Abstract
Introduction and importance
The breast angiosarcoma is a rare malignant vascular neoplasm; it represents nearly 0.05% of all breast cancers. Clinically, it could look like a haemangioma or pseudoangiomatous hyperplasia. Here, we report a case of a primary angiosarcoma of the breast (PAB) that mimics a giant fibroadenoma in physical examination and ultrasound features.
Case presentation
A 22 year-old woman came to our hospital complaining of a mobile non-tender mass in her right breast. It was monitored for a while until it became an 8 × 7 cm2. Past medical and family histories were unremarkable. Ultrasonography showed a well circumscribed hypoechoic lobular mass. The wide excision was performed and the pathological study showed angiosarcoma. The patient was re-operated for total mastectomy, screened for distant Metastases and followed-up closely for one year.
Clinical discussion
Fibroadenoma-like lesions are not uncommon and physicians should pay an attention for any breast mass even in the patient who is young and has no risk factors of the traditional breast cancer. PAB is used to be missed in the clinical practice over the world; it is extremely rare and is proved by Immunohistochemistry. The full management could be totally completed by a mastectomy with/out axillary node dissection.
Conclusion
The primary angisarcoma of the breast (PAB) could resemble a fibroadenoma in pre-operative investigations. In many reviews, PAB mimicked many diseases. Thus, the medical literature needs more case reports and series to identify an ideal protocol of diagnosis and management.
Keywords: Breast angiosarcoma, Fibroadenoma, Breast lesion work-up
Abbreviations: PAB, Primary angiosarcoma of breast; T1W, T1-weighted; T2W, T2-weighted; USG, Ultrasonography; 18F-FDG PET/CT scan, 18F-fluorodeoxyglucose positron emission tomography/computed tomography scan; FNA, Fine needle biopsy
Highlights
-
•
Breast angiosarcoma still causes a diagnostic problem in young women.
-
•
Clinically presentation and ultrasound features could mimic fibroadenoma.
-
•
Pathological findings and immunohistochemistry make the definitive diagnosis.
-
•
Young women shouldn't ignore the following-up of any breast lump.
1. Introduction
This work has been reported in line with the SCARE 2020 criteria [1]. Primary angiosarcoma of the breast (PAB) is a rare malignant vascular neoplasm that originates from endothelial cells without any known risk factors, it represents nearly 0.05% of all breast cancers [2], and has a predilection for young women aged between 20 and 40 years [3]. Angiosarcoma can also arise secondarily following breast radiation [4].
Commonly, this type of sarcoma could be undetected pre-operatively; mammograms may appear completely normal in one-third of PAB cases with minor observations of skin thickening [5], Ultrasonography features are non-specific and on MRI the tumor tends to have low intensity on T1W and high intensity on T2W images [5].
Furthermore, there are no characteristic pathological imaging features for angiosarcoma; it may be misdiagnosed as a benign lesion such as a haemangioma or pseudoangiomatous hyperplasia [2]. So, immunohistochemistry plays the main role in making the definitive diagnosis and arranging the useful management.
Here, we report a case of PAB that presented with benign features. Full medical history, physical examination and ultrasonography findings directed the primary physician to deal with the lesion as a fibroadenoma; the patient was reassured until the mass became a giant (>5 cm) and then she was operated.
2. Case presentation
A 22 year-old woman came to our hospital complaining of a palpable mass in her right breast. The patient had full-examined and reassured by her primary physician for months as the detected mass had been named a fibroadenoma. Later, she stated that the mass enlarged remarkably. She didn't mention any risk factor in her medical or family histories. Also, there was no predicted cause of the mass by previous intervention, drugs or trauma.
By physical examination, we found a mobile, non-tender mass measuring about 8 × 7 cm2 with an important asymmetry at the expense of upper-outer area of the right breast. No nipple retraction, lymphadenopathy, nodules or discoloration of the skin was evident (Fig. 1).
Fig. 1.
Mobile and non-tender mass in the right breast. The asymmetry is clear. No nipple retraction, nodules or discoloration of the skin.
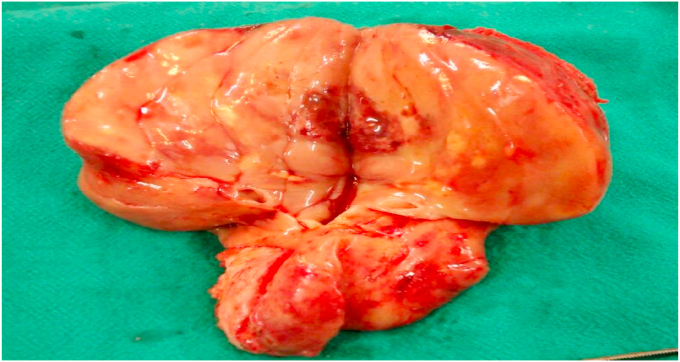
Ultrasonography showed a well circumscribed, hypoechoic lobular mass measuring 8.5 × 7 cm2. According to this presentation, the fibroadenoma was suggested as an expected diagnosis. The excision of whole mass was planned and then performed under general anesthesia, it showed lobulated tan-gray tissue with small foci of necrosis and ill-defined borders (Fig. 2).
