Abstract
The purpose of this case report is to report the long-term outcome following shoulder hemiarthroplasty in a patient with dwarfism. A 60-year old female with pseudoachondroplasia dwarfism presented 17 years post-operative with a Subjective Shoulder Value of 90% and minimal pain. Custom designed implants were critical for surgical success. Preoperative planning with a CT scan was important in assessing glenoid dysplasia and determining the feasibility of glenoid resurfacing. The emergence of 3D CT virtual preoperative planning tools can further assist in the recognition of deformity to determine if custom designed implants are needed. Shoulder arthroplasty in dwarfism can lead to excellent long-term outcomes.
Key words: Dwarfism, Shoulder Arthroplasty, Hemiarthroplasty, Outcomes
Introduction
Pseudoachondroplasia (PSACH) is a rare (1/30,000 estimated birth prevalence),1 autosomal-dominant form of rhizomelic dwarfism first described in 1959 by Maroteaux and Lemy.2 Abnormalities are caused by a defect in the cartilage oligomeric matrix protein (COMP) on chromosome 19. This results in calcium-binding and protein export dysfunction which ultimately triggers chondrocyte death during linear growth.1,3 The classic manifestations of PSACH include abnormalities in the long bones, joints and spine. Clinical findings include early-onset osteoarthritis, ligamentous laxity, genu valgum, and bowing deformities of the lower extremity.1,4,5 Radiographically, these patients exhibit disproportionate shortening of the proximal long bones, irregular epiphyseal plates, and widened metaphysis. Findings include delayed maturation of the carpal bones, underossification of the spine leading to exaggerated lordosis and scoliosis, and osteoarthritic joint changes in the second or third decade of life.6,7
Symptomatic osteoarthritis presents first and more commonly in the hips and knees and may present later in the shoulders, elbows, ankles and feet. As such, hip and knee arthroplasty in PSACH has been reported more frequently.8-13 To our knowledge, the literature to date reports on only two cases of shoulder hemiarthroplasty in patients with PSACH.14,15 In assessing early outcomes, the authors described marked improvements in function and pain but long-term follow-up is lacking. The current case describes 17-year clinical follow-up of one of two patients originally reported by Pennington et al. in 2011.15
Case Report
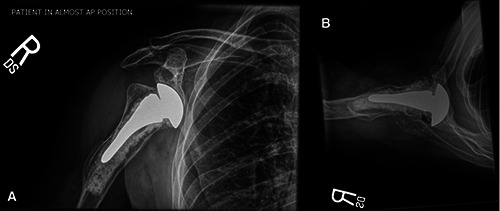
An otherwise healthy, 60-year-old female with PSACH presented to clinic 17 years following a right shoulder hemiarthroplasty with custom-designed implants. She initially presented as a 43-year-old patient with debilitating right dominant shoulder pain rated at a 12 on a 1 to 10 visual analog pain scale that disturbed her sleep nightly. Prior to the index procedure, her active range of motion was limited, with 80 degrees of forward elevation, 10 degrees of external rotation and internal rotation to the greater trochanter of the hip. Orthogonal radiographs of the right shoulder demonstrated glenohumeral osteoarthritis with marked varus deformity of the proximal humerus, flattening of the humeral head, and anterior bowing of the humeral shaft (Figure 1A). The glenoid was severely deformed and dysplastic with inferior inclination of the articular surface confirmed with pre-operative computed tomography (CT) scan (Figure 1B). Due to her severe pain which significantly affected her quality of life and failure of nonoperative treatment, she underwent a right shoulder hemiarthroplasty with custom designed implants, performed by the senior author (JJPW).
As previously described,15 due to her short stature the patient was positioned on a long bean bag. Also, because of her shortened extremity a padded mayo stand was used to support the operative arm instead of an arm positioner. An extended deltopectoral approach was utilized. A custom size 6- mm stem and a 36-mm head were created for this patient (Anatomical Shoulder SystemTM, Zimmer-Biomet, Warsaw, IN, USA). Given the severity of her bony deformity, the humeral component was cemented and the glenoid was elected not to be resurfaced due to the severe glenoid dysplasia. Though shortened and scarred, the subscapularis was able to be repaired at the completion of the case with transosseous sutures. Three years following surgery, the patient had no pain (0 out of 10 on a visual analogue pain scale) and improved motion, symmetric to the contralateral side (forward flexion 120 degrees, external rotation 20 degrees, and internal rotation to the T12 thoracic level). Her belly press test was normal, and radiographs showed a well-positioned prosthesis concentrically seated on the glenoid.
The patient provided an interval history now 17 years after surgery. Ten years postoperative, she became wheelchair-bound due to severe dysplasia and osteoarthritis in both hips. Over the last two years she had an exacerbation of pain in her right shoulder because she was required to wheel herself long distances to and from work. She recently changed her job location and this pain has subsided. On examination she is 52 inches tall, and weighs 80 pounds. Her subjective shoulder value (SSV) is 90 percent. She rates her pain as 2 out of 10 on a visual analogue pain scale, without any night pain. On examination, she can forward flex to 130 degrees, externally rotate to 30 degrees, and internally rotate to the T10 thoracic level (Figure 2). Her abduction is 90 degrees and external rotation in abduction is 80 degrees. She has a normal belly press test. Orthogonal radiographs demonstrate a wellpositioned cemented humeral component with severe erosion of the inferior glenoid (Figure 3).
