Abstract
Cerebellar tonsillar descent can be seen on head magnetic resonance imaging in both Chiari malformation type 1 and spinal cerebrospinal fluid leak creating the potential for misdiagnosis. We report five cases of spinal cerebrospinal fluid leak at Stanford University initially misdiagnosed and treated as Chiari malformation type 1 based on cerebellar tonsillar descent demonstrated on imaging. All five cases had sustained relief at the 6-month follow up visit from epidural blood patches for the treatment of spinal cerebrospinal leak after unsuccessful suboccipital decompression surgeries. A misdiagnosis of Chiari malformation type 1 in patients with spinal cerebrospinal fluid leak may lead to unnecessary surgeries instead of the less invasive treatment, such as epidural blood patches. It is imperative to consider a spinal cerebrospinal fluid leak in the differential based on clinical-radiological correlation and not solely on cerebellar tonsillar descent demonstrated on imaging.
Keywords: Cerebrospinal fluid leak, Chiari malformation type 1, Cerebellar tonsillar descent, Chronic headaches, Orthostatic headaches
Cerebrospinal fluid leak, Chiari malformation type 1, cerebellar tonsillar descent, chronic headaches, orthostatic headaches
1. Introduction
A spinal cerebrospinal fluid (sCSF) leak occurs when a dural defect causes cerebrospinal fluid (CSF) to flow into the extradural space. It can lower the CSF pressure within the intradural space, and the resultant intracranial hypotension (IH) is an important differential diagnosis to consider in patients presenting with chronic headaches. IH can often be confused with other chronic headache disorders, including Chiari Malformation Type 1 (CM) [1]. CM is a disorder related to abnormally low-positioned cerebellar tonsils with disruption of normal CSF flow dynamics at the craniocervical junction [2]. Cerebellar tonsillar descent (TD) can be seen on head imaging such as magnetic resonance imaging (MRI) in both CM and a sCSF leak. We present 5 patients with sCSF leaks misdiagnosed initially as CM based on TD (greater than 3mm below the foramen magnum) demonstrated on imaging.
2. Case reports
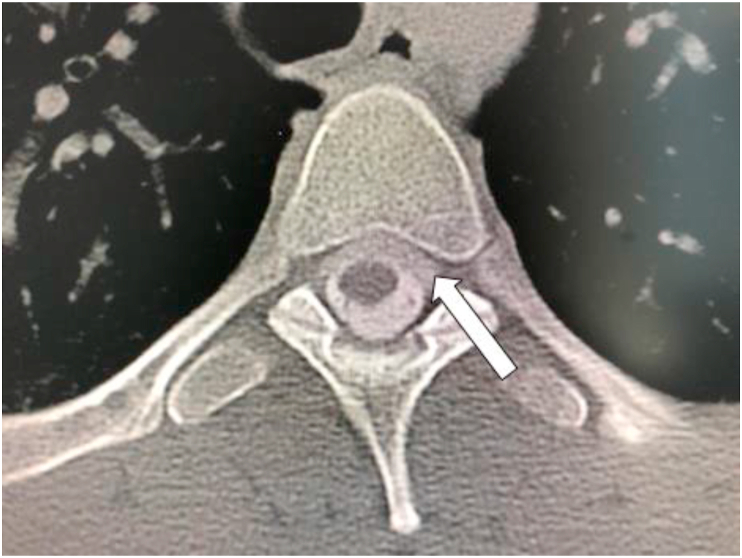
A 25-year-old female presented with a 10-year history of headaches. Her medical history was significant for migraine. MRI head demonstrated TD (Figure 1a) and she was diagnosed with CM. She received two suboccipital decompression surgeries resulting in no relief. A sCSF leak was suspected based on her history of worsening headaches upon standing. Computed tomography myelography (CTM) demonstrated extradural contrast spread at multiple cervical and thoracic levels (Table 1) (Figure 2). Multi-level targeted epidural autologous blood patches (EBPs) resulted in immediate symptom improvement.
Figure 1.
a, b, c, d: MRI Head (T1 Sagittal FLAIR sequence) demonstrated inferior displacement of the cerebellar tonsils. (Case 1–4).