Fig. 2.
Lobulated tan-gray tissue with small foci of necrosis.
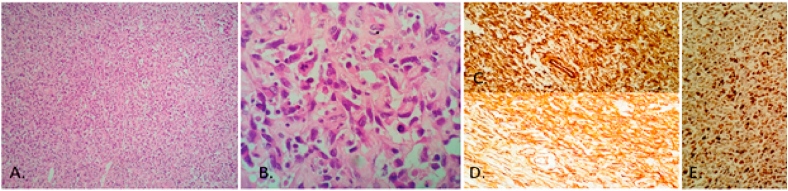
Microscopically, we figure out a hypercellular tumor composed of proliferated spindled and epithelioid large atypical cells having large pleomorphic nuclei with coarse chromatin and frequent mitoses. The tumor growth formed alveolar pattern and solid areas, foci of tumor necrosis were also present (Fig. 3; A &B). Immunohistochemistry revealed negative result for CD117, Desmin, S100, SMA, and CK7, but there was a strong positive staining for Vimentin and CD34 (vascular endothelial markers). Ki-67 revealed very high index (>50%) (Fig. 3; C, D &E).
Fig. 3.
A. H&E, Low power field, alveolar growth of spindle and epithelioid large atypical cells, B. H&E, High power view, prominent mitotic activity, C. Anti-Vimentin positive staining, D. Anti-CD34 positive staining. E. Ki-67: High index.
These descriptions were unique for an angiosarcoma. 18F-FDG PET, chest and abdominal computed tomography (CT) scan denied any distant metastasis. Total mastectomy with free surgical and pathological margins was done. After one year, no recurrence or metastases were detected.
3. Discussion
Breast angiosarcoma is a rare neoplasm that accounts for almost 1% of all soft tissue breast tumors [6]. It can be primary (about 0.05% of all primary breast malignancies) or secondary that arises mostly in the presence of antecedent radiotherapy or chronic lymphedema after radical mastectomy [3, 4]].
Reviewing PubMed Library in the last decade shows that PAB mimicked benign haemangioma [7], lactating tubular adenoma [8], acute mastitis [9] and fibroadenoma (but it progressed later a nipple retraction) [10].
Additionally, Angiosarcomas have variable features on ultrasound examination and these may present as well-circumscribed or poorly marginated masses. They could be hypoechoic or have mixed echogenicity on ultrasonography (USG) [10]. Unfortunately, fibroadenomas usually present as hypoechoic, well circumscribed encapsulated lesions on USG [10]. That makes the angiosarcoma as an extremely rare differential diagnosis of fibroadenoma [5].
When the diagnosis of PAB is highly suspicious, MRI has an important value in distinguishing hypervascular, hemorrhagic, and heterogeneous masses [11]. Although that core needle biopsy plays the most important role in the diagnosis pre-surgery, it might be difficult to be performed due to the vascular nature of the tumor [12].
Total mastectomy with or without axillary node dissection is the preferred surgical treatment [13]. Metastases are usually hematogenous to the lungs, liver, bones, skin and the contralateral breast [14], and because of the rarity of breast angiosarcoma, randomized trials of adjuvant radiotherapy or chemotherapy are not yet available and the efficacy of this therapy still lacks evidence [15].
4. Conclusion
Physicians should pay an attention for any breast mass even in the patient who is young and has no risk factors of the traditional breast cancer. In our case, a primary angiosarcoma in the breast of resembled a fibroadenoma in pre-operative investigations. In many reviews, PAB mimicked many diseases. Thus, the medical literature needs more case reports and series to identify an ideal protocol of diagnosis and management.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Ethical approval
Informed consent was taken for this case report. Our study ethical aspects were reviewed and approved by Damascus University deanship, Damascus, Syria.
Sources of funding
No funding was received for this study.
Author contribution
All the authors made an equal contribution to the creation of the presented clinical case.
Muhammad Alshaar, Mahmoud Alkhatib, Samer Sara, Mhd Belal Alsabek.
Consent
The consent was obtained from the patient for medical publishing purposes, all the information including images. A copy of the written consent is available for review by the editors of this journal.
Registration of research studies
Not applicable.
Our manuscript is a case report.
Guarantor
Mhd Belal Alsabek.
Declaration of competing interest
The authors declare that there is no conflict of interests regarding the publication of this paper.
Contributor Information
Muhammad Alshaar, Email: muhamma.alshaar87@gmail.com.