Discussion
Prior reports of shoulder arthroplasty in dwarfism demonstrate good outcomes at short and mid-term follow-up.14,15 However, long-term outcomes of shoulder arthroplasty in this patient population have not been reported. We present the case of a patient with pseudoachondroplasia who returned for follow-up 17 years after hemiarthroplasty. Despite inferior glenoid erosion on plain films, the patient had an SSV of 90%, minimal pain with most activities, and excellent motion and strength.
Preoperative recognition of her severe proximal humeral and glenoid deformity with a 2-dimensional (2D) CT scan was essential to the successful outcome demonstrated in this case. This led to the decision to perform a hemiarthroplasty with custom designed implants necessary to match the patient’s unique anatomy. Recent evidence has shown that CT with 3-dimensional (3D) reconstruction is more reliable in terms of assessing glenoid retroversion and deformity as compared to 2D CT.4,13 This technology can be used to perform virtual preoperative planning to select optimal size and positioning of implants prior to surgery and can be particularly helpful in those with severe deformity. The senior author (JJPW) has used virtual 3D CT planning software for subsequent arthroplasty cases in patients with dwarfism to determine the need for custom implants on a case-by-case basis. For instance, this patient with achondroplasia underwent virtual surgery with 3D CT planning and it was determined that the smallest implants available for this particular implant design fit the patient, as such, custom implants were not needed (Figure 4). Future dependence on upper extremity weight-bearing in this patient population should not be overlooked given the high incidence of hip and knee osteoarthritis and lower extremity bowing deformities. Most of the current literature in this setting focuses on patients with paraplegia.18-21 Functional and patient-reported outcomes for wheelchair-dependent patients 2-5 years following reverse shoulder arthroplasty have been positive but complication rates are high.18,19,21 These complications include humeral loosening, baseplate failure, scapular notching, and dislocation.3,21 In the present case, the patient’s pain levels necessitated a job change to reduce the burden of powering the wheelchair with her arms over long distances. Pain and function improved as her circumstances changed. This information can be critically important during preoperative and postoperative counseling with prospective patients.
There are other aspects of care which are critical to mention and unique for the treatment of patients with dwarfism. This includes the use of a bean bag to cradle the patient on a large operating room table, the use of a padded Mayo stand instead of a hydraulic arm positioner, and obtaining a pediatric sling and polar care for use postoperatively (Figure 5). Additionally, it is important to coordinate for a pediatric gown for the patient to wear during and after surgery to avoid tripping over a longer gown on the hospital floor. Consideration and coordinating these finer details prior to and during the perioperative care period will help to optimize the patient’s satisfaction and outcome.
Figure 1.

(A) Preoperative Grashey radiograph of the right shoulder shows severe humeral deformity and inferior glenoid inclination. (B) Preoperative computed tomography demonstrates glenoid dysplasia on axial cuts.
Figure 2.

17-year right-sided postoperative range of motion assessment demonstrating: (A) forward flexion, (B) external rotation in abduction, (C) external rotation, and (D) internal rotation. Note, she has now developed degenerative glenohumeral disease on the left side, which prompted this clinic visit.
Figure 3.
17-year postoperative (A) Grashey and (B) axillary lateral radiographs demonstrating a well-fixed hemiarthroplasty with progressive glenoid wear.
Figure 4.

Preoperative 3D computed tomography planning example for a patient with achondroplasia demonstrates the need for smallest possible implants without custom design. (A) Retroversion, inclination, and posterior humeral head subluxation are automatically calculated. (B) Glenoid planning permits site modification and placement on the glenoid vault for maximal fixation. (C) This case permitted the use of a kneeled rather than pegged glenoid due to the small site of available glenoid bone stock. (D) Humeral planning allows for sizing and determination as to whether a stemmed or stemless implant can be used. (E) This screenshot shows the final plan and produces calculation of version and inclination correction.
Conclusions
The current case study describes the long-term clinical outcome following shoulder hemiarthroplasty in a patient with dwarfism due to pseudoachondroplasia. At final follow-up, the patient had an SSV of 90% with minimal pain 17-years following surgery. Custom designed implants were critical to the success of the surgery. Preoperative planning with a 2D CT scan is important in assessing glenoid dysplasia in this population to determine if the glenoid should be resurfaced. The emergence of 3D CT virtual preoperative planning tools will assist in the recognition of both humeral and glenoid deformity and assist in determining if custom designed implants are needed.
Figure 5.

Example of pre-operative positioning in the beach chair using a molded bean bag for support.
Funding Statement
Funding: None.