Table 1.
Summary.
| Case | Age (Sex) | PMH | Orthostatic Headache (worse upright) | MRI | CTM | Intervention | Outcome: Headache improvement∗ |
|---|---|---|---|---|---|---|---|
| 1 | 25 (F) | Migraine | Yes | CTD | Multiple spinal level contrast spread at level C6-T1, T4-5, T7-8 level | Multi-level EBPs | Yes |
| 2 | 26 (F) | EDS, POTS | Yes | CTD | Multiple nerve root sleeves enhancement from C4 to T1, and T6 to L4 Opening pressure -4cm H20 |
Multi-level EBPs | Yes |
| 3 | 57 (F) | EDS, migraine | Yes | CTDa | Multiple nerve root sleeves enhancement from T7-S3 | Multi-level EBPs | Yes |
| 4 | 29 (M) | Alcohol Dependence | Yes | CTD | Multiple nerve root sleeves enhancement from T11-S1 | Multi-level EBPs | Yes |
| 5 | 41 (F) | POTS | Yes | CTDb | Negative∗∗ | Surgical repair | Yes |
PMH: Past Medical History MRI: Magnetic Resonance Imaging CTM: Computed Tomography Myelogram.
EDS: Ehler Danlos Syndrome POTS: Postural Orthostatic Tachycardia Syndrome CTD: Cerebellar tonsillar descent EBPs: Epidural blood patches.
Duration, intensity, orthostatic features, concomitant symptoms at the 6-month follow up visit.
Digital subtraction myelography – CSF venous fistula arising on the left at T4 and T5.
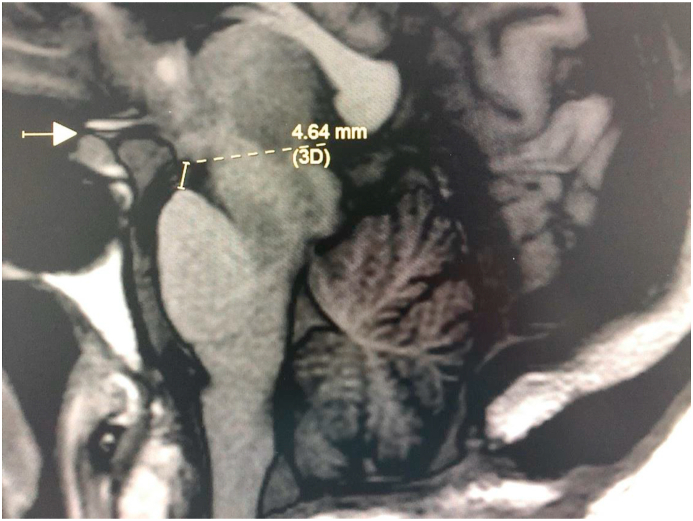
MRI also demonstrated reduced mamillopontine distance of 4.64 mm, abnormal pontomesencephalic angle less than 50°, convex pituitary with near complete effacement of the suprasellar cistern.
MRI also demonstrated TD, crowding of the posterior fossa, pituitary enlargement and effacement of the basilar cisterns.
Figure 2.
Computed tomography myelogram (axial view) demonstrated a ventral cervicothoracic epidural CSF collection (arrow) extending from the mid cervical spine to mid thoracic level. (Case 1).
A 26-year-old female presented with a 17-year history of headaches, neck pain and tinnitus following a motor vehicle accident at age 9. Her medical history was significant for Ehler-Danlos Syndrome (EDS) and Postural Orthostatic Tachycardia Syndrome (POTS). CM was diagnosed initially based on an MRI head demonstrating TD (Figure 1b). Suboccipital decompression surgery was unsuccessful. A sCSF leak was suspected based on the orthostatic feature of her headaches (worse upright) and the lack of response to surgery. CTM demonstrated multiple nerve root sleeves enhancement from cervical to lumbar levels (Table 1). Opening pressure was measured at 4 cm H20. Multi-level targeted EBPs resulted in symptom improvement immediately.