Mahmoud Alkhatib, Email: mahmoudalkhatib42@gmail.com.
Samer Sara, Email: samersara976@gmail.com.
Mhd Belal Alsabek, Email: drsabekb@gmail.com.
References
- 1.Agha R.A., Franchi T., Sohrabi C., Mathew G. The SCARE 2020 guideline: updating consensus surgical case report (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 2.Bordoni D., Bolletta E., Falco G., Cadenelli P., Rocco N., Tessone A., Guarino S., Accurso A., Amato B., Magalotti C. Primary angiosarcoma of the breast. Int J Surg Case Rep. 2016;20S:12–15. doi: 10.1016/j.ijscr.2016.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang X.Y., Jakowski J., Tawfik O.W., Thomas P.A., Fan F. Angiosarcoma of the breast: a clinicopathologic analysis of cases from the last 10 years. Ann. Diagn. Pathol. 2009;13(3):147–150. doi: 10.1016/j.anndiagpath.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 4.Hui A., Henderson M., Speakman D., Skandarajah A. Angiosarcoma of the breast: a difficult surgical challenge. Breast. 2012;21(4):584–589. doi: 10.1016/j.breast.2012.01.001. [DOI] [PubMed] [Google Scholar]
- 5.Varghese B., Deshpande P., Dixit S., Koppiker C.B., Jalnapurkar N. Primary angiosarcoma of the breast: a case report. J. Radiol. Case Rep. 2019;13(2):15–25. doi: 10.3941/jrcr.v13i2.3449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arora T.K., Terracina K.P., Soong J., Idowu M.O., Takabe K. Primary and secondary angiosarcoma of the breast. Gland Surg. 2014;3(1):28–34. doi: 10.3978/j.issn.2227-684X.2013.12.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bennani A., Chbani L., Lamchahab M., Wahbi M., Alaoui F.F., Badioui I. Primary angiosarcoma of the breast: a case report. Diagn. Pathol. 2013;8:66. doi: 10.1186/1746-1596-8-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abbad F., Idrissi N.C., Fatih B., Fakhir B., Drissi J., Khouchani M., Rais H. Primary breast angiosarcoma: a rare presentation of rare tumor - case report. BMC Clin. Pathol. 2017;17:17. doi: 10.1186/s12907-017-0055-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mumin N.A., Rahmat K., Hamid M.T.R., Lin N.W., Yee C.W., Ying C.X., Hoong S.M., Har Y.C. Primary breast angiosarcoma: utilisation of pre-surgical magnetic resonance imaging (MRI) for accurate tumour characterization and planning - a case report and literature review. Curr Med Imaging. 2020 doi: 10.2174/1573405616666201007161119. [DOI] [PubMed] [Google Scholar]
- 10.Taghipour Z.S., Sefidrokh S.N., Rahmani K. Primary breast angiosarcoma: pathological and radiological diagnosis. Malays. J. Med. Sci. 2014;21(5):66–70. [PMC free article] [PubMed] [Google Scholar]
- 11.Yang Wei Tse, Bryan T., Hennessy J., Mark Dryden J., Valero Vicente, Savitri Krishnamurthy. Mammary angiosarcomas: imaging findings in 24 patients. Radiology. 2007 Mar;242(3):725–734. doi: 10.1148/radiol.2423060163. [DOI] [PubMed] [Google Scholar]
- 12.Assalia A., Schein M. Severe haemorrhagic complication following needle or open biopsy of a breast mass: suspect angiosarcoma. Br. J. Surg. 1992;79:469. doi: 10.1002/bjs.1800790525. [DOI] [PubMed] [Google Scholar]
- 13.Kaklamanos I.G., Birbas K., Syrigos K.N., Vlachodimitropoulos D., Goutas N., Bonatsos G. Breast angiosarcoma that is not related to radiation exposure: a comprehensive review of the literature. Surg. Today. 2011;41(2):163–168. doi: 10.1007/s00595-010-4341-x. [DOI] [PubMed] [Google Scholar]
- 14.Bhosale S.J., Kshirsagar A.Y., Patil M.V., Wader J.V., Nangare N., Patil P.P. Primary angiosarcoma of breast: a case report. Int J Surg Case Rep. 2013;4(4):362–364. doi: 10.1016/j.ijscr.2013.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sasahara A., Tanabe M., Hayashi K., Konishi T., Oya M., Sakiyama K., Morizono A., Harada M., Otsuji K., Ishibashi Y., Sato A., Kikuchi Y., Niwa T., Hinata M., Nishioka K., Seto Y. A case of primary breast angiosarcoma with multiple discontinuous small lesions. Surg Case Rep. 2019 Oct 25;5(1):157. doi: 10.1186/s40792-019-0704-8. [DOI] [PMC free article] [PubMed] [Google Scholar]