References
- 1.Posey KL, Alcorn JL, Hecht JT. Pseudoachondroplasia/COMP—translating from the bench to the bedside. Matrix Biol 2014;37:167-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maroteaux P, Lamy M. Pseudo-achondroplastic forms of spondylo-epiphyseal dysplasias. Presse Med 1959;67:383-6. [PubMed] [Google Scholar]
- 3.Luo H, Yu S, Lin Y, et al. A novel deleterious mutation in the COMP gene that causes pseudoachondroplasia. Hum Genome Var 2016;3:16009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Posey KL, Hayes E, Haynes R, Hecht JT. Role of TSP-5/COMP in pseudoachondroplasia. Int J Biochem Cell Biol 2004;36:1005-12. [DOI] [PubMed] [Google Scholar]
- 5.Unger S, Hecht JT. Pseudoachondroplasia and multiple epiphyseal dysplasia: new etiologic developments. Am J Med Genet 2001;106:244-50. [PubMed] [Google Scholar]
- 6.Briggs MD, Wright MJ. Pseudoachondroplasia. 2004 Aug 20 [Updated 2018 Aug 16]. Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2019. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1487/. [Google Scholar]
- 7.El-Sobky TA, Shawky RM, Sakr HM, et al. A systematized approach to radiographic assessment of commonly seen genetic bone diseases in children: A pictorial review. J Musculoskelet Surg Res 2017;1:25-32. [Google Scholar]
- 8.Ain MC, Andres BM, Somel DS, et al. Total hip arthroplasty in skeletal dysplasias: patient selection, preoperative planning, and operative techniques. J Arthroplasty 2004;19:1-7. [DOI] [PubMed] [Google Scholar]
- 9.Chiavetta JB, Parvizi J, Shaughnessy WJ, Cabanela ME. Total hip arthroplasty in patients with dwarfism. J Bone Joint Surg Am 2004;86-A:298-304. [DOI] [PubMed] [Google Scholar]
- 10.Feibel JB, Steensen RN. Bilateral total knee arthroplasty in an achondroplastic dwarf 43 years after bilateral tibial osteotomies. J Knee Surg 2002;15:39-40. [PubMed] [Google Scholar]
- 11.Helenius I, Remes V, Lohman M, et al. Total knee arthroplasty in patients with diastrophic dysplasia. J Bone Joint Surg Am 2003;85-A:2097-102. [DOI] [PubMed] [Google Scholar]
- 12.Helenius I, Remes V, Tallroth K, et al. Total hip arthroplasty in diastrophic dysplasia. J Bone Joint Surg Am 2003;85-A:441-7. [DOI] [PubMed] [Google Scholar]
- 13.McKeand J, Rotta J, Hecht JT. Natural history study of pseudoachondroplasia. Am J Med Genet 1996;63:406-10. [DOI] [PubMed] [Google Scholar]
- 14.Holschen M, Witt K-A, Steinbeck J. Bilateral stemless shoulder hemiarthroplasty in a female patient suffering from pseudoachondroplasia: A case report. J Orthop Sci 2018. (in press). [DOI] [PubMed] [Google Scholar]
- 15.Pennington SD, Dias CM, Warner JJ. Shoulder arthroplasty in patients with dwarfism: a report of 2 cases. J Shoulder Elbow Surg 2011;20:e1-e6. [DOI] [PubMed] [Google Scholar]
- 16.Budge MD, Lewis GS, Schaefer E, et al. Comparison of standard two-dimensional and three-dimensional corrected glenoid version measurements. J Shoulder Elbow Surg 2011;20:577-83. [DOI] [PubMed] [Google Scholar]
- 17.Iannotti JP, Weiner S, Rodriguez E, et al. Three-dimensional imaging and templating improve glenoid implant positioning. J Bone Joint Surg Am 2015;97:651-8. [DOI] [PubMed] [Google Scholar]
- 18.Alentorn-Geli E, Wanderman NR, Assenmacher AT, et al. Reverse Shoulder Arthroplasty in Weight- Bearing Shoulders of Wheelchair- Dependent Patients: Outcomes and Complications at 2 to 5 years. PM&R 2018;10:607-15. [DOI] [PubMed] [Google Scholar]
- 19.Cuff DJ, Santoni BG. Reverse shoulder arthroplasty in the weight bearing vs. non-weight bearing shoulder: mid-term outcomes with minimum five years of follow-up. Orthopedics 2018;41:e328-33. [DOI] [PubMed] [Google Scholar]
- 20.De Loubresse CG, Norton M, Piriou P, Walch G. Replacement arthroplasty in the weight-bearing shoulder of paraplegic patients. J Shoulder Elbow Surg 2004;13:369-72. [DOI] [PubMed] [Google Scholar]
- 21.Kemp AL, King JJ, Farmer KW, Wright TW. Reverse total shoulder arthroplasty in wheelchair-dependent patients. J Shoulder Elbow Surg 2016;25:1138-45. [DOI] [PubMed] [Google Scholar]