A 57-year-old female presented with a 30-year history of orthostatic headaches, neck pain, visual disturbance and imbalance. Her medical history was significant for EDS, migraine and orthostatic hypotension. MRI head demonstrated TD (Figure 1c) and a reduced mamillopontine distance of 4.64 mm, abnormal pontomesencephalic angle less than 50°, convex pituitary with near complete effacement of the suprasellar cistern. A sCSF leak was suspected based on the unsuccessful suboccipital decompression surgery and clinical-radiographic features of IH. CTM demonstrated multiple nerve root sleeves enhancement from thoracic to sacral levels (Table 1). EBPs targeted between T7-S3 resulted in symptom improvement immediately.
A 29-year-old male suffered from orthostatic headaches and tinnitus for 2 years without a clear inciting event. His medical history was significant for alcohol dependence. MRI head demonstrated TD (Figure 1d) and he underwent suboccipital decompression surgery 1 year after symptom onset without relief. CTM demonstrated multiple nerve roots sleeve enhancement from thoracic to sacral levels (Table 1) with transverse process fractures at L1 and sharp edge osteophyte at T11. A sCSF leak was suspected and EBPs targeted at T11 and L1 resulted in symptom resolution immediately.
A 41-year-old female presented with a 15-year history of orthostatic and suboccipital headaches without a clear inciting event. Her medical history was significant for POTS. MRI head demonstrated TD, crowding of the posterior fossa, pituitary enlargement and effacement of the basilar cisterns. A suboccipital decompression surgery was unsuccessful. CTM did not demonstrate evidence of a leak and blind EBPs proved ineffective. She underwent digital subtraction myelography of the thoracic spine, which demonstrated a CSF-venous fistula arising on the left at T4-5 region (Figure 3). Surgical repair resulted with symptom resolution.
Figure 3.
Digital subtraction myelogram (lateral decubitus position) demonstrated venous spread of contrast via CSF venous fistula. (Case 5).
At the 6-month follow-up visit, all 5 patients demonstrated sustained symptom relief without recurrence of symptoms. Please refer to Table 1 for a summary of the cases. It is to be noted that the orthostatic feature of the headaches was not clearly obtained or elicited prior to CM decompression surgeries for the 5 patients. Prior to suboccipital decompression surgeries, all 5 patients had orthostatic headaches and worsening of existing headaches associated with Valsalva maneuvers, such as coughing, but not “new onset” headaches. Post-operatively, the headache characteristics for the patients remain unchanged.
Written consent for publication was obtained from each patient.
3. Discussion
While CM and sCSF leak each have distinct clinical presentations, there are overlapping symptoms, such as chronic headaches that make it challenging to differentiate between the two conditions. The accompanying headache with sCSF leak has been variously described as an orthostatic headache, second half of the day headache [3], constant headache [4, 5, 6, 7]. In a study of children with CM and its associated symptoms, the most common symptom was pain, especially in the neck/occipital area [2]. Some types of headaches that CM patients experience are short attacks of “cough-headache,” migraine phenotype, long lasting headaches, and headaches that worsen with Valsalva maneuvers, physical exertion, head dependency, and sudden posture changes [2].
Headache with orthostatic features is the hallmark of symptomatic sCSF leak and most recognizably occurs within thirty minutes of standing and disappears within thirty minutes of lying down at least at initial presentation [8]. Steps can be taken to properly assess for a suspected leak, because orthostatic headaches and associated symptoms should improve after prolonged recumbency, especially early on in the disease course [8].
