. J Pers Soc Psychol 1995;69:603-10. [DOI] [PubMed]
- 22.Barsky AJ. The paradox of health. N Engl J Med 1988;318:414-8. [DOI] [PubMed]
- 23.Weinstein ND. Optimistic biases about personal risks. Science 1989;246:1232-3. [DOI] [PubMed]
- 24.Taylor SE, Wood JV, Lichtman RR. It could be worse: selective evaluation as a response to victimization. J Soc Issues 1983;2:19-40.
- 25.Taylor SE, Brown JD. Illusion and well-being: a social psychological perspective on mental health. Psychol Bull 1988;103:193-210. [PubMed]
- 26.Nisbett RE, Schacter S. Cognitive manipulation of pain. J Exp Soc Psychol 1966;2:227-36.
- 27.Sox HC Jr, Margulies I, Sox CH. Psychologically mediated effects of diagnostic tests. Ann Intern Med 1981;95:680-5. [DOI] [PubMed]
- 28.Schwarz N, Strack F, Kommer D, Wagner D. Soccer, rooms, and the quality of your life: mood effects on judgment of satisfaction with life in general and with specific life domains. Eur J Soc Psychol 1987;17:69-79.
- 29.Schwarz N. Stimmung als Information: zum Einfluss von Stimmungen auf die Beurteilung des eigenen Lebens. In: Luers G, editor. Bericht über den 33: Kongress der deutschen Gesellschaft für Psychologie in Mainz. Göttingen (Germany): Hogree; 1983. p. 35-45.
- 30.Schwarz N, Strack F, Kommer D, Wagner D. Soccer, rooms, and the quality of your life: mood effects on judgment of satisfaction with life in general and with specific life domains. Eur J Soc Psychol 1987;17:69-79.
- 31.Schwarz N, Clore GL. Mood, misattribution, and judgments of well-being: informative and directive functions of affective states. J Pers Soc Psychol 1983; 45:513-23.
- 32.Ayers I, Siegelman P. Race and gender discrimination in bargaining for a new car. Am Econ Rev 1995;85:304-21.
- 33.Redelmeier DA. Drug dependence in journal club. ACP J Club 1999;4:A13-5. [PubMed]
- 34.Schulman KA, Berlin JA, Harless W, Kerner JF, Sistrunk S, Gersh BJ, et al. The effect of race and sex on physicians' recommendations for cardiac catheterization. N Engl J Med 1999;340:618-26. [DOI] [PubMed]
- 35.Schwartz LM, Woloshin S, Welch HG. Misunderstandings about the effects of race and sex on physicians' referrals for cardiac catheterization. N Engl J Med 1999;341:279-83. [DOI] [PubMed]
- 36.Helft G, Worthley SG, Chokron S. Race, sex, and physicians' referrals for cardiac catheterization [letter]. N Engl J Med 1999;341:285. [DOI] [PubMed]
- 37.Davidoff F. Race, sex, and physicians' referrals for cardiac catheterization [letter]. N Engl J Med 1999;341:285-7. [PubMed]
- 38.Shulman KA, Berlin JA, Escarce JJ. Race, sex, and physicians' referrals for cardiac catheterization [letter]. N Engl J Med 1999;341:286. [DOI] [PubMed]
- 39.Curfman GD, Kassirer JP. Race, sex, and physicians' referrals for cardiac catheterization [letter]. N Engl J Med 1999;341:287. [PubMed]
- 40.Ezzat S, Forster MJ, Berchtold P, Redelmeier DA, Boerlin V, Harris AG. Acromegaly. Clinical and biochemical features in 500 patients. Medicine 1994;73:233-40. [PubMed]