When evaluating a patient with radiologic evidence of TD, other MRI features can help build suspicion that the patient has IH due to a leak, including pachymeningeal enhancement (MRI with contrast), pituitary hyperemia, subdural collections and venous engorgement [8, 9]. Pachymeningeal enhancement is the most specific head imaging finding for IH due to a sCSF leak [9]. Recent studies have provided quantitative measures with a suprasellar cistern less than 4mm, mamillopontine distance less than 6.5 mm and prepontine cistern less than 5 mm (illustrated in Case 3, Figure 4), all predicting an increased likelihood of finding a leak with spinal imaging [10]. The reduced mamillopontine distance and abnormal pontomesecephalic angle (Case 3), crowding of the posterior fossa and pituitary enlargement and effacement of the basilar cisterns (Case 5) were features identified retrospectively and were not reported initially. Other radiographic clues associated with CM include syringomyelia and tethered cord which are not commonly seen in a sCSF leak [2]. In addition, recent evidence has suggested that reduced clivus volume and increased sphenoid sinus volume are associated with CM [11]. These findings were absent in all 5 patients. The initial diagnostic work-up to differentiate between the two conditions should include an MRI head with and without contrast and an MRI full spine [8]. It is prudent to provide all clinical details to the radiologists, including the differential diagnoses in consideration, so these supporting radiographic features could be assessed.
Figure 4.
MRI Head (T1 Sagittal FLAIR sequence): Arrow: Effacement of suprasellar cistern above convex pituitary surface. Dotted line: Reduced mamillopontine distance less than 6.5 mm. Previous Chiari decompression and cerebellar tonsillar descent noted. (Case 3).
There has been a previously published case report of identifying a sCSF leak after suboccipital decompression for presumed CM failed to resolve symptoms. A 12-year-old girl with Marfan's syndrome and sacral dural ectasia had occipital and biparietal orthostatic headaches, a waning appetite, nausea when upright, and tonsillar herniation. She went through a decompression surgery for her foramen magnum, which did not help her condition. Radiographic imaging demonstrated a possible sCSF leak and she underwent an autologous EBP. All symptoms resolved over the next 15 months [12]. A number of authors have reported sCSF leaks masquerading as CM, but primarily describe this in terms of mishaps avoided. They describe how they nearly treated CM with suboccipital decompression, but realized they were dealing with a sCSF leak prior to engaging in surgery [13, 14, 15].
Since the neurosurgical procedures were performed in the peripheral centers, one of the major limitations to these cases are the lack of neurosurgical details available in terms of the initial decision making, type of surgeries performed and the rationale in proceeding to surgeries. Secondly, 4 out of the 5 patients did not have an opening pressure measured from their CTM. Although these were unavailable, other clinical and radiographic features discussed were suggestive of a sCSF leak. An opening pressure of less than 6 cm H20 is suggestive of a sCSF leak [8], however patients with a chronic leak can have a normal opening pressure due to a compensatory mechanism [8]. A low opening pressure should be regarded as specific, but not sensitive [8, 9]. The retrospective nature and the small case series are major limitations to this study. While one could postulate there are a number of existing cases of patients with sCSF leak who were initially misdiagnosed with CM, there is no data on trends in these misdiagnoses as this study only identified the patients who were seen at the headache clinic.
4. Conclusion
A misdiagnosis of CM in patients with sCSF leak may lead to unnecessary surgeries instead of a less invasive treatment, such as EBPs. Therefore, it is imperative to consider a sCSF leak in the differential based on clinical-radiological correlation and not solely on TD demonstrated on imaging. This type of misdiagnosis can largely be avoided with proper pre-surgical evaluation via a comprehensive anamnesis and examination in combination with suitable radiographic diagnostic imaging. Future studies should explore a larger database of patients who failed CM decompression surgeries with radiographic TD and identify the prevalence and common clinical-radiologic features of this population.
Declarations
Author contribution statement
All authors listed have significantly contributed to the investigation, development and writing of this article.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
Data will be made available on request.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
References
- 1.Mokri B. Spontaneous CSF leaks: low CSF volume syndromes. Neurol. Clin. 2014 May 1;32(2):397–422. doi: 10.1016/j.ncl.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 2.Mea E., Chiapparini L., Leone M., Franzini A., Messina G., Bussone G. Chronic daily headache in the adults: differential diagnosis between symptomatic Chiari I malformation and spontaneous intracranial hypotension. Neurol. Sci. 2011 Dec;32(Suppl 3):S291–S294. doi: 10.1007/s10072-011-0698-x. [DOI] [PubMed] [Google Scholar]
- 3.Leep Hunderfund A.N., Mokri B. Second-half-of-the-day headache as a manifestation of spontaneous CSF leak. J. Neurol. 2012 Feb;259(2):306–310. doi: 10.1007/s00415-011-6181-z. [DOI] [PubMed] [Google Scholar]
- 4.Schievink W.I., Smith K.A. Nonpositional headache caused by spontaneous intracranial hypotension. Neurology. 1998 Dec;51(6):1768–1769. doi: 10.1212/wnl.51.6.1768. [DOI] [PubMed] [Google Scholar]
- 5.Mea E., Chiapparini L., Savoiardo M., Franzini A., Bussone G., Leone M. Clinical features and outcomes in spontaneous intracranial hypotension: a survey of 90 consecutive patients. Neurol. Sci. 2009 May;30(Suppl 1):S11–S13. doi: 10.1007/s10072-009-0060-8. [DOI] [PubMed] [Google Scholar]
- 6.Ferrante E., Savino A. Nonpostural headache by spontaneous intracranial hypotension. Headache. 2003 Feb;43(2):127–129. doi: 10.1046/j.1526-4610.2003.03030.x. [DOI] [PubMed] [Google Scholar]
- 7.Wang S.-J., Fuh J.-L. Exertional but not postural headache resulting from spontaneous intracranial hypotension. Acta Neurol. Taiwan. 2005 Mar;14(1):36–37. [PubMed] [Google Scholar]
- 8.Schievink W.I. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. JAMA. 2006 May 17;295(19):2286–2296. doi: 10.1001/jama.295.19.2286. [DOI] [PubMed] [Google Scholar]
- 9.Kranz P.G., Tanpitukpongse T.P., Choudhury K.R., Amrhein T.J., Gray L. Imaging signs in spontaneous intracranial hypotension: prevalence and relationship to CSF pressure. AJNR Am. J. Neuroradiol. 2016 Jul;37(7):1374–1378. doi: 10.3174/ajnr.A4689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dobrocky T., Grunder L., Breiding P.S., Branca M., Limacher A., Mosimann P.J. Assessing spinal cerebrospinal fluid leaks in spontaneous intracranial hypotension with a scoring system based on brain magnetic resonance imaging findings. JAMA Neurol. 2019 Feb 18 doi: 10.1001/jamaneurol.2018.4921. [Internet] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nwotchouang B.S.T., Eppelheimer M.S., Bishop P., Biswas D., Andronowski J.M., Bapuraj J.R. Three-dimensional CT morphometric image analysis of the clivus and sphenoid sinus in chiari malformation type I. Ann. Biomed. Eng. 2019 Nov;47(11):2284–2295. doi: 10.1007/s10439-019-02301-5. [DOI] [PubMed] [Google Scholar]
- 12.Puget S., Kondageski C., Wray A., Boddaert N., Roujeau T., Di Rocco F. Chiari-like tonsillar herniation associated with intracranial hypotension in Marfan syndrome [Internet] J. Neurosurg. Pediatr. 2007;106:48–52. doi: 10.3171/ped.2007.106.1.48. [DOI] [PubMed] [Google Scholar]
- 13.Yoshimoto S., Takai K., Takahashi K., Yasui T., Taniguchi M. Intracranial hypotension and hypertension: reversible Chiari malformation due to dynamic cerebrospinal fluid abnormalities in Gorham-Stout disease. Case report. J. Neurosurg. Pediatr. 2018 Nov 1;22(5):508–512. doi: 10.3171/2018.5.PEDS1859. [DOI] [PubMed] [Google Scholar]
- 14.Hatae R., Kohri R., Maeda K., Miyazono M. A rare case of chiari type-1 malformation accompanied by symptomatic cerebrospinal fluid hypovolemia: comparison of congenital chiari type-1 malformation and acquired chiari malformation secondary to cerebrospinal fluid hypovolemia: case report [Internet] Neurol. Med.-Chir. 2014;54:558–562. doi: 10.2176/nmc.cr.2013-0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Samii C., Möbius E., Weber W., Heienbrok H.W., Berlit P. Pseudo Chiari type I malformation secondary to cerebrospinal fluid leakage. J. Neurol. 1999 Mar;246(3):162–164. doi: 10.1007/s004150050327. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.